Published online Dec 25, 2024. doi: 10.5501/wjv.v13.i4.98551
Revised: August 14, 2024
Accepted: September 2, 2024
Published online: December 25, 2024
Processing time: 111 Days and 6.2 Hours
Vaccine hesitancy is a major challenge in the fight against the coronavirus disease 2019 (COVID-19) pandemic. Identifying the sociodemographic factors associated with vaccine acceptance among Nigerians is crucial for improving vaccine uptake.
To assess the acceptance rate of COVID-19 vaccine and its related determinants among Nigerians.
An online cross-sectional survey (observational study) was conducted between February 2021 and May 2021, using a questionnaire hosted on SurveyMonkey. The invitation to take part in the poll was sent out to participants through social networking platforms. A logistic regression was used to determine which sociodemographic factors were associated with vaccine acceptance constructs.
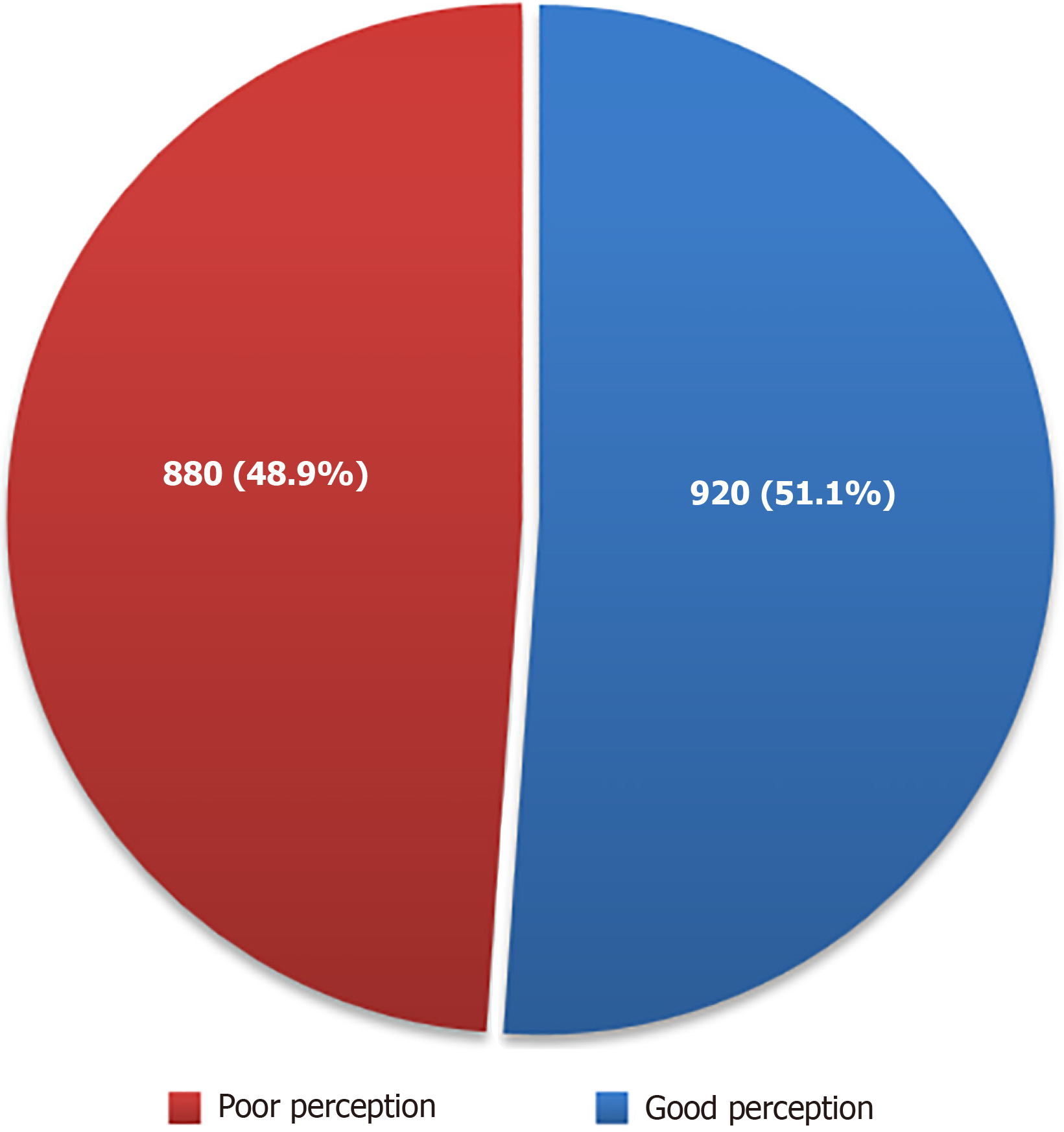
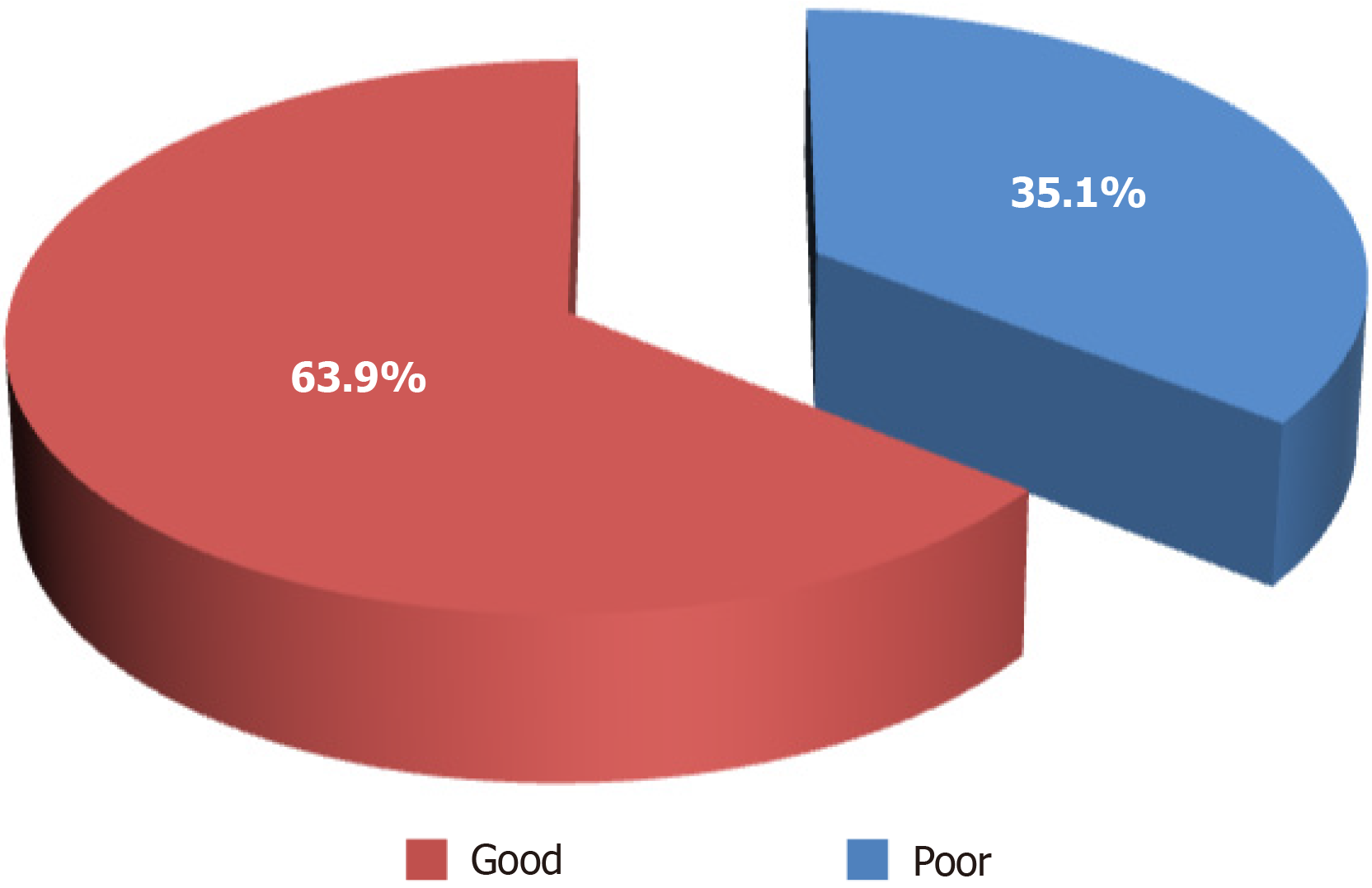
A total of 1800 persons responded to the survey, a larger proportion of whom were males (53.9%) and within the age group of 21-30 years (29.4%) and earned an average income of less than $500 per month (43.3%). Only 0.56% of participants had a high perceived risk of COVID-19 infection, while only 1.11% had a perceived risk of dying from COVID-19. The perception rate of the COVID-19 vaccine among participants was 51.1%, while the acceptance rate was 63.9%. There was no significant association between the COVID-19 vaccine acceptance rate and related determinants assessed, particularly age (χ² = 3.049, P = 0.550), sex (χ² = 0.102, P = 0.749), average income (χ² = 3.802, P = 0.875), and religion (χ² = 2.819, P = 0.420). Participants with chronic conditions demonstrated a higher acce
Despite the positive perception observed and substantial vaccine acceptance rate among the study participants, more public health interventions are still needed to enhance vaccine acceptability in Nigeria.
Core Tip: This study assessed coronavirus disease 2019 vaccine acceptance among Nigerians through an online survey with 1800 respondents. Despite a substantial acceptance rate of 63.9%, sociodemographic factors (age, sex, income, and religion) did not significantly influence vaccine uptake. Positive perceptions of vaccination were common, yet financial barriers af
- Citation: Ezigbo ED, Enitan SS, Adejumo EN, Durosinmi AE, Akele RY, Dada MO, Itodo GE, Idoko AM, Edafetanure-Ibeh OM, Okafor EN, Abdulsalam AA, Oyedoyin OI, Yelpoji PU, Opeyemi OO, Nmesomachi OS, Oyekale AO, Onyeji CB. Acceptance of COVID-19 vaccine and its related determinants in Nigeria: An online survey. World J Virol 2024; 13(4): 98551
- URL: https://www.wjgnet.com/2220-3249/full/v13/i4/98551.htm
- DOI: https://dx.doi.org/10.5501/wjv.v13.i4.98551
The coronavirus disease 2019 (COVID-19), which first surfaced in China in December 2019 and has since spread to pra
Vaccination is one of the most cost-effective methods for preventing and controlling infectious diseases. However, certain individuals and segments of the public are opposed to vaccination[9]. The volume of knowledge on why indi
Patients are more likely to get vaccinated and are less hesitant if medical workers have a positive attitude toward vaccines[17]. The level of knowledge and attitude regarding immunization that healthcare professionals have will impact their likelihood of using it and promoting it to their patients. Since healthcare workers are on the front lines of the current epidemic, governments have prioritized immunizing them first. However, there have been increasing cases of vaccine refusal[18,19]. Policymakers, academics, and health officials need to understand how well the COVID-19 vaccine is accepted by healthcare workers and what influences their acceptance or rejection to develop effective strategies to reduce vaccination hesitancy. While more than half of the world’s population (59.5%) has received the COVID-19 vaccine, significant disparities in immunization rates persist across nations[20,21]. The Horn of Africa has the world’s lowest immunization rate, at less than 20%. Delays in vaccination may be due to perceived dangers, religious beliefs, and inadequate information and awareness[22].
Understanding the factors influencing vaccine acceptance is essential not only for managing the COVID-19 pandemic but also for addressing future infectious diseases that require vaccination. Insights gained from studying COVID-19 vaccine acceptance can inform strategies to enhance vaccine uptake for other infectious diseases, thereby improving global health outcomes.
Hypothesis 1: Sociodemographic factors such as age, sex, income, and religion are significant predictors of COVID-19 vaccine acceptance among Nigerians.
Hypothesis 2: Individuals with chronic conditions in Nigeria are more likely to accept the COVID-19 vaccine compared to those without chronic conditions.
This observational study collected data on COVID-19 vaccine acceptance and related sociodemographic factors, without manipulating any variables or providing interventions.
Setting/period: The nation-wide online web-based survey was conducted from February 1, 2021 to May 31, 2021.
Cross-sectional: The data was collected at a single point in time, providing a snapshot of the population’s attitudes and behaviors during the survey period.
Target population: The Nigerian populace.
Inclusion/exclusion criteria: Consenting respondents with access to the internet participated in the online survey.
Survey instrument: The questionnaire was hosted on SurveyMonkey, designed to gather information on vaccine ac
Mode of distribution: The invitation to participate was disseminated via social networking platforms, including Fa
Validity of the instrument: To ensure the validity of the instrument, both face and content validity were assessed. Experts in public health and survey methodology reviewed the questionnaire to ensure it was appropriate and comprehensive for the study objectives. Demographic information was collected to identify potential sampling biases, including differences between participants and non-participants. This helped address the potential bias that might arise from the selective participation of certain demographic groups.
Independent variables: Sociodemographic factors such as age, sex, income, religion, and the presence of chronic conditions.
Dependent variable: COVID-19 vaccine acceptance, measured as the primary outcome.
Other variables: Perceived risk of infection and death from COVID-19.
The data for this study were sourced from an online cross-sectional survey conducted between February 2021 and May 2021. The survey was hosted on SurveyMonkey, and participants were recruited through social networking platforms, which facilitated broad access across the Nigerian population.
COVID-19 vaccine acceptance: Vaccine acceptance was assessed using specific questions within the survey designed to capture participant willingness to receive the COVID-19 vaccine. This was measured as a categorical variable, with par
Sociodemographic factors: These variables (age, sex, income, and religion) were self-reported by participants through the survey. Age was captured in predefined categories (e.g., 21-30 years), sex was reported as male or female, income was categorized based on monthly earnings (e.g., less than $500 per month), and religion was also categorized (e.g., Chri
Chronic conditions: Participants were asked if they had any chronic health conditions, with the presence of such con
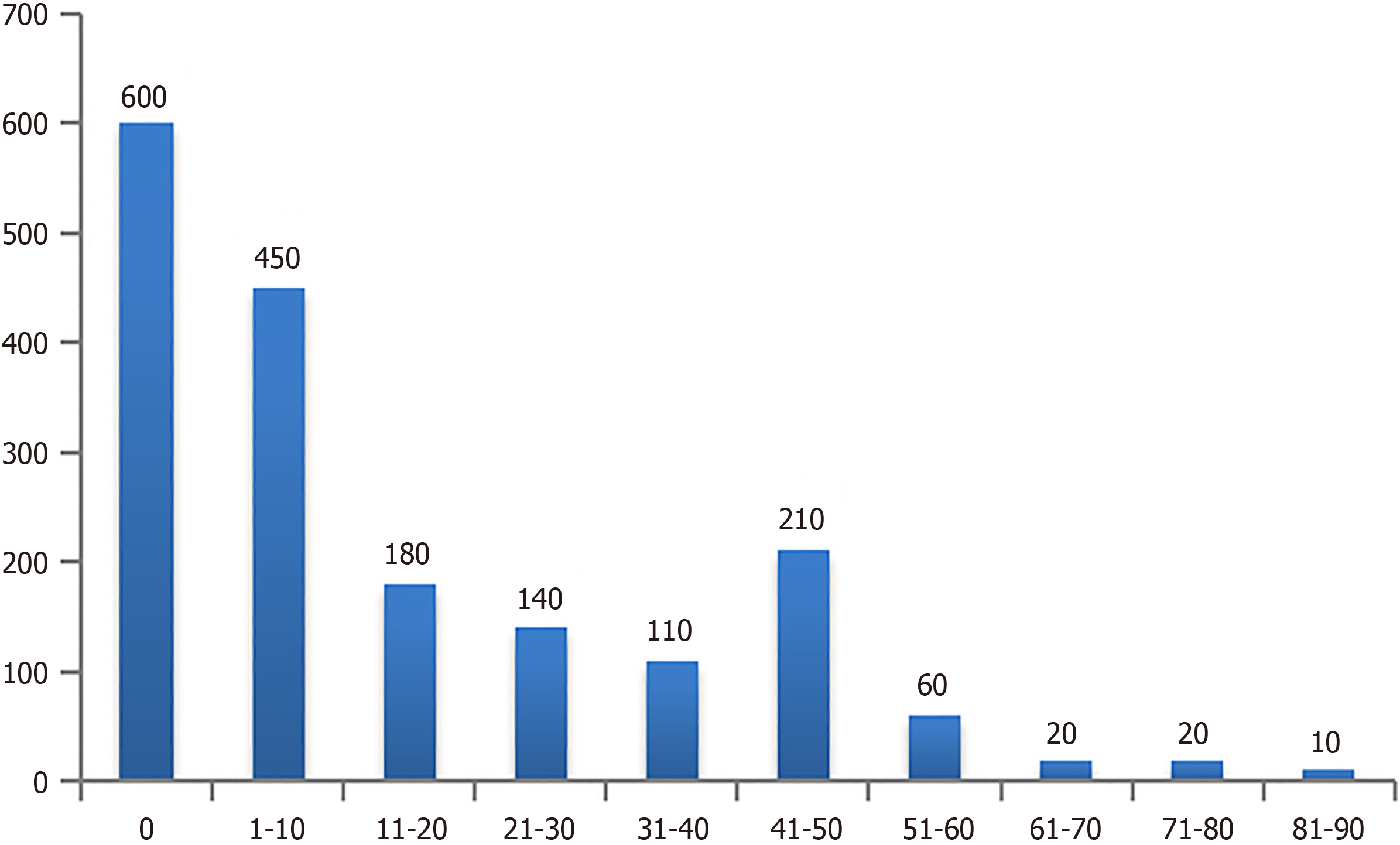
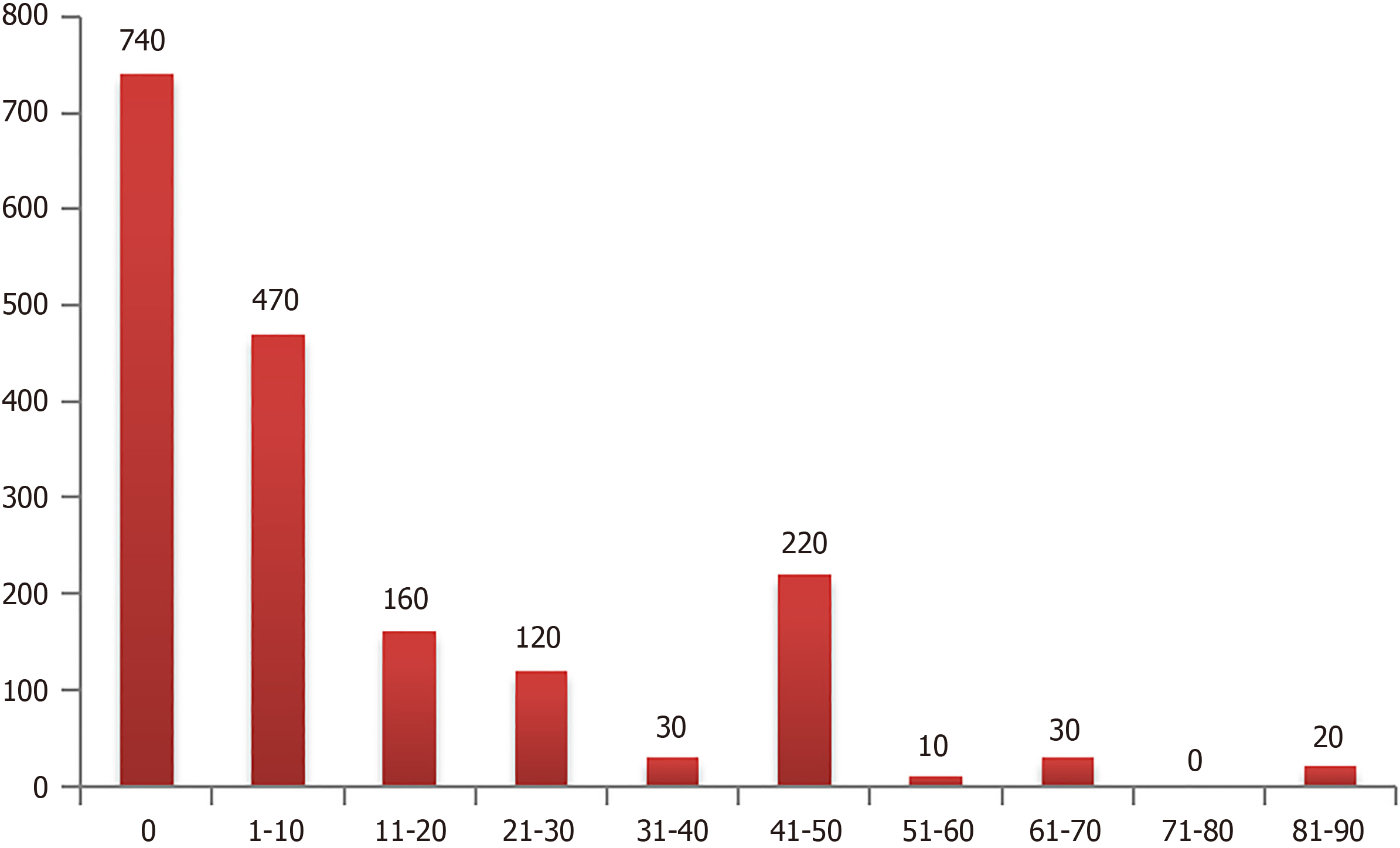
Perceived risk of COVID-19 infection and death: Perceived risk was assessed through survey questions where participants rated their perceived likelihood of contracting COVID-19 and their perceived risk of dying from it. These perceptions were measured on a percentage scale (e.g., 0%, 1%-10%, 11%-20%, 21%-30%, etc.).
Comparability of assessment methods: All participants in the study completed the same standardized survey, ensuring that the methods of data collection and measurement were consistent across the entire sample. As the study did not involve multiple groups subjected to different assessment methods, the comparability of assessment methods was inherently maintained. This uniform approach minimized the risk of measurement bias and ensured that the data collected were comparable across all respondents.
It is important to acknowledge potential bias related to the mode of survey distribution. The survey was disseminated via social media platforms, which means that individuals without access to these platforms were not represented in the sample. This limitation may affect the generalizability of the findings. Due to the nature of social media distribution, the total number of individuals who received the survey invitation could not be determined. Therefore, the exact response rate could not be calculated. This represents a limitation of the study, as it prevents us from assessing the representativeness of the sample accurately.
After data collection, responses were reviewed for completeness and usability. This involved checking for any missing or incomplete responses that could compromise the data quality. Only fully completed questionnaires were included in the analysis to maintain the integrity of the data. By considering these limitations and addressing potential biases, this study aimed to provide a comprehensive understanding of the acceptance of the COVID-19 vaccine and its related determinants among Nigerians.
A total of 1800 participants completed the survey. This sample size was not predetermined prior to the survey (because the research team aimed to achieve a sample size that would be sufficiently large to provide the necessary statistical power for detecting potential associations between sociodemographic factors and COVID-19 vaccine acceptance). Rather, it was determined by the number of respondents who actually engaged with the survey during the collection period from February 2021 to May 2021. This final number of participants was influenced by factors such as the reach of the survey distribution channels and participant engagement.
In the study, quantitative variables, such as age, income, and perceived risk of COVID-19 infection and death, were initially collected in their continuous or original forms. However, for the purpose of analysis, these variables were grouped into categorical ranges to facilitate logistic regression and χ2 tests.
Age: Age was categorized into predefined groups, such as 21-30 years, 31-40 years, etc. This grouping allowed for easier interpretation of the data and comparison across different demographic groups. It also helped in managing potential variability and simplified the analysis, making it more straightforward to identify trends or associations with vaccine acceptance.
Income: Income was categorized into ranges (e.g., less than $500 per month, $500-$1000 per month, etc.) to reflect different socioeconomic strata within the population. This categorization helped in assessing whether income levels influenced vaccine acceptance and made it easier to interpret the effects of economic factors on participants’ decisions.
Perceived risk of COVID-19 infection and death: Perceived risk was categorized into percentage ranges (e.g., 0%, 1%-10%, 11%-20%, etc.). This grouping method allowed the study to assess how different levels of perceived risk correlated with vaccine acceptance. It also helped in simplifying the analysis by reducing the complexity of dealing with continuous data, making it easier to identify patterns and draw conclusions.
Quantitative data were analyzed using Statistical Package for the Social Sciences, version 25 (IBM Corp., Armonk, NY, United States), in alignment with the study’s objectives. The analysis focused on respondents’ answers to closed-ended questions with a limited set of response options, where quantitative techniques were appropriate.
Statistical methods and control for confounding: Descriptive statistics, including frequency distributions, percentages, mean scores, and standard deviations, were calculated and presented in tabular form. χ² tests were employed for bivariate analyses to explore the associations between sociodemographic factors and vaccine acceptance. To control for potential confounding variables, logistic regression analysis was conducted, allowing for the adjustment of multiple sociodemographic factors simultaneously. The level of statistical significance was set at P = 0.05.
Subgroup and interaction analysis: Subgroup analyses were performed to examine interactions between key sociodemographic variables and vaccine acceptance. For example, separate logistic regression models were run for different age groups, income levels, and participants with chronic conditions to identify whether these subgroups exhibited different patterns of vaccine acceptance. Interaction terms were also tested within the regression models to assess whether the effect of one variable on vaccine acceptance was modified by another variable (e.g., the interaction between age and income).
Handling of missing data: There was no missing data in this study. All respondents completed the survey in full, en
Analytical methods: To ensure that the findings were as representative as possible, the following analytical methods were employed: (1) Descriptive statistics: Frequency distributions, percentages, mean scores, and standard deviations were computed to describe the characteristics of the sample and the distribution of responses; (2) χ² tests: They were used for bivariate analyses to explore the associations between sociodemographic variables (e.g., age, sex, and income) and vaccine acceptance. χ² tests helped identify significant relationships within the sample; (3) Logistic regression analysis: This method was employed to assess the relationship between sociodemographic factors and vaccine acceptance while adjusting for potential confounders. Logistic regression allowed for the evaluation of the influence of multiple variables simultaneously; and (4) Weighting considerations: Although the study used a convenience sampling method, the analysis considered potential biases by comparing the sample demographics with known population characteristics where possible. This comparison helped in interpreting the findings and understanding their generalizability.
The cross-sectional design of the study provided a snapshot of vaccine acceptance at a single point in time. Due to the non-random sampling method, the results were interpreted with caution regarding their generalizability to the broader Nigerian population. The findings reflected the attitudes and perceptions of the sample group and may not fully capture the diversity of the entire population.
In this study, sensitivity analyses were conducted to ensure the robustness and reliability of the findings and ensure that the results were not unduly affected by methodological choices or specific assumptions. The following sensitivity analyses were performed.
Alternative cutoff points for vaccine acceptance: To test the stability of the vaccine acceptance measure, different cutoff points for categorizing participants as having poor or good acceptance rate were examined. This analysis aimed to determine whether the conclusions regarding vaccine acceptance remained consistent across different classification schemes. It helped verify that the results were not unduly influenced by the choice of cutoff points.
Subgroup analyses: Additional analyses were performed within specific subgroups, such as different age ranges, income levels, and chronic condition statuses. These subgroup analyses were conducted to check whether the main findings held true within different segments of the population and to identify any potential variations in vaccine acceptance based on these factors.
A total of 1800 Nigerians participated in the survey.
Reporting numbers at each stage of the study: (1) Potentially eligible participants: The survey was distributed through social networking platforms. The exact number of individuals who received the survey invitation could not be dete
Reasons for non-participation at each stage: The survey did not track individual responses beyond submission. Ho
The sociodemographic characteristics of the study participants are presented in Table 1. A larger proportion of the respondents were male (53.9%) and within the age group of 21-30 years (29.4%), earned an average income of less than $500 per month (43.3%), and lived in urban areas (90.6%). Table 2 shows the existence of underlying conditions among the study participants. A small percentage reported underlying conditions, including diabetes (8.3%), heart disease (2.2%), pulmonary disease (1.1%), with none indicating hypertension (0%). Table 3 presents the impacts of the COVID-19 pandemic on the work life of the study participants. According to the survey, 48.9% of respondents were employed, with most perceiving the COVID-19 pandemic as having negative effects on their careers. Nearly one-third of the respondents were receiving less pay for their work.
| Variable | Categories | Frequency |
| Age group in yr | ≤ 20 | 310 (17.2) |
| 21-30 | 530 (29.4) | |
| 31-40 | 460 (25.6) | |
| 41-50 | 380 (21.1) | |
| > 51 | 120 (6.7) | |
| Sex | Female | 830 (46.1) |
| Male | 970 (53.9) | |
| Location | Rural | 170 (9.4) |
| Urban | 1630 (90.6) | |
| Average income | Less than $500 per month | 780 (43.3) |
| $1000-$1999 per month | 190 (10.6) | |
| $2000-$2999 per month | 240 (13.3) | |
| $3000-$4999 per month | 110 (6.1) | |
| $5000-$7999 per month | 60 (3.3) | |
| $500-$999 per month | 280 (15.6) | |
| $8000-$9999 per month | 40 (2.2) | |
| $10000-$12999 per month | 30 (1.7) | |
| $13000 or more per month | 70 (3.9) | |
| Religion | Catholic | 280 (15.6) |
| Christian/Protestant/Methodist/Lutheran/Baptist | 1130 (62.8) | |
| Muslim | 380 (21.1) | |
| Other | 10 (0.6) |
| Underlying conditions | Frequency (%) |
| Have diabetes | 150 (8.3) |
| Have heart disease | 40 (2.2) |
| Have pulmonary disease | 20 (1.1) |
| Have hypertension | 0 (0.0) |
| Variable | Categories | Frequency |
| Are you currently | Employed for wages | 880 (48.9) |
| Homemaker | 10 (0.6) | |
| Out of work for 1 year or more | 30 (1.7) | |
| Out of work for less than 1 year | 80 (4.4) | |
| Self-employed | 150 (8.3) | |
| Student | 650 (36.1) | |
| How much has your work changed as a result of the COVID-19 pandemic | I was let go from my job | 80 (4.4) |
| I work fewer hours | 340 (18.9) | |
| I work more hours | 250 (13.9) | |
| No change. I work the same amount | 530 (29.4) | |
| Not applicable (not working) | 600 (33.3) | |
| How much has your salary changed as a result of the COVID-19 pandemic | I am getting paid less | 660 (36.7) |
| I am getting paid more | 40 (2.2) | |
| No change. I am getting paid the same | 1100 (61.1) | |
| In the past week, how often have you gone to work or school outside of the home | 0 day | 260 (14.4) |
| 1 day | 30 (1.7) | |
| 2 days | 150 (8.3) | |
| 3 days | 160 (8.9) | |
| 4 days | 180 (10.0) | |
| 5 days | 510 (28.3) | |
| 6 days | 180 (10.0) | |
| 7 days | 330 (18.3) | |
| Did you wear a mask at work/school | No | 20 (1.1) |
| Not applicable (not going out a whole week) | 150 (8.3) | |
| Yes, during my whole time at work/school | 1020 (56.7) | |
| Yes, for part of the time at work/school | 610 (33.9) | |
| In the past week, how often have you gone to a grocery store or other food vendor | 0 day | 170 (9.4) |
| 1 day | 510 (28.3) | |
| 2 days | 520 (28.9) | |
| 3 days | 360 (20.0) | |
| 4 days | 40 (2.2) | |
| 5 days | 90 (5.0) | |
| 6 days | 50 (2.8) | |
| 7 days | 60 (3.3) | |
| Did you wear a mask at the grocery store or other food vendor | No | 130 (7.2) |
| Not applicable (not going out to grocery store or other food vendor whole week) | 80 (4.4) | |
| Yes, during my whole time at the store | 1280 (71.1) | |
| Yes, for part of the time at the store | 310 (17.2) |
The perception of vaccination and social distancing measures among the study participants is presented in Table 4. The majority of respondents had a positive perception of vaccination and social distancing measures. Most participants stro
| Variable | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree |
| Vaccines are important for my health | 790 (43.9) | 780 (43.3) | 170 (9.4) | 20 (1.1) | 40 (2.2) |
| Vaccines are effective | 650 (36.1) | 870 (48.3) | 240 (13.3) | 10 (0.6) | 30 (1.7) |
| Being vaccinated is important for the health of others in my community | 860 (47.8) | 740 (41.1) | 140 (7.8) | 50 (2.8) | 10 (0.6) |
| All routine vaccines recommended by the healthcare workers are beneficial | 580 (32.2) | 850 (47.2) | 300 (16.7) | 60 (3.3) | 10 (0.6) |
| New vaccines carry more risks than older vaccines | 330 (18.3) | 490 (27.2) | 670 (37.2) | 220 (12.2) | 90 (5.0) |
| The information I receive about vaccines from the government is reliable and trustworthy | 130 (7.2) | 610 (33.9) | 770 (42.8) | 220 (12.2) | 70 (3.9) |
| Getting vaccines is a good way to protect me from disease | 740 (41.1) | 820 (45.6) | 150 (8.3) | 50 (2.8) | 40 (2.2) |
| Generally, I follow vaccine recommendations from my doctor or health care provider | 650 (36.1) | 950 (52.8) | 140 (7.8) | 50 (2.8) | 10 (0.6) |
| Social distancing can protect yourself from COVID-19 | 970 (53.9) | 730 (40.6) | 70 (3.9) | 20 (1.1) | 10 (0.6) |
| Social distancing can protect your child or children from COVID-19 | 1030 (57.2) | 650 (36.1) | 100 (5.7) | 20 (1.1) | 0 (0.0) |
| Social distancing can protect your parents from COVID-19 | 1030 (57.2) | 670 (37.2) | 80 (4.4) | 20 (1.1) | 0 (0.0) |
| Variable | Strongly agree | Agree | Neither agree nor disagree | Disagree | Strongly disagree |
| Vaccines are important for my health | 200 (95.2) | 10 (4.76) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Vaccines are effective | 200 (95.2) | 10 (4.76) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Being vaccinated is important for the health of others in my community | 210 (100) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| All routine vaccines recommended by the healthcare workers are beneficial | 200 (95.2) | 10 (4.76) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| New vaccines carry more risks than older vaccines | 0 (0.0) | 20 (9.52) | 80 (38.1) | 100 (47.6) | 10 (4.76) |
| The information I receive about vaccines from the government is reliable and trustworthy | 200 (95.2) | 10 (4.76) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Getting vaccines is a good way to protect me from disease | 200 (95.2) | 10 (4.76) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Generally, I follow vaccine recommendations from my doctor or health care provider | 200 (95.2) | 10 (4.76) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Social distancing can protect yourself from COVID-19 | 210 (100) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Social distancing can protect your child or children from COVID-19 | 200 (95.2) | 5 (2.38) | 5 (2.38) | 0 (0.0) | 0 (0.0) |
| Social distancing can protect your parents from COVID-19 | 200 (95.2) | 5 (2.38) | 5 (2.38) | 0 (0.0) | 0 (0.0) |
The association between the sociodemographic characteristics and perception of vaccination as well as social distancing measures among the study participants is presented in Table 6. There was no significant association between the ob
| Variable | Categories | Poor perception | Good perception | Total | χ² | P value | Odds ratio (95%CI) |
| Age group (yr) | ≤ 20 | 220 (12.2) | 90 (5.0) | 310 (17.2) | 8.449 | 0.076 | |
| 21-30 | 260 (14.4) | 270 (15.0) | 530 (29.4) | 1.25 (0.94-1.65) | |||
| 31-40 | 200 (11.1) | 260 (14.4) | 460 (25.6) | ||||
| 41-50 | 160 (8.9) | 220 (12.2) | 380 (21.1) | ||||
| > 51 | 40 (2.2) | 80 (4.4) | 120 (6.7) | ||||
| Sex | Female | 450 (25.0) | 380 (21.1) | 830 (46.1) | 1.75 | 0.186 | |
| Male | 430 (23.9) | 540 (30.0) | 970 (53.9) | 0.74 (0.38-1.44) | |||
| Location | Rural | 110 (6.1) | 60 (3.3) | 170 (9.4) | 1.88 | 0.17 | |
| Urban | 770 (42.8) | 860 (47.8) | 1630 (90.6) | 0.50 (0.16-1.51) | |||
| Average income | Less than $500 per month | 410 (22.8) | 370 (20.6) | 780 (43.3) | 1.17 (0.14-9.43) | ||
| $500-$999 per month | 110 (6.1) | 170 (9.4) | 280 (15.6) | 0.94 (0.17-5.27) | |||
| $1000-$1999 per month | 80 (4.4) | 110 (6.1) | 190 (10.6) | 7.15 | 0.521 | ||
| $2000-$2999 per month | 110 (6.1) | 130 (7.2) | 240 (13.3) | 0.38 (0.07-2.21) | |||
| $3000-$4999 per month | 40 (2.2) | 70 (3.9) | 110 (6.1) | 1.19 (0.46-3.10) | |||
| $5000-$7999 per month | 30 (1.7) | 30 (1.7) | 60 (3.3) | 1.33 (0.34-5.13) | |||
| $8000-$9999 per month | 20 (1.1) | 20 (1.1) | 40 (2.2) | 1.59 (0.64-3.96) | |||
| $10000-$12999 per month | 30 (1.7) | 0 (0) | 30 (1.7) | 1.26 (0.44-3.65) | |||
| $13000 or more per month | 50 (2.8) | 20 (1.1) | 70 (3.9) | 0.00 (0.00-0.00) | |||
| Religion | Catholic | 150 (8.3) | 130 (7.2) | 280 (15.6) | 2.819 | 0.42 | |
| Christian/Protestant/Methodist/Lutheran/ Baptist | 580 (32.2) | 550 (30.6) | 1130 (62.8) | 0.00 (0.00-0.00) | |||
| Muslim | 150 (8.3) | 230 (12.8) | 38 (21.1) | 0.00 (0.00-0.00) | |||
| Other | 0 (0.0) | 10 (0.6) | 1 (0.6) | 0.00 (0.00-0.00) |
The perceived risk of COVID-19 infection among participants was as follows: 0% (600), 1%-10% (450), 11%-20% (180), 21%-30% (140), 31%-40% (110), and higher percentages. Only ten people considered themselves to have 81%-90% risk of getting infected (Figure 2). On the other hand, the perceived risk of dying from COVID-19 if infected was as follows: 0% (740), 1%-10% (470), 11%-20% (160), 21%-30% (120), 31%-40% (30), etc. Twenty people considered themselves to have an 81%-90% risk of dying if infected (Figure 3). The occurrence of COVID-19 and the severity among the study participants is presented in Table 7. Ten of them (5.6%) indicated that they have been diagnosed with COVID-19 by a doctor, of which only 2.2% had very serious cases, while 3.3% of the cases were not very serious.
| Variable | Categories | Frequency |
| Diagnosed with COVID-19 by a doctor | No | 1700 (94.4) |
| Yes | 100 (5.6) | |
| How serious was the course of illness when you were infected with COVID-19 | Not applicable | 1700 (94.4) |
| Not very serious | 60 (3.3) | |
| Somewhat serious | 40 (2.2) | |
| Do you know people in your immediate social environment (close friends or family members) who are or have been infected with COVID-19 | Do not know | 420 (23.3) |
| No | 670 (37.2) | |
| Yes | 710 (39.4) | |
| How serious was the course of illness when your friend or family member was infected with the COVID-19? If you know multiple people who have had COVID-19, think about the most recent one | Not applicable | 1090 (60.6) |
| Not very serious | 260 (14.4) | |
| Somewhat serious | 300 (16.7) | |
| Very serious | 150 (8.3) | |
| Have you seen or read about individuals infected with the COVID-19 on social media or TV | No | 30 (1.7) |
| Yes | 1770 (98.3) | |
| How serious was the course of illness for the most recent COVID-19 case you have seen or read about in social media or on the TV | No idea | 30 (1.7) |
| Not very serious | 260 (14.4) | |
| Somewhat serious | 620 (34.4) | |
| Very serious | 890 (49.4) | |
| Have you ever heard that your local health facilities stop the vaccination service for kids due to COVID-19 pandemic | No | 1550 (86.1) |
| Yes | 250 (13.9) |
Table 8 shows the COVID-19 vaccine acceptance rates among the study participants. A vaccine with 95% efficacy if the government was offering it as a free and optional vaccine would be accepted by 1380 participants (76.7%). Only 70.0% of the study participants indicated that they would buy and get vaccinated if the vaccine was 95% effective, had a 5% chance of a side effect like a fever or local pain, and was sold for US$50, while 1150 (63.9%) said they would buy and get va
| Variable | Categories | Frequency |
| Imagine that a new COVID-19 vaccine has just been developed. It has received the same testing as the adult influenza vaccine. The government is offering it as a FREE and optional vaccine. Would you accept a COVID-19 vaccine if the vaccine was 95% effective | No | 420 (23.3) |
| Yes | 1380 (76.7) | |
| The vaccine is 50% effective, with a 5% chance of a side effect like a fever (50% effective means that there is a 50% reduction in disease among those vaccinated compared to those unvaccinated) | No | 860 (47.8) |
| Yes | 940 (52.2) | |
| The vaccine is 95% effective, with a 20% chance of a side effect like a fever (95% effective means that there is a 95% reduction in disease among those vaccinated compared to those unvaccinated) | No | 550 (30.6) |
| Yes | 1250 (69.4) | |
| The vaccine is 75% effective, with a 5% chance of a side effect like a fever (75% effective means that there is a 75% reduction in disease among those vaccinated compared to those unvaccinated) | No | 400 (22.2) |
| Yes | 1400 (77.8) | |
| The vaccine is 75% effective, with a 20% chance of a side effect like a fever (75% effective means that there is a 75% reduction in disease among those vaccinated compared to those unvaccinated) | No | 990 (55.0) |
| Yes | 810 (45.0) | |
| For a COVID-19 vaccine that is 95% effective and a 5% chance of a side effect like fever or local pain? If the price was US$50 for complete vaccination. Would you buy the vaccine and get vaccinated | No | 540 (30.0) |
| Yes | 1260 (70.0) | |
| If the COVID-19 vaccine price was US$100. Would you buy the vaccine and get vaccinated | No | 650 (36.1) |
| Yes | 1150 (63.9) | |
| If the COVID-19 vaccine price was US$200. Would you still buy the vaccine and get vaccinated | No | 570 (31.7) |
| Yes | 1230 (68.3) | |
| If the COVID-19 vaccine price is reduced to US$25. Would you buy the vaccine and get vaccinated | No | 550 (30.6) |
| Yes | 1250 (69.4) | |
| If the COVID-19 vaccine price was US$12.5. Would you buy the vaccine and get vaccinated | No | 1210 (67.2) |
| Yes | 590 (32.8) | |
| If the COVID-19 vaccine price was US$5 only. Would you buy the vaccine and get vaccinated | No | 630 (35.0) |
| Yes | 1170 (65.0) |
| Variable | Categories | Frequency |
| Imagine that a new COVID-19 vaccine has just been developed. It has received the same testing as the adult influenza vaccine. The government is offering it as a free and optional vaccine. Would you accept a COVID-19 vaccine if the vaccine was 95% effective? | No | 0 (0.0) |
| Yes | 210 (100.0) | |
| The vaccine was 50% effective, with a 5% chance of a side effect like a fever? (50% effective means that there is a 50% reduction in disease among those vaccinated compared to those unvaccinated) | No | 10 (4.8) |
| Yes | 200 (95.2) | |
| The vaccine was 95% effective, with a 20% chance of a side effect like a fever? (95% effective means that there is a 95% reduction in disease among those vaccinated compared to those unvaccinated) | No | 30 (14.3) |
| Yes | 180 (85.7) | |
| The vaccine was 75% effective, with a 5% chance of a side effect like a fever? (75% effective means that there is a 75% reduction in disease among those vaccinated compared to those unvaccinated) | No | 25 (11.9) |
| Yes | 185 (88.09) | |
| The vaccine was 75% effective, with a 20% chance of a side effect like a fever? (75% effective means that there is a 75% reduction in disease among those vaccinated compared to those unvaccinated) | No | 30 (14.3) |
| Yes | 180 (85.7) | |
| For a COVID-19 vaccine that was 95% effective and a 5% chance of a side effect like a fever or local pain? If the price is US$50 for complete vaccination. Would you buy the vaccine and get vaccinated? | No | 0 (0.0) |
| Yes | 210 (100) | |
| If the COVID-19 vaccine price was US$100. Would you buy the vaccine and get vaccinated? | No | 0 (0.0) |
| Yes | 210 (100.0) | |
| If the COVID-19 vaccine price was US$200. Would you buy the vaccine and get vaccinated? | No | 10 (4.8) |
| Yes | 200 (95.2) | |
| If the COVID-19 vaccine price was reduced to US$25. Would you buy the vaccine and get vaccinated? | No | 0 (0.0) |
| Yes | 210 (100.0) | |
| If the COVID-19 vaccine price was US$12.5. Would you buy the vaccine and get vaccinated? | No | 0 (0.0) |
| Yes | 210 (100.0) | |
| If the COVID-19 vaccine price was US$5 only. Would you buy the vaccine and get vaccinated? | No | 0 (0.0) |
| Yes | 210 (100.0) |
The association between the sociodemographic characteristics and COVID-19 vaccine acceptance rates among the study participants is presented in Table 10. No significant associations (P > 0.05) were found between sociodemographic characteristics and COVID-19 vaccine acceptance rates. The overall mean score for vaccine acceptance among participants showed significant differences (P < 0.05) between those willing to accept the vaccine (8.44 ± 1.14) and those not willing (4.18 ± 1.66) (Table 11).
| Variable | Categories | Poor | Good | Total | χ² | P value | Odds ratio (95%CI) |
| Age group (yr) | ≤ 20 | 70 (3.9) | 240 (13.3) | 310 (17.2) | 3.049 | 0.55 | |
| 21-30 | 200 (11.1) | 330 (18.3) | 530 (29.4) | 0.76 (0.57-1.02) | |||
| 31-40 | 180 (10.0) | 280 (15.6) | 460 (25.6) | ||||
| 41-50 | 150 (8.3) | 230 (12.8) | 380 (21.1) | ||||
| > 51 | 50 (2.8) | 70 (3.9) | 120 (6.7) | ||||
| Sex | Female | 310 (17.2) | 520 (28.9) | 830 (46.1) | 0.102 | 0.749 | |
| Male | 340 (18.9) | 630 (35.0) | 970 (53.9) | 0.83 (0.42-1.62) | |||
| Location | Rural | 60 (3.3) | 110 (6.1) | 170 (9.4) | 0.005 | 0.941 | |
| Urban | 590 (32.8) | 1040 (57.8) | 1630 (90.6) | 0.90 (0.29-2.78) | |||
| Average income | Less than $500 per month | 310 (17.2) | 470 (26.1) | 780 (43.3) | 2.74 (0.25-30.32) | ||
| $500-$999 per month | 110 (6.1) | 170 (9.4) | 280 (15.6) | 4.14 (0.44-38.90) | |||
| $1000-$1999 per month | 40 (2.2) | 150 (8.3) | 190 (10.6) | 3.802 | 0.875 | ||
| $2000-$2999 per month | 90 (5.0) | 150 (8.3) | 240 (13.3) | 0.81 (0.16-4.05) | |||
| $3000-$4999 per month | 40 (2.2) | 70 (3.9) | 110 (6.1) | 1.25 (0.47-3.29) | |||
| $5000-$7999 per month | 10 (0.6) | 50 (2.8) | 60 (3.3) | 1.33 (0.34-5.22) | |||
| $8000-$9999 per month | 10 (0.6) | 30 (1.7) | 40 (2.2) | 1.08 (0.43-2.68) | |||
| $10000-$12999 per month | 10 (0.6) | 20 (1.1) | 30 (1.7) | 2.76 (0.81-9.42) | |||
| $13000 or more per month | 30 (1.7) | 40 (2.2) | 70 (3.9) | 1.14 (0.09-13.78) | |||
| Religion | Catholic | 100 (5.6) | 180 (10.0) | 280 (15.6) | 1.804 | 0.614 | |
| Christian/Protestant/Methodist/Lutheran/Baptist | 440 (24.4) | 690 (38.3) | 1130 (62.8) | 0.00 (0.00-0.00) | |||
| Muslim | 110 (6.1) | 270 (15.0) | 380 (21.1) | 0.00 (0.00-0.00) | |||
| Other | 0 (0.0) | 10 (0.6) | 10 (0.6) | 0.00 (0.00-0.00) |
| Variable | Poor | Good | P value |
| Overall score on perception of vaccination and social distancing measures among the study participants | 8.49 ± 2.72 | 9.04 ± 1.88 | 0.112 |
| Overall score on the coronavirus disease 2019 vaccine acceptance rates among the study participants. | 4.18 ± 1.66 | 8.44 ± 1.14 | 0.000 |
Unadjusted estimates: The study found no significant associations between sociodemographic characteristics (age, sex, location, average income, and religion) and COVID-19 vaccine acceptance rates. For instance, the χ² test results showed non-significant P values for these variables (age: χ² = 3.049, P = 0.550; sex: χ² = 0.102, P = 0.749; location: χ² = 0.005, P = 0.941; income: χ² = 3.802, P = 0.875; religion: χ² = 2.819, P = 0.420).
Confounder-adjusted estimates: Logistic regression analysis was conducted to assess the association between so
Perceived risk of COVID-19 infection: 0% (600 respondents), 1%-10% (450 respondents), 11%-20% (180 respondents), 21%-30% (140 respondents), 31%-40% (110 respondents), and higher percentages, including 81%-90% (10 respondents).
Perceived risk of dying from COVID-19: 0% (740 respondents), 1%-10% (470 respondents), 11%-20% (160 respondents), 21%-30% (120 respondents), 31%-40% (30 respondents), and higher percentages, including 81%-90% (20 respondents).
Translation of relative risk into absolute risk: The study did not specifically translate relative risk into absolute risk. However, the provided percentages of perceived risk can be used to infer the perceived likelihood of infection and death among participants. For instance, if 48.9% perceived their risk of infection to be between 1%-10%, it suggests that nearly half of the participants consider their risk relatively low.
Other analyses performed: (1) Subgroup and interaction analyses: Subgroup analyses were performed to explore variations in vaccine acceptance based on underlying conditions. Participants with underlying conditions showed high acceptance rates, with 100% acceptance for a vaccine with 95% efficacy if offered free. Sensitivity to price and effectiveness was also examined, revealing high acceptance even with variations in vaccine cost and potential side effects; and (2) Sensitivity analyses: Sensitivity analyses involved testing different cutoff points for categorizing vaccine acceptance and examining the effect of various model specifications on the findings. The study tested alternative thresholds for vaccine acceptance and adjusted for different sociodemographic factors in the regression models. Additionally, analyses of subgroups, such as those with underlying conditions, were conducted to assess the stability of the main findings across different groups.
The results of the current study, which examined COVID-19 vaccine acceptance and its determinants among 1800 respondents in Nigeria, revealed several key findings and trends that can be compared with previous studies conducted in Nigeria and beyond.
The study revealed a vaccine acceptance rate of 63.9% among the Nigerian participants. This indicates a majority willingness to receive the COVID-19 vaccine under the conditions described in the survey. A significant portion of respondents demonstrated a positive perception of both the COVID-19 vaccine and social distancing measures. Spe
No significant association was found between age and vaccine acceptance, with odds ratios (OR) ranging from 0.94 to 1.65 across different age groups. Male participants showed a lower OR of vaccine acceptance (OR = 0.74, 95%CI: 0.38-1.44), though this result was not statistically significant. Urban residents had a lower adjusted OR (OR = 0.50, 95%CI: 0.16-1.51) for vaccine acceptance compared to rural residents, but this result was also not statistically significant. The OR varied across different income brackets, with no consistent trend and confidence intervals suggesting limited precision. No significant differences were found in vaccine acceptance across different religious groups, with OR indicating no significant associations. Participants’ perceived risk of COVID-19 infection and death was low, with a majority estimating their risk in the lower percentage range (0%-10%). This lower perceived risk may impact their motivation for vaccine uptake. High acceptance was noted when the vaccine was offered free with 95% efficacy. Acceptance rates remained high even when the vaccine cost increased, though there was a slight decline as the price rose to US$200.
The study indicated an overall COVID-19 vaccine acceptance rate of 63.9%, which aligns with similar trends observed in related research, though variations exist across different demographic and professional groups.
The relationship between sociodemographic factors and COVID-19 vaccine acceptance in Nigeria has yielded mixed results across studies. The current study found no significant association between factors like age, sex, income, and religion and vaccine acceptance, aligning with findings by Iwuafor et al[24], who also reported no significant predictors of vaccine refusal among healthcare professionals in Cross River State. This suggests that vaccine hesitancy may be more influenced by individual perceptions and external factors such as misinformation than by demographic variables. Ho
Eze et al[26] identified sex, religion, ethnicity, and geographical location as significant predictors, noting that male sex, Christianity, and Northern residence were positively associated with acceptance. Al-Mustapha et al[27] also found age and income to be significant predictors, with older individuals and those with higher incomes more likely to accept the vaccine. Alice et al[28] reported that increasing age, male sex, and trust in government and public health authorities were associated with higher vaccine acceptance. Njoga et al[29] emphasized the role of geopolitical zones, education, and oc
While our study focused on age, sex, location, average income, and religion of the study participants, we recognize the importance of education and socioeconomic status as determinants of vaccine acceptance. Previous studies[30-34] have shown that higher education levels and socioeconomic status correlate with greater vaccine acceptance due to better health literacy and perceived risk. These contrasting findings suggest that the influence of sociodemographic factors on vaccine acceptance may vary by context, and targeted interventions considering these variables may be necessary to address vaccine hesitancy effectively in Nigeria.
Our study revealed that a majority of respondents have a positive perception of vaccination and social distancing measures. Specifically, 43.9% strongly agreed on the importance of vaccines for health, and 47.8% believed vaccination is crucial for community health. These perceptions are comparable to the findings by Tijani et al[35], who reported a significant association between educational level and monthly income with vaccine uptake, highlighting the importance of awareness and financial stability in fostering positive perceptions towards vaccination.
The current study indicated that nearly half of the respondents (48.9%) felt that the COVID-19 pandemic negatively impacted their careers, with many reporting reduced pay. This economic impact likely influenced their perceptions and acceptance of vaccination, similar to findings by Zakari et al[36], where economic factors and skepticism about vaccine efficacy were major reasons for hesitancy among university community members.
A notable finding from the current study was the high acceptance rate (76.7%) for a vaccine with 95% efficacy if provided for free, which dropped to 63.9% if the vaccine costs $100. This trend of price sensitivity aligns with Padonou et al[37], who also observed that financial constraints and economic conditions significantly affected vaccine acceptance rates in Benin. In comparison to the findings from Omale et al[38], where health workers’ acceptance was primarily driven by perceptions of vaccine importance and safety, the respondents in the current study similarly indicated good perception (51.1%) vs poor perception (48.9%) of vaccination measures. This further emphasizes that improving perceptions through education and communication is crucial for enhancing vaccine uptake.
More than two-thirds of respondents in this study expressed willingness to be vaccinated for various reasons, while 64% indicated readiness to get vaccinated for a range of reasons. In terms of willingness to be vaccinated, the result of this current study is higher than those from Italy (53.7%), Russia (54.9%), Poland (56.3%), the United States (56.9%), Greece (57.7%), and France (58%)[39-41]. On the other side, countries such as Ecuador (97.0%), Malaysia (94.3%), Indonesia (93.3%), and China (91.3%) had the highest rates of vaccine acceptability, whilst Jordan (28.4%) and Kuwait (23.6%) had the lowest[40]. Since these factors were shown to be connected with the willingness to become vaccinated, the variation in vaccination rates might be attributed to the respondent’s level of education, employment, or social standing.
In addition, it has been reported that non-governmental groups make significant improvements to the vaccination programs in countries that have a low or moderate income. People living in remote areas and communities that are dif
The COVID-19 vaccination has been deemed safe and effective by 60% and 60.1% of individuals, as determined by different systematic reviews and meta-analyses[40,41]. According to the findings of an in-depth study as well as a meta-analysis, 81.65% of the general population was eager to be vaccinated against COVID-19. However, this number was far lower than those who actually received the vaccine[42]. This might provide an explanation for how the COVID-19 epi
Furthermore, our study observed that a higher percentage of male respondents supported vaccination compared to female respondents. This was in line with the results of a prior study that showed males were much more willing to acquire vaccinations. This might be due to the fact that roughly two-thirds of the males who participated in this study were literate. As a result, they were probably aware of the potentially harmful effects of COVID-19, which increased the likelihood that they would acquire the vaccine. When the vaccine became available, most people elected to get it because they were terrified of getting COVID-19. This fear may have prompted them to make this decision. The lack of under
The study assessed perceived risks of infection and death from COVID-19, revealing that a significant number of re
Perceived sickness risks have been connected to health-related activity[45]. However, the majority of research on risk perceptions focused primarily on the possibility of being ill[46]. The majority of the respondents in this study had a hig
The degree of association between these risk measures was relatively weak, and they cannot be used as proxies. Although the majority of participants in this study had good knowledge regarding vaccination, some also exhibited comparatively lower percentages of COVID-19 acceptability, and this might be due to low level of exposure and the perceived risk of dying among the respondents. Moreover, respondents in the age group of 51 years and above demon
If these people had been better informed about the vaccines and the degree to which the government was unprepared for them, it is possible that they would have been more worried about the accessibility and safety of the immunizations. On the contrary, they had a tendency to become worse. On the other hand, herd immunity against the COVID-19 out
Compared to the study by Mustapha et al[51], which found a vaccine acceptance rate of 40.0% among students, the acceptance rate of the current study was higher. However, both studies highlight the need for targeted education and public health campaigns to address misconceptions and improve vaccine uptake. The present study also suggested the necessity of making vaccines more affordable and accessible, which aligns with recommendations from Kolawole et al[52] and Mahmood et al[53], who emphasized the role of public health professionals and trust in vaccines.
Our findings indicate a significant relationship between a history of chronic illness and openness to receiving the COVID-19 vaccine. People who had a previous diagnosis of a chronic illness had a higher likelihood of responding fa
However, some uncertainty remains regarding the risks associated with new vaccines, highlighting the need for clear, evidence-based information to prevent hesitancy. The implications of high COVID-19 vaccine acceptance rates among individuals with underlying conditions are significant for public health, policy, and society. High acceptance, especially for a free vaccine that is 95% effective, underscores the willingness to get vaccinated, which is vital for achieving herd immunity and controlling the spread of COVID-19. Even with some side effects, acceptance remains high, though slightly lower with increased side effect likelihood. This emphasizes the importance of transparent risk-benefit communication. Vaccines with higher efficacy rates are more likely to be accepted, suggesting that public health efforts should focus on distributing and promoting the most effective vaccines.
Affordability is a key factor, with 100% acceptance for vaccines priced up to $100 and a slight decrease at $200. Policymakers should ensure vaccines are affordable or free, especially for vulnerable populations with underlying conditions. Subsidies, insurance coverage, and financial assistance programs can help maintain high vaccination rates. Ensuring equitable access to vaccines is essential for those more susceptible to severe outcomes from COVID-19. This is consistent with previous studies[54-58]. Both an Australian study and a report by the World Health Organization support these fin
Studies on vaccine history, also known as past vaccination behavior, are accurate predictors of future vaccination behavior[62,63]. A previous survey found that between 2010 and 2015, only 3.4% to 44.1% of healthcare workers in the Kingdom of Saudi Arabia received the influenza vaccine[13]. In addition, earlier studies that used a cross-sectional approach indicated that if people in Russia and Indonesia were not given sufficient knowledge regarding the efficacy and safety of vaccines, they would not support them. This was the case in both countries[62]. In addition, there is a major shortage of COVID-19 vaccines in Nigeria since the country does not get them on a consistent basis or in adequate qu
The study on COVID-19 vaccine acceptance among Nigerians, while providing valuable insights, had several limitations that could affect the interpretation of the results.
Sampling bias (non-random sampling): The study used an online survey distributed through social networking plat
Response bias: The study relied on self-reported data, which can introduce response bias. Participants might provide socially desirable answers or overstate their acceptance of the vaccine to align with perceived social norms. This could lead to an overestimation of vaccine acceptance and a more positive perception of vaccination and social distancing measures. The impact of response bias is difficult to quantify but could be considerable, especially in the context of sen
Response rate calculation: Due to the nature of social media distribution, it was impossible to determine the total number of individuals who received the survey invitation. Without this data, accurately calculating the response rate is unfea
Measurement issues: The study used percentage-based categories for perceived risk rather than more granular or standardized scales. This method may lack precision and could lead to misclassification of participants’ perceptions. This imprecision could obscure the true distribution of perceived risk and affect the accuracy of the associations with vaccine acceptance. The magnitude of this imprecision could vary but may limit the ability to detect more silent differences in perceived risk.
Cross-sectional design: As a cross-sectional study, it captured data at a single point in time, making it challenging to infer causality or changes in vaccine acceptance over time. The snapshot nature of the data may not reflect shifts in attitudes or external factors affecting vaccine acceptance that occurred after the study period. This limitation is inherent to cross-sectional studies and affects all results similarly, though the exact impact on conclusions about causality is sig
Sample size: While the sample size of 1800 participants is relatively large, it was not calculated based on formal power analysis. This means the study may have limited power to detect smaller associations or differences. Without an adequate power analysis, the study might not detect significant associations that exist, or it might find associations that are not robust. The lack of power analysis could affect the reliability of the study’s conclusions, particularly for subgroup analyses where sample sizes are smaller.
Confounding variables: Despite adjusting for some sociodemographic factors, other potential confounders such as health literacy, exposure to misinformation, and prior experiences with vaccines were not assessed. The study did not consider education and socioeconomic status, which are crucial determinants of vaccine acceptance. Previous research indicated that individuals with higher education levels and better socioeconomic positions were more likely to understand the benefits of vaccination and perceive higher risks of COVID-19, influencing their acceptance rates. Unmeasured con
Overall interpretation: The study provided valuable insights into the level of COVID-19 vaccine acceptance and the general perception of vaccination and social distancing among Nigerians. However, the limitations regarding sampling methods, response bias, and measurement precision necessitate a cautious interpretation of the results. The relatively high acceptance rate and positive perceptions suggest a generally supportive attitude towards COVID-19 vaccination among the surveyed group, particularly among those with underlying health conditions. The non-random sampling method and potential response biases imply that the findings may not fully represent the broader Nigerian population. The results should be interpreted with caution, acknowledging that the actual acceptance rates and perceptions might differ in the general population.
Generalizability: The findings may not be generalizable to all Nigerians or other populations due to the specific nature of the sample (e.g., higher internet usage and urban focus). This limits the ability to apply the findings broadly and could result in different vaccine acceptance patterns in other demographic groups. The extent of this generalizability issue is substantial, given the specific sociodemographic characteristics of the sample.
Based on the above limitations, we hereby make the following recommendations: (1) Future studies should employ a multimodal distribution strategy, including face-to-face interviews, telephone surveys, and distribution through traditional media channels (e.g., radio, television) to reach a broader and more diverse population, including those without internet access; (2) It is crucial to incorporate education levels and detailed socioeconomic status indicators in future surveys. These factors significantly influence vaccine acceptance and would provide a clearer understanding of the determinants of vaccine uptake; (3) Conduct longitudinal studies to track changes in vaccine acceptance over time. This approach would help identify trends, evaluate the long-term effectiveness of public health interventions, and observe shifts in public perception as the pandemic evolves; (4) To mitigate social desirability bias, consider using anonymous surveys and validated instruments designed to reduce the impact of self-reporting biases. Additionally, incorporating qualitative methods (e.g., focus groups and in-depth interviews) can provide deeper insights into the reasons behind vaccine acceptance or hesitancy; (5) Based on the study findings, public health campaigns should be tailored to address the specific concerns and barriers identified in the survey. These campaigns should emphasize the safety, efficacy, and importance of COVID-19 vaccines, particularly targeting groups with lower acceptance rates; (6) Governments and policymakers should consider providing vaccines for free or at subsidized rates to alleviate financial barriers. Economic support measures, such as compensation for potential side effects or paid time off for vaccination, could also enhance acceptance; (7) Engage community leaders, healthcare providers, and influencers to build trust and disseminate accurate information about COVID-19 vaccines. This grassroots approach can help counteract misinformation and skepticism, particularly in communities with historically low trust in governmental or medical institutions; and (8) Increase the number and accessibility of vaccination centers, especially in rural and underserved areas. Mobile clinics and community-based vaccination drives can help reach populations with limited access to healthcare facilities.
By addressing these limitations and implementing the recommended strategies, future research and public health efforts can more effectively enhance vaccine acceptance and uptake, contributing to better control of the COVID-19 pandemic in Nigeria.
The findings of this study provided valuable insights into the determinants of COVID-19 vaccine acceptance in Nigeria, highlighting the significant role of economic factors, perceptions of vaccine efficacy and safety, and the impact of the pandemic on individuals’ lives. Despite the observed positive perception and a substantial acceptance rate of 63.9% among the study participants, the analysis revealed that sociodemographic factors such as age, sex, income, and religion did not significantly influence vaccine uptake. However, individuals with a history of chronic conditions demonstrated a higher likelihood of accepting the vaccine, underscoring the importance of targeted interventions. To enhance vaccine acceptability and achieve herd immunity, it is imperative to implement comprehensive public health strategies. These should include economic support to alleviate financial barriers, extensive educational campaigns to improve under
We thank the respondents of this study for their willingness to participate in the survey.
| 1. | Okai GA, Abekah-Nkrumah G. The level and determinants of COVID-19 vaccine acceptance in Ghana. PLoS One. 2022;17:e0270768. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 2. | Dhama K, Khan S, Tiwari R, Sircar S, Bhat S, Malik YS, Singh KP, Chaicumpa W, Bonilla-Aldana DK, Rodriguez-Morales AJ. Coronavirus Disease 2019-COVID-19. Clin Microbiol Rev. 2020;33:e00028- e00020. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 689] [Cited by in RCA: 605] [Article Influence: 121.0] [Reference Citation Analysis (0)] |
| 3. | Ehrenberg JP, Utzinger J, Fontes G, da Rocha EMM, Ehrenberg N, Zhou XN, Steinmann P. Efforts to mitigate the economic impact of the COVID-19 pandemic: potential entry points for neglected tropical diseases. Infect Dis Poverty. 2021;10:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Burki T. Global COVID-19 vaccine inequity. Lancet Infect Dis. 2021;21:922-923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 50] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 5. | Ahmed MAM, Colebunders R, Gele AA, Farah AA, Osman S, Guled IA, Abdullahi AAM, Hussein AM, Ali AM, Siewe Fodjo JN. COVID-19 Vaccine Acceptability and Adherence to Preventive Measures in Somalia: Results of an Online Survey. Vaccines (Basel). 2021;9:543. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 6. | Kwok KO, Li KK, Wei WI, Tang A, Wong SYS, Lee SS. Editor's Choice: Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int J Nurs Stud. 2021;114:103854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 433] [Cited by in RCA: 431] [Article Influence: 107.8] [Reference Citation Analysis (0)] |
| 7. | Ripabelli G, Tamburro M, Buccieri N, Adesso C, Caggiano V, Cannizzaro F, Di Palma MA, Mantuano G, Montemitro VG, Natale A, Rodio L, Sammarco ML. Active Surveillance of Adverse Events in Healthcare Workers Recipients After Vaccination with COVID-19 BNT162b2 Vaccine (Pfizer-BioNTech, Comirnaty): A Cross-Sectional Study. J Community Health. 2022;47:211-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 8. | Sallam M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines (Basel). 2021;9:160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1150] [Cited by in RCA: 1150] [Article Influence: 287.5] [Reference Citation Analysis (0)] |
| 9. | Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34:6700-6706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 382] [Cited by in RCA: 562] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 10. | Manning ML, Gerolamo AM, Marino MA, Hanson-Zalot ME, Pogorzelska-Maziarz M. COVID-19 vaccination readiness among nurse faculty and student nurses. Nurs Outlook. 2021;69:565-573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 77] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 11. | Askarian M, Fu LY, Taghrir MH, Borazjani R, Shayan Z, Taherifard E, Taherifard E, Akbarialiabad H, Longtin Y, Askarian A, Kavousi S. COVID-19 Vaccination Acceptance in Iran, a Nationwide Survey on Factors Associated with the Willingness toward Getting Vaccinated. Int J Prev Med. 2022;13:130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Pelčić G, Karačić S, Mikirtichan GL, Kubar OI, Leavitt FJ, Cheng-Tek Tai M, Morishita N, Vuletić S, Tomašević L. Religious exception for vaccination or religious excuses for avoiding vaccination. Croat Med J. 2016;57:516-521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 13. | McFadden SM, Demeke J, Dada D, Wilton L, Wang M, Vlahov D, Nelson LE. Confidence and Hesitancy During the Early Roll-out of COVID-19 Vaccines Among Black, Hispanic, and Undocumented Immigrant Communities: a Review. J Urban Health. 2022;99:3-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 66] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 14. | Thangaraju P, Venkatesan S. WHO Ten threats to global health in 2019: Antimicrobial resistance. CUMJ. 2019;44:1150-1151. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Wagner AL, Rajamoorthy Y, Taib NM. Impact of economic disruptions and disease experiences on COVID-19 vaccination uptake in Asia: A study in Malaysia. Narra J. 2021;1:e42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Hassan W, Kazmi SK, Tahir MJ, Ullah I, Royan HA, Fahriani M, Nainu F, Rosa SGV. Global acceptance and hesitancy of COVID-19 vaccination: A narrative review. Narra J. 2021;1:e57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 17. | Asma S, Akan H, Uysal Y, Poçan AG, Sucaklı MH, Yengil E, Gereklioğlu Ç, Korur A, Başhan İ, Erdogan AF, Özşahin AK, Kut A. Factors effecting influenza vaccination uptake among health care workers: a multi-center cross-sectional study. BMC Infect Dis. 2016;16:192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 18. | Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, Yeo LLL, Ahmad A, Ahmed Khan F, Napolean Shanmugam G, Sharma AK, Komalkumar RN, Meenakshi PV, Shah K, Patel B, Chan BPL, Sunny S, Chandra B, Ong JJY, Paliwal PR, Wong LYH, Sagayanathan R, Chen JT, Ying Ng AY, Teoh HL, Tsivgoulis G, Ho CS, Ho RC, Sharma VK. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559-565. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1009] [Cited by in RCA: 996] [Article Influence: 199.2] [Reference Citation Analysis (0)] |
| 19. | Sun S, Lin D, Operario D. Interest in COVID-19 vaccine trials participation among young adults in China: Willingness, reasons for hesitancy, and demographic and psychosocial determinants. Prev Med Rep. 2021;22:101350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 20. | Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1142] [Cited by in RCA: 1638] [Article Influence: 327.6] [Reference Citation Analysis (0)] |
| 21. | Karafillakis E, Larson HJ; ADVANCE consortium. The benefit of the doubt or doubts over benefits? A systematic literature review of perceived risks of vaccines in European populations. Vaccine. 2017;35:4840-4850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 194] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 22. | Harapan H, Anwar S, Yufika A, Sharun K, Gachabayov M, Fahriani M, Husnah M, Raad R, Abdalla RY, Adam RY, Khiri NM, Ismaeil MI, Ismail AY, Kacem W, Dahman NB, Teyeb Z, Aloui K, Hafsi M, Ferjani M, Deeb DA, Emad D, Abbas KS, Monib FA, Sami FS, Subramaniam R, Panchawagh S, Anandu S, Haque MA, Ferreto LE, Briones MF, Morales RB, Díaz SA, Aburto JT, Rojas JE, Balogun EO, Enitan SS, Yomi AR, Durosinmi A, Ezigbo ED, Adejumo EN, Babadi E, Kakemam E, Malik NI, Ullah I, Rosiello DF, Emran TB, Wendt GW, Arab-Zozani M, Wagner AL, Mudatsir M. Vaccine hesitancy among communities in ten countries in Asia, Africa, and South America during the COVID-19 pandemic. Pathog Glob Health. 2022;116:236-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 23. | Boche B, Kebede O, Damessa M, Gudeta T, Wakjira D. Health Professionals' COVID-19 Vaccine Acceptance and Associated Factors in Tertiary Hospitals of South-West Ethiopia: A Multi-Center Cross- Sectional Study. Inquiry. 2022;59:469580221083181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 24. | Iwuafor A, Ogban G, Ita O, Offiong A, Owai P, Udoh U, Elem D. Determinants of COVID-19 vaccine acceptance amongst doctors practising in Cross River State, Nigeria. Af J Clin Exp Micro. 2023;24:147-157. [DOI] [Full Text] |
| 25. | Olu-Abiodun O, Abiodun O, Okafor N. COVID-19 vaccination in Nigeria: A rapid review of vaccine acceptance rate and the associated factors. PLoS One. 2022;17:e0267691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 34] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 26. | Eze UA, Ndoh KI, Ibisola BA, Onwuliri CD, Osiyemi A, Ude N, Chime AA, Ogbor EO, Alao AO, Abdullahi A. Determinants for Acceptance of COVID-19 Vaccine in Nigeria. Cureus. 2021;13:e19801. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 27. | Al-Mustapha AI, Okechukwu O, Olayinka A, Muhammed OR, Oyewo M, Owoicho SA, Abubakar AT, Olabisi A, Jibril A, Ereh S, Fakayode OE, Ogundijo OA, Elelu N, Adetunji VO. A national survey of COVID-19 vaccine acceptance in Nigeria. Vaccine. 2022;40:4726-4731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 28. | Alice TE, Okonofua M, Adeke A, Obi A. Willingness to Accept a COVID-19 Vaccine in Nigeria: A Population-based Cross-sectional Study. CAJPH. 2021;7:53. [DOI] [Full Text] |
| 29. | Njoga EO, Mshelbwala PP, Abah KO, Awoyomi OJ, Wangdi K, Pewan SB, Oyeleye FA, Galadima HB, Alhassan SA, Okoli CE, Kwaja EZ, Onwumere-Idolor OS, Atadiose EO, Awoyomi PO, Ibrahim MA, Lawan KM, Zailani SA, Salihu MD, Rupprecht CE. COVID-19 Vaccine Hesitancy and Determinants of Acceptance among Healthcare Workers, Academics and Tertiary Students in Nigeria. Vaccines (Basel). 2022;10:626. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 30. | Nindrea RD, Usman E, Katar Y, Sari NP. Acceptance of COVID-19 vaccination and correlated variables among global populations: A systematic review and meta-analysis. Clin Epidemiol Glob Health. 2021;12:100899. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 31. | Reed-Thryselius S, Fuss L, Rausch D. The Relationships Between Socioeconomic Status, COVID-19 Risk Perceptions, and the Adoption of Protective Measures in a Mid-Western City in the United States. J Community Health. 2022;47:464-474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Fenta ET, Tiruneh MG, Delie AM, Kidie AA, Ayal BG, Limenh LW, Astatkie BG, Workie NK, Yigzaw ZA, Bogale EK, Anagaw TF. Health literacy and COVID-19 vaccine acceptance worldwide: A systematic review. SAGE Open Med. 2023;11:20503121231197869. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 33. | Kirbiš A. The Impact of Socioeconomic Status, Perceived Threat and Healthism on Vaccine Hesitancy. Sustainability. 2023;15:6107. [DOI] [Full Text] |
| 34. | Montagni I, Ouazzani-Touhami K, Mebarki A, Texier N, Schück S, Tzourio C; CONFINS group. Acceptance of a Covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health (Oxf). 2021;43:695-702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 140] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 35. | Tijani B, Filani T, Oluyide O, Odis A, Ezike E, Adewemimo A, Benjamin A, Joseph I, Sagar M, Akinreni T. COVID-19 Vaccine Uptake and its Determinants: Findings From A Web-Based Survey in Nigeria. EJMED. 2023;5:48-52. [DOI] [Full Text] |
| 36. | Zakari S, Ogbu CO, Zakari H, Chioma ES, Ijimbili SB, Idoko JE, Emmanuel AO, Nnenna AD, Agwara BC, Adokiye ES, Idowu AO, Edegbene OA, Anejo-okopi J. Acceptance and hesitancy of COVID-19 vaccine among university community members of Otukpo, Nigeria: a cross-sectional study. Discov glob soc. 2023;1:5. [DOI] [Full Text] |
| 37. | Padonou SGR, Kakaï Glèlè C, Accrombessi M, Adegbite BR, Dangbenon E, Bah H, Akogbeto E, Bah Chabi AI, Kaucley L, Sourakatou S, Dossou A, Batonon A, Bissouma-Ledjou T, Hounkpatin B. Assessment of COVID-19 Vaccine Acceptance and Its Associated Factors during the Crisis: A Community-Based Cross-Sectional Study in Benin. Vaccines (Basel). 2023;11:1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 38. | Omale UI, Oka OU, Amuzie CI, Uduma VU, Adeke AS, Ikegwuonu CO, Nkwo GE, Nwali UIA, Iyare O, Ewah RL, Nnachi OO, Ukpabi OO, Okeke IM. COVID-19 vaccination acceptance (uptake, hesitancy, intention to receive and timeliness of the intention to receive) and the determinants among health workers in Ebonyi state, Nigeria: an analytical cross-sectional study. BMJ Open. 2023;13:e068668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 39. | Cordina M, Lauri MA, Lauri J. Attitudes towards COVID-19 vaccination, vaccine hesitancy and intention to take the vaccine. Pharm Pract (Granada). 2021;19:2317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 114] [Article Influence: 28.5] [Reference Citation Analysis (0)] |
| 40. | Kourlaba G, Kourkouni E, Maistreli S, Tsopela CG, Molocha NM, Triantafyllou C, Koniordou M, Kopsidas I, Chorianopoulou E, Maroudi-Manta S, Filippou D, Zaoutis TE. Willingness of Greek general population to get a COVID-19 vaccine. Glob Health Res Policy. 2021;6:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 97] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 41. | Isiguzo GC, Stefanovics E, Unamba NN, Mbam TT, Anyaehie UG, Chukwu CC, Anyaehie UB, Osy-Eneze C, Ibezim EO, Okoro UG, Njoku PO, Adimekwe AI, Ibediro K, Stefanovics G, Iheanacho T. Perceptions of the COVID-19 Vaccine and Willingness to Receive Vaccination among Health Workers in Nigeria: A Cross-sectional Study. Niger J Clin Pract. 2024;27:102-108. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 42. | Kamal AM, Sarkar T, Khan MM, Roy SK, Khan SH, Hasan SMM, Hossain MS, Dell CA, Seale H, Islam MS. Factors Affecting Willingness to Receive COVID-19 Vaccine Among Adults: A Cross-sectional Study in Bangladesh. JHM. 2023;25:414-423. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 43. | Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021;39:2024-2034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 364] [Cited by in RCA: 348] [Article Influence: 87.0] [Reference Citation Analysis (0)] |
| 44. | Olawa B, Lawal A, Odoh I, Azikiwe J, Olawole A, Odusina E, Ayodele I, Ajayi O. Mistrust in government and COVID-19 vaccination acceptance in Nigeria: investigating the indirect roles of attitudes towards vaccination. J Egypt Public Health Assoc. 2023;98:1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 45. | Nehal KR, Steendam LM, Campos Ponce M, van der Hoeven M, Smit GSA. Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis. Vaccines (Basel). 2021;9:1071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 104] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 46. | Wang Q, Yang L, Jin H, Lin L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev Med. 2021;150:106694. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 214] [Cited by in RCA: 201] [Article Influence: 50.3] [Reference Citation Analysis (0)] |
| 47. | Gachabayov M, Sharun K, Felsenreich DM, Nainu F, Anwar S, Yufika A, Ophinni Y, Yamada C, Fahriani M, Husnah M, Raad R, Khiri NM, Abdalla RY, Adam RY, Ismaeil MI, Ismail AY, Kacem W, Teyeb Z, Aloui K, Hafsi M, Ferjani M, Dahman NBH, Deeb DA, Emad D, Abbas KS, Monib FA, Sami FS, Ramanarayanan S, Panchawagh S, Anandu S, Haque MA, Ferreto LE, Briones MF, Morales RB, Lazcano-Díaz S, Aburto JT, Rojas JE, Balogun EO, Kusuma HI, Yeni CM, Utami NA, Enitan SS, Yomi AR, Durosinmi A, Adejumo EN, Ezigbo ED, Babadi E, Kakemam E, Ullah I, Malik NI, Rosiello F, Emran TB, Imelda E, Wendt GW, Arab-Zozani M, Dhama K, Mudatsir M, Harapan H. Perceived risk of infection and death from COVID-19 among community members of low- and middle-income countries: A cross-sectional study. F1000Res. 2022;11:345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Reference Citation Analysis (0)] |
| 48. | Fojnica A, Osmanovic A, Đuzic N, Fejzic A, Mekic E, Gromilic Z, Muhovic I, Kurtovic-Kozaric A. COVID-19 vaccine acceptance and rejection in an adult population in Bosnia and Herzegovina. PLoS One. 2022;17:e0264754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 49. | Rhodes A, Hoq M, Measey MA, Danchin M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2021;21:e110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 153] [Cited by in RCA: 173] [Article Influence: 43.3] [Reference Citation Analysis (0)] |
| 50. | Yıldırım M, Güler A. Positivity explains how COVID-19 perceived risk increases death distress and reduces happiness. Pers Individ Dif. 2021;168:110347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 127] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 51. | Mustapha M, Lawal BK, Sha'aban A, Jatau AI, Wada AS, Bala AA, Mustapha S, Haruna A, Musa A, Ahmad MH, Iliyasu S, Muhammad S, Mohammed FZ, Ahmed AD, Zainal H. Factors associated with acceptance of COVID-19 vaccine among University health sciences students in Northwest Nigeria. PLoS One. 2021;16:e0260672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 52. | Kolawole OM, Aun II, Ogah JI, Folahan FF, Kolawole CF. Determinants of COVID-19 vaccine uptake in Kwara State, Nigeria: The role of public health management professionals in driving behavioral change. GHES. 2024;2:2462. [DOI] [Full Text] |
| 53. | Mahmood MY, Ashiru A, Shettima FB, Abdullahi AA, Ngulde AM, Abbas ZU, Jibrin IM, Musami UB, Wakawa IA. Personality Traits as Key Determinants of COVID-19 Vaccine Uptake among Healthcare Workers in Nigeria. NJM. 2023;32:293-301. [DOI] [Full Text] |
| 54. | Elsehrawy MG. Acceptance to take COVID-19 vaccine and its relation to COVID-19 infection. Ital J Med. 2024;18. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 55. | Gunawardhana N, Baecher K, Boutwell A, Pekwarake S, Kifem M, Ngong MG, Fondzeyuf A, Halle-Ekane G, Mbah R, Tih P, Dionne-Odom J, Tebit DM. COVID-19 vaccine acceptance and perceived risk among pregnant and non-pregnant adults in Cameroon, Africa. PLoS One. 2022;17:e0274541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 56. | Kreps S, Prasad S, Brownstein JS, Hswen Y, Garibaldi BT, Zhang B, Kriner DL. Factors Associated With US Adults' Likelihood of Accepting COVID-19 Vaccination. JAMA Netw Open. 2020;3:e2025594. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 468] [Cited by in RCA: 502] [Article Influence: 100.4] [Reference Citation Analysis (0)] |
| 57. | Masoud M, Bassyouni RH, Abdel-wahed WY, Al Hawamdeh MI, Nassar FM, Arishi N, Ziad A, Elsidig LA, Hamed NS. Acceptance of COVID-19 vaccination and associated factors in Middle East countries: a multinational study. AJM. 2024;60:1-10. [DOI] [Full Text] |
| 58. | Tran VD, Pak TV, Gribkova EI, Galkina GA, Loskutova EE, Dorofeeva VV, Dewey RS, Nguyen KT, Pham DT. Determinants of COVID-19 vaccine acceptance in a high infection-rate country: a cross-sectional study in Russia. Pharm Pract (Granada). 2021;19:2276. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 59. | Gallè F, Sabella EA, Roma P, De Giglio O, Caggiano G, Tafuri S, Da Molin G, Ferracuti S, Montagna MT, Liguori G, Orsi GB, Napoli C. Knowledge and Acceptance of COVID-19 Vaccination among Undergraduate Students from Central and Southern Italy. Vaccines (Basel). 2021;9:638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 85] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 60. | Ferrer R, Klein WM. Risk perceptions and health behavior. Curr Opin Psychol. 2015;5:85-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 525] [Article Influence: 52.5] [Reference Citation Analysis (0)] |
| 61. | Boonsaeng T, Carpio CE, Guerrero P, Sarasty O, Borja I, Hudson D, Macharia A, Shibia M. Perceived Risks of Infection, Hospitalization, and Death From COVID-19 at the Equator: Ecuador and Kenya. Disaster Med Public Health Prep. 2021;17:e34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 62. | Bartsch SM, O'Shea KJ, Ferguson MC, Bottazzi ME, Wedlock PT, Strych U, McKinnell JA, Siegmund SS, Cox SN, Hotez PJ, Lee BY. Vaccine Efficacy Needed for a COVID-19 Coronavirus Vaccine to Prevent or Stop an Epidemic as the Sole Intervention. Am J Prev Med. 2020;59:493-503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 206] [Cited by in RCA: 196] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 63. | Hossain MA, Hossain KMA, Sakel M, Kabir MF, Saunders K, Faruqui R, Hossain MS, Uddin Z, Kader M, Walton LM, Haque MO, Shafin R, Chakrovorty SK, Jahid IK. Knowledge, Attitudes, Behavioural Practises, and Psychological Impact Relating to COVID-19 Among People Living With Spinal Cord Injury During In-Patient Rehabilitation in Bangladesh. Front Neurol. 2021;12:739354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 64. | Olaoye I, Ekong A, Samuel A, Kelaiditi E, Myrissa K, Jacdonmi T, Gboyega F. Public beliefs and willingness to accept COVID-19 vaccines among adults in South-Western Nigeria: A cross-sectional study. AIMS Public Health. 2023;10:1-15. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 65. | Abate BB, Tilahun BD, Yayeh BM. Global COVID-19 vaccine acceptance level and its determinants: an umbrella review. BMC Public Health. 2024;24:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 19] [Article Influence: 19.0] [Reference Citation Analysis (0)] |