Published online Dec 25, 2024. doi: 10.5501/wjv.v13.i4.96476
Revised: September 14, 2024
Accepted: September 30, 2024
Published online: December 25, 2024
Processing time: 163 Days and 13.9 Hours
Experts expressed severe concerns over the possibility of increasing burden of infectious diseases as the planet’s climate began to change years ago. There have been increased rates of climate-related catastrophes and as global temperatures rise, emergence of certain viruses has become a serious concern. Vectors are su
Core Tip: Changing core temperatures and increased incidence of climate change catastrophes have led to certain infectious disease outbreaks across the globe. As the climate continues to change and leads to the destruction of local biodiversity, the consequent spread of vectors is predicted to lead to further escalation in vector-borne diseases. The global community has also expressed significant concern regarding the spread of known lethal pathogens such as malaria and the West Nile viruses. Development and implementation of National Health Adaptation Plans is recommended to predict and tackle these emerging threats effectively.
- Citation: Ali A, Shaikh A, Sethi I, Surani S. Climate change and the emergence and exacerbation of infectious diseases: A review. World J Virol 2024; 13(4): 96476
- URL: https://www.wjgnet.com/2220-3249/full/v13/i4/96476.htm
- DOI: https://dx.doi.org/10.5501/wjv.v13.i4.96476
Climate change is one of the most predictable and detrimental global hazards with significant long-term consequences on human health and well-being. Health impacts are visible on every continent as temperatures increase, sea levels rise, and a greater incidence of flooding and drought is observed[1,2]. These changes are significant as they threaten individual health crises and present a prominent threat to the public health sector. While a myriad of adverse health complaints, such as respiratory diseases, malnutrition, heat-related morbidity, and mortality, are escalated due to climate change, the emergence and dissemination of infectious diseases is of particular concern[2].
The relationship between climate change and infectious diseases is intricate, requiring views from multiple stand
This review aims to explore climate change's role in surfacing of infectious diseases through direct effects. By exploring this multifaceted relationship between climate change and infectious disease, this review aims to identify significant trends, highlight the ramifications, provide adaptation and mitigation strategies, and analyze the existing gaps. Through this, effective policy change decisions can be taken to prevent public health crises related to climate change.
Diseases transmitted through infected arthropod species, such as mosquitoes, sandflies, and ticks, are classified as vector-borne diseases. Climate readily affects the biological traits of both the vector and pathogen. Temperature variations can reshape the emergence of zoonotic diseases through changes in the number of vectors, transmission cycles, and the con
Dengue: Dengue, transmitted by Aedes mosquitoes, is among the most important vector-borne diseases worldwide with a high disease burden. Increasing temperatures exhibit an almost exponential pattern on the species’ physiological traits, such as biting and development rates for vectors up to a certain level before tapering off. Similarly, increased rainfall facilitates the development of mosquito breeding sites up to a certain threshold, after which flooding demolishes them[6]. The primary vectors for dengue Aedes aegyptii and Ae. Albopictus has increased in transmission by 10% and 15% since 1950 due to greater climate suitability[7]. Increased precipitation and temperatures due to climate change are pro
Moreover, long-term weather and population estimations predict 50%-60% of the population to be at threat of dengue virus by 2085 compared to 35% of the population at risk if climate change did not ensue[9]. These projections are alar
Malaria: Malaria is a life-threatening disease caused by the Plasmodium parasites transmitted by the female Anopheles mosquitoes. Although the past five years have witnessed a decrease in the incidence of this disease owing to a range of human interventions, climate change can still cause increased transmission[6]. Spread of malaria is affected by ecological factors such as temperatures, precipitation, and topography[10]. As a result, equatorial regions with lower altitudes, increased rainfall, warmer temperatures, and higher humidity are favorable for the vector’s reproduction and longevity. Studies demonstrate that based on the projected climate change scenarios of longer monsoon periods and increased temperatures in tropical areas of Africa, the Anopheles vector is expected to widen its distribution area[8]. Similarly, geographical expansion of the virus is predicted in various other parts of the world, such as in Southern Europe, South Africa, China, and the highland areas of Columbia and Ethiopia[8,9]. These predicted projections underscore the global impact of climate change on public health and serve as a reminder to adopt enhanced policies for vector control and slowing down climate change to mitigate the risks of infectious diseases.
West Nile virus: West Nile virus (WNV), primarily transmitted by the Culex species of mosquitoes, can cause serious health infections ranging from mild febrile illness to severe meningitis or encephalitis. The principal hosts for these mosquitoes are wild migratory birds, but there have been cases of human-to-human transmission (through blood or transplacental transfusions)[10]. Temperature appears to be the predominant factor in WNV transmission. Optimum temperatures regulate vector growth rate, mosquito survival, and external incubation time period[11]. As temperatures increase (up to a certain threshold), the virus develops within vectors, and their transmission becomes increasingly effi
Lyme disease is the most common vector-borne disease in North America and Europe. It is caused by the Borrelia bur
Similarly, a 10% increase in infection susceptibility at the end of the century is predicted for Slovenia, a country that is already vulnerable to Lyme disease[17]. These alarming projections raise concerns 1about the pervasive influence of climate change on disease proliferation. Without proper mitigation strategies to minimize climate change, increasing suitable habitats and disease prevalence run the risk of aggravating public health catastrophes.
Food-borne diseases are those transmitted by eating food infected with pathogens or toxins. The risk of foodborne illness can be directly modified through high temperatures, causing amplification of replication cycles and growth, survival, and easy transfer of the pathogens. Drastic heat and precipitation can influence pathogens, worsening the risk of gastroin
Salmonella is another food-borne pathogen causing global outbreaks. Increase in temperatures directly influences Salmonella’s reproduction rates as an upsurge in ambient temperature correlates with incidence spikes. In Maryland, the likelihood of infection was related to extreme heat events between 2002-2012[20]. According to studies, a 5.6% and 8.8% increase in the incidence of cases was anticipated with a 1°C increase in mean weekly minimum and maximum temperatures, respectively[21].
Meningococcal meningitis is an infection of meninges, caused by the bacteria Neisseria meningitidis, that causes high death rates in developing countries. It is believed that increased concentration of dust, high winds, elevated temperatures, and low humidity may cause damage to nasopharyngeal mucosa leading to increased susceptibility to meningitis[22].
COVID-19 cases and temperature have also shown a positive correlation[23]. It is possible that extreme heat forces people indoors which can increase the risk of virus transmission.
A detailed review published in Nature expanded upon how often, and through which mechanisms, climate change aggravates infectious diseases. It found that more than 50% of pathogenic diseases have, at some point, been exacerbated directly by climate change with most cases being impacted by warming, precipitation, and flooding leading to the aggravation in vector-borne, waterborne and airborne diseases, respectively[24].
Some pragmatic mechanisms that have been identified include increase in proximity of pathogens and human beings through these changes in climate. Wildlife migration due to changing temperatures and habitability of regions[25] cou
In addition to this, the World Health Organization, more than a decade ago, found that climate change will cause an additional burden of certain diseases, such as diarrheal disease, directly due to the impact of climate change. It also suggested increased rates of malaria by up to 5% due to temperature surges[29].
The Center for Disease Control reports that infectious diseases have been on an upward trajectory. For example, cases of tick-borne diseases have increased from 10000 cases per year to 60000 cases per year from 2001 to 2019 in the United States[30]. Furthermore, currently it is assumed that 25% of the global population consumes fecally contaminated water. As droughts worsen due to increased temperatures in certain parts of the world and access to clean drinking water is further restricted, these rates will likely rise in certain vulnerable regions leading to worsening of water-borne diseases in these geographies[31]. Certain viruses such as Zika and Chikungunya have also been demonstrating increased geogra
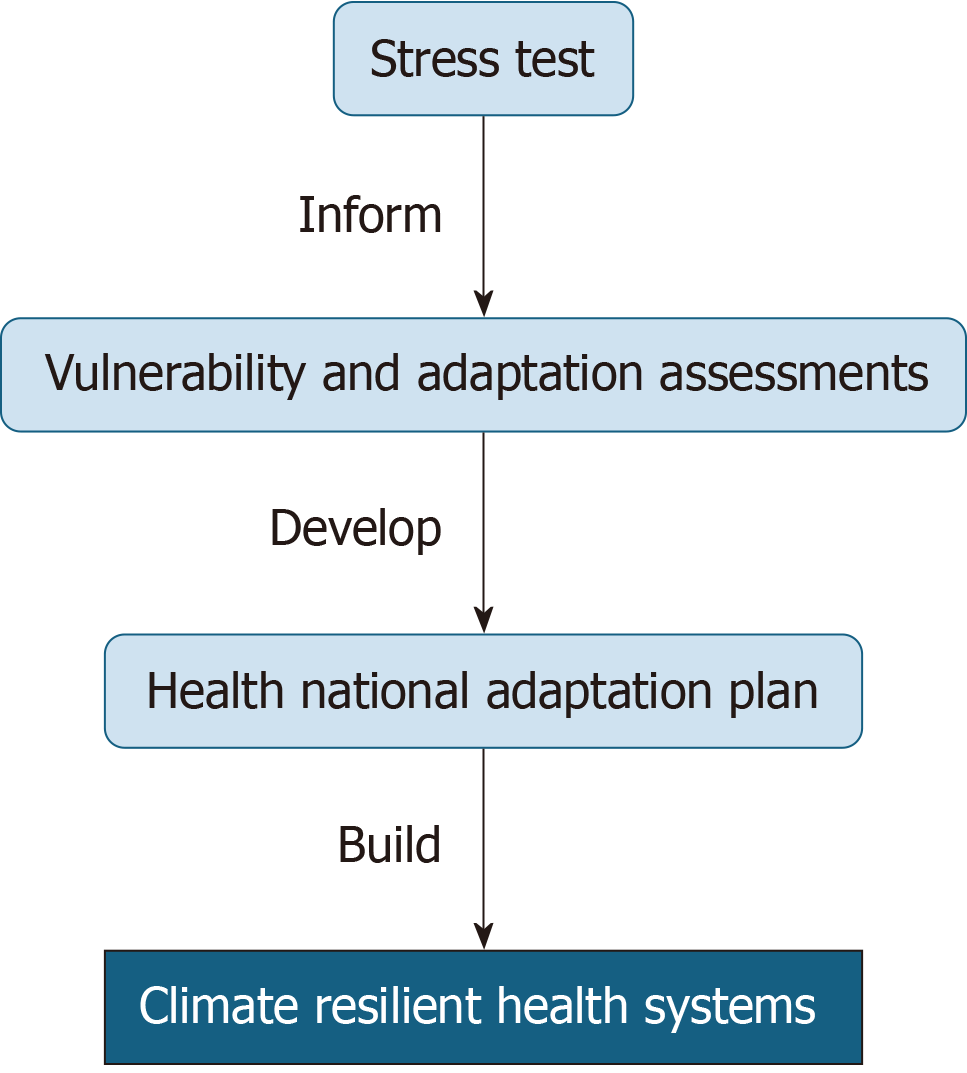
Adaption and mitigation strategies are crucial in diminishing climate change's ramifications on infectious diseases. Adaptation strategies focus on tackling climate change[33]. Key strategies include modeling climate resilient health systems that include a (1) Well-informed health workforce equipped with the necessary mechanisms to assist climate resilience; (2) Health information systems that facilitate skillful handling of health risks arising from extreme events caused by climate change; (3) Efficient service distribution including necessary foundations in cases of emergencies; and (4) Sufficient financing[34] and improving education[35]. However, in order to build these climate-resilient health sys
Vulnerability and adaptation assessments should inspect the capabilities of health systems and services to resist extreme events caused by climate change. Stress tests can provide scenario-based evaluations to complement these assessments through recognition of circumstances under which health systems would struggle to manage climate-dependent health outcomes[37,38]. A summary of these key adaptation strategies is illustrated below in Figure 1.
Adaptation strategies go in junction with mitigation measures that are also important in controlling the ramifications of climate change on health systems. Mitigation denotes to pursuits that curb greenhouse gas emissions or remove them from the atmosphere[33]. Afforestation and tree-planting programs, intensifying energy effectiveness in operations, and greening vehicle fleets are all helpful mitigation strategies for reducing the impact of climate change[33,37]. A multidis
Despite the strong relationship between climate change and infectious diseases, significant limitations persist in research. While the effects of climate change and infectious diseases are commonly studied in developed countries, underdeve
Infectious diseases related to climate change can be prevented. This review highlights sufficient evidence to emphasize climate change's role in exacerbating and developing infectious diseases, particularly vector-borne and food-borne, in regions where they did not exist previously. Without proper adaptations and mitigation strategies, the projections pro
| 1. | Watts N, Amann M, Arnell N, Ayeb-Karlsson S, Beagley J, Belesova K, Boykoff M, Byass P, Cai W, Campbell-Lendrum D, Capstick S, Chambers J, Coleman S, Dalin C, Daly M, Dasandi N, Dasgupta S, Davies M, Di Napoli C, Dominguez-Salas P, Drummond P, Dubrow R, Ebi KL, Eckelman M, Ekins P, Escobar LE, Georgeson L, Golder S, Grace D, Graham H, Haggar P, Hamilton I, Hartinger S, Hess J, Hsu SC, Hughes N, Jankin Mikhaylov S, Jimenez MP, Kelman I, Kennard H, Kiesewetter G, Kinney PL, Kjellstrom T, Kniveton D, Lampard P, Lemke B, Liu Y, Liu Z, Lott M, Lowe R, Martinez-Urtaza J, Maslin M, McAllister L, McGushin A, McMichael C, Milner J, Moradi-Lakeh M, Morrissey K, Munzert S, Murray KA, Neville T, Nilsson M, Sewe MO, Oreszczyn T, Otto M, Owfi F, Pearman O, Pencheon D, Quinn R, Rabbaniha M, Robinson E, Rocklöv J, Romanello M, Semenza JC, Sherman J, Shi L, Springmann M, Tabatabaei M, Taylor J, Triñanes J, Shumake-Guillemot J, Vu B, Wilkinson P, Winning M, Gong P, Montgomery H, Costello A. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397:129-170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1058] [Cited by in RCA: 839] [Article Influence: 209.8] [Reference Citation Analysis (0)] |
| 2. | Rocque RJ, Beaudoin C, Ndjaboue R, Cameron L, Poirier-Bergeron L, Poulin-Rheault RA, Fallon C, Tricco AC, Witteman HO. Health effects of climate change: an overview of systematic reviews. BMJ Open. 2021;11:e046333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 412] [Article Influence: 103.0] [Reference Citation Analysis (0)] |
| 3. | Tajudeen YA, Oladunjoye IO, Adebayo AO, Adebisi YA. The need to adopt planetary health approach in understanding the potential influence of climate change and biodiversity loss on zoonotic diseases outbreaks. Public Health Pract (Oxf). 2021;2:100095. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 4. | Coates SJ, Enbiale W, Davis MDP, Andersen LK. The effects of climate change on human health in Africa, a dermatologic perspective: a report from the International Society of Dermatology Climate Change Committee. Int J Dermatol. 2020;59:265-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Esposito MM, Turku S, Lehrfield L, Shoman A. The Impact of Human Activities on Zoonotic Infection Transmissions. Animals (Basel). 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 50] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 6. | Colón-González FJ, Sewe MO, Tompkins AM, Sjödin H, Casallas A, Rocklöv J, Caminade C, Lowe R. Projecting the risk of mosquito-borne diseases in a warmer and more populated world: a multi-model, multi-scenario intercomparison modelling study. Lancet Planet Health. 2021;5:e404-e414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 193] [Article Influence: 48.3] [Reference Citation Analysis (0)] |
| 7. | Kulkarni MA, Duguay C, Ost K. Charting the evidence for climate change impacts on the global spread of malaria and dengue and adaptive responses: a scoping review of reviews. Global Health. 2022;18:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 55] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 8. | Semenza JC, Rocklöv J, Ebi KL. Climate Change and Cascading Risks from Infectious Disease. Infect Dis Ther. 2022;11:1371-1390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 114] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 9. | Rupasinghe R, Chomel BB, Martínez-López B. Climate change and zoonoses: A review of the current status, knowledge gaps, and future trends. Acta Trop. 2022;226:106225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 69] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 10. | Chala B, Hamde F. Emerging and Re-emerging Vector-Borne Infectious Diseases and the Challenges for Control: A Review. Front Public Health. 2021;9:715759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 151] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 11. | D'Amore C, Grimaldi P, Ascione T, Conti V, Sellitto C, Franci G, Kafil SH, Pagliano P. West Nile Virus diffusion in temperate regions and climate change. A systematic review. Infez Med. 2022;31:20-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 12. | Farooq Z, Sjödin H, Semenza JC, Tozan Y, Sewe MO, Wallin J, Rocklöv J. European projections of West Nile virus transmission under climate change scenarios. One Health. 2023;16:100509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 31] [Reference Citation Analysis (0)] |
| 13. | Beermann S, Dobler G, Faber M, Frank C, Habedank B, Hagedorn P, Kampen H, Kuhn C, Nygren T, Schmidt-Chanasit J, Schmolz E, Stark K, Ulrich RG, Weiss S, Wilking H. Impact of climate change on vector- and rodent-borne infectious diseases. J Health Monit. 2023;8:33-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 14. | Frank C, Schmidt-Chanasit J, Ziegler U, Lachmann R, Preußel K, Offergeld R. West Nile Virus in Germany: An Emerging Infection and Its Relevance for Transfusion Safety. Transfus Med Hemother. 2022;49:192-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | Alkishe A, Raghavan RK, Peterson AT. Likely Geographic Distributional Shifts among Medically Important Tick Species and Tick-Associated Diseases under Climate Change in North America: A Review. Insects. 2021;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 16. | Carignan A, Valiquette L, Laupland KB. Impact of climate change on emerging infectious diseases: Implications for Canada. J Assoc Med Microbiol Infect Dis Can. 2019;4:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Deshpande G, Beetch JE, Heller JG, Naqvi OH, Kuhn KG. Assessing the Influence of Climate Change and Environmental Factors on the Top Tick-Borne Diseases in the United States: A Systematic Review. Microorganisms. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 18. | Kuhn KG, Nygård KM, Guzman-Herrador B, Sunde LS, Rimhanen-Finne R, Trönnberg L, Jepsen MR, Ruuhela R, Wong WK, Ethelberg S. Campylobacter infections expected to increase due to climate change in Northern Europe. Sci Rep. 2020;10:13874. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 19. | Djennad A, Lo Iacono G, Sarran C, Lane C, Elson R, Höser C, Lake IR, Colón-González FJ, Kovats S, Semenza JC, Bailey TC, Kessel A, Fleming LE, Nichols GL. Seasonality and the effects of weather on Campylobacter infections. BMC Infect Dis. 2019;19:255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 20. | Welch K, Shipp-Hilts A, Eidson M, Saha S, Zansky S. Salmonella and the changing environment: systematic review using New York State as a model. J Water Health. 2019;17:179-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Dietrich J, Hammerl JA, Johne A, Kappenstein O, Loeffler C, Nöckler K, Rosner B, Spielmeyer A, Szabo I, Richter MH. Impact of climate change on foodborne infections and intoxications. J Health Monit. 2023;8:78-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 22. | World Bank Group. Data: Nigeria. [Cited August 2024]. Available from: http://data.worldbank.org/country/nigeria. |
| 23. | Shenoy A, Sharma B, Xu G, Kapoor R, Rho HA, Sangha K. God is in the rain: The impact of rainfall-induced early social distancing on COVID-19 outbreaks. J Health Econ. 2022;81:102575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 24. | Mora C, McKenzie T, Gaw IM, Dean JM, von Hammerstein H, Knudson TA, Setter RO, Smith CZ, Webster KM, Patz JA, Franklin EC. Over half of known human pathogenic diseases can be aggravated by climate change. Nat Clim Chang. 2022;12:869-875. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 322] [Article Influence: 107.3] [Reference Citation Analysis (0)] |
| 25. | Butler CD, Harley D. Primary, secondary and tertiary effects of eco-climatic change: the medical response. Postgrad Med J. 2010;86:230-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 26. | Guzman Herrador BR, de Blasio BF, MacDonald E, Nichols G, Sudre B, Vold L, Semenza JC, Nygård K. Analytical studies assessing the association between extreme precipitation or temperature and drinking water-related waterborne infections: a review. Environ Health. 2015;14:29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 27. | Gubler DJ, Reiter P, Ebi KL, Yap W, Nasci R, Patz JA. Climate variability and change in the United States: potential impacts on vector- and rodent-borne diseases. Environ Health Perspect. 2001;109 Suppl 2:223-233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 204] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 28. | Anwar A, Anwar S, Ayub M, Nawaz F, Hyder S, Khan N, Malik I. Climate Change and Infectious Diseases: Evidence from Highly Vulnerable Countries. Iran J Public Health. 2019;48:2187-2195. [PubMed] |
| 29. | Shuman EK. Global climate change and infectious diseases. N Engl J Med. 2010;362:1061-1063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 117] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 30. | NETEC. Climate Change and Infectious Diseases. Cited: 2024 September. Available from: https://netec.org/2024/03/25/climate-change-and-infectious-diseases/#:~:text=Climate%20change%20trends%20such%20as,the%20spread%20of%20infectious%20diseases. |
| 31. | Gall AM, Mariñas BJ, Lu Y, Shisler JL. Waterborne Viruses: A Barrier to Safe Drinking Water. PLoS Pathog. 2015;11:e1004867. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 150] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 32. | Taylor L. Dengue and chikungunya cases surge as climate change spreads arboviral diseases to new regions. BMJ. 2023;380:717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 33. | Ngonghala CN, Ryan SJ, Tesla B, Demakovsky LR, Mordecai EA, Murdock CC, Bonds MH. Effects of changes in temperature on Zika dynamics and control. J R Soc Interface. 2021;18:20210165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 34. | Buse CG, Patrick R. Climate change glossary for public health practice: from vulnerability to climate justice. J Epidemiol Community Health. 2020;74:867-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 35. | Ebi KL, Vanos J, Baldwin JW, Bell JE, Hondula DM, Errett NA, Hayes K, Reid CE, Saha S, Spector J, Berry P. Extreme Weather and Climate Change: Population Health and Health System Implications. Annu Rev Public Health. 2021;42:293-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 271] [Article Influence: 67.8] [Reference Citation Analysis (0)] |
| 36. | World Health Organization. Operational framework for building climate resilient health systems [Internet]. Geneva: World Health Organization; 2015. [Cited: March 2024]. Available from: https://iris.who.int/handle/10665/189951. |
| 37. | Ebi KL, Berry P, Hayes K, Boyer C, Sellers S, Enright PM, Hess JJ. Stress Testing the Capacity of Health Systems to Manage Climate Change-Related Shocks and Stresses. Int J Environ Res Public Health. 2018;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 38. | Jacobsen AP, Khiew YC, Duffy E, O'Connell J, Brown E, Auwaerter PG, Blumenthal RS, Schwartz BS, McEvoy JW. Climate change and the prevention of cardiovascular disease. Am J Prev Cardiol. 2022;12:100391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |