Published online Jun 25, 2024. doi: 10.5501/wjv.v13.i2.92115
Revised: April 4, 2024
Accepted: April 18, 2024
Published online: June 25, 2024
Processing time: 160 Days and 17.6 Hours
Birth-dose (Hep-BD) followed by three additional doses (Hep-B3) of hepatitis B virus (HBV) vaccine are key to eliminating HBV by 2030. Unfortunately, Hep-BD and Hep-B3 coverage in our country is poor.
To studied the parent’s knowledge and awareness about HBV infection, its prevention, consequences and vaccination.
Parents of 6 months to 8 years old children were interviewed to assess their knowledge & awareness about hepatitis B, its transmission, prevention, illness caused by this, and vaccination. Eighteen close-ended questions were admini
Parents (58.3% mothers) of 384 children (89.9% age < 5 years; 82% age-appropriately vaccinated) were included. Three hundred and twenty-two (83.9%) children were Hep-B3 vaccinated. 94.3%, 87.5%, and 29.2% parents knew about polio, tetanus, and hepatitis B vaccine. Overall, 41.2%, 15.8%, and 23% parents knew about hepatitis B transmission, consequences of infection, and prevention respectively. Only 7.6% parents knew about three-dose schedule of hepatitis B vaccination. Only 23% parents believed that vaccine could prevent HBV, 15.7% knew that HBV affects liver. Parents of Hep-B3 vaccinated children were significantly more aware about HBV than the parents of unvaccinated children (P < 0.05 for 17/18 questions).
The knowledge and awareness among the parents about hepatitis B is poor. The Increasing knowledge/awareness about HBV among parents may improve Hep-B3 vaccination coverage.
Core Tip: Hepatitis B infection can be prevented with vaccination. Birth dose followed by three doses of hepatitis B vaccine in infancy is one of the key intervention to prevent hepatitis B transmission. Unfortunately, the coverage of hepatitis B vaccination among newborns are not adequate in India. Our article identified that the parents have poor knowledge about the hepatitis B and increasing knowledge/awareness about hepatitis B virus among parents may improve Hepatitis B vaccine coverage in the country.
- Citation: Chhavi N, Srivastava G, Waseem M, Yadav A, Singh S, Singh R, Goel A. Parents’s knowledge and awareness about hepatitis B can influence the vaccination of their children. World J Virol 2024; 13(2): 92115
- URL: https://www.wjgnet.com/2220-3249/full/v13/i2/92115.htm
- DOI: https://dx.doi.org/10.5501/wjv.v13.i2.92115
Hepatitis B virus (HBV) infection is common in India. Chronic hepatitis B (CHB) infection could lead to liver cirrhosis and hepatocellular carcinoma. Globally, over two billion people have evidence of past HBV infection, 360 million are living with CHB, and 600000 people die annually from the consequences of HBV infection[1]. Recent estimates suggest that 2.9% people in India have HBV infection[2] and it accounts for approximately 11% of cirrhosis burden in the country[3].
HBV infection progresses to CHB in approximately 90% of infants, approximately 20% in children of 1–5 years of age, and 5%–10% in children over 5 years of age and adults[4]. Globally, most of the HBV infections to children are trans
The World Health Organization (WHO) aims to eliminate HBV as a public health problem by the end of year 2030. Hepatitis B elimination is defined as 90% and 65% reduction in new HBV cases and HBV related deaths respectively from baseline estimates of 2015. Successful elimination of HBV can be achieved by attaining the proposed WHO targets. One of the targets is to vaccinate 90% or more newborns with Hep-BD and Hep-B3[5].
Though we are only a few years away from 2030, the Hep-BD and Hep-B3 coverages in our country is far less than the proposed target of ≥ 90%. Several factors are responsible for the inadequate HBV vaccination in our country. Inadequate knowledge and awareness of the parents about the HBV may be one of them[6]. Data are limited to the awareness and knowledge of the parents about HBV. Our aim was to study the association of parents’ knowledge and awareness about HBV infection, its prevention, and sequelae with the hepatitis B vaccination status of their children.
Prospective, single arm, observational, cross-sectional study was conducted in Era’s Lucknow Medical College and Hospital, Lucknow, India. Participants were enrolled between March 2020-December 2021.
Parents accompanying their 6 months to 8 years old children in out-patient clinic were screened and eligible parents were included after written informed consent for participation and publication of data. Parents with one or more HBsAg positive family members on either of the parent’s side were excluded. If both the parents were available for participation, then data were collected from only mother.
Data were collected in a predefined data collection form which had three sections; first section explored the awareness of the parents about the various vaccine given to prevent common childhood illness; second section included data from the vaccination card of the child to assess the vaccination status of the child; third section, explored the parents’ knowledge and awareness about HBV infection, its prevention and transmission. The data collection form was completed by the parents with the help of a physician in an isolated and silent place and sufficient time was given to understand and respond.
We applied close-ended questions and responses were recorded as ‘yes’, ‘no’, or ‘not sure’. It took 10-15 min to complete the data collection form. The knowledge and awareness of the parents on HBV were assessed about disease epidemiology (three questions), routes of transmission (seven question), consequences of its infection (four questions), prevention (three questions), and treatment (one question). The questions were drafted after discussion with faculty members, and the viral hepatitis experts, who were working at various level of seniority. Before starting the study, we piloted our questionnaire in 25 parents and made appropriate changes.
HBV knowledge score of a participant was calculated based on the sum of correct answers given to the set of 18 questions. A correct response to each question received one point. Responses recorded as either incorrect, not sure, or missing scored zero point. Data in various domains were summarized as median. Categorical data are presented as number (%) and numerical data are expressed as median (interquartile range). Data are compared using χ2 tests and Mann-Whitney U tests with level of significance kept as P < 0.05.
Study was approved by the institute ethic committee (ELMC & H/R_Cell/EC/2020/20).
Of the 408 parents who participated in the study, 24 were excluded because of incomplete data (n = 16) or having HBsAg positive family member (n = 8). Data from the remaining 384 were analyzed. Demographic characteristics of the parents and their children are summarized in Table 1. In our cohort, 58.3% respondents were mothers, and 89.9% children were of < 5 years of age. Over 86% children had received their primary vaccination primarily in government hospital. Among children, 315 (82%) were age appropriately vaccinated at the time of interview of their parents, and 322 (83.9%) had received all the three doses of Hep-B3.
| Character | Value |
| Gender of the child (boys) | 226 (58.9) |
| Age (months) | |
| ≤ 18 | 167 (43.5) |
| 19-59 | 175 (45.6) |
| ≥ 60 | 42 (10.9) |
| Birth order | |
| First | 208 (54.2) |
| Second | 116 (30.2) |
| Third | 38 (9.9) |
| Fourth | 17 (4.4) |
| Fifth | 5 (1.3) |
| Place of delivery | |
| Home delivery | 22 (5.7) |
| Hospital delivery | 362 (94.3) |
| Religion | |
| Hindu | 200 (52.1) |
| Muslim | 181 (47.1) |
| Other religion | 3 (0.8) |
| Residence | |
| Rural | 83 (21.6) |
| Urban | 301 (78.4) |
| Information provided by | |
| Mother | 224 (58.3) |
| Father | 135 (35.2) |
| Any other guardian | 25 (6.5) |
| Education of mother | |
| Illiterate | 76 (19.8) |
| Up to class 8th | 65 (16.9) |
| Class 9th to class 12th | 106 (27.6) |
| Graduate | 108 (28.1) |
| Postgraduate or professional | 29 (7.6) |
| Education of father | |
| Illiterate | 52 (13.5) |
| Up to class 8th | 78 (20.3) |
| Class 9th to class 12th | 98 (25.5) |
| Graduate | 109 (28.4) |
| Postgraduate or professional | 47 (12.2) |
| Setting in which vaccination were primarily done | |
| Public hospital | 331 (86.2) |
| Private hospital | 53 (13.8) |
| Parents perception about the vaccines | |
| Vaccine is a nutritional supplement | |
| Yes | 10 (2.6) |
| No | 317 (82.6) |
| Not sure | 57 (14.8) |
| Vaccine is given to promote growth | |
| Yes | 20 (5.2) |
| No | 311 (81) |
| Not sure | 53 (13.8) |
| Vaccine is given to prevent infections | |
| Yes | 359 (93.5) |
| No | 4 (1) |
| Not sure | 21 (5.5) |
Overall, 93.5% parents were aware that vaccines are given to prevent infections. Though a large proportion of parents were aware about vaccines against polio (94.3%) and tetanus (87.5%), only 29.2% parents had awareness about hepatitis B vaccine. Among Hep-B3 vaccinated children, 29.5% parents were aware about hepatitis B vaccine.
Parents were asked about the illness for which vaccines are given during the childhood. Their awareness was assessed by asking whether a vaccine is given for a particular childhood illness or not? The responses of the parents are summarized in Table 2. The awareness was highest for polio (94.3%) vaccine followed by tetanus (87.5%) and diarrhea (70%). Only 29.2% parents were aware that hepatitis B vaccine is also included in childhood immunization schedule.
| Vernacular name of the childhood illness | Response of the parents | |
| Yes | No | |
| Tuberculosis | 51.8 | 48.2 |
| Poliomyelitis | 94.3 | 5.7 |
| Hepatitis B virus | 29.2 | 70.8 |
| Diphtheria (Gal Ghotu) | 20 | 80 |
| Pertussis (Kali Khanshi) | 7.8 | 92.2 |
| Measles (Khasara) | 68 | 32 |
| Mumps (Galsua) | 29.7 | 70.3 |
| Pneumonia | 69 | 31 |
| Tetanus | 87.5 | 12.5 |
| Rubella | 10.2 | 89.8 |
| Diarrhoea | 70 | 30 |
| Meningitis/Encephalitis (Dimagi Bukhar) | 56.5 | 43.4 |
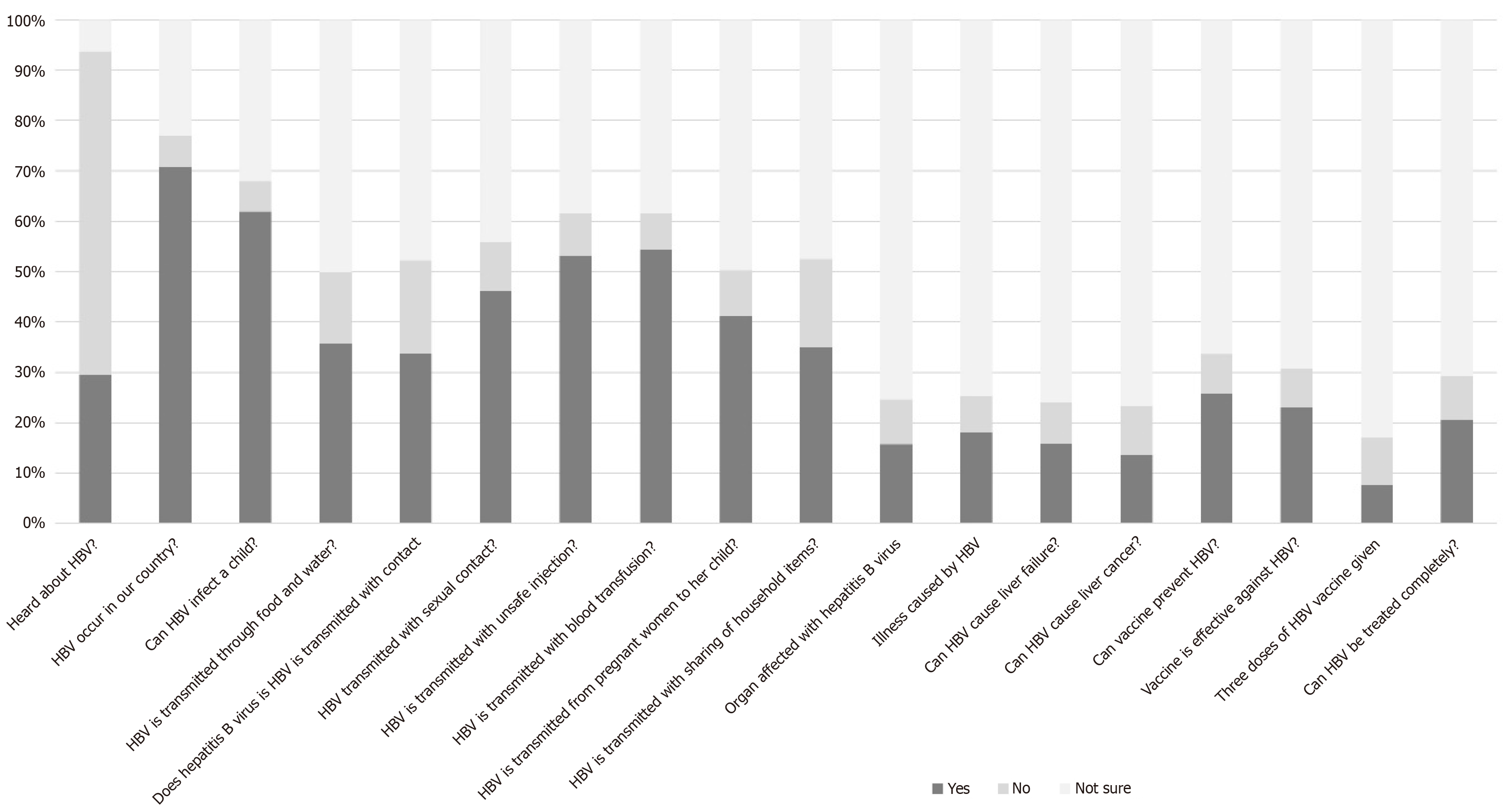
Of the 384 participants, 41.2% were aware about the routes of transmission, 15.8% had knowledge about the consequences of HBV infection, and 23% knew about prevention. Only 7.6% parents knew that three doses of HBV vaccine are given (Table 3). However, only 23% parents believed that vaccine could effectively prevent HBV infection. Further, only 15.7% of parents knew that HBV affects liver (Figure 1). None of the parents could correctly answer all eighteen questions.
| Domain examined | No. | Question | Response of the parents | Domain performance | ||
| Yes | No | Not sure | ||||
| Epidemiology | 1 | Have you heard about hepatitis B vaccine? | 29.5 | 64.2 | 6.3 | 61.9 |
| 2 | Does hepatitis B virus infection occur in our country? | 70.8 | 6.2 | 23 | ||
| 3 | Can hepatitis B virus infect a child? | 61.9 | 6.0 | 32.1 | ||
| Route of transmission | 4 | Does hepatitis B virus transmit through food and water? | 35.8 | 14.1 | 50.1 | 41.2 |
| 5 | Does hepatitis B virus transmit with casual contacts such as playing, handshake etc.? | 33.7 | 18.5 | 47.8 | ||
| 6 | Does hepatitis B virus transmit with sexual contact? | 46.2 | 9.7 | 44.1 | ||
| 7 | Does hepatitis B virus transmit with unsafe injection? | 53.2 | 8.4 | 38.4 | ||
| 8 | Does hepatitis B virus transmit with blood transfusion? | 54.3 | 7.3 | 38.4 | ||
| 9 | Does hepatitis B virus transmit from pregnant women to her child? | 41.2 | 9.1 | 49.7 | ||
| 10 | Does hepatitis B virus transmit with sharing of food, bed, utensils etc.? | 35.0 | 17.5 | 47.5 | ||
| Consequences of hepatitis B virus infection | 11 | Which organ is affected with hepatitis B virus? | 15.7 | 8.9 | 75.4 | 15.8 |
| 12 | What illness is caused by hepatitis B virus? (correct answer was Jaundice or similar phrases) | 18.0 | 7.3 | 74.7 | ||
| 13 | Can hepatitis B virus cause liver failure? | 15.9 | 8.1 | 76.0 | ||
| 14 | Can hepatitis B virus cause liver cancer? | 13.6 | 9.7 | 76.7 | ||
| Prevention of HBV infection | 15 | Is there any vaccine to prevent hepatitis B infection? | 25.8 | 7.8 | 66.4 | 23.0 |
| 16 | Is the vaccine effective against hepatitis B infection? | 23.0 | 7.8 | 69.2 | ||
| 17 | How many doses of hepatitis B vaccine are given in routine vaccination? (correct answer is three dose) | 7.6 | 9.4 | 83.0 | ||
| Treatment of hepatitis B | 18 | Can hepatitis B be treated completely? | 20.6 | 8.6 | 70.7 | 70.7 |
Demographic characteristics of the children with or without Hep-B3 vaccination were comparable (Table 4). As compared to the children without Hep-B3 vaccination, a significantly higher proportion of Hep-B3 vaccinated children were delivered in hospital (87% vs 96%; P < 0.01) and had received vaccines in a private clinic (73% vs 89%; P < 0.01). The parents of Hep-B3 vaccinated children were significantly more aware about hepatitis B than parents of Hep-B3 unvaccinated children (Table 5).
| Character | Values | P value | |
| Child is vaccinated for hepatitis B (n = 322) | Child is not vaccinated for hepatitis B (n = 62) | ||
| Gender of the child (boys) | 59 | 58 | 0.89 |
| Age (months) | 0.548 | ||
| ≤ 18 | 37 | 73 | |
| 19-59 | 51 | 18 | |
| ≥ 60 | 11 | 9 | |
| Birth order | 0.4 | ||
| First | 56 | 45 | |
| Second | 29 | 39 | |
| Third | 10 | 11 | |
| Fourth | 4 | 5 | |
| Fifth | 1 | 0 | |
| Place of delivery | < 0.01 | ||
| Home delivery | 4 | 13 | |
| Hospital delivery | 96 | 87 | |
| Religion | 0.08 | ||
| Hindu | 54 | 40 | |
| Muslim | 45 | 60 | |
| Other religion | 1 | 0 | |
| Residence | 0.14 | ||
| Rural | 23 | 14 | |
| Urban | 77 | 86 | |
| Education of mother | 0.13 | ||
| Illiterate | 20 | 16 | |
| Up to class 8th | 15 | 24 | |
| Class 9th to class 12th | 28 | 26 | |
| Graduate | 30 | 21 | |
| Postgraduate or professional | 7 | 13 | |
| Education of father | 0.32 | ||
| Illiterate | 14 | 13 | |
| Up to class 8th | 19 | 26 | |
| Class 9th to class 12th | 26 | 22 | |
| Graduate | 30 | 21 | |
| Postgraduate or professional | 11 | 18 | |
| Setting in which vaccination were primarily done | < 0.01 | ||
| Public hospital | 73 | 89 | |
| Private hospital | 27 | 11 | |
| Any family member has or had hepatitis B infection | 0.36 | ||
| Yes | 2 | 3 | |
| No | 90 | 84 | |
| Not sure | 8 | 13 | |
| No. | Question related to hepatitis B knowledge and awareness | Parents’ response | Childs vaccination status | P value | |
| Child is vaccinated for hepatitis B (n = 322) | Child is not vaccinated for hepatitis B (n = 62) | ||||
| 1 | Have you heard about hepatitis B vaccine? | Yes | 29 | 36 | 0.39 |
| No | 65 | 56 | |||
| Not sure | 6 | 8 | |||
| 2 | Does hepatitis B virus infection occur in our country? | Yes | 73 | 58 | 0.02 |
| No | 5 | 13 | |||
| Not sure | 22 | 29 | |||
| 3 | Can hepatitis B virus infect a child? | Yes | 65 | 47 | < 0.01 |
| No | 4 | 16 | |||
| Not sure | 31 | 37 | |||
| 4 | Does hepatitis B virus transmit through food and water? | Yes | 38 | 24 | 0.04 |
| No | 13 | 23 | |||
| Not sure | 49 | 53 | |||
| 5 | Does hepatitis B virus transmit with casual contacts such as playing, handshake etc.? | Yes | 37 | 19 | < 0.01 |
| No | 16 | 32 | |||
| Not sure | 47 | 49 | |||
| 6 | Does hepatitis B virus transmit with sexual contact? | Yes | 49 | 32 | < 0.01 |
| No | 8 | 21 | |||
| Not sure | 43 | 47 | |||
| 7 | Does hepatitis B virus transmit with unsafe injection? | Yes | 55 | 47 | 0.01 |
| No | 6 | 18 | |||
| Not sure | 39 | 35 | |||
| 8 | Does hepatitis B virus transmit with blood transfusion? | Yes | 56 | 43 | < 0.01 |
| No | 6 | 18 | |||
| Not sure | 38 | 39 | |||
| 9 | Does hepatitis B virus transmit from pregnant women to her child? | Yes | 44 | 29 | 0.01 |
| No | 7 | 18 | |||
| Not sure | 49 | 53 | |||
| 10 | Does hepatitis B virus transmit with sharing of food, bed, utensils etc.? | Yes | 38 | 21 | 0.02 |
| No | 16 | 27 | |||
| Not sure | 46 | 52 | |||
| 11 | Which organ is affected with hepatitis B virus? | Yes | 15 | 23 | 0.02 |
| No | 7 | 16 | |||
| Not sure | 78 | 61 | |||
| 12 | What illness is caused by hepatitis B virus? (answer was Jaundice or similar phrases) | Yes | 17 | 23 | < 0.01 |
| No | 6 | 18 | |||
| Not sure | 77 | 59 | |||
| 13 | Does hepatitis B virus cause liver failure? | Yes | 15 | 19 | < 0.01 |
| No | 6 | 19 | |||
| Not sure | 79 | 62 | |||
| 14 | Does hepatitis B virus cause liver cancer? | Yes | 13 | 18 | < 0.01 |
| No | 7 | 22 | |||
| Not sure | 80 | 60 | |||
| 15 | Is there any vaccine to prevent hepatitis B infection? | Yes | 26 | 27 | < 0.01 |
| No | 6 | 18 | |||
| Not sure | 68 | 55 | |||
| 16 | Is the vaccine effective to prevent hepatitis B infection? | Yes | 23 | 23 | < 0.01 |
| No | 6 | 18 | |||
| Not sure | 71 | 59 | |||
| 17 | How many doses of hepatitis B vaccine are given in routine vaccination? | Yes | 20 | 23 | < 0.01 |
| No | 6 | 21 | |||
| Not sure | 74 | 56 | |||
| 18 | Can hepatitis B be treated completely? | Yes | 8 | 6 | < 0.01 |
| No | 7 | 21 | |||
| Not sure | 85 | 73 | |||
The study showed that though 84% of children were vaccinated with Hep-B3 only 29% parents were aware about hepatitis B vaccine, and 7.6% knew about Hep-B3 vaccination schedule. This shows that the parents had poor faith on effectiveness of hepatitis B vaccine and only 23% believed that vaccine can prevent HBV infection. Overall, the knowledge about hepatitis B was poor among parents as none could correctly answer all the questions and only 15.7% knew that HBV affects liver.
The Expanded Program of Immunization (EPI) started in 1978, laid the foundation of childhood vaccination program in India. EPI provide vaccination for six vaccine preventable diseases, namely diphtheria, pertussis, tetanus, polio, tuberculosis, and measles. The Government of India accepted the WHO recommendation and included Hep-B3 in EIP in 2002 and gradually expanded to the entire country under the aegis of Universal Immunization Program. As of now, our national immunization schedule recommends Hep-BD within 24 h of birth followed by three doses of Hep-B3 at 6, 10 and 14 wk[7].
National Family Health Survey (NFHS)-5 reported that 77% and 70% of 12-23 months old children in the country and the state of Uttar Pradesh respectively, had received complete basic vaccination. In our study, 82% children were age-appropriately vaccinated. Our proportion was slightly higher than the national and state average because 78% were from urban background, 50% were first child of the family, 58% were boys, and only 20% mothers were illiterate. The NFHS-5 report suggests that these factors are associated with better vaccination coverage in the country[8].
We found that the parents had limited knowledge and awareness about the HBV, its transmission, illness caused by the virus, methods of HBV prevention, and its treatment. Poor awareness of the parents may be one of the reasons for the inadequate coverage for Hep-BD and Hep-B3 doses in the country. The NFHS-5 survey reported that only 67% and 84% of 12-23 months aged children were given Hep-BD and Hep-B3 in our country. The Hep-BD and Hep-B3 coverage was even lower in the state of Uttar Pradesh and stood at 50% and 78% respectively[8]. The national and state coverage of Hep-BD and Hep-B3 are way below the target of > 90%, which is to be achieved in a short period of next seven years, i.e, 2030.
Efforts are being made at national and international levels to identify the risk factors for incomplete vaccination so that appropriate corrective measures can be taken to improve the vaccination coverage. Poor knowledge and attitude of the parents towards childhood vaccination had been identified as a global issue, particularly in resource constraint developing countries. A recent systematic review identified that 22% of 838 reasons for under-vaccination was linked to parents’ knowledge and attitude towards the vaccination; similarly, 42% of 19 reasons for non-vaccination were liked to parents’ knowledge about vaccination[9]. Other factors were related to immunization systems, family characteristics, and communication and inadequate information. The authors further concluded from the data that under-vaccination and non-vaccination due to parental attitudes and knowledge are more difficult to address.
The risk factors for incomplete childhood vaccination in Indian community, are non-institutional delivery[10], female gender, muslim religion, lower caste, fewer antenatal care visits, non-receipt of maternal tetanus vaccination, education status of the mother[11], and poor financial status of the family. None of the studies from India had exclusively focused on parents’ knowledge about hepatitis B vaccine. Though, another study from Pakistan has also revealed that parents’ knowledge and unawareness is a risk factor for the poor coverage of hepatitis B vaccine[12].
A large proportion of parents had lack of knowledge and awareness about hepatitis. Multiple studies have reported the low knowledge score about hepatitis B among parents[13], pregnant women[14], general population[15], as well as medical students[16]. We found that the parents of the children who were given Hep-B3, had significantly more knowledge and awareness about hepatitis B than their counterparts of children without Hep-B3. Another study from India has concluded that interventions to improve the knowledge of parents about vaccination have potential to improve the vaccination overage in India[17]. We understand that this association of parents’ knowledge with hepatitis B vaccination may be an effect instead of the cause for the same. We need to explore this association in future studies.
Our study is the first study from the country which exclusively focused on hepatitis B vaccine and evaluated the knowledge and awareness of the parents about hepatitis B. Our study had a reasonable sample size and included children of different age groups. On the other hand, our study lacked a control arm to compare our results. We need to validate our results in multicentric studies before intervention can be implemented.
Coverage of Hep-BD and Hep-B3 vaccine is inadequate in the country. The parents have inadequate knowledge and awareness about hepatitis-B which may be partially responsible for poor vaccination coverage in their children. Measures shall be taken to raise the level of knowledge and awareness of the parents which could results in improved hepatitis B vaccination coverage in the country and may reduce HBV related morbidity and mortality in long term.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Virology
Country of origin: India
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade C
Creativity or Innovation: Grade C
Scientific Significance: Grade C
P-Reviewer: Ahboucha S, Morocco S-Editor: Lin C L-Editor: A P-Editor: Wang WB
| 1. | World Health Organization. Global Hepatitis Report 2017. [cited 4 April 2024]. Available from: https://iris.who.int/bitstream/handle/10665/255016/9789241565455-eng.pdf?sequence=1. |
| 2. | GBD 2019 Hepatitis B Collaborators. Global, regional, and national burden of hepatitis B, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol Hepatol. 2022;7:796-829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 416] [Cited by in RCA: 412] [Article Influence: 137.3] [Reference Citation Analysis (0)] |
| 3. | Swaroop S, Vaishnav M, Arora U, Biswas S, Aggarwal A, Sarkar S, Khanna P, Elhence A, Kumar R, Goel A, Shalimar. Etiological Spectrum of Cirrhosis in India: A Systematic Review and Meta-analysis. J Clin Exp Hepatol. 2024;14:101291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 2] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | McMahon BJ, Alward WL, Hall DB, Heyward WL, Bender TR, Francis DP, Maynard JE. Acute hepatitis B virus infection: relation of age to the clinical expression of disease and subsequent development of the carrier state. J Infect Dis. 1985;151:599-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 541] [Cited by in RCA: 502] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 5. | World Health Organization. Global health sector strategy on viral hepatitis 2016-2021. Towards ending viral hepatitis. [cited 4 April 4 2024]. Available from: https://iris.who.int/handle/10665/246177. |
| 6. | Francis MR, Nohynek H, Larson H, Balraj V, Mohan VR, Kang G, Nuorti JP. Factors associated with routine childhood vaccine uptake and reasons for non-vaccination in India: 1998-2008. Vaccine. 2018;36:6559-6566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 7. | National Health Mission. Immunization. [cited 4 April 4 2024]. Available from: https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=824&lid=220. |
| 8. | National Family Health Survey, India. National Family Health Survey (NFHS-5), 2019-21. [cited 4 April 4 2024]. Available from: https://rchiips.org/nfhs/factsheet_NFHS-5.shtml. |
| 9. | Rainey JJ, Watkins M, Ryman TK, Sandhu P, Bo A, Banerjee K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: findings from a systematic review of the published literature, 1999-2009. Vaccine. 2011;29:8215-8221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 268] [Article Influence: 19.1] [Reference Citation Analysis (1)] |
| 10. | Shenton LM, Wagner AL, Bettampadi D, Masters NB, Carlson BF, Boulton ML. Factors Associated with Vaccination Status of Children Aged 12-48 Months in India, 2012-2013. Matern Child Health J. 2018;22:419-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Devasenapathy N, Ghosh Jerath S, Sharma S, Allen E, Shankar AH, Zodpey S. Determinants of childhood immunisation coverage in urban poor settlements of Delhi, India: a cross-sectional study. BMJ Open. 2016;6:e013015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 12. | Naeem M, Khan MZ, Abbas SH, Adil M, Khan MU, Naz SM. Factors associated with low hepatitis B vaccination; a user and provider perspective study in Peshawar. J Pak Med Assoc. 2011;61:1125-1127. [PubMed] |
| 13. | Hyun S, Lee S, Ventura WR, McMenamin J. Knowledge, Awareness, and Prevention of Hepatitis B Virus Infection Among Korean American Parents. J Immigr Minor Health. 2018;20:943-950. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Okenwa UJ, Dairo MD, Bamgboye E, Ajumobi O. Maternal knowledge and infant uptake of valid hepatitis B vaccine birth dose at routine immunization clinics in Enugu State - Nigeria. Vaccine. 2020;38:2734-2740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Zhou Y, Su Y, Yan R, Tang X, Deng X, Zhu Y, Xu X, He H. Knowledge and awareness of viral hepatitis and influencing factors among the general population aged 15-69 years in Zhejiang Province, China. Hum Vaccin Immunother. 2023;19:2252241. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Naqid IA, Mosa AA, Ibrahim SV, Ibrahim NH, Hussein NR. Hepatitis B vaccination status and knowledge, attitude, and practice towards Hepatitis B virus among medical sciences students: A cross-sectional study. PLoS One. 2023;18:e0293822. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 17. | Francis MR, Nuorti JP, Kompithra RZ, Larson H, Balraj V, Kang G, Mohan VR. Vaccination coverage and factors associated with routine childhood vaccination uptake in rural Vellore, southern India, 2017. Vaccine. 2019;37:3078-3087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |