Published online Sep 25, 2022. doi: 10.5501/wjv.v11.i5.331
Peer-review started: April 24, 2022
First decision: May 12, 2022
Revised: June 1, 2022
Accepted: August 25, 2022
Article in press: August 25, 2022
Published online: September 25, 2022
Processing time: 152 Days and 18.4 Hours
Coronavirus disease 2019 (COVID-19) is a pandemic caused by the severe acute respiratory syndrome coronavirus in 2019. Although the real-time reverse tr-anscription PCR test for viral nucleic acids is the gold standard for COVID-19 diagnosis, computed tomography (CT) has grown in importance.
To evaluate the sensitivity and specificity of thoracic CT findings of COVID-19 pneumonia according to age groups.
PCR and CT results from 411 patients were reviewed. The diagnosis of COVID-19 pneumonia was made by three radiologists. Lymphadenopathy, pericardial effusion, pleurisy, pleural thickening, pleural effusion, location features of the lesions, ground glass, consolidation, air bronchogram, vascular enlargement, bronchial dilatation, halo finding, inverted halo sign, nodularity, air bubble, subpleural band (curvilinear density), reticular density, crazy paving pattern, and fibrosis findings were recorded. The patients were divided into nine groups by decades while calculating the sensitivity, specificity, and diagnostic efficacy for CT positivity.
The mean age of the cases was 48.1 ± 22.7 years. The CT finding with the highest diagnostic power was ground glass. Vascular enlargement and bronchial dilatation followed ground glass. Peri-cardial effusion was the finding with the lowest diagnostic accuracy. The incidence of lymphadenopathy, pleurisy, pleural thickening, peripheral localization, bilateral, ground glass, vascular enlargement, bronchial dilatation, subpleural band, reticular density, crazy paving appearance, and fibrosis all increased increase significantly with age in patients with positive real-time reverse transcription PCR test.
There are few publications comparing sensitivity and specificity of thoracic CT findings according to age. In cases of COVID-19 pneumonia, there is an increase in the variety and frequency of CT findings with age, and parallel to this the sensitivity and specificity of the findings increase. COVID-19 cases in the pediatric age group have fewer lung findings than adults, and this situation decreases the diagnostic value of CT in pediatric patients.
Core Tip: Despite its high sensitivity for identifying coronavirus disease 2019 (COVID-19) pneumonia, the diagnostic potential of computed tomography findings has not been thoroughly investigated, particularly in relation to age subgroups. It is worth noting that the prevalence of COVID-19 pneumonia can vary by age. Even common results, such as ground glass opacities, can be reduced in younger individuals, particularly in the pediatric population. Additionally, the findings of this study may raise awareness about the proper use of computed tomography scans in children and contribute to radiation protection by limiting computed tomography scans in age groups with low sensitivity.
- Citation: Karavas E, Unver E, Aydın S, Yalcin GS, Fatihoglu E, Kuyrukluyildiz U, Arslan YK, Yazici M. Effect of age on computed tomography findings: Specificity and sensitivity in coronavirus disease 2019 infection. World J Virol 2022; 11(5): 331-340
- URL: https://www.wjgnet.com/2220-3249/full/v11/i5/331.htm
- DOI: https://dx.doi.org/10.5501/wjv.v11.i5.331
The World Health Organization has declared coronavirus disease 2019 (COVID-19) a pandemic caused by severe acute respiratory syndrome coronavirus 2[1,2]. Although fever and cough are the most common clinical symptoms, other symptoms such as fatigue, shortness of breath, and headache may also be present[3]. However, because all of these symptoms are not unique to the disease and because the disease can progress quickly to severe pneumonia, diagnostic tests are required.
Although the real-time reverse transcription (RT)-PCR test for viral nucleic acids is the gold standard in the diagnosis of COVID-19, computed tomography (CT) has become increasingly important in the diagnosis due to false negative results and the inability to obtain results quickly[4]. Because CT has a sensitivity of 97 %, it is frequently used, and algorithms are developed accordingly[5]. Even if the RT-PCR is negative, treatment and filiation are initiated in close contacts[6]. However, because CT contains ionizing radiation, there is a risk of unintentional use. The expected harms of ionizing radiation are greater in children than in adults. Seeing that, we aim to define the change of the CT findings as well as the sensitivity and the specificity of these findings according to age.
The local (33216249-50.01.02-E.25467) medical ethics committee approved this study. The ethics committee waived informed consent as a result of the retrospective nature.
The study included 411 patients with suspected COVID-19 who applied to a tertiary healthcare center. The registration period began on March 15, 2020 and ended on May 15, 2020. All patients had laboratory RT-PCR testing of respiratory secretions obtained via nasopharyngeal or oropharyngeal swab. Clinical data from electronic medical records were reviewed.
All patients had a CT scan without intravenous contrast material on the day they were admitted to the hospital (Siemens SOMATOM Sensation 16, Forchheim, Germany). All patients were scanned in the supine position using an adult CT protocol; reconstruction images of the 1.5 mm lung window were obtained using tube voltage = 130kV, effective mAs = 70, slice thickness = 5 mm, collimation = 16 × 1.2, pitch = 0.8. In children, reconstruction images of the lung window of 1.5 mm were obtained with protocol tube voltage = 110kV, effective mAs = 60, slice thickness = 8 mm, collimation = 16 × 1.2, pitch = 0.8 (14 years and younger).
All CT images were reviewed by three thorax imaging experts who were not aware of the RT-PCR test results, and the final decision was reached by consensus. The North American Society of Radiology Expert Consensus Statement on Reporting of Lung CT Findings Related to COVID-19[7] (Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19) was followed in the evaluation for pneumonia caused by COVID-19. Typical and indeterminate appearance were considered positive for COVID-19 infection, whereas atypical appearance and negative for pneumonia were considered negative for infection. Lymphadenopathy, pericardial effusion, pleurisy, pleural thickening, pleural effusion, lesion location features (peripheral-central-diffuse, posterior, bilateral-unilateral, etc), ground glass, consolidation, air bronchogram, vascular enlargement, bronchial dilatation, halo sign, reverse halo sign, nodularity, air bubble, subpleural band (curvilinear density), reticular density, crazy paving pattern, and fibrosis findings were recorded.
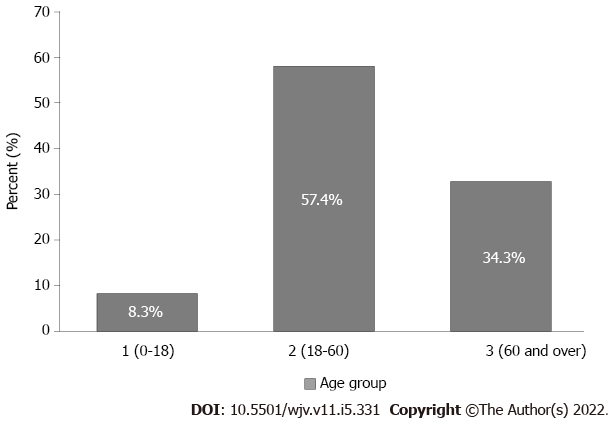
The patients were divided into nine groups by decades when calculating the sensitivity, specificity, and significance for CT positivity. The ninth group was defined as people aged 80 and up. To avoid decreasing statistical power, the sensitivity, specificity, and significance of the CT findings were divided into three groups determined by the World Health Organization (age group 1: 0-18, age group 2: 18-60, age group 3: 60 and above).
IBM SPSS 22 was used for statistical analyses (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY, United States: IBM Corp.). The Kolmogorov-Smirnov test was used to determine whether the data conformed to a normal distribution. Numerical variables with a normal distribution were represented as mean and standard deviation values, variables without a normal distribution as median (minimum-maximum) values, and categorical variables as number (n) and percentage values (percent) When calculating CT diagnostic accuracy measures, RT-PCR was used as the gold standard. CT sensitivity and specificity were reported along with their 95% confidence intervals. Exact Clopper-Pearson confidence intervals for sensitivity and specificity were calculated. A P value of less than 0.05 was considered as statistically significant.
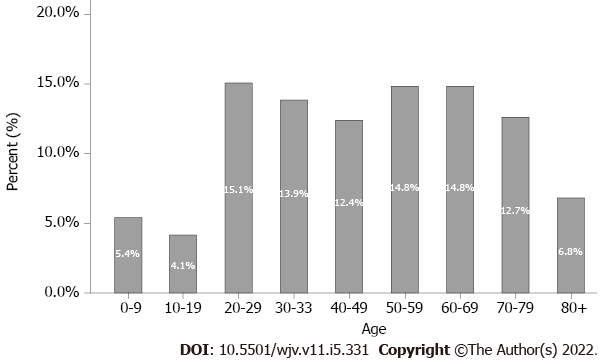
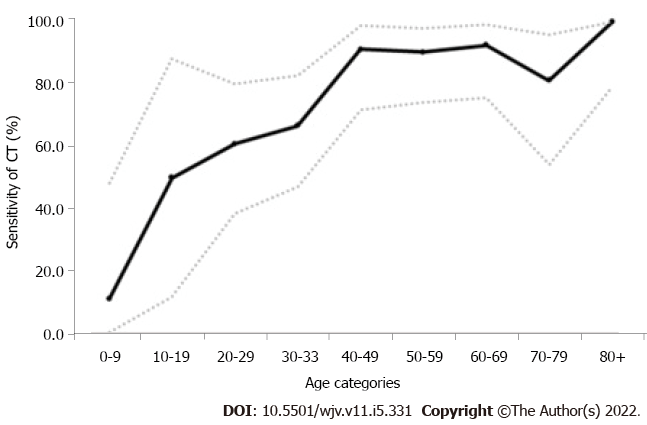
The average age of the 411 cases was 48.1 ± 22.7 years (median: 49, range: 0-99), with 241 (58.8%) males and 170 (41.4%) females. Figure 1 depicts the distribution of the number of patients by decade, while Figure 2 depicts the distribution by group. There were 181 positive RT-PCR results and 230 negative RT-PCR results out of 411 patients, for a positive rate of 41% (181/411). There was no statistically significant difference in age or gender between patients with positive and negative RT-PCR results (P > 0.05). There were 141 positive and 40 negative CT findings in 181 cases, for a positive rate of 77.9% (141/181). The overall and age-segregated sensitivity and specificity of CT were calculated and reported based on RT-PCR results. CT sensitivity was found to be 77.9% (95% confidence interval: 71.15 to 83.72) for all patients. However, when the sensitivity value was stratified based on age, it was discovered that it had changed. The findings revealed that the sensitivity of CT increased with age (Table 1, Figures 3 and 4).
| Age | CT | RT-PCR | Sensitivity, % (95%CI) | Specificity, % (95%CI) | ||
| COVID-19 negative | COVID-19 positive | |||||
| Age categories | 0-9 | Negative | 3 | 8 | 11.11 (0.28-48.25) | 23.08 (5.04-53.81) |
| Positive | 10 | 1 | ||||
| 10-19 | Negative | 0 | 3 | 50.00 (11.81-88.19) | 0.00 (0.00-28.49) | |
| Positive | 11 | 3 | ||||
| 20-29 | Negative | 10 | 9 | 60.87 (38.54-80.29) | 25.64 (13.04-42.13) | |
| Positive | 29 | 14 | ||||
| 30-39 | Negative | 5 | 10 | 66.67 (47.19-82.71) | 18.52 (6.30-38.08) | |
| Positive | 22 | 20 | ||||
| 40-49 | Negative | 9 | 2 | 91.30 (71.96-98.93) | 32.14 (15.88-52.35) | |
| Positive | 19 | 21 | ||||
| 50-59 | Negative | 4 | 3 | 90.32 (74.25-97.96) | 13.33 (3.76-30.72) | |
| Positive | 26 | 28 | ||||
| 60-69 | Negative | 3 | 2 | 92.59 (75.71-99.09) | 8.82 (1.86-23.68) | |
| Positive | 31 | 25 | ||||
| 70-79 | Negative | 4 | 3 | 81.25 (54.35-95.95) | 11.11 (3.11-26.06) | |
| Positive | 32 | 13 | ||||
| 80+ | Negative | 4 | 0 | 100.00 (79.41-100.0) | 33.33 (9.92-65.11) | |
| Positive | 8 | 16 | ||||
| Overall | Negative | 42 | 40 | 77.90 (71.15-83.72) | 18.26 (13.49-23.87) | |
| Positive | 188 | 141 | ||||
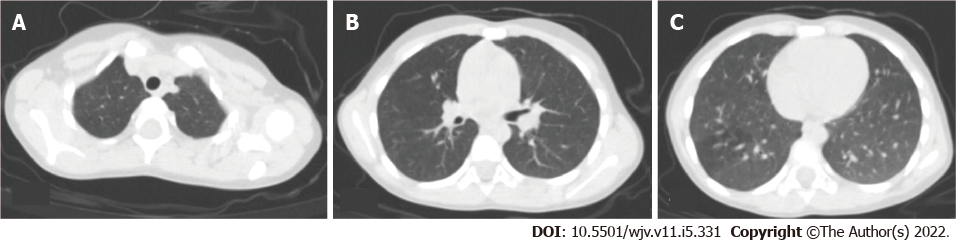
Table 2 showed the diagnostic accuracy of the findings recorded in RT-PCR test negative and positive cases across the entire population. According to these findings, ground glass opacity had the highest diagnostic accuracy of 62.5 % (sensitivity 84.4%, specificity 33.7%), followed by vascular enlargement at 58.5% and bronchial dilatation at 58.3% (Figure 5A). With a diagnostic accuracy of 40.0%, pericardial effusion is the finding with the lowest diagnostic accuracy.
| Findings | Sensitivity, % | Specificity, % | Diagnostic accuracy, % |
| Lymphadenopathy | 60.3 | 44.7 | 46.9 |
| Pleurisy | 78.3 | 45.6 | 48.0 |
| Pericardial effusion | 80.0 | 40.0 | 40.0 |
| Pleural thickening | 19.3 | 86.1 | 48.0 |
| Peripheral location | 46.5 | 53.6 | 49.6 |
| Posterior location | 65.1 | 22.0 | 48.5 |
| Bilateral location | 69.3 | 22.0 | 51.4 |
| Ground glass | 84.4 | 33.7 | 62.5 |
| Consolidation | 45.9 | 71.1 | 56.7 |
| Air bronchogram | 31.2 | 81.3 | 52.8 |
| Vascular enlargement | 53.2 | 65.7 | 58.5 |
| Bronchial dilatation | 50.5 | 68.7 | 58.3 |
| Halo sign | 28.9 | 75.3 | 48.9 |
| Reverse halo sign | 1.4 | 95.8 | 42.1 |
| Nodularity | 37.2 | 68.1 | 50.5 |
| Air bubble | 16.1 | 87.3 | 46.8 |
| Subpleural band | 27.1 | 70.5 | 45.8 |
| Reticular density | 11.9 | 88.6 | 45.0 |
| Crazy paving appearance | 11.0 | 97.6 | 48.4 |
| Fibrosis | 15.6 | 90.3 | 47.7 |
Table 3 showed the frequency of findings in cases with positive RT-PCR tests based on age groups. Lymphadenopathy, pleurisy, pleural thickening, peripheral localization, bilateral, ground glass, vascular enlargement, bronchial dilatation, subpleural band, reticular density, crazy paving appearance, and fibrosis all increased with age (P < 0.05) (Figure 5B). Although there was a significant difference in consolidation, air bronchogram, and air bubble findings between age groups, it was not related to patient age (Figure 5C). There was no significant difference in the rates of bilateral involvement, posterior location, pericardial effusion, halo, reverse halo, and nodularity between the three groups (P > 0.05) (Figure 5D).
| Findings | Age group 1, % | Age group 2, % | Age group 3, % | P value |
| Lymphadenopathy | 0 | 8.1 | 29.8 | 0.001 |
| Pleurisy | 0 | 2.2 | 20.8 | 0.002 |
| Pericardial effusion | 0 | 0.5 | 3.1 | 0.092 |
| Pleural thickening | 3.0 | 12.7 | 27.5 | 0.005 |
| Peripheral location | 36.4 | 61.5 | 65.1 | 0.04 |
| Posterior location | 59.1 | 67.1 | 74.6 | 0.09 |
| Bilateral location | 50.0 | 62.1 | 88.5 | 0.07 |
| Ground glass | 51.5 | 69.1 | 94.7 | 0.007 |
| Consolidation | 39.4 | 29.5 | 52.7 | 0.02 |
| Air bronchogram | 36.4 | 18.2 | 35.1 | 0.001 |
| Vascular enlargement | 30.3 | 38.2 | 59.5 | 0.03 |
| Bronchial dilatation | 30.3 | 36.7 | 53.4 | 0.005 |
| Halo sign | 24.2 | 26.8 | 24.2 | 0.055 |
| Reverse halo sign | 0 | 2.3 | 3.8 | 0.06 |
| Nodularity | 36.4 | 34.1 | 35.9 | 0.067 |
| Air bubble | 0 | 0 | 0.8 | 0.04 |
| Subpleural band | 12.1 | 21.8 | 42.8 | 0.002 |
| Reticular density | 0 | 9.1 | 18.3 | 0.001 |
| Crazy paving appearance | 3.0 | 4.1 | 13.0 | 0.02 |
| Fibrosis | 0 | 2.7 | 33.8 | 0.001 |
On March 11, 2020, the World Health Organization declared COVID-19 a global epidemic. The disease’s high contagiousness necessitated the development of a rapid and highly sensitive test. In addition to the low sensitivity of the gold standard RT-PCR test, test results were provided within days or weeks due to a lack of testing centers, particularly in the 1st months of the pandemic. This circumstance has resulted in a more rapid and accessible test requirement. The impact of COVID-19 infection on the lower respiratory tract has brought thoracic CT examination to the forefront. Thoracic CT is useful for detecting viral lung infection, determining the nature and extent of pulmonary lesions, and monitoring disease activity[8-11]. In addition, the latest studies revealed that CT perfusion examinations can reveal perfusion deficits in COVID-19 pneumonia[12]. In these circumstances, in addition to the potential for rapid diagnosis of COVID-19 by thoracic CT, identification of pulmonary changes and base images of the cases to be followed may be an added benefit.
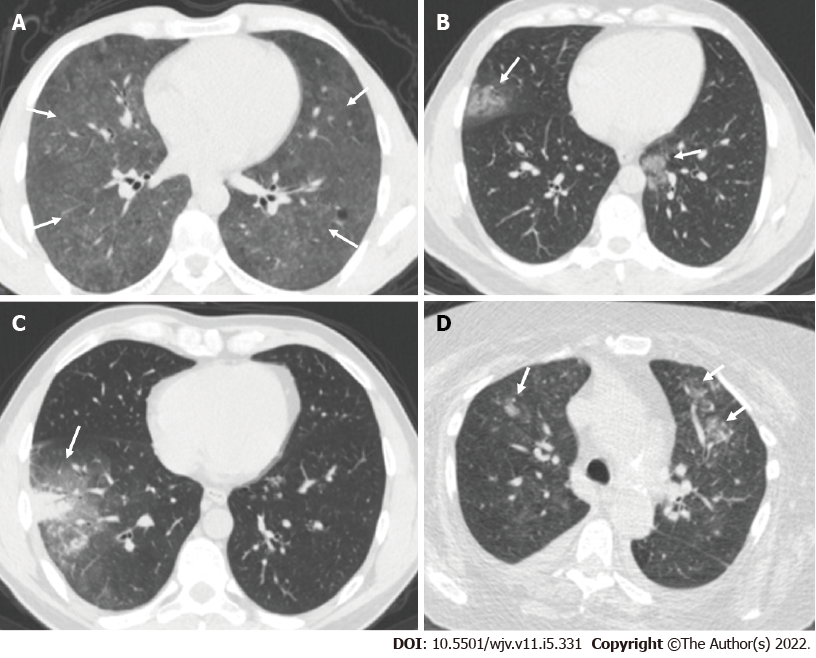
Multiple, peripheral, bilateral, irregular, subsegmental or segmental ground glass opacities, mostly bronchovascular bundles, and areas of consolidation scattered throughout the subpleural space are typical COVID-19 chest CT imaging features. The presence of associated intralobular septal thickening in areas of ground glass opacity, crazy paving appearance, consolidation, and air bronchograms with areas of bronchial wall thickening and less frequently thickening of the adjacent or interlobar pleura as well as a small amount of pleural effusion are also COVID-19 chest CT imaging features[7,13,14]. When all cases were considered in our study, the findings of ground glass density, vascular enlargement, bronchial dilatation, consolidation, and bilaterality stood out for diagnostic accuracy.
In limited studies, pediatric patients with COVID-19 have relatively mild clinical symptoms, a higher prevalence of negative CT scans, and atypical, peribronchial distribution of lung opacities and bronchial wall thickening are more common[15,16]. The incidence of any finding other than an air bronchogram and nodular appearance is not higher in this age group than in other age groups. Posterior location, bilaterality, and ground glass density are the most common findings. Among these findings is that the prevalence of ground glass density is significantly lower in this age group than in other age groups. The sensitivity of CT diagnosis in the 0-9 age group was found to be quite low in our study.
For the diagnosis of COVID-19, various algorithms have been developed. Due to the large number of cases, doctors from fields other than chest diseases or infectious diseases had to play an active role in disease diagnosis in many hospitals. Due to a lack of experience in physical examination, doctors from various fields frequently rely on thoracic CT exam-ination, with the tendency to deviate from algorithms and make an easy and quick diagnosis. RT-PCR may be negative in the early stages of the disease and due to other variants as well as the inadequacy of the RT-PCR test contributes to the overuse of thoracic CT[17,18]. Routine thoracic CT screening for COVID-19 is not recommended, and confirmatory diagnosis is based on RT-PCR. When a low-dose CT scan is required, it is preferable for the pediatric population. Follow-up imaging is only necessary in cases of clinical deterioration and should be kept to a minimum.
The study’s most significant limitation is the small number of cases in the 0-18 age range. The main reason for this is that clinical symptoms in this age group are unclear, and pediatricians in our hospital are actively treating patients with suspected COVID-19.
Despite its high sensitivity for identifying COVID-19 pneumonia, the diagnostic potential of CT findings has not been thoroughly investigated, particularly in relation to age subgroups. It is worth noting that the prevalence of COVID-19 pneumonia can vary by age. Even common results, such as ground glass opacities, can be reduced in younger individuals, particularly in the pediatric population. Additionally, the findings of this study may raise awareness about the proper use of CT scans in children and contribute to radiation protection by limiting CT scans in age groups with low sensitivity.
Coronavirus disease 2019 (COVID-19) is a pandemic caused by the severe acute respiratory syndrome coronavirus in 2019. Although the real-time reverse transcription (RT)-PCR test for viral nucleic acids is the gold standard for COVID-19 diagnosis, computed tomography (CT) has grown in importance.
There is a risk of unintentional use because CT contains ionizing radiation. Ionizing radiation is expected to cause more harm to children than to adults.
We aim to define the change of the CT findings as well as the sensitivity and the specificity of these findings according to age.
The study included 411 patients with suspected COVID-19 who sought treatment at a tertiary healthcare facility. RT-PCR testing of respiratory secretions obtained via nasopharyngeal or oropharyngeal swab was performed on all patients. Clinical information from electronic medical records was examined. On the day they were admitted to the hospital, all patients had a CT scan without intravenous contrast material. Three thorax imaging experts who were not aware of the RT-PCR test results reviewed all CT images, and the final decision was reached by consensus. When calculating the sensitivity, specificity, and significance for CT positivity, the patients were divided into nine groups based on decades. The group was defined as people aged 80 and up for the ninth group. The sensitivity, specificity, and significance of CT findings into three groups (age group 1: 0-18, age group 2: 18-60, age group 3: 60 and above) was determined.
There were 181 positive RT-PCR results and 230 negative RT-PCR results out of 411 patients, for a positive rate of 41% (181/411). There were 141 positive and 40 negative CT findings in 181 cases, for a positive rate of 77.9 % (141/181). CT sensitivity was found to be 77.9 % (95% confidence interval: 71.15 to 83.72) for all patients. The findings revealed that the sensitivity of CT increased with age. Ground glass opacity had the highest diagnostic accuracy of 62.5 %, followed by vascular enlargement at 58.5% and bronchial dilatation at 58.3%. Lymphadenopathy, pleurisy, pleural thickening, peripheral localization, bilateral, ground glass, vascular enlargement, bronchial dilatation, subpleural band, reticular density, crazy paving appearance, and fibrosis all increased with age (P < 0.05).
Due to the large number of cases, doctors from various fields frequently rely on thoracic CT examination, with the tendency to deviate from algorithms and make an easy and quick diagnosis. The inadequacy of the RT-PCR test contributes to the overuse of thoracic CT. The sensitivity of CT diagnosis in the 0-9 age group was found to be quite low in our study. When a low-dose CT scan is required, it is preferable for the pediatric population. Follow-up imaging is only necessary in cases of clinical deterioration and should be kept to a minimum.
Further research should be conducted to determine the diagnostic potential of COVID-19 CT findings in relation to age subgroups. Additionally, the findings of this study may raise awareness about the proper use of CT scans in children and contribute to radiation protection by limiting CT scans in age groups with low sensitivity.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bellini MI, Italy; Wang MK, China S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ
| 1. | Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R, Niu P, Zhan F, Ma X, Wang D, Xu W, Wu G, Gao GF, Tan W; China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18987] [Cited by in RCA: 17646] [Article Influence: 3529.2] [Reference Citation Analysis (0)] |
| 2. | WHO. Coronavirus disease (COVID-19) pandemic. 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. |
| 3. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30120] [Article Influence: 6024.0] [Reference Citation Analysis (3)] |
| 4. | Majidi H, Niksolat F. Chest CT in patients suspected of COVID-19 infection: A reliable alternative for RT-PCR. Am J Emerg Med. 2020;38:2730-2732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Ai T, Yang Z, Hou H, Zhan C, Chen C, Lv W, Tao Q, Sun Z, Xia L. Correlation of Chest CT and RT-PCR Testing for Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. Radiology. 2020;296:E32-E40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3614] [Cited by in RCA: 3285] [Article Influence: 657.0] [Reference Citation Analysis (0)] |
| 6. | Sağlık Bakanlığı TC. Covid-19 Genel bi̇lgi̇ler, epi̇demi̇yoloji̇ ve tanı. Halk Sağlığı Genel Müdürlüğü. 2020;19:1-32 Available from https://covid19.saglik.gov.tr/. |
| 7. | Simpson S, Kay FU, Abbara S, Bhalla S, Chung JH, Chung M, Henry TS, Kanne JP, Kligerman S, Ko JP, Litt H. Radiological Society of North America Expert Consensus Statement on Reporting Chest CT Findings Related to COVID-19. Endorsed by the Society of Thoracic Radiology, the American College of Radiology, and RSNA - Secondary Publication. J Thorac Imaging. 2020;35:219-227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 400] [Cited by in RCA: 564] [Article Influence: 112.8] [Reference Citation Analysis (0)] |
| 8. | Zhao W, Zhong Z, Xie X, Yu Q, Liu J. Relation Between Chest CT Findings and Clinical Conditions of Coronavirus Disease (COVID-19) Pneumonia: A Multicenter Study. AJR Am J Roentgenol. 2020;214:1072-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 665] [Cited by in RCA: 696] [Article Influence: 139.2] [Reference Citation Analysis (0)] |
| 9. | Liu J, Chen T, Yang H, Cai Y, Yu Q, Chen J, Chen Z, Shang QL, Ma C, Chen X, Xiao E. Clinical and radiological changes of hospitalised patients with COVID-19 pneumonia from disease onset to acute exacerbation: a multicentre paired cohort study. Eur Radiol. 2020;30:5702-5708. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 10. | Aydin S, Kantarci M, Fatihoglu E, Yesilyurt H, Karavas E. COVID-19 CT Severity and Handedness: Is There a Relation? Imaging Interv. 2021;28:1-5. [DOI] [Full Text] |
| 11. | Aydin S, Unver E, Karavas E, Yalcin S, Kantarci M. Computed tomography at every step: Long coronavirus disease. Respir Investig. 2021;59:622-627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Aydin S, Kantarci M, Karavas E, Unver E, Yalcin S, Aydin F. Lung perfusion changes in COVID-19 pneumonia: a dual energy computerized tomography study. Br J Radiol. 2021;94:20201380. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Hani C, Trieu NH, Saab I, Dangeard S, Bennani S, Chassagnon G, Revel MP. COVID-19 pneumonia: A review of typical CT findings and differential diagnosis. Diagn Interv Imaging. 2020;101:263-268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 231] [Cited by in RCA: 263] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 14. | Dennie C, Hague C, Lim RS, Manos D, Memauri BF, Nguyen ET, Taylor J. Canadian Society of Thoracic Radiology/Canadian Association of Radiologists Consensus Statement Regarding Chest Imaging in Suspected and Confirmed COVID-19. Can Assoc Radiol J. 2020;71:470-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 15. | Chen A, Huang JX, Liao Y, Liu Z, Chen D, Yang C, Yang RM, Wei X. Differences in Clinical and Imaging Presentation of Pediatric Patients with COVID-19 in Comparison with Adults. Radiol Cardiothorac Imaging. 2020;2:e200117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 16. | Duan YN, Zhu YQ, Tang LL, Qin J. CT features of novel coronavirus pneumonia (COVID-19) in children. Eur Radiol. 2020;30:4427-4433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 67] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 17. | Erturk SM. CT of Coronavirus Disease (COVID-19) Pneumonia: A Reference Standard Is Needed. AJR Am J Roentgenol. 2020;215:W20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Bellini MI, Fresilli D, Lauro A, Mennini G, Rossi M, Catalano C, D'Andrea V, Cantisani V. Liver Transplant Imaging prior to and during the COVID-19 Pandemic. Biomed Res Int. 2022;2022:7768383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |