DISCUSSION
Epidemiology
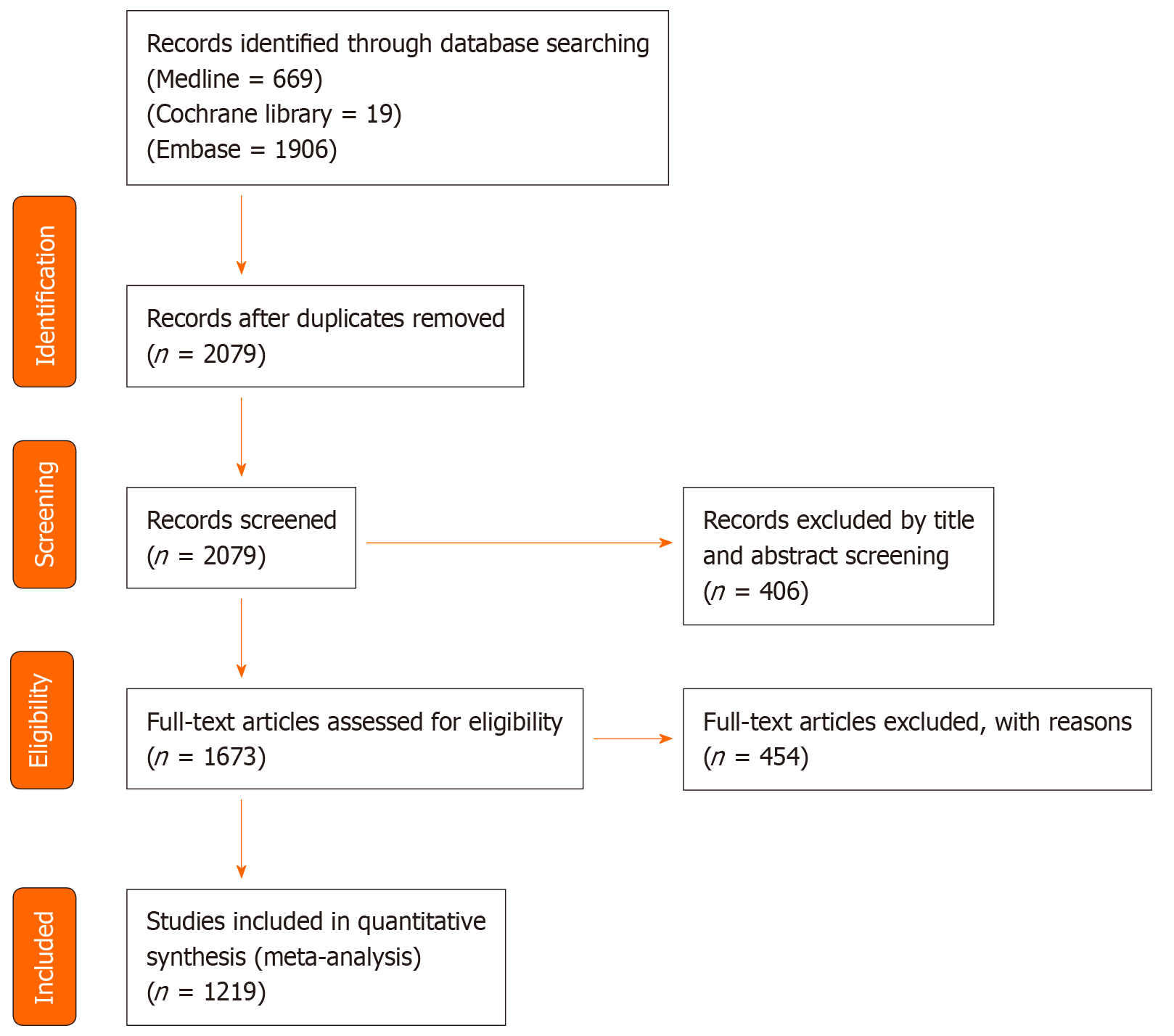
We have reviewed 171 systematic reviews regarding the epidemiology of COVID-19 infection. The incubation period of COVID-19 showed a median of 5.1 d with the 95th percentile of 11.7 d. The incubation period of COVID-19 that induced severe acute respiratory distress syndrome had an average of 6.0 d[3].
Several systematic reviews showed mortality with hospitalization was invasive mechanical ventilation was 13%[4]. Higher mortality was seen in patients with the following factors: Living in the European region, male sex, older age, active smoking, alcohol use, intensive care unit admission, comorbid conditions such as DM, obesity, hypertension, chronic lung disease, cerebrovascular disease, coronary heart disease, chronic renal disease, chronic liver disease and presence of malignancies[5,6]. The fatality rate was approximately 0.68%, with very high heterogeneity[5]. Some reviews described specific gene susceptibilities and recommended further genetic research[6]. O blood group is thought to be protective against COVID-19 with regard to mortality and susceptibility[7].
Several systematic reviews showed the most common laboratory or radiological finding of COVID-19 was lymphopenia, bilateral ground opacities in lungs, elevated C-reactive protein (CRP), lactate dehydrogenase (LDH), procalcitonin, D-dimer, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and/or creatinine. Fever, cough, and fatigue were the most common presenting clinical symptoms[8]. Dyspnea, anosmia, diarrhea, and myalgia were also frequently found in patients[9]. Healthcare workers (HCWs) who were positive with real-time reverse transcription polymerase chain reaction (RT-PCR) showed no symptoms in 40% of cases, 5% showed severe clinical complications, and 0.5% unfortunately died[9].
Regarding personal protective equipment (PPE), face mask users had decreased transmission, especially with N95 or similar equipment level[10]. Maintaining a physical distance of 1 meter or more and eye protection also revealed lower transmission rates[11]. Reusing masks did not yield a statistically significant result. Duration of PPE usage was recommended for no more than six hours of continuous use, with a break needed every two to three hours. PPE use is advised with appropriate hydration and skincare. The use of a powered air-purifying respirator (PAPR) is associated with greater heat tolerance but lower scores for mobility and communication ability. However, the reviews do not indicate a difference in HCW infection utilizing PAPR devices vs other compliant respiratory equipment. PPE can also be reused if they receive the appropriate dose of ultraviolet germicidal irradiation (UVGI) treatment[12].
Systematic reviews regarding disinfectants recommended using UVGI with vaporized hydrogen peroxide, non-thermal plasma, and air filters with photocatalytic disinfection[13]. Irritability of skin with propanol and isopropanol use was noticed but was less than frequent hand washing with detergent[14].
Systematic reviews regarding transmission showed inconclusive evidence about the viability and infectivity of SARS-CoV-2 in aerosol-generating procedures, but some studies showed an increased risk of infection with endotracheal intubation[15]. Clusters of infection played an important role. Frequently touching the T-zone (eyes, nose, mouth, chin) increases the chance of COVID-19 infection[16]. Transmission from an asymptomatic/pre-symptomatic patient is possible and more significant with pre-symptomatic patients. Quarantine is an essential factor in reducing the incidence of transmission[17]. No sexual or vertical transmission was observed and was not related to the route of delivery or breastfeeding[18]. A warm and humid climate reduced the spread of COVID-19. Viral carriage on the outer surface of surgical masks worn by HCW who treat patients with clinical respiratory illness is low[19].
Transmission
In a review of the 18 systematic reviews regarding the transmission of SARS-CoV-2, the consensus remains that respiratory infection via droplet and aerosolization in the human-to-human setting remains the most likely form of infection and that other forms such as contact with fomites and vertical transmission played a small role in contamination with the disease[20,21].
In one review article, the aerosolized transmission of SARS-CoV-2 showed that the virus was still viable. However, no correlation was shown regarding aerosolized transmission and disease[20]. If infection were to occur, contact would have to be in an enclosed environment. For aerosol transmission, the highest risk was related to health care workers involved in aerosol-generating procedures with the high-risk involving direct airway manipulation such as manual ventilation with intubation[15].
With the onset of the SARS-CoV-2 pandemic, data regarding all transmission forms has been researched, leading to one systematic review that found no direct virologic evidence of vertical transmission. Another review concluded that neonatal infection with SARS-CoV-2 was uncommon and that the rate of infection was no more significant than when the baby was born vaginally, via cesarean section, or if the baby breastfed and remained with the mother[22].
As human-to-human contact is responsible for SARS-CoV-2 infection, one systematic review analyzed 108 cluster infections from 13 countries[23]. This concludes that because the most common places associated with infection were family contact, community transmission, transportation, and healthcare-related facilities[23], minimizing unnecessary contact and social distancing should be strictly implemented to contain infection clusters.
Screening and diagnosis
One hundred seventy-seven articles were reviewed regarding the screening and diagnosis of COVID-19. The most common presenting symptoms to screen for were fever and cough. Studies also showed associated anosmia and loss of taste[24]. The most susceptible patients seem to be those with hypertension, diabetes, coronary artery disease, cerebrovascular disease, and chronic obstructive pulmonary disease. Males older than 50 with comorbidities were more likely than females to have severe pneumonia and dyspnea[25]. The pediatric population presented more commonly with diarrhea, and the infection was notably less severe. Innovations in technology such as contact tracing applications and telemedicine have been able to help promote surveillance of the disease and have been integrated into traditional medicine. Contact tracing tools have been shown to reduce transmission but can be challenging to implement in large populations[26]. There are privacy concerns, and further studies would be needed to show their effectiveness. Furthermore, infrared thermal screening was studied against the traditional thermometer, and it showed a low positive predictive value during the initial outbreak but continued to have a high negative predictive value throughout the pandemic's early and later stages[23].
Many labs were significantly appropriate for screening purposes. Elevated inflammatory markers, biochemical biomarkers, and hematological markers such as CRP, erythrocyte sedimentation rate (ESR), troponin, decreased lymphocyte count, fibrinogen, fibrinogen degradation products level, LDH, ferritin, and D-dimer on admission were associated with a poor outcome and were predictive of the severity and mortality of COVID-19 pneumonia[27]. An elevated D-dimer was linked to an overdiagnosis of disseminated intravascular coagulation (DIC) and led to inappropriate treatment with anticoagulation therapy[28]. Platelet count did not correlate with the severity of the disease. High levels of ferritin and interleukin-6 (IL-6) were elevated due to the cytokine storm from COVID-19, which correlated with increased intensive care unit (ICU) stays and mechanical ventilation requirements. The most common abnormality for the liver function test was hypoalbuminemia. However, some studies have shown elevated ALT, AST, and total bilirubin. An elevated Red Cell Distribution Width also correlated with the disease's severity[29].
There were numerous tools used for diagnosis. Stool studies exhibited more viral shedding than respiratory tract samples, which were easier to collect from the pediatric population. Studies showed that the RNA strains could be found in the saliva within seven to ten days of onset. Nasopharyngeal swabs showed more sensitivity than oropharyngeal swabs. Salivary samples are questionable, with inadequate sample power to comfortably substitute for the PCR based nasopharyngeal swab. The Reverse Transcriptase PCR has a sensitivity of 64% and specificity of nearly 100% but should not be used alone as the gold standard due to bias in measurements[30]. No evidence has shown a practical point of care serologic test at the time of this analysis. The virus uses Angiotensin-converting enzyme-2 (ACE2) receptors to enter the body. ACE2 receptors are found in the respiratory epithelium, gastrointestinal mucosa, and liver cholangiocytes. A portion of the adult patients presented with gastrointestinal symptoms, where computed tomography (CT) scans of the abdomen showed findings including small and large bowel wall thickening and pneumatosis intestinalis. The indications that the Infectious Disease Society of America recommends for serologic testing for antibodies are patients with clinical symptoms who have a negative diagnostic test and children with multisystem inflammatory syndrome to estimate antibody levels against the disease. The virus is positive in blood, urine, and stool, with higher viral shedding in blood and stool. Urine has been shown to have increased viral shedding in more severe patients with systemic disease and those requiring ICU admissions[31].
COVID-19 has predominantly been diagnosed using a real-time PCR test and/or chest CT with no consensus on which method is superior[32,33]. CT scans are sensitive but not specific, as imaging cannot differentiate coronavirus from other respiratory diseases. A chest CT with no pathologic findings cannot exclude COVID-19 alone, even if the patient has no symptoms. Also, positive CT findings with no symptoms may still warrant further testing because 90% of those patients later developed symptoms. The most common findings are ground-glass opacities with a distribution in the peripheral regions[34,35]. Other common findings are interlobular septal thickening and air bronchograms. COVID-19 lung pathology has consistently shown histology consistent with acute respiratory distress syndrome (ARDS) with frequent microthrombi[36]. Patients do not usually present with lymphadenopathy or pleural effusions. Lung ultrasounds of COVID-19 patients most commonly show the B-line interstitial pathology pattern[37]. CT scans of the chest still seem to be the most helpful imaging modality in pediatric patients and can detect pneumonia even before presenting symptoms.
Clinical presentation
We included 204 systematic review articles looking at clinical presentations of COVID-19. This disease can present in many ways. Nearly all organ systems can be affected, including the respiratory, cardiovascular, renal, gastrointestinal, endocrine, reproductive, central nervous system, bone marrow, and skin. Although most COVID-19 patients typically present with respiratory symptoms, ranging from upper airway disease to severe ARDS with multiorgan failure, many systematic reviews examined other organ systems implicated in the body. Several review studies concluded that cardiac and renal complications following respiratory complications are the most common clinical complications of COVID-19[38,39]. The most prevalent comorbid condition in patients with COVID-19 is diabetes, with it being both a significant risk factor and an indicator of poor prognosis[40]. Also, studies have shown that the elderly population has been affected by COVID-19 with high severity[41].
High rates of cardiovascular disease have been reported, and several studies showed a significant association with increased mortality and ICU admissions. Arrhythmias are prevalent and are reportedly the second most common cardiovascular complication[42,43].
Many reports are available that look at COVID-19 infection and the prothrombotic state, explained by coagulation activation, endothelial dysfunction, and formation of in situ thrombi rather than embolization of peripheral thrombi. This cascade of events causes deep venous thrombosis, pulmonary microthrombi, pulmonary embolism, cerebral venous thrombosis, and acute ischemic strokes that in some cases lead to a critical condition with poor long-term outcomes, residual disability, and prolonged rehabilitation[44]. Some studies showed ischemic strokes to be the most important prognostic marker and indicator of severity and poor clinical outcome. Prompt evaluation and early treatment with anticoagulation were associated with reduced mortality and better clinical outcome[45].
It has been found that many patients experience digestive symptoms as the primary complaint. Some studies have reported that patients with digestive symptoms had a trend to develop severe critical illnesses. Several available meta-analyses suggest that acute liver injury and elevated liver enzymes were significantly associated with COVID-19 severity and predicted worse outcomes.
Acute kidney injury (AKI) is a common complication of COVID-19. AKI's incidence is between 8%-20% depending on the study. In some studies, the presence of AKI is associated with a 13-fold increased risk of mortality[46]. Age, DM, hypertension, and baseline serum creatinine (SCr) levels are associated with increased AKI incidence. Concerns have emerged about the potential impact of COVID-19 on male reproductive organs and male fertility.
There is strong evidence of neurological involvement ranging from Guillain–Barré syndrome, delirium, and encephalitis, to cerebral venous thrombosis and ischemic strokes, with acute ischemic strokes being the most frequently reported complication with the highest mortality rate. Neurologic manifestations are shown to develop approximately one to two weeks following the onset of respiratory symptoms[47]. Olfactory and gustatory dysfunction have been described and used to aid in clinical diagnosis as they present reasonably early after the disease's contraction. Cutaneous involvement has been described in several review articles and was shown to manifest occasionally in asymptomatic carriers. Several ongoing studies investigate the role of early identification of cutaneous involvement, which may be vital to early diagnosis and lead to a possible better prognosis[39].
Finally, several systematic reviews have looked at the implication of COVID-19 on mental health and reported increased suicide risk, depression, and anxiety levels in the general population irrespective of COVID-19 status.
Gastrointestinal
We included 57 systematic review articles regarding the association of COVID-19 with the gastrointestinal system. These studies found that those with high rates of digestive symptoms, acute liver injury, and elevated liver enzymes are more likely to develop severe/critical illnesses. Common presenting gastrointestinal symptoms included abdominal pain, nausea, vomiting, and diarrhea. Frequent abnormalities in liver function tests included hypoalbuminemia, derangements in gamma-glutamyl-transferase, increased bilirubin values, prolonged prothrombin time, and deranged aminotransferases[48]. Patients with preexisting liver abnormalities such as hepatocellular carcinoma, metabolic associated fatty liver disease, and chronic liver disease had an increased risk of COVID-19 disease progression, more severe COVID-19 infection, and increased mortality rates[49]. Two systematic reviews found that in patients with inflammatory bowel disease and COVID-19, diarrhea occurred more frequently; however, these patients did not appear to be at a higher risk of developing COVID-19 than those in the general population[50,51]. One systematic review investigated the relationship between COVID-19 and fecal nucleic acid testing in the pediatric population and found that the positive rate for fecal nucleic acid testing in COVID-19 children was relatively high, suggesting that fecal nucleic acids can be used as a method of detecting COVID-19 in this population[52]. Additionally, several studies observed that the gastrointestinal manifestation of COVID-19 raises the question of possible transmission through the fecal-oral route in both the adult and pediatric populations, indicating that healthcare workers should exercise caution when collecting stool samples.
Cardiovascular
We included 39 systematic reviews about patients' cardiovascular manifestations with COVID-19 infection and the clinical significance of biomarkers, preexisting cardiovascular disease, and thromboembolic disease risk.
The most common comorbidities associated with increased mortality among patients with COVID-19 infection were hypertension, coronary artery disease, and heart failure. These factors were positively correlated with an augmented risk of hospitalization, poor outcomes, and death. Although preexisting conditions consistently demonstrated increased complications and mortality, COVID-19 also increased cardiovascular disease by inducing cytokine storms[53]. There was an association between COVID-19 infection and direct cardiovascular complications, including myocardial injury, heart failure, myocardial infarction, myocarditis, arrhythmias, and blood clots, leading to increased mortality and adverse outcomes. There was poor documentation about the incidence and nature of arrhythmias in the setting of COVID-19. A systematic review reported Takotsubo syndrome could be associated with COVID-19 infection and demonstrated a higher prevalence in older women with higher rates of complications[54].
The biomarkers associated with increased mortality were LDH, creatinine kinase, brain natriuretic peptide, and troponin I. Lastly, the coagulopathies observed in patients with COVID-19 infection ranged from mild laboratory alterations to DIC. It is proposed that the endotheliopathy could be from direct endothelial infection with SARS-CoV-2 and indirect damage caused by the inflammation.
Cardiovascular complications added to the elevated morbidity and mortality in patients with preexisting cardiovascular risk factors. Further studies could help better to identify the role of SARS-CoV-2 in this population.
Neurology
The most common neurological symptoms in our analyses of COVID-19 patients included chemosensory dysfunction, vascular events, neurologic syndromes, encephalopathies, and inflammation[55,56]. Strokes were associated with the highest mortality rate. Neurological manifestations developed one to two weeks after the onset of respiratory disease, but they were also seen in patients who did not have any respiratory disease. One systematic review article regarding the severity assessment of COVID-19 patients with neurological symptoms described that the predominant central nervous system symptoms were headaches and dizziness, while the most common peripheral nervous system symptoms were dysfunction in taste and smell.
Neurologic similarities were seen in the symptomatology of COVID-19, SARS, and Middle East respiratory syndrome[53,57]. All three viral syndromes were associated with similar neurologic complications, such as fatigue, headache, and smell and taste disorders. The myriad of neurological manifestations in COVID-19 syndrome should be further explored to elucidate the pathogenesis of COVID-19 related neurologic disease.
Stroke
According to 13 articles, including multiple meta-analyses and systematic reviews, COVID-19 infection has been associated with significant neurological manifestations within the central nervous system, including stroke, intracranial hemorrhage, encephalomyelitis, and acute myelitis. We included one systematic review and meta-analysis that suggests an increased risk of stroke in hospitalized patients with preexisting cerebral vascular disease. This increased risk of stroke was associated with an increase in adverse outcomes, most notably mortality. One multicenter study and meta-analysis suggest that more severe COVID-19 infections are associated with a higher risk of stroke, with an overall pooled risk estimated at 2.9%[58].
One systematic review and analysis showed COVID-19 patients who suffered from stroke symptoms developed neurologic symptoms after an average of nine days from the onset of their respiratory illness[59]. Multiple studies suggest that pro-inflammatory markers associated with COVID-19 infection, including D-dimer, IL-6, ferritin, and fibrinogen, may contribute to an inflammatory process mediating cerebrovascular accidents. One study found correlations with large vessel thrombosis and anterior circulation strokes[60], but more data and institutional collaboration of information are needed to understand the significance of the anatomic locality of strokes associated with COVID-19 infection. This multi-centered approach may elucidate future guidelines for certain patients, risk factors, or clinical findings unique to COVID-19 patients with neurologic symptoms.
Thrombosis
We included 16 systematic review articles regarding arterial and venous thromboembolism in patients with COVID-19 infection. Thromboembolic events in the deep veins of the lower extremities, pulmonary arteries, and cerebral veins suggested that the high rate of pulmonary artery occlusion was secondary to both embolic events from deep veins of legs and in situ thrombosis in pulmonary arteries. The proposed mechanism for these thrombotic events includes a combination of endothelial injury, platelet activation, hyperviscosity, blood flow abnormalities, and immune reactions. Segmental and subsegmental arteries were more commonly involved than the main pulmonary arteries[61]. The severity of COVID-19 infection correlates directly with thrombotic events, with a higher incidence of pulmonary embolism reported in ICU patients than general medical floor patients.
Additionally, it was discovered that ICU level patients also experienced a higher incidence of failed or inappropriate dosing of anticoagulation, whether preventive or therapeutic. Overall, higher mortality was seen in COVID-19 patients with thromboembolic events. However, data is limited in addressing whether or not there are mortality benefits seen with anticoagulation.
Anosmia and dysgeusia
There are 14 systematic review articles about chemosensory dysfunction. Ten articles discussed anosmia and dysgeusia, three articles for anosmia only, and one article for dysgeusia. Anosmia and dysgeusia are common early symptoms of COVID-19. There is a discrepancy in the prevalence of anosmia and dysgeusia according to sensitivity[62]. The prevalence of anosmia in an average individual was shown to vary according to age, sex, and testing technique[63]. The prevalence of anosmia, dysgeusia, or both as a symptom for COVID-19 was less often seen in male and geriatric patients. Anosmia was shown to be highly specific for COVID-19 and should be included in the evaluation process of suspected patients. As these dysfunctions were often seen early in the disease course, their presence may indicate early disease onset and indicate the clinician recommended isolation to prevent transmission. The mechanism of viral pathogenesis and causality remains a topic of study.
Ocular manifestations
The most common ocular presentations of COVID-19 are conjunctivitis, hyperemia, photophobia, dry eyes, chemosis, epiphora, blurry vision, foreign body sensation, ocular pain, floaters, and eyelid dermatitis. Patients may present with mild eyelid edema and/or tender, palpable preauricular and submaxillary lymph nodes. Rare presentations include herpes-like pseudo-dendritic infiltration of the cornea and bilateral pseudomembranous conjunctivitis.
COVID-19 virus entry is mediated by the binding of viral surface spike (S) glycoprotein to the ACE2 receptor[64]. Two primary mediators (the ACE-2 receptor and cell surface protease enzyme, TMPRSS2) are involved in this mechanism. Immunohistochemistry has shown the presence of ACE-2 receptors on the conjunctiva, limbus, and cornea. The ocular manifestations' treatment options include topical and systemic preparations, with antibiotic eye drops and artificial tears with or without corticosteroid eye drops.
COVID-19 patients treated with proning have had additional side effects, including exposure keratopathy, microbial keratitis, increased intraocular pressures, occlusion of the central retinal artery, and in some severe cases, orbital compartment syndrome. The prevention of acute orbital compartment syndrome was achieved with surgical interventions such as lateral canthotomy and cantholysis. Keratopathy can be prevented by lubricant ointments, moisture chambers, and polyethylene films. Topical viscous lubricants and mechanical closure of the eyes with hypoallergenic tapes or topical dressings may also be used.
This meta-analysis emphasizes the need for PPE for all healthcare workers involved in the care of COVID-19 patients to prevent exposure and infection. Along with a gown and gloves, wearing eye protection is also essential to prevent the spread of COVID-19 infection as eye mucous membranes can play a crucial part in transmitting COVID-19 viral particles.
Nephrology
A review of 10 literature publications showed that kidney injury incidence varies widely across studies, depending primarily on the severity of the disease. In one pooled analysis, AKI was detected in 8.3% of patients with COVID-19 vs 19.9% in critically ill patients[65]. Moreover, the association between renal impairment and poor outcomes is well established, with significantly increased mortality and need for ICU level of care. These findings were irrespective of age, sex, or other comorbidities such as hypertension, diabetes, and respiratory diseases. The association of mortality between preexisting chronic kidney disease (CKD) and the severity of COVID-19 infection has been studied[66]. The need for renal replacement therapy (RRT) correlated with poor outcomes. Mortality was also significantly increased in renal transplant recipients. Several studies found a statistically significant rise in SCr and blood urea nitrogen in patients with COVID-19, as well as the severity of proteinuria, hematuria, and decline in estimated glomerular filtration rate. Viral RNA positivity was detected in the urine of 5.7% of patients in some studies[67], but it is unclear if this correlated with disease severity. While both the occurrence of and mortality due to kidney injury seem to be declining (≥ 75% in critically ill patients with mortality of 67% in studies published before the end of May 2020), it still constitutes a significant morbidity and mortality factor in COVID-19 patients. For this reason, health experts call for the early detection of renal dysfunction in patients with COVID-19 to prevent further kidney damage and provide appropriate renal support.
Cutaneous manifestations
While respiratory and gastrointestinal manifestations are the predominant presenting features of COVID-19 patients, reports on cutaneous manifestations are increasingly noted. In some studies, the estimated prevalence of cutaneous manifestations in COVID-19 ranges between 0.2%-20%. The cutaneous manifestations recorded are urticaria, chilblain-like lesions, livedo reticularis, petechial rash, and finger/toe gangrene, with the majority of lesions localized on the trunk, followed by extremities[68]. Cutaneous involvement usually follows the respiratory symptoms; nonetheless, in the minority, it preceded systemic features.
Histopathological analyses suggested a predominance of spongiosis, perivascular infiltrate of lymphocytes, and thrombogenic vasculopathy, but the potential mechanisms remain to be investigated. One small systematic review of 507 European patients suggested that the presence of the ACE-2 receptor on skin keratinocytes proposes that skin might be a potential target for the virus[69].
A systematic review from Switzerland mentions vesicular rashes during an initial diagnosis of COVID-19, suggesting cutaneous involvement as a valuable prognostic factor for disease progression and correlation to disease severity[70].
Overall, developing a comprehensive understanding of all clinical manifestations of COVID-19 infection will require knowledge of all possible disease presentations. It is suggested that accurate and rapid identification of cutaneous manifestations may be vital to early diagnosis and can portend a better prognosis in COVID-19 patients. Notably, the majority of these studies failed to report any correlation between COVID-19 severity and skin lesions.
Severity assessment
Although the reported mortality rates through the pandemic's progression have decreased, ICU mortality rates remain higher than those seen in ICU admissions for non-COVID viral pneumonia. Over 110 systematic review articles investigating the aspects of severe COVID-19 infection were analyzed with the goal of risk stratification and the mitigation of poor outcomes.
Predisposing factors which increase the patient's risk of severe disease should be assessed at the onset of admission. Multiple studies found that individuals with obesity, cardiovascular disease, hypertension, diabetes, chronic lung disease/smoking history, CKD, chronic liver disease, history of cerebrovascular events, male sex, or older age were found to have a more severe illness (with hypertension, cardiovascular disease, and diabetes conferring the most significant risk). Specific clinical assessments were found to have a greater likelihood of severe disease burden, including dyspnea at presentation, elevated pro-inflammatory markers, evidence of coagulopathy, signs of cardiac damage, acute kidney injury, lymphopenia, or neutrophilia[71].
Next, physical and lab assessments that have been found to indicate a greater likelihood of more severe disease are patients presenting with dyspnea, elevated inflammatory markers (CRP, ESR, somatostatin analogue, IL-6, IL-8, PCT, D-dimers, ferritin, interferon-α, tumor necrosis factor-α), evidence of coagulopathies (elevated D-dimers, thrombocytopenia, DIC, thromboembolic events), signs of cardiac damage (elevated LDH, IL-6, creatine kinase MB, elevated Pro-B-type natriuretic peptide, right ventricular dilation/evidence of right heart strain, emerging arrhythmias), acute kidney injury, and white blood cell findings consistent with either lymphopenia or neutrophilia (the high neutrophil-to-lymphocyte ratio is positively associated with disease severity)[72,73].
Critical care management of diffuse alveolar damage and pulmonary vasculature microthrombi can be achieved through mechanical ventilation or extracorporeal membrane oxygenation (ECMO). However, there have been increasing incidents of complications seen in patients requiring ECMO with concurrent COVID-19 infection, likely due in part to the hematological dynamic changes inherently involved in ECMO, coupled with the pro-inflammatory and pro-coagulopathic nature of the COVID-19 disease itself. Due to the reliable association with IL-6 and COVID-19 disease severity, tocilizumab and monoclonal antibody therapy early in the disease course have shown promising results. Additionally, RAAS inhibitors in hypertensive patients showed an improved prognosis in many cases[74].
The severity of COVID-19 infection in adults with the comorbidities mentioned above differs from pediatric and immunosuppressed patients. While the severity of the organic disease is severe, the psychological burden develops as the global pandemic continues. Studies show that isolation and social distancing measures necessary in epidemic states to minimize the spread of communicable diseases have significant psychological impacts on parents, children, and adolescents. Although long-term and persistent effects of the pandemic are currently unknown in instances of anxiety, depression, stress, and other mental strains yet to be discovered, what has been observed is that the duration of the isolation is having a more significant impact on the mental well-being of children and adolescents than the intensity of isolation. Solutions to mediate psycho-social burdens associated with the pandemic are evolving, but the child and adolescent developmental impact remain to be seen.
D-dimer
D-dimer elevations as a sign of pro-inflammation are significantly related to COVID-19 infections. The activation of the coagulation cascade is a common feature of DIC and adverse clinical outcomes in COVID-19. D-dimer is an important prognostic tool that is often found to be elevated in patients with severe infection. Regardless of the D-dimer reference value, the studies show that D-dimer concentrations were significantly higher in patients with more severe infection than non-severe forms and were associated with an increased risk of mortality[75]. Early integration of D-dimer testing can be practical for better risk stratification and guidance in clinical decision-making. Further investigation is warranted to evaluate the appropriateness of D-dimer monitoring as a management tool for this disease.
Lymphocytes
Meta-analyses evaluating the feasibility of specific markers in assessing the severity and prognosis of COVID-19 patients demonstrated a significant inverse association of peripheral lymphocyte levels with progression and mortality. Those patients with a low lymphocyte count at baseline were found to have a higher risk of disease severity. A meta-analysis reported that lymphopenia and neutrophilia on admission were significantly associated with increased risk of progression to severe disease and death, suggesting that these variables may help risk stratification models[76].
However, the results of studies regarding the prognostic value of lymphocyte subsets are inconsistent. A meta-analysis concluded that increased neutrophil/ lymphocyte levels and a low lymphocyte-to-CRP ratio might indicate a poor prognosis in COVID-19 patients[77]. COVID-19 predictive equations were generated in another meta-analysis based on CRP and D-dimer levels and lymphocyte or the neutrophil count. These equations exhibited high specificity, sensitivity, positive and negative predictive values and suggested that the equations could predict the severity of outcomes of COVID-19 patients[78].
Treatment
Treatment articles reviewed included those studying antiviral drugs such as Lopinavir/Ritonavir, Favipiravir, and Remdesivir. Lopinavir/Ritonavir did not show any significant difference in mortality or progression to a more severe course or cure. However, some benefits were seen in the duration of hospital stay. Favipiravir may have some role in improving clinical and radiological imaging but has no benefit on oxygen requirements or viral clearance. Remdesivir is the only antiviral drug that has been shown to improve recovery and reduce serious adverse events[79-81]. Additionally, it may reduce mortality, though some studies did not show mortality benefits. It was also seen that five-day treatment with Remdesivir might provide similar benefits with fewer harmful effects than a 10-d course[82].
The prevalence of venous thromboembolism in COVID-19 patients has been reported to be about 10%-35%, with autopsy results rising to 60%. Biomarkers related to platelet activation like D-dimer have been shown to have prognostic value in COVID-19 patients. There was a slight tendency to reduce the mortality rate using therapeutic anticoagulation in patients with COVID-19 on mechanical ventilation.
Current evidence shows no benefit in using HCQ in patients with mild to moderate COVID-19 infection. Additionally, HCQ has been associated with higher adverse events, including skin pigmentation, ocular toxicity, QT prolongation, and worsening psoriasis lesions[83].
The effect of convalescent plasma products is based on randomized controlled trials (RCT). In these trials, convalescent plasma did not decrease all-cause mortality, but early initiation may decrease mortality rate compared to late initiation. Convalescent plasma and immunoglobulin were both effective in relieving symptoms of COVID-19[84,85].
Corticosteroids may reduce mortality in patients with COVID-19 and ARDS, but the evidence is inconsistent for patients with COVID-19 without ARDS. Excessive inflammatory response and lymphopenia were both associated with severity, leading to the recommendation that, if not contraindicated, steroids should be considered in the absence of adverse effects.
Tocilizumab is an interleukin-6 receptor antagonist that has been used in the treatment of severe COVID-19 infections[86]. There are indications that tocilizumab can reduce mortality and prevent mechanical ventilation in severe COVID-19 infections, but results need to be confirmed with high-quality clinical trials before the drug is implemented as a standard of care.
Anticoagulation
Anticoagulation methods studied in the treatment of COVID-19 included unfractionated and low molecular heparin, apixaban, clopidogrel, dipyridamole, and tissue plasminogen activator. The association between mortality rate and incidence of thromboembolic events in patients with COVID-19 infection receiving venous thromboembolism prophylaxis was evaluated as combination therapy or single-drug therapy, with studies showing no superiority of any anticoagulant.
According to one article that looked at three separate studies[87], thromboembolism in COVID-19 infected patients does not warrant a change in guidance on thromboprophylaxis among hospitalized patients, but the studies have overall poor quality due to methodological limitations. The rest of the articles emphasize the importance of anticoagulation. Overall, the findings indicate that therapeutic doses might be associated with better survival compared to prophylactic doses. Data suggests that prophylactic and therapeutic anticoagulation may reduce mortality in COVID-19 patients[88].
Antiviral
Favipiravir, Lopinavir/Ritonavir, and Remdesivir were evaluated in our analysis, being studies in combination or as single-agent therapy. These articles compared antiviral drugs with other medications used for COVID-19 or standard of care. Favipiravir has a more favorable safety profile than other antivirals with mild and manageable side effects. The available data about combination therapy of Favipiravir with Lopinavir/Ritonavir is not enough to favor this combination over other treatments[89]. Remdesivir showed a positive impact on the hospitalized patients compared to the standard of care. The safety profile of Remdesivir in COVID-19 patients requires further studies with adequate design and power.
Convalescent plasma
Articles focusing on the effectiveness of convalescent blood product (CBP) therapy in COVID-19 infection and severe acute respiratory infections of viral etiology showed that most of the included studies had a critical risk of bias, leading to their exclusion from the analysis. From the remaining studies, a decline of all-cause mortality was observed only in observational studies, where using CBPs earlier compared to using CBPs later was associated with a significant reduction in all-cause mortality. Additionally, CBPs did not increase the risk of adverse events between intervention and control groups. However, in RCTs, the all-cause mortality showed no difference between the interventional and control groups.
Overall, the certainty of the evidence was low to very low. The effectiveness of CBPs in COVID-19 infection has poor validated results, but their use appears to be safe[90]. This observation contrasts with SARS coronavirus infection, which was similarly low to very low-quality studies that have effectively proven CBPs reduce both all-cause mortality and symptom duration.
Immunosuppressants
The role of immunosuppressants has been proposed as a possible treatment for the hyper-immune response in later stages of the infection, developing acute respiratory distress syndrome, multiorgan failure, and increasing mortality. The most discussed drug in our evaluation was the interleukin-6 receptor inhibitor monoclonal antibody tocilizumab (all six reviews), followed by corticosteroids, calcineurin inhibitors, and other immunosuppressants (one systematic review). The efficacy, mortality reduction, complication prevention, and their use alone or with the standard of care were discussed. The majority of the reviews show that the use of tocilizumab (either alone or in addition to the standard of care) has the potential to treat effectively, reduce mortality, and prevent mechanical ventilation[91]. One of the reviews evaluated provided no conclusive findings based on the low quality of evidence.
Corticosteroids
The administration of systemic corticosteroids compared with usual care or placebo in critically ill patients with COVID-19 was associated with lower 28-d-all-cause mortality[92]. Most studies show that the late administration of steroids in the course of the disease provides benefit in most patients and more severe, critically ill patients; however, other studies instead demonstrated that there was no survival benefit found with the use of corticosteroids[93] and that mortality risk was increased with the use of corticosteroids, likely secondary to a longer length of stay, a higher rate of bacterial infection, hypokalemia, and several other adverse effects[94]. Therefore, although the use of corticosteroids in some cases improved the clinical features of viral pneumonia, there was no confirmed evidence of corticosteroid therapy reducing the mortality in all COVID-19 patients. Results from the RECOVERY trial highlighted that steroids could potentially be an excellent therapeutic weapon against the coronavirus[95]. There was also a significant reduction in death with dexamethasone, which was seen only in severe cases of patients on ventilators or moderate cases requiring supplemental oxygen therapy[96]. However, there was no benefit observed in mild to moderate patient cases without hypoxia who did not require oxygen. Nonetheless, further studies are required to account for the range of co-variables and confounders, which would detail the dosing regimen and the duration of corticosteroid therapy and the stage at which therapy should be initiated to benefit patients and avoid adverse effects of corticosteroids.
HCQ
HCQ is an antimalarial drug used to treat rheumatological conditions, such as rheumatoid arthritis and systemic lupus erythematosus. It has been shown to have antiviral properties against COVID-19 "in vitro," but the evidence regarding its efficacy "in vivo" lacks the scientific support for its use[97]. Although considered a commonly well-tolerated drug, adverse effects to the gastrointestinal, cardiac, ocular, nervous, and dermatological systems were noted. The use of HCQ to treat SARS-COV-2 infection lacks efficacy in decreasing the risk of hospitalization or short-term mortality. This finding challenges the proposed association with increased mortality (either alone or in combination with azithromycin) and elicits the need for high-quality data from multicentric randomized control trials.
RAAS
A review of 21 systematic reviews of dozens of studies across the globe has, for the most part, failed to find a significant association between RAAS blockade by either agent–or even by both combined in some studies–with the risk, severity, or mortality of COVID-19 infection.
A massive debate on the role of angiotensin-converting enzyme inhibitors (ACEi) and angiotensin receptor blockers (ARBs) in patients with COVID-19 and whether these agents should be continued in infected individuals was a significant question in the medical community at the onset of the pandemic[64,98]. Many global studies have mostly failed to find a significant association between RAAS blockade with risk, severity, or mortality in COVID-19 patients. While the viral spike coat protein of SARS-CoV-2 binds to the human ACE-2 cell surface receptor to cause infection, those hypertensive patients currently managed on ACEi or ARBs had a small, albeit significant, decrease in mortality. Some studies found this mortality benefit to be associated only with ARBs, not ACEi, while others have reduced death rates with both classes of medicines. This fact has encouraged some health experts to suggest that RAAS inhibition may be protective against COVID-19; however, such a recommendation requires more robust evidence. Current guidelines advise that hypertensive patients should continue taking ACEi or ARBs if they become infected with COVID-19; they do not recommend the initiation of ACEi or ARBs to treat COVID-19 infection.
Technology
We included 24 systematic review articles about the technology used to deliver quality healthcare during the COVID-19 pandemic. As face-to-face encounters have become more restricted over the past several months, the rise of telemedicine has allowed many health care professionals to provide continuity of care for patients. The introduction of various telecommunication modalities, including videoconferencing, telerehabilitation, tele-neuropsychology, teledermatology, telemonitoring, teletherapy, and telementoring, have been a great way to curb the transmission of COVID-19, increase access to healthcare, and triaging patients suffering from various ailments[99]. Analysis of these articles has revealed that the general population has adopted an overall favorable telemedicine response because of its convenience and comfort.
Unfortunately, telemedicine also has several drawbacks. Many patients do not have adequate internet access and/or are not technology savvy. Furthermore, patients may have limited care because telemedicine services do not always guarantee the same medical care team. Additionally, telemedicine is more beneficial for patients with chronic conditions that do not always require a physical examination. Although telemedicine benefits are irrefutable, we will need more RCT to determine the long-term effects and costs of telemedicine on society.
Special populations
Regarding special populations with COVID-19, we included 263 systematic reviews. Of these, children were the most common, with 33 articles reported. These articles' overall consensus pointed out that most children tend to have mild disease and a better prognosis. Physicians needed to be mindful of this population: Multisystem inflammatory syndrome cases in children (MIS-C), which is fatal if early recognition, supportive management, and early immunomodulators are not implemented. Morbidity and mortality were low overall In the neonatal population[100-102]. The second special population we looked at was pregnant women, with 16 articles evaluated. Most pregnant women were reported to be asymptomatic, although it was observed that preterm birth rates in some women were higher compared to COVID-19 negative pregnant women. Some unique findings included decreased white cell count and possible impairment in follicular and luteal phases. Vertical transmission of COVID-19 was reported to be low.
Patients with malignancies and COVID-19 were reviewed, included in 19 articles. Cancer patients tend to have higher inflammatory markers at presentation, more severe symptoms clinically, greater risk of complications, and increased ICU admissions. Chemotherapy in these patients has not been associated with an increased risk of severe COVID-19. Delay in cancer treatment in COVID-19 positive cancer patients has been favored by many oncologists, although no evidence of interactions of COVID-19 treatment and chemotherapy has been identified[103].
Regarding diabetic patients with COVID-19 infection, they were reported to have a higher prevalence of progression to ARDS, which led to a higher rate of ICU admissions and subsequent mortality. It was also noted that diabetic ketoacidosis (DKA) in COVID-19 patients tended to lead to mortality that approached 50%. Eight articles regarding smoking and COVID-19 were analyzed. There seems to be a positive correlation between smoking and disease severity. This applies to both current and past smokers, although further studies need to be performed before establishing this connection. The obese population was reviewed in five articles. Findings showed obese individuals had a higher risk of contracting COVID-19, increased risk of ICU hospitalizations, severe disease, as well as diminished prophylactic and therapeutic responses to standard treatment. Lastly, we evaluated transplant patients with COVID-19 infection, covered in five articles. Higher mortality rates were observed in patients with solid organ transplants older than 60 years of age. There was a low incidence of reported COVID-19 infections in renal transplant patients; however, patients were reported to have more severe disease progression in those who were infected. This particular population was at greater risk of acute renal failure, ICU admission, and RRT[104]. As we look at the diverse populations studied, we find that COVID-19 not only impacts our ability to diagnose and treat early but may affect each population differently.
DM
We included two systematic review articles regarding the epidemiology of COVID-19 patients with DM. The articles found diabetes had a negative effect on the health impact of COVID-19, and the prevalence of DM in patients with severe COVID-19 was significantly higher than moderate patients with COVID-19. Five systematic review articles were evaluated regarding the clinical features of COVID-19 in patients with DM; these articles concluded that those with severe COVID-19 had higher blood glucose levels, especially with the use of corticosteroids. It was observed that DM was associated with increased mortality, severe COVID-19 infection, ARDS, and disease progression[105,106].
We included three articles regarding the treatment of COVID-19 patients with DM. Due to media coverage of dexamethasone benefits in COVID-19, this may increase patients' self-medicating themselves[107]. Studies have shown that corticosteroid use in diabetic patients puts them at a higher risk of hospitalization due to diabetic complications. Therefore, healthcare workers should be avidly aware of the potential risk of using these medications[107].
One systematic review demonstrated COVID-19 patients with combined DKA and hyperosmolar hyperglycemic state (HHS) had higher mortality than DKA alone, with DKA/HHS representing 20% of the total cases of DKA, concluding the importance of differentiating between these two groups[108]. One meta-analysis showed an increased risk of ICU admission for COVID-19 in diabetic patients and increased mortality in these populations[109]. The majority of studies were performed in COVID-19 patients with DM type 2; DM type 1 poses unique challenges, with research showing that in COVID-19 patients with DM type 1, modified management and telemedicine have been practical tools for patient care.
Obesity
We reviewed a total of 14 systematic review articles on the relationship between obesity and COVID-19. We included one systematic review article regarding the epidemiology of obesity pertaining to COVID-19[110]. Obese patients with hypertension, type 2 DM, active smokers, lung disease, and/or cardiovascular disease are at higher risk for ICU admissions, severe COVID-19, and disease progression. The six articles discussed patients suffering from obesity and COVID-19 show a positive correlation between higher body mass index and severe COVID-19 cases. COVID-19 patients with obesity were significantly affected and had a worse prognosis than those without. In one particular review article, the mechanistic pathways in obese individuals were investigated, evaluating factors linked with COVID-19 risk, severity, and the potential for diminished therapeutic and prophylactic treatments among these individuals. These studies concluded that individuals with obesity are linked with a significant risk of morbidity and mortality from COVID-19[111].
Regarding the severity assessment of COVID-19 in obesity, there were seven articles discussed. A meta-analysis suggested a linear association between the severity and mortality of COVID-19 and body mass index (BMI)[112]. Also, a BMI ≥ 30 kg/m2 was associated with a higher risk of increased severity in COVID-19 and in-hospital mortality. Furthermore, the study revealed obesity and being overweight were represented as unfavorable factors for COVID-19 infection, where the higher the BMI, the worse the outcome. This occurred by worsening infection, resulting in increased hospitalizations, worse outcomes, and markedly significant mortality, especially when coinciding with other chronic conditions and in the elderly. BMI is an essential routine measurement that should be regularly assessed in the management of COVID-19 patients, and special attention should be given to patients with obesity. Obesity may serve as a clinical predictor for adverse outcomes; therefore, BMI in prognostic scores may play an essential role in predicting the clinical outcomes[113].
Pregnancy
We included one systematic review assessing the clinical presentation of COVID-19 infection in pregnant women[114], which found the most reported clinical symptoms were fever, cough, and dyspnea. Commonly reported laboratory abnormalities included elevated CRP or procalcitonin, lymphopenia, and elevated transaminases. Some complications also included preterm birth and maternal ICU admission. Maternal mortality, however, reported a low prevalence. Another systematic review article evaluated screening and diagnosis of COVID-19 during pregnancy[115], demonstrating the most common symptoms included fever and cough, and for accurate diagnosis, RT-PCR and CT scan can be used together. Further studies showed the clinical characteristics of pregnant women with COVID-19 are similar to those of non-pregnant adults[116], but available data only include pregnant women infected in their third trimesters.
One systematic review article regarding the epidemiology of pregnancy showed insufficient data to suggest if there is transplacental transmission to neonates, with only one neonatal death reported, and 3.4% of neonates suffered from COVID-19[117]. Regarding the special population of pregnancy, we included 16 systematic review articles that showed there is not enough evidence to suggest vertical transmission, most articles stating that it is unlikely although suggesting that it cannot be ruled out. However, the data suggested an increased risk of preterm birth and SARS-CoV-2, leading to an increased need for cesarean delivery. The clinical presentation might not be drastically different as compared to non-pregnant adults[118]. The effect on fertility is not apparent[119].
Children
We looked at 39 systematic review articles regarding the relationship between COVID-19 and the pediatric population. Compared to adults, children presented with milder symptoms. The most common symptoms included fever, cough, vomiting, and diarrhea. Approximately one-third of the pediatric population were asymptomatic, raising concerns for children unknowingly transmitting the virus to at-risk individuals[116]. Overall, the disease course for children was milder, with fewer hospitalizations, ICU admissions, mechanical ventilation, and mortality. There are multiple theories as to why the pediatric population is not severely affected by COVID-19. The theories are as follows: an immature immune system resulting in no cytokine storm, poorly developed ACE2-receptors, fewer comorbidities, and the development of antibodies due to children being infected by other respiratory viruses that can protect against COVID-19[117].
The primary avenue for children contracting the virus was through family members. If a family member tested positive, it is recommended that children be tested as asymptomatic carriers[120].
Children were rarely the cause of significant outbreaks, bringing into question the efficacy of school closures. According to public health experts, school closures could do more harm than good. School closures could increase childhood depression and anxiety rates and cut children from vital resources such as meals, school nurses, and quality education. A small percentage of children did develop severe symptoms of COVID-19 resulting in ICU admissions, mechanical ventilation, and death. Children with comorbidities were at increased risk of a more severe form of infection. The comorbidities most associated with severe COVID-19 infections included cardiac diseases, diabetes, chronic non-asthmatic pulmonary disease, asthma, and obesity. Several MIS-C were reported, which resulted in shock, multiorgan failure, and death[121,122]. However, a clear correlation between COVID-19 and MIS-C does not exist. It must be determined if COVID-19 increases the risk of MIS-C or if there is simply a temporal relationship between both conditions. The primary form of treatment for severely ill children included intravenous immunoglobulins, corticosteroids, and immunomodulators. However, the efficacy of these treatments is not known. Therefore, the systematic review articles highlight the potential for additional studies to truly understand the effects of COVID-19 in children. The areas that need to be further studied include the possibility of vertical transmission, the extent to which children are transmitters of the virus, the efficacy of school closures in fighting the outbreak, and the ideal treatment course for severely infected children[120].
Mental health
Sixty-three articles were reviewed regarding the mental health impact of COVID-19. COVID-19 has caused many mixed emotions and has impacted people from a mental health perspective due to the isolation and "social distancing" components. It is estimated that a quarter of the population experienced significant stress due to the pandemic. Given that many stores had limited supplies, it created a panic buying atmosphere[123]. This was mainly due to the survival of the fittest mentality, the fear of the unknown, and coping mechanisms. Bereavement and grief were important aspects many dealt with due to the numerous deaths from the pandemic. Having afterlife ceremonies such as funerals benefited many family members as it was a more sentimental way of saying goodbye[124].
Studies showed that isolation could cause neuroendocrine-immune changes, which further exacerbates COVID-19 and mental health associations. The early stages of the virus caused delirium in a large proportion of the patients. Pulmonary insults of the disease tended to show high amounts of cognitive dysfunction. The elderly were at an increased risk from both a physical and mental perspective from the increased social distancing. It was recommended that this group have more activity and exercise planned before enforcing the lockdowns. The pediatric population's most common disorders were acute stress disorder, post-traumatic stress disorder, adjustment disorder, and grief[125]. The younger population of children also will have higher effects from depression and anxiety. Laws should be more intentional about providing counseling[126].
Though beneficial from a public health standpoint, quarantine has the propensity to impact an individual's psyche negatively and has in some ways passed the brink of being considered clinically relevant. Many of the mental health problems included depression, anxiety, mood disorders, and lack of self-control. Age and sex did not correlate with anxiety disorders. These conditions not only impacted the public and patients but healthcare providers as well[127].
Healthcare workers may be presented with anxiety, depression, and insomnia. Studies showed that HCWs who worked in areas with fewer resources and protective gear tended to be more stressed. Comparing HCWs to non-healthcare workers found their psychological stress level was similar in many factors, except that HCWs had higher amounts of insomnia. Physicians and nurses were the most impacted and resulted in many sleep disturbances. Other studies showed evidence that those with comorbidities had even more stress than health care workers. The virus has shed light on the importance of and need for solutions to improve the well-being of HCWs by providing more education and counseling through policy change[125].
Smoking
We included 16 systematic review articles that investigated the relationship between smoking and COVID-19 infection. Severity, progression, and adverse outcomes of COVID-19 infection were discussed in relation to smoking status, comparing past and current smokers to non-smokers[128]. Severe cases were defined as critical with the need for ICU, refractory, and non-survivors. Several studies found patients who are both current and former smokers are at an increased risk of severe infection and progression[129]. Meanwhile, a few studies suggested that current smokers have a reduced risk of infection than both former and non-smokers, evidenced by an unexpectedly low prevalence of current smokers among hospitalized patients with COVID-19. However, those hospitalized were at higher odds of adverse outcomes than non-smokers and lower odds than former smokers. Furthermore, due to the low prevalence of hospitalized current smokers, further exploration of nicotine as a therapeutic option is suggested as a potential treatment in COVID-19.
In particular, patients with the chronic obstructive pulmonary disease have a significantly higher odds ratio of severe infection vs current smokers[130]. Findings showed that these patients were older and predominantly males compared to non-severe cases. With most studies finding an increased risk between smoking and COVID-19 severity, a continued focus on smoking cessation efforts is recommended[131].
Cancer
Twenty articles were reviewed regarding the special populations of cancer patients with COVID-19 infection. It was hypothesized that the unique nature of the pathophysiology and the treatment protocols utilized for cancer patients might lend themselves to specific considerations regarding precautions, screening, treatment, and outcomes. Overall, cancer patients were more likely to experience severe COVID-19 disease when compared to those without malignancy. Additionally, cancer patients were found to have lower platelet levels with higher inflammatory markers, leading to increased susceptibility for complications[132].
Certain risk factors were found to be significantly predictive of increased mortality in this population. It was found that the male gender, age greater than 65 years, history of hypertension, and history of chronic obstructive pulmonary disease were associated with an elevated risk of death. Interestingly, many studies found that while symptoms on admission such as dyspnea, cough, and increased sputum were more likely to predict severity, the use of antibiotics, glucocorticoids, interferon, and invasive ventilation were associated with a higher probability of death. This finding likely elucidates the fact that severe infections were treated with complex, invasive medical care. Patients undergoing chemotherapy targeted radiotherapy or immunotherapy had a more aggressive infection course, with significant interactions seen with tocilizumab, ruxolitinib, and colchicine[103]. However, increased mortality was not significantly associated with recent anti-cancer treatments, except when patients were given chemotherapy within 28 d of infection or immunotherapy within 90 d of infection[133]. These findings led to the recommendation that deviations from the standard of care for more extended periods (i.e., beyond four to six weeks) may not be necessary and indeed may lead to a significant impact on overall outcomes.
While many studies have proposed identifying outcomes in all-cause mortality within the general cancer population, some studies have focused on specific cancer types. Multiple myeloma patients were found to have a higher risk of a severe infection due to their immunocompromised status, while treatment protocols for prostate cancer patients with very low, low, or favorable intermediate-risk diseases were avoided or delayed[134].
Overall, it was found that compared to other types of cancer, lung and colorectal cancer patients were more susceptible to COVID-19 infection[135]. Cancer patients are a special population due to their immunocompromised status, cytotoxicity of their treatment regimen, nutritional status, and already increased inflammatory markers.
Cancer patients had worse outcomes from COVID-19 when compared with the general population. Despite all efforts, finding the ideal approach for cancer patients with COVID-19 is not evident. The approach to high-risk patients in this group should include vigorous screening and intensive surveillance. The approach must be dynamic and anti-cancer treatment should be modified based on the cancer type and the patient's prognosis[135].
Transplant medicine
Five systematic review articles evaluated the presentation of COVID-19 in kidney transplant recipients, who had poorer outcomes on average compared to the general adult population. This subpopulation of patients developed acute kidney injury at higher rates, subsequently requiring RRT. Kidney transplant recipients had increased rates of hospitalizations, ICU admissions, and mechanical ventilation. Compared to the general adult population, the kidney transplant subgroup was elder and had higher mortality rates. Presenting symptoms in this subgroup differed from the general population, presenting with atypical symptoms such as lack of fever and predominance of gastrointestinal symptoms[136]. An area that will need further exploration is the treatment of COVID-19 in kidney transplant recipients. The systematic review articles discussed the risks vs benefits of down-titrating immunosuppressive medications while patients are infected with COVID-19.
Additionally, HCQ showed no additional benefit in kidney transplant recipients in the treatment of COVID-19[108,137]. The systematic review articles highlight the need for additional studies to determine the optimal therapeutic approach for the treatment of COVID-19 in this population. A better understanding of treating kidney transplant recipients could potentially lead to the development of guidelines for any transplant recipient’s treatment.