Published online Jul 25, 2021. doi: 10.5501/wjv.v10.i4.156
Peer-review started: December 24, 2020
First decision: March 8, 2021
Revised: March 21, 2021
Accepted: May 20, 2021
Article in press: May 20, 2021
Published online: July 25, 2021
Processing time: 209 Days and 19.7 Hours
There were only 75 confirmed cases of coronavirus disease 2019 (COVID-19) reported in Libya by the National Center for Disease Control during the first two months following the first confirmed case on 24 March 2020. However, there was dramatic increase in positive cases from June to now; as of 19 November 2020, approximately 357940 samples have been tested by reverse transcription polymerase chain reaction, and the results have revealed a total number of 76808 confirmed cases, 47587 recovered cases and 1068 deaths. The case fatality ratio was estimated to be 1.40%, and the mortality rate was estimated to be 15.90 in 100000 people. The epidemiological situation markedly changed from mid-July to the beginning of August, and the country proceeded to the cluster phase. COVID-19 has spread in almost all Libyan cities, and this reflects the high transmission rate of the virus at the regional level with the highest positivity rates, at an average of 14.54%. Apparently, there is an underestimation of the actual number of COVID-19 cases due to the low testing capacity. Consequently, the Libyan health authority needs to initiate a large-scale case-screening process and enforce testing capacities and contact testing within the time frame, which is not an easy task. Advisably, the Libyan health authority should improve the public health capacities and conduct strict hygienic measures among the societies and vaccinate as many people against COVID-19 to minimize both the case fatality ratio and socio-economic impacts of the pandemic in Libya.
Core Tip: This review is aimed to explain and show potential reasons for having only 75 confirmed cases of coronavirus disease 2019 (COVID-19) reported in Libya during the first two months following the first confirmed case till hundreds of positive cases everyday in the following months. The epidemiological situation markedly changed from mid-July to the beginning of August as the country proceeded to the cluster phase and COVID-19 has spread in almost all Libyan cities. The Libyan health authority needs to improve its service in order to do better job to control the pandemic and reduce the virus spread within the country.
- Citation: Mahmoud AS, Dayhum AS, Rayes AA, Annajar BB, Eldaghayes IM. Exploiting epidemiological data to understand the epidemiology and factors that influence COVID-19 pandemic in Libya. World J Virol 2021; 10(4): 156-167
- URL: https://www.wjgnet.com/2220-3249/full/v10/i4/156.htm
- DOI: https://dx.doi.org/10.5501/wjv.v10.i4.156
In late December 2019, the etiologic agent responsible for the epidemic outbreak emerged in Wuhan, China, where about 27 cases of acute respiratory pneumonia was reported by the Wuhan Municipal Health Commission[1,2]. The first spread was reported in the Huanan Seafood Wholesale Market, an area that is well known for selling live animals[3]. On 9 January 2020, Chinese investigators were able to isolate and obtain the genetic sequence of the virus in a short period of time, which led to the preliminary identification of this novel virus[3,4]. Later, the disease was diagnosed as coronavirus and named ‘severe acute respiratory syndrome coronavirus 2’ (SARS-CoV-2). According to serological and phylogenetic analyses, coronaviruses are divided into four genera, named Alpha-, Beta-, Gamma- and Delta-coronavirus[5]. SARS-CoV-2 is a β coronavirus of group 2B with at least 70% similarity in its genetic sequence to SARS-CoV[6-8]. SARS-CoV-2 is the seventh member of the family of coronaviruses that infect humans[7]. Despite the coronavirus having been reported in China in late December 2019 and the first sporadic case reported outside China on 13 January 2020, it was not until 30 January 2020 that the World Health Organization (WHO) declared the outbreak as a public health emergency of international concern. In fact, it took a long time for WHO to then announce the coronavirus outbreak as a pandemic on 11 March 2020[9]. Since then, the coronavirus disease 2019 (COVID-19) has spread and struck many countries with a high case fatality rate while others with a moderate to low case fatality rate. Significantly, variations were highly considered and needed to be explained further and clarified. The epidemiological patterns of COVID-19 are unique all over the world, characterized by a highly pathogenic index and strong socio-economic impacts. However, there is a clear variation with respect to the temporal and spatial distribution of COVID-19 among different countries at the same regional level. These variations may be due to factors that influence the distribution of the disease in the populations, many of which remain unknown[10].
Still, there is a little knowledge about the epidemiology and course of COVID-19 in Libya. Therefore, in this review, we have explored the relevant data to understand the epidemiological patterns of COVID-19 in Libya.
The first confirmed case of COVID-19 in Libya was reported on 24 March 2020; the affected was a man in Tripoli who had a history of travelling to Saudi Arabia[11]. Since then, many infected cases were reported with mild clinical signs. It is well known that COVID-19 seems to affect some people more critically than others — some people experience only mild symptoms while others end up hospitalized, requiring intensive care and ventilation[12-14]. During the first two months following the first confirmed case, the epidemic curve was flattened with only 75 confirmed cases[15]. In fact, the low number of reported cases during the months of March, April and May could be attributed to the various reasons provided in the study of Rayes et al[15].
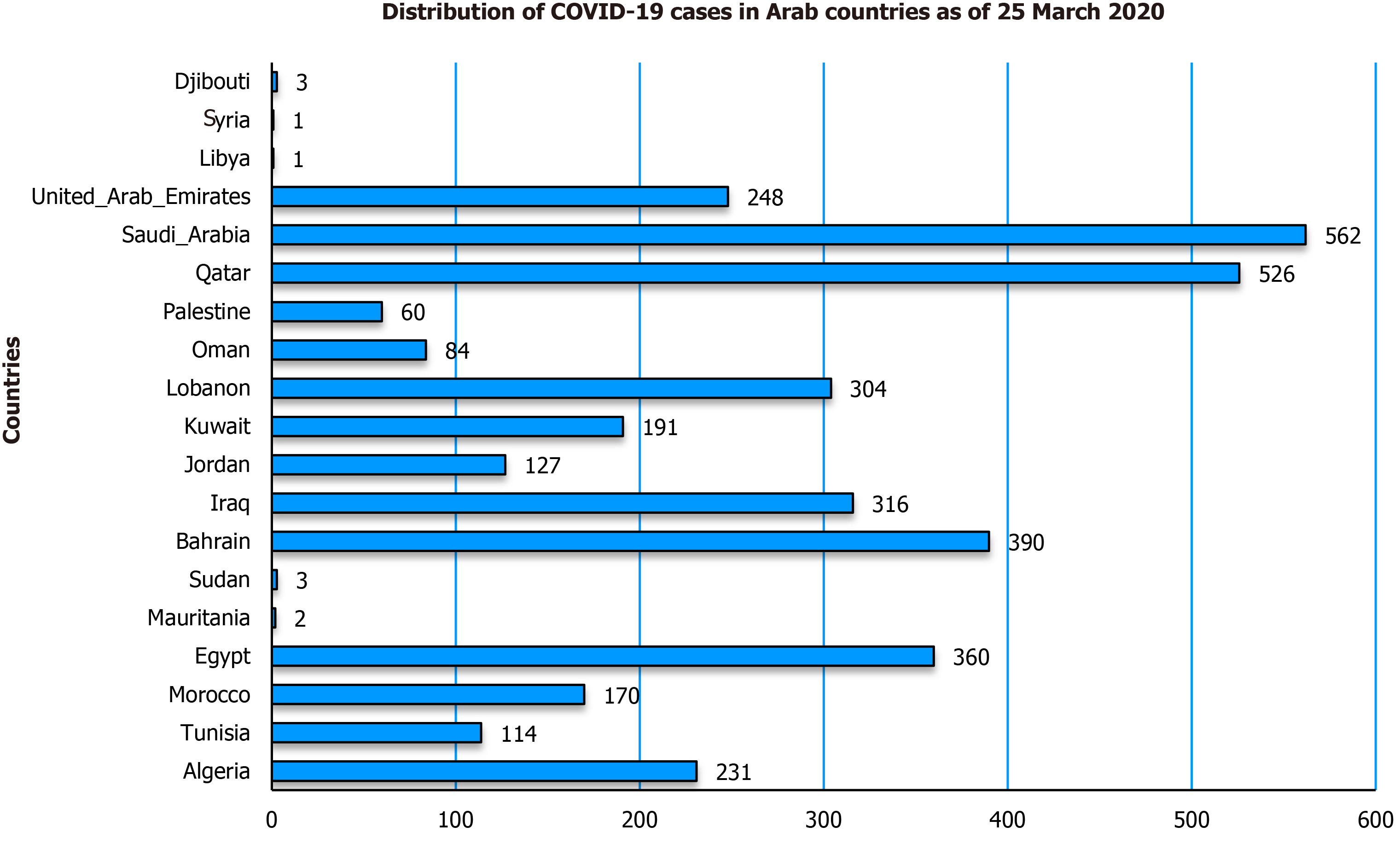
The first confirmed case in Libya was on 24 March 2020. The next day, there were huge differences between the total number of confirmed COVID-19 cases reported in Libya and those of the neighbouring Arab countries (Figure 1).
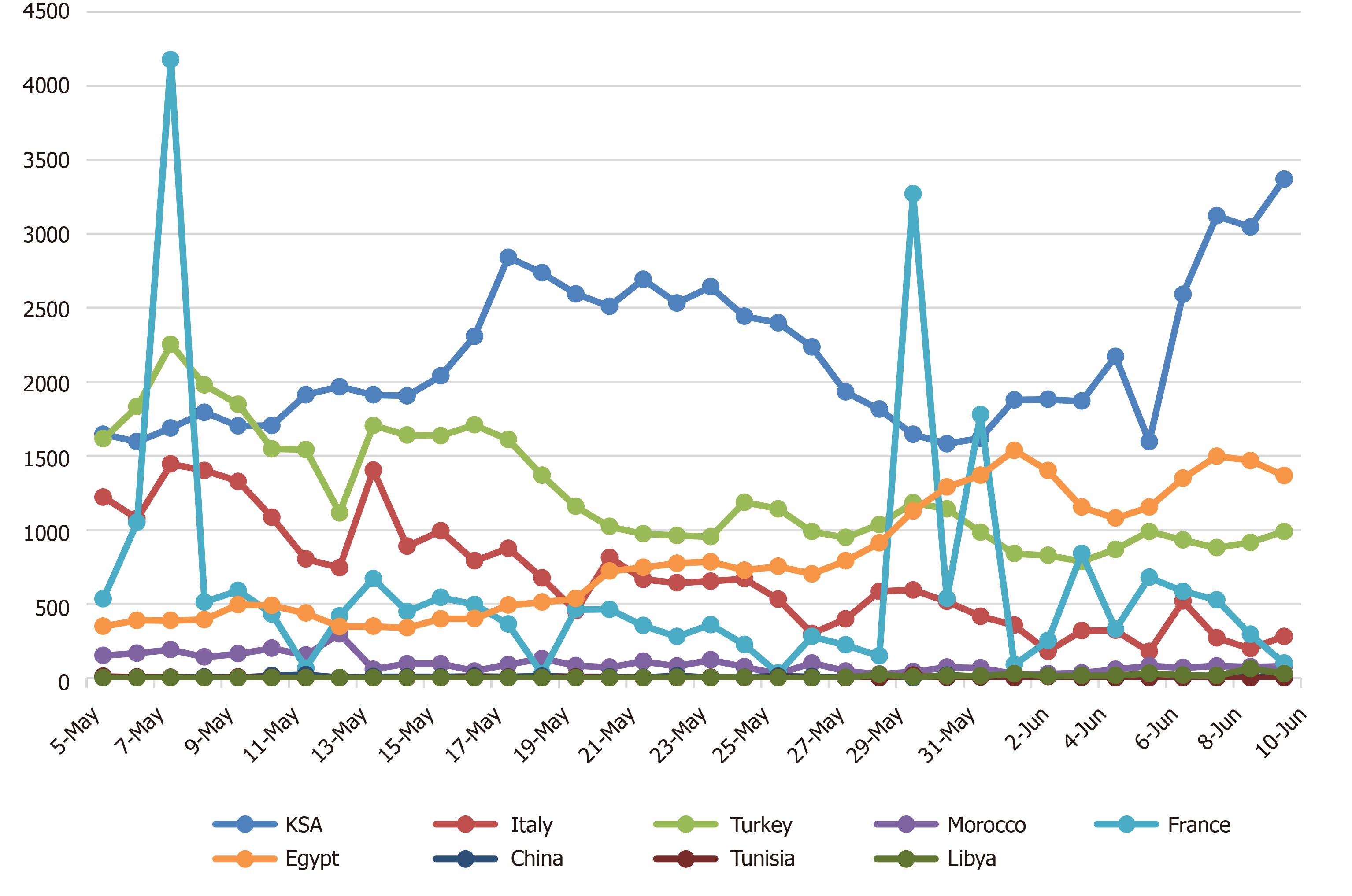
The epidemic curve of COVID-19 in Libya could have been influenced by the travellers returning from different countries (Figure 2).
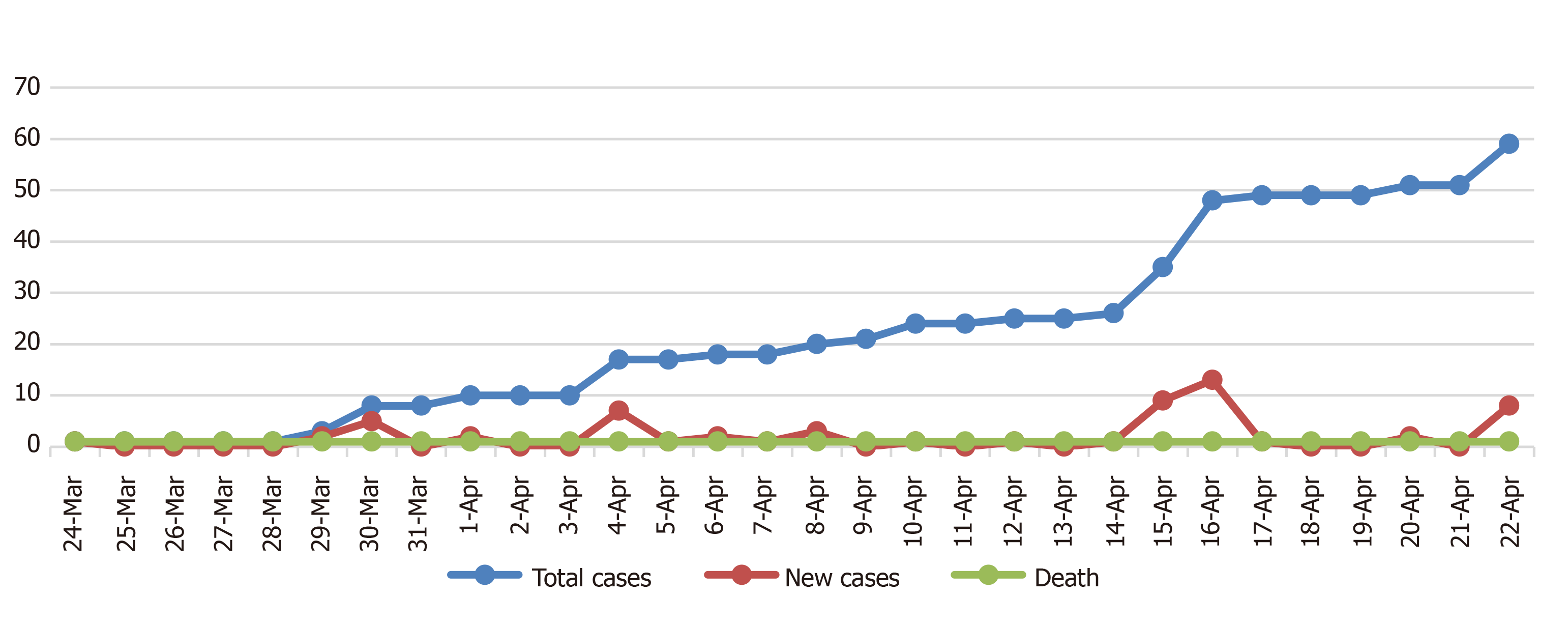
The distribution of the number of daily cases, total cases and deaths of SARS-CoV-2 reported between 24 March and 22 April 2020, i.e., over a 30-d period, with about 1181 samples screened by reverse transcription polymerase chain reaction, revealed 59, 1 and 15 confirmed cases, deaths, and recovered cases respectively (Figure 3). However, the epidemiological situations of the neighbouring countries were highly variable and significant in comparison to the confirmed cases reported in Libya (Figure 1).
The first confirmed case of COVID-19 in Egypt was on 14 February 2020, in Algeria on 25 February 2020, in Morocco on 2 March 2020, in Tunisia on 4 March 2020 and in Libya on 24 March 2020; however, the disease pattern was different for each country[16].
In Libya, there were 9 and 13 confirmed cases of COVID-19 reported on 14 and 15 April respectively, clearly indicating the presence of asymptomatically underestimated active cases before this time[17,18]. Consequently, on 16 April 2020, following the recommendation of the Scientific Advisory Committee (SAC), the Libyan authorities imposed a complete lockdown for one week, starting from 17 April 2020. Indeed, the early lockdown and various precautionary measures that were taken by Libyan authorities were highly significant in preventing the transmission of the virus among the populations.
Several precautionary measures have been implemented by Libyan authorities following the recommendation of SAC, including the closing of schools, cancelling of all festivals, closing of airports, and lockdown of most commercial private industrial units. These precautionary measures were taken for COVID-19 control and prevention, as recommended by WHO, to reduce the exposure and transmission of virus infection among the population.
Thus, the country attempted to prevent the spread of the infection and minimize the risk of virus transmission. Further, the political instability of the country and civilian war indirectly impacted the prevention of virus transmission at the beginning of COVID-19 in Libya.
Despite the precautionary measures taken to minimize the possibility of transmission of the virus from travellers coming from infected countries, there were many confirmed cases of SARS-CoV-2 among those who returned to Libya. These travellers belong to different regions of the country, which resulted in a change in the epidemiological situation of the disease and led to an increase in the number of cases recorded in different cities.
The first batch of returning flights to Libya was on 5 May 2020, during which time the epidemiological situation of COVID-19 in Libya was stable, and the number of confirmed cases started to increase by the end of May (Figure 4).
On 26 May 2020, two cases (36-year-old male and 55-year-old female) of COVID-19 were reported for the first time in the southern region of the country (Sabha province). These cases might be linked with the history of the travellers returning from countries highly affected by COVID-19. However, according to the National Center for Disease Control (NCDC), the COVID-19 cases that were reported in Sabha were found to have resulted from contact with a woman who had been suffering from respiratory symptoms and died on 26 May 2020. In fact, there are two potential pathways for the entrance of disease to the south of Libya: first, the return of travellers from infected countries; and second, from asymptomatically infected immigrants crossing the southern Libyan border from the neighbouring countries. It took only one week, i.e., from the end of May to the beginning of June, for southern Libya to report 80 new confirmed cases of COVID-19. Therefore, the epidemiological patterns of COVID-19 in southern Libya, especially in the Sabha province, were totally different from the Tripoli area and the rest of the Libyan region. For the given period, the WHO published an estimation of R0 to be 1.4-2.5 in the southern region (Sabha), which was higher than that of Tripoli. Expectedly, a high number of COVID-19 confirmed cases reported in the southern region were attributed to multifactorial determinant causes correlated to the social lifestyle of the people in the area, which included unrestricted transitional movements between small villages and cities of the south. Additionally, weak quarantine measures that led to the easy movement of people from known infected areas to others without control from the authorities was another contributing factor. Consequently, on 28 May 2020, the Libyan authorities decided to block all the administrative borders of Sabha city and impose a lockdown and curfew within the city for seven days.
The return of Libyan travellers from high-risk areas was considered the principal factor for the entrance of COVID-19 into the southern region, despite the measures taken by the Libyan authorities to minimize the likelihood of the virus’ entrance into the country. Over the previous years, various transboundary viral diseases of public health and socio-economic importance, including the rift valley fever, were reported in the southern region of the country[19,20]. Further, despite the period of pre-quarantine measures and the quarantine throughout the pandemic, there was uncontrolled transportation between the cities and within the cities of the country, which potentially influenced the positive test rate of COVID-19. According to the CDC, Libya, the individuals who were COVID-19 positive, as reported in different Libyan cities, had a history of traveling to the southern region. At the beginning of June 2020, 30 of the 62 confirmed cases of COVID-19 were linked to people with a history of traveling to infected countries.
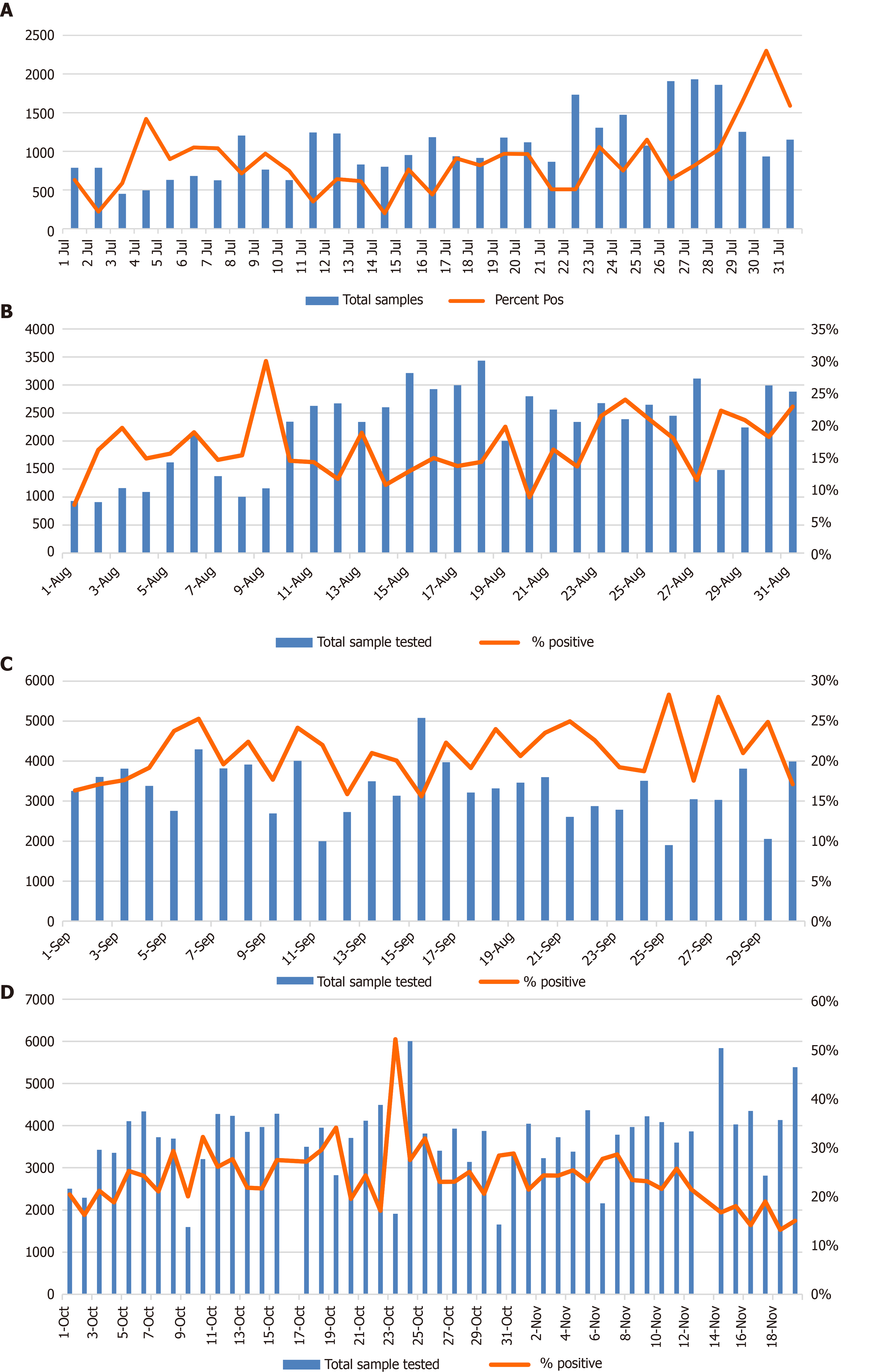
Predictably, the epidemiological situation markedly changed from mid-July to the beginning of August, and the country proceeded to the cluster phase. There was an increase in the testing capacities by mid-July; consequently, the positive test rate increased as well. The average daily positivity rate from mid-July to August was estimated to be 14.54% (Figure 5A and B), while throughout September this rate was estimated to be 21% (Figure 5C). The average positivity rate from October to 19 November 2020 was estimated to be 23.84% (Figure 5D).
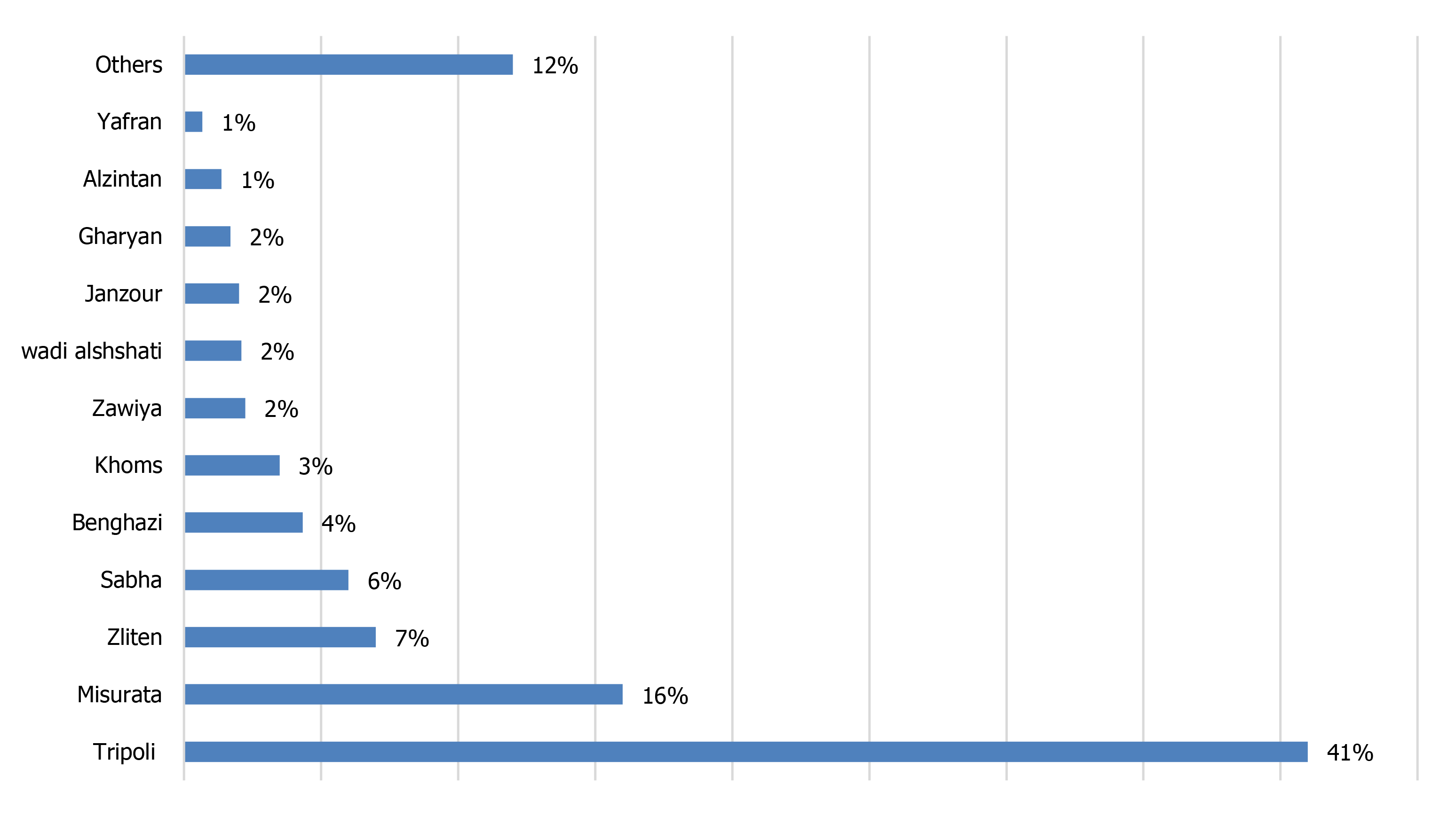
COVID-19 prevalence has been reported in many cities of the country, and this reflects the high transmission rate of the virus at the regional level (Figure 6). However, a significant difference in the prevalence rate of COVID-19 has been found between the cities. This variation might be attributable to the following factors: (1) The number of samples tested per day; (2) Population density in each city; (3) Different activities for different cities; and (4) Different cultural and social lifestyles in each city. The highest positivity rates were estimated to be 44.09%, 36.56%, 23.05%, 22.23%, 18.50% and 16.14% in the cities of Surman, Alzintan, Sabratha, Zliten, Sabha and Misrata respectively, while the lowest positivity rates were estimated to be 11.05%, 11.39%, 7.90% and 4.90% in Zawiya, Nalut, Tripoli and Benghazi respectively. The aforementioned rates in Libyan cities have not been constant and have changed every month. Indeed, the high average positivity rates in Libya from September to mid-November (21%; 23.84%) constitute another indicator of the high transmission rate among the population (Figure 5C and D). According to the WHO’s recommendation, the capacity for testing should be increased, and the positivity rate should remain below 10%. A positivity rate of less than 5% is recommended before the reopening of schools and businesses. According to the CDC, Libya, 76808 confirmed cases, 28153 active cases, 47587 recovered cases and 1068 deaths have been announced as of 19 November 2020, while the case fatality ratio (CFR) was estimated to be 1.40%; and as of 19 November 2020, Libya has a COVID-19 mortality rate of 15.90 deaths/100000 people.
The epidemiological situation of COVID-19 in Libya may be influenced by the following potential risk factors: the government’s level of transparency, prevention and control measures, population density, susceptibility of the population, age structure, etc. These factors contribute to and potentially influence the course of the disease in the country, and they might be variable in different environments.
In general, if any government has low or a complete lack of transparency, it will have a negative impact on the success of any strategy to combat or confront the pandemic. However, if the government prioritizes transparency, it would prompt trust and sentiments of solidarity and belief among the citizens. It is difficult to build up trust between the government and citizens. Therefore, all the governmental authorities must work hard in collaboration to improve their communications and make all the relevant information available. It is clear that transparency and the sharing of information among the authorities are of great importance to the success of the prevention and control strategies of COVID-19. Indeed, misleading and false information as well as a shortage of data about the epidemiological situation in the country could lead to the wrong decision by the government with regard to the implementation of strategies for the prevention and control of COVID-19.
The strategy for the prevention and control of the epidemic must be well designed and established according to the situation of the country and epidemiological patterns of the disease in the country so that it can be linked to and complemented by the data collected; therefore, this strategy reflects the real situation of the epidemic. The Libyan strategy for prevention and control of COVID-19 was performed and implemented according to the WHO recommendation criteria[21]. The Libyan Ministry of Health and CDC of Libya formulated response plans and alertness measures and issued early announcements, recommending the government authorities to prepare for combating the novel pandemic. As a result, the Libyan government designated members for the SAC of COVID-19. The Libyan SAC of COVID-19 has issued many sanctions, which include recommendations related to the strategy for combating the disease all over the country. Since the first case of COVID-19 was reported in Libya, the government authorities have followed these recommendations and have taken early action responses, as mentioned previously.
Consequently, at the beginning of the pandemic, Libyan citizens were strictly following all those recommendations related to the basic principles and precaution measures for preparedness and prevention from the infection and transmission of the virus. During the first two months following the first reported case, the number of confirmed cases were low as compared to other countries.
Currently, the epidemiological situation of COVID-19 has changed and worsened; there are many reasons for this, such as people losing their trust in the government and several people not following the health instructions. As a consequence, it was considerably difficult to implement the Libyan national strategy for the prevention and control of COVID-19.
The countries with the weakest and lowest strength of the public health system face the most challenges in the control and prevention of COVID-19. The public health system capacities play a crucial role in the control of the infection, and any weakness affects the strategy for the control and prevention of COVID-19. The Libyan authorities did not sufficiently prepare to improve their health capacities to face the pandemic. The diagnostic capacity and the tracing of contacts or suspected cases are crucial factors in combatting and minimizing the virus infection among the populations. Notwithstanding the high financial support extended by the Libyan authorities, the medical capacities are still lacking to address the minimum healthcare priorities. Most of the healthcare workers (HCWs) at the beginning of the pandemic were afraid because they did not have proper preventive measures in place; moreover, there was a deficiency in the availability of personal protective equipment (PPE). In the healthcare units, there is a shortage in the medical supplements and most of the hospitals do not provide triages or filter rooms. In fact, the challenge is that when a country faces a rise in the COVID-19 cases above their public health capacity, they will not be able to mitigate deaths from the viral spread within the community or among their HCWs. The efficiency of health services in isolation centres and hospitals is a significant factor that contributes to reducing the impact of the viral spread and improving the recovery of infected patients. The health sector, including HCWs, laboratory technicians and groups of high-risk professionals, are considered the first line of defence during the COVID-19 pandemic in all medical care units; therefore, those in the frontline during an infectious disease’s outbreak must especially be well trained. Healthcare units must meet the standard level and follow the criteria as required by the WHO and Libyan CDC to prevent the medical staff from exposure to the viral infection. Many HCWs have been infected by SARS-CoV-2 and sacrificed their lives to save their patients during the COVID-19 pandemic; according to data published on 23 July 2020 by the WHO, approximately over 10000 HCWs in Africa were infected with COVID-19. Many countries had low levels of medical service and a lack of PPE at the beginning of the pandemic. In contrast, the scenario in China has indicated that the Chinese health authorities were well prepared to combat the outbreak of any epidemic disease, having learnt from previous outbreaks such SARS 2003, HIV and human avian flu; accordingly, China was able to implement a consolidated and comprehensive blended strategy for the prevention and control of COVID-19 and also strengthen the public health capacity, which is one of the key factors for the effective combating of COVID-19. The strict quarantine measures constituted another key factor for success of the Chinese strategy. The Chinese health authorities were further able to isolate the virus and perform the genetic sequence of SARS-CoV-2 in a short time[22].
Libya is situated on the coast of North Africa, and it belongs to the Maghreb region in North Africa, bordered by the Mediterranean Sea to the north, Egypt to the east, Sudan to the southeast, Chad to the south, Niger to the southwest, Algeria to the west and Tunisia to the northwest. It is a large country with a relatively small population density of about 50 persons per km² (130/sq. mi.). 90% of the people live in less than 10% of the area, primarily along the coast. About 88% of the population is urban, mostly concentrated in the largest cities such as Tripoli (1150989), Benghazi (650629), Misrata (386120), Tarhuna (210697) and Al Khums (201943). Libya has a population of about 6.7 million, and about four people per km² (10 people/ sq. mi), calculated on a total land area of 1759540 km² (679362 sq. miles)[23,24]. The population density is one of the potential factors that increases community spread and individual risk of COVID-19. Consequently, the epidemiological patterns of COVID-19 in Libya could also be greatly influenced by the crowded situation due to the high population density; however, in contrast, most of the Libyan population live in independent department with low crowded. Therefore, the risk of exposure to SARS-CoV-2 infection among the Libyan community is limited as compared to other international societies characterized by crowded situations and of high public traffic within cities. According to the population data, it was suggested that the population density might be linked with the COVID-19 pandemic, especially in the urban areas and big cities around the world that are characterized by intense crowds, which could lead to the virus spreading within and outside those cities[25,26]. In contrast to study led by Johns Hopkins University, the study revealed that urban density is not linked to higher COVID-19 infection and death[27].
Libya is a country with a moderate level of population displacement. According to the data published by the UNHCR and the International Organization for Migration (IOM), the country had the worst displacement scenario for a period of time since 2014, with approximately 217002 people being displaced inside the country and 348372 internally displaced persons[28]. The instability of the country and the fragility of the quarantine measures in Libyan borders made it easy for refugees to travel alongside migrants through dangerous routes towards Europe. In Libya, about 43113 refugees and asylum-seekers are registered with UNHCR. However, since 2016, the IOM and Displacement Tracking Matrix identified and located 276957 migrants out of around 700000 to 1 million migrants expected to be within the country[28].
Libya is one of the self-financing participants under the COVAX facility. Total of 9.7 million US dollars has been transferred to the COVAX Facility to secure 2.8 million doses of COVID-19 vaccines. This amount of vaccine doses will be enough to vaccinate around 1.25 million people as two doses per person in addition to 10% as vaccine wastage. However, the country is hosting over 574 000 migrants and refugees who have not been included in Libya’s national vaccination plan for COVID-19. The government is revising the plan to add a component addressing those vulnerable group. Once the revised plan is endorsed, WHO will ask the Global Vaccine Alliance to consider making vaccines available for around 16200 high-risk migrants and refugees under its Humanitarian Buffer fund.
The Libyan Ministry of Health has secured enough vaccines from the COVAX Facility to immunize approximately 20% of the Libyan population. Priority will be given to frontline health care workers, adults over 60 years of age, and patients with chronic underlying health conditions in all areas of the country[29]. Online registration for COVID-19 vaccination has already started in Libya on the first of March 2021 using the following link: https://www.eservices.ly.
The Libyan NCDC is responsible for coordinating vaccination throughout the country.
The Libyan Government of National Unity has received the first shipment of 101250 doses of Sputnik V vaccines on the April 4, 2021, and the second shipment with 100000 doses of Sputnik V vaccines was received on the 9th of April.
The only vaccine that was sent to Libya through COVAX Facility was AstraZeneca vaccine on the 8th of April with a total of 57600 doses.
A shipment of a total of 150000 doses of Sinovac vaccine was received as a gift to Libya from the Turkish government on the 14th of April. The vaccination campaign has started on the 10th of April and up to the 10th of May a total of about 100000 people have been vaccinated with a single dose.
The information and data across the country regarding COVID-19 still remain unclear; consequently, the Libyan authorities need to initiate large-scale case screening, improve testing capacities and enforce contact tracing within the time frame, which are not easy tasks to perform in a country facing troubles, conflicts and instability. Currently, neither an increase in the testing capacities nor quarantine or lockdown of the cities would be a unique solution or strategy for the control and prevention of COVID-19. Advisably, the Libyan health authority should improve the public health capacities and enforce strict hygiene measures within the societies to minimize both the CFR and socio-economic impacts of the SARS-CoV-2. Most important that Ministry of health and NCDC should focus and do all possible efforts in order to get as many people vaccinated within a short period of time.
Manuscript source: Invited manuscript
Specialty type: Virology
Country/Territory of origin: Libya
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Gallo G, Khachfe H S-Editor: Gao CC L-Editor: A P-Editor: Xing YX
| 1. | Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol. 2020;92:401-402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1670] [Cited by in RCA: 1767] [Article Influence: 353.4] [Reference Citation Analysis (0)] |
| 2. | Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020;382:1199-1207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11224] [Cited by in RCA: 9308] [Article Influence: 1861.6] [Reference Citation Analysis (0)] |
| 3. | Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, Wang W, Song H, Huang B, Zhu N, Bi Y, Ma X, Zhan F, Wang L, Hu T, Zhou H, Hu Z, Zhou W, Zhao L, Chen J, Meng Y, Wang J, Lin Y, Yuan J, Xie Z, Ma J, Liu WJ, Wang D, Xu W, Holmes EC, Gao GF, Wu G, Chen W, Shi W, Tan W. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565-574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8473] [Cited by in RCA: 7582] [Article Influence: 1516.4] [Reference Citation Analysis (0)] |
| 4. | Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang RD, Liu MQ, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. Addendum: A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;588:E6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 394] [Cited by in RCA: 495] [Article Influence: 99.0] [Reference Citation Analysis (0)] |
| 5. | International Committee on Taxonomy of Viruses. Virus Taxonomy: 2019 Release. [cited 10 September 2020]. In: International Committee on Taxonomy of Viruses [Internet]. Available from: https://talk.ictvonline.org/taxonomy/. |
| 6. | Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, Hu Y, Tao ZW, Tian JH, Pei YY, Yuan ML, Zhang YL, Dai FH, Liu Y, Wang QM, Zheng JJ, Xu L, Holmes EC, Zhang YZ. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265-269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6893] [Cited by in RCA: 7472] [Article Influence: 1494.4] [Reference Citation Analysis (0)] |
| 7. | Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5:536-544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5202] [Cited by in RCA: 4620] [Article Influence: 924.0] [Reference Citation Analysis (0)] |
| 8. | Su S, Wong G, Shi W, Liu J, Lai ACK, Zhou J, Liu W, Bi Y, Gao GF. Epidemiology, Genetic Recombination, and Pathogenesis of Coronaviruses. Trends Microbiol. 2016;24:490-502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1725] [Cited by in RCA: 1871] [Article Influence: 207.9] [Reference Citation Analysis (0)] |
| 9. | World Health Organization. Archive Timeline of COVID-19. [cited 21 October 2020]. In: World Health Organization [Internet]. Available from: https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19. |
| 10. | Njenga MK, Dawa J, Nanyingi M, Gachohi J, Ngere I, Letko M, Otieno CF, Gunn BM, Osoro E. Why is There Low Morbidity and Mortality of COVID-19 in Africa? Am J Trop Med Hyg. 2020;103:564-569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 125] [Article Influence: 25.0] [Reference Citation Analysis (0)] |
| 11. | National Center for Diseases Control. COVID-19 Updates in Libya. [cited 20 November 2020]. In: National Center for Diseases Control [Internet]. Available from: https://www.covid19.ly. |
| 12. | Bi Q, Wu Y, Mei S, Ye C, Zou X, Zhang Z, Liu X, Wei L, Truelove SA, Zhang T, Gao W, Cheng C, Tang X, Wu X, Sun B, Huang S, Sun Y, Zhang J, Ma T, Lessler J, Feng T. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis. 2020;20:911-919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1284] [Cited by in RCA: 1238] [Article Influence: 247.6] [Reference Citation Analysis (0)] |
| 13. | Backer JA, Klinkenberg D, Wallinga J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20-28 January 2020. Euro Surveill. 2020;25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1082] [Cited by in RCA: 915] [Article Influence: 183.0] [Reference Citation Analysis (0)] |
| 14. | Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14869] [Cited by in RCA: 12962] [Article Influence: 2592.4] [Reference Citation Analysis (1)] |
| 15. | Rayes AA, Annajar BB, Dayhum AS, Eldaghayes IM. Why there were few cases of coronavirus disease 2019 in Libya during the first two months of the pandemic? Int J One Health. 2020;6:160-164. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. [cited 21 October 2020]. In: World Health Organization [Internet]. Available from: https://covid19.who.int/table. |
| 17. | World Health Organization. Interim guidance: Clinical Management of Severe Acute Respiratory Infection (SARI) when COVID-19 Disease is Suspected. Geneva: World Health Organization, 2020. |
| 18. | World Health Organization. Transmission of COVID-19 by asymptomatic cases. [cited 30 August 2020]. In: World Health Organization [Internet]. Available from: http://www.emro.who.int/health-topics/corona-virus/transmission-of-covid-19-by-asymptomatic-cases.html. |
| 19. | OIE. Rift Valley Fever in Libya. 2020. [cited 29 October 2020]. In: OIE [Internet]. Available from: https://www.oie.int/wahis_2/public/wahid.php/Reviewreport/Review?reportid=32934. |
| 20. | Mahmoud AS, Di Sabatino D, Danzetta ML, Iapaolo F, Tolari F, Forzan M, Mazzei M, Dayhum A, De Massis F, Monaco F. Rift Valley fever virus: a serological survey in Libyan ruminants. Open Vet J. 2018;8:204-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | World Health Organization. Country and technical Guidance – Coronavirus Disease (COVID-19). [cited 10 September 2020]. In: World Health Organization [Internet]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance-publications. |
| 22. | Zhang YZ. Initial Genome Release of Novel Coronavirus. Novel 2019 coronavirus genome - SARS-CoV-2 coronavirus. [cited 30 October 2020]. In: Virological [Internet]. Available from: https://virological.org/t/novel-2019-coronavirus-genome/319. |
| 23. | United Nations. 2019 Revision of World Population Prospect. [cited 3 July 2020]. In: United Nations [Internet]. Available from: https://population.un.org/wpp/. |
| 24. | Worldometer. 2020. Libya Demographics. [cited 25 July 2020]. In: Worldometer [Internet]. Available from: https://www.worldometers.info/demographics/Libya-demographics. |
| 25. | Wheaton WC, Thompson AK. The Geography of COVID19 growth in the US: Counties and Metropolitan Areas. SSRN. 2020;. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 26. | Carozzi F, Provenzano S, Roth S. Urban Density and COVID-19. IZA DP No. 13440. [cited 29 August 2020]. In: Institute of Labor Economics [Internet]. Available from: Available at: https://www.iza.org/publications/dp/13440/urban-density-and-covid-19. |
| 27. | Hamidi S, Sabouri S, Ewing R. Does Density Aggravate the COVID-19 Pandemic? J Am Plan Assoc. 2020;86:495-509. [DOI] [Full Text] |
| 28. | International Organization for Migration. IOM Libya Brief. 2021. [cited 29 August 2020]. In: International Organization for Migration [Internet]. Available from: https://www.iom.int/countries/Libya. |
| 29. | Health response to COVID-19 in Libya. WHO update # 23. Reporting period: 24 December 2020 to 31 January 2021. [cited 15 March 2021]. In: Health response to COVID-19 in Libya [Internet]. Available from: https://reliefweb.int/sites/reliefweb.int/files/resources/Libya_covid_update_23_final.pdf. |