Published online Feb 24, 2017. doi: 10.5500/wjt.v7.i1.88
Peer-review started: November 3, 2016
First decision: December 1, 2016
Revised: December 19, 2016
Accepted: January 11, 2017
Article in press: January 12, 2017
Published online: February 24, 2017
Processing time: 114 Days and 3.4 Hours
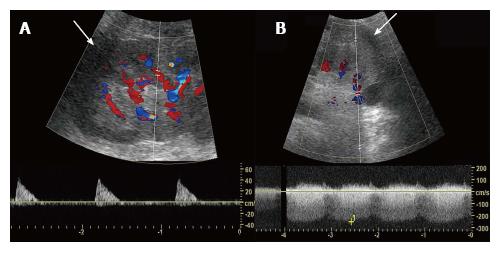
We report a rare case of allograft loss from acute Page kidney secondary to trauma that occurred 12 years after kidney transplantation. A 67-year-old Caucasian male with a past surgical history of kidney transplant presented to the emergency department at a local hospital with left lower abdominal tenderness. He recalled that his cat, which weighs 15 lbs, jumped on his abdomen 7 d prior. On physical examination, a small tender mass was noticed at the incisional site of the kidney transplant. He was producing a normal amount of urine without hematuria. His serum creatinine level was slightly elevated from his baseline. Computer tomography revealed a large subscapular hematoma around the transplant kidney. The patient was observed to have renal trauma grade II at the hospital over a period of three days, and he was finally transferred to a transplant center after his urine output significantly decreased. Doppler ultrasound demonstrated an extensive peri-allograft hypoechoic area and abnormal waveforms with absent arterial diastolic flow and a patent renal vein. Despite surgical decompression, the allograft failed to respond appropriately due to the delay in surgical intervention. This is the third reported case of allograft loss from acute Page kidney following kidney transplantation. This case reinforces that kidney care differs if the kidney is solitary or a transplant. Early recognition and aggressive treatments are mandatory, especially in a case with Doppler signs that are suggestive of compression.
Core tip: We experienced a rare case of allograft loss from acute Page kidney secondary to trauma that occurred 12 years after kidney transplantation. This case reinforces that care for a transplanted kidney differs from care of a native kidney. Early recognition and aggressive treatments are mandatory, especially when Doppler signs suggest there is compression of the transplanted kidney. To the best of our knowledge, our case is the third case of allograft loss from Page kidney following kidney transplantation.
- Citation: Takahashi K, Prashar R, Putchakayala KG, Kane WJ, Denny JE, Kim DY, Malinzak LE. Allograft loss from acute Page kidney secondary to trauma after kidney transplantation. World J Transplant 2017; 7(1): 88-93
- URL: https://www.wjgnet.com/2220-3230/full/v7/i1/88.htm
- DOI: https://dx.doi.org/10.5500/wjt.v7.i1.88
The Page kidney (PK) phenomenon occurs with compression of the kidney by a hematoma or mass, leading to arterial hypertension[1]. More than 100 cases have been described in the literature[2-4]; however, no systematic review has focused on post-transplant PK. In this case, report, we describe a rare case of allograft loss from PK secondary to trauma that occurred 12 years after kidney transplantation. This is the third reported case of allograft loss from PK following kidney transplantation[5,6]. We describe this case alongside a review of the literature.
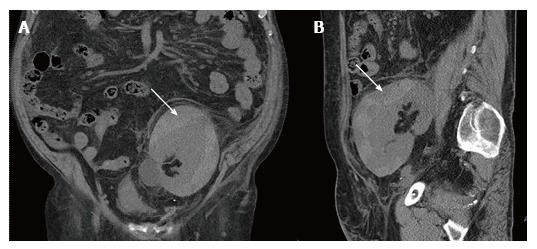
A 67-year-old Caucasian male presented to the emergency department at a local hospital for left lower abdominal tenderness. The patient had undergone a living unrelated kidney transplant into his left iliac fossa 12 years prior due to chronic glomerulonephritis. His stable immunosuppression regimen included tacrolimus (1 mg every 12 h), mycophenolate mofetil (500 mg every 12 h), and prednisone (5 mg daily). Except for one episode of acute cellar rejection a month after kidney transplantation, he had been doing well with a baseline serum creatinine level of 2.0 mg/dL. On arrival, his body temperature was 36.6 °C, blood pressure was 163/54 mmHg, and pulse was 61 beats/min. He reported that he had been active until the day before without noticing any injuries, but he recalled his cat, weighing 15 lbs, jumped on his abdomen seven days prior. On physical examination, his abdomen was soft and flat without rebound or guarding, except for a small tender mass noticed at the incisional site of the kidney transplant. His hemoglobin was 7.1 g/dL. His serum creatinine level was elevated from his baseline to 2.5 mg/dL. He was producing a normal amount of urine without hematuria. Computed tomography (CT) without intravenous contrast revealed a 12 cm × 2.5 cm subcapsular hematoma around the transplanted kidney (Figure 1). Urology was consulted, and the decision was made to conservatively observe the patient, as he met criteria of a renal trauma grade II according to the renal trauma grading system by the American Association for the Surgery of Trauma.
On admission, the patient received a red blood cell transfusion and was started on labetalol for hypertension. His systolic blood pressure was controlled within a range of 110-140. Within three days, his serum creatinine level increased to 5.4 mg/dL and his urine output decreased. His blood pressure was elevated up to 156/80 mmHg. The patient was transferred to a transplant center for further treatment.
At the transplant center, Doppler ultrasound (US) demonstrated an extensive peri-allograft hypoechoic area, abnormal arterial waveforms with absent diastolic flow in the arcuate arteries and a patent renal vein (Figure 2). He underwent emergent laparotomy for hematoma decompression. A substantial portion of the hematoma was evacuated by capsulotomy. Concurrent kidney biopsy showed no evidence of rejection. His postoperative course was uncomplicated and uneventful. The patient resumed tacrolimus, mycophenolate mofetil, and prednisone. However, his kidney function continued to deteriorate and he became dependent on hemodialysis. He is currently maintained with mycophenolate mofetil monotherapy and is awaiting a second kidney transplant.
PK was first described by Irvine Page in 1939, when he wrapped animal kidneys with cellophane and observed the development of acute hypertension[1]. The typical presentation of PK is distinguished by the presence of acute renal dysfunction in conjunction with hypertension. Trauma, spontaneous hemorrhage in patients with predisposing factors (anticoagulation), bleeding after interventions (surgery, biopsy, nephrostomy, and lithotripsy), tumors, renal cysts, urinoma, and lymphocele have been proposed as etiological factors[1-4]. Hypoperfusion and microvascular ischemia in the kidney are considered to stimulate the renin-angiotensin-aldosterone system and cause hypertension[1]. If the involved kidney is solitary, or if the contralateral organ is damaged, renal failure may ensue. There are a variety of treatment options, including conservative management as the hematoma is absorbed[7]; surgical decompression by capsulotomy as part of a laparoscopic intervention[8]; and, in extreme cases, nephrectomy[9,10]. Improvement of renal function after evacuation of the hematoma, in the absence of rejection or ureteral obstruction, confirms the diagnosis. In our case, CT demonstrated a large subcapsular hematoma compressing the parenchyma with a significant Doppler US finding of “absent arterial diastolic flow with patent renal vein”. Furthermore, a kidney biopsy failed to demonstrate evidence of rejection, which further supported the diagnosis of PK.
PK after kidney transplantation was first described in 1976 as “pseudorejection” by Cromie et al[11]. This was because PK causes acute deterioration of graft function, which resembles rejection. Since then, 30 cases of post-transplant PK have been reported in the literature (Table 1)[4-6,10-31]. The most common causes are iatrogenic (kidney biopsy in 18 cases, renal artery stenting in 1 case, ureteral stenting in 1 case, and nephrostomy in 1 case); trauma (3 cases)[5,6]; spontaneous (2 cases)[15,27]; and postoperative bleeding (2 cases)[11,12]. Surgical decompression with capsulotomy and evacuation of hematoma have been performed in most cases (25 cases), and interventional radiographic drainage was performed in 1 case[14], while 3 cases were conservatively observed with complete improvement of kidney function[19,26]. The diagnosis is most commonly made by Doppler US findings of “absent arterial diastolic flow, reversible arterial diastolic flow, or significant increase of arterial resistive index, with a large peri-allograft hypoechoic area,” suggesting extrinsic compression of renal parenchyma and subsequent cortical ischemia. In most cases, these findings have prompted surgical or radiographic intervention. On the other hand, allograft losses have been reported in 2 cases[10,21]. One allograft was saved with a surgical intervention performed 2 d after the onset[11], while one allograft was lost despite immediate intervention[21]. In our case, the patient was observed at a local hospital and noted to have renal trauma grade II; the patient did not undergo Doppler US evaluation for the first three days of hospitalization. He was finally transferred to a transplant center after his urine output significantly decreased. His graft loss may have been preventable if he had been evaluated with Doppler US upon presentation to the local hospital as well as if timely surgical intervention or transfer to a transplant center had been requested earlier. This case reinforces that care of the kidney differs if the kidney is solitary or a transplant. Early recognition of PK and aggressive treatments are mandatory, especially when Doppler findings suggest compression of a solitary or transplanted kidney.
| Year | Ref. | Age/sex | Onset after transplant | Cause | Modality for diagnosis | Positive US sign1 | Type of intervention | Intervention time after onset | Result |
| 2016 | Takahashi | 67/M | 12 yr | Trauma | US/CT | Yes | Surgical decompression | 3 d | AL |
| 2015 | Sedigh et al[6] | 67/M | 12 yr | Trauma | US | Yes | Surgical decompression | 12 h | CR |
| 2015 | Ay et al[12] | 50/M | 1 d | Postoperative bleeding | US | Yes | Surgical decompression | Immediately | CR |
| 2014 | Adjei-Gyamfi et al[13] | 12/M | 7 wk | Txp kidney biopsy | US/CT | No | Surgical decompression | Immediately | CR |
| 2014 | Adjei-Gyamfi et al[13] | 18/F | 1 yr | Txp kidney biopsy | US | No | Surgical decompression | Immediately | CR |
| 2013 | Hamidian Jahromi et al[14] | 19/M | 5 wk | Txp renal arterial stenting | US/Angio | Yes | IR drainage | 6 h | CR |
| 2012 | Gandhi et al[15] | 46/M | 17 yr | Spontaneous | US | Yes | Surgical decompression | Immediately | CR |
| 2011 | Maurya et al[16] | 30/M | 7 d | Txp kidney biopsy | US/CT | Unknown | Surgical decompression | Immediately | CR |
| 2011 | Okecgukwu et al[17] | 32/M | 8 d | Txp ureter stenting | US | Unknown | Surgical decompression | Immediately | CR |
| 2010 | Butt et al[4] | 61/F | 24 d | Spontaneous | CT | - | Surgical decompression | Immediately | CR |
| 2010 | Posadas et al[18] | 55/M | 3 mo | Txp kidney biopsy | US | Yes | Surgical decompression | Immediately | CR |
| 2009 | Kamar et al[19] | 47/M | 1 yr | Txp kidney biopsy | US | Yes | Observation | - | CR |
| 2009 | Kamar et al[19] | 59/M | 1 yr | Txp kidney biopsy | US | Yes | Observation | - | CR |
| 2009 | Caldés et al[20] | 60/M | 1 mo | Percutaneous nephrostomy | US | Yes | Surgical decompression | 24 h | CR |
| 2008 | Chung et al[21] | 27/F | 11 d | Txp kidney biopsy | US/CT | Yes | Surgical decompression | Immediately | CR |
| 2008 | Chung et al[21] | 39/F | Several days | Txp kidney biopsy | US | Yes | Surgical decompression | Immediately | CR |
| 2008 | Chung et al[21] | 35/M | 4 d | Txp kidney biopsy | US/CT | Unknown | Surgical decompression | Immediately | AL |
| 2008 | Chung et al[21] | 33/F | 9 mo | Txp kidney biopsy | US | Yes | Surgical decompression | Immediately | CR |
| 2008 | Heffernan et al[22] | 64/M | 4 mo | Txp kidney biopsy | US | Yes | Surgical decompression | Immediately | CR |
| 2007 | Patel et al[23] | 69/M | 7 yr | Txp kidney biopsy | US/CT | Unknown | Surgical decompression | Immediately | CR |
| 2005 | Gibney et al[24] | 32/M | 1 yr | Txp kidney biopsy | US/Angio | Unknown | Surgical decompression | Immediately | CR |
| 2000 | Rea et al[25] | 34/M | 3 yr | Txp kidney biopsy | US | Yes | Surgical decompression | Immediately | CR |
| 1996 | Machida et al[26] | 32/M | 4 mo | Txp kidney biopsy | CT/Scinti | - | Observation | - | PR |
| 1996 | Goyal et al[5] | 41/M | 12 yr | Trauma | CT/MRI/Scinti | - | Unknown | Unknown | Unknown |
| 1994 | Nguyen et al[27] | 26/M | 12 h | Spontaneous | Scinti | - | Surgical decompression | Immediately | CR |
| 1993 | Dempsey et al[28] | 19/F | 2 yr | Txp kidney biopsy | US | Yes | Surgical decompression | Immediately | CR |
| 1993 | Ben Hamida et al[29] | 32/M | 7 mo | Heparin after renal vein thrombosis | US | Yes | Observation | - | CR |
| 1991 | Kliewer et al[10] | 56/F | 2 wk | Txp kidney biopsy | US | Yes | Nephrectomy | Unknown | AL |
| 1988 | Figueroa et al[30] | 40/F | 11 mo | Txp kidney biopsy | CT/Angio | - | Surgical decompression | 30 h | CR |
| 1988 | Yussim et al[31] | 40/F | 5 mo | Postoperative lymphocele | US | Unknown | Surgical decompression | Unknown | CR |
| 1976 | Cromie et al[11] | 35/M | 10 d | Postoperative bleeding | US | Unknown | Surgical decompression | 2 d | CR |
We recommend the following care for acute PK. Patients without pre-existing kidney disease who have unilateral PK need to be admitted for monitoring of vitals, including blood pressure, heart rate, urine output, serum creatinine levels and hemoglobin levels. Abdominal/pelvic CT scan is preferable for accurate initial staging and diagnosis of the etiology of PK. Ongoing hemorrhage in a stable patient can be controlled by embolization with interventional radiology. After the initial diagnosis has been made, follow-up with US is appropriate. An initial attempt should be made to stabilize hypertension with antihypertensive medication. Conservative management and evaluation of the etiology are recommended as part of first-line treatment. Unstable patients might be more appropriate for surgery.
In the case of transplant patients, patients with a single kidney, and patients with bilateral PK, the patient should be transferred to a transplant center or a center capable of caring for the patient with acute PK and the underlying etiology. Vitals, including the blood pressure, heart rate and urine output, serum creatinine level and hemoglobin levels, should be carefully monitored. In addition to CT scanning for staging and diagnosis, Doppler US should be performed to evaluate parenchymal compression. Hypertension should be managed using antihypertensive medication and strict fluid balance. If the patient has an elevated serum creatinine level or a decrease in urine output as well as positive Doppler signs, prompt surgical intervention should be considered.
We experienced a rare case of allograft loss from acute PK secondary to trauma after kidney transplantation. The care of PK in a transplant kidney differs from PK in the native kidney. Early recognition and aggressive treatments are mandatory, especially in a case with positive Doppler signs.
A 67-year-old male with a past surgical history of kidney transplantation (12 years prior) presented to the emergency department for left lower abdominal tenderness after a cat jumped on his abdomen (seven days prior).
The abdomen was soft and flat without rebound or guarding, except for a small tender mass noted at the incision site of the kidney transplant.
Lymphocele, urinoma, seroma, hematoma, renal cell cancer, renal cyst.
On initial presentation, all labs were normal except for a hemoglobin of 7.1 g/dL and serum creatinine level of 2.5 mg/dL.
Computed tomography without intravenous contrast revealed a 12 cm × 2.5 cm subcapsular hematoma around the transplanted kidney.
The transplant kidney biopsy showed no evidence of rejection.
Emergent laparotomy for decompression of the hematoma.
A renal trauma grade II is usually observed according to the renal trauma grading system of the American Association for the Surgery of Trauma.
The Page kidney phenomenon occurs from kidney compression by a hematoma or a mass, leading to arterial hypertension. If the involved kidney is solitary, or the contralateral organ is damaged, renal failure may ensue.
This case reinforces that kidney care differs if the kidney is solitary or transplanted. Early recognition and aggressive treatments are mandatory, especially in a case with Doppler signs suggestive of compression.
The topic is very interesting. The authors presented their experience with Page kidney phenomenon after kidney transplantation. It is relatively unfrequent complication but with possible serious complications on graft.
Manuscript source: Unsolicited manuscript
Specialty type: Transplantation
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Markic D, Niu CY, Salvadori M, Scharman EJ S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Haydar A, Bakri RS, Prime M, Goldsmith DJ. Page kidney--a review of the literature. J Nephrol. 2003;16:329-333. [PubMed] |
| 2. | Aragona F, Artibani W, Calabrò A, Villi G, Cisternino A, Ostardo E. Page kidney: a curable form of arterial hypertension. Case report and review of the literature. Urol Int. 1991;46:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Dopson SJ, Jayakumar S, Velez JC. Page kidney as a rare cause of hypertension: case report and review of the literature. Am J Kidney Dis. 2009;54:334-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 4. | Butt FK, Seawright AH, Kokko KE, Hawxby AM. An unusual presentation of a Page kidney 24 days after transplantation: case report. Transplant Proc. 2010;42:4291-4294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Goyal M, Zukerberg B, Ozgen P, Graves M, Scheff A. Large subcapsular hematoma in transplant kidney seen on renal scan. Clin Nucl Med. 1996;21:345-346. [PubMed] |
| 6. | Sedigh O, Lasaponara F, Dalmasso E, Gai M, Hayashi Y, Bosio A, Pasquale G, Lillaz B, Biancone L, Frea B. Subcapsular Hematoma Causing Anuria After Renal Graft Trauma. Exp Clin Transplant. 2015; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Salgado OJ, Vidal AM, Semprun P, Garcia R. Conservative management of an extensive renal graft subcapsular hematoma arising during living donor nephrectomy. Role of Doppler sonographic posttransplant follow-up. J Clin Ultrasound. 2010;38:164-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Çiftçi S, Stuart Wolf J. Laparoscopic treatment of Page kidney: a report of two cases and review of the literature. Turk J Urol. 2013;39:126-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Sterns RH, Rabinowitz R, Segal AJ, Spitzer RM. ‘Page kidney’. Hypertension caused by chronic subcapsular hematoma. Arch Intern Med. 1985;145:169-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Kliewer MA, Carroll BA. Ultrasound case of the day. Page kidney phenomenon in a transplanted kidney after biopsy. Radiographics. 1991;11:336-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Cromie WJ, Jordan MH, Leapman SB. Pseudorejection: the Page kidney phenomenon in renal allografts. J Urol. 1976;116:658-659. [PubMed] |
| 12. | Ay N, Beyazıt Ü, Alp V, Duymus R, Sevük U, Anıl M, Danış R. Rupture of a Subcapsular Hematoma After Kidney Transplant: Case Report. Exp Clin Transplant. 2015; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Adjei-Gyamfi Y, Koffman G, Amies T, Easty M, Marks SD, McHugh K. Reversible acute anuric kidney injury after surgical evacuation of perinephric hematomas as a complication of renal transplant biopsies. Pediatr Transplant. 2014;18:E262-E265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Hamidian Jahromi A, Fronek J, Kessaris N, Bydawell G, Patel U, MacPhee IA. Acute page kidney complicating kidney transplant artery stenting: presentation of a case and novel management. Iran J Kidney Dis. 2013;7:352-355. [PubMed] |
| 15. | Gandhi V, Khosravi M, Burns A. Page kidney in a 17-year-old renal allograft. BMJ Case Rep. 2012;2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Maurya KK, Bhat HS, Mathew G, Kumar G. Page kidney following renal allograft biopsy - early recognition and treatment. Saudi J Kidney Dis Transpl. 2011;22:1012-1013. [PubMed] |
| 17. | Okechukwu O, Reddy S, Guleria S. A page in transplantation. Saudi J Kidney Dis Transpl. 2011;22:796-798. [PubMed] |
| 18. | Posadas MA, Yang V, Ho B, Omer M, Batlle D. Acute renal failure and severe hypertension from a page kidney post-transplant biopsy. ScientificWorldJournal. 2010;10:1539-1542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Kamar N, Sallusto F, Rostaing L. Acute Page kidney after a kidney allograft biopsy: successful outcome from observation and medical treatment. Transplantation. 2009;87:453-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Caldés S, Fernández A, Rivera M, Merino JL, González R, Amezquita Y, Marcén R, Burgos FJ, Ortuño J. A Page kidney case report with diastolic flow reversion in Doppler ultrasonography. Transplantation. 2009;87:303-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Chung J, Caumartin Y, Warren J, Luke PP. Acute Page kidney following renal allograft biopsy: a complication requiring early recognition and treatment. Am J Transplant. 2008;8:1323-1328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 22. | Heffernan E, Zwirewich C, Harris A, Nguan C. Page kidney after renal allograft biopsy: sonographic findings. J Clin Ultrasound. 2009;37:226-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 23. | Patel TV, Goes N. Page kidney. Kidney Int. 2007;72:1562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Gibney EM, Edelstein CL, Wiseman AC, Bak T. Page kidney causing reversible acute renal failure: an unusual complication of transplant biopsy. Transplantation. 2005;80:285-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Rea R, Anderson K, Mitchell D, Harper S, Williams T. Subcapsular haematoma: a cause of post biopsy oliguria in renal allografts. Nephrol Dial Transplant. 2000;15:1104-1105. [PubMed] [DOI] [Full Text] |
| 26. | Machida J, Kitani K, Inadome A, Wada Y, Kawabata K, Yoshida M, Ueda S. Subcapsular hematoma and hypertension following percutaneous needle biopsy of a transplanted kidney. Int J Urol. 1996;3:228-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 27. | Nguyen BD, Nghiem DD, Adatepe MH. Page kidney phenomenon in allograft transplant. Clin Nucl Med. 1994;19:361-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Dempsey J, Gavant ML, Cowles SJ, Gaber AO. Acute Page kidney phenomenon: a cause of reversible renal allograft failure. South Med J. 1993;86:574-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 29. | Ben Hamida F, Westeel PF, Achard JM, Filloux V, Tribout B, Bouzernidj M, Petit J, Fournier A. Favorable outcome under simple heparin therapy of recurrent anuria due to graft renal vein thrombosis and subcapsular hematoma. Transplant Proc. 1993;25:2341-2342. [PubMed] |
| 30. | Figueroa TE, Frentz GD. Anuria secondary to percutaneous needle biopsy of a transplant kidney: a case report. J Urol. 1988;140:355-356. [PubMed] |
| 31. | Yussim A, Shmuely D, Levy J, Servadio C, Shapira Z. Page kidney phenomenon in kidney allograft following peritransplant lymphocele. Urology. 1988;31:512-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |