Published online Dec 24, 2016. doi: 10.5500/wjt.v6.i4.736
Peer-review started: June 27, 2016
First decision: August 11, 2016
Revised: September 13, 2016
Accepted: October 25, 2016
Article in press: October 27, 2016
Published online: December 24, 2016
Processing time: 173 Days and 19.3 Hours
To identify the risk factors and the post-transplant psychological symptoms that affect adherence to therapy in a population of kidney transplant recipients.
The study examined the psychological variables likely responsible for the non-adherent behavior using a psychological-psychiatric assessment, evaluation of the perception of patients’ health status, and an interview regarding the anti-rejection drug therapy assumption. The study included 74 kidney transplant recipients.
Individuals with a higher level of education and more years since transplantation showed better mental balance. Regarding gender, women appeared to be less adherent to therapy. Further, the years since transplantation adversely affected the proper pharmacological assumption. Adherence to therapy did not significantly change with the mental health index.
The biopsychosocial illness model provides a conceptual frame of reference in which biological, psychological, and social aspects take on the same importance in the adherence to treatment protocols. For effective management, it is necessary to understand the patients’ personal experiences, their assumptions about the disease, health status perception, and mood, and to identify any “barriers” that could cause them to become noncompliant.
Core tip: Therapeutic Adherence after transplantation is of fundamental importance for the patient’s short- and long-term well-being and assumes a set of adaptations to a new lifestyle. The authors in this study analyzed the psychological characteristics of a sample of transplant recipients and different temperament styles, yet not studied in other research on transplantation. The results suggested that different temperaments influence in different ways the treatment compliance and showed that the transplant experience change behaviors and quality of life based on the personality and temperament characteristics. In conclusion, post-transplant psychological support positively affects adherence to treatment, and coping strategies of the subject.
- Citation: De Pasquale C, Veroux M, Fornaro M, Sinagra N, Basile G, Gozzo C, Santini R, Costa A, Pistorio ML. Psychological perspective of medication adherence in transplantation. World J Transplant 2016; 6(4): 736-742
- URL: https://www.wjgnet.com/2220-3230/full/v6/i4/736.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i4.736
The theme of therapeutic adherence (TA) plays a central role in research on education and health promotion[1]. Adherence to immunosuppressive therapy after transplantation is of fundamental importance for the patients’ well-being both short- and long-term and assumes a set of adaptations to a new lifestyle. The treatment effectiveness and transplant success not only depend on the correct choice of immunosuppressive drugs, but also on the patients’ active participation in the therapeutic program that often includes psychological support and appropriate motivation[2,3].
Non-adherence to therapy in transplant patients is one of the emerging causes of early and late graft loss. Patients with an organ transplant must take immunosuppressive drugs daily for the prevention of acute and chronic rejection. There is an obvious relationship between the discontinuity in the use of immunosuppressive drugs and the incidence of transplant failures in the medium and long term[4]. Non-adherence to the transplant medication regimen can lead to graft rejection, post-transplant mortality, increase in healthcare costs, and decrease in quality of life[5,6]. One meta-analysis found non-adherence to medication across all organ transplants to be 22.6%[7]. An estimated 50% of late acute rejections and 15% of graft losses are associated with non-adherence[8]. An essential aspect to ensure full adherence to the treatment is the assessment of transplant recipient needs and his/her expectations while establishing a good therapeutic alliance[9]. Many studies evaluating the relationship between the healthcare team and the patient highlighted the need for a relationship based on trust and clarity for the sharing of information regarding the treatment course[10,11]. Even psychological and psychosocial aspects can alter the response to treatment[12,13]: Mood disorders, high levels of anxiety, hostility, and the presence of “unstable” personality traits are associated with an increased risk of non-adherence to medical prescriptions in kidney transplant recipients[14-16].
Adherence to therapy thus is a complex variable and influenced by many factors: Socio-demographics, psychological characteristics, transplant recipient self-efficacy, factors related to immunosuppressive therapy, and the doctor-patient relationship. The aim of this study is to identify the risk factors and post-transplant psychological symptoms that affect adherence to therapy in a population of kidney transplant recipients.
The study examined the psychological variables that are likely responsible for the non-adherent behavior using a psychological-psychiatric assessment, evaluation of the perception of patients’ health status, and an interview regarding the anti-rejection drug therapy assumption. The psychological-psychiatric assessment involved the use of the following tests:
The Symptom Checklist-90-Revised (SCL-90-R) evaluated psychological symptoms. It is a relatively brief self-report psychometric instrument (questionnaire) published by the Clinical Assessment division of the Pearson Assessment and Information group. It is one of the most widely used measures of psychological distress in clinical practice and research and is designed to evaluate a broad range of psychological problems and symptoms of psychopathology. According to the overview given by the publisher, the SCL-90-R is normed on individuals 13 years and older. It consists of 90 items and takes 12-15 min to administer. The following primary symptom dimensions are assessed: Somatization (SOM), obsessive-compulsive (OBS), interpersonal sensitivity (INT), depression (DEP), anxiety (ANX), hostility (HOS), phobic anxiety (PHOB), paranoid ideation (PAR), psychoticism (PSY), and a category of “additional items” that helps clinicians assess other aspects of the patient’s
symptoms[17,18]. A large number of studies have been conducted demonstrating the reliability, validity, and utility of the instrument[19-22].
Personality study has provided an analysis of the temperament variables by the TEMPS-A (Temperament Evaluation of Memphis, Pisa and San Diego Autoquestionnaire). The features of temperament as well as its intensity may exert a constructive or destructive impact on the quality of life[23]. The TEMPS-A contains 110 items (109 in the version for males) measuring affective temperament traits occurring throughout life of the subject, as represented by five dimensions: Depressive (DT), cyclothymic (CT), hyperthymic (HT), irritable (IT), and anxious (AT). Questions about the various types are grouped together. The TEMPS-A measures the severity of the temperament traits ranging from 0 to 1. The calculation of points for each temperament is done by dividing the sum of points obtained in a given subscale by the number of questions contained therein[24,25].
Quality of life was examined with the Short Form Health Survey (SF-36) that assesses the degree of self-perceived psychological well-being. The SF-36 consists of eight subscales: Vitality, physical functioning, bodily pain, general health perceptions, physical role functioning, emotional role functioning, social role functioning, and mental health. Subscales are presented as scores between 0 and 100; a lower score indicates more disability and a higher score less disability. The two considered variables in this study were the physical index score (PIS) and mental index score (MIS). The validity and reliability of the SF-36 has been confirmed in patients with renal disease[26,27].
Therapeutic adherence was studied through the Basel Assessment of Adherence to Immunosuppressive Medication instrument (BAASIS), which was developed to assess adherence to immunosuppressive medication in adult transplant patients. The instrument measures patients’ taking, skipping, timing (± 2 h from the prescribed time, TM), and dose reduction of drugs. The recall period is limited to four weeks. The BAASIS comprises four questions with a 6-point scale for responses ranging from never (0) to every day (5). In addition, the BAASIS has a visual analogue scale (VAS) ranging from 0% (medication never taken as prescribed) to 100% (medication always taken as prescribed)[28,29].
The current study included 74 kidney transplant recipients (32 females, 43.25%), with a mean age of 48.3 ± 13.6 years (range 22-75). Demographic data regarding years since transplant procedure (first transplantation), occupation, level of education are presented in Table 1. All patients underwent a standardized immunosuppressive protocol with tacrolimus, mycophenolate mofetil, and steroids. The basic psychological-psychiatric assessment excluded the presence of lifetime psychiatric disorders (axis I) according to the Diagnostic and Statistical Manual for Mental Disorders (5th ed., DSM-5) or concomitant use of drugs that could influence cognitive and emotional aspects[30]. All patients provided written informed consent after the procedures were fully explained by a trained physician (MD, psychiatrist) or a psychologist.
| Years since transplantation procedure, mean ± SD (range) | 5.39 ± 3.74 (1.00-14.00) |
| Education | |
| Basic | 36% |
| High school | 56% |
| University | 8% |
| Occupation | |
| Employed | 31.17% |
| Unemployed | 56.82% |
| Retired | 12.01% |
The data were examined for normality and transformed if necessary. Pearson’s R correlation test was performed using the “Statistical Package for Social Sciences” (SPSS, Version 17). The P value of less than 0.05 (P < 0.05) was considered statistically significant. In addition, we applied multivariate linear regression analysis to predict the outcome variable (BAASIS total score, BT) from predictor variables (patterns of personality and demographic characteristics).
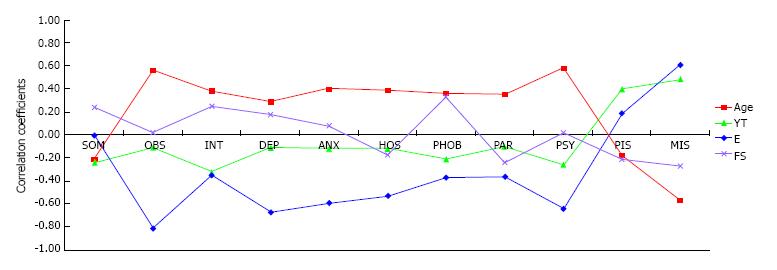
The current study included 74 kidney transplant recipients (32 females, 43.25%), with a mean age of 48.3 ± 13.6 years (range 22-75). Demographic data regarding years since transplant procedure (first transplantation), occupation, level of education are presented in Table 1. All patients underwent a standardized immunosuppressive protocol with tacrolimus, mycophenolate mofetil, and steroids. Correlations by the Pearson coefficient between results of the SCL-90-R, SF-36 (physical and mental index score), and demographic characteristics of the sample are shown in Figure 1. Individuals with a higher level of education (E) and with more years of transplantation (YT) showed higher mental balance (E/MIS r = 0.61; YT/MIS r = 0.48). Specifically, the level of education was negatively correlated with anxious, obsessive-compulsive, and depression aspects (E/OBS r = -0.81; E/DEP r = -0.67; E/ANX r = -0.59).
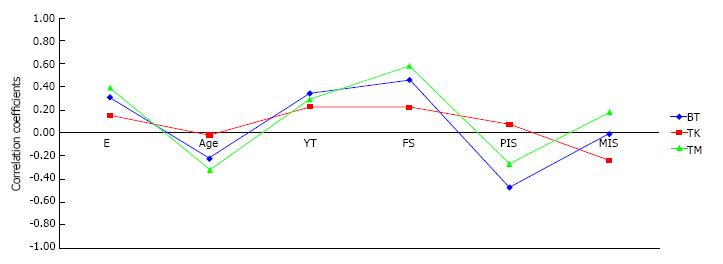
Correlations by the Pearson coefficient between results of the BAASIS, SF-36 (physical and mental index score), and demographic characteristics of the sample are shown in Figure 2. Regarding gender, women (female sex, FS) appeared to be less adherent to therapy in our study (FS/BT r = 0.46), while years of transplantation adversely affected the proper pharmacological assumption (YT/BT r = 0.34). In addition, as the index of subjective physical well-being increases, compliant behavior increases as well (PIS/BT r = -0.47), especially with regards to the treatment assumption of correct timing (PIS/TM r = -0.27). Adherence to therapy was not significantly correlated with the mental health index (MIS/BT r = -0.01).
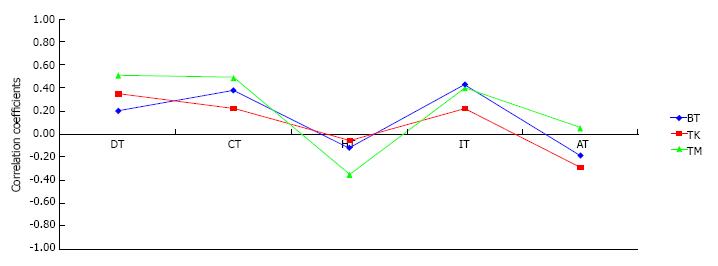
Correlations by the Pearson coefficient between the results of the TEMPS-A, BAASIS of the sample are shown in Figure 3. The temperament variables measured with the TEMPS-A were correlated with treatment adherence. Specifically, the cyclothymic, irritable, and depression personality adversely affected adherent behavior (BT/CT r = 0.39; BT/IT r = 0.44; BT/DT r = 0.21); however, a moderate positive correlation was found between the timing scale of the BAASIS and depressive temperament variable (TM/DT r = 0.52), suggesting time management difficulties for patients with a depressive personality.
Multivariate linear regression analysis showed high associations between predictor variables (sex and years since transplant procedure, cyclothymic temperament, and anxious temperament) and outcome variable (BAA SIS total score), whereas no consistent associations between other predictor variables (age, irritable temperament, IT) and outcome variable (BAASIS total score) were detected (Tables 2 and 3).
| B | SE B (SE) | β | P | |
| Constant | -0.98 (-3.44 to 1.47) | 1.13 | 0.00 | 0.39 |
| Sex | 1.53 (0.33 to 2.74) | 0.55 | 0.75 | 0.01 |
| Age | 0.01 (-0.03 to 0.05) | 0.02 | 0.14 | 0.58 |
| YT | 0.15 (0.03 to 0.27) | 0.06 | 0.58 | 0.01 |
| B | SE B (SE) | β | P | |
| Constant | 0.87 (-0.14 to 1.88) | 0.39 | 0.00 | 0.06 |
| CT | 0.51 (0.10 to 0.93) | 0.16 | 1.92 | 0.02 |
| IT | -0.17 (-0.58 to 0.23) | 0.16 | -0.48 | 0.32 |
| AT | -0.28 (-0.46 to -0.09) | 0.07 | -1.44 | 0.01 |
Similar studies on the subject have revealed significant psychological and behavioral differences between adherent and non-adherent transplanted patients, differences that express a greater vulnerability of the latter and which lead to consider that, next to drug therapy, psychological therapy is required[5,31]. Still not considered in other studies on the transplant topic is the temperament. “Temperament has been contemporarily defined as a biologically determined, hereditary core of the personality, being stable and relatively unchangeable throughout life, which determines the basic level of reactivity, mood and energy of given individual”[24].
Based on these assumptions, this study has allowed us to analyze different temperament styles and suggested that different temperaments can influence in different ways the treatment compliance and quality of life of transplant recipients.
In this study, the biopsychosocial illness model (BIM) provided a conceptual frame of reference within which biological, psychological, and social aspects took on the same importance in explaining the adherence to treatment protocols[32]. For good treatment management, it is necessary to understand the patients’ personal experiences, their beliefs about the disease, health status perception, and mood, and to identify any “barriers” that could make them noncompliant. The analysis of the variables that are responsible for the behavior of not adhering to the treatment regimen should provide suggestions for psychological support and psychiatric treatment. Treatment adherence towards the prescribed medication is critical for the safe and successful delivery of efficacious interventions, especially for complex tasks such as the management of transplant patients[33,34].
The study revealed that years of transplantation positively affected mental health, but on the other hand, adversely affected therapeutic adherence, while the level of education was positively correlated with good mental balance. Studies examining the non-pharmacological risk factors that influence therapeutic adherence thus need further confirmation[5,35]. Another finding that requires careful reflection concerns the long-term negative impact that the cyclothymic and anxious personalities could have on adherent behavior, while the presence of post-transplant psychological symptoms (mental health index) did not affect treatment adherence[36-39]. This finding could be related to the notion that while people with mental problems feel the need to be cared for and are more willing to properly follow the treatment protocol, patients with mood swings (cyclothymic temperament) and those in an alert and apprehensive state (anxious temperament) are not prepared to calmly accept the rigorous therapeutic protocol and require constant attention by healthcare staff[40]. Thus, the quality of care is not just about the correct prescription but also about the patients’ active participation through an assessment of their expectations and preferences. Patients adopt adherent behavior when they accept the type of care in terms of the therapeutic project[41]. Helpful in this regard is cognitive behavioral therapy aimed at increasing transplant recipients’ awareness[42].
Immediately after transplant, patients must be assisted to increase the capacity for self-efficacy and resilience necessary to achieve the correct lifestyle for maintaining the graft. In a next step, it would be desirable to establish a cognitive and psychosocial rehabilitation plan to improve coping strategies and strengthen the patients’ resources in order to positively influence the final outcome of the transplant process. These efforts therefore must operate simultaneously at several levels on the basis of an integrated strategy that organizes and coordinates the various types of treatment-medication, psychotherapy, assistance-and the operators’ different functions, in an intervention program formulated on the basis of the characteristics and needs of each individual patient[43,44].
The authors would thank Professor Sabina De Geest for providing the BAASIS questionnaire used in this research.
Adherence to immunosuppressive therapy after transplantation is of fundamental importance for the patients’ well-being both short- and long-term and assumes a set of adaptations to a new lifestyle. I pazienti trapiantati devono assumere quotidianamente farmaci immunosoppressori per la prevenzione del rigetto acuto e cronico (infezioni, complicanze secondarie). The treatment effectiveness and transplant success not only depend on the correct choice of immunosuppressive drugs, but also on the patients’ active participation in the therapeutic program that often includes psychological support and appropriate motivation. Adequate adherence to doctor’s orders is a resource for both patients and the health care system and society, as it reduces the costs for therapies, for minor complications associated with the disease, the health care interventions, morbidity and mortality. However various social, cultural, financial and psychological aspects affect adherence to immunosuppressive therapy.
Although most research has focused on adherence to drug treatment, the concept of adherence must include other behaviors related to health protection involving the doctor-patient relationship, the service delivery system and change their living habits. The communication characteristics of the doctor, the kind of language used and the setting are essential to strengthen the motivation and awareness of the need for a cure. Future programs should provide the ability to support the transplanted in transplant experience, helping him to properly follow treatment, help him to learn cognitive and behavioral strategies of self-regulation.
Studies of the Italian population have revealed significant differences in psychological and personality traits among transplant patients adherent and non-adherent to therapy, differences that express a greater vulnerability of the latter and which lead to consider that, next to drug therapy, you are required psychological therapy. This study also allows to analyze different temperament styles, yet not studied in other research on transplantation and suggests that different temperaments influence in different ways the treatment compliance.
The data in this study suggested that psychological and psycho-educational support to the transplanted patient could yield favorable outcomes about adherence to immunosuppressive therapy. Furthermore, this study also provided readers with important informations about psychological problems that could highlight on transplanted subject.
TA is the patient’s ability to be able to follow precisely the prescribed cure. Specifically, the concept of adherence to therapy includes the compliance and persistence: Compliance reflects the acceptance of the patient to medical prescription (number of daily dose), the persistence instead indicates the time period between the start and the interruption of the treatment. BIM provided a conceptual frame of reference within which biological, psychological, and social aspects took on the same importance in explaining the adherence to treatment protocols. You must operate simultaneously at several levels in an intervention program formulated on the basis of the characteristics and needs of each individual patient.
Studies concerning the influence of temperament to the therapeutic adherence are scarce. The authors in this study analyzed the psychological characteristics of a sample of transplant recipients followed as outpatients at a transplant center. The results showed that the transplant experience change behaviors and quality of life based on the personality and temperament characteristics.
Manuscript source: Invited manuscript
Specialty type: Transplantation
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Kedzierska K, Martinez-Mier G, Touchard G S- Editor: Qiu S L- Editor: A E- Editor: Lu YJ
| 1. | Vanholder R, Lameire N, Annemans L, Van Biesen W. Cost of renal replacement: how to help as many as possible while keeping expenses reasonable? Nephrol Dial Transplant. 2016;31:1251-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Chisholm-Burns MA, Spivey CA, Sredzinski E, Butler SL. Intervention toolbox to promote immunosuppressant therapy adherence in adult renal transplant recipients. J Am Pharm Assoc (2003). 2012;52:816-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Low JK, Williams A, Manias E, Crawford K. Interventions to improve medication adherence in adult kidney transplant recipients: a systematic review. Nephrol Dial Transplant. 2015;30:752-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 116] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 4. | Williams A, Crawford K, Manias E, Ellis C, Mullins K, Howe K, Kennedy E, Maney O, Mark T, Gregory D. Examining the preparation and ongoing support of adults to take their medications as prescribed in kidney transplantation. J Eval Clin Pract. 2015;21:180-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Butler JA, Peveler RC, Roderick P, Smith PW, Horne R, Mason JC. Modifiable risk factors for non-adherence to immunosuppressants in renal transplant recipients: a cross-sectional study. Nephrol Dial Transplant. 2004;19:3144-3149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 114] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 6. | Prihodova L, Nagyova I, Rosenberger J, Majernikova M, Roland R, Groothoff JW, van Dijk JP. Adherence in patients in the first year after kidney transplantation and its impact on graft loss and mortality: a cross-sectional and prospective study. J Adv Nurs. 2014;70:2871-2883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 70] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 7. | Dew MA, Dabbs AD, Myaskovsky L, Shyu S, Shellmer DA, DiMartini AF, Steel J, Unruh M, Switzer GE, Shapiro R. Meta-analysis of medical regimen adherence outcomes in pediatric solid organ transplantation. Transplantation. 2009;88:736-746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 188] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 8. | Denhaerynck K, Dobbels F, Cleemput I, Desmyttere A, Schäfer-Keller P, Schaub S, De Geest S. Prevalence, consequences, and determinants of nonadherence in adult renal transplant patients: a literature review. Transpl Int. 2005;18:1121-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 315] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 9. | De Pasquale C, Veroux M, Indelicato L, Sinagra N, Giaquinta A, Fornaro M, Veroux P, Pistorio ML. Psychopathological aspects of kidney transplantation: Efficacy of a multidisciplinary team. World J Transplant. 2014;4:267-275. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 66] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Lussier MT, Richard C, Glaser E, Roberge D. The impact of a primary care e-communication intervention on the participation of chronic disease patients who had not reached guideline suggested treatment goals. Patient Educ Couns. 2016;99:530-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Moore LA, Kaufman MD, Algozzine R, Irish N, Martin M, Posey CR. Adherence to therapy: using an evidence-based protocol. Rehabil Nurs. 2007;32:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Prihodova L, Nagyova I, Rosenberger J, Roland R, Groothoff JW, Majernikova M, van Dijk JP. Health-related quality of life 3 months after kidney transplantation as a predictor of survival over 10 years: a longitudinal study. Transplantation. 2014;97:1139-1145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | De Pasquale C, Pistorio ML, Corona D, Sinagra N, Giaquinta A, Zerbo D, Veroux P, Veroux M. Role of “self-efficacy” in the process of long-term care in kidney transplant recipients. Transplant Proc. 2014;46:2235-2237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Prihodova L, Nagyova I, Rosenberger J, Roland R, van Dijk JP, Groothoff JW. Impact of personality and psychological distress on health-related quality of life in kidney transplant recipients. Transpl Int. 2010;23:484-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | De Pasquale C, Pistorio ML, Sorbello M, Parrinello L, Corona D, Gagliano M, Giuffrida G, Giaquinta A, Sinagra N, Zerbo D. Body image in kidney transplantation. Transplant Proc. 2010;42:1123-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Pistorio ML, Veroux M, Corona D, Sinagra N, Giaquinta A, Zerbo D, Giacchi F, Gagliano M, Tallarita T, Veroux P. The study of personality in renal transplant patients: possible predictor of an adequate social adaptation? Transplant Proc. 2013;45:2657-2659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale--preliminary report. Psychopharmacol Bull. 1973;9:13-28. [PubMed] |
| 18. | Derogatis LR. SCL-90 Manual of Clinical Psychometrics Research Unit. Baltimore: University School of Medicine 1977; . |
| 19. | Brophy CJ, Norvell NK, Kiluk DJ. An examination of the factor structure and convergent and discriminant validity of the SCL-90R in an outpatient clinic population. J Pers Assess. 1988;52:334-340. [PubMed] |
| 20. | Jin S, Xiang B, Zhong L, Yan L, Chen Z, Wang W, Xu M, Yang J. Quality of life and psychological distress of adult recipients after living donor liver transplantation. Transplant Proc. 2013;45:281-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | De Pasquale C, Pistorio ML, Lauretta I, Fatuzzo P, Fornaro M, Conti D, Di Nuovo S, Sinagra N, Giaquinta A, Zerbo D. Somatopsychic correlates and quality of life of the dialyzed patient: a cross-sectional study. Transplant Proc. 2014;46:2199-2202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Depasquale C, Pistorio ML, Corona D, Mistretta A, Zerbo D, Sinagra N, Giaquinta A, Tallarita T, Esker B, Mociskyte D. Correlational study between psychic symptoms and quality of life among hemodialysis patients older than 55 years of age. Transplant Proc. 2012;44:1876-1878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Cloninger CR, Zohar AH. Personality and the perception of health and happiness. J Affect Disord. 2011;128:24-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 207] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 24. | Dembińska-Krajewska D, Rybakowski J. [The Temperament Evaluation of Memphis, Pisa and San Diego Autoquestionnaire (TEMPS-A)--an important tool to study affective temperaments]. Psychiatr Pol. 2014;48:261-276. [PubMed] |
| 25. | Pompili M, Girardi P, Tatarelli R, Iliceto P, De Pisa E, Tondo L, Akiskal KK, Akiskal HS. TEMPS-A (Rome): psychometric validation of affective temperaments in clinically well subjects in mid- and south Italy. J Affect Disord. 2008;107:63-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 26. | Fujisawa M, Ichikawa Y, Yoshiya K, Isotani S, Higuchi A, Nagano S, Arakawa S, Hamami G, Matsumoto O, Kamidono S. Assessment of health-related quality of life in renal transplant and hemodialysis patients using the SF-36 health survey. Urology. 2000;56:201-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 122] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 27. | De Pasquale C, Pistorio ML, Veroux P, Giuffrida G, Sinagra N, Ekser B, Zerbo D, Corona D, Giaquinta A, Veroux M. Quality of life in kidney transplantation from marginal donors. Transplant Proc. 2011;43:1045-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 28. | Dobbels F, Berben L, De Geest S, Drent G, Lennerling A, Whittaker C, Kugler C. The psychometric properties and practicability of self-report instruments to identify medication nonadherence in adult transplant patients: a systematic review. Transplantation. 2010;90:205-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 177] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 29. | Cleemput I, Dobbels F. Measuring patient-reported outcomes in solid organ transplant recipients: an overview of instruments developed to date. Pharmacoeconomics. 2007;25:269-286. [PubMed] |
| 30. | American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM 5). Washington DC: New School Library 2013; . |
| 31. | Calia R, Lai C, Aceto P, Luciani M, Camardese G, Lai S, Fantozzi C, Pietroni V, Salerno MP, Spagnoletti G. Emotional self-efficacy and alexithymia may affect compliance, renal function and quality of life in kidney transplant recipients: results from a preliminary cross-sectional study. Physiol Behav. 2015;142:152-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Lindau ST, Laumann EO, Levinson W, Waite LJ. Synthesis of scientific disciplines in pursuit of health: the Interactive Biopsychosocial Model. Perspect Biol Med. 2003;46:S74-S86. [PubMed] |
| 33. | Colivicchi F, Abrignani MG, Santini M. [Therapeutic non-adherence: the hidden risk factor]. G Ital Cardiol (Rome). 2010;11:124S-127S. [PubMed] |
| 34. | Tielen M, van Exel J, Laging M, Beck DK, Khemai R, van Gelder T, Betjes MG, Weimar W, Massey EK. Attitudes to medication after kidney transplantation and their association with medication adherence and graft survival: a 2-year follow-up study. J Transplant. 2014;2014:675301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 35. | Delara M, Woodgate RL. Psychological Distress and its Correlates among University Students: A Cross-Sectional Study. J Pediatr Adolesc Gynecol. 2015;28:240-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Chisholm MA, Kwong WJ, Spivey CA. Associations of characteristics of renal transplant recipients with clinicians’ perceptions of adherence to immunosuppressant therapy. Transplantation. 2007;84:1145-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 37. | Chisholm MA, Williamson GM, Lance CE, Mulloy LL. Predicting adherence to immunosuppressant therapy: a prospective analysis of the theory of planned behaviour. Nephrol Dial Transplant. 2007;22:2339-2348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 38. | Haynes RB, Montague P, Oliver T, McKibbon KA, Brouwers MC, Kanani R. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2000;CD000011. [PubMed] |
| 39. | Weng FL, Chandwani S, Kurtyka KM, Zacker C, Chisholm-Burns MA, Demissie K. Prevalence and correlates of medication non-adherence among kidney transplant recipients more than 6 months post-transplant: a cross-sectional study. BMC Nephrol. 2013;14:261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 77] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 40. | Fornaro M, Ventriglio A, De Pasquale C, Pistorio ML, De Berardis D, Cattaneo CI, Favaretto E, Martinotti G, Tomasetti C, Elassy M. Sensation seeking in major depressive patients: relationship to sub-threshold bipolarity and cyclothymic temperament. J Affect Disord. 2013;148:375-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 41. | Chisholm-Burns M, Pinsky B, Parker G, Johnson P, Arcona S, Buzinec P, Chakravarti P, Good M, Cooper M. Factors related to immunosuppressant medication adherence in renal transplant recipients. Clin Transplant. 2012;26:706-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 72] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 42. | Sharp J, Wild MR, Gumley AI, Deighan CJ. A cognitive behavioral group approach to enhance adherence to hemodialysis fluid restrictions: a randomized controlled trial. Am J Kidney Dis. 2005;45:1046-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 85] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 43. | van Lint CL, van der Boog PJ, Wang W, Brinkman WP, Rövekamp TJ, Neerincx MA, Rabelink TJ, van Dijk S. Patient experiences with self-monitoring renal function after renal transplantation: results from a single-center prospective pilot study. Patient Prefer Adherence. 2015;9:1721-1731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 44. | Cameron LD, Leventhal H. The Self-regulation of Health and Illness Behaviour. London: Routledge 2003; . |