Published online Jun 24, 2016. doi: 10.5500/wjt.v6.i2.429
Peer-review started: January 15, 2016
First decision: February 2, 2016
Revised: February 18, 2016
Accepted: April 14, 2016
Article in press: April 18, 2016
Published online: June 24, 2016
Processing time: 160 Days and 19.8 Hours
AIM: To increase inspiratory muscle strength and improve the quality of life of candidates for liver transplantation.
METHODS: Twenty-three candidates for liver transplantation participated in the control group and 14 made up the intervention group. The control group consisted of 18 men and 5 women, body mass index (BMI) 27.3 ± 4.5 kg/m2 and Model for End-Stage Liver Disease (MELD) 18.2 ± 6.1. The intervention group consisted of 11 men and 3 women, BMI 28.6 ± 5.4 kg/m2 and MELD 18 ± 4.5. The presence or absence of ascites was identified in the first patient evaluation and after three months. We evaluated maximal inspiratory pressure (MIP) and maximal expiratory pressure, spirometry, root mean square (RMS) of diaphragm and rectus abdominis, and the quality of life. The exercises were performed daily by patients at home for three months and were supervised at distance monthly. The manual consisted of diaphragmatic breathing exercises, diaphragmatic isometric exercise, Threshold IMT®, lifting upper limbs with a bat and strengthening the abdomen.
RESULTS: There was significant difference (P = 0.01) between the first (initial) and the third month (final) MIP in the control group and in the intervention group, but there was no difference (P = 0.45) between the groups. The RMS of the diaphragm was lower (P = 0.001) and the functional capacity was higher (P = 0.006) in the intervention group compared to the control. The general health and mental health domains received higher scores after three months in the control group (P = 0.01) and the intervention group (P = 0.004), but there was no significant difference between them. The comparison between the presence of initial ascites with the presence of ascites was performed after three months in the control group (P = 0.083) and intervention group (P = 0.31). There was no significant difference, in relation to the presence of ascites after three months between groups (P = 0.21). In the intervention group, patients with ascites at the end of the time period had decreased scores on the social aspects SF-36 domain (P = 0.023) compared to those who had no ascites.
CONCLUSION: The proposed exercises provide an increase in the inspiratory muscle strength and improve functional capacity, consequently bettering the quality of life of liver disease patients.
Core tip: Studies on the effects of exercises, mainly those on breathing for liver transplant patients on the waiting list, are rare in the literature. This study proposes a manual of exercises for this group in order to increase muscle strength and improve their quality of life, as sarcopenia found in these patients contributes to a worsening of quality of life and is associated with mortality. The results are encouraging and may represent the beginning of further studies in the area and the establishment of exercise protocols for liver diseases.
- Citation: Limongi V, Dos Santos DC, Oliveira da Silva AM, Boin IFSF, Stucchi RSB. Exercise manual for liver disease patients. World J Transplant 2016; 6(2): 429-436
- URL: https://www.wjgnet.com/2220-3230/full/v6/i2/429.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i2.429
Liver transplantation means a chance of survival for individuals with advanced chronic liver diseases or acute liver failure when there are no clinical treatments available[1-3]. However, there is a disproportion between the supply of organs[4] and those in need of transplantation, increasing the time on the waiting list and the chance of complications[5] such as fatigue, decreased aerobic capacity, malnutrition, sarcopenia[6] and impaired ventilator mechanics due to ascites[7].
Sarcopenia may be associated with mortality in cirrhotic patients[8,9] and contributes to an impaired of quality of life in these patients[10-13].
Probably also due to loss of muscle mass, according to the authors Oliveira da Silva et al[7], and da Silva et al[14], the liver disease patients showed on average higher RMS of the diaphragm when compared to healthy subjects. This means that the respiratory muscles of patients with liver disease should try harder to gain the best resistance in the basal ventilation profile, in order for the electrical activity of the diaphragm to be higher.
Studies of Dharancy et al[15], Pieber et al[16] and Wiesinger et al[17], suggest that a change from the predominance of aerobic metabolism to anaerobic metabolism occurs early during exercise in individuals with cirrhosis compared to healthy subjects[8].
The findings in cardiopulmonary exercise testing, early termination of exercise with low peak VO2 (oxygen consumption), hyperventilation precocious and reduced or unattainable ventilatory threshold[15,18] may correspond to a fatigue at the beginning of exercise or indicate deconditioning thus hampering the exercise. This reflects the difficulty that cirrhotic patients have to performing everyday activities, as well as feeling fatigue[17] even when they are hospitalized.
All these complications in the preoperative period, which also influence the recovery after transplantation, can be mitigated with well-defined and specific intervention programs for this group.
Therefore, the aim of the study was to increase inspiratory muscle strength and improve quality of life for liver disease patients with the proposed manual of breathing exercises.
In this prospective, randomized and controlled trial, data collection was performed at the Unit of Liver Transplantation, Hospital de Clinicas, State University Campinas (Unicamp). The study protocol followed the Ethics Committee of the Medical Sciences Faculty, Unicamp, CEP: 922/2009. Each study participant signs the Informed consent statement.
Liver disease patients were included, men and women, aged over 18 years, with or without a diagnosis of cardiorespiratory disease and those with any Model for End-Stage Liver Disease (MELD) score obtained. All patients filled out a form for identification, age, gender and diagnosis of liver disease. The MELD and body mass index (BMI) were calculated. The presence or absence of ascites was identified in the first patient evaluation and after three months.
Exclusion criteria were: The inability to understand verbal commands, patients with poor general condition (for example, bed reset condition), the failure to perform the evaluations and acute liver failure diagnosis.
The study population was selected from the liver transplant waiting list from August 2012 to February 2014. From the 49 patients evaluated, 27 individuals were chosen through a random draw for participation in the control group. However, four patients were excluded; three died and one was submitted to a liver transplantation. Thus, 23 patients made up the control group. Twenty-two patients were randomly picked to take part in the intervention group, through a random draw. However, eight patients were excluded as three died, two had liver transplant operations and three individuals declined to perform the exercises. Thus, 14 patients constituted the intervention group. Software for randomization and allocation was not used; the names of the patients were placed in identical envelopes and drawn by the researcher, one by one, to make up the control group and intervention.
The control group was composed of 18 men (78.3%) and five women (21.7%) and the intervention group consisted of 11 men (78.6%) and three women (21.4%). Table 1 shows the demographic and baseline characteristics of the patients.
| Features | Control (n = 23) | Intervention (n = 14) | P |
| Male/female | 18 (78.3%)/5 (21.7%) | 11 (78.6%)/3 (21.4%) | 1.00 |
| Age (yr) | 55.4 ± 9.9 | 55.8 ± 5.4 | 0.97 |
| BMI (kg/m2) | 27.3 ± 4.5 | 28.6 ± 5.4 | 0.58 |
| Diagnosis | |||
| HCV | 5 (21.7%) | 4 (28.6%) | |
| HCC + HCV | 4 (17.4%) | ||
| Alcohol | 3 (13%) | 3 (21.4%) | |
| HCC | 3 (13%) | ||
| Alcohol + HCV | 3 (13%) | 2 (14.2%) | |
| Alcohol + HCC | 1 (4.3%) | ||
| Alcohol + HCV + HCC | 1 (4.3%) | 2 (14.2%) | |
| Autoimmune hepatitis | 1 (4.3%) | ||
| Polycystic liver disease | 1 (4.3%) | ||
| Cryptogenic cirrhosis | 1 (7.1%) | ||
| Sclerosing cholangitis | 1 (7.1%) | ||
| HBV + HCV | 1 (7.1%) |
The respiratory pressures, maximal inspiratory pressure (MIP) and maximal expiratory pressure (MEP) were measured using an analog manometer Gerarmed® (SP, Brazil), with unit scale in cmH2O, coupled to a mouthpiece and nose clip, always with the patient seated. The data were always collected by the same researcher.
To measure the MIP was requested a maximum exhalation until residual volume and after, a maximal inspiratory effort. To measure the MEP a maximal inspiratory effort was asked for in order to achieve the level of total lung capacity, and then a maximum expiratory effort. The maneuvers were repeated three to five times at intervals of 30 s and it was considered the highest value obtained[19].
The surface electromyography EMG System of Brazil Ltda®, Series 00405, Model 210C (SP, Brazil) was used to obtain the electrical activity of the diaphragm and rectus abdominis, represented by the root mean square (RMS). Electrodes 3M Brazil® (Sumare, SP, Brazil) were used for the study of electrical activity in these muscles.
The electronic circuit acquisition captures and processes the signals, making them available to the EMG System of Brasil® software, it was installed on a computer Intelbras I21® (SP, Brazil).
The participants were positioned at 45° in order to study the electrical activity of the diaphragm. A passive electrode was adapted in the paraxiphoid position about 5 cm from the xiphoid process and another 16 cm from the right costal margin. To measure the rectus abdominis an electrode was adapted in the rectus abdominis muscle 5 cm away from the umbilicus and another about 15 cm along the involved muscle[7]. On the left hand side was positioned a ground electrode. Participants breathe normally while the electrical activity was recorded for ten seconds. A heavy breathing was requested every three seconds. For rectus abdominis was used 500 Hz of frequency and 500 μV of the sensitivity of signal amplitude[7]. For the diaphragm was used 300 Hz frequency and 300 μV of the sensitivity of signal amplitude[7].
Through EasyOne Diagnostic Espirometer World® (Zurich, Switzerland), it was possible to perform spirometry, following the Guidelines for Pulmonary Function Tests[20]. Forced vital capacity (FVC), forced expiratory volume in one second (FEV1) and forced expiratory flow rate at 25%-75% of FVC curve (FEF25%-75%) were measured.
The “short form 36” (SF-36)[21] was used to evaluate the quality of life of the participants. The questionnaire consisted of 36 items related to eight domains covering different concepts of health, functional capacity, physical role, pain, general health, vitality, social aspects, emotional role and mental health.
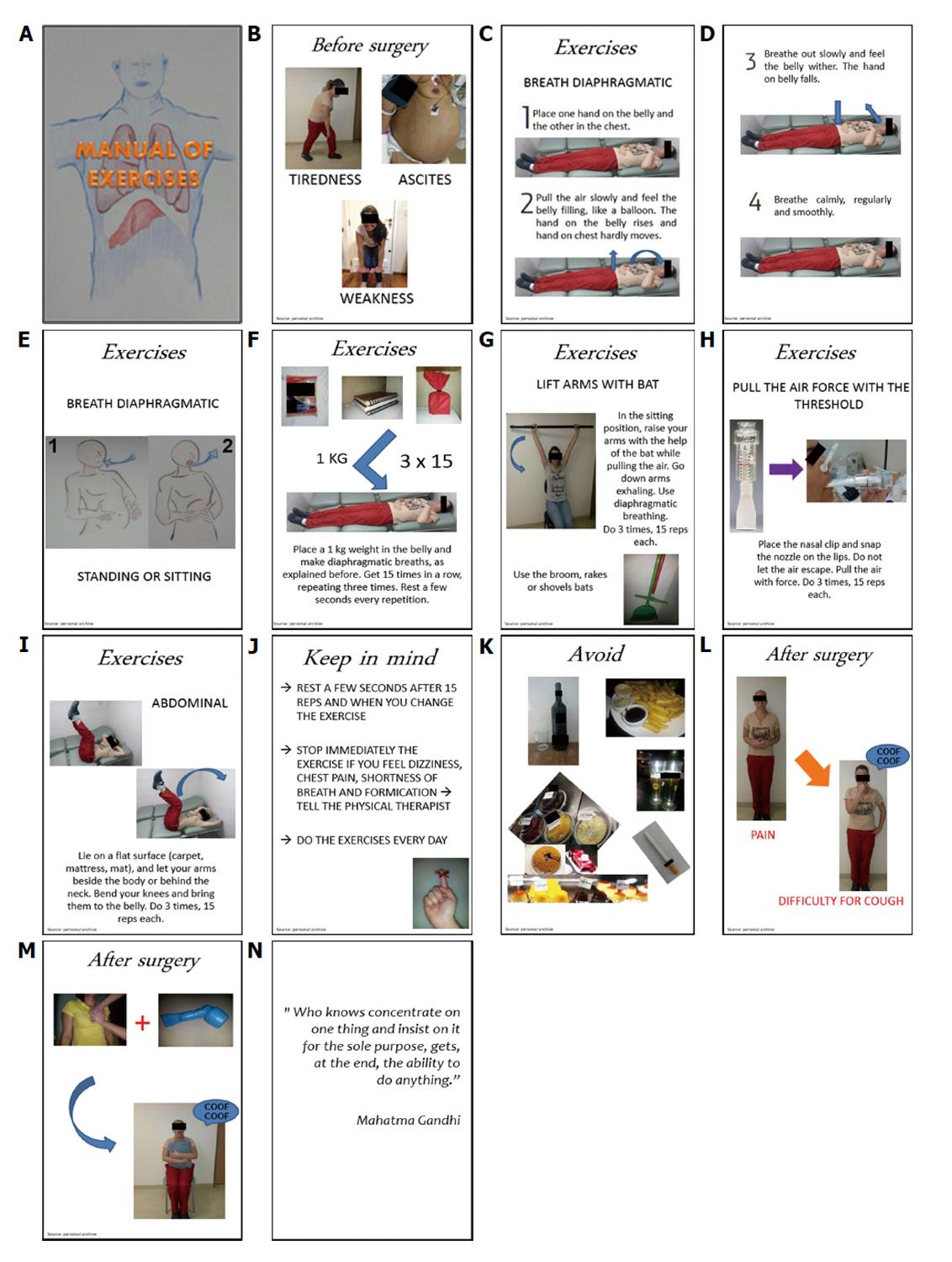
Participants in the intervention group received a manual with illustrations and explanations to be held at home for three months and they received orientation from the therapist at the time of the delivery of the material. The first evaluation was made at this time; the second was made after three months. Figure 1 shows the prepared manual.
The therapist remained available for any questions and followed up these patients monthly by phone.
Patients were aware regarding diaphragmatic breathing and instructed to perform this breathing in all the exercises.
In addition to the diaphragmatic breathing, the exercises described in the manual were: Diaphragmatic isometric exercise with the patient in the supine position and 1kg of weight placed on the diaphragm muscle, exercise with Threshold inspiratory muscular training (IMT)® (Philips Respironics®), elevation of upper limbs with the help of a bat and strengthening the abdominal muscles.
The manual contained information of the possible complications during the postoperative period. It was highlighted the importance of bronchial hygiene and the proper way to cough in the postoperative period. Patients were instructed to perform the exercises in three sets of fifteen repetitions.
The control group did not perform the exercises; the second evaluation was done three months after the first.
The patients’ tolerance was a parameter for the choice of load for training with the Threshold IMT®, since it is already established in the literature that liver disease patients have fatigue[17,22,23] and interrupt the exercise early with low peak VO2[15,18].
The manual also contained orientation for patients regarding the avoidance of alcohol, cigarettes, sweets and fried foods and had information about the importance of exercises during postoperative recovery from liver transplantation, especially concerning bronchial hygiene and effective cough.
The Statistical Analysis System (SAS) System for Windows (SAS Institute Inc, Cary, NC, United States), version 9.2 was used for statistical analysis.
Position and dispersion measures were used for numerical variables and frequency tables for categorical variables, for descriptive analysis.
For comparison of proportions, the χ2 test or Fisher’s exact test were used when necessary. For comparison of numerical measurements between two groups the exact Mann-Whitney test was used. For comparison of measurements between groups and times, ANOVA for repeated measurements was employed or post hoc transformation. To compare changes in proportions, the McNemar test was used. The significance level used was P < 0.05.
There was significant difference (P = 0.01) between the first (initial) and the third month (final) MIP in the control group and in the intervention group, but there was no difference (P = 0.45) between the groups.
After three months, the electromyography of the diaphragm represented by RMS decreased in the intervention group (P = 0.001) compared to that of the control group.
The score of the domain functional capacity (SF-36) was not statistically different between the groups; however, in the intervention group there was a significant increase in the score (P = 0.006) after three months.
The general health and mental health domains received higher scores after three months in the control group (P = 0.01) and the intervention group (P = 0.004), but there was no significant difference between them.
The descriptive analysis and comparison between groups are detailed in Table 2.
| Control (n = 23) | Intervention (n = 14) | P | |||
| Initial | Final | Initial | Final | ||
| MIP (cmH2O) | 88.5 (44.1) | 98.3 (39.2) | 101.1 (34.4) | 117.9 (43) | 0.45 |
| MEP (cmH2O) | 108.3 (46.3) | 116.5 (51.8) | 113.6 (31) | 128.2 (35) | 0.61 |
| EMG rectus (μV) | 52.9 (51.1) | 46.1 (29.7) | 32.5 (12.4) | 28.8 (7.9) | 0.65 |
| EMG diaphragm (μV) | 43.8 (14.9) | 53.8 (22.4) | 55.7 (34.7) | 35.6 (15.8) | 0.0011 |
| FVC (%) | 84.6 (13.9) | 85.5 (16.1) | 88.3 (14.5) | 92.6 (14.2) | 0.42 |
| FEV1 (%) | 84.6 (15.1) | 85.4 (14.5) | 88.6 (20) | 90 (14.1) | 0.5 |
| FEF25%-75% (%) | 92.4 (31.2) | 94.7 (24.6) | 100.7 (47.1) | 102.9 (44.2) | 0.72 |
| Funcional capacity | 68.5 (24.5) | 71.7 (21.7) | 69.3 (21.4) | 84.6 (14.5) | 0.0062 |
| Physical role | 52.2 (39.1) | 45.7 (38.9) | 60.7 (38.9) | 55.4 (38.2) | 0.92 |
| Pain | 61 (32) | 61.3 (21.1) | 62 (27.9) | 56.7 (30.1) | 0.78 |
| General health | 52.8 (26.2) | 58.4 (26.3) | 59.3 (20.1) | 68.4 (19.3) | 0.4 |
| Vitality | 61.7 (23.9) | 59.8 (23.2) | 58.9 (15.2) | 65 (25.2) | 0.33 |
| Social aspects | 58.2 (34.9) | 67.9 (29.9) | 68.8 (37.3) | 75.9 (30) | 0.93 |
| Emotional role | 60.8 (39.8) | 56.5 (44.3) | 45.1 (44.5) | 61.9 (36.6) | 0.16 |
| Mental health | 59.1 (26.4) | 64.5 (24) | 64.9 (20.7) | 78.3 (22) | 0.14 |
In the first evaluation, 10 patients had ascites in the control group and 3 had ascites in the intervention group. After three months, 13 patients had ascites in the control group and 5 patients had ascites in the intervention group.
The comparison between the presence of initial ascites with the presence of ascites was performed after three months in the control group (P = 0.083) and intervention group (P = 0.31). There was no significant difference in relation to the presence of ascites after three months between groups (P = 0.21).
The presence or absence of ascites three months after the first assessment was compared with age, BMI, MIP, MEP, RMS of the diaphragm and rectus abdominis, FVC, FEV1, FEF25%-75% and the SF-36 domains.
There was no significant difference between the variables in the control group. In the intervention group, patients with ascites at the end of the time period had decrease of scores on the social aspects domain (P = 0.023) compared to those who had no ascites.
Patients on the waiting list for liver transplantation waiting a long time for the new organ and consequently, there may be complications in this period, such as sarcopenia. Therefore, rehabilitation becomes an important alternative in order to reduce inactivity, increase muscle performance, as well as exercise tolerance, and to avoid complications in the post-operative period[24].
The results of this study showed that most patients were men, aged above 50 years and BMI revealing overweight. These findings are consistent with other studies[9,25].
Several authors[26,27] have recommended IMT in order to minimize respiratory muscle dysfunction in the postoperative period of cardiac, thoracic and abdominal surgery. Despite the literature employing a 40%[28] initial MIP load for IMT and increasing it over time training, patients’ tolerance has been responsible for the choice of load for training with the Threshold IMT®, since it is already established in the literature that liver disease patients have fatigue[20-23].
In the current study, there was a significant increase of MIP in the intervention group after the final evaluation.
In the study of Gosselink et al[29], a meta-analysis was performed on the effects of IMT in patients with chronic obstructive pulmonary disease. The study revealed better results in the inspiratory muscle strength, functional capacity and dyspnea after strength training.
In the study by Serón et al[28], the Threshold IMT® was effective for strengthening inspiratory muscles.
One possible explanation for the non-significant increase in MEP in the present study is that the main focus of the prepared manual was to strengthen the inspiratory muscles. Unlike what was expected, the control group also showed a significant increase in MIP after three months. One possible explanation is that the patients were not discouraged from performing physical activities or were advised to stop exercising because they were participating in the research.
The intervention proved to be effective in this study; after three months there was a reduction of the RMS of the diaphragm in the intervention group, and due to the increase of the inspiratory muscle strength, the diaphragm needed to perform less force in order to overcome the same resistance. In other words, the action’s potential decreased since only a small amount of fibers were needed to be recruited during normal breathing. No articles on the effects of inspiratory muscle training on electromyography of the diaphragm have been found; therefore, further studies are required for a broader discussion on the issue.
The exercise program also provided relevant improvement in functional capacity domain. This means that the difficulty in performing daily life activities decreased, and individuals became more active and willing. Regarding liver transplant, two authors[30,31] proved that the quality of life can be improved with physical exercises.
The general and mental health areas received higher scores after three months in the intervention and control groups, demonstrating that the patients’ perception of their health improved. The control group may have presented positive changes in the mentioned aspects for the same reasons already explained above.
Also, one must consider, on average, an increase of some values of variables (FVC, FEV 1, FEF 25%-75%, vitality, social aspects and emotional role) at the end time, in the intervention group, showing the positive effects of the intervention performed.
The two groups were not ideally matched, because the incidence of ascites was lower in the intervention group in the first evaluation and after three months. However, the presence of ascites did not affect the respiratory variables evaluated. In the intervention group, patients with ascites had worse scores on the social aspects domain. In the final stage of cirrhosis, ascites causes the appearance of symptoms that can impair the performance of activities of daily living[32]. All these factors contribute to social isolation being away from work and low self-esteem. According to Saab et al[33], the ascites, associated or not with encephalopathy, was associated with poorer quality of life.
Certainly, new studies on the benefits of breathing exercises will be necessary after liver transplantation. However, the results of the present study are satisfactory regarding the improvement of quality of life as well as the electrical diaphragm activity result using the exercises learnt in the preoperative manual. This study is the beginning of exercise protocols developed specifically for this group, and it may prompt new research with a larger population sample.
The authors also thank Philips Respironics® who kindly provided the Threshold IMT® for the study. Our acknowledgments to Stephen A Shaw for the English revision.
Some changes usually affect the quality of life of patients with chronic liver disease, such as fatigue, malnutrition and predominance of anaerobic metabolism. In order to improve the functionality, muscle strength and physical conditioning of the liver disease patients and physically prepare them for transplantation, minimizing possible postoperative complications, specific preoperative rehabilitation programs for this population become necessary.
The liver transplant waiting list patients belong to the Unit of Liver Transplantation at the Hospital de Clinicas/Unicamp, and are from several cities in the state of Sao Paulo, and other regions of Brazil. Therefore, it was difficult to weekly or even monthly require patients to participate in evaluations or in the respiratory intervention group at the Unit of Liver Transplantation. In addition, these patients are constantly doing exams, have difficult schedules, and often need help for locomotion. As a result, these patients were followed up by phone each month. Despite these hardships, in the current study, only three participants were excluded from the trial, since they declined to perform the exercises. The other patients satisfactorily agreed to the exercises. Due to lack of financial resources, the authors used the analog manometer and some Thresholds inspiratory muscular training (IMT)® were donated by Philips Respironics®. Each participant remained with the Threshold IMT® for three months. This contributed to the reduced sample in the intervention group, in addition to other factors, such as death, abandonment or the transplant itself.
An illustrative and explanatory manual was prepared with breathing exercises to be performed by patients at home, for a period of three months. Monthly, they were accompanied by the same researcher by telephone, and doubts were resolved.
The results found in the group that performed the exercises were encouraging; there was a decrease in the electrical activity of the diaphragm and increase some scores of the short form 36 domains. These results represent a start for new rehabilitation programs which are developed preoperatively. Still, the proposed manual in this article may be used in other studies, with extended samples, and further positive results may be found.
The manual of the exercises was prepared by the researchers and consisted of breathing exercises, including the Threshold IMT®. The Threshold is a device designed for respiratory muscle training in which the load is independent of the air flow. It consists of a chamber where at the distal end there is a valve which is held closed by the positive pressure (graduated in cmH2O) of a spring. If a negative pressure with an absolute value greater than the spring pressure is generated, the valve will open and allow the air passage.
Studies on the effects of exercises, mainly those on breathing, in liver disease awaiting transplantation are rare in the literature. This issue can spark interest in other researchers who want to study the manual exercises in an enlarged sample of liver disease patients and who also want to follow up these patients postoperatively, evaluating the effects of exercises in this period. Another possibility is to use this study as a basis for development of new specific exercise programs before surgery for this population.
P- Reviewer: Bramhall S, Marino IR, Qin JM, Salvadori M, Sugawara Y S- Editor: Qiu S L- Editor: A E- Editor: Liu SQ
| 1. | Ahmed A, Keeffe EB. Current indications and contraindications for liver transplantation. Clin Liver Dis. 2007;11:227-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Murray KF, Carithers RL. AASLD practice guidelines: Evaluation of the patient for liver transplantation. Hepatology. 2005;41:1407-1432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 563] [Cited by in RCA: 516] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 3. | Consensus conference: Indications for Liver Transplantation, January 19 and 20, 2005, Lyon-Palais Des Congrès: text of recommendations (long version). Liver Transpl. 2006;12:998-1011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Moon DB, Lee SG. Liver transplantation. Gut Liver. 2009;3:145-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Fisher NC, Nightingale PG, Gunson BK, Lipkin GW, Neuberger JM. Chronic renal failure following liver transplantation: a retrospective analysis. Transplantation. 1998;66:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 248] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 6. | Galant LH, Ferrari R, Forgiarini LA, Monteiro MB, Marroni CA, Dias AS. Relationship between MELD severity score and the distance walked and respiratory muscle strength in candidates for liver transplantation. Transplant Proc. 2010;42:1729-1730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Oliveira da Silva AM, Maturi S, Boin IF. Comparison of surface electromyography in respiratory muscles of healthy and liver disease patients: preliminary studies. Transplant Proc. 2011;43:1325-1326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Jones JC, Coombes JS, Macdonald GA. Exercise capacity and muscle strength in patients with cirrhosis. Liver Transpl. 2012;18:146-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 107] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 9. | Montano-Loza AJ, Meza-Junco J, Prado CM, Lieffers JR, Baracos VE, Bain VG, Sawyer MB. Muscle wasting is associated with mortality in patients with cirrhosis. Clin Gastroenterol Hepatol. 2012;10:166-173, 173.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 537] [Cited by in RCA: 609] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 10. | Larson AM, Curtis JR. Integrating palliative care for liver transplant candidates: “too well for transplant, too sick for life”. JAMA. 2006;295:2168-2176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 79] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Mehta G, Rothstein KD. Health maintenance issues in cirrhosis. Med Clin North Am. 2009;93:901-15, viii-ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Norman K, Kirchner H, Lochs H, Pirlich M. Malnutrition affects quality of life in gastroenterology patients. World J Gastroenterol. 2006;12:3380-3385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 67] [Cited by in RCA: 86] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Panagaria N, Varma K, Nijhawan S, Mathur A, Rai RR. Quality of life and nutritional status in alcohol addicts and patients with chronic liver disease. Trop Gastroenterol. 2007;28:171-175. [PubMed] |
| 14. | da Silva AM, Cliquet A, Boin IF. Profile of respiratory evaluation through surface electromyography, manovacuometry, and espirometry in candidates on the liver transplant waiting list. Transplant Proc. 2012;44:2403-2405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Dharancy S, Lemyze M, Boleslawski E, Neviere R, Declerck N, Canva V, Wallaert B, Mathurin P, Pruvot FR. Impact of impaired aerobic capacity on liver transplant candidates. Transplantation. 2008;86:1077-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 98] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Pieber K, Crevenna R, Nuhr MJ, Quittan M, Peck-Radosavljevic M, Fialka-Moser V, Wiesinger GF. Aerobic capacity, muscle strength and health-related quality of life before and after orthotopic liver transplantation: preliminary data of an Austrian transplantation centre. J Rehabil Med. 2006;38:322-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Wiesinger GF, Quittan M, Zimmermann K, Nuhr M, Wichlas M, Bodingbauer M, Asari R, Berlakovich G, Crevenna R, Fialka-Moser V. Physical performance and health-related quality of life in men on a liver transplantation waiting list. J Rehabil Med. 2001;33:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Lemyze M, Dharancy S, Nevière R, Wallaert B. Cardiopulmonary response to exercise in patients with liver cirrhosis and impaired pulmonary gas exchange. Respir Med. 2011;105:1550-1556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Sociedade Brasileira de Pneumologia e Tisiologia. Diretrizes para testes de função pulmonar. J Pneumol. 2002;28:2-237. |
| 21. | Ciconelli RM, Ferraz MB, Santos W, Meinão I, Quaresma MR. Portuguese version of the SF-36. A reliable and valid quality of life outcome measure. Rev Bras Reumatol. 1999;39:143-150. |
| 22. | van den Berg-Emons R, van Ginneken B, Wijffels M, Tilanus H, Metselaar H, Stam H, Kazemier G. Fatigue is a major problem after liver transplantation. Liver Transpl. 2006;12:928-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Jones EA. Fatigue complicating chronic liver disease. Metab Brain Dis. 2004;19:421-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Abdeldayem H. Physiotherapy in Liver Transplantation. In: Senduran M, Yurdalan U. Liver Transplantation -Technical Issues and Complications 2012; Available from: http//www.intechopen.com/books/liver-transplantation-technical-issues-and-complications/physiotherapy-in-liver-transplantation. |
| 25. | Galant LH, Forgiarini Junior LA, Dias AS, Marroni CA. Functional status, respiratory muscle strength, and quality of life in patients with cirrhosis. Rev Bras Fisioter. 2012;16:30-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | McClean KM, Kee F, Young IS, Elborn JS. Obesity and the lung: 1. Epidemiology. Thorax. 2008;63:649-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 214] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 27. | Lawrence VA, Cornell JE, Smetana GW. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006;144:596-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 286] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 28. | Serón P, Riedemann P, Muñoz S, Doussoulin A, Villarroel P, Cea X. [Effect of inspiratory muscle training on muscle strength and quality of life in patients with chronic airflow limitation: a randomized controlled trial]. Arch Bronconeumol. 2005;41:601-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Gosselink R, De Vos J, van den Heuvel SP, Segers J, Decramer M, Kwakkel G. Impact of inspiratory muscle training in patients with COPD: what is the evidence? Eur Respir J. 2011;37:416-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 318] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 30. | Beyer N, Aadahl M, Strange B, Kirkegaard P, Hansen BA, Mohr T, Kjaer M. Improved physical performance after orthotopic liver transplantation. Liver Transpl Surg. 1999;5:301-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 87] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 31. | Painter P, Krasnoff J, Paul SM, Ascher NL. Physical activity and health-related quality of life in liver transplant recipients. Liver Transpl. 2001;7:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 114] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 32. | Perri GA. Ascites in patients with cirrhosis. Can Fam Physician. 2013;59:1297-1299; e538-540. [PubMed] |
| 33. | Saab S, Ibrahim AB, Shpaner A, Younossi ZM, Lee C, Durazo F, Han S, Esrason K, Wu V, Hiatt J. MELD fails to measure quality of life in liver transplant candidates. Liver Transpl. 2005;11:218-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 89] [Article Influence: 4.5] [Reference Citation Analysis (0)] |