Published online Jun 24, 2016. doi: 10.5500/wjt.v6.i2.347
Peer-review started: November 30, 2015
First decision: December 28, 2015
Revised: January 31, 2016
Accepted: March 9, 2016
Article in press: March 14, 2016
Published online: June 24, 2016
Processing time: 207 Days and 9.2 Hours
AIM: To performed remains a subject of debate and is the principal aim of the study.
METHODS: This retrospective analysis included 73 patients with emphysema (2000-2012). The outcomes of patients undergoing single-lung transplantation (SL) (n = 40) or double-lung transplant (DL) (n = 33) were compared in a Cox multivariate analysis to study the impact of the technique, postoperative complications and acute and chronic rejection on survival rates. Patients were selected for inclusion in the waiting list according to the International Society of Heart Lung Transplantation criteria. Pre and postoperative rehabilitation and prophylaxis, surgical technique and immunosuppressive treatment were similar in every patients. Lung transplantation waiting list information on a national level and retrospective data on emphysema patient survival transplanted in Spain during the study period, was obtained from the lung transplantation registry managed by the National Transplant Organization (ONT).
RESULTS: Both groups were comparable in terms of gender and clinical characteristics. We found significant differences in the mean age between the groups, the DL patients being younger as expected from the inclusion criteria. Perioperative complications occurred in 27.6% SL vs 54% DL (P = 0.032). Excluding perioperative mortality, median survival was 65.3 mo for SL and 59.4 mo for DL (P = 0.96). Bronchiolitis obliterans and overall 5-year survival were similar in both groups. Bacterial respiratory infection, cytomegalovirus and fungal infection rates were higher but not significant in SL. No differences were found between type of transplant and survival (P = 0.48). To support our results, national data on all patients with emphysema in waiting list were obtained (n = 1001). Mortality on the waiting list was 2.4% for SL vs 6.2% for DL. There was no difference in 5 year survival between 235 SL and 430 DL patients transplanted (P = 0.875).
CONCLUSION: Our results suggest that SL transplantation in emphysema produce similar survival than DL with less postoperative complication and significant lower mortality in waiting list.
Core tip: This is a retrospective and comparative study of 2 cohort of patients with advanced-stage emphysema who were performed uni or bilateral lung transplant. The results of this study support the realization of single-lung transplantation in most of the cases of emphysema because it is technically simpler, it has less risk of surgical sutures, and finally it has less immediate postoperative complications. Single and double lung transplantation has a similar long-term survival. Moreover, if a second transplant is needed in the long-term, the contralateral transplantation has the same initial transplant survival if the patient remains in a similar clinical situation. Survival Spanish national register does not show difference between the two techniques too, supporting the results of our relatively small series. This strategy of performing single lung transplantation in most of the cases of emphysema would encourage and enhance the use of donors thanks to the twining procedure, and would decrease mortality in the waiting list as shown in the National Transplant Organization patients analysed. Proper pre and postoperative prophylaxis and postoperative early extubation protocol is essential to achieve good results.
- Citation: Borro JM, Delgado M, Coll E, Pita S. Single-lung transplantation in emphysema: Retrospective study analyzing survival and waiting list mortality. World J Transplant 2016; 6(2): 347-355
- URL: https://www.wjgnet.com/2220-3230/full/v6/i2/347.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i2.347
The number of solid organ transplantations performed in Spain has steadily increased in the last 20 years from around 1300 in 1989 to over 4000 in 2009[1]. This has been possible thanks to a greater number of donors, achieved as a consequence of a set of organizational measures, known as the “Spanish Model”, directed by the Spanish National Transplant Organization (ONT)[1]. However, this increase in organ donation does not meet all lung transplantation requirements and, as in the rest of the world, organ availability remains the main limitation[2]. The latest data available indicate that 238 lung transplantations, including combined transplantations, were performed in Spain in 2012. Only 48% of candidates on the waiting list were transplanted during this same year[2]. The median time on the waiting list was 163 d in 2011 (interquartile range: 65-303). Waiting list mortality in the same period was 4.6%. Moreover, 2.7% were taken off the waiting list due to clinical worsening[3].
Advanced-stage pulmonary emphysema is the most common indication for lung transplantation[4]. In 2011, 29.5% of advanced emphysema patients were in need of this intervention, 26.2% of whom had chronic obstructive pulmonary disease (COPD) type 1, and 3.3% α1-antitrypsin deficiency[4]. The question remains whether single or double-lung transplantation should be performed[5-9]. Single-lung transplantation (SL) has the advantage of making optimal use of available organs, but some studies indicate better outcomes and survival in patients with double-lung transplant (DL) compared to SL recipients[8,10]. However, SL is often performed in older and retransplanted patients, who generally present with more comorbidities[11]. One of the main problems in SL is native lung hyperinflation[12,13], but minimally invasive techniques such as video-assisted thoracoscopic surgery (VATS)[14] or bronchoscopic lung volume reduction[15,16] are now available and have shown good results. An appropriate clinical protocol implementing these recent developments might help narrow the gap in survival rates of single and DL patients reported in the literature.
Our first goal was to evaluate our group’s 10-year experience in lung transplantation in patients with emphysema, in order to assess and compare survival and outcomes of SL and DL recipients. We further compared and assessed our results against national data available in the Spanish Lung Transplant Registry (RETP), in order to explore the impact of SL or DL on patient survival and waiting list progress, and discuss the consequences of the different approaches.
We conducted a retrospective study of the records of patients transplanted in our center between 2000 and 2012. This study was approved by the Clinical Research Ethics Committee of the Galician Healthcare Authorities overseeing Complejo Hospitalario Universitario A Coruña (CHUAC). All procedures were performed in compliance with Spanish regulations and the Declaration of Helsinki.
Further assessment of our data required comparison with Spanish national registry data. The 7 centers performing lung transplantation in Spain started around the same time; the economic and social status of the population attended is similar in all of them, and all use similar techniques and postoperative care protocols.
Lung transplantation waiting list information (1999 to 2012) on a national level was obtained from the ONT. All Spanish transplantation teams pool their data in the RETP that began its activity in 2001, the first year of complete data availability. Follow up information from patients transplanted between 2001 and 2012 was selected.
Patients were selected for inclusion in the waiting list according to the International Society of Heart Lung Transplantation criteria[17]. Between 2000 and 2003, DL was preferred in emphysema patients < 60 years of age, and SL was reserved for those > 60 years or with comorbidities. However, in view of the good clinical results with SL, we decided in 2003 that SL would be the preferred approach in all cases, including α1-antitrypsin deficiency. According to our protocol, the patient performs physical and respiratory exercises during the waiting period. Postoperative tracheostomy is used when necessary due to prolonged intubation. In addition, SL candidate receive antifungal prophylaxis with weekly amphotericin B lipid complex via aerosol. Patients with a history of recurrent infections also receive tobramycin before surgery[18].
The surgical technique used by our group has not undergone substantial changes since our program began in 1999, and is similar to the recently described[19]. Ventilation difficulties during the immediate postoperative period are critical in SL in emphysema[20]. Patients are routinely extubated in the surgery room, or within the following 6 h whenever possible. This is possible in most cases, but patients requiring assisted ventilation after surgery also benefit from an optimized care protocol, including ventilation with 2 respiratory units.
Immunosuppressive treatment is described elsewhere[18], and consisted of triple therapy including basiliximab for induction, oral or intravenous cyclosporine, azathioprine and decreasing doses of corticosteroids in all cases. Cyclosporine and/or azathioprine were switched to tacrolimus and/or mycophenolate after repeated acute rejection or persistent rejection. All patients received antibacterial prophylaxis with amoxicillin and clavulanic acid, modified after transplantation according to the postoperative cultures of bronchial aspirate. In addition, all patients received antiviral prophylaxis with valganciclovir for 3-6 mo depending on their Cytomegalovirus (CMV) serology risk; antifungal prophylaxis with fluconazole, followed by amphotericin B lipid complex as described elsewhere[21], and trimethoprim with sulfamethoxazole on alternate days were prescribed to prevent infection by Pneumocystis carinii.
Hyperinflation during the long-term postoperative period was treated with surgical or bronchoscopic volume reduction[22].
Transplanted patients (in our center and on the national waiting list) were classified into 2 groups: SL or DL transplantation. Combined transplants were not included.
The total of 73 patients in this single-center analysis (see RESULTS) allows for the detection of a hazard ratio (HR) ≥ 2.6 with a confidence of 95%, and a statistical power of 80%, assuming 56% of censored measurements (percentage of patients alive after 5 years) and 54.7% of exposed patients (percentage of patients receiving DL transplantation). A retrospective analysis of the single-center data was performed comparing the demographic characteristics of the SL and DL groups, followed by univariate analysis to compare the qualitative variables, using the χ2 test and student t-test for quantitative ones. Kaplan-Meier survival curves were compared using the log-rank test. The impact of the type of transplant, infections (cytomegalovirus or bacterial), and acute and chronic rejection on patient survival was determined in the local setting using a Cox multivariate analysis. Statistical analyses were performed with SPSS 16.0. The statistical analyses were review by Professor Salvador Pita, head of biostatistics department and paper coautor.
A total of 280 patients were transplanted in CHUAC between 2000 and 2012, of whom 73 had a previous diagnosis of advanced-stage pulmonary emphysema: 40 underwent SL and 33 received DL. Both groups were comparable in terms of gender and clinical characteristics (Table 1). We found significant differences in the mean age between the groups, the DL patients being younger (Table 1), as expected from the inclusion criteria.
| Study cohort | Single-lung | Double-lung | P-value | |
| n = 73 | n = 40 | n = 33 | ||
| Age in years (mean ± SD) | 54.9 ± 7.1 | 57.3 ± 6.1 | 51.9 ± 7.3 | 0.001 |
| Gender (male) | 62 (85%) | 33 (82.5%) | 29 (87.9%) | 0.520 |
| Underlying disease | 0.940 | |||
| α1-antitrypsin deficiency | 18 (24.6%) | 10 (25%) | 8 (24.2%) | |
| Chronic obstructive pulmonary disease | 55 (75.3%) | 30 (75%) | 25 (75.2%) |
The average preoperative forced expiratory volume in 1 s (FEV1) was 22.89% ± 6.95% (range 12%-49%). The median follow-up of the series was 67.4 mo (range: 0-156.5 mo; interquartile range: 22.4-96.4). Perioperative medical and surgical complications (hemothorax, lung edema, broncho-vascular sutures problems) were reported in 11 patients (27.6%) in the SL group, compared to 18 subjects (54%) in the DL group, which was significantly higher (P = 0.032).
Complications reported during follow-up were similar in both groups (Table 1). Rejection episodes were treated with steroid boluses, combined with a modification of the patient’s immunosuppressive treatment when deemed necessary.
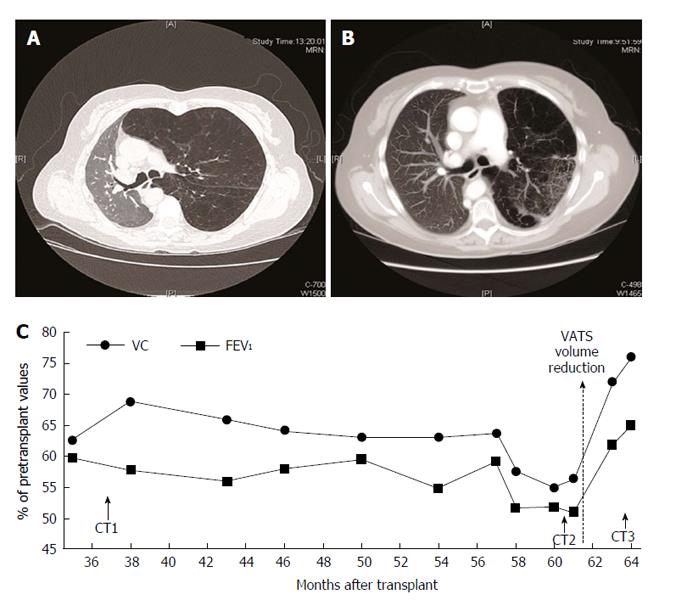
Clinically significant hyperinflation of the native lung was detected in 3 SL patients during the follow-up period. This was diagnosed by worsening respiratory function, decreased %FEV1 compared to initial post-transplant values, and confirmed by high-resolution computed tomography (CT). Transbronchial biopsy was performed to rule out other possible causes of functional deterioration, including bronquiolitis obliterative sindrome (BOS).
Volume reduction surgery by VATS was performed in 2 patients. The first case experienced a significant improvement in functional capacity (Figure 1), recovering pretransplant spirometric values, leading to a clear improvement in the patient’s quality of life. The second patient died 3 wk after the intervention due to sepsis caused by lung infection. The third patient underwent video-assisted bronchoscopic volume reduction. Endobronchial valves were placed in 3 segmental bronchi of the right upper lobe without incidents. Postoperative CT imaging showed atelectasis at this site[22]; the patient experienced clinical improvement from stage 3 to 2 in the Medical Research Council dyspnea functional scale[23], improved exercise tolerance and better quality of life, with no significant changes in spirometry. Lung volume reduction by bullae resection was performed in a fourth patient during the transplantation procedure without incidents.
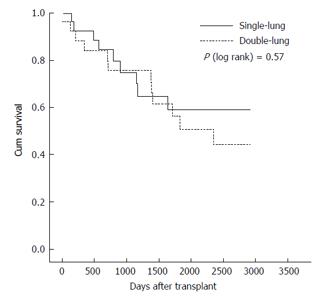
Postoperative mortality (within 30 d after surgery), was significantly higher in DL: 4 patients (5.57%) died in the immediate postoperative period, compared to 2 (2.73%) in the SL group. Regarding survival, 85% of SL patients were alive one year after the intervention, 72.5% 3 years later, and 52.4% after 5 years, and in DL, 78.8%, 66.7% and 51.5% respectively (Figure 2). Survival probabilities are shown in Table 2. There were no significant differences between the 2 survival curves (P = 0.976). Multivariate regression analysis revealed that the type of transplant performed, single or double-lung, was not related to survival (P = 0.802), while age and having COPD as the underlying disease did not reach statistical significance (Table 3). Univariate and multivariate analyses of postoperative complications, presented in Table 4, show that the occurrence of complications was not related to the type of transplant, even after adjustment for age, gender and underlying disease.
| Time until | Single-lung | Double-lung | ||
| transplantation | No. at risk | Survival probability | No. at risk | Survival probability |
| 1 yr | 34 | 85.0% | 26 | 78.8% |
| 2 yr | 31 | 77.5% | 24 | 72.7% |
| 3 yr | 29 | 72.5% | 22 | 66.7% |
| 4 yr | 23 | 57.5% | 20 | 60.6% |
| 5 yr | 20 | 52.4% | 17 | 51.5% |
| B | SE | Wald | P-value | HR | 95%CI HR | |
| Age in years | 0.040 | 0.024 | 2.780 | 0.095 | 1.041 | 0.993-1.091 |
| Gender (female) | 0.475 | 0.391 | 1.481 | 0.224 | 1.609 | 0.748-3.459 |
| Underlying disease (COPD) | 0.737 | 0.407 | 3.278 | 0.070 | 2.088 | 0.941-4.651 |
| Type of transplant (double-lung) | -0.086 | 0.345 | 0.063 | 0.802 | 0.917 | 0.466-1.804 |
| Single-lung n = 40 | Double-lung n = 33 | Univariate analysis | Multivariate analysis1 | ||
| P-value | P-value | OR (95%CI) | |||
| Complications during follow-up | |||||
| Bronchiolitis obliterans syndrome | 22 (55.0) | 16 (48.5) | 0.579 | 0.475 | 0.7 (0.2-1.9) |
| Acute rejection episodes | 18 (45.0) | 18 (54.5) | 0.417 | 0.397 | 1.6 (0.6-4.4) |
| Bacterial respiratory infections | 27 (67.5) | 22 (68.8) | 0.910 | 0.597 | 0.7 (0.2-2.3) |
| CMV infection/disease | 19 (47.5) | 9 (27.3) | 0.077 | 0.104 | 0.4 (0.1-1.2) |
| Fungal infections | 12 (30.0) | 8 (24.2) | 0.583 | 0.807 | 0.9 (0.3-2.7) |
The analyses of waiting-list national data included a total of 1001 patients with emphysema, COPD or alfa-1 antitrypsin deficiency: 343 were SL patients and 658 DL (Table 5).
| Final waiting list status | Total | |||||
| Active | Excluded | Deceased | Transplanted | |||
| SL | No. | 25 | 25 | 9 | 284 | 343 |
| Total SL % | 7.3% | 7.3% | 2.6% | 82.8% | 100.0% | |
| DL | No. | 35 | 51 | 40 | 532 | 658 |
| Total DL % | 5.3% | 7.8% | 6.1% | 80.9% | 100.0% | |
| Total | No. | 60 | 76 | 49 | 816 | 1001 |
| Total % | 6.0% | 7.6% | 4.9% | 81.5% | 100.0% | |
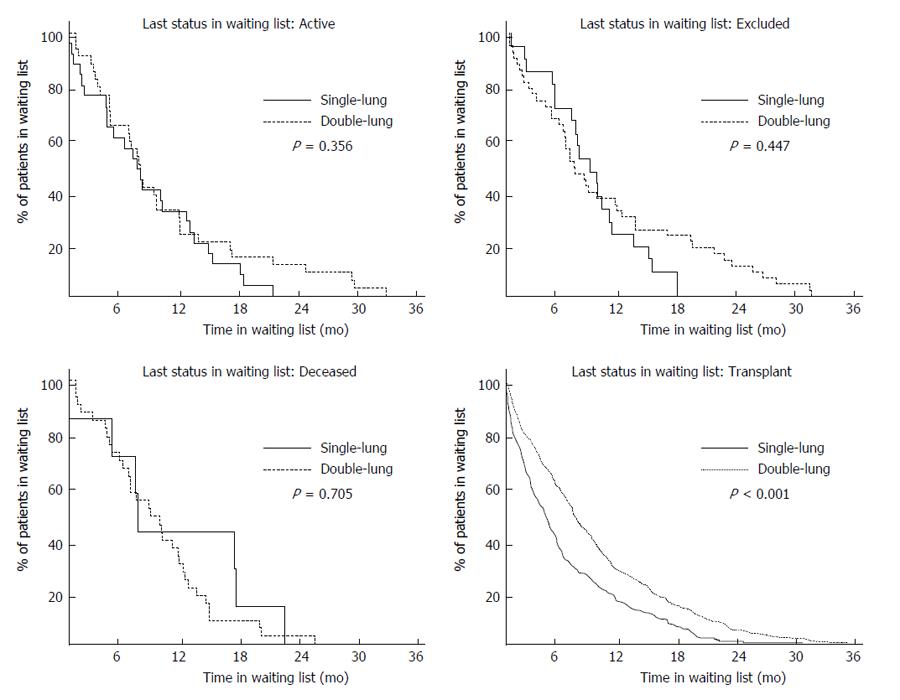
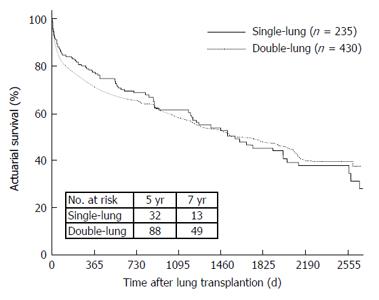
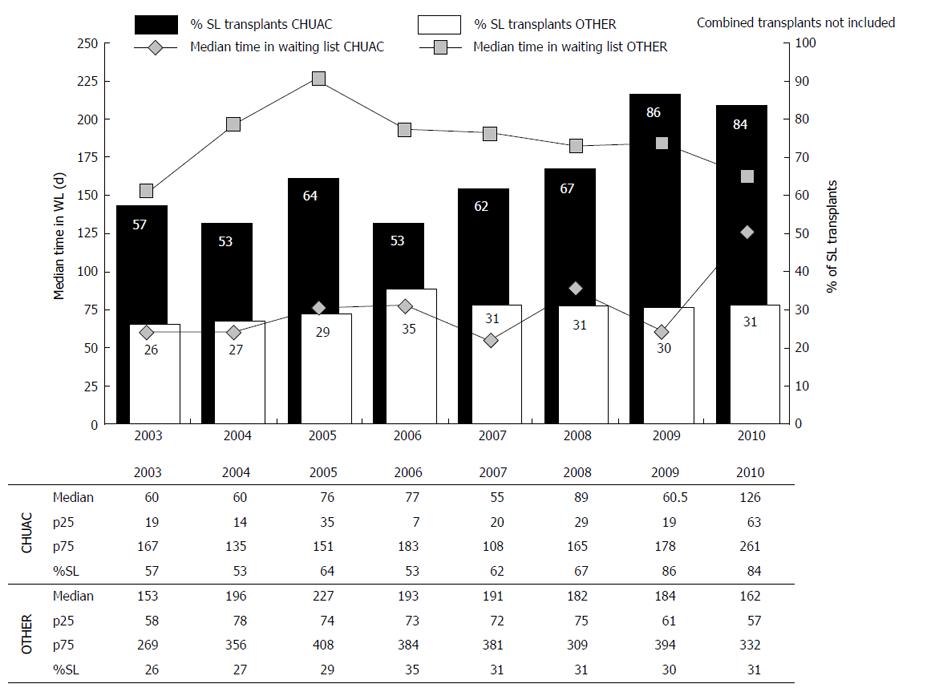
Patient progress in the waiting list differed (P = 0.068) depending on the type of transplant awaited: 83% of those waiting for SL were transplanted, compared to 81% of DL waitlisted. In contrast, waiting list mortality was higher in DL group (6.1% vs 2.6%) (Table 5). In addition, time on the waiting list at national level was longer in the DL than in the SL group (P < 0.001), explained by the fact that patients in the SL group were transplanted earlier (Figure 3). Notably, no significant difference was found in survival-time curves between DL and SL in patients with COPD, emphysema or α1-antitrypsin deficiency in the RETP (P = 0.875), shown in Figure 4.
Several previous studies have compared follow-up results of DL vs SL transplantation for emphysema, and the general conclusion has been that survival rates were better in the former case, at least in youger patients[8,10,11]. However, comparison groups were not homogeneous and confounding factors were often present. Cassivi et al[10] reported 5-year survival rates of 66.7% in DL recipients, vs 44.9% in SL transplanted patients, but most of the younger patients with α1-antitrypsin deficiency had received 2 lungs. We considered the question of age, as Thabut et al[8] concluded in their study that patients aged over 60 years may not have a survival benefit after receiving both lungs, but younger patients presented better survival rates after bilateral lung transplantation[8]. Our single-center series is small compared to those of other reports exploring this topic, with the obvious limitations this brings, but on the other hand, this means that our protocols and surgical techinques were totally homogenous. Multicenter studies are based on large databases that can be inaccurate or incomplete, and details that would have allowed to investigate the mechanisms responsible for greater survival after DL are often missing. For this reason, Thabut et al[8] were unable to differentiate causes of death. Our study shows no differences in terms of complications and survival in DL and SL patients. The benefits of a slightly better long-term survival reported in previous studies for DL recipients could be cancelled out by higher waiting list mortality, if DL is the preferred approach. Our results might be influenced by our preoperative prophylaxis protocol aimed at prevention of native lung colonization, early extubation (frecuentely extubated in the surgical room in SL), appropriate management of ventilation complications during the early postoperative period, and long-term management of hyperinflation. Our aim was to analyse fully comparable groups, and this was achieved in general terms, as can be observed in the demographic and clinical characterization of our series. Although the SL group was older than the DL group, our results showed no difference between the study groups in terms of long-term mortality, nor was morbidity higher in the SL group, as suggested in previous studies. Many authors have advocated bilateral transplantion[7,10-12,24], arguing that native lung hyperinflation may be responsible for poorer results after SL transplantation. In our series, lung volume reduction surgery was performed in 4 patients with generally good results, and increasing numbers of centers are implementing techniques such as VATS and endobronchial valves[25-28]. In the present clinical setting, the possibility of appropriately controlling this complication is high, and, moreover, SL is technically simpler, anatomically less aggressive, and involves shorter total ischemia time[5], which would explain the lower perioperative morbidity and mortality rates in our series. Furthermore, recent techniques such as normothermic ex vivo lung perfusion systems may allow the conservation and transplant of lungs in optimal conditions, likely improving the present results[29,30]. Another possible benefit of SL is the treatment of BOS[31], currently the main limiting factor for survival during follow-up. The therapeutic strategy in SL-transplanted patients is retransplantation in the contralateral side, which has shown lower morbidity and mortality in various series, compared to retransplantation in patients with a previous bilateral transplant[32].
The results of our single-center series suggest that SL and DL transplantation have similar outcomes in terms of survival, but SL recipients presented fewer complications. Although this is a small series, our findings correlate with the data from the national registry. further showing lower mortality on the waiting list, we believe SL transplantation would be the preferable option in the context of organ shortages and waiting lists, as suggested elsewhere[6,9,33,34]. Figure 5 shows how our preference for SL has clearly reduced the median number of waiting list days, compared to the rest of Spanish hospitals performing this procedure. In addition, our policy of performing preferably SL has led to the implementation of the “twinning procedure”, 2 SL performed simultaneously from 1 donor[35]. Twinning in the same hospital has been shown to be feasible with adequate planning, permitting better use of donors and reducing waiting list time and mortality. Our analysis of the data from the Spanish Registry indicates that patient progress on the waiting list is influenced by the type of transplant awaited. Patient survival is associated with the extra waiting time for DL, and advanced patients presenting would clearly benefit from shorter waiting times. Munson et al[34] advocate shortening waiting list times with an optimized allocation program and, specifically, the performance of SL, arguing that bilateral transplantation maximizes the total number of life-years gained post-transplant only when waiting lists are short or if the local survival benefits of DL compared with SL are large[34].
Our study, being small, retrospective and single-center, has several limitations and therefore conclusions drawn must be equally limited. However, it offers a comparison of outcomes of both transplantation possibilities in emphysema, while excluding the possible confounders occurring in multicenter studies, such as different care protocols used in the various hospitals, different surgical tecniques, surgical teams or the lack of complete, validated data, among others. In these conditions, we have observed that the survival of both groups is similar. The postoperative complications in our group, with mortality rates twice those of DL transplant recipients, are consistent with longer and more complex interventions requiring double the number of sutures that increase the risk of complications.
In conclusion, our results suggest that SL could be the best option in the present clinical scenario, and we believe that this should be the treatment of choice in most of emphysema patients. This approach, in our experience, has no impact on patient survival or complications, may alleviate donor organ shortage, and contributes to decreasing morbidity and mortality on the national waiting list. In addition, this approach also allows contralateral transplantation, if needed to solve future complications[36].
The authors thank the staff of the Spanish National Transplant Organization for their collaboration, providing national data and sharing comments and opinions.
Advanced-stage pulmonary emphysema is the most frequent indication for lung transplantation. However, whether single-lung transplantation (SL) or double-lung transplant (DL) transplantation should be performed remains a subject of debate.
It is known that the quality of life in single lung transplantation is usually similar to double lung. Therefore, the shortage of organs and the consequent waiting list mortality encouraged to make unilateral transplantation is emphysema patients since it would reduce waiting list times, if they can provided that long-term survival were similar for both.
These study results show similar survival for uni and bilateral lung transplantation in patients with emphysema, with less immediate postoperative morbidity and mortality. Survival Spanish national register does not show difference between the two techniques too. Likewise, mortality in national waiting list is significantly higher in the group of both lungs. Only infections are more prevalent in the group-lung without statistical significance.
The results obtained reinforce their decision that single lung transplant is the transplantation of choice in most cases of emphysema without bacterial or fungal colonization.
This article is interesting and has a good potential.
P- Reviewer: Hilmi I, Nosotti M, Salvadori M S- Editor: Qiu S L- Editor: A E- Editor: Liu SQ
| 1. | Matesanz R, Domínguez-Gil B, Coll E, de la Rosa G, Marazuela R. Spanish experience as a leading country: what kind of measures were taken? Transpl Int. 2011;24:333-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 145] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 2. | Matesanz R. Newsletter Transplant. International Figures on Donation and Transplantation 2012. Madrid: Organización Nacional de Trasplantes 2013; . |
| 3. | Trasplante Pulmonar en Espana. In: Organizacion Nacional de Transplantes. Spanish Ministry of Health. 2011;. |
| 4. | The ISHLT International Registry for Heart and Lung Transplantation. In: International Society for Heart and Lung Transplantation (ISHLT). 2012;. |
| 5. | Cano JR, Algar FJ, Cerezo F, Moreno P, Espinosa D, Alvarez A, Baamonde C, Santos F, Salvatierra A. Results of lung transplantation in patients with chronic obstructive pulmonary disease. Transplant Proc. 2008;40:3073-3075. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Delgado M, Borro JM, De La Torre MM, Fernández R, González D, Paradela M, García JA, Fieira E, Rama P. Lung transplantation as the first choice in emphysema. Transplant Proc. 2009;41:2207-2209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Hadjiliadis D, Angel LF. Controversies in lung transplantation: are two lungs better than one? Semin Respir Crit Care Med. 2006;27:561-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Thabut G, Christie JD, Ravaud P, Castier Y, Brugière O, Fournier M, Mal H, Lesèche G, Porcher R. Survival after bilateral versus single lung transplantation for patients with chronic obstructive pulmonary disease: a retrospective analysis of registry data. Lancet. 2008;371:744-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 134] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 9. | Lederer DJ, Arcasoy SM. Two, one, or none for chronic obstructive pulmonary disease: who decides and how? Am J Respir Crit Care Med. 2011;184:1226-1227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Cassivi SD, Meyers BF, Battafarano RJ, Guthrie TJ, Trulock EP, Lynch JP, Cooper JD, Patterson GA. Thirteen-year experience in lung transplantation for emphysema. Ann Thorac Surg. 2002;74:1663-1669; discussion 1669-1670. [PubMed] |
| 11. | Meyer DM, Bennett LE, Novick RJ, Hosenpud JD. Single vs bilateral, sequential lung transplantation for end-stage emphysema: influence of recipient age on survival and secondary end-points. J Heart Lung Transplant. 2001;20:935-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 106] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Mal H, Brugière O, Sleiman C, Rullon I, Jebrak G, Groussard O, Reffas T, Stern JB, Lesèche G, Fournier M. Morbidity and mortality related to the native lung in single lung transplantation for emphysema. J Heart Lung Transplant. 2000;19:220-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Samano MN, Junqueira JJ, Teixeira RH, Caramori ML, Pêgo-Fernandes PM, Jatene FB. [Lung hyperinflation after single lung transplantation to treat emphysema]. J Bras Pneumol. 2010;36:265-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | McKenna RJ, Benditt JO, DeCamp M, Deschamps C, Kaiser L, Lee SM, Mohsenifar Z, Piantadosi S, Ramsey S, Reilly J. Safety and efficacy of median sternotomy versus video-assisted thoracic surgery for lung volume reduction surgery. J Thorac Cardiovasc Surg. 2004;127:1350-1360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 57] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Geddes D, Davies M, Koyama H, Hansell D, Pastorino U, Pepper J, Agent P, Cullinan P, MacNeill SJ, Goldstraw P. Effect of lung-volume-reduction surgery in patients with severe emphysema. N Engl J Med. 2000;343:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 250] [Cited by in RCA: 235] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 16. | Huang W, Wang WR, Deng B, Tan YQ, Jiang GY, Zhou HJ, He Y. Several clinical interests regarding lung volume reduction surgery for severe emphysema: meta-analysis and systematic review of randomized controlled trials. J Cardiothorac Surg. 2011;6:148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Trulock EP. Lung Transplantation for COPD. Chest. 1998;113:269S-276S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Borro JM. Advances in immunosuppression after lung transplantation. Med Intensiva. 2013;37:44-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Boasquevisque CH, Yildirim E, Waddel TK, Keshavjee S. Surgical techniques: lung transplant and lung volume reduction. Proc Am Thorac Soc. 2009;6:66-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Pilcher DV, Auzinger GM, Mitra B, Tuxen DV, Salamonsen RF, Davies AR, Williams TJ, Snell GI. Predictors of independent lung ventilation: an analysis of 170 single-lung transplantations. J Thorac Cardiovasc Surg. 2007;133:1071-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Borro JM, Solé A, de la Torre M, Pastor A, Fernandez R, Saura A, Delgado M, Monte E, Gonzalez D. Efficiency and safety of inhaled amphotericin B lipid complex (Abelcet) in the prophylaxis of invasive fungal infections following lung transplantation. Transplant Proc. 2008;40:3090-3093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Pato O, Rama P, Allegue M, Fernández R, González D, Borro JM. Bronchoscopic lung volume reduction in a single-lung transplant recipient with natal lung hyperinflation: a case report. Transplant Proc. 2010;42:1979-1981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 23. | Stenton C. The MRC breathlessness scale. Occup Med (Lond). 2008;58:226-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 244] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 24. | Weill D, Keshavjee S. Lung transplantation for emphysema: two lungs or one. J Heart Lung Transplant. 2001;20:739-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Shen Y, Chen JY, Wei YC, Luo YR, Xu LH, Liu YZ, Yuan L. [Single lung transplantation with concomitant contralateral lung volume reduction for end- stage emphysema]. Nanfang Yike Daxue Xuebao. 2007;27:895-896. [PubMed] |
| 26. | Reece TB, Mitchell JD, Zamora MR, Fullerton DA, Cleveland JC, Pomerantz M, Lyu DM, Grover FL, Weyant MJ. Native lung volume reduction surgery relieves functional graft compression after single-lung transplantation for chronic obstructive pulmonary disease. J Thorac Cardiovasc Surg. 2008;135:931-937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Arango E, Espinosa D, Illana J, Carrasco G, Moreno P, Algar FJ, Alvarez A, Cerezo F, Baamonde C, Requejo A. Lung volume reduction surgery after lung transplantation for emphysema-chronic obstructive pulmonary disease. Transplant Proc. 2012;44:2115-2117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 28. | Wilson H, Carby M, Beddow E. Lung volume reduction surgery for native lung hyperinflation following single-lung transplantation for emphysema: which patients? Eur J Cardiothorac Surg. 2012;42:410-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Warnecke G, Moradiellos J, Tudorache I, Kühn C, Avsar M, Wiegmann B, Sommer W, Ius F, Kunze C, Gottlieb J. Normothermic perfusion of donor lungs for preservation and assessment with the Organ Care System Lung before bilateral transplantation: a pilot study of 12 patients. Lancet. 2012;380:1851-1858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 161] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 30. | Borro JM. New methods to facilitate lung transplantation. Lancet. 2012;380:1799-1801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Brugière O, Thabut G, Castier Y, Mal H, Dauriat G, Marceau A, Lesèche G. Lung retransplantation for bronchiolitis obliterans syndrome: long-term follow-up in a series of 15 recipients. Chest. 2003;123:1832-1837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Kon ZN, Bittle G, Wehman B, Griffith BP, Pierson Iii RN. 50 Ipsilateral, Contralateral, or Double? Procedure Incidence and Associated Outcomes in a Retrospective UNOS Review of Re-Transplantation Following Prior Single Lung Transplantation. J Heart Lung Transplant. 2012;31:S26. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 33. | Rinaldi M, Sansone F, Boffini M, El Qarra S, Solidoro P, Cavallo N, Ruffini E, Baldi S. Single versus double lung transplantation in pulmonary fibrosis: a debated topic. Transplant Proc. 2008;40:2010-2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 34. | Munson JC, Christie JD, Halpern SD. The societal impact of single versus bilateral lung transplantation for chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2011;184:1282-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 35. | de la Torre MM, Borro JM, Fernández R, González D, Delgado M, Paradela M, García JA, Lemos C. Results of “twinning procedure” in lung transplantation: experience in a single center. Transplant Proc. 2009;41:2213-2215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 36. | Sakornpant P, Kasemsarn C, Yottasurodom C. Retransplantation after single lung transplantation. Transplant Proc. 2008;40:2617-2619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |