Published online Jun 24, 2016. doi: 10.5500/wjt.v6.i2.272
Peer-review started: October 21, 2015
First decision: December 28, 2015
Revised: April 2, 2016
Accepted: April 14, 2016
Article in press: April 18, 2016
Published online: June 24, 2016
Processing time: 247 Days and 3.9 Hours
Accurate dissection of the hepatoduodenal ligament in the recipient is vital for the success of liver transplantation surgery. High incidence of anatomic variations at the hepatic artery, portal vein and biliary ducts in the hepatoduodenal ligament is well known. Surgical experience is important to be able to foresee the most common anatomic diversities and the possible variations, in order to make a safe and accurate dissection in the hepatic hilum. Before anastomosis, all these hilar structures must be well identified, safely dissected and must also have a sufficient length for the coming implantation process. At the beginning of our program, we were starting the hepatic hilum dissection close to the liver. In time, however, we modified our surgical technique, preferring to start further away from the liver (closer to the duodenum). This length increased progressively over 1500 liver transplantations (80% living donor liver transplantation). During this process, our main purpose was the early control of the hepatic artery (artery first approach). In this paper, our aim is to share our latest version of the hepatoduodenal ligament dissection technique. We also describe alternative approaches used in extraordinary situations.
Core tip: The hepatic artery is one of the main components of the hepatoduodenal ligament and exhibits high anatomic variability, which may change the outcome and success of liver transplantation. In our experience, early control of the hepatic artery (artery first approach) and by the guidance of the hepatic artery, dissection of the rest of the hepatoduodenal ligament components is more practical. In this paper, we share our latest version of the hepatoduodenal ligament dissection technique, developed over the course of 1500 liver transplantations (80% living donor liver transplantation) in our clinic.
- Citation: Kayaalp C, Tolan K, Yilmaz S. Hepatoduodenal ligament dissection technique during recipient hepatectomy for liver transplantation: How I do it? World J Transplant 2016; 6(2): 272-277
- URL: https://www.wjgnet.com/2220-3230/full/v6/i2/272.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i2.272
The Mercedes incision is probably the most widely preferred incision technique for liver transplantation in the world. When we first started performing liver transplantations, we used the Mercedes incision as well. However, we observed a high incidence of incisional hernia with this technique[1]. In time, we reduced the size of the incision and started to use the “reverse L” right upper quadrant incision. Nowadays, we prefer the Mercedes incision only in special occasions (obesity, extensive adhesions due to previous surgery). The extension of “reverse L” incision on the right should extend laterally enough to permit the exposure of the segment VI of the liver. The tip of the incision on the midline extends up to the xiphoid process, high enough for exposure of the supra-hepatic vena cava. In some selected patients, we performed the liver transplantation only through a supra-umbilical median incision[2]. After laparotomy, the falciform ligament is divided, trimmed and ligated. A sternum lifting mechanical retractor is placed after the suturing of the skin flap to the drape on the right.
The left triangular ligament is divided and the gastro-hepatic ligament is examined for an accessory left hepatic artery (HA) arising from the left gastric artery; if there is one, it should first be controlled by a vascular bulldog clamp and then cut close to the liver. We do not prefer to use ligamentum Teres for traction of a cirrhotic liver, which usually tends to bleed from the liver capsule during traction. To achieve better exposure of the hepatoduodenal ligament in a cirrhotic liver, we prefer to first mobilize the right lobe of the liver and place a large piece of gauze behind the liver to move the hepatoduodenal ligament anteriorly. In other words, we position the hepatoduodenal ligament closer to the surgeon. Mobilization of the right liver lobe at the beginning of the procedure provides exposure of the retro-hepatic vena cava at full length. This also allows for total hepatic vascular occlusion when necessary, particularly in emergency conditions. One or two blades of the automatic liver retractors are placed on the visceral surface of the right and/or left lobes of the liver. Then we can easily and clearly expose the hepatoduodenal ligament. A dilated gall bladder may sometimes lay over the hepatoduodenal ligament, preventing good exposure, and its tractions can result in hemorrhage from the liver capsule. In these situations, a partial cholecystectomy may be useful[3].
At the beginning of our liver transplantation program, we began the hepatoduodenal ligament dissection as close as possible to the liver. This was done to avoid injuries to the proximal parts of the components of the hepatoduodenal ligament. However, we experienced some difficulties while working closer to the liver hilum. At first, it was difficult to perform a dissection in such a small area and increased risk of liver capsule bleeding. Secondly, there was difficulty in identifying the arteries from their distal ends, and we observed more intimal injuries during the dissection of these small caliber arteries if there was no proximal vascular control by a vascular bulldog clamp.
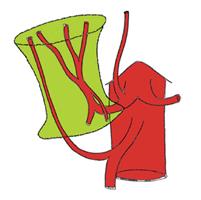
HA is one of the three main components of the hepatoduodenal ligament. It has the highest rates of variation, which may change the outcome and success of the liver transplantation. The surgeon performing the recipient hepatectomy is responsible for the protection of all the arteries that may have a potential use during the implantation process. It is obvious that the arteries that must be protected during the dissection are not limited to two (right and left). In every case, five potential arteries (right, left, segment IV, right HA from the superior mesenteric artery, left HA from the left gastric artery, Figure 1) must be encountered. In our experience, early control of the hepatic artery (artery first approach) and by the guidance of it, dissection of the rest of the hepatoduodenal ligament components is more practical.
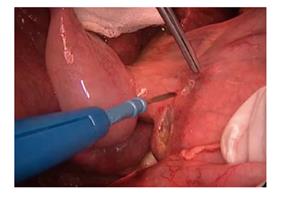
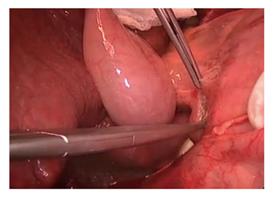
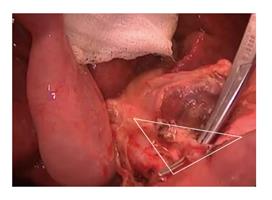
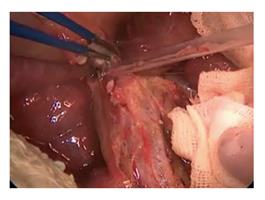
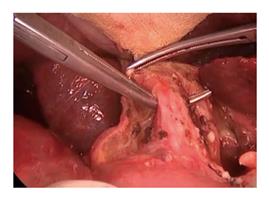
The hepatoduodenal dissection is started just above the duodenal margin (Figure 2). We proceed from laterally to medially with the ligation of the peritoneum and the vessels under the peritoneum (Figures 3 and 4). Trimming of the anterior-inferior leaf of the hepatoduodenal ligament makes it possible to identify the common bile duct with the help of 3 and 9 o’clock vessels. The direction of the dissection is towards the common HA, which is the main point of our hilar dissection at this stage. Above the duodenum, while dissecting medially, the right gastric artery that arises from the hilum and travels to the stomach must be ligated and transected. Inexperienced surgeons may worry about transecting this artery for fear of harming the common HA. However, the right gastric artery is more superficial than the HA, and it runs to the stomach and not into the hepatoduodenal ligament.
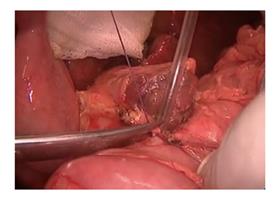
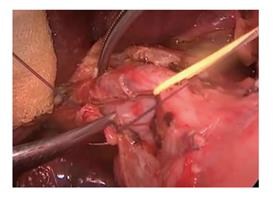
On the medial side of the hepatoduodenal ligament, just above the duodenum, the largest lymph node of the superficial hepatoduodenal lymph nodes can be seen (Figures 5 and 6). This lymph node is located on the trace of the common HA, acting as a landmark for hilar dissection. Once this lymph node is identified, it should be removed carefully after palpation of the common HA under this lymph node. In terms of the newest hemostatic technologies, like Ligasure or Ultrascission[4], we generally prefer to use the suture ligation with low voltage adjusted (25 Watt) monopolar and bipolar electrocautery for hepatoduodenal ligament dissection. Clamps and scissors can also be used for dissection of the common HA to avoid intimal injury due to thermal effects. The common HA is separated from the upper border of the pancreas and completely mobilized. At this stage, the gastroduodenal artery is searched for in the triangle formed by the medial aspect of the distal common bile duct, the trace of the HA, and the upper side of the duodenum (Figure 7). Ligation and transection of the gastroduodenal artery makes the portal vein visible just beneath it (Figures 8 and 9). After this step, the main three components of the hepatoduodenal ligament can be partly identified. We place an atraumatic bulldog clamp to the common HA to decrease the intraluminal pressure in the arterial lumen and to prevent intimal dissection[5] (Figure 10). The gastroduodenal artery is usually divided for several reasons, such as prolonging the HA for a living donor liver transplantation, avoiding steal syndrome through the gastroduodenal artery, and performing an arterial anastomosis to the bifurcation of the gastroduodenal artery and common HA during a deceased liver transplantation.
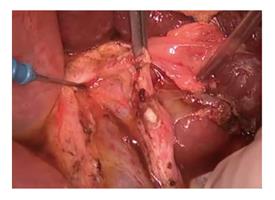
Generally, there are no main branches arising on the anterior side of the common HA. This knowledge is particularly valuable when dissecting of the hepatoduodenal ligament by the arterial route. Hanging the tissues on the common HA with the help of a right-angle clamp and cutting them via electrocautery will help in visualizing the distal branches of the proper HA. This dissection meticulously moves toward the bifurcations of the right, left and segment IV hepatic arteries. There may be some small arterial branches going toward the lymph nodes. However, because the common HA is clamped by a bulldog, these will not cause any major bleedings. Even so, it is advisable to perform careful dissection to prevent hemorrhage. The left HA and segment segment IV hepatic arteries artery should be followed as far as their entrance into the liver parenchyma. The spatial relationship between the right HA and the bile duct should be evaluated. Generally, the right HA crosses posterior to the common bile duct (Figure 11). However, it sometimes crosses anteriorly and we cut this HA as closely as possible to the liver and continue on to bile duct dissection later. If the right HA is passing posteriorly, then the common bile duct dissection can be started before arterial transections.
The cystic duct is identified, clipped and divided. The common bile duct and ductus choledochus can be identified with the help of the up traction of the cystic duct stump (Figure 12). The lateral side of the common hepatic duct is dissected caudally and cranially.
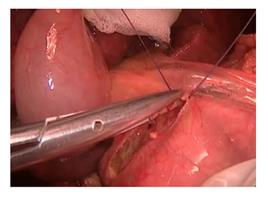
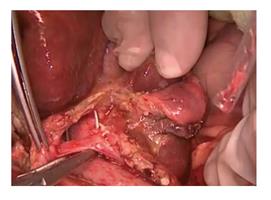
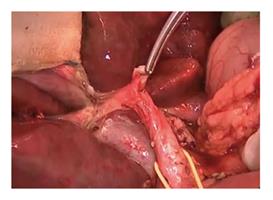
For better and safer exposure of the extra-hepatic bile ducts, we peel back the peritoneal sheet that covers the common bile duct, starting from the side of the duodenum and moving to the liver hilum. In our daily surgical practice, we call this “undressing the coat” of the hepatoduodenal ligament. This allows us to safely go underneath the hilar plate that covers the main anatomic contents of the portal hilum. Here, so as not to damage the vascular supply of the choledochus AA and common bile duct, bleeding must be controlled with fine suturing (Figure 13). In this way, the 3 and 9 o’clock arteries become more visible. These are the landmarks for the medial and the lateral margins of the common bile duct. The common bile duct can be lifted using a right-angle clamp (Figure 14). The peri-choledochal plexus supplying the bile ducts from the 3 and 9 o’clock arteries should be preserved. Electrocautery and excessive skeletonization must be avoided here in order to preserve the blood supply of the remnant bile duct, preventing future anastomosis strictures[6]. The remaining tissues along the lateral part of the common bile duct and the portal vein should be divided (Figure 15). However, if there is an accessory right HA arising from the superior mesenteric artery, the surgeon must be careful not to harm it. We prefer to dissect all the lymph nodes around the hepatoduodenal ligament. In this way, the portal vein, bile duct and arteries can be better identified. It also preserves the length of bile duct, arterial branches and the portal vein, which is particularly important for living donor liver transplantations (Figure 16).
After identification of all hilar contents, we first cut the HA and then the main bile duct as closely as possible to the liver. The portal vein is then cut just before the un-hepatic phase. In cases in which the hepatoduodenal ligament cannot be dissected easily due to fibrosis or adhesions, we use alternative techniques. In such cases, we perform a double Pringle’s maneuver to control the hepatoduodenal ligament, and then resect the ligament together with the contents as closely to the liver as possible. Next, we try to retrospectively identify the contents one by one. Once all of the contents have been identified, the Pringle’s maneuvers are released. Also, in cases of portal vein thrombosis, we make available a Foley urinary catheter on the operating table for any unexpected bleeding from the porto-mesenteric veins during endovenectomy[7].
Experience and expertise, especially in the surgical field, where many variations can be seen, is extremely important for performing safe and successful dissection. We are still improving our technique for recipient hepatectomy day by day. We hope that these technical details will be helpful to our colleagues dealing with the liver transplantation and hepatobiliary surgery.
P- Reviewer: Hilmi I, Konigsrainer A S- Editor: Qiu S L- Editor: A E- Editor: Liu SQ
| 1. | Ozgor D, Dirican A, Ates M, Yilmaz M, Isik B, Yilmaz S. Incisional hernia in recipients of adult to adult living donor liver transplantation. World J Surg. 2014;38:2122-2125. |
| 2. | Kayaalp C, Aydin C, Unal B, Baskiran A, Ozgor D, Aydinli B, Yilmaz S. Liver transplantation from an upper midline incision. Exp Clin Transplant. 2011;9:273-276. |
| 3. | Ara C, Ozdemir F, Ateş M, Ozgör D, Kutlutürk K. Partial cholecystectomy: a technique that makes hilar dissection easier in recipient hepatectomy. Transplant Proc. 2014;46:216-218. |
| 4. | Olmez A, Karabulut K, Aydin C, Kayaalp C, Yilmaz S. Comparison of harmonic scalpel versus conventional knot tying for transection of short hepatic veins at liver transplantation: prospective randomized study. Transplant Proc. 2012;44:1717-1719. |
| 5. | Duffy JP, Hong JC, Farmer DG, Ghobrial RM, Yersiz H, Hiatt JR, Busuttil RW. Vascular complications of orthotopic liver transplantation: experience in more than 4,200 patients. J Am Coll Surg. 2009;208:896-903; discussion 903-905. |
| 6. | Vellar ID. Preliminary study of the anatomy of the venous drainage of the intrahepatic and extrahepatic bile ducts and its relevance to the practice of hepatobiliary surgery. ANZ J Surg. 2001;71:418-422. |
| 7. | Aydin C, Ersan V, Baskiran A, Unal B, Kayaalp C, Yilmaz S. Controlling massive hemorrhage from the retropancreatic portal vein as a complication of thromboendovenectomy during liver transplantation with balloon catheter tamponade: how to do it. Surg Today. 2014;44:792-794. |