Published online Mar 24, 2016. doi: 10.5500/wjt.v6.i1.233
Peer-review started: August 21, 2015
First decision: October 30, 2015
Revised: January 20, 2016
Accepted: February 14, 2016
Article in press: February 16, 2016
Published online: March 24, 2016
Processing time: 212 Days and 5.8 Hours
AIM: To investigate outcomes and predictors of in-hospital morbidity and mortality after total pancreatectomy (TP) and islet autotransplantation.
METHODS: The nationwide inpatient sample (NIS) database was used to identify patients who underwent TP and islet autotransplantation (IAT) between 2002-2012 in the United States. Variables of interest were inherent variables of NIS database which included demographic data (age, sex, and race), comorbidities (such as diabetes mellitus, hypertension, and deficiency anemia), and admission type (elective vs non-elective). The primary endpoints were mortality and postoperative complications according to the ICD-9 diagnosis codes which were reported as the second to 25th diagnosis of patients in the database. Risk adjusted analysis was performed to investigate morbidity predictors. Multivariate regression analysis was used to identify predictors of in-hospital morbidity.
RESULTS: We evaluated a total of 923 patients who underwent IAT after pancreatectomy during 2002-2012. Among them, there were 754 patients who had TP + IAT. The most common indication of surgery was chronic pancreatitis (86%) followed by acute pancreatitis (12%). The number of patients undergoing TP + IAT annually significantly increased during the 11 years of study from 53 cases in 2002 to 155 cases in 2012. Overall mortality and morbidity of patients were 0% and 57.8 %, respectively. Post-surgical hypoinsulinemia was reported in 42.3% of patients, indicating that 57.7% of patients were insulin independent during hospitalization. Predictors of in-hospital morbidity were obesity [adjusted odds ratio (AOR): 3.02, P = 0.01], fluid and electrolyte disorders (AOR: 2.71, P < 0.01), alcohol abuse (AOR: 2.63, P < 0.01), and weight loss (AOR: 2.43, P < 0.01).
CONCLUSION: TP + IAT is a safe procedure with no mortality, acceptable morbidity, and achieved high rate of early insulin independence. Obesity is the most significant predictor of in-hospital morbidity.
Core tip: Total pancreatectomy (TP) is the last resort to control the severe pain in patients with chronic pancreatitis due to the morbidity of the operation and the frequent severe resultant diabetes. Islet auto-transplantation (IAT) following TP is reported, by well experienced groups, to be an effective therapy to prevent post-surgical diabetes. However, there is limited nationwide data analysis during the last few decades. The objective of this study was to investigate outcomes and predictors of in-hospital morbidity and mortality after TP + IAT.
- Citation: Fazlalizadeh R, Moghadamyeghaneh Z, Demirjian AN, Imagawa DK, Foster CE, Lakey JR, Stamos MJ, Ichii H. Total pancreatectomy and islet autotransplantation: A decade nationwide analysis. World J Transplant 2016; 6(1): 233-238
- URL: https://www.wjgnet.com/2220-3230/full/v6/i1/233.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i1.233
Chronic pancreatitis (CP) is a progressive inflammation of the pancreas resulting in irreversible damage of the pancreas structure and function. CP has a broad spectrum of symptoms ranging from steatorrhea and malabsorption to diabetes and abdominal pain[1]. Managing the symptoms is critical in order to provide optimum treatment. Any uncontrolled symptoms may hinder the treatment approach, affecting a patient’s quality of life and activity. Diabetes and malabsorption can be managed by insulin and oral pancreatic enzyme supplements respectively; however, the primary challenge is pain management[2]. Although multiple factors and mechanisms have been hypothesized and investigated, the pathogenesis of the pain in CP remains unknown[3]. Therapeutic options for the pain are limited but include extensive surgery, less invasive endoscopic procedures, and medical management. Although an aggressive approach, partial or total pancreatectomy (TP) is on occasion, the only therapeutic option that can provide complete relief in patients with severe pain that could not be alleviated by other treatments[4-7].
Although the utilization of pancreatectomy in patients with CP show positive results in managing pain, there are various unsolicited complications associated with the procedure. Exocrine insufficiency and surgical diabetes have been identified as the most significant complications. Islet autotransplantation (IAT) combined with total or partial pancreatectomy can be effective in preventing or minimizing surgical diabetes[8-11]. The surgical technique includes TP and pylorus- and distal-sparing duodenectomy with orthotopic reconstruction by means of duodenostomy and choledochoduodenostomy. During TP, the blood supply to the pancreas should be preserved as long as possible to lessen the effects of warm ischemia on the islets. To do so, never separate the distal pancreas from the splenic vessels. If the splenic vessels are ligated in the hilum, the spleen may survive on its collateral vessels, but usually it has to be taken[9].
The utilization of IAT following the surgical procedure of TP was introduced by Sutherland et al[12] in 1977. Since then, several centers have followed this dual procedure in patients with CP[13-17]. After pancreas excision, the duodenum and spleen (if attached) were removed on the back table. Purified enzyme blend (collagenase) was injected to the pancreatic main duct to separate islet from pancreatic tissue using modified Ricordi method. Then, digested pancreatic tissue with islets were infused into liver through the portal vein[10]. Because this dual procedure is surgically quite different from simple TP, the morbidity rate and related risks differ. Therefore, the morbidity rate for this procedure will be higher than simple TP procedure[7,18,19].
Despite the higher morbidity rate, several studies have reported that TP + IAT procedure produces significant pain relief, reduced narcotic dependency, and decreased life-threatening hypoglycemic episodes. These benefits support the primary goal of utilizing this treatment[7,20-22].
In the last few decades, no nationwide retrospective analysis of the trends and short term outcomes of TP + IAP have been reported. To our knowledge, this is the first research study to use nationwide inpatient sample (NIS) database to report the most common indications, short term outcomes, and predictors of in-hospital morbidities of patients who underwent combined TP and IAT in the United States.
A retrospective analysis of the NIS database from 2002 through 2012 was performed for this study. NIS is the largest inpatient care database in the United States maintained by the Agency for Healthcare Research. It is an annually compiled database containing information on more than 8 million hospital admissions each year, which represents 20% of all United States hospital discharges to calculate population estimates[23]. The informed consent was obtained from individual patients within the individual hospital’s patient consent forms by NIS. This study evaluated patients who underwent IAT and TP according to the International Classification of Diseases, 9th Revision, clinical modifications (ICD-9-CM) procedure codes of 52.84 and 52.6 during 2002-2012. We extracted all the patients who had undergone IAT from database, then we selected patients who also had TP. Patients’ diagnoses of surgery were extracted using ICD-9-CM diagnosis codes of 577.1 for CP and 577.0 for acute pancreatitis (AP).
Variables of interest were inherent variables of NIS database which included demographic data (age, sex, and race), comorbidities (such as diabetes mellitus, hypertension, and deficiency anemia), and admission type (elective vs non-elective). The primary endpoints were mortality and postoperative complications according to the ICD-9 diagnosis codes which were reported as the second to 25th diagnosis of patients in the database. Risk adjusted analysis was performed to investigate morbidity predictors.
Statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) software, Version 22 (SPSS Inc., Chicago, IL). The main analysis was multivariate analysis using logistic regression. The associations of morbidity with the variable of interest were examined using a multivariable logistic regression model. We included all the potential confounder variables in the model as covariates which were all variables of the study. The estimated adjusted odds ratio (AOR) with a 95%CI was calculated. The level of significance was set at P < 0.05.
We identified 923 patients who underwent IAT during 2002-2012. Among them, there were 754 patients who had TP and IAT. The mean and median patient age were 39 ± 13 and 41 years old respectively; the majority of the patients were Caucasian (88%) and female (68.3%). Overall, 87.7% of patients were operated electively. The most common comorbidity was diabetes mellitus (26.8%) followed by hypertension (25%). Also, 20.4% of patients had anemia prior the operation. The most common indication of TP was CP (86%) followed by acute pancreatitis (12%). The mean hospitalization length of patients was sixteen days. Demographics and clinical characteristics of patients are shown in Table 1.
| Variables | TP and islet auto-transplantation (sample size = 754) | |
| Age | Mean ± SD (yr) | 39 ± 13 |
| Median (yr) | 41 | |
| Sex | Female | 513 (68%) |
| Race | White | 260/295 (88%)1 |
| Black or African American | 20/295 (6.7%)1 | |
| Hispanic | 5/295 (1.6%)1 | |
| Asian | 5/295 (1.6%)1 | |
| Other | 5/295 (1.6%)1 | |
| Comorbidity | Diabetes mellitus | 202 (26.8%) |
| Hypertension | 188 (25%) | |
| Deficiency anemia | 153 (20.4%) | |
| Chronic pulmonary disease | 98 (13.1%) | |
| Drug abuse | 88 (11.7%) | |
| Coagulopathy | 63 (8.3%) | |
| Alcohol abuse | 44 (5.9%) | |
| Obesity | 25 (3.3%) | |
| Weight loss | 22 (29.l3%) | |
| Admission type | Elective | 660 (87.7%) |
| Non-elective | 93 (12.3%) | |
| Patient diagnosis/indication of surgery | Chronic pancreatitis | 648 (86%) |
| Acute pancreatitis | 90 (12%) | |
| Other diagnosis | 15 (2.1%) | |
| Other factors | Preoperative fluid and electrolyte disorders | 216 (28.7%) |
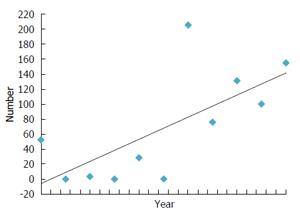
There was a steady increase in number of patients who underwent TP + IAT during 2002-2012 (Figure 1). The number of patients increased from 53 in 2002 to 155 cases in 2012. Also, the number of procedures was significantly higher during 2008-2012 compared to 2002-2007 (667 vs 87, P < 0.01). The overall mortality and morbidity of patients who underwent TP + IAT was 0% and 57.8% respectively (Table 2).
| Complications | Rate |
| Mortality | 0 (0%) |
| Overall morbidity | 435 (57.8%) |
| Post surgical hypoinsulinemia | 318 (42.3%) |
| Acute renal failure | 90 (12%) |
| Wound infection | 63 (8.4%) |
| Pneumonia | 56 (7.4%) |
| Hemorrhagic complications | 50 (6.6%) |
| Peritoneal abscess | 34 (4.5%) |
| Thrombosis of portal vein | 25 (3.3%) |
| Acute myocardial infarction | 15 (2%) |
| Wound disruption | 14 (1.9%) |
| Acute respiratory failure | 10 (1.3%) |
| Thromboembolic complications | 10 (1.3%) |
| Deep vein thrombosis | 1 |
| Biliary stricture | 1 |
Post-surgical hypoinsulinemia was reported in 42.3% of patients, indicating 57.7% of patients were insulin independent during hospitalization. Also, 8.4% of patients had wound infections (Table 2).
Risk adjusted analysis of factors associated with morbidity of patients is reported in Table 3. Patients with obesity (AOR: 3.02, P < 0.01), preoperative fluid and electrolyte disorders (AOR: 2.71, P < 0.01), alcohol abuse (AOR: 2.63, P < 0.01), and weight loss (AOR: 2.43, P = 0.03) had significantly higher morbidity risk.
| Variables | Adjusted odds ratio | 95%CI | P value | |
| Age | Age | 1.01 | 1.01-1.02 | 0.82 |
| Sex | Female | 1.95 | 1.30-2.94 | < 0.01 |
| Comorbidity | Diabetes mellitus | 1.06 | 0.68-1.63 | 0.78 |
| Hypertension | 0.70 | 0.45-1.08 | 0.11 | |
| Deficiency anemia | 0.85 | 0.57-1.27 | 0.43 | |
| Chronic pulmonary disease | 0.56 | 0.34-0.91 | 0.19 | |
| Drug abuse | 0.55 | 0.33-0.93 | 0.27 | |
| Coagulopathy | 1.24 | 0.63-2.44 | 0.52 | |
| Alcohol abuse | 2.63 | 1.23-5.63 | 0.01 | |
| Obesity | 3.02 | 1.00-9.11 | 0.049 | |
| Weight loss | 2.43 | 1.64-3.60 | < 0.01 | |
| Other factors | Preoperative fluid and electrolyte disorders | 2.71 | 1.79-4.09 | < 0.01 |
CP is associated with severe pain that may cause serious effects on a patient’s quality of life and activity. TP has been established as the last resort for patients with refractory chronic pain. However, many studies have shown significant improvements in patient quality of life, as well as reduction of narcotic use[24-26]. The combination of TP + IAT allows removal of the entire diseased gland while minimizing the risk of surgical diabetes. Post-operative narcotic use, insulin use, and standardized pain assessments have been reported by several groups, however the data on risks and morbidities of TP + IAT were limited to single-institution series. In addition, a large scale analysis of nationwide patients has not yet been reported[7,20,21,25].
This study focuses on morbidity rates and short-term outcomes of the patients during hospitalization. The data showed an overall morbidity of 57.8%, which is consistent with data reported in existing literature that have shown morbidity in 58%-69% of patients[7,21,24]. Despite a high morbidity, the mortality rate was 0% in patients with TP + IAT when compared to other studies where the rate indicated 0%-3.5%[7,22,27]. The zero mortality rate can be explained by the fact that NIS database exclusively contains patient information only while they are hospitalized. Therefore, the data for mid-term and long-term complications are not available in the NIS. Among comorbid conditions, we found obesity to have the strongest association with morbidity of patients who underwent TP + IAT. Obesity alone is a significant risk factor for many surgical complications such as wound infection, blood loss, and a longer operation time[28]. On the other hand, many clinical studies have shown that obesity may contribute to recovering more viable islets from pancreas isolation and achieving better metabolic control when compared to lean patients who undergo TP + IAT[29,30]. The data suggested that physicians should objectively evaluate both negative and positive effects of obesity before surgical therapy. In addition, we found fluid and electrolyte disorders as a second morbidity predictor, which indicated that the pre-operative care and reversing fluid and electrolyte status is critical to minimizing potential post-surgical morbidities.
Patients become insulin dependent after TP due to the lack of beta-cells. IAT is an effective treatment preventing surgical diabetes after TP in patient with CP. Recently, Sutherland et al[22] showed that there was a 30% insulin-independence rate in a single-center study after long-term follow-up[16]. Furthermore, other clinical studies have shown comparative insulin-free rates during the last decade[15,21,27]. In this study, the data clearly indicates that IAT can achieve more than a 50% insulin-free rate if using combination of TP + IAT. However, the limitation of this study was that we were only able to analyze the short-term outcomes during the hospitalization.
TP + IATs were performed mainly in a limited amount of medical facilities due to the highly required equipped facilities and well experienced isolation team. However, the total number of patients who underwent TP + IAT in the United States has been continuously increasing during the last decade. Considering the outcomes of no mortality, acceptable morbidity, and islet graft function during the hospitalization, this procedure may be applicable for more centers nationwide.
The main limitation of the study was that it is retrospective which makes any definitive conclusion difficult. The number of transplanted patients was limited in this study; therefore, the power of the study was too low to run multivariate analysis. Also, 61.4% of the race variable’s data was missing. NIS does not provide information regarding long term outcomes and follow up information of patients; therefore, there is no available data for quality of life measurement and narcotic independency status. Despite these limitations, this study is one of the first studies reporting and analyzing outcomes of patients who underwent TP and IAT with a nationwide database.
Between 2002-2012, the overall number of patients who underwent TP + IAT has been increasing.
The most common indication of the procedure was CP followed by AP. This study showed that TP + IAT is a safe and feasible procedure with no mortality and with acceptable morbidity rates, and that insulin independence can be achieved. Obesity and fluid and electrolyte disorders are the most significant predictors of in-hospital morbidity.
Chronic pancreatitis (CP) has a broad spectrum of symptoms and signs that interferes with patient’s daily performance and quality of life. Exocrine insufficiency and severe pain are the significant manifestations that require proper management. The standard treatments include medical, endoscopic, and surgical intervention. Total pancreatectomy (TP) is the last resort treatment for pain management in CP patients. TP is related with high rate of morbidity and complications. Post surgical hypoinsulinemia is one of the important TP complications, which needs a proper intervention. Islet autotransplantation (IAT) following TP helps to decrease hypoinsulinemia episodes.
This study is the first TP + IAT nationwide analysis. The authors think that TP + IAT must have a nationwide application to provide the best care for patients. The findings of this study support the fact that utilizing IAT after TP may help patients to experience less hypoinsulinemia episodes. For evaluating the pain control measures, studies with long term follow up is needed.
TP + IATs has been performed mainly in a limited amount of medical facilities due to the highly required equipped facilities and well experienced isolation team. But, this is the first nationwide analysis, which evaluates in-hospital mortality and morbidity. Considering the outcomes of no mortality, acceptable morbidity, and islet graft function during the hospitalization, this study suggests that TP + IAT may be applicable for more centers nationwide.
Patients with advanced stage CP who suffer from pain will benefit from IAT. Patients with IAT after pancreas removal can achieve insulin independence status and less pain. These benefits help patients to have better life quality and performance in their daily life.
CP is progressive inflammatory changes that happens in pancreas gland leads to physiological and structural damage. This process result in exocrine and endocrine malfunction. IAT is a procedure to isolate pancreatic islet cells and transplant these cells into the patient’s body. The transplanted islet cells have physiologic function to secret insulin, which prevents hypoinsulinemia episodes.
Very good result of TP and IAT in patients of chronic pancreatitis on a large series of retrospective study.
P- Reviewer: Kumar A S- Editor: Ji FF L- Editor: A E- Editor: Wang CH
| 1. | Klöppel G, Maillet B. Pathology of acute and chronic pancreatitis. Pancreas. 1993;8:659-670. [PubMed] |
| 2. | Andersen DK. Mechanisms and emerging treatments of the metabolic complications of chronic pancreatitis. Pancreas. 2007;35:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Bornman PC, Marks IN, Girdwood AW, Berberat PO, Gulbinas A, Büchler MW. Pathogenesis of pain in chronic pancreatitis: ongoing enigma. World J Surg. 2003;27:1175-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Steer ML, Waxman I, Freedman S. Chronic pancreatitis. N Engl J Med. 1995;332:1482-1490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 418] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 5. | Nair RJ, Lawler L, Miller MR. Chronic pancreatitis. Am Fam Physician. 2007;76:1679-1688. [PubMed] |
| 6. | Chen WX, Zhang WF, Li B, Lin HJ, Zhang X, Chen HT, Gu ZY, Li YM. Clinical manifestations of patients with chronic pancreatitis. Hepatobiliary Pancreat Dis Int. 2006;5:133-137. [PubMed] |
| 7. | Argo JL, Contreras JL, Wesley MM, Christein JD. Pancreatic resection with islet cell autotransplant for the treatment of severe chronic pancreatitis. Am Surg. 2008;74:530-536; discussion 536-537. [PubMed] |
| 8. | Wahoff DC, Papalois BE, Najarian JS, Kendall DM, Farney AC, Leone JP, Jessurun J, Dunn DL, Robertson RP, Sutherland DE. Autologous islet transplantation to prevent diabetes after pancreatic resection. Ann Surg. 1995;222:562-575; discussion 575-579. [PubMed] |
| 9. | Blondet JJ, Carlson AM, Kobayashi T, Jie T, Bellin M, Hering BJ, Freeman ML, Beilman GJ, Sutherland DE. The role of total pancreatectomy and islet autotransplantation for chronic pancreatitis. Surg Clin North Am. 2007;87:1477-1501, x. [PubMed] |
| 10. | White SA, Davies JE, Pollard C, Swift SM, Clayton HA, Sutton CD, Weymss-Holden S, Musto PP, Berry DP, Dennison AR. Pancreas resection and islet autotransplantation for end-stage chronic pancreatitis. Ann Surg. 2001;233:423-431. [PubMed] |
| 11. | Helling TS. Surgical management of chronic pancreatitis and the role of islet cell autotransplantation. Curr Surg. 2003;60:463-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Sutherland DE, Matas AJ, Najarian JS. Pancreatic islet cell transplantation. Surg Clin North Am. 1978;58:365-382. [PubMed] |
| 13. | Ong SL, Gravante G, Pollard CA, Webb MA, Illouz S, Dennison AR. Total pancreatectomy with islet autotransplantation: an overview. HPB (Oxford). 2009;11:613-621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Sutherland DE, Gruessner AC, Carlson AM, Blondet JJ, Balamurugan AN, Reigstad KF, Beilman GJ, Bellin MD, Hering BJ. Islet autotransplant outcomes after total pancreatectomy: a contrast to islet allograft outcomes. Transplantation. 2008;86:1799-1802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Webb MA, Illouz SC, Pollard CA, Gregory R, Mayberry JF, Tordoff SG, Bone M, Cordle CJ, Berry DP, Nicholson ML. Islet auto transplantation following total pancreatectomy: a long-term assessment of graft function. Pancreas. 2008;37:282-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Chinnakotla S, Radosevich DM, Dunn TB, Bellin MD, Freeman ML, Schwarzenberg SJ, Balamurugan AN, Wilhelm J, Bland B, Vickers SM. Long-term outcomes of total pancreatectomy and islet auto transplantation for hereditary/genetic pancreatitis. J Am Coll Surg. 2014;218:530-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Walsh RM, Saavedra JR, Lentz G, Guerron AD, Scheman J, Stevens T, Trucco M, Bottino R, Hatipoglu B. Improved quality of life following total pancreatectomy and auto-islet transplantation for chronic pancreatitis. J Gastrointest Surg. 2012;16:1469-1477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 18. | Fujino Y, Matsumoto I, Ajiki T, Kuroda Y. Clinical reappraisal of total pancreatectomy for pancreatic disease. Hepatogastroenterology. 2009;56:1525-1528. [PubMed] |
| 19. | Janot MS, Belyaev O, Kersting S, Chromik AM, Seelig MH, Sülberg D, Mittelkötter U, Uhl WH. Indications and early outcomes for total pancreatectomy at a high-volume pancreas center. HPB Surg. 2010;2010:pii: 686702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Bellin MD, Carlson AM, Kobayashi T, Gruessner AC, Hering BJ, Moran A, Sutherland DE. Outcome after pancreatectomy and islet autotransplantation in a pediatric population. J Pediatr Gastroenterol Nutr. 2008;47:37-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Ahmad SA, Lowy AM, Wray CJ, D’Alessio D, Choe KA, James LE, Gelrud A, Matthews JB, Rilo HL. Factors associated with insulin and narcotic independence after islet autotransplantation in patients with severe chronic pancreatitis. J Am Coll Surg. 2005;201:680-687. [PubMed] |
| 22. | Sutherland DE, Radosevich DM, Bellin MD, Hering BJ, Beilman GJ, Dunn TB, Chinnakotla S, Vickers SM, Bland B, Balamurugan AN. Total pancreatectomy and islet autotransplantation for chronic pancreatitis. J Am Coll Surg. 2012;214:409-424; discussion 424-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 23. | HCUP Nationwide Inpatient Sample (NIS). Healthcare Cost and Utilization Project (HCUP). 2000-2010. Agency for Healthcare Research and Quality, Rockville, MD. Available from: http://www.hcup-us.ahrq.gov/nisoverview.jsp. |
| 24. | Rodriguez Rilo HL, Ahmad SA, D’Alessio D, Iwanaga Y, Kim J, Choe KA, Moulton JS, Martin J, Pennington LJ, Soldano DA. Total pancreatectomy and autologous islet cell transplantation as a means to treat severe chronic pancreatitis. J Gastrointest Surg. 2003;7:978-989. [PubMed] |
| 25. | Ris F, Niclauss N, Morel P, Demuylder-Mischler S, Muller Y, Meier R, Genevay M, Bosco D, Berney T. Islet autotransplantation after extended pancreatectomy for focal benign disease of the pancreas. Transplantation. 2011;91:895-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 26. | Crippa S, Tamburrino D, Partelli S, Salvia R, Germenia S, Bassi C, Pederzoli P, Falconi M. Total pancreatectomy: indications, different timing, and perioperative and long-term outcomes. Surgery. 2011;149:79-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Garcea G, Weaver J, Phillips J, Pollard CA, Ilouz SC, Webb MA, Berry DP, Dennison AR. Total pancreatectomy with and without islet cell transplantation for chronic pancreatitis: a series of 85 consecutive patients. Pancreas. 2009;38:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 81] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 28. | Tjeertes EK, Hoeks SE, Beks SB, Valentijn TM, Hoofwijk AG, Stolker RJ. Obesity--a risk factor for postoperative complications in general surgery? BMC Anesthesiol. 2015;15:112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 128] [Cited by in RCA: 209] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 29. | Brandhorst H, Brandhorst D, Hering BJ, Federlin K, Bretzel RG. Body mass index of pancreatic donors: a decisive factor for human islet isolation. Exp Clin Endocrinol Diabetes. 1995;103 Suppl 2:23-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Takita M, Naziruddin B, Matsumoto S, Noguchi H, Shimoda M, Chujo D, Itoh T, Sugimoto K, Tamura Y, Olsen GS. Body mass index reflects islet isolation outcome in islet autotransplantation for patients with chronic pancreatitis. Cell Transplant. 2011;20:313-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |