Published online Jun 18, 2025. doi: 10.5500/wjt.v15.i2.99401
Revised: November 25, 2024
Accepted: December 25, 2024
Published online: June 18, 2025
Processing time: 214 Days and 8.6 Hours
Coronavirus disease 2019 (COVID-19) disrupted healthcare and led to increased telehealth use. We explored the impact of COVID-19 on liver transplant eva
To understand the impact of telehealth on LTE during COVID-19 and to identify disparities in outcomes disaggregated by sociodemographic factors.
This was a retrospective study of patients who initiated LTE at our center from 3/16/20-3/16/21 (“COVID-19 era”) and the year prior (3/16/19-3/15/20, “pre-COVID-19 era”). We compared LTE duration times between eras and explored the effects of telehealth and inpatient evaluations on LTE duration, listing, and pre-transplant mortality.
One hundred and seventy-eight patients were included in the pre-COVID-19 era cohort and one hundred and ninety-nine in the COVID-19 era cohort. Twenty-nine percent (58/199) of COVID-19 era initial LTE were telehealth, compared to 0% (0/178) pre-COVID-19. There were more inpatient evaluations during COVID-19 era (40% vs 28%, P < 0.01). Among outpatient encounters, telehealth use for initial LTE during COVID-19 era did not impact likelihood of listing, pre-transplant mortality, or time to LTE and listing. Median times to LTE and listing during COVID-19 were shorter than pre-COVID-19, driven by increased inpatient evaluations. Sociodemographic factors were not predictive of telehealth.
COVID-19 demonstrates a shift to telehealth and inpatient LTE. Telehealth does not impact LTE or listing duration, likelihood of listing, or mortality, suggesting telehealth may facilitate LTE without negative outcomes.
Core Tip: The coronavirus disease 2019 pandemic led to a shift to telehealth for liver transplant (LT) evaluations (LTEs). In this study, the authors found that telehealth did not have an impact on likelihood of listing, waitlist mortality, or evaluation length for patients undergoing LTE. These findings suggest that telehealth is a safe alternative for LTEs, and that outcomes are no different to in-person evaluations. These findings have important implications: Telehealth can help improve access to LT services, especially as telehealth can be of increased convenience to patients.
- Citation: Jowell AH, Kwong AJ, Reguram R, Daugherty TJ, Kwo PY. Changes in the liver transplant evaluation process during the early COVID-19 era and the role of telehealth. World J Transplant 2025; 15(2): 99401
- URL: https://www.wjgnet.com/2220-3230/full/v15/i2/99401.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i2.99401
The coronavirus disease 2019 (COVID-19) pandemic presented a number of unprecedented challenges to the medical field. In light of national shelter-in-place orders, telemedicine rose in prominence, including in hepatology and liver transplant (LT) services[1,2]. Telemedicine presents both opportunities and challenges. Opportunities include the ability to provide subspecialized access to remote and underserved populations, increased monitoring of patients with chronic diseases (such as glycemic control with telemonitoring), and decreased costs and waiting times for patients needing to obtain medical care[1,3]. Challenges include limited ability to conduct a complete physical exam, difficulty to ensure a private space between patient and provider, barriers to establishing rapport, the potential for technological disruptions, and difficulties with access to or ability to use internet or digital devices[1,2,4]. In the LT space specifically, additional benefits of telehealth include the potential of reduced time from LT referral to evaluation and listing as well as the opportunity to facilitate relationships between LT centers and community physicians[5-7]. Challenges specific to the LT population include difficulty with remotely assessing patient frailty and the dependability of social support[6].
While telemedicine has the opportunity to increase access to healthcare, significant disparities also exist. Telemedicine may be susceptible to “intervention-generated inequalities”, where an intervention can worsen inequities given its disproportionate benefits for certain groups of people[8]. For example, decreased educational access, non-English language proficiency, a lack of internet, economic instability, and older age are all factors that increase patients’ barriers to digital access, which has the potential to exacerbate disparities in outcomes. Understanding telehealth disparities is especially important in LT, where inequities in access to and outcomes of LT have been noted even before the COVID-19 pandemic[9].
Along with changes in telehealth usage, the early COVID-19 era was associated with a general reduction in hospitalizations for non-COVID-19 conditions[10], including heart failure, chronic obstructive pulmonary disease, myocardial infarction, and appendicitis, as well as a decrease in elective surgical procedures, such as bariatric surgery[11,12]. Interestingly, a study of patients with chronic liver disease found that while the early COVID-19 pandemic led to decreased overall hospitalizations, there was an increased proportion of non-voluntary hospitalizations and patients admitted to the intensive care unit. The authors also found that hospitalized patients with cirrhosis and non-elective admissions presented with higher model for end-stage liver disease (MELD) scores, as well as increased mortality compared with pre-COVID-19 patients[13].
There has been a growing body of evidence exploring the use of telemedicine among patients in hepatology. For example, a study of patients with chronic hepatitis C found that direct-acting anti-viral treatment prescribed via telehealth achieved a 97% sustained viral remission[14]. A meta-analysis published by Muftah and colleagues explored telehealth among patients with chronic liver disease and found that telehealth interventions among patients with chronic liver disease typically led to equal or superior outcomes overall[15]. The only study included in this meta-analysis exploring telehealth use in the pre-LT population during COVID-19 was by Delman and colleagues, who found that during the first 6 months of COVID-19, patients evaluated using telehealth had similar rates of transplant and no differences in outcomes 90 days post-transplant[16]. To our knowledge, there are no additional studies exploring the use of telehealth specifically for LT evaluation (LTE) among patients during the COVID-19 era that either extend beyond the first 6 months of the pandemic or disaggregate by sociodemographic factors. Therefore, our understanding of outcomes for candidates undergoing LTE during the COVID-19 era using telehealth is limited.
LT candidates with decompensated cirrhosis are an important population to explore telehealth use given their significant burden of disease, overall poor health, and high healthcare utilization. In this study, we sought to explore the initial impact of the COVID-19 pandemic on outpatient and inpatient LTEs, specifically telehealth usage on LT outcomes before and after the onset of the COVID-19 pandemic. In addition, we aimed to identify and understand disparities in outcomes disaggregated by sociodemographic factors including race/ethnicity, insurance, language, and distance to our hospital.
This was a retrospective cohort study of patients who initiated LTE at our institution in Northern California from March 16, 2020 to March 16, 2021 (“COVID-19 era”) and the year prior from March 16, 2019 to March 15, 2020 (“pre-COVID-19 era”). Shortly after the onset of the COVID-19 pandemic, our medical center and transplant program developed the capacity to offer a telehealth option in lieu of an in-person office visit, per the provider or patient preference, similar to most medical centers. There were no center specific restrictions to determine which patients could use telehealth. While in-person visits early in the COVID-19 era were never formally removed, our center had extremely low numbers of such visits. All patients undergoing LTE at our center were expected to see a separate hepatologist as part of the evaluation, in addition to their usual gastroenterology or hepatology care.
All adults undergoing LTE were included in our analysis, including multiorgan transplants (liver-kidney, liver-heart, liver-lung, liver-intestine-pancreas), living donor LT, and exception cases. Only the first LTE was included for patients who initiated LTE more than once during our study period. Status 1 / acute liver disease patients were excluded from our analysis.
We performed a separate sub-group analysis of patients who began LTE in the pre-COVID-19 era but who had completed their LTE and possible listing in the COVID-19-era (n = 34). All patients in our study cohort completed LTE, and we included data through July 31, 2021.
Sociodemographic data including age, sex, race/ethnicity, preferred language, distance to our center, and insurance status were obtained from the electronic medical record. Preferred language was based on documentation in the electronic medical record, and distance to our hospital was based on coordinates. The encounter type (office visit, telehealth, or inpatient) was extracted for initial hepatology LTE, which is defined as a patient’s first presentation to our transplant center. Mode of telehealth delivery (phone vs video visit) was also collected. Additional data included: Etiology of liver disease, MELD with sodium (MELD-Na) score at evaluation, MELD-Na score at committee review meeting, presence of hepatocellular carcinoma (HCC), history of alcohol use, and markers of liver disease decompen
This study was approved by the Stanford University Institutional Review Board, Panel on Medical Human Subjects in accordance with both the Declarations of Helsinki and Istanbul (Institutional Review Board number 40095). This study received a waiver of informed consent.
The primary outcomes were likelihood of “telehealth evaluation” and time to first committee review meeting (referred to as “LTE length”). Secondary outcomes included: likelihood of other encounter type (office visit, inpatient); likelihood of telehealth video vs phone visit; whether a patient was listed, transplanted, or died during evaluation or while on the waitlist (“pre-transplant mortality”); time to listing; and time to transplant. We conducted all analyses for the COVID-19 era cohort; we only focused on time to LTE, time to listing, and likelihood of listing for the pre-COVID 19 era cohort.
Descriptive statistics for these data were generated for the overall cohort demographics, with discrete variables summarized by proportions, and continuous variables by the median and 25th through 75th percentile (p 25-p 75) of the data. We used logistic regression to analyze predictors of telehealth usage and linear regression to analyze predictors of LTE length and time to listing. Variables with P < 0.10 in the univariable model were entered into the multivariable model. Differences between groups were compared using t-tests, χ2 tests, one-way analysis of variance, and Kruskal Wallis tests as appropriate. P < 0.05 was considered significant for this study. Statistical analyses were performed using SAS, GraphPad, and R.
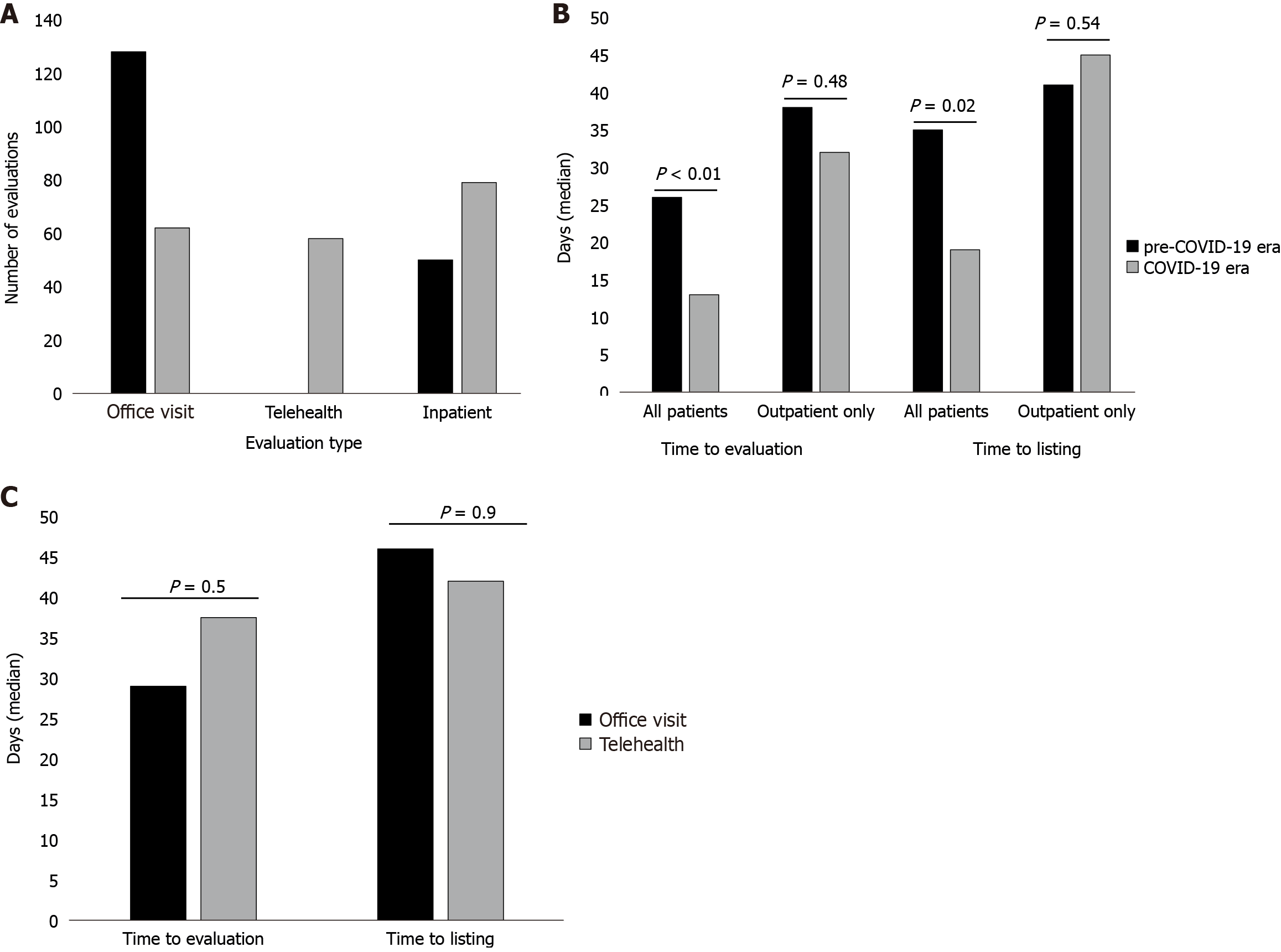
Table 1 outlines overall cohort demographics and outcomes of the 178 patients evaluated in the pre-COVID-19 era and 199 patients in the COVID-19 era. There were no significant differences for patient race/ethnicity, insurance status, language, sex, or distance to our hospital in the pre-COVID-19 vs COVID-19 eras. In the COVID-19 era, more initial hepatology evaluations were inpatient (39.7% vs 28.1%) or telehealth (29.1% vs 0%), compared with the pre-COVID-19 era (P < 0.01; Figure 1A). Patients in the COVID-19 era had a higher median MELD-Na score at evaluation than in the pre COVID-19 era (21 vs 17, P < 0.01). There were no significant differences among the likelihood of patients being listed during the pre-COVID-19 vs COVID-19 eras (P = 0.83). The risk of mortality during evaluation or waitlisting (“pre-transplant mortality”) during the COVID-19 era was 25.6%, and 20.8% among outpatient only encounters.
| Pre-COVID era, n = 178 | COVID era, n = 199 | P value | |
| Median age, years (p 25-p 75) | 62 (55-67) | 58 (47-65) | 0.002 |
| Sex (male) | 112 (64.0) | 129 (64.8) | 0.85 |
| Preferred language other than English | 45 (25.3) | 40 (20.1) | 0.28 |
| Race/ethnicity | 0.89 | ||
| White | 90 (50.6) | 93 (46.7) | |
| Asian | 13 (7.3) | 17 (8.5) | |
| Hispanic | 66 (37.1) | 79 (39.7) | |
| Black | 2 (1.1) | 4 (2.0) | |
| Other | 7 (3.9) | 6 (3.0) | |
| Insurance | 0.78 | ||
| Private | 63 (35.4) | 75 (37.7) | |
| Medicare | 66 (37.1) | 67 (33.7) | |
| Medi-cal | 49 (27.5) | 57 (28.6) | |
| Etiology of liver disease | |||
| Hepatitis C only | 21 (11.8) | 18 (9.0) | |
| Hepatitis C + alcohol induced liver disease | 15 (8.4) | 11 (5.5) | |
| Alcohol induced liver disease only | 73 (41) | 92 (46.2) | |
| Hepatitis B | 9 (5.1) | 5 (2.5) | |
| Primary sclerosing cholangitis | 4 (2.2) | 4 (2.0) | |
| Primary biliary cholangitis | 4 (2.2) | 6 (3.0) | |
| Autoimmune hepatitis | 1 (0.6) | 5 (2.5) | |
| Non-alcoholic steatohepatitis | 36 (20.2) | 32 (16.1) | |
| Alpha 1 anti-trypsin | 1 (0.6) | 1 (0.5) | |
| Wilson’s disease | 0 (0.0) | 1 (0.5) | |
| Hemochromatosis | 14 (7.9) | 24 (12.1) | |
| Median MELD-Na at evaluation (p 25-p 75) | |||
| All patients | 17 (9-23) | 21 (13-29) | < 0.001 |
| Outpatient only | 13 (8-19) | 16 (10-20) | 0.02 |
| Median distance to Stanford Hospital (p 25-p 75) miles | 58.0 (17.1-114.3) | 58.6 (15.8-131.8) | 0.91 |
| Alcohol etiology | 88 (49.4) | 103 (51.8) | 0.73 |
| HCC diagnosis | 60 (33.7) | 42 (21.1) | 0.008 |
| Hepatology liver transplant evaluation | < 0.001 | ||
| Office visit | 128 (71.9) | 62 (31.2) | |
| Telehealth | 0 (0.0) | 58 (29.1) | |
| Inpatient | 50 (28.1) | 79 (39.7) | |
| Median days from evaluation to initial committee review (p 25-p 75) | |||
| All patients | 26 (11-60) | 13 (6-48) | 0.004 |
| Outpatient only | 38 (15-69) | 32 (11-69) | 0.48 |
| COVID era median days from evaluation to initial committee review (p 25-p 75) | |||
| Office visit | N/A | 29 (11-63) | 0.5 |
| Telehealth | N/A | 37.5 (11.3-74.8) | |
| Median days from evaluation to listing (p 25- p 75) | |||
| All patients | 35 (18-81) | 19 (7-69) | 0.02 |
| Outpatient only | 41 (19-104) | 45 (11-102) | 0.54 |
| COVID era median days from evaluation to listing (p 25-p 75) | |||
| Office visit | N/A | 46 (11-102) | 0.9 |
| Telehealth | N/A | 42 (12-92.5) | |
| Listed | 100 (56.2) | 115 (57.8) | 0.83 |
| COVID era listed | |||
| Office visit | N/A | 41 (66.1) | |
| Telehealth | N/A | 28 (48.3) | 0.07 |
| Pre transplant mortality | |||
| All patients | N/A | 51 (25.6) | N/A |
| Outpatient only | 25 (20.8) | ||
| COVID era pre transplant mortality | 0.25 | ||
| Office visit | N/A | 16 (25.8) | |
| Telehealth | N/A | 9 (15.5) | |
| Transplanted | N/A | 59 (29.6) | N/A |
| COVID era transplanted | |||
| Office visit | N/A | 13 (21.0) | 0.8 |
| Telehealth | N/A | 14 (24.1) |
Median times to LTE and listing during COVID-19 era were shorter than the pre-COVID-19 era (13 vs 26 days and 19 vs 35 days, P < 0.01; Figure 1B). When only outpatient encounters were considered, there was no significant difference in median time to LTE and listing during COVID-19 era vs pre-COVID-19 era (P = 0.48 and P = 0.54, respectively; Figure 1B). In COVID-19 era, there was no difference in time to LTE or listing among patients with initial telehealth vs office visit evaluation (P = 0.5 and 0.9, respectively (Figure 1C). Sub-group analysis excluding patients who began LTE during pre-COVID-19, but completed LTE or listing during COVID era, yielded similar results.
Table 2 identifies predictors of telehealth use among outpatients during the COVID-19 era. Neither sociodemographic variables including age, sex, preferred language, race/ethnicity, insurance type, distance to our hospital, nor clinical variables such as MELD-Na, alcohol-associated liver disease, or diagnosis of HCC, were associated with telehealth use among outpatients during the COVID-19 era. Under multi-variate analysis, patients with hepatic encephalopathy had an increased odds of telehealth use (OR 1.33, P < 0.05), whereas ascites and esophageal variceal bleeding were not associated with telehealth use.
| Univariable OR (95%CI) | P value | Multivariable OR (95%CI) | P value | |
| Age (per year increase) | 1.01 (0.98-1.05) | 0.46 | 1.01 (0.96-1.05) | 0.78 |
| Sex, male | 0.58 (0.27-1.24) | 0.16 | 0.64 (0.26-1.59) | 0.34 |
| Preferred language, non-English | 0.91 (0.39-2.11) | 0.82 | 0.97 (0.31-3.02) | 0.97 |
| Race/ethnicity (ref: White) | ||||
| Hispanic | 0.67 (0.30-1.49) | 0.33 | 0.64 (0.23-1.78) | 0.39 |
| Asian | 1.40 (0.44-4.45) | 0.57 | 2.01 (0.47-8.56) | 0.34 |
| Other | 0.47 (0.08-2.75) | 0.4 | 0.34 (0.03-3.94) | 0.39 |
| Insurance (ref: Private) | ||||
| Medicare | 1.92 (0.83-4.46) | 0.13 | 1.85 (0.61-5.62) | 0.28 |
| Medi-cal | 1.86 (0.72-4.80) | 0.2 | 1.73 (0.55-5.40) | 0.35 |
| MELD-Na at evaluation (per unit increase) | 0.97 (0.91-1.03) | 0.3 | 0.96 (0.89-1.04) | 0.29 |
| Distance to Stanford Hospital (per 50 miles) | 0.93 (0.76-1.14) | 0.48 | 0.94 (0.74-1.20) | 0.62 |
| Alcohol etiology | 1.38 (0.67-2.85) | 0.38 | 1.96 (0.78-4.90) | 0.15 |
| HCC diagnosis | 1.11 (0.52-2.36) | 0.8 | 0.67 (0.23-1.98) | 0.47 |
Tables 3 and 4 describe predictors of time to committee review and listing respectively during the COVID-19 era. When adjusting for MELD and visit type, language, race, distance, and alcohol etiology were not associated with time to committee review during the COVID or pre-COVID era. However, Medicare insurance and male sex were associated with increased time to committee review during the COVID era, but not during the pre-COVID era. Medicare insurance and alcohol as the etiology of liver disease were also associated with increased time from evaluation to listing in the COVID-19 era. In addition, inpatient evaluations were associated with shorter time to committee review and time to listing than outpatient encounters in the COVID-19 era. Once again, sub-group analysis excluding patients who began LTE during pre-COVID-19 but completed LTE or listing during COVID era yielded similar results. Among COVID-19 era outpatients, telehealth use was not associated with LTE nor listing (P < 0.05).
| Univariable beta | P value | Multivariable beta | P value | |
| Age | 0.41 | 0.12 | ||
| Sex, male | -14.6 | 0.03 | -15.38 | 0.02 |
| Preferred language, non-English | 10.99 | 0.18 | ||
| Race/ethnicity (ref: White) | ||||
| Hispanic | -0.56 | 0.06 | 1.18 | 0.86 |
| Asian | 23.22 | 0.5 | 14.6 | 0.2 |
| Other | -10.48 | 0.94 | -8.92 | 0.53 |
| Insurance (ref: Private) | ||||
| Medicare | -21.91 | 0.005 | -17.11 | 0.02 |
| Medi-cal | -9.46 | 0.25 | -4.84 | 0.55 |
| Hepatology visit type (ref: Office visit) | ||||
| Telehealth | 5.4 | 0.5 | 1.48 | 0.85 |
| Inpatient | -31.9 | < 0.001 | -36.7 | < 0.001 |
| MELD-Na at evaluation | -1.12 | < 0.001 | 0.34 | 0.43 |
| Distance to Stanford Hospital | -0.008 | 0.84 | ||
| Alcohol etiology | 8.05 | 0.22 | ||
| HCC diagnosis | 1.9 | 0.81 |
| Univariable beta | P value | Multivariable beta | P value | |
| Age | 0.2 | 0.72 | ||
| Sex, male | -17.5 | 0.22 | ||
| Preferred language, non-English | 14.64 | 0.39 | ||
| Race/ethnicity (ref: White) | ||||
| Hispanic | -2.18 | 0.88 | ||
| Asian | 15.02 | 0.53 | ||
| Other | -7.73 | 0.78 | ||
| Insurance (ref: Private) | ||||
| Medicare | 35.96 | 0.02 | 17.46 | 0.02 |
| Medi-cal | 31.2 | 0.08 | 11.52 | 0.13 |
| Hepatology visit type (ref: Office visit) | ||||
| Telehealth | -15.1 | 0.37 | 2.1 | 0.79 |
| Inpatient | -51.39 | < 0.001 | -33.78 | < 0.001 |
| MELD-Na at evaluation | -0.85 | 0.18 | ||
| Distance to Stanford Hospital | -0.02 | 0.79 | ||
| Alcohol etiology | 32.48 | 0.02 | 13.54 | 0.03 |
| HCC diagnosis | -24.26 | 0.13 |
Overall, there was no significant change in patient distance from our hospital between pre-COVID-19 and COVID-19 eras, and no difference regarding likelihood of listing or transplant based on distance during either era. Distance to our hospital was also not associated with likelihood of telehealth use. Patients living more than 40 miles from the hospital were not more likely to have an inpatient evaluation during the COVID-19 era compared to the pre-COVID-19 era.
No differences by race/ethnicity were observed during the COVID-19 era with regards to likelihood of listing. In terms of transplant, non-Hispanic Asian patients were more likely to be transplanted than non-Hispanic white patients in the COVID-19 era, with no differences observed among Hispanic ethnicity or other races. Patients with higher MELD scores were also more likely to be transplanted. No differences in percent or likelihood of listing, transplant rate, or pre-transplant death were noted among those who participated in telehealth evaluation vs office visits. Regarding mortality analysis, Hispanic ethnicity was associated with a higher risk of mortality. There were no differences in outpatient pre-transplant deaths found based on insurance, distance to our hospital, or incremental increase in MELD score (Table 5). There were too few post-transplant deaths (n = 4) for us to include this in our analysis.
| COVID era | P value | |
| Hepatology liver transplant evaluation - telehealth | 0.50 (0.19-1.33) | 0.17 |
| Race/ethnicity (ref: White) | ||
| Hispanic | 2.81 (1.01-7.79) | 0.05 |
| Asian | 0.52 (0.09-2.90) | 0.45 |
| Other | Inf | |
| Insurance (ref: Private) | ||
| Medicare | 1.20 (0.41-3.54) | 0.74 |
| Medi-cal | 0.43 (0.11-1.63) | 0.22 |
| Distance to Stanford Hospital (per 50 miles) | 0.73 (0.49-1.08) | 0.12 |
| MELD-Na at evaluation (per unit increase) | 1.00 (0.93-1.08) | 0.91 |
Among outpatients in the COVID-19 era, telehealth use was not associated with likelihood of listing, likelihood of death, nor likelihood of transplant (Table 1). There were eight telehealth patients in our sample size whose hepatology evaluation was assessed via phone rather than video visit. This sample was not of sufficient sample size to analyze meaningfully phone vs video visits.
In this study, we explore the initial impact of the COVID-19 pandemic on LTEs, with a focus on the impact of telehealth on LTE outcomes. As expected, we found that the COVID-19 pandemic was associated with a shift to telehealth among our LT patient population, which is well documented in hepatology and other specialties[15,17-20]. Reassuringly, we found that telehealth did not impact LTE duration or listing duration, likelihood of listing, or pre-transplant mortality, suggesting that telehealth may facilitate increased access to LT services without negative outcomes. Our findings are consistent with a recent meta-analysis which did not identify inferior outcomes among patients with chronic liver disease who used telehealth in comparison with in-person visits[15]. Our study adds to the literature by focusing on LTEs during the first year of the COVID-19 pandemic.
Telehealth has been shown to have numerous benefits, including increased convenience and decreased costs for patients[21,22]. While there are limited data regarding use of telehealth in LT patients during the pandemic, a pre-COVID-19 era randomized control trial found that a telemedicine-based home management program after LT was shown to result in decreased hospital readmissions and improved quality of life, suggesting that telehealth can provide benefits in our patient population[23]. Similarly, a study among COVID-19 era LT patients, many of whom received care via telehealth, demonstrated no change in 6 month post-transplant outcomes compared to outcomes in the pre-COVID-19 era[16]. While research from pre-COVID-19 suggests that telehealth expedites LTE and listing among Veterans Affairs patients[5], our study did not find this reduced time to evaluation and listing benefits.
We found that COVID-19 demonstrated a shift to inpatient evaluations, where patients presented with higher MELD-Na scores and shorter times to evaluation/listing compared to outpatient evaluations. This likely reflects that patients with higher MELD-Na scores had inpatient LTE due to severity of illness which resulted in fewer delays in access to care and testing, which were systemic problems during the COVID-19 era[24]. While one study reported overall decreased hospitalizations during the COVID-19 era for patients with chronic liver disease[13], we suspect that the increased length of our study period during the COVID-19 era allowed more patients to miss their routine liver care and therefore presented in a more advanced stage to our hospital. This report also found that among non-elective hospitalizations, patients had a higher MELD-Na score and greater mortality during COVID-19 era, in turn supporting our finding that patients during the COVID-19 era had higher MELD-Na scores and were more likely to undergo inpatient LTE.
Our study explored disparities in LT outcomes with the introduction of telehealth. Disparities in access to LT care based on race, ethnicity, gender, socioeconomic status, and insurance status are well documented in the literature[9]. For example, a study of patients in Detroit who underwent LTE found that non-Hispanic Black race, having alcohol-associated hepatitis, being unmarried, having inadequate insurance, and having a lower socioeconomic status were all factors that decreased an individual’s likelihood of being listed for LT[25]. The Northern California region is an especially important area to study health disparities given known existing inequities in income and health[26].
We found that non-private Medicare insurance, which we used as a proxy for socioeconomic status, was associated with increased time to evaluation and listing during the COVID-19 era. Studies have found that Medicare and Medicaid patients have poorer waitlist outcomes[27] and higher post-transplant mortality than their counterparts with private insurance[28], and our study adds to this evidence that patients with non-private insurance face additional barriers to LT. We also found that patients with alcohol use disorder presented with increased length of listing during the COVID-19 era, which we suspect is due to these patients being deferred for listing to demonstrate a longer duration of sobriety.
We found that patients with hepatic encephalopathy had an increased odds of telehealth use. This could be due to these patients’ altered mental status leading to increased difficulty arranging transportation to clinic, suggesting that telehealth might offer them additional benefits - though a support person may be required at the video visit to ensure maximal benefit. Interestingly, patients with ascites and esophageal variceal bleeding were not associated with telehealth use, which could possibly be due to their degree of decompensation meriting an in-person visit. Future work should further explore different markers of hepatic decompensation, and their impact on the LTE process with the introduction of telehealth.
Notably, none of the sociodemographic factors analyzed, including age, language, race/ethnicity, sex, insurance, and distance to our hospital, were predictors of telehealth use among outpatients during the COVID-19 era. These findings contrast with the current literature which has demonstrated sociodemographic disparities in telehealth access. A study of patients with liver disease found that older patients, non-Hispanic Black patients, and patients with Medicare/Medicaid faced disparities in access to telehealth during COVID-19, including a greater likelihood of completing phone visits instead of video visits[20]. Another report investigating oncology patients cared for in Southern California found decreased telehealth use among Hispanic and Asian patients, Spanish-speaking patients, and patients with Medicaid insurance[29].
We did find sociodemographic disparities regarding likelihood of transplantation and pre-transplant mortality in the COVID-19 era, as we found that non-Hispanic Asian patients were more likely to be transplanted, and patients with Hispanic ethnicity were associated with a higher risk of pre-transplant mortality. As this was a small, single center study, larger patient populations enabling further disaggregated analysis of data is needed to understand better the impact of sociodemographic and other factors on telehealth use during COVID-19.
Despite the increased telehealth usage in the COVID-19 era, we did not find a significant change in median patient distance from our hospital with the introduction of telehealth in the COVID-19 era. Furthermore, patients living further from our hospital were not more likely to use telehealth, in turn suggesting that the use of telehealth at our institution has not increased geographic diversity. This finding may be explained by lower technological and internet access in areas further from our hospital, which would be consistent with a recent report observing that patients living in counties with decreased access to LT services or local gastroenterology care face decreased access to technological devices and broadband internet as well as higher liver-related mortality[30]. Our findings suggest that without intentional outreach to geographically diverse populations that takes into account decreased access to technological devices and broadband internet, telehealth will not provide benefits to patients living at a greater distance from the hospital. This is particularly important given that patients living an increased distance from a LT center have been found to have decreased access to wait-listing and lower likelihood of LT[31].
Our study has several limitations. We did not have a large enough sample size to analyze robustly by phone vs video visits, as only eight of our telehealth visits were phone visits, which could reveal disparities in LT management[20]. Future research should explore disparities in LTE telehealth phone vs video visit use, and the impact on LT outcomes. Unfortunately, our study did not explore access to social support in the telehealth setting, which is important given that inadequate social support is a common barrier to LT, and it is difficult to assess reliable social support using telehealth[6]. An additional limitation is that we collected data only for the “initial” hepatology visit. Obtaining data for all visits leading up to LTE, listing, and transplant would allow us to access additional information regarding the impact of telehealth on LT outcomes. Finally, our analysis was limited by sample size, and all our patients were from a single center. Future multi-center research with a larger patient population would add additional power to this work and further elucidate the relationship between telehealth and LT outcomes.
In summary, we found that the COVID-19 era demonstrated a shift to telehealth and inpatient LTE as expected. We also found that telehealth did not impact LTE or listing duration, likelihood of listing, or mortality. Such findings suggest that telehealth may facilitate increased access to LTE services without negative outcomes, and should therefore continue to be used throughout LTEs even beyond the COVID-19 pandemic. There were more inpatient LTEs during the COVID-19 era which likely helped avoid delays in patients’ access to care and testing, as these were systemic problems encountered during this time. We found no predictors of telehealth use based on sociodemographic factors including race, ethnicity, insurance status, and distance to our hospital. Given that we did not identify any increased use of telehealth among patients living further from our hospital, we suggest that future prospective efforts and interventions are needed to enable telehealth to reach a more geographically diverse patient population to improve access to care for patients with decompensated liver disease with special attention to social support and other identified disparities.
The authors would like to acknowledge Michelle Lam for her assistance with data collection.
| 1. | Fung BM, Perumpail M, Patel YA, Tabibian JH. Telemedicine in Hepatology: Current Applications and Future Directions. Liver Transpl. 2022;28:294-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Fix OK, Serper M. Telemedicine and Telehepatology During the COVID-19 Pandemic. Clin Liver Dis (Hoboken). 2020;15:187-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Le LB, Rahal HK, Viramontes MR, Meneses KG, Dong TS, Saab S. Patient Satisfaction and Healthcare Utilization Using Telemedicine in Liver Transplant Recipients. Dig Dis Sci. 2019;64:1150-1157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 4. | Perisetti A, Goyal H. Successful Distancing: Telemedicine in Gastroenterology and Hepatology During the COVID-19 Pandemic. Dig Dis Sci. 2021;66:945-953. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 5. | John BV, Love E, Dahman B, Kurbanova N, Konjeti VR, Sundaram LT, Deng Y, Aubuchon S, Heuman D, Bajaj JS, Gilles H, Chang M, Qayyum R, Siddiqui MS. Use of Telehealth Expedites Evaluation and Listing of Patients Referred for Liver Transplantation. Clin Gastroenterol Hepatol. 2020;18:1822-1830.e4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 66] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 6. | Shroff H, Kulik L. Telemedicine for Liver Transplant Evaluations: The Benefits and Risks. Clin Liver Dis (Hoboken). 2022;19:157-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 7. | Serper M, Agha A, Garren PA, Taddei TH, Kaplan DE, Groeneveld PW, Werner RM, Shea JA. Multidisciplinary teams, efficient communication, procedure services, and telehealth improve cirrhosis care: A qualitative study. Hepatol Commun. 2023;7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 8. | Price JC, Simpson DC. Telemedicine and Health Disparities. Clin Liver Dis (Hoboken). 2022;19:144-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Wahid NA, Rosenblatt R, Brown RS Jr. A Review of the Current State of Liver Transplantation Disparities. Liver Transpl. 2021;27:434-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 53] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 10. | Dang A, Thakker R, Li S, Hommel E, Mehta HB, Goodwin JS. Hospitalizations and Mortality From Non-SARS-CoV-2 Causes Among Medicare Beneficiaries at US Hospitals During the SARS-CoV-2 Pandemic. JAMA Netw Open. 2022;5:e221754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 56] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 11. | Blecker S, Jones SA, Petrilli CM, Admon AJ, Weerahandi H, Francois F, Horwitz LI. Hospitalizations for Chronic Disease and Acute Conditions in the Time of COVID-19. JAMA Intern Med. 2021;181:269-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 107] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 12. | Angelo J, Soto M, Dai D, Spector D, Orav EJ, Tavakkoli A, Tsai TC. Impact of the COVID-19 Pandemic on Inpatient and Outpatient Utilization of Bariatric Surgery. Surg Endosc. 2023;37:4917-4925. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 13. | Hartl L, Semmler G, Hofer BS, Schirwani N, Jachs M, Simbrunner B, Bauer DJM, Binter T, Pomej K, Pinter M, Trauner M, Mandorfer M, Reiberger T, Scheiner B. COVID-19-Related Downscaling of In-Hospital Liver Care Decreased Patient Satisfaction and Increased Liver-Related Mortality. Hepatol Commun. 2021;5:1660-1675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Syed TA, Cherian R, Lewis S, Sterling RK. Telemedicine HCV treatment in department of corrections results in high SVR in era of direct-acting antivirals. J Viral Hepat. 2021;28:209-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Muftah AA, Banala C, Raasikh T, Jamali T, Bustamante G, Cholankeril G, Kanwal F, Flores A, Hernaez R. Telehealth interventions in patients with chronic liver diseases: A systematic review. Hepatology. 2023;78:179-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 16. | Delman AM, Turner KM, Jones CR, Vaysburg DM, Silski LS, King C, Luckett K, Safdar K, Quillin RC 3rd, Shah SA. Keeping the lights on: Telehealth, testing, and 6-month outcomes for orthotopic liver transplantation during the COVID-19 pandemic. Surgery. 2021;169:1519-1524. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Chao GF, Li KY, Zhu Z, McCullough J, Thompson M, Claflin J, Fliegner M, Steppe E, Ryan A, Ellimoottil C. Use of Telehealth by Surgical Specialties During the COVID-19 Pandemic. JAMA Surg. 2021;156:620-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 120] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 18. | Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20:1193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 995] [Cited by in RCA: 953] [Article Influence: 190.6] [Reference Citation Analysis (0)] |
| 19. | Lindberg LD, Mueller J, Haas M, Jones RK. Telehealth for Contraceptive Care During the COVID-19 Pandemic: Results of a 2021 National Survey. Am J Public Health. 2022;112:S545-S554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | Wegermann K, Wilder JM, Parish A, Niedzwiecki D, Gellad ZF, Muir AJ, Patel YA. Racial and Socioeconomic Disparities in Utilization of Telehealth in Patients with Liver Disease During COVID-19. Dig Dis Sci. 2022;67:93-99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 78] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 21. | Powell RE, Henstenburg JM, Cooper G, Hollander JE, Rising KL. Patient Perceptions of Telehealth Primary Care Video Visits. Ann Fam Med. 2017;15:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 317] [Article Influence: 39.6] [Reference Citation Analysis (0)] |
| 22. | Drerup B, Espenschied J, Wiedemer J, Hamilton L. Reduced No-Show Rates and Sustained Patient Satisfaction of Telehealth During the COVID-19 Pandemic. Telemed J E Health. 2021;27:1409-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 82] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 23. | Lee TC, Kaiser TE, Alloway R, Woodle ES, Edwards MJ, Shah SA. Telemedicine Based Remote Home Monitoring After Liver Transplantation: Results of a Randomized Prospective Trial. Ann Surg. 2019;270:564-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 24. | Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, Ali N, McMillan H, Wiley JF, Weaver MD, Czeisler CA, Rajaratnam SMW, Howard ME. Delay or Avoidance of Medical Care Because of COVID-19-Related Concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250-1257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 533] [Cited by in RCA: 1045] [Article Influence: 209.0] [Reference Citation Analysis (0)] |
| 25. | Jesse MT, Abouljoud M, Goldstein ED, Rebhan N, Ho CX, Macaulay T, Bebanic M, Shkokani L, Moonka D, Yoshida A. Racial disparities in patient selection for liver transplantation: An ongoing challenge. Clin Transplant. 2019;33:e13714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 26. | California Health Care Foundation. 2021 Edition — Health Disparities by Race and Ethnicity in California. Oct 22, 2021. [cited 6 January 6 2023]. Available from: https://www.chcf.org/publication/2021-edition-health-disparities-race-ethnicity-california/. |
| 27. | Robinson A, Hirode G, Wong RJ. Ethnicity and Insurance-Specific Disparities in the Model for End-Stage Liver Disease Score at Time of Liver Transplant Waitlist Registration and its Impact on Mortality. J Clin Exp Hepatol. 2021;11:188-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 28. | Stepanova M, Al Qahtani S, Mishra A, Younossi I, Venkatesan C, Younossi ZM. Outcomes of liver transplantation by insurance types in the United States. Am J Manag Care. 2020;26:e121-e126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 29. | Qian AS, Schiaffino MK, Nalawade V, Aziz L, Pacheco FV, Nguyen B, Vu P, Patel SP, Martinez ME, Murphy JD. Disparities in telemedicine during COVID-19. Cancer Med. 2022;11:1192-1201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 90] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 30. | Henson JB, Wegermann K, Patel YA, Wilder JM, Muir AJ. Access to technology to support telehealth in areas without specialty care for liver disease. Hepatology. 2023;77:176-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 31. | Goldberg DS, French B, Forde KA, Groeneveld PW, Bittermann T, Backus L, Halpern SD, Kaplan DE. Association of distance from a transplant center with access to waitlist placement, receipt of liver transplantation, and survival among US veterans. JAMA. 2014;311:1234-1243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 139] [Article Influence: 12.6] [Reference Citation Analysis (0)] |