Published online Jun 18, 2025. doi: 10.5500/wjt.v15.i2.100157
Revised: December 20, 2024
Accepted: January 21, 2025
Published online: June 18, 2025
Processing time: 196 Days and 23.7 Hours
The use of biomarkers, such as the neutrophil-to-lymphocyte ratio (NLR) and the neutrophil-to-platelet ratio (NPR), has shown promise in evaluating early outcomes after medical, interventional, and surgical treatments. NLR has emer
To analyze the correlation of NLR and NPR with the development of post-liver transplantation (LT) early complications after stratification for hepatocellular carcinoma diagnosis.
Consecutive patients undergone LT between January 2019 and December 2023 were enrolled. Data regarding the concentration of hemoglobin and the differential leukocyte count on postoperative days (POD) 0, 1, 3, and 5 were collected.
The dataset included 161 consecutive patients undergone LT. Clavien-Dindo IV-V complications had a good correlation with NLR POD 1 (P = 0.05), NLR POD 3 (P < 0.001), NLR POD 7 (P < 0.001), NPR POD 3 (P < 0.001). In addition, the NPR ratio on POD 3 correlated with the onset of 30-day hemorrhage (P = 0.009). Finally, 30-day mortality had a significant association with the NLR POD 1 (P = 0.03) and with NLR POD 7 (P = 0.004), while NPR had a significant correlation with 30-day mortality in NPR POD 7 (P = 0.004).
The analysis of NLR and NPR are strictly correlated with Clavien-Dindo IV-V complications and 30-day post-LT death.
Core Tip: The neutrophil-to-lymphocyte ratio (NLR) and neutrophil-to-platelet ratio (NPR) are emerging biomarkers used to predict early outcomes following liver transplantation. Elevated NLR indicates systemic inflammation, which can signal complications like infection or rejection. High NPR values can reflect underlying inflammation and potential vascular complications. Both ratios are calculated from routine blood tests, making them cost-effective and readily available. Studies suggest that higher pre-transplant NLR and NPR levels are associated with increased risk of poor graft function, longer hospital stays, and mortality. Monitoring these ratios helps in identifying at-risk patients, guiding post-operative care, and improving overall transplant success.
- Citation: Pascale MM, Frongillo F, Vasta P, Massimiani G, Nure E, Agnes S. Significance of the neutrophil-to-lymphocyte ratio and the platelet-to-lymphocyte ratio as prognostic predictors after liver transplantation. World J Transplant 2025; 15(2): 100157
- URL: https://www.wjgnet.com/2220-3230/full/v15/i2/100157.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i2.100157
Liver transplantation (LT) represents a life-saving treatment for patients with advanced liver diseases. However, despite advancements in surgery and immunosuppressive therapies, the long-term success of this intervention can be compromised by early post-operative complications and inadequate inflammatory and immune responses[1]. The early identification of patients at risk of complications is crucial for increasing clinical-laboratory surveillance and reducing the rate of failure to rescue. The use of biomarkers, such as the neutrophil-to-lymphocyte ratio (NLR) and the neutrophil-to-platelet ratio (NPR), has shown promise in evaluating early outcomes after medical, interventional and surgical treat
NLR, defined as the ratio between the number of neutrophils and the number of lymphocytes in peripheral blood, has emerged as an indicator of systemic inflammation and physiological stress. In patients undergoing LT, NLR may reflect the degree of inflammatory reaction associated with surgery, immune response to the transplanted graft, and the presence of post-operative complications[3]. Numerous studies have demonstrated a correlation between high NLR and an increased risk of early complications, including infection and tumor recurrence[4]. Furthermore, a high value of NLR has been associated with an unfavorable prognosis and reduced survival in the post-surgical period. Therefore, monitoring NLR in patients undergoing LT can provide valuable information for identifying patients at risk of deve
Similarly, NPR, representing the ratio between the number of neutrophils and the number of platelets in peripheral blood, has emerged as a potential indicator of inflammation and thrombotic risk in the context of surgical and radio
However, it is important to emphasize that the interpretation of results obtained using NLR and NPR should be performed with caution, considering several factors that may influence the levels of these biomarkers. The presence of a neoplasia as hepatocellular carcinoma (HCC) may influence the inflammatory and immunological profile of patients, thereby altering NLR and NPR values[11]. Additionally, the onset of acute complications in the post-LT period could modify the levels of these markers. Currently, there is a lack of consistent data in the literature evaluating the role of immunological biomarkers in LT. The aim of our study is to analyze the correlation of NLR and NPR with the develop
Consecutive patients undergone LT with whole graft from a deceased donor between January 2019 and December 2023 in the Liver Transplant Unit of the Polyclinic “A. Gemelli” Foundation were enrolled. The LT cases with history of Coronavirus Disease 2019 (COVID-19) syndrome in the donor or in the recipient and the donor grafts undergone a machine perfusion treatment were excluded. This choice was made to avoid factors that could alter cellular elements’ concentration and blood distribution in the early post-transplant period. Clinicopathological characteristics of the patients were recorded and compared. The variables analyzed were sex, age, type of cirrhosis, diabetes, number of packed red blood cell unit transfused, duration of the surgical procedure, post-LT length of stay (LOS), 30-days post-LT complications according to the Clavien-Dindo classification[12], 30-days death. Furthermore, data regarding the concentration of hemoglobin and the differential leukocyte count on postoperative days (POD) 0, 1, 3, and 5 were collected. In particular, the concentration of neutrophils, lymphocytes and platelets was used to develop the NLR and NPR. This study protocol was reviewed and approved by the local Institutional Research Ethic Committee. This research, involving human participants, adhered to the Declaration of Helsinki guidelines. Artificial intelligence was not used at any stage of the development of this project.
The matching between donor and recipient was carried out by first considering blood group typing according to the ABO system. Subsequently, the recipient’s body size requirement and clinical needs were evaluated. LT was performed by three surgeons working in the same group. In a few cases a temporary vascular bypass was obtained through a portocaval anastomosis or an extracorporeal circulation.
Immunosuppression was initiated in the 1st POD using tacrolimus, according to the weight of the patient. Blood tacrolimus concentration goal was set between 6 and 8 ng/mL. The induction immunosuppressive therapy involved the administration of methylprednisolone at 160 mg, reduced to 10 mg starting from the 4th POD and discontinued after 2 months from the LT. Mycophenolate mofetil was included in the immunosuppression protocol and was discontinued if the leukocyte blood concentration fell below 2 × 109 g/dL.
Clinical data were collected in an anonymized center database. Included variables were analyzed with a Student’s t-test or a Mann-Whitney test. Factors correlated with the endpoints were used for a linear regression pondered with the age of the patients and the diagnosis of HCC. Afterwards, a binomial logistic regression was used to estimate the sensibility and the specificity of humoral biomarker through a receiving operating characteristic curve. The P value < 0.05 was con
The dataset included 161 consecutive patients undergone LT. Three cases of retransplant were excluded. Moreover, 3 cases of COVID-19 syndrome in donor o recipient were excluded, to avoid variability of the leukocytes due to the viral infection. The final cohort of the study accounted 155 LT from Liver Transplant Unit of “Agostino Gemelli” Polyclinic in Rome. All the clinical parameters are shown in Table 1. The mean age of the recipients was 58.1 years (54-65 years) and 127 of them (81.9%) were male. The mean model for end stage disease score was 21.6 (15-26). The indications for LT were: Alcohol (35.5%), metabolic syndrome (22.6%), hepatitis C virus infection (16.1%), hepatitis B virus infection (11%), biliary cirrhosis (5.2%), hemochromatosis (3.5%), cryptogenic cirrhosis (2.6%), acute liver failure (1.3%), and autoimmune cirrhosis (0.6%). HCC was diagnosed in 55.5% of LT cases. Postoperative complications were registered in 28.7% of LT. In particular, complications Clavien-Dindo III-V were seen in 10.2% of cases, with a percentage of 4.2% for complications Clavien-Dindo IV-V. Infections were the most recurrent complication with a rate of 25% of cases. Instead, the severe infections or sepsis were identified in 4% of cases. Hemorrhage was present in 3.8% of cases. Among the LT-specific complications, acute rejection was recognized in 7.5%. On the other hand, the 30-day mortality rate was 3.2%.
| Characteristics (n = 155) | Patients | P value |
| Donor age, median (IQR) | 68 (56-78) | |
| Donor BMI, median (IQR) | 24 (21-27) | |
| ECD | 48 (31) | |
| Recipient age, median (IQR) | 58.1 (54-65) | |
| Recipient male gender | ||
| Female | 28 (18.1) | 0.0017 |
| Male | 127 (81.9) | |
| Recipient BMI, median (IQR) | 26 (22-29) | |
| MELD at listing, median (IQR) | 18 (11-26) | |
| MELD at LT, median (IQR) | 21.6 (15-32) | |
| Main indication to LT | 0.038 | |
| Alcohol | 55 (35.5) | |
| Hepatitis C virus disease | 25 (16.1) | |
| Hepatitis B virus disease | 17 (11) | |
| MAFLD | 34 (22.6) | |
| Cholestatic | 8 (5.2) | |
| Cryptogenic | 4 (2.6) | |
| Haemochromatosis | 6 (3.9) | |
| Acute liver failure | 2 (1.3) | |
| Autoimmune | 1 (0.6) | |
| HCC co-indication | 86 (55.5) | |
| Intra-operative RBC transfusions, median (IQR) | 4 (0-12) | |
| 30-day Clavien-Dindo complications | ||
| I-IIIB | 72 (46.5) | 0.002 |
| IV-V | 7 (4.5) | |
| 30-day infection | 39 (25.2) | |
| 30-day sepsis | 6 (4) | |
| 30-day hemorrhage | 6 (4) | |
| Post-LT ICU stay, median (IQR) | 7 (2-16) | |
| Post-LT LOS, median (IQR) | 18 (14.5-28) | |
| Acute rejection diagnosis | 12 (7.7) | |
| 30-day patient death | 5 (3.2) | |
| 30-day graft loss | 6 (3.9) |
The absolute values of lymphocytes, neutrophils, and platelets showed no significant correlation with the outcomes. Specifically, univariate analysis between lymphocyte concentrations on POD 1, 3 and 7 and Clavien-Dindo grade IV-V complications presented P values of 0.16, 0.09, and 0.08, respectively. Neutrophil concentrations on POD 1, 3 and 7, in correlation with Clavien-Dindo grade IV-V complications, gave P values of 0.14, 0.09, and 0.07. Finally, the ratios between platelet concentrations on POD 1, 3 and 7 and Clavien-Dindo grade IV-V complications produced P values of 0.19, 0.1, and 0.09, respectively.
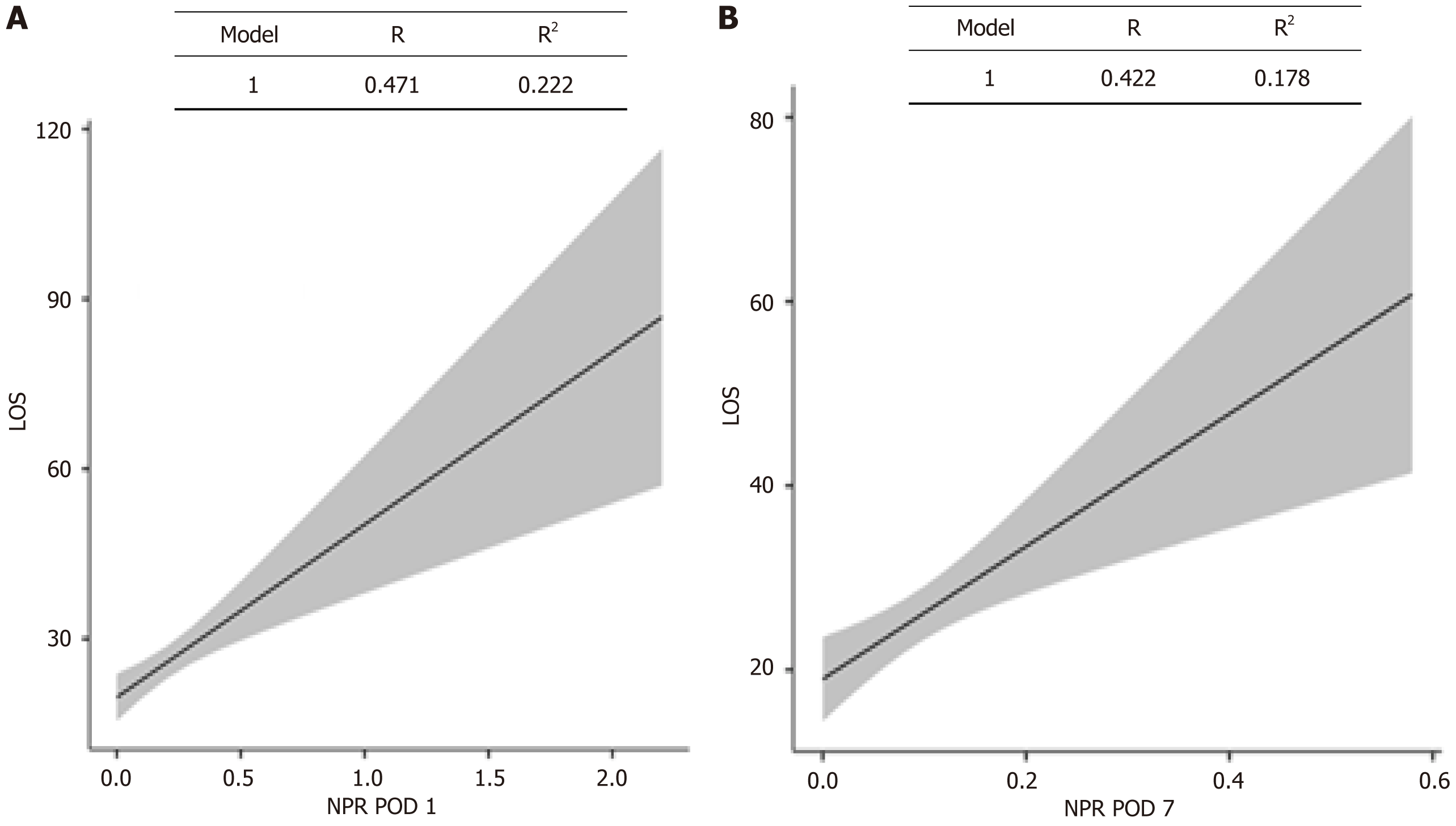
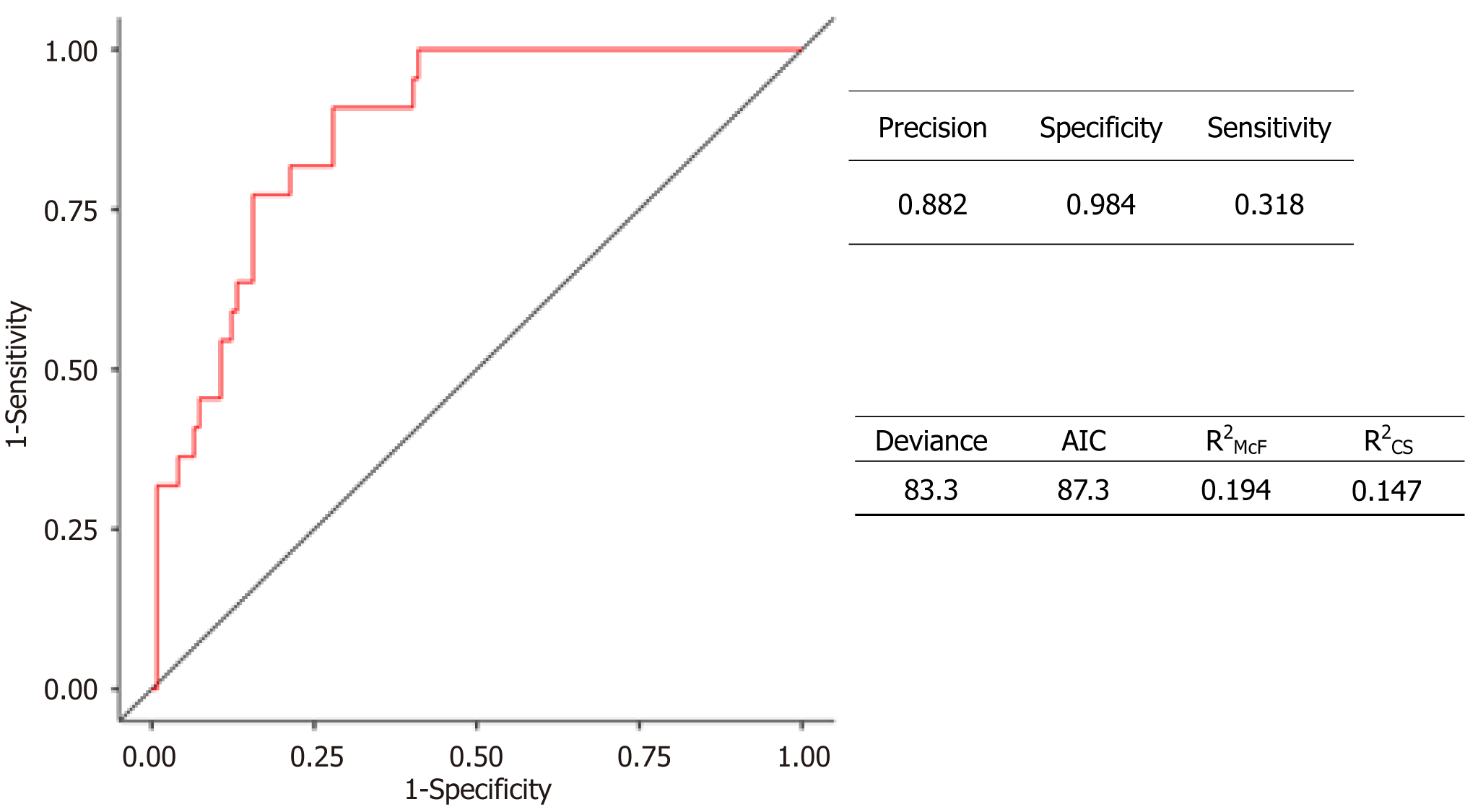
On the other hand, Clavien-Dindo IV-V complications had a good correlation with high values of NLR POD 1 (P = 0.05), NLR POD 3 (P < 0.001), NLR POD 7 (P < 0.001), and NPR POD 3 (P < 0.001). Specifically, the NPR ratio on POD 3 correlated with the onset of 30-day hemorrhage (P = 0.009). Finally, 30-day mortality had a significant association with the high NLR POD 1 (P = 0.03) and with high NLR POD 7 (P = 0.004), while high NPR had a significant correlation with 30-day mortality in NPR POD 7 (P = 0.004). The significant resulting ratios were correlated with LOS. Weighted linear regression adjusted for patient age and stratified by HCC diagnosis found a significant correlation between high NPR on POD 1 and LOS (P < 0.001) (Figure 1A). The same correlation was observed between high NPR on POD 7 and LOS (P < 0.001) (Figure 1B). Furthermore, the predictive ability of the analyzed ratios on the onset of the analyzed outcomes was evaluated through binomial logistic regression. High NPR on POD 7 exhibited a specificity and sensitivity in diagnosing Clavien-Dindo grade IV-V complications of 98.4% and 31.8%, respectively. The Z value was 4.23, with a P value of < 0.001 and an R2 value of 0.21 (Figure 2).
This study has demonstrated the predictive value of common biomarkers, which show clinical significance in correlating with fundamental clinical outcomes when compared with each other. In particular, high NLR and NPR ratios on POD 1, 3 and 7 have shown satisfactory results in predicting prolonged LOS, the development of 30-day severe complications, or 30-day patient mortality. The intuition behind the use of immunological markers dates back several years. The influence of interactions among immune cells on clinical outcomes was a niche topic until 2008. This year, several groups began to publish work specifically in hepatobiliary surgery. Thus, the importance of the NLR ratio as a prognostic factor in hepatic resections for both HCC and colorectal liver metastases was demonstrated[13,14]. Over time, the application of NLR and NPR ratios has expanded to other medical fields. In the neurological field, NLR has shown reliable prognostic power following thrombolysis in acute ischemic stroke[15]. In a retrospective study involving 117 patients, the NLR ratio has also been shown to predict early perihematomal edema expansion following intracerebral hemorrhage reliably[16]. In the cardiological context, furthermore, the NLR ratio was associated with hospitalization and long-term prognosis in patients with acute myocardial infarction after percutaneous coronary intervention[17]. In various fields of abdominal surgery, immune markers have consistently correlated with surgical outcomes and survival[18-20]. In our cohort, NLR and NPR ratios have confirmed their utility in predicting the complexity of surgical outcomes. Thus, it is desirable to stratify post-surgical risk, thereby focusing surveillance on patients who are at higher risk. The correlation between inflammatory markers and mortality aligns precisely with correlations observed with severe postoperative complications: Patients at higher risk of severe complications also exhibit higher mortality rates. Identifying an at-risk population by analyzing NLR and NPR also allows for a tangible advantage in reducing failure-to-rescue. The literature shows that NLR and NPR ratios are closely correlated with the patient’s nutritional status. Zhang et al[21] demonstrated the high prognostic value of NLR in a large population of patients with neoplastic cachexia. Therefore, patients on the waiting list for LT could benefit from NLR to further analyze the pre-LT metabolic status and directly correlate it with post-LT prognosis.
Inflammatory markers are increasingly significant in the oncological field as well. A 2022 study demonstrated that a reduced concentration of lymphocytes correlates with an incomplete response to liver-directed chemotherapy for HCC, increasing the risk of patient dropout while awaiting LT[22]. Subsequently, a prospective study involving 157 patients with HCC confirmed the prognostic role of inflammatory markers and demonstrated the predictive role of lymphocyte concentration in the success of transarterial chemoembolization[23]. Considering the evidence in the literature, our cohort was stratified based on the diagnosis of HCC. This approach helps to avoid selection bias among patients with HCC who were listed for LT after responding to downstaging treatment for HCC. The relationship between inflammatory markers and HCC has also been observed in hepatic resection surgery. Chen et al[24] demonstrated that patients with a high NLR level have a worse prognosis after hepatic resection for HCC. In a 2024 review, the influence of inflammatory processes on the surgical and oncological prognosis of HCC has been definitively recognized[25].
However, the most important studies on HCC do not involve patients undergoing LT. Our study is among the first to correlate post-LT 30-day outcomes with inflammatory markers. Our work confirmed that NLR and NPR have good predictive value not only for survival outcomes but also for the onset of severe complications within the first 30 days after LT. This result was not so obvious considering the goal of immunosuppression achieved with dedicated drugs in transplant patients. The high specificity achieved by NPR on POD VII towards severe complications also allows for optimal management of clinical resources for patients at higher risk of complications, allowing for more precise and personalized post-LT management. The determined advantages can be immediately utilized in any LT center, as no additional analysis is required beyond laboratory tests performed protocol-wise. Furthermore, the parameters are reproducible and comparable, as the complete blood count with leukocyte differential presents a low variability rate[26].
However, the blood count test results and related inflammatory markers can be altered by acute events such as infections, acute rejection, or the toxic effect of immunosuppressive drugs. A future study could be developed to evaluate the impact of acute events on the predictive power of inflammatory biomarkers. Another limitation of this work is the retrospective nature of the data, which may affect the accuracy of the recorded biochemical and clinical parameters. Furthermore, the single-center origin of the data could be an additional limitation to data interpretation due to a reduced number of enrolled cases and the application of a constant post-LT management protocol. Despite these limitations, the use of biomarkers such as NLR and NPR offers a non-invasive and convenient approach to assessing the risk of early complications and prognosis in the post-LT period. Integrating these markers into post-operative monitoring protocols could allow for more timely and targeted management of complications, thereby improving outcomes for patients undergoing this life-saving procedure.
The analysis of NLR and NPR are strictly correlated with Clavien-Dindo IV-V complications and 30-day post-LT death. These ratios can be integrated into clinical practice to improve the management and outcomes of patients undergoing LT. Further research is needed to confirm the accuracy of the markers as prognostic indicators in patients undergoing LT and to identify any interactions with other risk factors and outcome predictors.
| 1. | Alconchel F, Tinguely P, Frola C, Spiro M, Ciria R, Rodríguez G, Petrowsky H, Raptis DA, Brombosz EW, Ghobrial M; ERAS4OLT. org Working Group. Are short-term complications associated with poor allograft and patient survival after liver transplantation? A systematic review of the literature and expert panel recommendations. Clin Transplant. 2022;36:e14704. [PubMed] [DOI] [Full Text] |
| 2. | Kartal M, Aksungur N, Korkut E, Altundaş N, Kara S, Öztürk G. Significance of the Neutrophil-to-Lymphocyte Ratio, Platelet-to-Lymphocyte Ratio, and Preoperative Nutritional Index as Predictors of Morbidity in Patients Who Underwent Liver Resection for Alveolar Echinococcosis. Cureus. 2023;15:e44842. [PubMed] [DOI] [Full Text] |
| 3. | Kim KS, Kim JH, Kwon HM, Moon YJ, Shin WJ, Kim SH, Jun IG, Song JG, Hwang GS. Neutrophilia is more predictive than increased white blood cell counts for short-term mortality after liver transplantation in patients with acute-on-chronic liver failure. Anesth Pain Med (Seoul). 2023;18:389-396. [PubMed] [DOI] [Full Text] |
| 4. | Dai Y, Feng Q, Huang J. A new nomogram use neutrophil-to-lymphocyte ratio and fibrinogen-to-lymphocyte ratio to predict the recurrence of colorectal adenoma. J Gastrointest Oncol. 2023;14:1898-1899. [PubMed] [DOI] [Full Text] |
| 5. | Umman V, Gumus T, Kivratma HG, Tabatabayi P, Uguz A, Zeytunlu M, Emre S. Predictive Value of Red Blood Cell Distribution Width, Platelet Count to Lymphocyte Count Ratio, and Neutrophil Count to Lymphocyte Count Ratio Values for the Detection of Postoperative Infection in Patients Undergoing Liver Transplantation. Transplant Proc. 2023;55:1257-1261. [PubMed] [DOI] [Full Text] |
| 6. | Li BH, Wang LR, Huang J, Yang S, Huang B, Jia LJ, Zhou S, Guo FQ, Wang JH, Yu NW. Predictive role of neutrophil-to-platelet ratio in futile recanalization of patients after endovascular therapy. Biomark Med. 2024;18:137-143. [PubMed] [DOI] [Full Text] |
| 7. | Shaafi S, Bonakdari E, Sadeghpour Y, Nejadghaderi SA. Correlation between red blood cell distribution width, neutrophil to lymphocyte ratio, and neutrophil to platelet ratio with 3-month prognosis of patients with intracerebral hemorrhage: a retrospective study. BMC Neurol. 2022;22:191. [PubMed] [DOI] [Full Text] |
| 8. | Pang J, Liu J, Liang W, Yang L, Wu L. High Neutrophil-to-Platelet Ratio Is Associated with Poor Survival in Patients with Acute Aortic Dissection. Dis Markers. 2022;2022:5402507. [PubMed] [DOI] [Full Text] |
| 9. | Inaoka K, Kanda M, Uda H, Tanaka Y, Tanaka C, Kobayashi D, Takami H, Iwata N, Hayashi M, Niwa Y, Yamada S, Fujii T, Sugimoto H, Murotani K, Fujiwara M, Kodera Y. Clinical utility of the platelet-lymphocyte ratio as a predictor of postoperative complications after radical gastrectomy for clinical T2-4 gastric cancer. World J Gastroenterol. 2017;23:2519-2526. [PubMed] [DOI] [Full Text] |
| 10. | Nonogaki A, Kanda M, Ito S, Mochizuki Y, Teramoto H, Ishigure K, Murai T, Asada T, Ishiyama A, Matsushita H, Tanaka C, Kobayashi D, Fujiwara M, Murotani K, Kodera Y. Preoperative neutrophil-to-platelet ratio as a potential prognostic factor for gastric cancer with positive peritoneal lavage cytology in the absence of other non-curative factors: a multi-institutional dataset analysis. Surg Today. 2023;53:198-206. [PubMed] [DOI] [Full Text] |
| 11. | Xiao Y, Zhu G, Xie J, Luo L, Deng W, Lin L, Tao J, Hu Z, Shan R. Pretreatment Neutrophil-to-Lymphocyte Ratio as Prognostic Biomarkers in Patients with Unresectable Hepatocellular Carcinoma Treated with Hepatic Arterial Infusion Chemotherapy Combined with Lenvatinib and Camrelizumab. J Hepatocell Carcinoma. 2023;10:2049-2058. [PubMed] [DOI] [Full Text] |
| 12. | Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibañes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187-196. [PubMed] [DOI] [Full Text] |
| 13. | Halazun KJ, Aldoori A, Malik HZ, Al-Mukhtar A, Prasad KR, Toogood GJ, Lodge JP. Elevated preoperative neutrophil to lymphocyte ratio predicts survival following hepatic resection for colorectal liver metastases. Eur J Surg Oncol. 2008;34:55-60. [PubMed] [DOI] [Full Text] |
| 14. | Gomez D, Farid S, Malik HZ, Young AL, Toogood GJ, Lodge JP, Prasad KR. Preoperative neutrophil-to-lymphocyte ratio as a prognostic predictor after curative resection for hepatocellular carcinoma. World J Surg. 2008;32:1757-1762. [PubMed] [DOI] [Full Text] |
| 15. | Zhang T, Fu S, Cao X, Xia Y, Hu M, Feng Q, Cong Y, Zhu Y, Tang X, Wu M. Correlation of Peripheral Blood Inflammatory Indicators to Prognosis After Intravenous Thrombolysis in Acute Ischemic Stroke: A Retrospective Study. Int J Gen Med. 2024;17:985-996. [PubMed] [DOI] [Full Text] |
| 16. | Mao Y, Huang L, Ji G, Wang L, Wang X, Zheng X. Neutrophil-to-lymphocyte ratio on admission predicts early perihematomal edema growth after intracerebral hemorrhage. Medicine (Baltimore). 2024;103:e37585. [PubMed] [DOI] [Full Text] |
| 17. | Zhang S, Diao J, Qi C, Jin J, Li L, Gao X, Gong L, Wu W. Predictive value of neutrophil to lymphocyte ratio in patients with acute ST segment elevation myocardial infarction after percutaneous coronary intervention: a meta-analysis. BMC Cardiovasc Disord. 2018;18:75. [PubMed] [DOI] [Full Text] |
| 18. | Zeng Q, Wang S, Bai Z, Nie Y, Xu L, Chang D. Platelet-lymphocyte ratio predicts chemotherapy response and prognosis in patients with gastric cancer undergoing radical resection. Front Oncol. 2024;14:1279011. [PubMed] [DOI] [Full Text] |
| 19. | Chen X, Zhang Y, Liu Z, Song J, Li J. The inflammation score predicts the prognosis of gastric cancer patients undergoing Da Vinci robot surgery. J Robot Surg. 2024;18:131. [PubMed] [DOI] [Full Text] |
| 20. | Wang CY, Li XL, Ma XL, Yang XF, Liu YY, Yu YJ. Preoperative neutrophil-to-lymphocyte ratio predicts symptomatic anastomotic leakage in elderly colon cancer patients: Multicenter propensity score-matched analysis. World J Gastrointest Surg. 2024;16:438-450. [PubMed] [DOI] [Full Text] |
| 21. | Zhang KL, Zhou MM, Wang KH, Weng M, Zhou FX, Cui JW, Li W, Ma H, Guo ZQ, Li SY, Chen JQ, Wu XH, Zhao QC, Li JP, Xu HX, Shi HP, Song CH. Integrated neutrophil-to-lymphocyte ratio and handgrip strength better predict survival in patients with cancer cachexia. Nutrition. 2024;122:112399. [PubMed] [DOI] [Full Text] |
| 22. | Núñez KG, Sandow T, Fort D, Hibino M, Wright P, Cohen AJ, Thevenot PT. PD-1 expression in hepatocellular carcinoma predicts liver-directed therapy response and bridge-to-transplant survival. Cancer Immunol Immunother. 2022;71:1453-1465. [PubMed] [DOI] [Full Text] |
| 23. | Wang H, Huang H, Liu T, Chen Y, Li J, He M, Peng J, Liang E, Li J, Liu W. Peripheral blood lymphocyte subsets predict the efficacy of TACE with or without PD-1 inhibitors in patients with hepatocellular carcinoma: a prospective clinical study. Front Immunol. 2024;15:1325330. [PubMed] [DOI] [Full Text] |
| 24. | Chen JL, Guo L, Wu ZY, He K, Li H, Yang C, Han YW. Prognostic value of circulating tumor cells combined with neutrophil-lymphocyte ratio in patients with hepatocellular carcinoma. World J Gastrointest Oncol. 2024;16:372-385. [PubMed] [DOI] [Full Text] |
| 25. | She S, Shi J, Zhu J, Yang F, Yu J, Dai K. Impact of inflammation and the immune system on hepatocellular carcinoma recurrence after hepatectomy. Cancer Med. 2024;13:e7018. [PubMed] [DOI] [Full Text] |
| 26. | Yuana Y, Bertina RM, Osanto S. Pre-analytical and analytical issues in the analysis of blood microparticles. Thromb Haemost. 2011;105:396-408. [PubMed] [DOI] [Full Text] |