Published online Sep 18, 2024. doi: 10.5500/wjt.v14.i3.92859
Revised: May 6, 2024
Accepted: May 23, 2024
Published online: September 18, 2024
Processing time: 174 Days and 8.3 Hours
The probability of developing primary dysfunction (PD) is a function of the probability of ischemia/reperfusion (I/R) injury. The probability of I/R injury in turn, is a function of several donor and transplantation process variables, among which is ischemia time. Custodio et al studied the duration of a special type of warm ischemia and showed, contrary to what is known, that a longer duration is not statistically different from a shorter one in PD development. This finding opens the door to the unforeseen opportunity of training fellows in performing hepatectomies, since the duration will not jeopardize liver transplant outcomes, albeit with some precautions.
Core Tip: Custodio et al studied the duration of a novel warm ischemia, finding no differences in liver primary dysfunction among long and short times. Longer ischemia time is known to increase primary dysfunction probability, so this contradictory finding opens the door for an unforeseen opportunity that can improve liver transplantation outcomes.
- Citation: Gonzalez Cohens F, Gonzalez FM. Donor hepatectomy time and liver transplantation outcomes: An opportunity that cannot be dismissed. World J Transplant 2024; 14(3): 92859
- URL: https://www.wjgnet.com/2220-3230/full/v14/i3/92859.htm
- DOI: https://dx.doi.org/10.5500/wjt.v14.i3.92859
Solid organ transplantation is a complex process that includes four subprocesses: donor procurement, retrieval of organs from the donor (living or non-living donor), graft allocation, and surgical implantation of the organ in the recipient. An organized and properly conducted process can maximize the probability of graft function recovery, allowing long-term health of the recipient.
Primary graft non-function or dysfunction (depending on the severity of the condition) mostly adheres to three of the former subprocesses, excluding the allocation. The main determinants for primary dysfunction (PD) are: donor age, hepatic steatosis, cold ischemia time and liver ischemia/reperfusion (I/R) injury[1], transfusion of fresh frozen plasma[2], extended criteria donor[3], and place of procurement (local vs regional or national)[4]. However, not all of these factors impact the risk of PD similarly, as seen in Briceño et al[1] by logistic regression[1]: probability of I/R injury = e-0.7844 + 0.45 × high dopamine doses (yes 1/no 0) + 1.29 × macrosteatosis II–III (yes 1/no 0) + 0.1040 × cold ischemia time (hr) + 0.5844 × prolonged intensive care units (ICU) stay (yes 1/no 0) + 0.0172 × donor age(year).
In turn, the probability of developing PD is better explained by a simple third-order function of the probability of I/R injury (P [I/R]) as: Probability of PD = 0.106 + 0.169 × P(I/R) + 1.209 × P(I/R)2 - 0.0886 × P(I/R)3
From a clinical perspective, these regression models teach us that an extended criteria non-living donor which is also hard to manage (prolonged ICU stay and high inotropic support) jeopardizes the liver graft (even more if the graft presents macrosteatosis) by making it more prone to develop I/R injury, which also predispose to experiencing PD. In other words, I/R injury is the most important predisposing factor to the development of postoperative liver graft dysfunction.
Interestingly, the previous cubic function describes that the probability of experiencing PD has a morphology similar to a Gompertz function and the hemoglobin oxygen saturation and dissociation function (sigmoidal or S-shaped), suggesting that there is a window of opportunity to prevent PD. Window that is strongly dependent on maintaining the I/R damage below a certain threshold (Figure 1).
Even though cold ischemia time is one of the smallest contributors towards I/R injury probability (and as such, less considered in studies), Custodio et al[5] looked for the effect of the donor hepatectomy time, which is a “novel” type of warm ischemia time between the aortic cross-clamping and inserting the liver in a storage and transportation system maintained at low temperatures, presumably in a static temperature cooler. In a Brazilian multicenter retrospective study, they found that the hepatectomy time in those patients who developed PD was not statistically different from those patients who did well. Moreover, the crude time lapses tended to be longer in this last group, contradicting “common sense.”
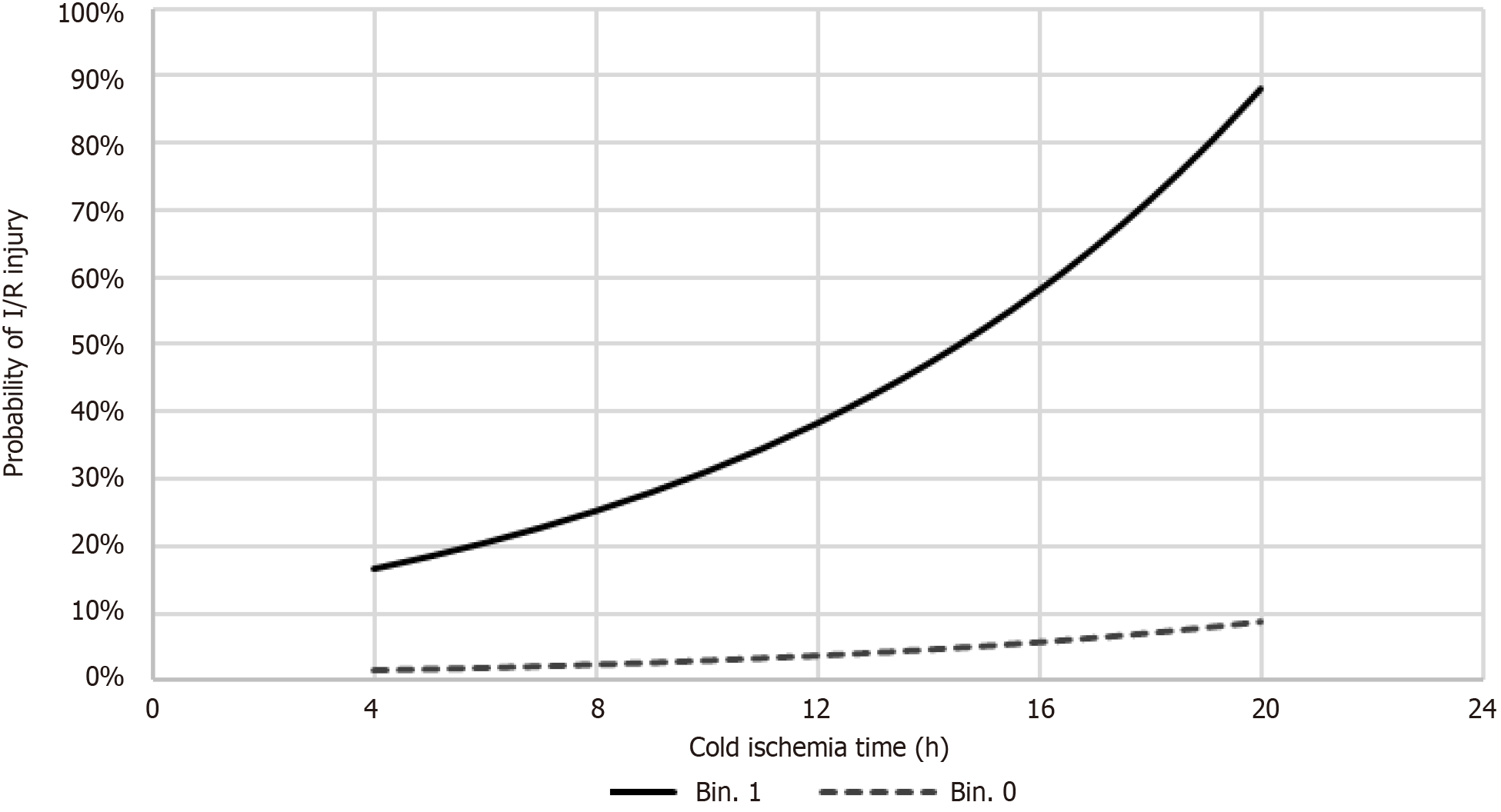
PD in Custodio´s experience was 25% compared to 21%-26% in a literature review[2], showing that their experience could be comparable to other liver transplantation teams. Figure 2 shows the probability of I/R injury against cold ischemia time, which includes the donor hepatectomy time according to Custodio et al[5]. It is clear that I/R injury has a low probability of occurrence if the donor was healthy, but it will be much more probable in expanded criteria donors.
By proving that the short period of warm ischemia does not significantly impact the probability of I/R injury, and thus PD, their findings open the door for an important and unexpected opportunity. Currently, procurement teams know that they can train their fellows to perform hepatectomies without significantly jeopardizing the graft postoperative course. Nonetheless, and as shown in Figure 2, this suggestion is only safe when fellow are allowed to retrieve the liver from donors with good prognostic indexes since ischemia time will not significantly impact the probability of I/R injury. In cases of expanded criteria donors, it is still advisable to have senior surgeons perform their hepatectomies (Figure 2).
After a hepatectomy, cold storage for transporting the liver to the transplant institution plays a significant role. There are two main mechanisms for that: standard static temperature coolers and cold perfusion machines. As this last one is associated with a lower probability of PD, especially in expanded criteria donors[6], using them could be another tool to increase training opportunities for fellows, even for expanded criteria donors.
Custodio et al[5] teaches us that training fellows in their surgical capabilities can increase the supply of livers for transplantation for the ill or severely ill patients on waiting lists. Better surgical abilities can improve the quality of organs, which consequently enhances the recovery of these patients’ health, preventing premature death. In other words, there is room for improving liver transplant results from an unexpected stage of the procurement process. But there are other subprocesses of the transplantation process that can certainly be improved to obtain better transplant outcomes. These include expediting the procurement process by improving the detection and referral of possible organ donors to the procurement units[7], enhancing physiological maintenance in the critical care units of severely ill potential non-living organ donors, expediting organ donation requests, improving harvesting surgeries by avoiding delays, main
| 1. | Briceño J, Ciria R, de la Mata M, Rufián S, López-Cillero P. Prediction of graft dysfunction based on extended criteria donors in the model for end-stage liver disease score era. Transplantation. 2010;90:530-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 74] [Article Influence: 4.9] [Reference Citation Analysis (35)] |
| 2. | Salviano MEM, Lima AS, Tonelli IS, Correa HP, Chianca TCM. Primary liver graft dysfunction and non-function: integrative literature review. Rev Col Bras Cir. 2019;46:e2039. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (36)] |
| 3. | Vodkin I, Kuo A. Extended Criteria Donors in Liver Transplantation. Clin Liver Dis. 2017;21:289-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 140] [Article Influence: 17.5] [Reference Citation Analysis (35)] |
| 4. | Nicolau-Raducu R, Cohen AJ, Bokhari A, Bohorquez H, Bruce D, Carmody I, Bugeaud E, Seal J, Sonnier D, Nossaman B, Loss G. Predictive model and risk factors associated with a revised definition of early allograft dysfunction in liver transplant recipients. Clin Transplant. 2017;31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (38)] |
| 5. | Custodio G, Massutti AM, Caramori A, Pereira TG, Dalazen A, Scheidt G, Thomazini L, Leitão CB, Rech TH. Association of donor hepatectomy time with liver transplantation outcomes: A multicenter retrospective study. World J Transplant. 2024;14:89702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (17)] |
| 6. | Liang A, Cheng W, Cao P, Cai S, Zhang L, Zhong K, Nie Y. Effects of machine perfusion strategies on different donor types in liver transplantation: a systematic review and meta-analysis. Int J Surg. 2023;109:3617-3630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 13] [Article Influence: 6.5] [Reference Citation Analysis (35)] |
| 7. | Gonzalez F, Vera F, Gonzalez F, Velasquez JD. Kefuri: A novel technological tool for increasing organ donation in Chile. 2020 IEEE/WIC/ACM International Joint Conference on Web Intelligence and Intelligent Agent Technology (WI-IAT). 2020;. [DOI] [Full Text] |