Published online Jun 18, 2024. doi: 10.5500/wjt.v14.i2.89825
Revised: February 16, 2024
Accepted: April 16, 2024
Published online: June 18, 2024
Processing time: 200 Days and 2.7 Hours
With an ongoing demand for transplantable organs, optimization of donor management protocols, specifically in trauma populations, is important for obta
To determine if levothyroxine use in combination with steroids in BPODs increased the number of organs donated in trauma patients.
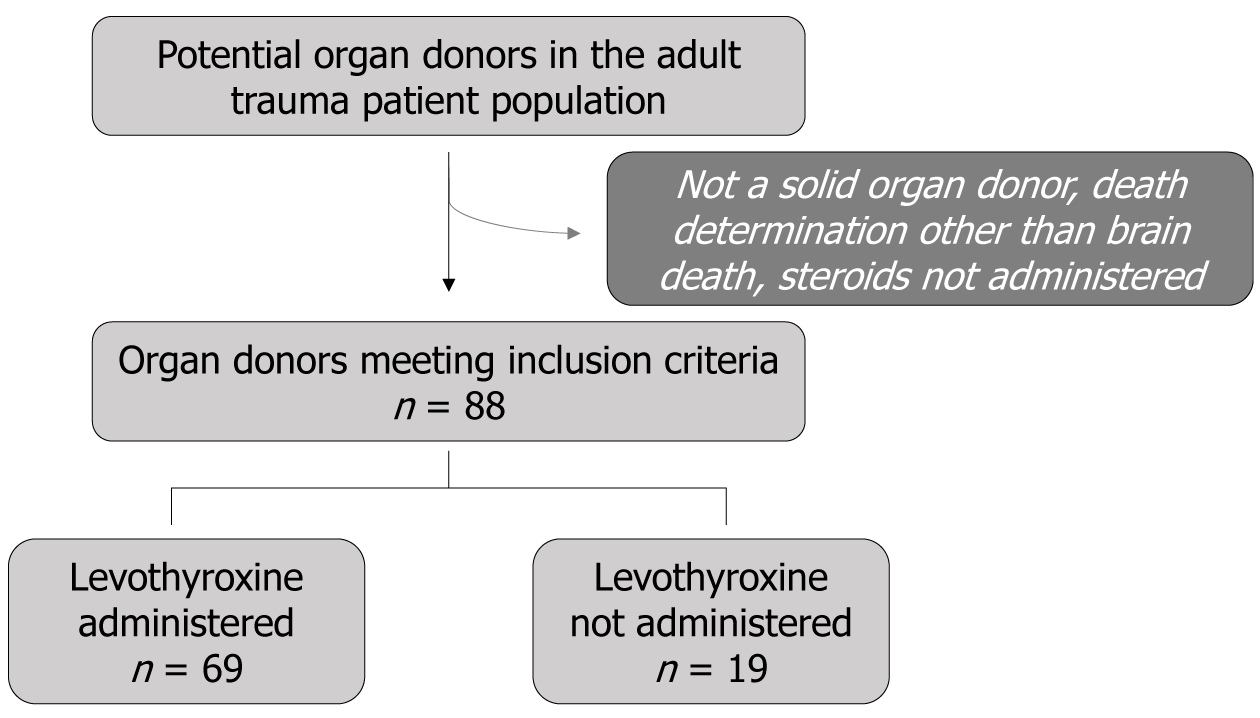
A retrospective review of adult BPODs from a single level 1 trauma center over ten years was performed. Exclusion criteria included patients who were not solid organ donors, patients who were not declared brain dead (donation after circulatory death), and patients who did not receive steroids in their hospital course. Levothyroxine and steroid administration, the number of organs donated, the types of organs donated, and demographic information were recorded. Univariate analyses were performed with P < 0.05 considered to be statistically significant.
A total of 88 patients met inclusion criteria, 69 (78%) of whom received levothyroxine and steroids (ST/LT group) vs 19 (22%) receiving steroids without levothyroxine (ST group). No differences were observed between the groups for gender, race, pertinent injury factors, age, or other hormone therapies used (P > 0.05). In the ST/LT group, 68.1% (n = 47) donated a high yield (3-5) of organ types per donor compared to 42.1% (n = 8) in the ST group (P = 0.038). There was no difference in the total number of organ types donated between the groups (P = 0.068).
This study suggests that combining levothyroxine and steroid administration increases high-yield organ donation per donor in BPODs in the trauma patient population. Limitations to this study include the retrospective design and the relatively small number of organ donors who met inclusion criteria. This study is unique in that it mitigates steroid administration as a confounding variable and focuses specifically on the adjunctive use of levothyroxine.
Core Tip: The present study considers the impact of combination endocrine management on the number of solid organs donated in brain-dead organ donors. Specifically, we focused on the use of steroids alone or steroids and levothyroxine in organ donors of the trauma patient population from a single level 1 trauma center. We showed a significant association between a high yield of organs donated per donor and the use of combination hormone replacement therapy as compared to steroids alone. These data complement published literature on combination endocrine management and highlight the role of levothyroxine on the number of organs recovered per organ donor.
- Citation: Gallegos EM, Reed T, Deville P, Platt B, Leonardi C, Bellfi L, Dufrene J, Chaudhary S, Hunt J, Stuke L, Greiffenstein P, Schoen J, Marr A, Paramesh A, Smith AA. Does the use of double hormone replacement therapy for trauma patient organ donors improve organ recovery for transplant. World J Transplant 2024; 14(2): 89825
- URL: https://www.wjgnet.com/2220-3230/full/v14/i2/89825.htm
- DOI: https://dx.doi.org/10.5500/wjt.v14.i2.89825
Aggressive organ donor management has been shown to yield positive outcomes for organ donation[1-4]. With an ongoing demand for transplantable organs, optimization of donor management protocols, specifically in trauma populations, is important for obtaining a high yield of viable organs per patient. Hormone replacement therapy is an area of intensive care protocols that the Society of Critical Care Medicine has advised, however there is little evidence supporting its efficacy[1,4,5]. Hormone therapy may preserve the potential for organ donation in patients that have experienced non-survivable catastrophic brain injuries or after brain death declaration, but protocols for implementing these interventions are ill-defined[1,6]. The value of combination steroid and thyroid hormone replacement in hemodynamically stable or unstable patients is still under debate, as studies looking at the beneficial effects of these interventions show mixed results[4,7].
The goal of this study was to assess the role of double hormone replacement therapy, including steroid and levo
A retrospective review of adult patients who were eligible for organ donation from a level 1 trauma center between July 2012 and March 2021 was performed. The trauma registry was used to find patients meeting the inclusion criteria. Inclusion criteria were as follows: Patients 18 years of age or older who were declared brain dead, were solid organ donors and were administered steroids (methylprednisolone, hydrocortisone, or both) during their hospital course. These patients underwent chart review using electronic medical records and records from the associated organ procurement organization. Exclusion criteria were patients younger than 18 years of age, patients who were not solid organ donors, patients who were not declared brain dead (such as patients who donated after circulatory death), and patients who did not receive steroids (methylprednisolone, hydrocortisone, or both) in their hospital course (Figure 1). Brain death determination was made using two confirmatory brain death exams and, in some cases, ancillary tests including cerebral perfusion scans. The Institutional Review Board approved this study, and a waiver of informed consent was obtained. There were no set trauma intensive care unit guidelines for management of potential organ donors, and management was left to the discretion of the attending physician.
Demographic data such as age, race, and gender were collected. Pertinent injury factors were recorded, including injury severity score, type of injury (blunt or penetrating), and presence of traumatic brain injury (TBI). A donated organ was defined as any organ recovered by the organ procurement organization. The type of solid organs donated, including lungs, kidneys, heart, liver, and pancreas, were recorded. The types of solid organs donated were then summed to range between 1-5 organ types per donor. For example, two donated kidneys would still only be counted as one type. A high yield of organs recovered per donor was defined as 3-5 organ types donated by an individual donor.
Data on treatment for other endocrine disorders, such as diabetes insipidus (DI) and hyperglycemia, were also collected. DI treatment was identified as desmopressin or vasopressin administration following suspected DI due to polyuria (> 2.5-3 mL/h/kg), hypernatremia (> 150 mEg/L), high serum osmolarity (> 295 mOsm/L), and/or low urine osmolarity (< 200 mOsm/L)[10]. Insulin requirement was recorded as hyperglycemia treatment.
Patients were then divided into two groups: Those receiving levothyroxine plus steroids (ST/LT group) vs those only receiving steroids without levothyroxine (ST group). Data was analyzed using statistic analysis system (SAS) version 9.4 (SAS Institute Inc, Cary, NC, United States). Variables collected are reported as either median and minimum and maximum for not normally distributed count variables or proportions for categorical variables. Univariable analyses were conducted to compare demographic and clinical donors’ characteristics and donated organs between two groups (ST vs ST/LT) using the χ2 test or the exact test when comparing proportions and the Mann-Whitney U test when comparing medians. A two-sided P value less than 0.05 indicated statistical significance.
Of the patients reviewed, a total of eighty-eight organ and tissue donors met the study inclusion criteria (Figure 1). Of these organ donors, 78% received levothyroxine and steroids (ST/LT group, n = 69) vs 22% receiving steroids alone (ST group, n = 19).
No significant differences were observed between the two groups in the reported patients’ demographical and clinical characteristics (Table 1). Patients’ ages ranged from 18 years-75 years old in the ST group and 20 years-75 years old in the ST/LT group, with the majority in each being male (68.4% vs 81.2%, P = 0.232, respectively). In the ST compared to the ST/LT group, 31.6% vs 46.4% were African American/Black, 57.9% vs 43.5% were Caucasian/White, and 10.5% vs 10.1% were of a different racial background, respectively (P = 0.483). Regarding clinical characteristics of the patients, the median injury severity score was 25 (4–54) in the ST group and 29 (9-75) in the ST/LT group (P = 0.911). Blunt injuries occurred in 73.7% (n = 14) of the ST group patients and 60.9% of the ST/LT group patients, with 26.3% and 39.1%, respectively, having penetrating injuries (P = 0.304). In the ST group, 84.2% of patients had a TBI, and in the ST/LT group, 94.2% had a TBI (P = 0.169). Other than LT and ST, endocrine protocols used were insulin administration for hyperglycemia treatment and desmopressin or vasopressin administration for DI treatment. Insulin was administered in 57.9% of ST group patients and 55.1% of ST/LT patients (P = 0.826). Finally, DI was treated in 31.6% of ST group patients and 40.6% of ST/LT group patients (P = 0.476) (Table 1).
| Item | ST (n = 19) | ST/LT (n = 69) | P value | |
| Age (yr), median (min–max) | 36 (20–75) | 32 (18–75) | 0.214 | |
| Gender | 0.232 | |||
| Male | 68.4 (13) | 81.2 (56) | ||
| Female | 31.6 (6) | 18.8 (13) | ||
| Race | 0.483 | |||
| African American/Black | 31.6 (6) | 46.4 (32) | ||
| Caucasian/White | 57.9 (11) | 43.5 (30) | ||
| Other | 10.5 (2) | 10.1 (7) | ||
| Injury type | 0.304 | |||
| Blunt | 73.7 (14) | 60.9 (42) | ||
| Penetrating | 26.3 (5) | 39.1 (27) | ||
| ISS, median (min–max) | 25 (4–54) | 29 (9–75) | 0.911 | |
| TBI | 84.2 (16) | 94.2 (65) | 0.169 | |
| Insulin | 57.9 (11) | 55.1 (38) | 0.826 | |
| DI | 31.6 (6) | 40.6 (28) | 0.476 | |
Organ donation summaries for the patients are reported in Table 2. The median number of organ types donated [median (min-max)] was not significantly different between the two groups and were 2 (1-5) for the ST group and 3 (1-5) for the ST/LT group (P = 0.068, Table 2). A significantly higher proportion of patients with a high yield of organs (3-5 organ types per donor) was observed in the ST/LT group compared to the ST group (68.1% vs 42.1%, P = 0.038, Table 2). No individual organ type was donated at a significantly higher proportion between the treatment groups (P > 0.05, Table 2). Furthermore, although non-statistically significant, all organs were donated at a numerically higher proportion for the ST/LT group compared to the ST group, except for kidneys, which had a very high donation rate (> 90% in both treatment groups, Table 2).
| Item | ST (n = 19) | ST/LT (n = 69) | P value |
| Total number, median (min-max) | 2 (1–5) | 3 (1–5) | 0.068 |
| Donation of 3 or more organs | 42.1 (8) | 68.1 (47) | 0.038 |
| Organ type | |||
| Heart | 42.1 (8) | 59.4 (41) | 0.179 |
| Kidney | 94.7 (18) | 91.3 (63) | 0.624 |
| Liver | 79.0 (15) | 92.8 (64) | 0.079 |
| Lung | 21.1 (4) | 39.1 (27) | 0.144 |
| Pancreas | 26.3 (5) | 36.2 (25) | 0.419 |
Meeting the demand for transplantable organs remains an ongoing challenge, making the optimization of interventional protocols, specifically in trauma populations, an essential part of maximizing the number of organs obtained per patient. Steroids are routinely used for potential brain-dead organ donors in the trauma population. However, the current literature lacks in consistently controlling for steroid use when comparing outcomes between combination therapies[4,8,11,12].
The present study compared steroids in adjunct with levothyroxine to steroids alone in brain-dead potential organ donors (BPODs) and found an increase in high-yield organ donation per donor (i.e., 3-5 organ types donated per donor) in the ST/LT group compared to the ST group. There was no difference in the total number donated or the number of individual organs donated between the groups. Notably, there was no decrease in organs donated in the ST/LT group compared to the ST group, suggesting there was no identifiable negative association of LT treatment in this cohort of organ donors in the trauma patient population.
The history of research on including levothyroxine as an intervention for potential organ donors has been mixed[1,7]. For a recent review of the literature on levothyroxine’s role in hormone replacement therapy, see Turco et al[5], 2019. In short, circulating levothyroxine was shown to decrease after brain death in several studies, and pre-clinical studies indicated a potential role of levothyroxine replacement in maintaining perfusion of organs via increased hemodynamic stability[5,13]. Following these findings, numerous clinical studies ranging from small prospective to large retrospective studies identified levothyroxine alone or in combination hormone replacement therapy as beneficial in regards to donor hemodynamic status or organ retrieval rates and outcomes[11,12,14,15]. Clinical trials studying levothyroxine, however, have failed to elucidate a beneficial effect of levothyroxine therapy on the organs of brain-dead donors[7,16-19]. Limitations to these studies include inconsistent outcome measures and, in the case of randomized controlled trials (RCTs), small numbers of hemodynamically unstable patients[19,20]. In addition, quality RCTs evaluating the benefit of combination hormone replacement therapy are lacking[21]. An ongoing multicenter randomized controlled trial including 800 brain-dead, hemodynamically unstable organ donors may clarify whether heart donation, heart function, and/or vasopressor requirements are impacted specifically by intravenous thyroxine treatment[22]. However, as organ procurement organizations are allowed to continue their other individual standard donor management protocols, it is not yet clear how or whether the contributions of other hormone replacement therapies, such as steroids, will be considered[22]. Still, a comparative study showed evidence that levothyroxine intervention before brain death was beneficial in increasing the number of organs donated[23]. One other study identified the timing of hormone replacement therapy as an important factor after catastrophic brain injury, but few studies have been able to give clear guidance on when hormone intervention should be initiated[6]. Timing, then, may also impact the findings in RCTs based on whether levothyroxine treatment was initiated before or after brain death and how long the patients were exposed to the treatment. Similarly, understanding the optimal timing of levothyroxine administration in relation to when steroid interventions are started will aid in determining appropriate endocrine protocols for BPODs in the trauma patient population. In summary, the proper usage of levothyroxine or combination replacement therapy in catastrophic brain injury or after brain death is still under debate. Still, previous literature, as well as the present study, highlight the potential benefits of LT and combination therapy in increasing organ donation after brain death.
While the present study did not focus on stability parameters of the patient population, prospective studies may be able to better differentiate the impact of levothyroxine and steroid therapies on stable compared to unstable patients. Study limitations include its retrospective and single-center nature. Other potential confounders of the results include the vasopressor requirements, cardiovascular stability, timing of hormone therapy administration, and length of time on the therapy. Future prospective studies controlling for these factors may elucidate other important aspects of treating potential organ donors in cases of imminent or confirmed brain death. With multiple cohort studies indicating significant impacts of combination therapy, more clinical trials with sufficient power investigating combination instead of single therapy are warranted.
In conclusion, this retrospective study showed an increase in high-yield organ donation per donor when levothyroxine was adjunctively administered with steroids in BPODs as compared to BPODs administered steroids alone. These results, along with previous reports from RCTs, call for further investigation of the use of levothyroxine in adjunct with steroids for the management of brain-dead organ donors.
| 1. | Kotloff RM, Blosser S, Fulda GJ, Malinoski D, Ahya VN, Angel L, Byrnes MC, DeVita MA, Grissom TE, Halpern SD, Nakagawa TA, Stock PG, Sudan DL, Wood KE, Anillo SJ, Bleck TP, Eidbo EE, Fowler RA, Glazier AK, Gries C, Hasz R, Herr D, Khan A, Landsberg D, Lebovitz DJ, Levine DJ, Mathur M, Naik P, Niemann CU, Nunley DR, O'Connor KJ, Pelletier SJ, Rahman O, Ranjan D, Salim A, Sawyer RG, Shafer T, Sonneti D, Spiro P, Valapour M, Vikraman-Sushama D, Whelan TP; Society of Critical Care Medicine/American College of Chest Physicians/Association of Organ Procurement Organizations Donor Management Task Force. Management of the Potential Organ Donor in the ICU: Society of Critical Care Medicine/American College of Chest Physicians/Association of Organ Procurement Organizations Consensus Statement. Crit Care Med. 2015;43:1291-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 227] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 2. | Joseph B, Aziz H, Sadoun M, Kulvatunyou N, Pandit V, Tang A, Wynne J, O' Keeffe T, Friese RS, Gruessner RW, Rhee P. Fatal gunshot wound to the head: the impact of aggressive management. Am J Surg. 2014;207:89-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Salim A, Martin M, Brown C, Rhee P, Demetriades D, Belzberg H. The effect of a protocol of aggressive donor management: Implications for the national organ donor shortage. J Trauma. 2006;61:429-33; discussion 433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 87] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Anwar ASMT, Lee JM. Medical Management of Brain-Dead Organ Donors. Acute Crit Care. 2019;34:14-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 44] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 5. | Turco LM, Glorsky SL, Winfield RD. Hormone replacement therapy in brain-dead organ donors: a comprehensive review with an emphasis on traumatic brain injury. J Trauma Acute Care Surg. 2019;86:702-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Lam L, Inaba K, Branco BC, Putty B, Salim A, Green DJ, Talving P, Demetriades D. The impact of early hormonal therapy in catastrophic brain-injured patients and its effect on organ procurement. Am Surg. 2012;78:318-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Latifi M, Bagherpour F, Rahban H, Pourhossein E, Dehghani S. Brain death hormone therapy and Graft survival: A systematic review of the literature. Transplant Rep. 2022;7:100098. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Dupuis S, Amiel JA, Desgroseilliers M, Williamson DR, Thiboutot Z, Serri K, Perreault MM, Marsolais P, Frenette AJ. Corticosteroids in the management of brain-dead potential organ donors: a systematic review. Br J Anaesth. 2014;113:346-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Pinsard M, Ragot S, Mertes PM, Bleichner JP, Zitouni S, Cook F, Pierrot M, Dube L, Menguy E, Lefèvre LM, Escaravage L, Dequin PF, Vignon P, Pichon N. Interest of low-dose hydrocortisone therapy during brain-dead organ donor resuscitation: the CORTICOME study. Crit Care. 2014;18:R158. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Zirpe K, Gurav S. Brain Death and Management of Potential Organ Donor: An Indian Perspective. Indian J Crit Care Med. 2019;23:S151-S156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Novitzky D, Mi Z, Sun Q, Collins JF, Cooper DK. Thyroid hormone therapy in the management of 63,593 brain-dead organ donors: a retrospective analysis. Transplantation. 2014;98:1119-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 12. | Rosendale JD, Kauffman HM, McBride MA, Chabalewski FL, Zaroff JG, Garrity ER, Delmonico FL, Rosengard BR. Aggressive pharmacologic donor management results in more transplanted organs. Transplantation. 2003;75:482-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 185] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 13. | Novitzky D, Wicomb WN, Cooper DK, Tjaalgard MA. Improved cardiac function following hormonal therapy in brain dead pigs: relevance to organ donation. Cryobiology. 1987;24:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Van Bakel AB, Pitzer S, Drake P, Kay NA, Stroud M, Sade RM. Early hormonal therapy stabilizes hemodynamics during donor procurement. Transplant Proc. 2004;36:2573-2578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Salim A, Martin M, Brown C, Inaba K, Roth B, Hadjizacharia P, Mascarenhas A, Rhee P, Demetriades D. Using thyroid hormone in brain-dead donors to maximize the number of organs available for transplantation. Clin Transplant. 2007;21:405-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Goarin JP, Cohen S, Riou B, Jacquens Y, Guesde R, Le Bret F, Aurengo A, Coriat P. The effects of triiodothyronine on hemodynamic status and cardiac function in potential heart donors. Anesth Analg. 1996;83:41-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Venkateswaran RV, Patchell VB, Wilson IC, Mascaro JG, Thompson RD, Quinn DW, Stockley RA, Coote JH, Bonser RS. Early donor management increases the retrieval rate of lungs for transplantation. Ann Thorac Surg. 2008;85:278-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 18. | Venkateswaran RV, Steeds RP, Quinn DW, Nightingale P, Wilson IC, Mascaro JG, Thompson RD, Townend JN, Bonser RS. The haemodynamic effects of adjunctive hormone therapy in potential heart donors: a prospective randomized double-blind factorially designed controlled trial. Eur Heart J. 2009;30:1771-1780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 99] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 19. | Macdonald PS, Aneman A, Bhonagiri D, Jones D, O'Callaghan G, Silvester W, Watson A, Dobb G. A systematic review and meta-analysis of clinical trials of thyroid hormone administration to brain dead potential organ donors. Crit Care Med. 2012;40:1635-1644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 92] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 20. | Bera KD, Shah A, English MR, Ploeg R. Outcome measures in solid organ donor management research: a systematic review. Br J Anaesth. 2021;127:745-759. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Wong J, Tan HL, Goh JPS. Management of the brain dead organ donor. Trends Anaesth Crit Care. 2017;13:6-12. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | Dhar R, Klinkenberg D, Marklin G. A multicenter randomized placebo-controlled trial of intravenous thyroxine for heart-eligible brain-dead organ donors. Trials. 2021;22:852. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Joseph B, Aziz H, Pandit V, Kulvatunyou N, Sadoun M, Tang A, O'Keeffe T, Green DJ, Friese RS, Rhee P. Levothyroxine therapy before brain death declaration increases the number of solid organ donations. J Trauma Acute Care Surg. 2014;76:1301-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |