Published online Aug 18, 2022. doi: 10.5500/wjt.v12.i8.259
Peer-review started: January 16, 2022
First decision: March 16, 2022
Revised: March 30, 2022
Accepted: July 31, 2022
Article in press: July 31, 2022
Published online: August 18, 2022
Processing time: 213 Days and 7.8 Hours
The average age of recipients and donors of liver transplantation (LT) is in
To assess the clinical characteristics, age-related trends, and outcomes of LT among the older population in the United States.
We analyzed data from the United Network for Organ Sharing database between 1987-2019. The sample was split into younger group (18-64 years old) and older group (≥ 65 years old).
Between 1987-2019, 155758 LT were performed in the United States. During this period there was a rise in median age of the recipients and percentage of LT recipients who were older than 65 years increased (P < 0.05) with the highest incidence of LT among older population seen in 2019 (1920, 23%). Common primary etiologies of liver disease leading to LT in older patients when compared to the younger group, were non-alcoholic steatohepatitis (16.4% vs 5.9%), hepatocellular carcinoma (14.9% vs 6.9%), acute liver failure (2.5% vs 5.2%), hepatitis C cirrhosis (HCV) (19.2 % vs 25.6%) and acute alcoholic hepatitis (0.13% vs 0.35%). In older recipient group female sex and Asian race were higher, while model for end-stage liver disease (MELD) score and rates of preoperative mechanical ventilation were lower (P < 0.01). Median age of donor, female sex, body mass index (BMI), donor HCV positive status, and donor risk index (DRI) were significantly higher in older group (P < 0.01). In univariable analysis, there was no difference in post-transplant length of hospitalization, one-year, three-year and five-year graft survivals between the two groups. In multivariable Cox-Hazard regression analysis, older group had an increased risk of graft failure during the five-year post-transplant period (hazard ratio: 1.27, P < 0.001). Other risk factors for graft failure among recipients were male sex, African American race, re-transplantation, presence of diabetes, mechanical ventilation at the time of LT, higher MELD score, presence of portal vein thrombosis, HCV positive status, and higher DRI.
While there is a higher risk of graft failure in older recipient population, age alone should not be a contraindication for LT. Careful selection of donors and recipients along with optimal manage
Core Tip: Liver transplantation (LT) among older patients is becoming more acceptable in the United States. The overall outcomes of LT for patients ≥ 65 years are comparable to younger recipients. While there is a higher risk of graft failure in older recipient population, age alone should not be a contraindication for LT. Careful selection of donors and recipients along with optimal management of risk factors during the postoperative period are necessary to maximize the transplant outcomes in this population.
- Citation: Okumura K, Lee JS, Dhand A, Sogawa H, Veillette G, John D, Misawa R, Bodin R, Wolf DC, Diflo T, Nishida S. Trends and outcomes of liver transplantation among older recipients in the United States. World J Transplant 2022; 12(8): 259-267
- URL: https://www.wjgnet.com/2220-3230/full/v12/i8/259.htm
- DOI: https://dx.doi.org/10.5500/wjt.v12.i8.259
Liver disease is one of the most frequent causes of death in the United States[1,2]. Liver transplantation (LT) is the most effective life-saving treatment for patients with end-stage liver disease and liver failure. Over the past few decades, the number of LT in the United States has increased and outcomes of these transplants have significantly improved[3,4]. According to the United Network for Organ Sharing (UNOS) database, in 1987 there were 1713 LT performed in the United States. Since then, there has been a more than five-fold increase in the number of LTs, with 8906 cases performed in 2020. As the general population becomes older, the average ages of LT recipients and donors have increased as well[5]. Over the past three decades, the characteristic of donors and recipients of LT for end-stage liver disease has changed considerably[3,6-8]. Our goal was to assess trends in the etiology of underlying liver disease, and outcomes of LT among older population in the United States.
We evaluated all patients 18 years or older who underwent LT in the United States from January 1, 1987 to December 31, 2019 in the UNOS database. Patients without a documented primary diagnosis were excluded from the analyses. This study was approved by our Institutional Review Board.
All data were collected from the UNOS registry. Demographic information, such as listing diagnosis, age, gender and race, along with time on waiting list prior to transplant were included in the analyses. Additional variables, such as model for end-stage liver disease (MELD) score at listing on the waitlist and at the time of transplant, body mass index (BMI), pre-transplant diabetes mellitus (DM), hepatitis C virus (HCV) status, dialysis prior to transplant, previous abdominal surgery, spontaneous bacterial peritonitis, trans-jugular intrahepatic portosystemic shunt, portal vein thrombosis, mechanical ventilation status and donor risk index (DRI)[9], were included as well. The study groups were defined as older (≥ 65 years old) and younger (18-64 years old).
Statistical analyses were performed using IBM SPSS Statistics 26.0 (IBM Corp., Armonk, NY, United States). Non-parametric analyses were used to compare continuous variables (Mann-Whitney U test) and categorical variables (Chi-square test or Fisher’s exact test). The overall survival and graft survival were calculated from the date of transplant to the date of the event using the Kaplan-Meier method. Survival curves were compared by using the log-rank test. Cox-Hazard regression analyses were applied to assess the association between multiple covariate factors and survival rates between two groups. Results were presented as hazard ratios and reported with 95% confidence intervals with P values. P < 0.01 was taken as statistically significant.
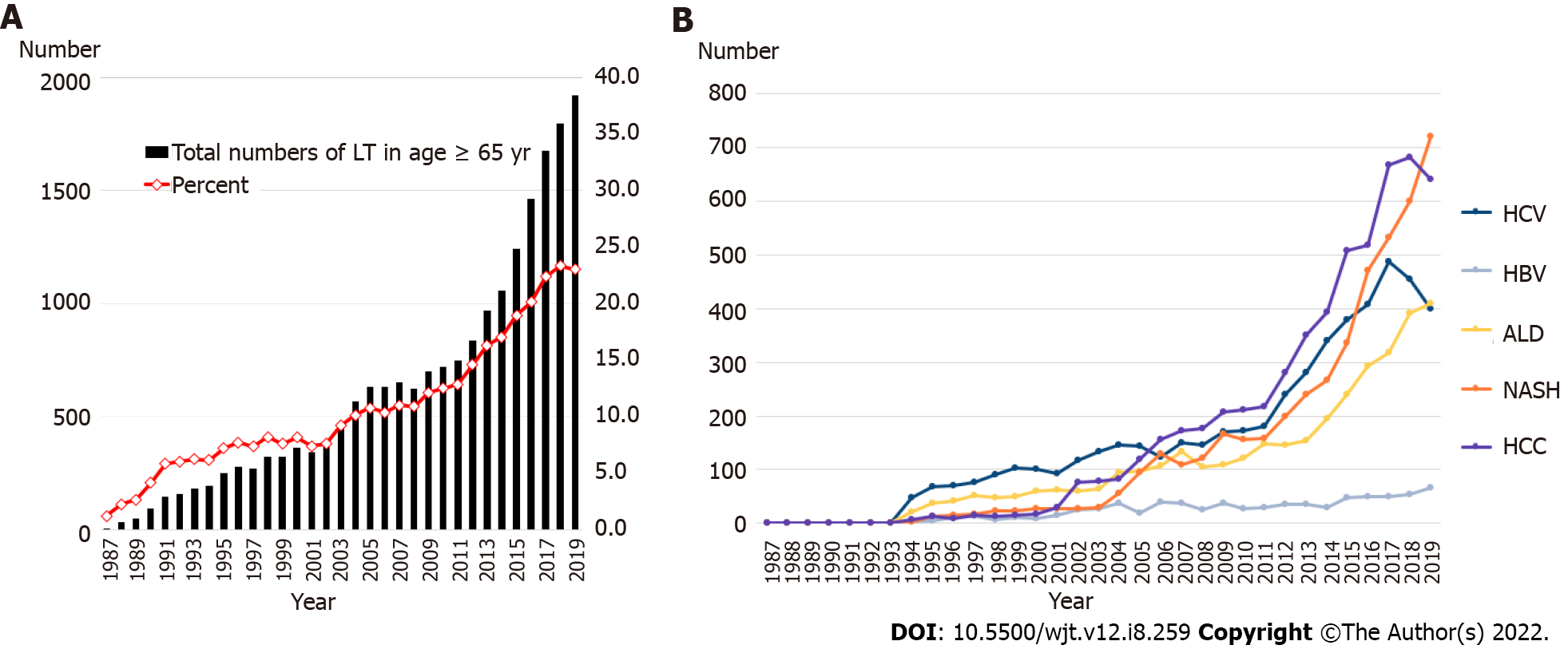
Of the 155758 individuals who received a LT during the study period, 20000 were in older group (≥ 65 years old) and 135758 patients were in younger group (18-64 years old). The trends of LT in older patients are shown in Figure 1A. The overall number and percentage of LT in older group increased over the years, and the percentage of older recipients became > 20% after 2016. The trends of indications for LT in the older population is shown in Figure 1B. HCV cirrhosis was the most common indication for LT from 1994 to 2005. The number of patients requiring LT due to hepatocellular carcinoma (HCC) and non-alcoholic steatohepatitis (NASH) also gradually increased during the study period. HCC became the most common indication for LT in older group from 2006 to 2018. In 2019, NASH became the most common indication for LT in older group.
Table 1 presents the characteristics of recipients who underwent LT during the study period. The median age of recipients was 52 years in the younger group and 67 years in the older group. Recipients in older group were more likely to be female, White, and Asian compared to those in younger group (P < 0.001). Recipients in younger group were more likely to be HCV positive and have portal vein thrombosis, while recipients in older group were more likely to have pre-transplant DM. For primary etiology of liver disease, younger group was more likely to have alcohol-related liver disease (ALD), HCV cirrhosis and acute liver failure, while older group was more likely to have NASH and HCC. Additionally, the younger group was more likely to be on mechanical ventilation at the time of LT and have a prior history of LT.
| Young group, age 18-64 (n = 135758) | Older group, age ≥ 65 (n = 20000) | P value | |
| Age (IQR) | 52 (45-58) | 67 (66-69) | < 0.001 |
| Female, n (%) | 47934 (35.3) | 7612 (38.1) | < 0.001 |
| Race, % | < 0.001 | ||
| White | 73.5 | 75.5 | |
| Black | 8.9 | 6.0 | |
| Hispanic/Latino | 12.5 | 12.1 | |
| Asian | 3.8 | 5.4 | |
| Others | 1.3 | 0.9 | |
| BMI (IQR) | 27.4 (24.0-31.7) | 27.7 (24.5-31.5) | 0.571 |
| HCV, % | 44876 (33.1) | 5236 (26.2) | < 0.001 |
| Diabetes, n (%) | 226584 (22.3) | 6784 (35.7) | < 0.001 |
| L1-MELD | 18 (12-26) | 15 (10-22) | < 0.001 |
| R2-MELD | 21 (14-30) | 18 (12-26) | < 0.001 |
| Primary disease, % | |||
| Alcohol cirrhosis | 22.3 | 15.3 | < 0.001 |
| HCV cirrhosis | 25.2 | 19.0 | < 0.001 |
| NASH | 5.9 | 16.4 | < 0.001 |
| HCC | 6.9 | 14.9 | < 0.001 |
| Acute liver failure | 5.2 | 2.5 | < 0.001 |
| Acute alcoholic hepatitis | 0.35 | 0.13 | < 0.001 |
| Previous surgery, n (%) | 48407 (35.7) | 8899 (44.5) | < 0.001 |
| SBP, n (%) | 9147 (6.7) | 1084 (5.4) | < 0.001 |
| TIPSS, n (%) | 7231 (5.3) | 1187 (5.9) | 0.001 |
| Portal vein thrombosis, n (%) | 4875 (3.6) | 1162 (5.8) | < 0.001 |
| Mechanical ventilation, n (%) | 10464 (7.6) | 888 (4.3) | < 0.001 |
| Dialysis, n (%) | 14284 (10.5) | 2059 (10.3) | 0.167 |
| Wait days, d (IQR) | 82 (16-263) | 118 (27-310) | < 0.001 |
| Re-transplant, n (%) | 10125 (7.5) | 727 (3.6) | < 0.001 |
The median donor age was higher in the older group (43 years vs 38 years, P < 0.001) (Table 2). The donors of older recipients were more likely to be female, have a higher BMI, and have a higher DRI.
| Young, age 18-64 (n = 135758) | Older, age ≥ 65 (n = 20000) | P value | |
| Donor age (IQR) | 38 (24-52) | 43 (28-56) | < 0.001 |
| Donor female, n (%) | 53967 (39.8) | 8434 (42.2) | < 0.001 |
| Donor race, % | < 0.001 | ||
| White | 70.3 | 68.2 | |
| Black | 14.6 | 15.5 | |
| Hispanic/Latino | 11.6 | 12.4 | |
| Asian | 2.1 | 2.4 | |
| Others | 1.4 | 1.6 | |
| Donor BMI (IQR) | 25.6 (22.5-29.5) | 26.2 (23.0-30.3) | < 0.001 |
| Donor HCV, n (%) | 4912 (3.6) | 907 (4.5) | < 0.001 |
| Cold ischemia time, h (IQR) | 6.9 (5.0-9.0) | 6.1 (4.8-8.0) | < 0.001 |
| Donor risk index (IQR) | 1.53 (1.35-1.81) | 1.61 (1.38-1.94) | < 0.001 |
| Outcomes | |||
| LOS, d (IQR) | 11 (7-20) | 10 (7-19) | 0.261 |
| Graft survival rate, (%) | |||
| 1 yr | 84.0 | 84.1 | 0.416 |
| 3 yr | 77.0 | 77.1 | 0.206 |
| 5 yr | 72.6 | 72.9 | 0.010 |
| Overall survival rate | |||
| 1 yr | 88.6 | 86.5 | < 0.001 |
| 3 yr | 82.5 | 79.5 | < 0.001 |
| 5 yr | 78.3 | 75.1 | < 0.001 |
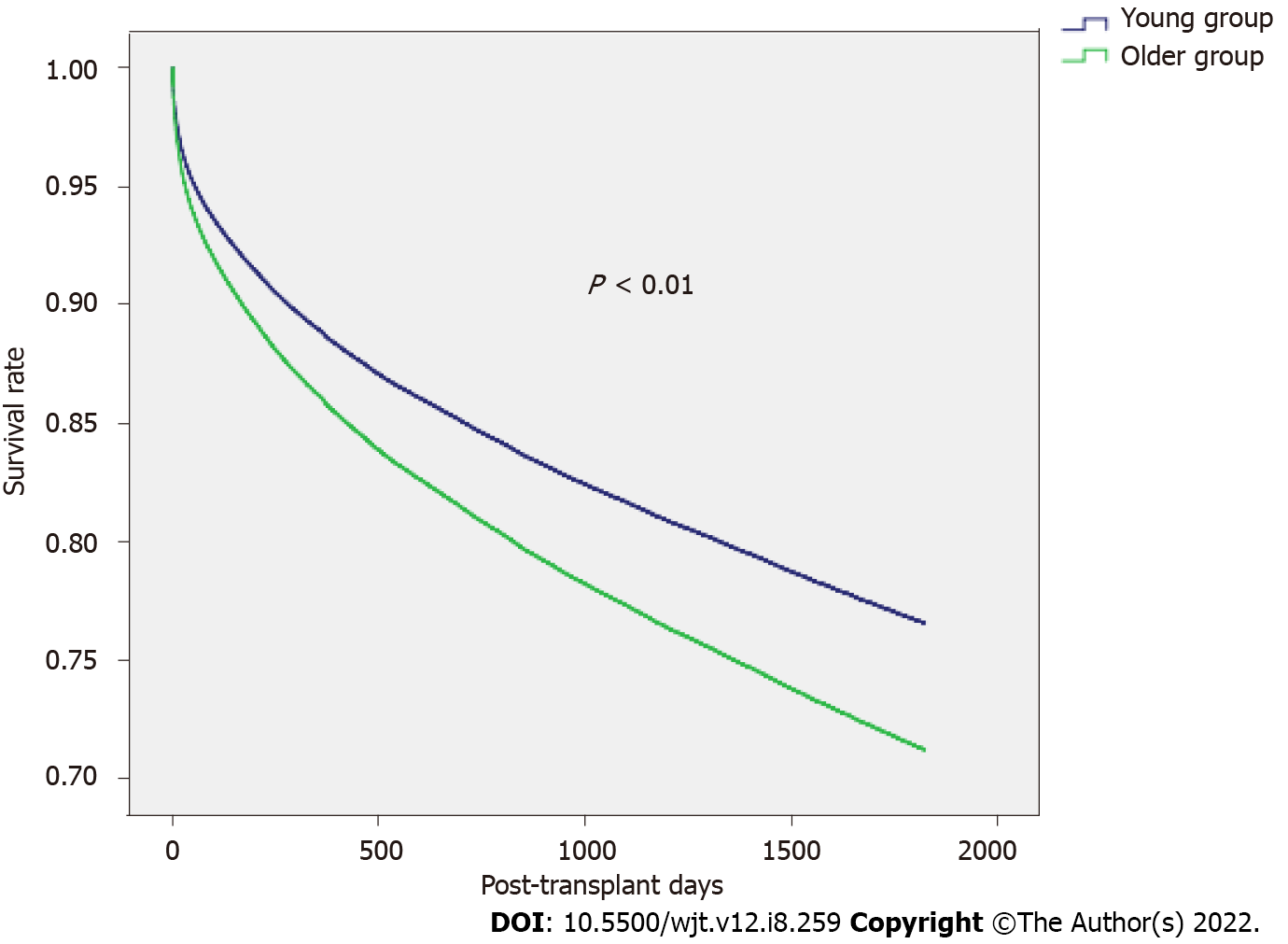
Kaplan-Meier survival analysis showed no significant differences in the 1, 3, and 5-year graft survival between the two groups, but overall survival was lower in the older group (Table 2). Multivariable Cox-Hazard regression analyses were performed to identify the factors associated with five-year graft failure (Table 3). Factors associated with five-year graft failure were recipient age ≥ 65 years, pre-LT DM, re-LT, male gender, African American race, ventilation at the time of LT, high MELD score (per 10), recipient portal vein thrombosis at time of LT, recipient HCV positive status, and high DRI. Transplants performed during the latter part of the study had a protective effect on five-year graft survival. In a subgroup analysis of older recipients, male gender, pre-LT DM, previous LT, ventilation at the time of LT, higher MELD score (per 10), portal vein thrombosis, HCV positive status, and higher DRI were associated with worse five-year graft survival (Table 4 and Figure 2).
| Variables | B (SE) | Hazard ratio (95%CI) | P value |
| Year of transplant | -0.04 (0.002) | 0.958 (0.955-0.961) | < 0.001 |
| Age ≥ 65 | 0.24 (0.02) | 1.27 (1.22-1.32) | < 0.001 |
| Male | 0.10 (0.02) | 1.11 (1.08-1.14) | < 0.001 |
| BMI (per10) | -0.05 (0.01) | 0.95 (0.93-0.98) | 0.001 |
| Race | 0.001 | ||
| Caucasian | Ref | 1.0 (Ref) | |
| African American | 0.23 (0.02) | 1.26 (1.21-1.31) | < 0.001 |
| Hispanic | -0.11 (0.02) | 0.90 (0.86-0.94) | < 0.001 |
| Asian | -0.21 (0.04) | 0.81 (0.75-0.87) | < 0.001 |
| Pre-LT diabetes | 0.20 (0.02) | 1.22 (1.18-1.26) | < 0.001 |
| Ventilation | 0.51 (0.03) | 1.67 (1.59-1.76) | < 0.001 |
| Pre-LT dialysis | 0.20 (0.02) | 1.23 (1.17-1.28) | < 0.001 |
| Retransplant | 0.44 (0.03) | 1.55 (1.47-1.63) | < 0.001 |
| PVT | 0.21 (0.03) | 1.23 (1.16-1.31) | < 0.001 |
| R1-MELD (per 10) | 0.04 (0.01) | 1.05 (1.03-1.06) | < 0.001 |
| HCV recipient | 0.28 (0.01) | 1.33 (1.29-1.36) | < 0.001 |
| Donor race | < 0.001 | ||
| Caucasian | Ref | 1.0 (Ref) | |
| African American | 0.06 (0.02) | 1.06 (1.02-1.10) | 0.001 |
| Hispanic | 0.10 (0.02) | 1.11 (1.06-1.16) | < 0.001 |
| Asian | 0.19 (0.04) | 1.21 (1.11-1.31) | < 0.001 |
| Donor risk index | 0.34 (0.03) | 1.41 (1.34-1.48) | < 0.001 |
| Cold ischemia time | 0.014(0.002) | 1.014 (1.010-1.019) | < 0.001 |
| Variables | B (SE) | Hazard ratio (95%CI) | P value |
| Year of transplant | -0.05 (0.004) | 0.954 (0.947-0.961) | < 0.001 |
| Male | 0.19 (0.04) | 1.21 (1.12-1.30) | < 0.001 |
| Re-transplant | 0.41 (0.08) | 1.50 (1.28-1.76) | < 0.001 |
| Pre-LT diabetes | 0.17 (0.04) | 1.18 (1.10-1.27) | < 0.001 |
| Ventilation | 0.42 (0.08) | 1.52 (1.30-1.76) | < 0.001 |
| Portal vein thrombosis | 0.18 (0.07) | 1.20 (1.05-1.36) | 0.006 |
| MELD (per 10) | 0.13 (0.02) | 1.14 (1.10-1.18) | < 0.001 |
| HCV Recipient | 0.21 (0.04) | 1.23 (1.15-1.33) | < 0.001 |
| Donor age (per 10) | 0.03 (0.01) | 1.03 (1.002-1.054) | 0.032 |
| Donor risk index | 0.25 (0.06) | 1.29 (1.15-1.44) | < 0.001 |
| Cold ischemia time | 0.017 (0.006) | 1.02 (1.01-1.03) | 0.003 |
This study utilized the UNOS database to analyze the trends and outcomes of LT in older patients. The results show an overall increase in total number of LT in older population over time, as well as significant changes in the trends of the primary etiology of LT. In older recipients, univariable analysis showed comparable graft survival, while multivariable analysis showed a lower graft and overall survival. But, these inferior results in older population may otherwise be considered acceptable.
The improvements in surgical techniques and perioperative care have allowed for a gradual increase LT for older recipients[4,5]. The presence of chronic liver diseases like HCV, NASH, and associated HCC in the older patients may have led to an increase in end-stage liver disease, requiring LT[10]. The recent improvements in HCV treatment has likely played a significant role in the change in primary indication for LT. Overall, the most current common indication for LT is ALD across all ages, however, our study shows that NASH and HCC are the leading causes of LT, with no increase in ALD in the older population. Durand et al[4] have shown that in LT, older recipients have a lower chance of liver allograft rejection. Additionally, they reported that patients with non-autoimmune conditions, such as NASH and alcoholic cirrhosis, do not require higher maintenance immunosuppression compared to other LT recipients[4]. Historically a subset of patients with positive HCV serostatus had a recurrence of HCV after LT[11]. HCV recurrence post-LT and subsequent chronic HCV infection would lead to drastic consequences, as chronic inflammation, fibrosis, and ultimately graft failure[12]. However, with the development of Direct-Acting Antivirals (DAA), there has been a major shift in the primary etiology of LT with the overall decrease in need of LT for chronic HCV infection[6]. Our analyses further showed that recipient HCV status was one of the risk factors for graft failure. This was likely before the availability of DAA, which has now become the therapy of choice for effectively curing HCV infection[13]. The recent studies show that DAA achieves high sustained virologic response in LT recipients and the elimination of HCV will prevent chronic inflammation, thereby avoiding the risk of compromising the graft[14,15].
As in our study, pre-transplant DM has previously been shown to be associated with worse outcomes in LT[16]. Diabetes is a metabolic disease and is associated with increased morbidity after LT[17,18]. The prevalence of NASH in patients with type 2 diabetes is more than 2-fold higher compared to the general population[19]. Poorly controlled diabetes is also strongly associated with NASH and accelerates the progression of liver disease. NASH and diabetes also increase cardiovascular risks[20]. These cumulative risk factors should be carefully evaluated for the post-transplant management of older patients.
In patients with cirrhosis, the requirement of mechanical ventilation at time of transplant is associated with an increased risk of post-operative mortality[21]. In our study, older patients were less likely to be intubated at the time of transplant, this would be related to cautious recipient selection. The patients’ requirements for dialysis and comorbidities of kidney dysfunction also had a significant impact on the outcomes of LT[22], which is further correlated with a higher MELD score. In our study, older patients had a lower MELD score and need for dialysis at the time of transplant, which might reflect the individual transplant center selection criteria for older recipients.
There were several limitations to this study. First, primary diagnosis at the time of listing for LT was used, but this diagnosis may not be accurate. If an alternative diagnosis is found post-transplant, these changes may not be recorded in the UNOS database. Secondly, we have evaluated only the patients who received LT, which means that older patients with comorbidities and/or severe clinical conditions who were not considered to be a candidate for LT, added to the selection bias in this study. Finally, long-term data regarding the graft and overall survival among older recipients is limited.
The number of LT in older recipients has significantly increased over time along with the change in indication of LT. Older age alone should not be a contraindication for LT, however, careful evaluation processes and postoperative care are necessary to improve the transplant outcomes.
The average age of liver transplant and the number of liver transplant in the older recipients is increasing.
We wanted to investigate the outcomes of expansion of criteria of liver transplantation (LT) with increasing inclusion of older recipients and donors. We also wanted to identify any potentially modifiable risk factors that may be associated lower with graft or patient survival.
We compared one, three- and five-year graft and patient survival between two groups of liver transplant recipients: Younger group (18-64 years old) and older group (≥ 65 years old) between the period of 1987-2019 in the United States.
We analyzed data from the United Network for Organ Sharing database between 1987-2019. The sample was split into younger group (18-64 years old) and older group (≥ 65 years old).
The number of LT for older patients was highest in 2019 (1920). In the older group, the percentage of non-alcoholic steatohepatitis and hepatocellular carcinoma as the primary etiology for LT was higher than younger group compared to the older group (16.4 % vs 5.9%; 14.9% vs 6.9%). On univariable analysis, there was no difference in post-transplant length of hospitalization, one-year and five-year overall survivals between the two groups. On multivariable Cox-Hazard regression analysis for graft survival, older group (hazard ratio: 1.27, P < 0.001) had higher risk of graft failure which was associated with male gender, pre-transplant diabetes, previous history of LT, ventilation at the time of LT, high model for end-stage liver disease score, recipient portal vein thrombosis, hepatitis C virus positive status, and higher donor risk index.
Older age alone should not be considered to be a contraindication for LT.
Careful evaluation process and postoperative care are necessary to improve transplant outcomes.
The data reported here have been supplied by the UNOS as the contractor for the OPTN. The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy of or interpretation by the OPTN or the United States Government.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Association for the Study of Liver Diseases.
Specialty type: Transplantation
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Costache RS, Romania; Pandey NM, India S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Kim D, Li AA, Gadiparthi C, Khan MA, Cholankeril G, Glenn JS, Ahmed A. Changing Trends in Etiology-Based Annual Mortality From Chronic Liver Disease, From 2007 Through 2016. Gastroenterology. 2018;155:1154-1163.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 173] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 2. | Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70:151-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1382] [Cited by in RCA: 2291] [Article Influence: 381.8] [Reference Citation Analysis (0)] |
| 3. | Kwong AJ, Kim WR, Lake JR, Smith JM, Schladt DP, Skeans MA, Noreen SM, Foutz J, Booker SE, Cafarella M, Snyder JJ, Israni AK, Kasiske BL. OPTN/SRTR 2019 Annual Data Report: Liver. Am J Transplant. 2021;21 Suppl 2:208-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 259] [Article Influence: 64.8] [Reference Citation Analysis (0)] |
| 4. | Durand F, Levitsky J, Cauchy F, Gilgenkrantz H, Soubrane O, Francoz C. Age and liver transplantation. J Hepatol. 2019;70:745-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 212] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 5. | Su F, Yu L, Berry K, Liou IW, Landis CS, Rayhill SC, Reyes JD, Ioannou GN. Aging of Liver Transplant Registrants and Recipients: Trends and Impact on Waitlist Outcomes, Post-Transplantation Outcomes, and Transplant-Related Survival Benefit. Gastroenterology. 2016;150:441-53.e6; quiz e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 152] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 6. | Puigvehí M, Hashim D, Haber PK, Dinani A, Schiano TD, Asgharpour A, Kushner T, Kakked G, Tabrizian P, Schwartz M, Gurakar A, Dieterich D, Boffetta P, Friedman SL, Llovet JM, Saberi B. Liver transplant for hepatocellular carcinoma in the United States: Evolving trends over the last three decades. Am J Transplant. 2020;20:220-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 7. | Mathurin P, Lucey MR. Liver transplantation in patients with alcohol-related liver disease: current status and future directions. Lancet Gastroenterol Hepatol. 2020;5:507-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 54] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 8. | Brancaccio G, Vitale A, Signoriello G, Gaeta GB, Cillo U. Changing indications for liver transplant: slow decline of hepatitis viruses in Italy. Infect Dis (Lond). 2020;52:557-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Feng S, Goodrich NP, Bragg-Gresham JL, Dykstra DM, Punch JD, DebRoy MA, Greenstein SM, Merion RM. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006;6:783-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1435] [Cited by in RCA: 1488] [Article Influence: 78.3] [Reference Citation Analysis (0)] |
| 10. | Shirazi F, Wang J, Wong RJ. Nonalcoholic Steatohepatitis Becomes the Leading Indication for Liver Transplant Registrants Among US Adults Born Between 1945 and 1965. J Clin Exp Hepatol. 2020;10:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Berenguer M. What determines the natural history of recurrent hepatitis C after liver transplantation? J Hepatol. 2005;42:448-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 106] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Berenguer M, Schuppan D. Progression of liver fibrosis in post-transplant hepatitis C: mechanisms, assessment and treatment. J Hepatol. 2013;58:1028-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 117] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 13. | Li H, Huang MH, Jiang JD, Peng ZG. Hepatitis C: From inflammatory pathogenesis to anti-inflammatory/hepatoprotective therapy. World J Gastroenterol. 2018;24:5297-5311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 66] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 14. | Cotter TG, Paul S, Sandıkçı B, Couri T, Bodzin AS, Little EC, Sundaram V, Charlton M. Improved Graft Survival After Liver Transplantation for Recipients With Hepatitis C Virus in the Direct-Acting Antiviral Era. Liver Transpl. 2019;25:598-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 73] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 15. | Kwong AJ, Wall A, Melcher M, Wang U, Ahmed A, Subramanian A, Kwo PY. Liver transplantation for hepatitis C virus (HCV) non-viremic recipients with HCV viremic donors. Am J Transplant. 2019;19:1380-1387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 110] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 16. | Zhang Q, Deng YL, Liu C, Huang LH, Shang L, Chen XG, Wang LT, Du JZ, Wang Y, Wang PX, Zhang H, Shen ZY. Diabetes mellitus may affect the long-term survival of hepatitis B virus-related hepatocellular carcinoma patients after liver transplantation. World J Gastroenterol. 2016;22:9571-9585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | John PR, Thuluvath PJ. Outcome of liver transplantation in patients with diabetes mellitus: a case-control study. Hepatology. 2001;34:889-895. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 114] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Gray M, Singh S, Zucker SD. Influence of Type 2 Diabetes Mellitus and Preoperative Hemoglobin A1c Levels on Outcomes of Liver Transplantation. Hepatol Commun. 2019;3:574-586. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Younossi ZM, Golabi P, de Avila L, Paik JM, Srishord M, Fukui N, Qiu Y, Burns L, Afendy A, Nader F. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol. 2019;71:793-801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 773] [Cited by in RCA: 1496] [Article Influence: 249.3] [Reference Citation Analysis (0)] |
| 20. | Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363:1341-1350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1326] [Cited by in RCA: 1487] [Article Influence: 99.1] [Reference Citation Analysis (0)] |
| 21. | Yuan H, Tuttle-Newhall JE, Chawa V, Schnitzler MA, Xiao H, Axelrod D, Dzebisashvili N, Lentine KL. Prognostic impact of mechanical ventilation after liver transplantation: a national database study. Am J Surg. 2014;208:582-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Weber ML, Ibrahim HN, Lake JR. Renal dysfunction in liver transplant recipients: evaluation of the critical issues. Liver Transpl. 2012;18:1290-1301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |