Copyright
©The Author(s) 2018.
World J Transplantation. Oct 22, 2018; 8(6): 220-231
Published online Oct 22, 2018. doi: 10.5500/wjt.v8.i6.220
Published online Oct 22, 2018. doi: 10.5500/wjt.v8.i6.220
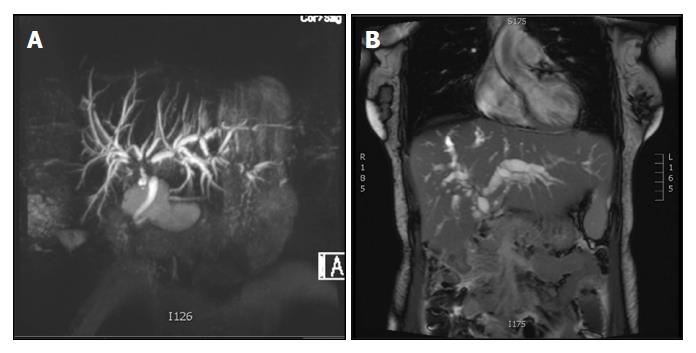
Figure 1 Magnetic resonance cholangiopancreatography images of ischemic-type biliary lesions following liver transplantation.
The images show two recipients of livers from donation after circulatory death donors that developed ischemic-type biliary lesions within 60 d following transplantation. Hepatic artery thrombosis and anastomotic biliary strictures were ruled out. A: A typical lesion is seen affecting the bifurcation of the common hepatic bile duct with moderate dilatation of the intrahepatic biliary tree; B: The image shows strictures at the bifurcation of the common hepatic bile duct, diffuse intra-hepatic strictures and a severe dilatation of the intrahepatic biliary tree.
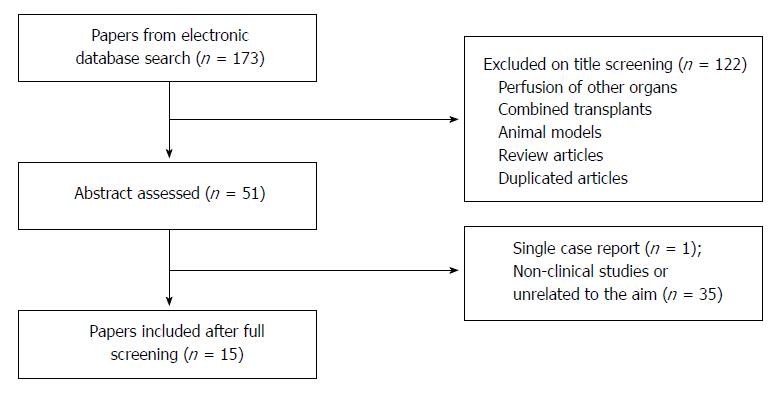
Figure 2 Study flow diagram for systematic review of the literature on the impact of machine perfusion of the liver and post-transplant biliary complications.
Following literature search duplicate articles were excluded and the titles screened. The selected abstracts were then read and non-clinical studies or reports unrelated to the aim of the review were excluded.
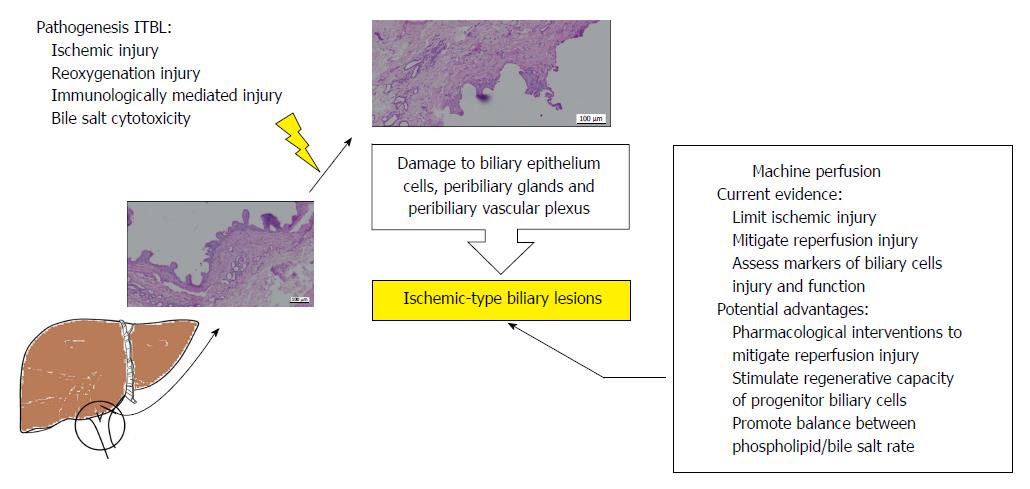
Figure 3 Diagrammatic summary of the current evidence for the impact of machine perfusion of the liver on post-transplant ischemic-type biliary lesions and future perspectives.
The current evidence suggests that ischaemic-type biliary lesions (ITBL) have a multifactorial pathogenesis. These diverse factors lead to injury to the biliary epithelium, peribiliary glands and peribiliary vascular plexus. Currently, there is evidence for the potential benefits of machine perfusion on post-transplant ITBL. The figure summarises those and possible future interventions that could enhance increase these benefits further.
- Citation: Boteon YL, Boteon AP, Attard J, Wallace L, Bhogal RH, Afford SC. Impact of machine perfusion of the liver on post-transplant biliary complications: A systematic review. World J Transplantation 2018; 8(6): 220-231
- URL: https://www.wjgnet.com/2220-3230/full/v8/i6/220.htm
- DOI: https://dx.doi.org/10.5500/wjt.v8.i6.220