Copyright
©The Author(s) 2016.
World J Transplant. Dec 24, 2016; 6(4): 632-645
Published online Dec 24, 2016. doi: 10.5500/wjt.v6.i4.632
Published online Dec 24, 2016. doi: 10.5500/wjt.v6.i4.632
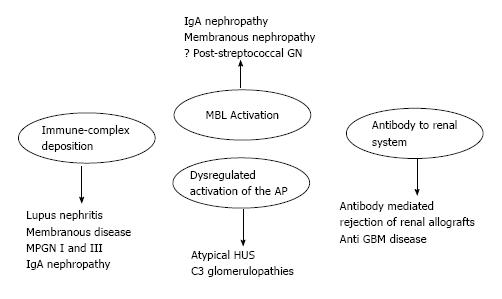
Figure 1 Mechanisms of complement activation in kidney disease.
HUS: Hemolytic uremic syndrome; MBL: Mannose binding lectin; IgA: Immunoglobulin A; MPGN: Membranoproliferative glomerulonephritis; GBM: Glomerular basement membrane; AP: Alternative pathway.
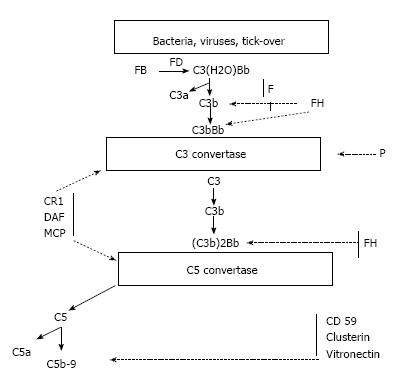
Figure 2 The C3 complement alternative pathway.
C3(H2O) Bb: Alternative pathway initiation convertase; FB: Complement factor B; FD: Complement factor D; FH: Complement factor H; FI: Complement factor I; CR1: Complement receptor 1; DAF: Decay accelerating factor; MCP: Membrane cofactor protein; P: Properdin.
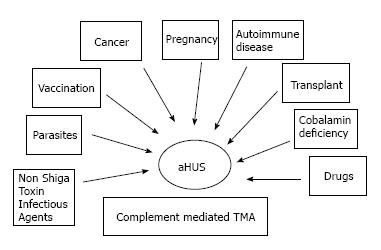
Figure 3 Heterogeneity of atypical hemolytic uremic syndrome.
TMA: Thrombotic microangiopathy; HUS: Hemolytic uremic syndrome.
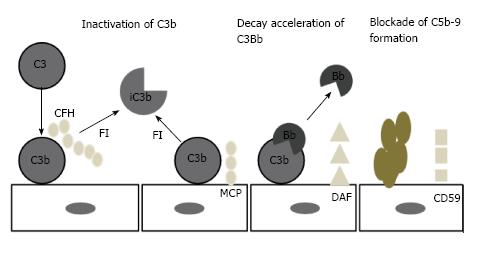
Figure 4 Regulation of complement on surfaces.
CFH: Complement factor H; FI: Complement factor I; iC3b: Inactivated C3b; MCP: Membrane cofactor protein; DAF: Decay accelerating factor; CD59: MAC inhibitor protein.
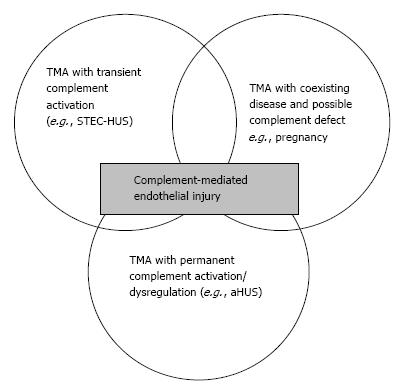
Figure 5 Spectrum of thrombotic microangiopathies.
TMA: Thrombotic microangiopathies; STEC-HUS: Shiga toxin-producing Escherichia coli-hemolytic uremic syndrome.
- Citation: Salvadori M, Bertoni E. Complement related kidney diseases: Recurrence after transplantation. World J Transplant 2016; 6(4): 632-645
- URL: https://www.wjgnet.com/2220-3230/full/v6/i4/632.htm
- DOI: https://dx.doi.org/10.5500/wjt.v6.i4.632