Copyright
©The Author(s) 2025.
World J Transplant. Jun 18, 2025; 15(2): 102384
Published online Jun 18, 2025. doi: 10.5500/wjt.v15.i2.102384
Published online Jun 18, 2025. doi: 10.5500/wjt.v15.i2.102384
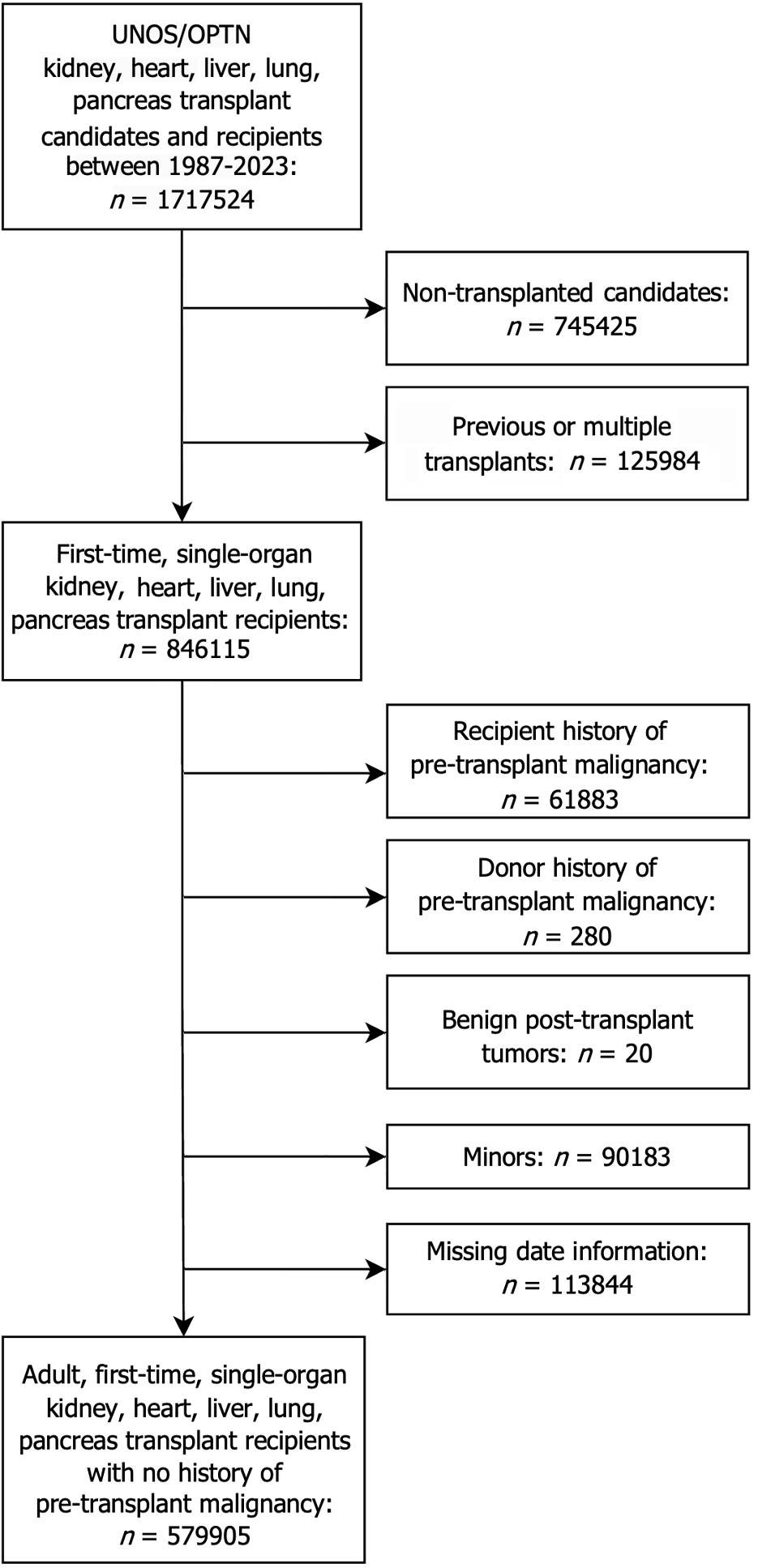
Figure 1 Flowchart of study inclusion and exclusion criteria.
This study analyzed United Network for Organ Sharing’s Organ Procurement and Transplantation Network data on adult, first-time, single-organ transplant recipients from 1987 to 2023. Major exclusions were recipients of prior, multiorgan, or simultaneous transplants, and those with pre-transplant malignancy or donors with a malignancy history. UNOS-OPTN: United Network for Organ Sharing’s Organ Procurement and Transplantation Network.
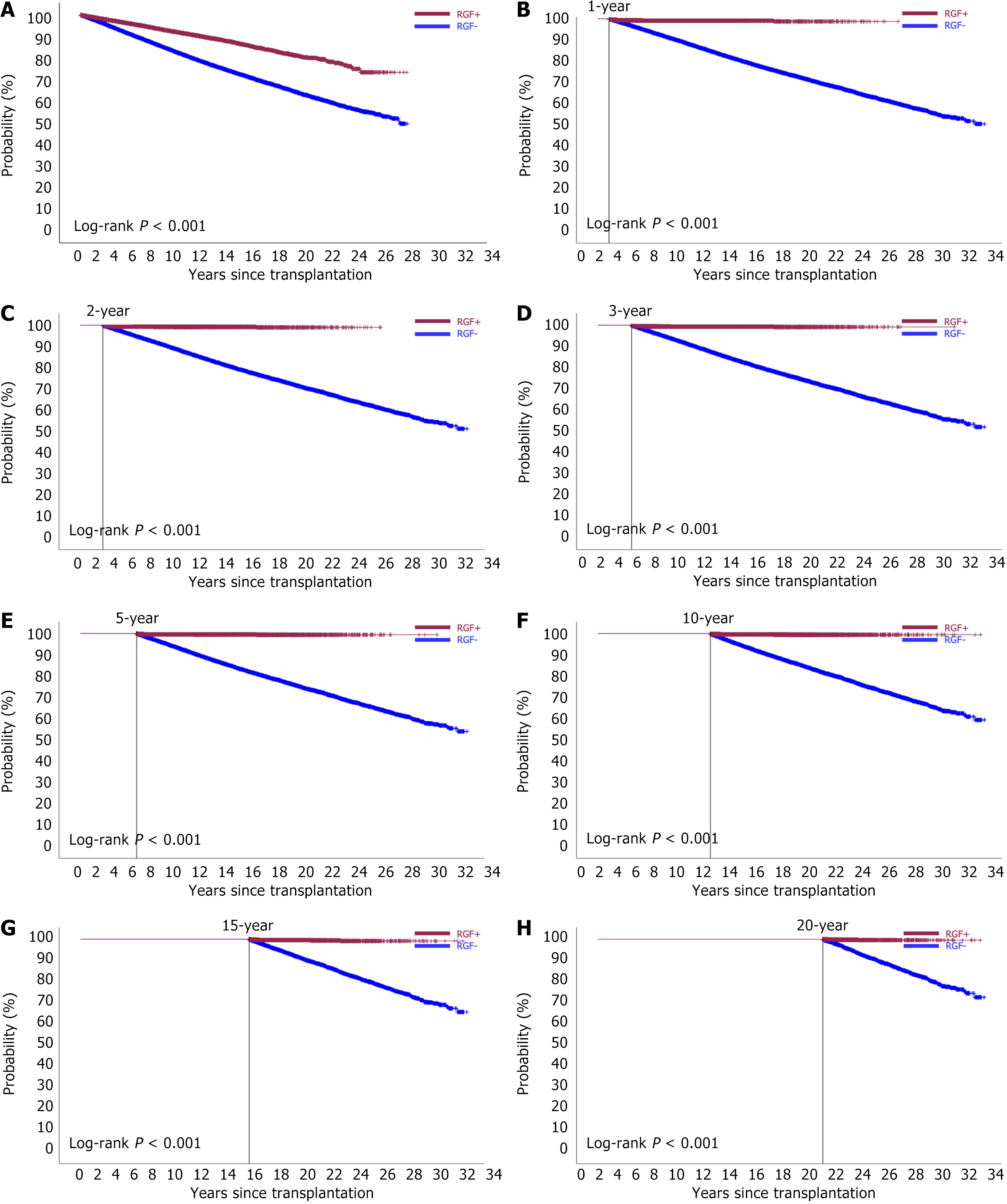
Figure 2 Landmark analysis of post-transplant malignancy risk in rejection-induced graft failure.
A: No landmark; B: 1-year landmark; C: 2-year landmark; D: 3-year landmark; E: 5-year landmark; F: 10-year landmark; G: 15-year landmark; H: 20-year landmark. Recipients with rejection-induced graft failure had a lower risk of developing malignancy over time compared to those without rejection. RGF: Rejection-induced graft failure.
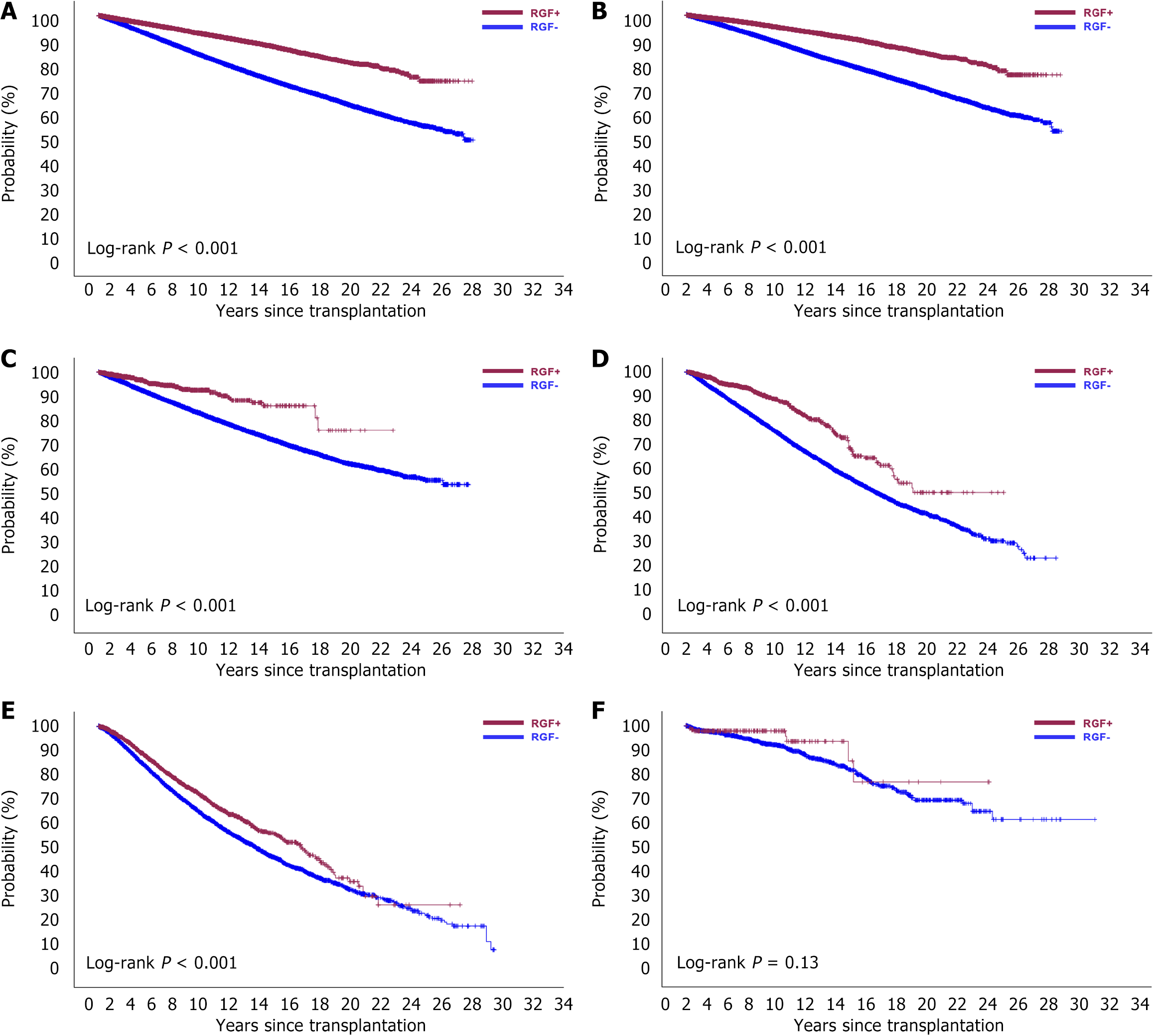
Figure 3 Post-transplant malignancy-free survival in rejection-induced graft failure.
A: All organ types; B: Kidney; C: Liver; D: Heart; E: Lung; F: Pancreas. Recipients with rejection-induced graft failure had higher malignancy-free rates after kidney, liver, heart, and lung transplants. RGF: Rejection-induced graft failure.
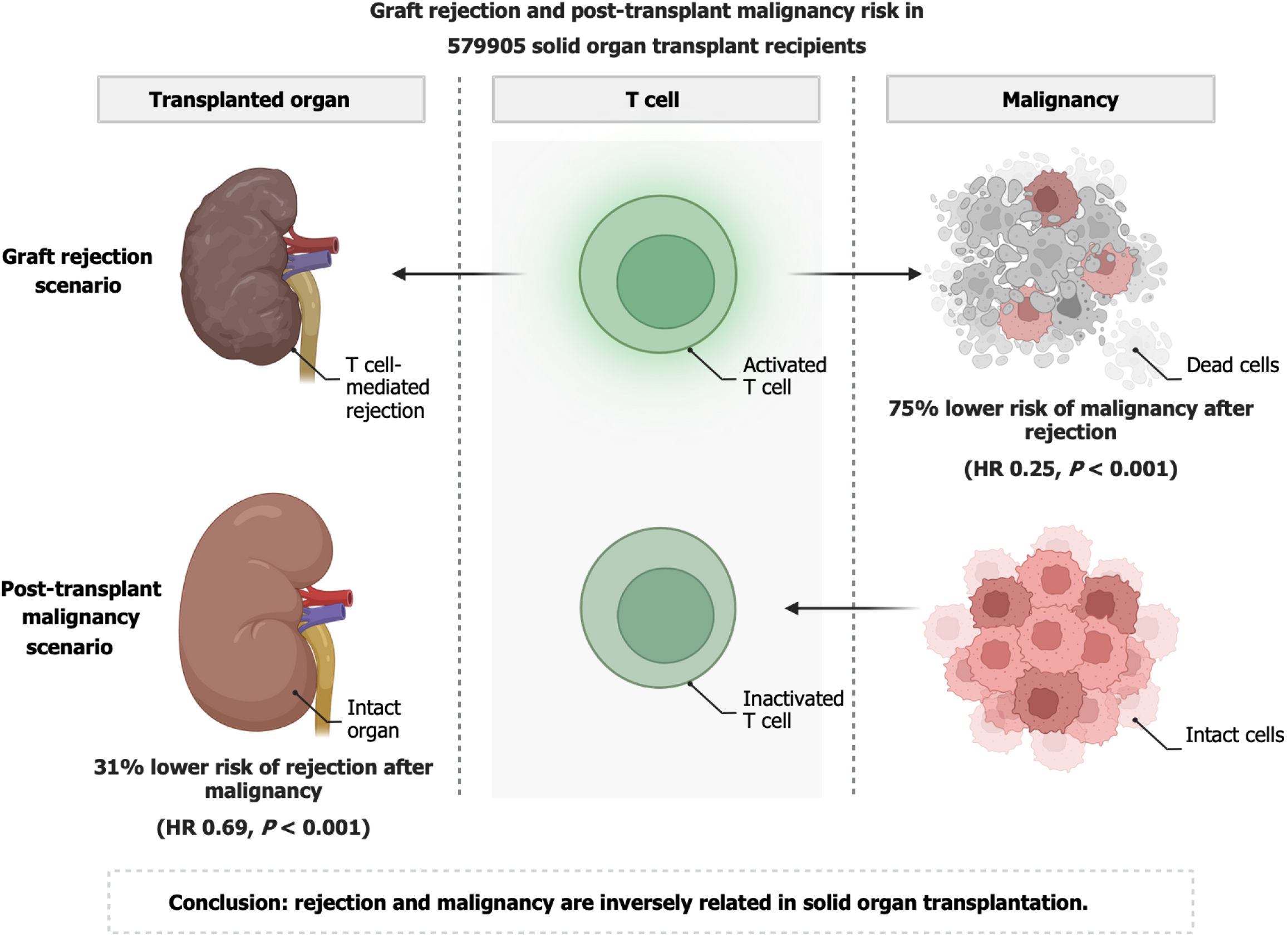
Figure 4 Immunological dynamics between graft rejection and post-transplant malignancy in solid organ transplantation.
Our findings strongly indicate an inverse relationship between immune activation in graft rejection and the immunosuppressive state in malignancy. HR: Hazard ratio.
- Citation: Kim HS, Woo W, Choi YG, Bharat A, Chae YK. Novel association between graft rejection and post-transplant malignancy in solid organ transplantation. World J Transplant 2025; 15(2): 102384
- URL: https://www.wjgnet.com/2220-3230/full/v15/i2/102384.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i2.102384