Copyright
©The Author(s) 2025.
World J Transplant. Jun 18, 2025; 15(2): 100373
Published online Jun 18, 2025. doi: 10.5500/wjt.v15.i2.100373
Published online Jun 18, 2025. doi: 10.5500/wjt.v15.i2.100373
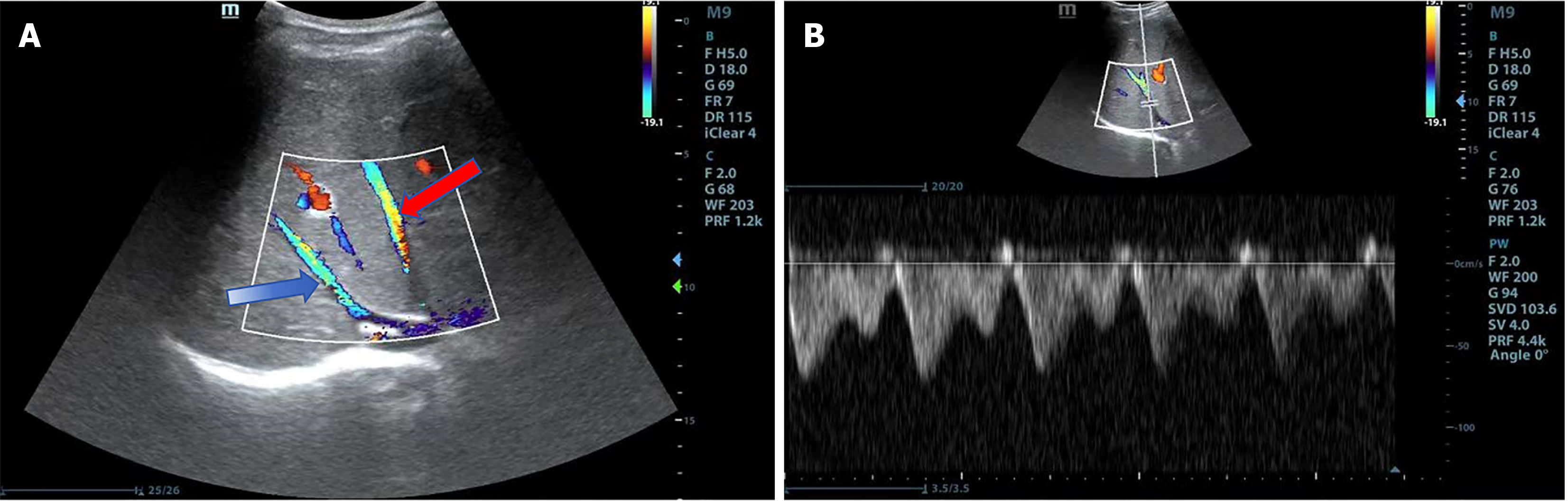
Figure 1 Normal hepatic veins.
A: Color Doppler imaging shows the right hepatic vein (blue arrow) and the middle hepatic vein (red arrow) draining into the inferior vena cava. Both the right and middle hepatic veins can be visualized simultaneously below the right costal margin. The left hepatic vein is difficult to display in the same plane due to its angle; B: Spectral Doppler imaging shows waveforms of the right hepatic vein. Post-liver transplantation, normal hepatic vein waveforms can appear triphasic, biphasic, or even monophasic. Greater variability in the amplitude of hepatic vein waveforms suggests fewer hepatic vein abnormalities. Blood flow velocity also varies significantly, influenced by the measurement location, patient respiration, and the degree of hepatic vein filling.
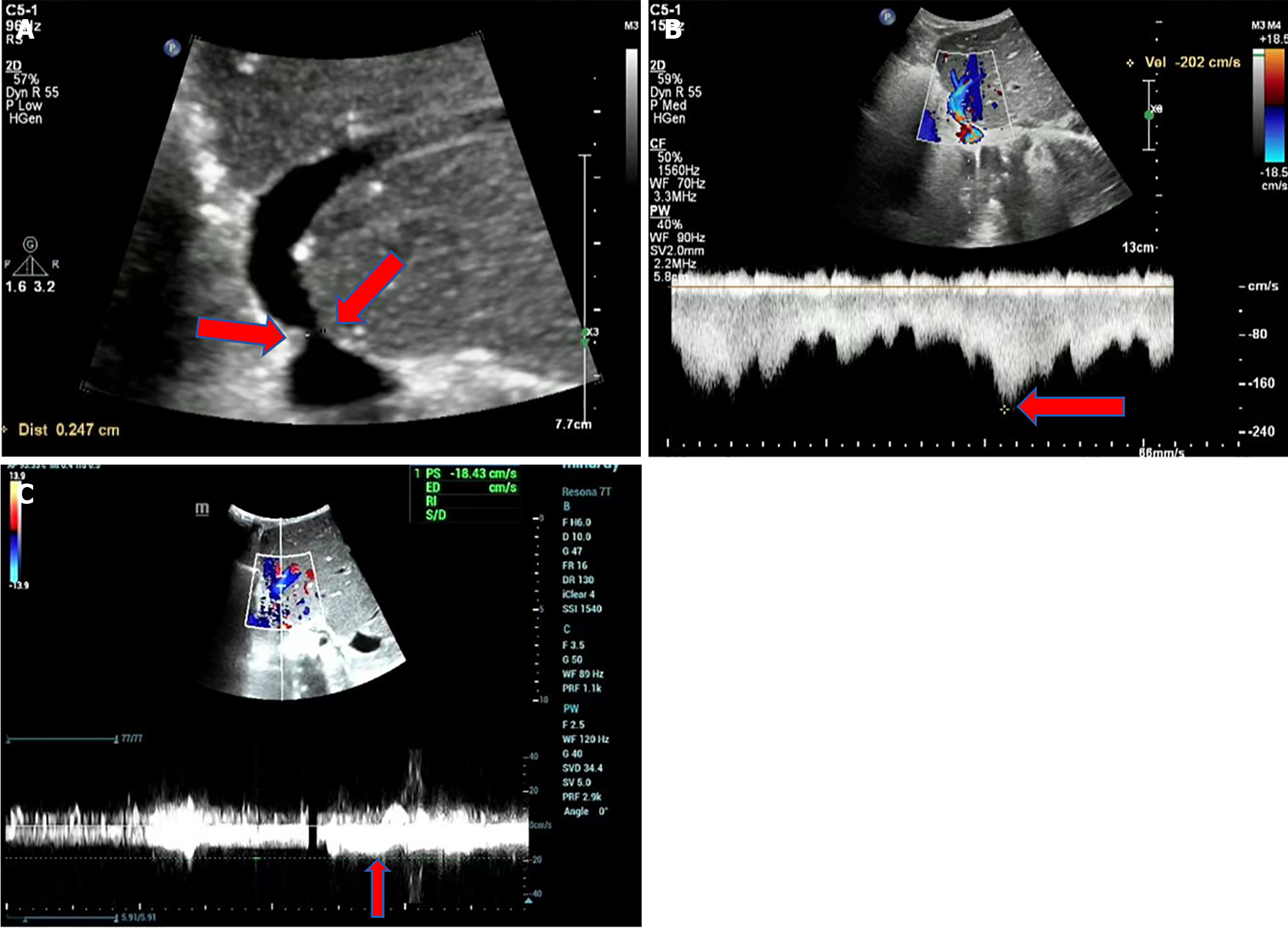
Figure 2 Hepatic vein stenosis in a 2-year-old girl with congenital biliary atresia.
A: Grayscale ultrasound shows a reduced diameter (2.4 mm) at the hepatic vein anastomosis site (red arrow). While grayscale ultrasound can reveal a narrowed diameter at the hepatic vein anastomosis site, the diagnosis of hepatic vein stenosis cannot be based solely on the reduced diameter; B: Color Doppler and spectral Doppler imaging demonstrate aliasing of blood flow signals and increased flow velocity (202 cm/second) at the hepatic vein anastomosis site; C: Spectral Doppler imaging shows decreased blood flow velocity in the main hepatic vein (18 cm/second). When the velocity ratio at the stenotic site to the pre-stenotic site exceeds 4:1, and there is a flattened hepatic vein waveform distal to the stenosis, hepatic vein outflow stenosis should be suspected. Surgical procedure: Left lobe living donor liver transplantation. Ultrasound examination: 2 years postoperatively. No abnormal clinical indicators.
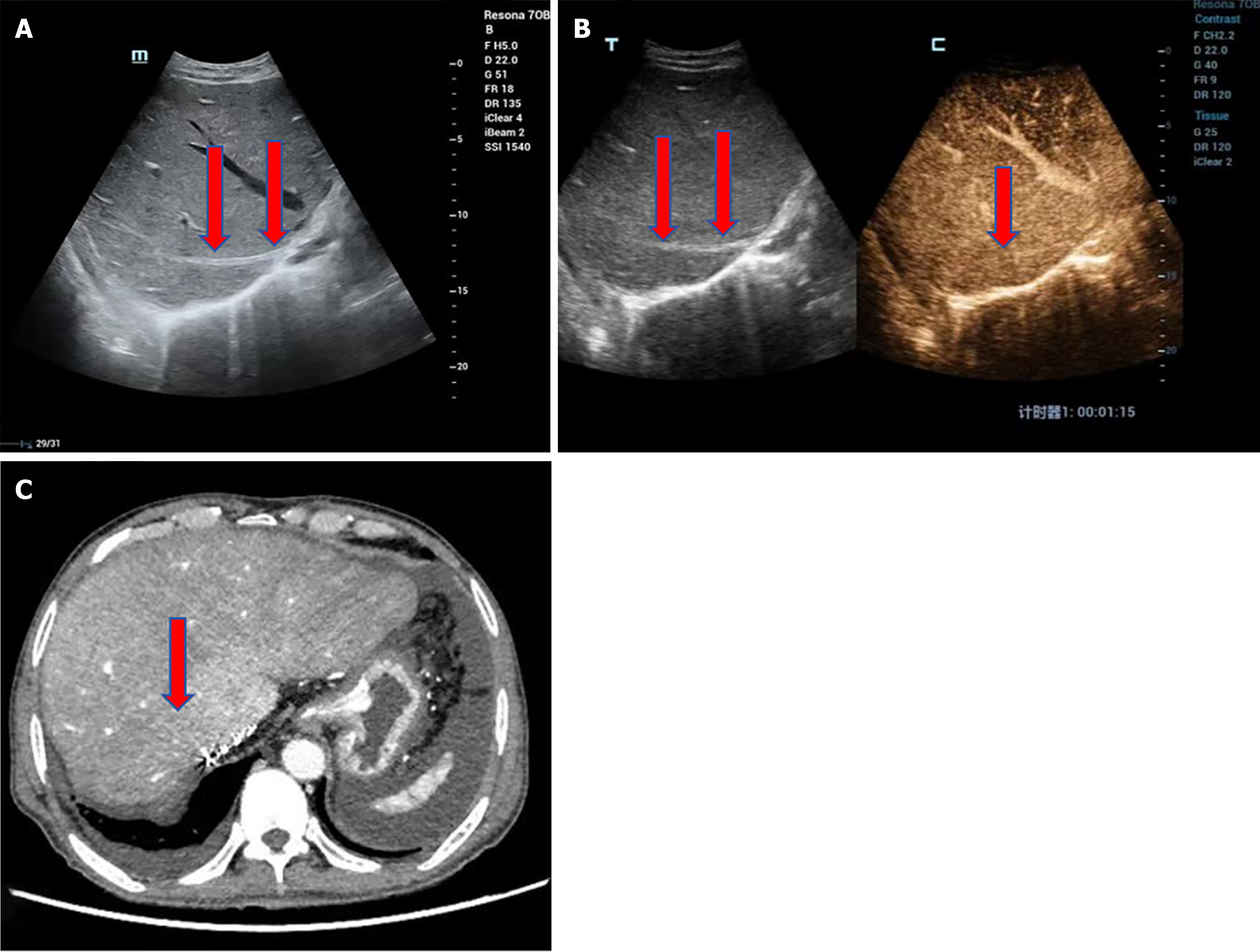
Figure 3 Hepatic vein occlusion in a 72-year-old male with decompensated hepatitis B cirrhosis.
A: The liver is significantly enlarged with coarse, dense parenchymal echotexture and patchy hypoechoic areas. The right hepatic vein appears narrowed with thickened, hyperechoic walls. Hepatic vein occlusion results in impaired hepatic blood outflow, leading to liver congestion and enlargement. Ultrasound can measure the maximum oblique diameter of the right lobe to assess liver size. One year post-transplantation, the liver size typically normalizes, with a right lobe maximum oblique diameter not exceeding 140 mm. In this patient, the liver is markedly enlarged. Chronic hepatic congestion can lead to increased parenchymal echogenicity and fibrosis, with patchy hypoechoic areas representing focal congestion; B: Contrast-enhanced ultrasound shows no enhancement within the right hepatic vein, confirming the diagnosis of right hepatic vein occlusion; C: Contrast-enhanced computed tomography reveals no enhancement in the right hepatic vein and heterogeneous liver density. Surgical procedure: Piggyback liver transplantation. Ultrasound examination: 14 years postoperatively. Clinical presentation: Massive ascites.
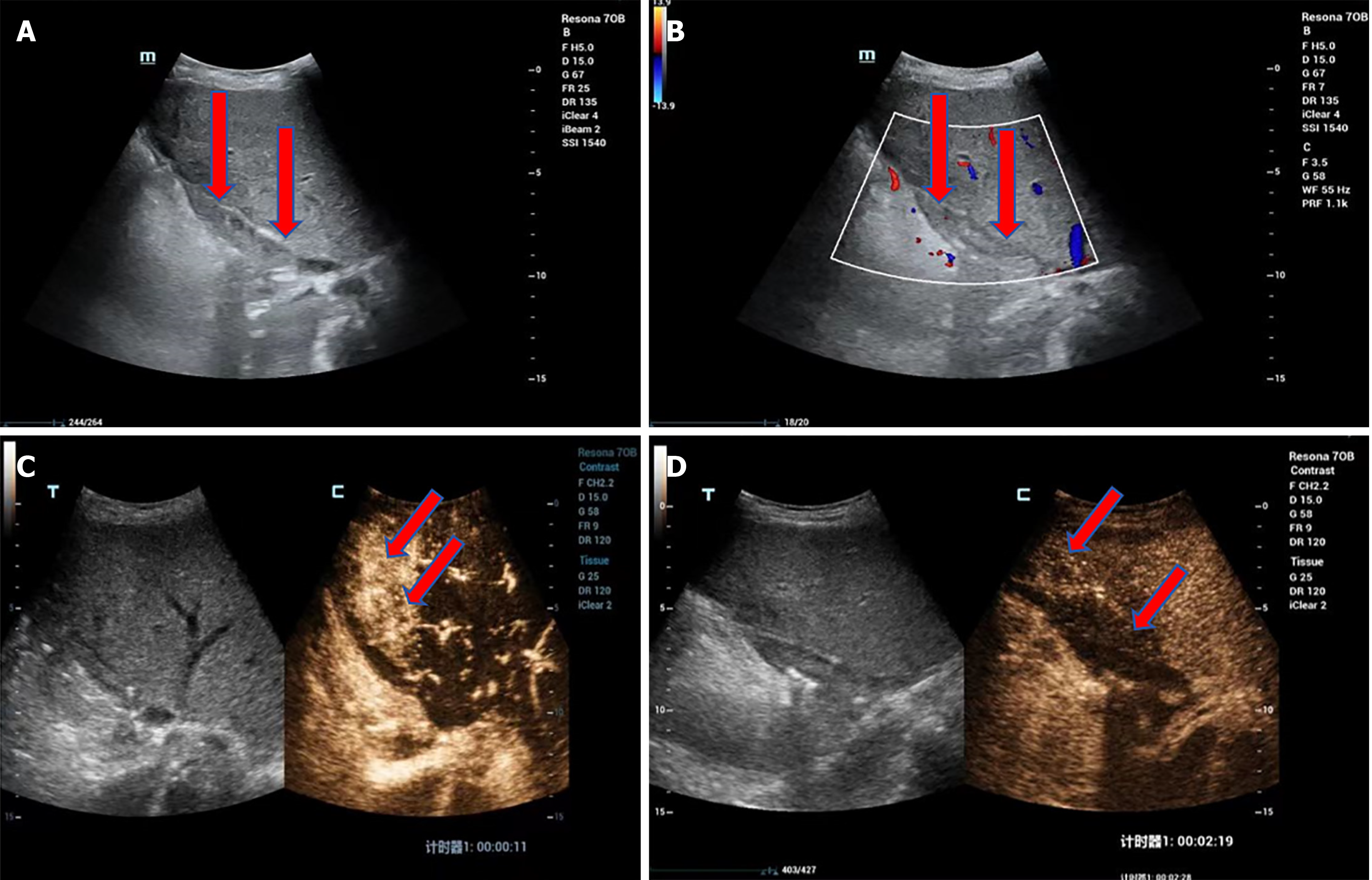
Figure 4 Bridging vein thrombosis in a 37-year-old female with primary sclerosing cholangitis and decompensated cirrhosis.
A: Grayscale ultrasound shows the bridging vein lumen filled with medium to low echogenic material; B: Color Doppler ultrasound shows no significant blood flow signal within the bridging vein lumen, suggesting occlusion due to bridging vein thrombosis; C: Contrast-enhanced ultrasound (CEUS) shows no enhancement within the bridging vein lumen, confirming complete occlusion. An interesting phenomenon observed on CEUS is arterial phase hyperenhancement in the drainage area of the bridging vein (segment 4, indicated by the arrow); D: CEUS shows delayed phase hypoenhancement in the drainage area of the bridging vein (segment 4, indicated by the arrow). The abnormal arterial phase enhancement of the hepatic parenchyma in the drainage area is associated with local liver sinusoidal congestion due to impaired hepatic outflow. Surgical procedure: split liver transplantation (including left hemiliver with the middle hepatic vein). The donor liver was from a dextran-binding domain adult, split along the middle hepatic vein, with the left liver graft allocated to this patient. Intraoperative reconstruction of the proximal end of the middle hepatic vein was performed. Ultrasound examination, 1 month postoperatively. Biochemical indicators show elevated transaminases and bilirubin.
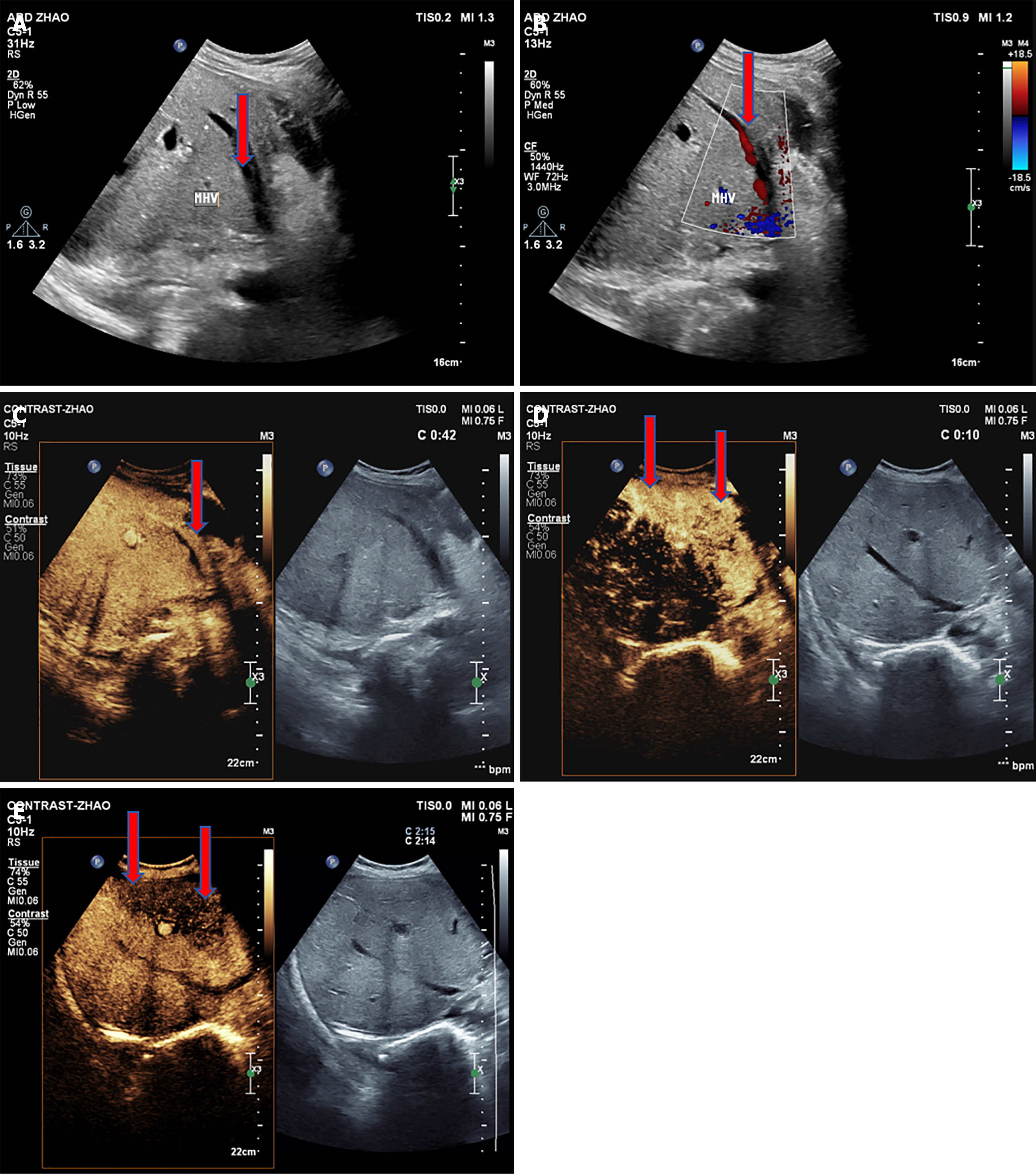
Figure 5 Hepatic vein thrombosis in a 53-year-old female with decompensated hepatitis B cirrhosis.
A: Grayscale ultrasound shows a solid hypoechoic mass within the middle hepatic vein lumen, not completely filling the vein; B: Color Doppler ultrasound shows no significant blood flow signal in parts of the hypoechoic mass within the middle hepatic vein lumen, with blood flow bypassing around the mass, suggesting hepatic vein thrombosis with incomplete luminal occlusion; C: Contrast-enhanced ultrasound (CEUS) shows a filling defect within the middle hepatic vein, with contrast agent flowing along the vein wall and encircling the thrombus, resulting in a consistent filling defect image; D: CEUS shows arterial phase hyperenhancement in the drainage area of the middle hepatic vein (segment 4, indicated by the arrow); E: CEUS shows delayed phase hypoenhancement in the drainage area of the middle hepatic vein (segment 4, indicated by the arrow). In this case, CEUS confirmed the presence of a middle hepatic vein thrombus, with hepatic parenchymal perfusion characteristics demonstrating arterial phase hyperenhancement and delayed phase hypoenhancement in the hepatic parenchyma of the drainage area. Surgical procedure: split liver transplantation (including right hemiliver with the middle hepatic vein). The donor liver was from a dextran-binding domain adult, split along the middle hepatic vein, with the right liver graft allocated to this patient. Ultrasound examination: 3 days postoperatively. Biochemical indicators showed elevated transaminases and bilirubin.
- Citation: Zhao NB, Luo Z, Li Y, Xia R, Zhang Y, Li YJ, Zhao D. Diagnostic value of ultrasonography for post-liver transplant hepatic vein complications. World J Transplant 2025; 15(2): 100373
- URL: https://www.wjgnet.com/2220-3230/full/v15/i2/100373.htm
- DOI: https://dx.doi.org/10.5500/wjt.v15.i2.100373