Copyright
©The Author(s) 2020.
World J Transplant. Feb 28, 2020; 10(2): 29-46
Published online Feb 28, 2020. doi: 10.5500/wjt.v10.i2.29
Published online Feb 28, 2020. doi: 10.5500/wjt.v10.i2.29
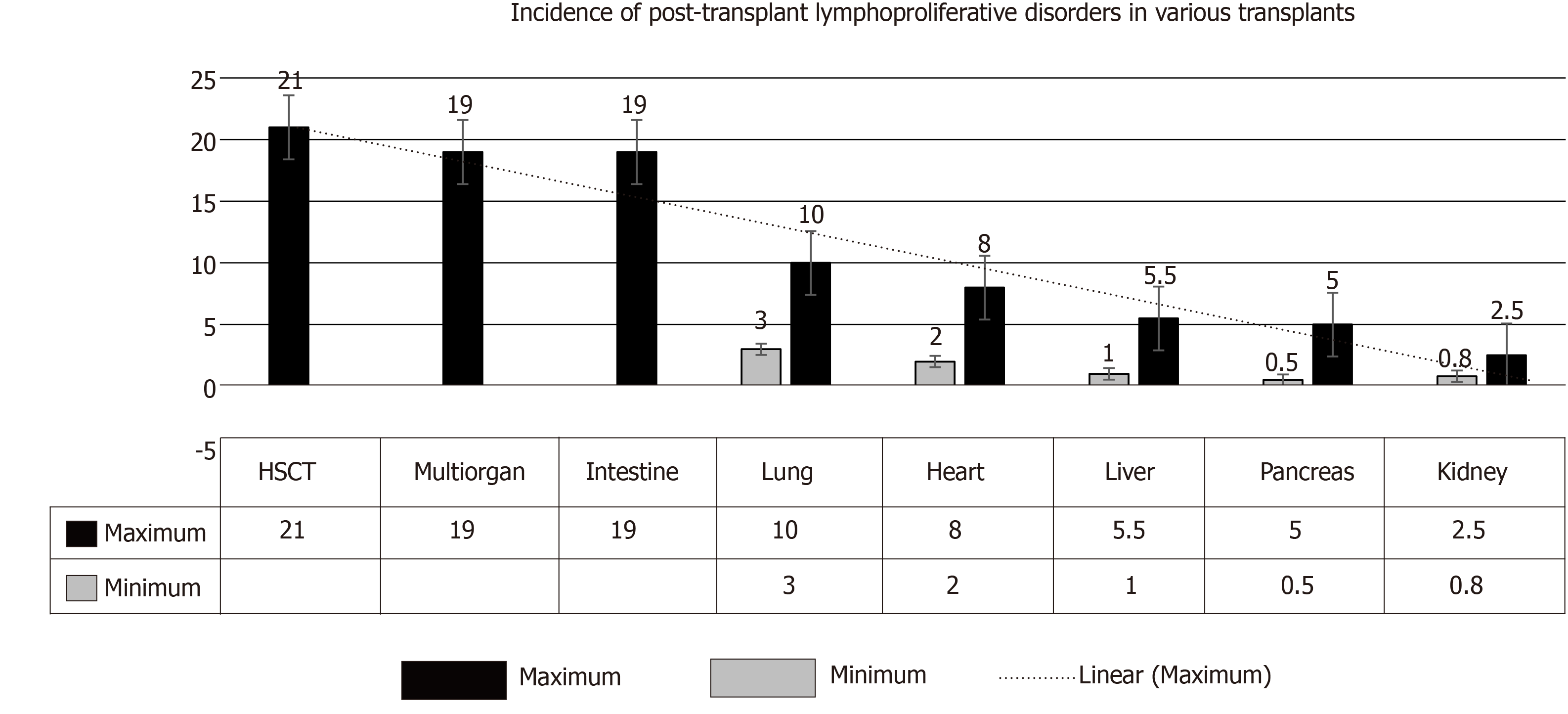
Figure 1 The range increased incidence of post-transplant lymphoproliferative disorders in various transplants.
Incidence in intestinal transplant and in multi-organ transplants it is < 20%, while in hematopoietic stem-cell transplant it is > 20% with selective T-cell depletion[4]. HSCT: Haplo-identical allogeneic hematopoietic stem-cell transplant.
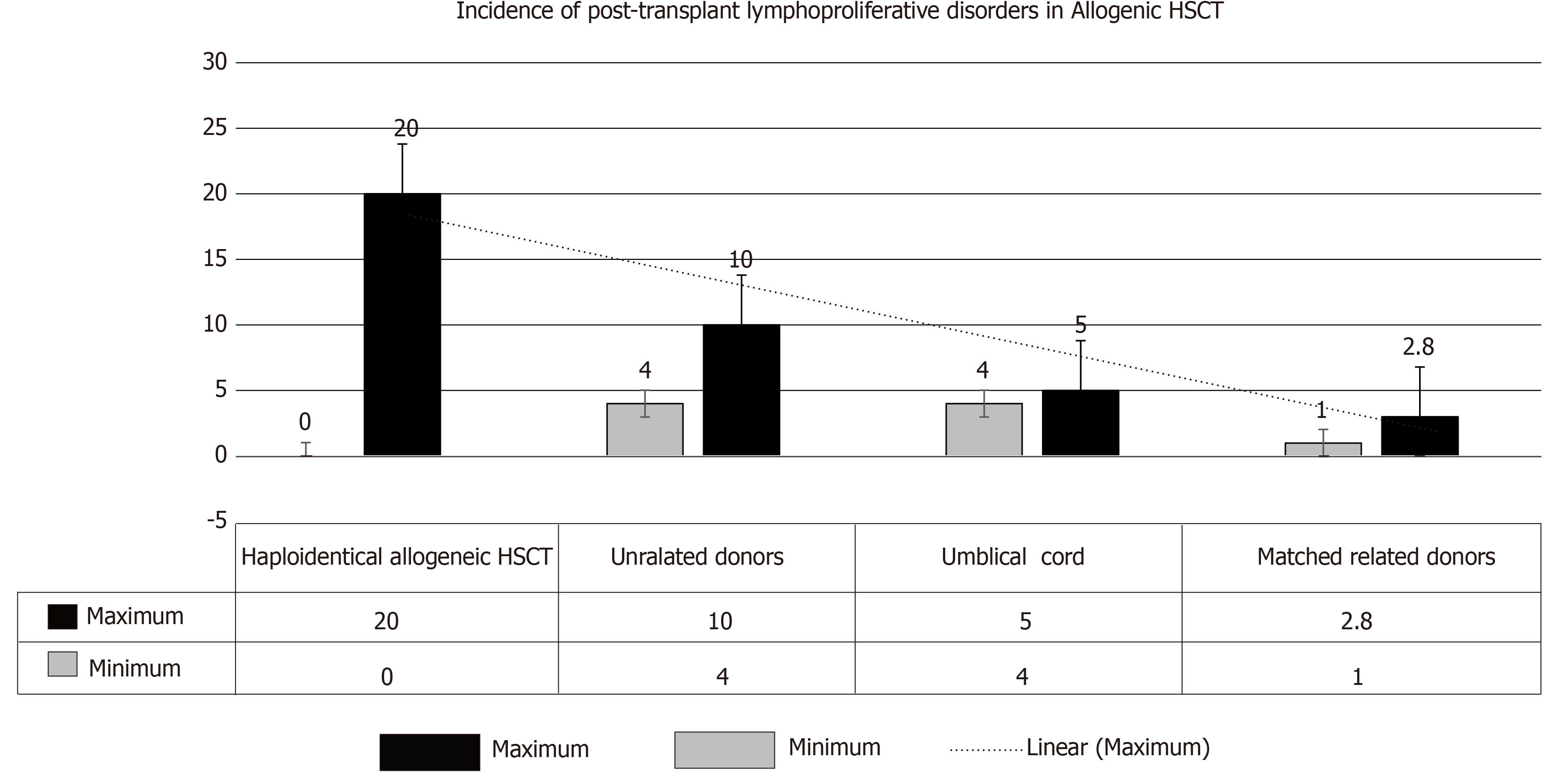
Figure 2 Incidence of post-transplant lymphoproliferative disorders after allogenic hematopoietic stem-cell transplant.
An additional risk factor in hematopoietic stem-cell transplantation is: recipient age of > 50 yr[4]. HSCT: Haplo-identical allogeneic hematopoietic stem-cell transplant.
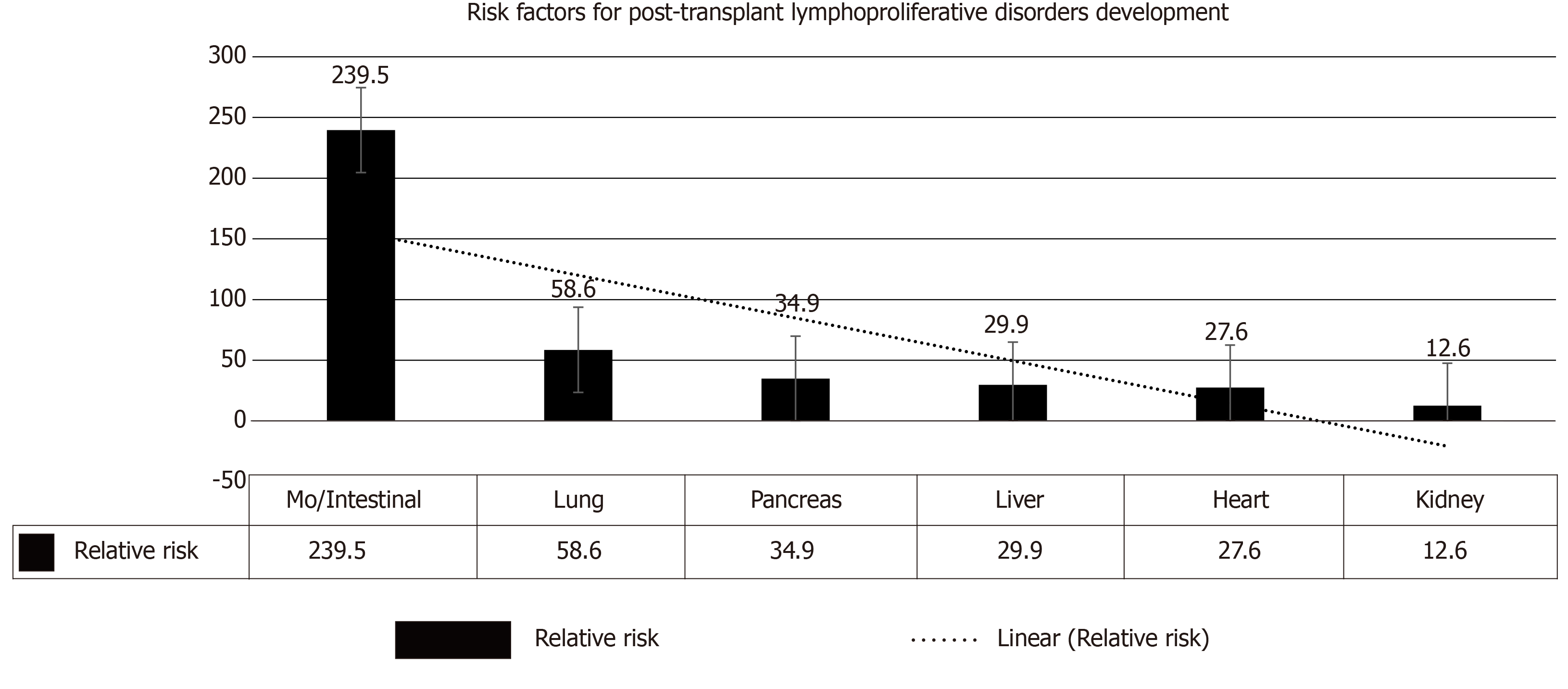
Figure 3 Risk factors for the development of post-transplant lymphoproliferative disorders after solid-organ transplantation[4].
MO: Multi-organ.
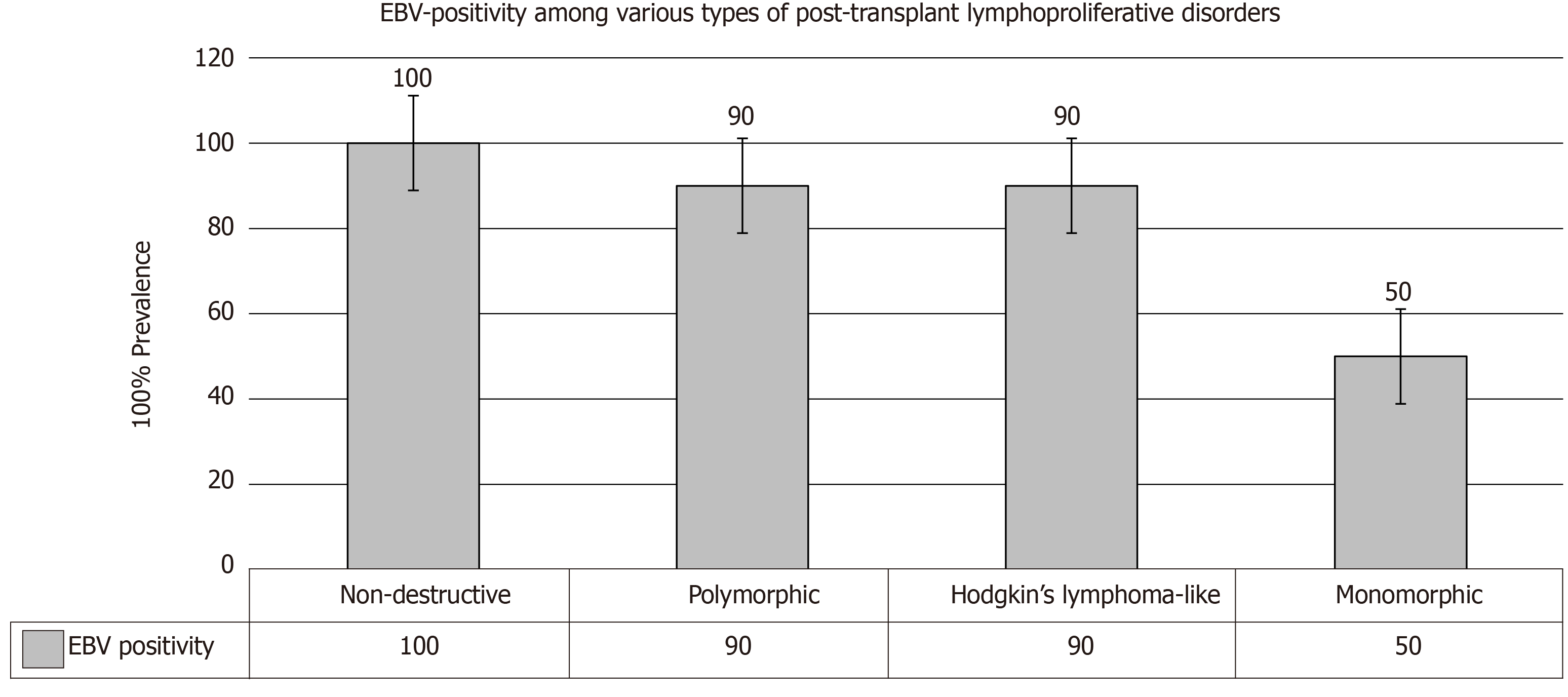
Figure 4 Epstein-Barr virus positivity among various types of post-transplant lymphoproliferative disorders[4].
EBV: Epstein-Barr virus.
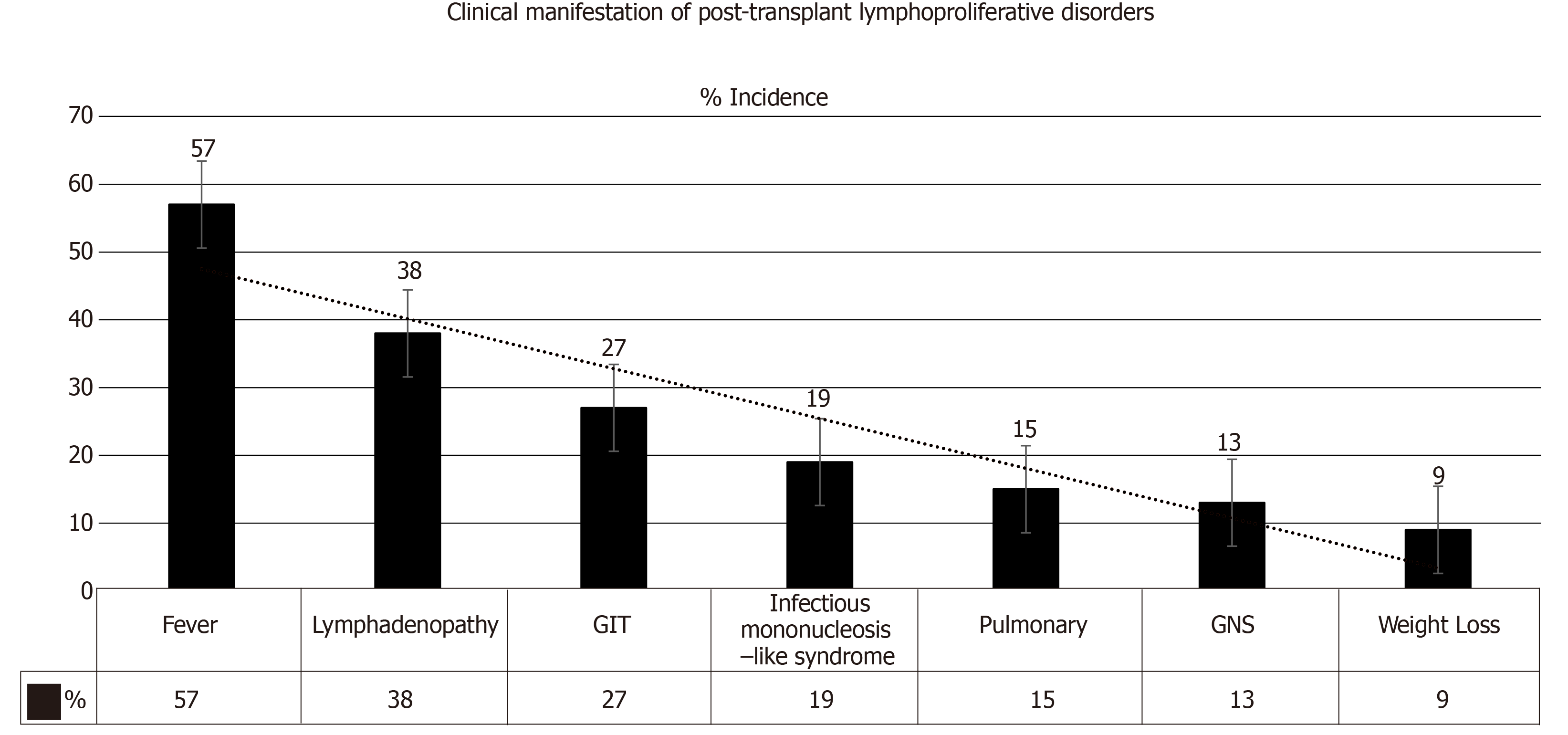
Figure 5 Clinical manifestations of post-transplant lymphoproliferative disorders[2].
GIT: Gastrointestinal tract; CNS: Central nervous system.
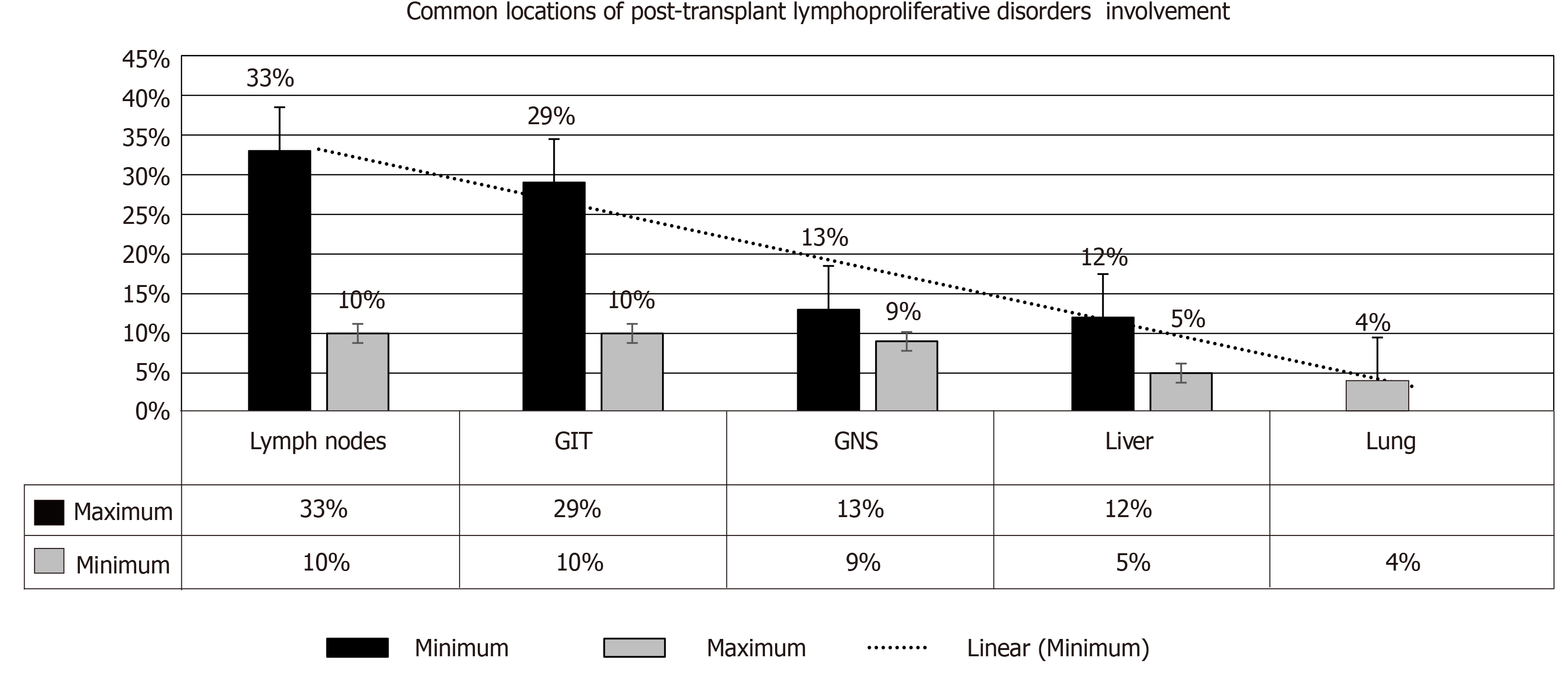
Figure 6 Common locations of post-transplant lymphoproliferative disorder involvement[1].
GIT: Gastrointestinal tract; CNS: Central nervous system.
- Citation: Abbas F, El Kossi M, Shaheen IS, Sharma A, Halawa A. Post-transplantation lymphoproliferative disorders: Current concepts and future therapeutic approaches. World J Transplant 2020; 10(2): 29-46
- URL: https://www.wjgnet.com/2220-3230/full/v10/i2/29.htm
- DOI: https://dx.doi.org/10.5500/wjt.v10.i2.29