Published online Jul 12, 2015. doi: 10.5499/wjr.v5.i2.90
Peer-review started: June 29, 2014
First decision: November 27, 2014
Revised: December 5, 2014
Accepted: March 16, 2015
Article in press: March 18, 2015
Published online: July 12, 2015
Processing time: 374 Days and 15.4 Hours
Trapeziometacarpal (TMC) joint is the secondly affected joint for osteoarthritis in the hand. TMC joint arthritis affects most commonly postmenopausal women after the fifth decade of life, due to hormonal and structural factors. Rhizarthrosis may lead to a clinical spectrum from subtle symptoms to advanced symptoms such as; severe pain, limitation of range of motion, muscular weakness, bony deformities, and end up ultimately with disability. Regardless of the etiopathogenesis; a variety of non-surgical and surgical methods have been used for the treatment of rhizarthrosis, depending on the age of the patient, symptomatology and the stage of the disease. The main goals of the treatments are as follows; relief of pain, conservation or restoration the stability and mobility of the TMC joint with the optimal preservation of the strength of surrounding musculature. In this article, the current methods, which have been used for the treatment of TMC joint osteoarthritis, will be mainly reviewed, together with concise up-to-date information on both its diagnosis and the anatomy of the TMC joint.
Core tip: The trapeziometacarpal joint is a common region in the body, where osteoarthritis is encountered, especially in the postmenopausal women. Although the exact etiology is not still certain, ligamentous laxity is a common finding in most of the cases. Regarding to the existing literature, the most commonly used treatment methods are conservative measures and trapeziectomy with ligament reconstruction tendon interposition. Moreover newer treatment methods have emerged in the recent years. In conclusion, if long-term prospective, randomized, comparative studies are performed, there will be an appropriate answer to choose the optimal treatment methods for each stage of rhizarthrosis.
- Citation: Bilge O, Karalezli N. Current review of trapeziometacarpal osteoarthritis (rhizarthrosis). World J Rheumatol 2015; 5(2): 90-95
- URL: https://www.wjgnet.com/2220-3214/full/v5/i2/90.htm
- DOI: https://dx.doi.org/10.5499/wjr.v5.i2.90
Trapeziometacarpal (TMC) joint is the secondly affected joint for osteoarthritis (OA) in the hand[1]. TMC OA or rhizarthrosis affects most commonly postmenopausal women after the fifth decade of life, due to hormonal and structural factors[2-4]. Rhizarthrosis may lead to a clinical spectrum from subtle symptoms to advanced symptoms such as; severe pain, limitation of range of motion, muscular weakness, bony deformities, and end up ultimately with disability.
Although the exact etiology of rhizarthrosis has not been clearly evidenced yet, most postulated theories related this entity with the surrounding ligamentous laxity or weakness of this joint, leading to the disturbed congruency between the trapezium and the basis of first metacarpus[5-9]. The incongruence and increased contact stresses end up eventually with rhizarthrosis.
Regardless of the etiopathogenesis; a variety of non-surgical and surgical methods have been used for the treatment of rhizarthrosis, depending on the age of the patient, symptomatology and the stage of the disease. The main goals of the treatments are as follows; relief of pain, conservation or restoration the stability and mobility of the TMC joint with the optimal preservation of the strength of surrounding musculature.
In this article, the current methods, which have been used for the treatment of rhizarthrosis, will be mainly reviewed, together with concise up-to-date information on both its diagnosis and the anatomy of the TMC joint.
The TMC joint of the thumb has a vital function nearly for all functions of the thumb, mainly by opposition. It is a combination of “saddle” and “universal” types of joint with confronting biconcave-convex shapes of trapezium and the basis of the first metacarpal bone. Its stability mostly depends on the ligaments, which support this joint mostly around the dorsal and volar regions. The understanding of this complex ligamentous anatomy is highly important for the stability of this joint, and its osteoarthritic process. This joint and its supporting ligamentous structures have been studied extensively in terms of anatomy, histopathology or biomechanics[5,9-18].
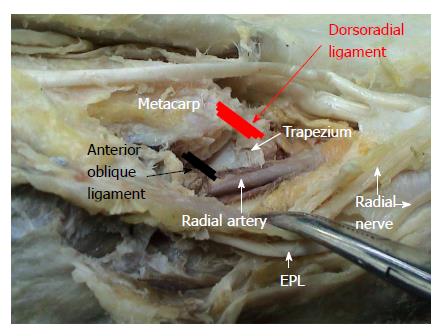
In general, 6 main ligaments of the TMC joint were consistently identified in the literature. These are as follows: dorsoradial ligament (DRL), anterior oblique ligaments (AOL, superficial and deep), intermetacarpal ligament, ulnar collateral ligament and posterior oblique ligament. The functions of these stabilizing ligaments are summarized in Table 1[19].
| Ligament | Description of the function | |
| Dorsoradial (Figure 1) | Shortest and thickest ligament (Recently possible) Primary stabilizer against dorsal translation of the joint Opposes anterior oblique ligaments Basis for Eaton-Littler procedure | |
| Anterior oblique (Figure 1) | Superficial | Stabilization against volar joint subluxation |
| Deep | Known as beak ligament Act as a pivot point Primary joint stabilizer against dorsal translation | |
| Posterior oblique | Stabilization of rotation | |
| Intermetacarpal | Stabilization during radiovolar translation Stabilization of the thumb against collapse especially after trapeziectomy | |
| Ulnar collateral | Helps to stabilization against volar joint subluxation |
Among these ligaments, AOL was shown to be the primary stabilizer of the TMC joint by Eaton, Littler and Pellegrini[7,8,20]. But, this information has been challenged by many recent studies, in such a way that the DRL is the primary stabilizer against dorsal translation of the TMC joint[9,15,18,21-25]. It seems that this controversial debate on the main stabilizing ligaments of the TMC joint will continue over the coming years by ending up with an ultimate prospective conclusion.
In general, patients with rhizarthrosis have a spectrum of symptomatology. On one hand a patient may be asymptomatic or may have subtle symptoms despite pantrapezial arthritis, on the other hand another patient may have severe symptoms despite a lower radiological stage. Although this disease interferes with recreational and professional activities and performances, most patients live by adapting themselves to this situation with the avoidance of some thumb movements, such as abduction and key pinch. So, the symptomatology may not correlate with the radiology in most of the times[26].
Symptomatic patients usually present with a pain located at the base of the thumb, which may radiate to the thenar region or metacarpophalangeal joint. It is usually worsened by some unique movements of the thumb (pinch or grip during turning a key, sewing, writing, opening a jar, etc.). As the disease progresses, the position of the thumb shifts from an adducted but lax position to a more ankylosed position, and the previously lax joint becomes stiffer. The final position of the deformity is defined as “pollux addustus” (adducted metacarpal shaft with metacarpophalangeal hyperextension).
In physical examination, tenderness and some provocative tests help to the establishment of the diagnosis. The tenderness is usually at the radiopalmar surface of the TMC joint, especially coexisting with inflammation at earlier stages. The provocative tests, which include the grind test and Glickel test, aim to reproduce pain at the TMC joint level[27,28].
In practice, radiography should at least include; posteroanterior (PA) neutral, PA clenched fist, lateral, and oblique views. The most popular and the most commonly used radiological classification of rhizarthrosis is the Eaton-Littler Classification, which uses a true lateral view of the thumb centered over the trapezium and sesamoids superimposed (Table 2)[13]. Later, a fifth stage was described as pan-trapezial arthritis, as TMC joint arthritis was observed rarely as an isolated entity[29].
| Stage | Definition |
| I | Normal articular surface |
| Possible widening of TMC joint indicating synovitis | |
| II | Joint space narrowing |
| Oteophytes < 2 mm | |
| Normal ST joint | |
| III | Severe TMC destruction with subchondral sclerosis |
| Osteophytes > 2 mm and presence of loose bodies | |
| Normal ST joint | |
| IV | TMC and ST joints are both affected |
The most common pathology co-existing with rhizarthrosis was reported to be the carpal tunnel syndrome[30]. Differential diagnosis of rhizarthrosis includes De Quervain’s disease, trigger thumb, scaphoid fracture (distal pole), flexor carpi radialis (FCR) tenosynovitis, scaphotrapezial arthritis, wrist arthritis and subsesamoid arthritis[19]. But careful and proper clinical and radiological evaluations will differentiate rhizarthrosis from the aforementioned clinical entities.
The treatment of rhizarthrosis has evolved in the last decade, especially in terms of surgical methods. In general, the treatment mainly aims to relieve pain, to regain stability, mobility of the joint, to reestablish the strength of surrounding structures and to increase the comfort and function of the patient clinically. Treatment methods will be summarized concisely in this section.
In general, non-surgical methods are preferred at the initial stages by most of the clinicians, as the initial method of management. The choices include: non-steroidal inflammatory drugs, splinting with thumb spica cast, physical therapy and injections (steroid and hyaluronic acid)[3,31-36]. It should be kept in mind that continuous and repeated steroid injections have been shown to weaken the joint capsule[37]. They may complicate further surgeries. Therefore they should be used specially at inflammatory flare-up periods, but should not be applied repeatedly. Another important point is that; although most studies on conservative methods report good-excellent results on pain and functional scores, the methodological quality of these studies was recently found to be poor to fair[38].
Surgical treatment is most commonly reserved for symptomatic patients who are unresponsive to conservative methods or who are at advanced stages of the disease. Although several surgical treatment methods have been introduced since last 50 years, none of them has achieved to be the single most efficient treatment of rhizarthrosis. As the detail of the surgical techniques of all described procedures is not the aim of this review, a concise explanation of these methods will be discussed together with clinical results of relevant studies.
Trapeziectomy with or without tendon interposition or ligament reconstruction: The total excision of the trapezium was described firstly in 1949[39]. It was also called as “hematoma arthroplasty”[40]. Although symptomatology was not believed to correlate with its late problems, trapeziectomy alone does carry the risk of shortening of trapezial height and scaphoid impingement. That is why when trapeziectomy is performed alone; fixation with a K-wire is advised to prevent the height loss to some extent[41]. Based on mostly short-term follow-up studies, trapeziectomy alone yielded good clinical results[41,42]. In a Level III study by Ritchie et al[43], it was shown that anterior approach yielded better clinical results than posterior approach.
There are two main methods, which can be added to total trapeziectomy; tendon interposition (TI) or ligament reconstruction (LR). The main aim of the LRTI is the reconstruction of AOL by using the half of flexor carpi radialis tendon or abductor pollicis longus tendon. TI arthroplasty by using the half of FCR tendon was firstly described in 1973[7]. The first description of LRTI arthroplasty was first described in 1986[37]. Although the strength and stability may not be restored fully with these procedures, it is possible to obtain a painless joint, as their main advantage[44]. Other than tendons, interposition with fascia lata, chondral tissue, Gelfoam, Gore-Tex, Marlex, Artelon implants, etc., were also reported[45-48]. Due to increased complications with non-autologous tissue, autologous tissue interposition should be preferred[45].
In a recent survey study among the active members of the American Academy for Surgery of the Hand, it was concluded that, trapeziectomy + LRTI was the treatment of choice by most surgeons and that the process of choosing treatment strategies was a question of future[49]. Longer follow-up clinical results also support the use of LRTI arthroplasty[50].
According to the current literature, three important results are obvious[42,51-54]. Firstly the addition of LR or TI to trapeziectomy has no clinical superiority over trapeziectomy alone. Secondly, trapeziectomy with LRTI was found to have more complications than trapeziectomy alone. At last, trapeziectomy alone or with LRTI have no evidence-based clinical superiority over other techniques.
TMC joint arthrodesis: Another alternative technique for the treatment of rhizarthrosis is the arthrodesis of this joint. The optimal position of the arthrodesis was defined classically as 45 degrees of abduction and antepulsion, slight pronation of the thumb[53]. Since the first report on its results[54], high-level randomized studies are still lacking. One problem related with arthrodesis is the relatively high rates of delayed union and non-union (8%-21%), especially when K-wire is used[55-58]. Although complication and reoperation rates are higher than that of trapeziectomy or trapeziectomy + LRTI, this was not found to be significant clinically[59]. In a recent prospective, randomized study by Vermuelen et al[60] arthrodesis was not recommended in the treatment of women who are forty years or older with stage II or III rhizarthrosis.
In conclusion, high-level randomized studies are still needed for definite conclusions of the clinical efficacy of TMC joint arthrodesis. So it should not be used as a first-line treatment especially in young patients.
TMC joint replacement: The first prosthetic replacement of TMC joint following trapeziectomy was performed by Swanson at late 1960s[61]. In this technique, trapezial Silicastic implants were used. In the two main review studies in the literature by Martou et al[53] and Wajon et al[54], it was pointed out that silicastic implants had high complication rates with only short term clinical satisfaction and that silicone arthroplasty had no additional benefits but comparable adverse effects when compared with trapeziectomy and LRTI, respectively. It was also revealed from these studies that these implants have more long-term complications such as subluxation, fractures and silicone synovitis[62].
Total TMC joint arthroplasty has evolved over time since its first development at early 1970s[63]. Currently, this option is advisable for stages II and III, with its reported mostly better outcomes and lesser implant failures[53,64-67]. The amelioration of the outcomes and decrements of failures may be attributable to the gradual improvement of the quality of the implants. Prospective randomized studies with long-term follow-up are required in order to make concrete conclusion on various arthroplasty options and on their cost-effectiveness.
Thumb metacarpal osteotomy: The closing wedge abduction osteotomy at the level of proximal metacarpus of the thumb was firstly introduced in 1973[68]. Although the studies lack both sufficient sample size and higher level of scientific evidence, it was advised to prefer this technique at earlier stages -at most stage I or II[69].
Other treatment methods of denervation of TMC joint, reconstruction of the volar beak ligament, suture button suspensionplasty and role of arthroscopy: Besides the core treatment options mentioned before, there are other methods described in the literature for Rhizarthrosis, such as: denervation of the TMC joint, reconstruction of the volar beak ligament, suture button suspensionplasty and TMC joint arthroscopy[70-72]. The common point for all of these procedures is that prospective, randomized, comparative studies are required in order to determine for using which method for which group of patients.
The TMC joint is a common region in the body, where OA is encountered, especially in the postmenopausal women. Although the exact etiology is not still certain, ligamentous laxity is a common finding in most of the cases. Regarding to the existing literature, the most commonly used treatment methods are conservative measures and trapeziectomy with LRTI. Moreover newer treatment methods have emerged in the recent years. In conclusion, if long-term prospective, randomized, comparative studies are performed, there will be an appropriate answer to choose the optimal treatment methods for each stage of rhizarthrosis.
P- Reviewer: Zhai G S- Editor: Tian YL L- Editor: A E- Editor: Jiao XK
| 1. | Peyron JG. Osteoarthritis. The epidemiologic viewpoint. Clin Orthop Relat Res. 1986;13-19. [PubMed] |
| 2. | Armstrong AL, Hunter JB, Davis TR. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg Br. 1994;19:340-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 354] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 3. | Swigart CR, Eaton RG, Glickel SZ, Johnson C. Splinting in the treatment of arthritis of the first carpometacarpal joint. J Hand Surg Am. 1999;24:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 97] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Clifton KB, Rodner C, Wolf JM. Detection of relaxin receptor in the dorsoradial ligament, synovium, and articular cartilage of the trapeziometacarpal joint. J Orthop Res. 2014;32:1061-1067. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Eaton RG, Littler JW. A study of the basal joint of the thumb. Treatment of its disabilities by fusion. J Bone Joint Surg Am. 1969;51:661-668. [PubMed] |
| 6. | Cho KO. Translocation of the abductor pollicis longus tendon. A treatment for chronic subluxation of the thumb carpometacarpal joint. J Bone Joint Surg Am. 1970;52:1166-1170. [PubMed] |
| 7. | Eaton RG, Littler JW. Ligament reconstruction for the painful thumb carpometacarpal joint. J Bone Joint Surg Am. 1973;55:1655-1666. [PubMed] |
| 8. | Pellegrini VD, Olcott CW, Hollenberg G. Contact patterns in the trapeziometacarpal joint: the role of the palmar beak ligament. J Hand Surg Am. 1993;18:238-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 139] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 9. | Lin JD, Karl JW, Strauch RJ. Trapeziometacarpal joint stability: the evolving importance of the dorsal ligaments. Clin Orthop Relat Res. 2014;472:1138-1145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Haines RW. The mechanism of rotation at the first carpo-metacarpal joint. J Anat. 1944;78:44-46. [PubMed] |
| 11. | Napier JR. The form and function of the carpo-metacarpal joint of the thumb. J Anat. 1955;89:362-369. [PubMed] |
| 12. | Bojsen-Moller F. Osteoligamentous guidance of the movements of the human thumb. Am J Anat. 1976;147:71-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Eaton RG, Lane LB, Littler JW, Keyser JJ. Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg Am. 1984;9:692-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 318] [Cited by in RCA: 305] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Drewniany JJ, Palmer AK, Flatt AE. The scaphotrapezial ligament complex: an anatomic and biomechanical study. J Hand Surg Am. 1985;10:492-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 81] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Bettinger PC, Linscheid RL, Berger RA, Cooney WP, An KN. An anatomic study of the stabilizing ligaments of the trapezium and trapeziometacarpal joint. J Hand Surg Am. 1999;24:786-798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 158] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 16. | Bettinger PC, Berger RA. Functional ligamentous anatomy of the trapezium and trapeziometacarpal joint (gross and arthroscopic). Hand Clin. 2001;17:151-168, vii. [PubMed] |
| 17. | Edmunds JO. Current concepts of the anatomy of the thumb trapeziometacarpal joint. J Hand Surg Am. 2011;36:170-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 114] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 18. | D’Agostino P, Kerkhof FD, Shahabpour M, Moermans JP, Stockmans F, Vereecke EE. Comparison of the anatomical dimensions and mechanical properties of the dorsoradial and anterior oblique ligaments of the trapeziometacarpal joint. J Hand Surg Am. 2014;39:1098-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 19. | Ghavami A, Oishi SN. Thumb trapeziometacarpal arthritis: treatment with ligament reconstruction tendon interposition arthroplasty. Plast Reconstr Surg. 2006;117:116e-128e. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Pellegrini VD. Osteoarthritis of the trapeziometacarpal joint: the pathophysiology of articular cartilage degeneration. I. Anatomy and pathology of the aging joint. J Hand Surg Am. 1991;16:967-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 175] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 21. | Strauch RJ, Behrman MJ, Rosenwasser MP. Acute dislocation of the carpometacarpal joint of the thumb: an anatomic and cadaver study. J Hand Surg Am. 1994;19:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 104] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Najima H, Oberlin C, Alnot JY, Cadot B. Anatomical and biomechanical studies of the pathogenesis of trapeziometacarpal degenerative arthritis. J Hand Surg Br. 1997;22:183-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Van Brenk B, Richards RR, Mackay MB, Boynton EL. A biomechanical assessment of ligaments preventing dorsoradial subluxation of the trapeziometacarpal joint. J Hand Surg Am. 1998;23:607-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 79] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Colman M, Mass DP, Draganich LF. Effects of the deep anterior oblique and dorsoradial ligaments on trapeziometacarpal joint stability. J Hand Surg Am. 2007;32:310-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 25. | Ladd AL, Lee J, Hagert E. Macroscopic and microscopic analysis of the thumb carpometacarpal ligaments: a cadaveric study of ligament anatomy and histology. J Bone Joint Surg Am. 2012;94:1468-1477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 87] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 26. | Glickel SZ, Kornstein AN, Eaton RG. Long-term follow-up of trapeziometacarpal arthroplasty with coexisting scaphotrapezial disease. J Hand Surg Am. 1992;17:612-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 51] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Eaton RG, Floyd WE. Thumb metacarpophalangeal capsulodesis: an adjunct procedure to basal joint arthroplasty for collapse deformity of the first ray. J Hand Surg Am. 1988;13:449-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 54] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Glickel SZ. Clinical assessment of the thumb trapeziometacarpal joint. Hand Clin. 2001;17:185-195. [PubMed] |
| 29. | Swanson AB, deGoot Swanson G, Watermeier JJ. Trapezium implant arthroplasty. Long-term evaluation of 150 cases. J Hand Surg Am. 1981;6:125-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 110] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Florack TM, Miller RJ, Pellegrini VD, Burton RI, Dunn MG. The prevalence of carpal tunnel syndrome in patients with basal joint arthritis of the thumb. J Hand Surg Am. 1992;17:624-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 66] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Day CS, Gelberman R, Patel AA, Vogt MT, Ditsios K, Boyer MI. Basal joint osteoarthritis of the thumb: a prospective trial of steroid injection and splinting. J Hand Surg Am. 2004;29:247-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 99] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 32. | Karalezli N, Ogun TC, Kartal S, Saracgil SN, Yel M, Tuncay I. The pain associated with intraarticular hyaluronic acid injections for trapeziometacarpal osteoarthritis. Clin Rheumatol. 2007;26:569-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Moran SL, Duymaz A, Karabekmez FE. The efficacy of hyaluronic acid in the treatment of osteoarthritis of the trapeziometacarpal joint. J Hand Surg Am. 2009;34:942-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Swindells MG, Logan AJ, Armstrong DJ, Chan P, Burke FD, Lindau TR. The benefit of radiologically-guided steroid injections for trapeziometacarpal osteoarthritis. Ann R Coll Surg Engl. 2010;92:680-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 35. | Becker SJ, Bot AG, Curley SE, Jupiter JB, Ring D. A prospective randomized comparison of neoprene vs thermoplast hand-based thumb spica splinting for trapeziometacarpal arthrosis. Osteoarthritis Cartilage. 2013;21:668-675. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 36. | Maddali-Bongi S, Del Rosso A, Galluccio F, Sigismondi F, Matucci-Cerenic M. Is an intervention with a custom-made splint and an educational program useful on pain in patients with trapeziometacarpal joint osteoarthritis in a daily clinical setting? Int J Rheum Dis. 2014;Mar 6; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 37. | Burton RI, Pellegrini VD. Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11:324-332. [PubMed] |
| 38. | Marks M, Schoones JW, Kolling C, Herren DB, Goldhahn J, Vliet Vlieland TP. Outcome measures and their measurement properties for trapeziometacarpal osteoarthritis: a systematic literature review. J Hand Surg Eur Vol. 2013;38:822-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 39. | Gervis WH. Excision of the trapezium for osteoarthritis of the trapezio-metacarpal joint. J Bone Joint Surg Br. 1949;31B:537-559, illust. [PubMed] |
| 40. | Jones NF, Maser BM. Treatment of arthritis of the trapeziometacarpal joint with trapeziectomy and hematoma arthroplasty. Hand Clin. 2001;17:237-243. [PubMed] |
| 41. | Varley GW, Calvey J, Hunter JB, Barton NJ, Davis TR. Excision of the trapezium for osteoarthritis at the base of the thumb. J Bone Joint Surg Br. 1994;76:964-968. [PubMed] |
| 42. | Davis TR, Brady O, Dias JJ. Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint: a study of the benefit of ligament reconstruction or tendon interposition. J Hand Surg Am. 2004;29:1069-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 219] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 43. | Ritchie JF, Belcher HJ. A comparison of trapeziectomy via anterior and posterior approaches. J Hand Surg Eur Vol. 2008;33:137-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 44. | Pellegrini VD, Burton RI. Surgical management of basal joint arthritis of the thumb. Part I. Long-term results of silicone implant arthroplasty. J Hand Surg Am. 1986;11:309-324. [PubMed] |
| 45. | Muermans S, Coenen L. Interpositional arthroplasty with Gore-Tex, Marlex or tendon for osteoarthritis of the trapeziometacarpal joint. A retrospective comparative study. J Hand Surg Br. 1998;23:64-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 56] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 46. | Park MJ, Lichtman G, Christian JB, Weintraub J, Chang J, Hentz VR, Ladd AL, Yao J. Surgical treatment of thumb carpometacarpal joint arthritis: a single institution experience from 1995-2005. Hand (N Y). 2008;3:304-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 47. | Jörheim M, Isaxon I, Flondell M, Kalén P, Atroshi I. Short-term outcomes of trapeziometacarpal artelon implant compared with tendon suspension interposition arthroplasty for osteoarthritis: a matched cohort study. J Hand Surg Am. 2009;34:1381-1387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 48. | Pritchett JW, Habryl LS. A promising thumb Basal joint hemiarthroplasty for treatment of trapeziometacarpal osteoarthritis. Clin Orthop Relat Res. 2012;470:2756-2763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 49. | Wolf JM, Delaronde S. Current trends in nonoperative and operative treatment of trapeziometacarpal osteoarthritis: a survey of US hand surgeons. J Hand Surg Am. 2012;37:77-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 117] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 50. | Tomaino MM, Pellegrini VD, Burton RI. Arthroplasty of the basal joint of the thumb. Long-term follow-up after ligament reconstruction with tendon interposition. J Bone Joint Surg Am. 1995;77:346-355. [PubMed] |
| 51. | Belcher HJ, Nicholl JE. A comparison of trapeziectomy with and without ligament reconstruction and tendon interposition. J Hand Surg Br. 2000;25:350-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 130] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 52. | Davis TR, Pace A. Trapeziectomy for trapeziometacarpal joint osteoarthritis: is ligament reconstruction and temporary stabilisation of the pseudarthrosis with a Kirschner wire important? J Hand Surg Eur Vol. 2009;34:312-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 86] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 53. | Martou G, Veltri K, Thoma A. Surgical treatment of osteoarthritis of the carpometacarpal joint of the thumb: a systematic review. Plast Reconstr Surg. 2004;114:421-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 136] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 54. | Wajon A, Carr E, Edmunds I, Ada L. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2009;CD004631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 55. | Muller GM. Arthrodesis of the trapezio-metacarpal joint for osteoarthritis. J Bone Joint Surg Br. 1949;31B:540-552, illust. [PubMed] |
| 56. | Taylor EJ, Desari K, D’Arcy JC, Bonnici AV. A comparison of fusion, trapeziectomy and silastic replacement for the treatment of osteoarthritis of the trapeziometacarpal joint. J Hand Surg Br. 2005;30:45-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 57. | Raven EE, Kerkhoffs GM, Rutten S, Marsman AJ, Marti RK, Albers GH. Long term results of surgical intervention for osteoarthritis of the trapeziometacarpal joint: comparison of resection arthroplasty, trapeziectomy with tendon interposition and trapezio-metacarpal arthrodesis. Int Orthop. 2007;31:547-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 58. | Singh HP, Hoare C, Beresford-Cleary N, Anakwe R, Hayton M. Nonunion after trapeziometacarpal arthrodesis: comparison between K-wire and internal fixation. J Hand Surg Eur Vol. 2015;40:351-355. [PubMed] |
| 59. | Forseth MJ, Stern PJ. Complications of trapeziometacarpal arthrodesis using plate and screw fixation. J Hand Surg Am. 2003;28:342-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 60. | Vermeulen GM, Brink SM, Slijper H, Feitz R, Moojen TM, Hovius SE, Selles RW. Trapeziometacarpal arthrodesis or trapeziectomy with ligament reconstruction in primary trapeziometacarpal osteoarthritis: a randomized controlled trial. J Bone Joint Surg Am. 2014;96:726-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 61. | Swanson AB. Silicone rubber implants for replacement of arthritis or destroyed joints in the hand. Surg Clin North Am. 1968;48:1113-1127. [PubMed] |
| 62. | Vermeulen GM, Slijper H, Feitz R, Hovius SE, Moojen TM, Selles RW. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011;36:157-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 341] [Cited by in RCA: 311] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 63. | de la Caffiniere JY, Aucouturier P. Trapezio-metacarpal arthroplasty by total prosthesis. Hand. 1979;11:41-46. [PubMed] |
| 64. | Amadio PC, De Silva SP. Comparison of the results of trapeziometacarpal arthrodesis and arthroplasty in men with osteoarthritis of the trapeziometacarpal joint. Ann Chir Main Memb Super. 1990;9:358-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 65. | Alnot JY, Muller GP. A retrospective review of 115 cases of surgically-treated trapeziometacarpal osteoarthritis. Rev Rhum Engl Ed. 1998;65:95-108. [PubMed] |
| 66. | Ulrich-Vinther M, Puggaard H, Lange B. Prospective 1-year follow-up study comparing joint prosthesis with tendon interposition arthroplasty in treatment of trapeziometacarpal osteoarthritis. J Hand Surg Am. 2008;33:1369-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 145] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 67. | Lluch AL, Garcia-Elias M, Lluch AB. Arthroplasty of the scaphoid-trapezium-trapezoid and carpometacarpal joints. Hand Clin. 2013;29:57-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 68. | Wilson JN. Basal osteotomy of the first metacarpal in the treatment of arthritis of the carpometacarpal joint of the thumb. Br J Surg. 1973;60:854-858. [PubMed] |
| 69. | Atroshi I, Axelsson G, Nilsson EL. Osteotomy versus tendon arthroplasty in trapeziometacarpal arthrosis: 17 patients followed for 1 year. Acta Orthop Scand. 1998;69:287-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 70. | Hartigan BJ, Stern PJ, Kiefhaber TR. Thumb carpometacarpal osteoarthritis: arthrodesis compared with ligament reconstruction and tendon interposition. J Bone Joint Surg Am. 2001;83-A:1470-1478. [PubMed] |
| 71. | Anley C, Ikram A, Y Elghawail, Wells M. Using a mini-TightRope (Arthrex) alone, to suspend the thumb metacarpal after a trapeziectomy: Is this a viable option? 1-year and 2 year results. J Hand Surg Eur. 2014;39E Suppl:92. |
| 72. | Slutsky DJ. The role of arthroscopy in trapeziometacarpal arthritis. Clin Orthop Relat Res. 2014;472:1173-1183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (1)] |