Published online Jul 12, 2015. doi: 10.5499/wjr.v5.i2.69
Peer-review started: November 19, 2014
First decision: February 7, 2015
Revised: February 25, 2015
Accepted: May 5, 2015
Article in press: May 6, 2015
Published online: July 12, 2015
Processing time: 231 Days and 10.3 Hours
Knee osteoarthritis (OA) is a progressive joint disease hallmarked by cartilage and bone breakdown and associated with changes to all of the tissues in the joint, ultimately causing pain, stiffness, deformity and disability in many people. Radiographs are commonly used for the clinical assessment of knee OA incidence and progression, and to assess for risk factors. One risk factor for the incidence and progression of knee OA is malalignment of the lower extremities (LE). The hip-knee-ankle (HKA) angle, assessed from a full-length LE radiograph, is ideally used to assess LE alignment. Careful attention to LE positioning is necessary to obtain the most accurate measurement of the HKA angle. Since full-length LE radiographs are not always available, the femoral shaft - tibial shaft (FS-TS) angle may be calculated from a knee radiograph instead. However, the FS-TS angle is more variable than the HKA angle and it should be used with caution. Knee radiographs are used to assess the severity of knee OA and its progression. There are three types of ordinal grading scales for knee OA: global, composite and individual feature scales. Each grade on a global scale describes one or more features of knee OA. The entire description must be met for a specific grade to be assigned. The Kellgren-Lawrence scale is the most commonly-used global scale. Composite scales grade several features of knee OA individually and sum the grades to create a total score. One example is the compartmental grading scale for knee OA. Composite scales can respond to change in a variety of presentations of knee OA. Individual feature scales assess one or more OA features individually and do not calculate a total score. They are most often used to monitor change in one OA feature, commonly joint space narrowing. The most commonly-used individual feature scale is the OA Research Society International atlas. Each type of scale has its advantages; however, composite scales may offer greater content validity. Responsiveness to change is unknown for most scales and deserves further evaluation.
Core tip: Radiographs are commonly used for the clinical assessment of knee osteoarthritis (OA) and to assess for risk factors. One risk factor for knee OA is malalignment of the lower extremities (LE). LE alignment is ideally measured from a full-length LE radiograph. While knee radiographs are sometimes used, the resulting angle is much more variable and should be used with caution. Knee radiographs are also used to assess the severity of knee OA. Global, composite and individual feature grading scales may be used. Each type of scale has its advantages; however composite scales may offer greater content validity.
- Citation: Sheehy L, Cooke TDV. Radiographic assessment of leg alignment and grading of knee osteoarthritis: A critical review. World J Rheumatol 2015; 5(2): 69-81
- URL: https://www.wjgnet.com/2220-3214/full/v5/i2/69.htm
- DOI: https://dx.doi.org/10.5499/wjr.v5.i2.69
Osteoarthritis (OA) is a progressive joint disease hallmarked by cartilage and bone breakdown. In knee OA, excessive or prolonged force or instability leads to fibrillation and thinning of the articular cartilage[1]. Associated with cartilage changes, the periarticular bone remodels, causes osteophytes. Erosion of the subchondral bone occurs as the cartilage continues to wear. Deeper into the bone structure, areas of sclerosis and cysts form. It has been acknowledged recently that other tissues, such as ligaments, menisci and synovium are also affected in knee OA. These whole joint changes ultimately cause pain, stiffness, deformity and disability in many people.
The prevalence of knee OA ranges from 5.4% in Italy to 38% in South Korea[2-9]. These numbers show the rate at which the population is affected by knee OA, and suggest that a significant portion of older adults, at least one in twenty, and up to one in three, may be dealing with knee pain, stiffness and related disability.
Despite the increasing use of magnetic resonance imaging (MRI) for knee OA research, radiographs are most commonly used for the clinical assessment of knee OA incidence and progression. Articular features of knee OA such as osteophytes, joint space narrowing (JSN), sclerosis and bony deformity may be observed on a knee radiograph, which is simple and fast to obtain. Radiographs are also used to assess frontal-plane alignment. This information may be used to identify the risk of knee OA incidence and progression and may be used for treatment planning. The first part of this review will address the measurement of tibiofemoral (TF) frontal-plane alignment. The measurement of knee OA severity and progression from knee radiographs will be discussed in the second part of this review.
Malalignment of the lower extremity (LE) has been identified as one factor associated with knee OA development[10]. Being bow-legged (varus, genu varum) is the most common frontal-plane malalignment; it leads to increased loading in the medial TF compartment[11]. Being knock-kneed (valgus, genu valgum) decreases the loading in the medial TF compartment but increases the loading in the lateral TF compartment. Increased loading is associated with an increased risk of OA in that TF compartment. Progression of existing knee OA is highly associated with varus [odds ratio (OR) 2.90 to 10.96, P < 0.05] and valgus (OR 3.42 to 10.44, P < 0.05) deformities[11-17]. The risk for progression increases with the degree of deformity[11,13,14,16,18]. The association of knee OA onset and malalignment is weaker (varus OR 2.1, P < 0.05; valgus OR 2.5, P < 0.05)[16,17].
It is important that LE alignment is measured accurately, so that interventions can be prescribed appropriately, and research studies which include LE alignment can be compared to one another. The presence of varus or valgus alignment may suggest the need for early intervention, for example, orthotics, braces or surgical correction (tibial osteotomy)[16,19]. An accurate measurement of alignment is also essential for proper placement of the implant during knee arthroplasty surgery. Proper placement resulting in restoration of neutral alignment ensures more even load distribution and prevention of premature wear and loosening of the implanted joints[20-25].
The diagnosis of knee OA is based on symptoms of pain and stiffness, and the presence of OA changes on a knee radiograph. Assessment of the knee by plain radiographs is routinely done to define the presence and severity of knee OA for diagnosis, to monitor progression and to guide treatment decisions[26-29]. In research studies, radiographic assessments are also used to guide participant eligibility and to stratify participants according to OA severity[5,30]. Individual characteristics such as biometrics (body mass index, age, etc.), involvement of other joints, malalignment, family history and history of injury are commonly correlated to measures of knee OA severity to investigate risk factors[30-36]. Studies of potentially disease-modifying OA drugs and other treatments also use knee OA assessments as outcome measures[37,38].
Grading scales are applied to knee radiographs to rate the severity of OA (Table 1). Current scales vary from poor to excellent in their reliability[26,39,40], poor to moderate in their sensitivity to change[41,42] and negligible to moderate in their relationship to other knee OA features (pain, alignment, function)[43-45]. Consistent use of a reliable, valid and responsive grading scale would ensure relevant longitudinal clinical evaluations and the ability to compare results between research studies.
| Scale type | Ref. | Pros | Cons | Uses |
| Global | Kellgren and Lawrence[67,69] | Widely used Adopted by the World Health Organization (1961) and at the 3rd International Symposium of Rheumatic Disease (1966) Moderate to excellent reliability | Multiple descriptions of the levels have been published Emphasizes osteophytes Poor sensitivity to change | Epidemiological studies Outcome measure (research) Clinical use |
| Ahlbäck[65] Galli[91] | One version uses a template, placed over a radiograph, to show typical bone contour | Poor reliability Emphasizes joint space narrowing | Epidemiological studies | |
| Sundaram et al[68] | No psychometric testing Defines early OA as osteophytes only | Epidemiological study for knee OA after tibial dome osteotomy | ||
| Brandt et al[66] | Good correlation to damage seen at arthroscopy | No reliability testing performed Emphasizes joint space narrowing | Classify participants for research studies | |
| Composite | Satku et al[97] | Includes a variety of features of knee OA | No psychometric testing | Used in research to describe OA development after anterior cruciate ligament tears |
| Kannus et al[96] | Includes many features of knee OA, in a variety of locations in the knee Good reliability | Very complicated | Used in research to describe OA development after anterior cruciate ligament tears | |
| McAlindon et al[99] | Moderate reliability Includes several compartments of the knee | Assesses both knees at once | Research on the association between knee pain, disability, strength and radiographic evidence of knee OA | |
| Merchant et al[98] | Includes several features of knee OA | No psychometric testing | Research on the onset of knee OA after ankle or lower leg injuries | |
| Compartmental grading scale for knee OA (CG) Cooke et al[100] | Includes several features of knee OA Excellent reliability | Epidemiological studies Part of the Knee Surgery Triage Tool | ||
| Individual | Osteoarthritis Research Society International atlas Altman et al[26] | Most commonly-used individual OA feature scale Moderate reliability | Often used to assess only joint space narrowing | Epidemiological studies Monitor progression of knee OA |
| Thomas et al[110] | No psychometric testing | |||
| Cooper et al[105] | No psychometric testing | |||
| Spector et al[30,34,109] Braga et al[116] O'Reilly et al[117] | Fair to excellent reliability | Epidemiological studies Classify participants for intervention studies | ||
| Scott feature based scoring system Scott et al[82] | Scores 8 different OA features Fair to excellent reliability | Epidemiological studies Outcome measure | ||
| Nottingham logically derived line drawing atlas Nagaosa et al[107] | Line drawings are meant to avoid problems using radiographs in an atlas Moderate reliability | Epidemiological studies Outcome measure (research) | ||
| Knee images digital analysis Marijnissen et al[130] Muraki et al[131] | Uses continuous scales Excellent reliability | Only good-quality radiographs can be used | Epidemiological studies | |
| Knee OA computer-aided diagnosis Oka et al[81] | Uses continuous scales Excellent reliability | Epidemiological studies |
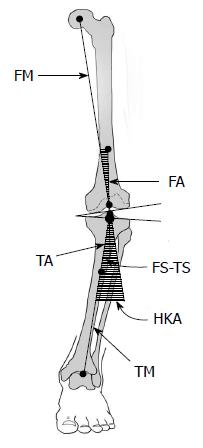
The criterion standard measure of frontal-plane LE alignment is the hip-knee-ankle (HKA) angle, also known as the mechanical axis angle, measured from a full-length LE radiograph[46-48]. This is the angle subtended by a line drawn from the centre of the femoral head to the center of the knee (femoral mechanical axis) with a line drawn from the center of the knee to the centre of the tibial plafond or ankle talus (tibial mechanical axis) (Figure 1). Varus angles are commonly designated negative and valgus angles positive[48]. “Normal” alignment in healthy adults is generally considered to be 1° to 1.5° of varus, or -1° to -1.5°[49-51].
The points used for determining the HKA angle have varied, especially around the knee[47,48]. The centre of the femoral head is found by placing a circle template over the femoral head on the radiograph, then marking the centre of this circle. There are several locations which may be used for the points at the knee. Many use a single point, often the centre of the tibial spines[11,47,49]. Moreland et al[51] used a single point at the knee that was the average of several measured knee landmarks. Others used the centre of the femoral intercondylar notch as the distal point for the femoral mechanical axis, and the centre of the tibial interspinous groove as the knee point for the tibial mechanical axis[11,48,52,53]. Using two points at the knee is preferred because it allows for the identification of the femoral and tibial contributions to deformity, and to define the extent of knee subluxation[48] (Figure 1). The centre of the talus or tibial plafond at the ankle is determined using a ruler placed on the radiographic image.
Use of a standardized and replicable approach for LE positioning is important for reliable and accurate alignment measurements. Changes in limb rotation, foot position and knee flexion alter the HKA angle[46,48,54,55]. For example, external rotation has been shown to increase the appearance of varus malalignment[56]. Some authors use a self-selected stance or the Romberg stance position (with medial borders of feet touching)[57]. Others use anatomical landmarks based on such features as the patella and the tibial tubercle[46]. None of these methods account for the variability between individuals with respect to rotation of the femur and tibia, position of the bony landmarks, flexibility of the feet (for example, pes planus leads to internal rotation of the tibia) and the relative length of the hip musculature (for example, a tight piriformis can lead to excessive external rotation of the hip when in a self-selected stance position).
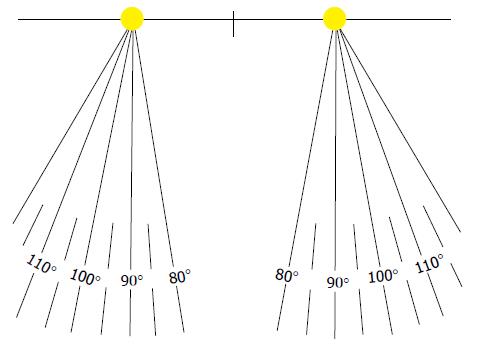
The LE should be positioned in neutral alignment such that the knee flexion angle is directly in the sagittal plane[46]. This is accomplished by positioning the patient or participant with the heels placed a standard distance apart (for example, 9 cm between the centres of the heels) and adjusting the rotation of the legs until the knee flexion axis, observed as the knee is flexed and extended, lies directly in the frontal plane. Foot position may be recorded from a template marked in degrees of internal and external rotation (Figure 2). Use of a template allows for reliable repositioning at subsequent assessments.
Full-length LE radiographs are not always used. They require specialized equipment and technician training, are more costly and expose the patient to higher doses of radiation, particularly at the pelvis. As a result, knee radiographs are often used to estimate alignment and the HKA angle[17,58]. The angle calculated on a knee radiograph is called the femoral shaft-tibial shaft (FS-TS) angle, or the anatomic axis angle[47]. This is the angle subtended by a line drawn from the centre of the femoral shaft proximal to the knee (femoral anatomic axis) and a line drawn from the centre of the tibial shaft distal to the knee (tibial anatomic axis). The femoral and tibial shaft points are generally measured 10 cm from the knee joint, to accommodate the portion of the long-bone shafts commonly seen on a knee radiograph[47,51]. The tibial anatomic axis is similar to the tibial mechanical axis (Figure 1). Similar to the definition of the HKA angle, one or two points at the knee may be chosen to determine the anatomic axes[59]. The tibial interspinous point is frequently used as a single point reference at the knee[47,49].
There are concerns that the FS-TS angle does not produce an accurate estimate of the HKA angle[53,60]. The FS-TS angle is offset towards valgus compared to the HKA angle by 4° to 6° for healthy individuals and 1.5° to 7° in individuals with knee OA[47,49,52,59,61], with a low to high correlation between the two measurements, r = 0.34 to 0.88, P < 0.005 in participants with knee OA[47,58,59,61,62]. The offset between the HKA and FS-TS angles is significantly greater in individuals with knee OA compared to healthy controls (t-test, P < 0.001)[52]. Two factors influence the relationship between the FS-TS and HKA angles. The first is the nature and severity of varus or valgus deformity[52,63,64]. The second factor is the length of the femoral and tibial shafts used when calculating the FS-TS angle[49,51]. In two studies, the FS-TS angle measured with a short femoral anatomic axis was 4.0° to 4.2° more valgus than the HKA angle, but with a long femoral anatomic axis the difference was 5.8° and when using the entire femoral shaft the difference was 4.9° to 5.9°[49,51]. In another study, the FS-TS angle measured with a short femoral anatomic axis for individuals with moderate to severe varus alignment, was an average of 7.4° more valgus than the HKA angle while for individuals with moderate to severe valgus alignment, the FS-TS angle was an average of 2.3° more valgus[60]. These studies illustrate how the shape of the femoral shaft impacts the relationship between the HKA and FS-TS angles. In order of importance, lateral bowing of the femoral shaft, tibial bowing and the angle between the tibial plateau and the tibial shaft all influence the relationship between these angles[52]. The FS-TS angle also shows more variability than the HKA angle[49,60]. The variability is increased when FS-TS angle measurements are calculated using a shorter amount of the femoral and tibial shaft lengths. Therefore it is recommended that the HKA angle, measured from a full-length LE radiograph, should be used to ensure an accurate measurement of LE alignment[62].
Because frontal-plane alignment is an important risk factor for the onset and especially the progression of knee OA, it is regularly assessed for research and clinical purposes. The “gold standard” evaluation of frontal-plane alignment is the HKA angle measured from a full-length LE radiograph; however knee radiographs are often used to calculate the FS-TS angle, used to estimate the HKA angle. There is an offset between these angles of 4° to 6°, but this offset varies depending on the type and degree of malalignment of the individual, and the method used to calculate the FS-TS angle. For the above reasons, we strongly recommend that the HKA angle be used for clinical and research purposes whenever accurate information on alignment is needed. Attention to careful positioning of the limb with the knee flexion axis directly in the frontal plane will reduce rotational errors.
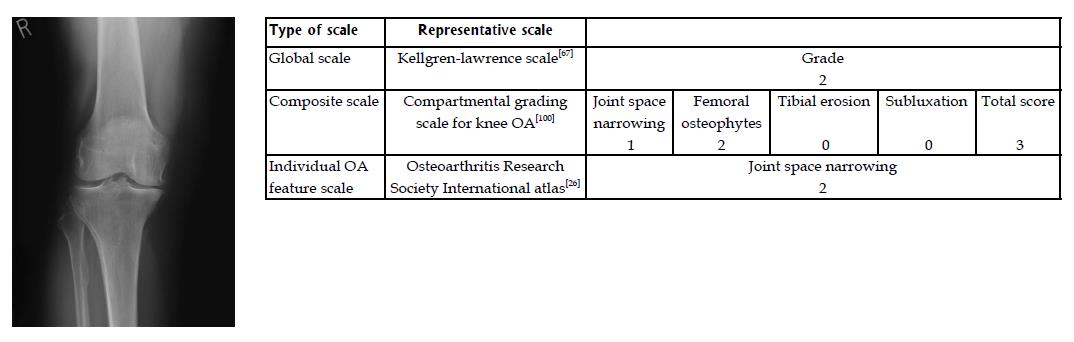
Global scales are ordinal scales that have specific descriptions for each grade[65-68]. Each level describes one or more features of OA that must be met for that particular level to be ascribed to a radiographic image. Global scales require an individual’s particular presentation of OA to “fit” all of the criteria for a given level of the scale. The earliest and by far the most commonly-used global scale is the Kellgren-Lawrence (KL) grading scale[67] (Figure 3). Others include those developed by Ahlback[65], Sundaram et al[68] and Brandt et al[66].
The KL scale, first described in 1957, gives an overall score of OA severity from zero to four[67,69]. Their scale was applied widely for any joints affected by OA and served as an important screening tool in epidemiological studies. In their initial publication the authors considered the following features evidence of OA: osteophytes on the joint margins or the tibial spines; periarticular ossicles; narrowing of joint space associated with sclerosis of subchondral bone; small pseudocystic areas, usually in the subchondral bone; and altered shape of the bone ends[67]. Both TF compartments of the knee were assessed using a standard set of radiographs for reference. Considering all features of OA, a grade of zero (no OA), one (doubtful OA), two (minimal OA), three (moderate OA), or four (severe OA) was given. Inter-rater reliability was reported (Pearson’s r = 0.83), but the authors acknowledged that one of the two readers consistently assessed the radiographs as showing more severe OA, illustrating the difficulty of using Pearson’s correlation coefficients to adequately assess reliability. Intra-rater reliability was the same (Pearson’s r = 0.83).
In 1963 an atlas (republished in 2005[70]) was produced by Kellgren et al[69] which included written descriptions of each grade: Grade 1: doubtful narrowing of joint space and possible osteophytic lipping; Grade 2: definite osteophytes and possible narrowing of joint space; Grade 3: moderate multiple osteophytes, definite narrowing of joint space and some sclerosis and possible deformity of bone ends; and Grade 4: large osteophytes, marked narrowing of joint space, severe sclerosis and definite deformity of bone ends.
Later, in a 1977 publication, Lawrence[71] described the grades as such: Grade 1: minute osteophyte of doubtful significance the only feature; Grade 2: definite osteophyte, joint space unimpaired; Grade 3: moderate diminution of joint space; and Grade 4: joint space greatly impaired, subchondral sclerosis.
The KL scale was adopted by the World Health Organization in 1961 and has remained the most prominent scale for screening OA and grading disease severity[72]. Its use as a standard evaluation for radiographic knee OA was reconfirmed at the third International Symposium on Rheumatic Disease in New York in 1966[73]. OA incidence is defined by a KL grade of two[67].
Despite its widespread use, there are continuing concerns about the KL scale[72,74,75]. As evident in the above descriptions, osteophytes must be present for a KL grade greater than zero to be given. The radiographic presentations of knee OA vary. Some show JSN but lack osteophytes; they would be assessed as grade zero on the KL scale[66]. For the Framingham OA Study, Felson et al[76] modified the KL scale by adding a second grade two category for radiographs showing JSN without osteophytes. None of their participants actually fit this new category, highlighting the difficulties of using the KL scale for assessment of knee OA[76].
A second important issue is that there are multiple descriptions of the KL grades which create variability in their interpretation[40,74,77,78]. This variability may allow individual research participants to be misidentified as having, or not having, OA, and creates difficulty in comparing research studies[74,79].
Several authors have assessed the intra- and inter-rater reliability of the KL scale[39,40,80-83]. Intra-rater reliability [Cohen’s weighted kappa 0.50 to 0.88; Cohen’s kappa 0.84 to 0.99; Spearman’s correlation coefficient 0.89; Intraclass correlation coefficient (ICC) 0.85 to 0.93] and inter-rater reliability (Cohen’s weighted kappa 0.56 to 0.80; Cohen’s kappa 0.59 to 0.76; Spearman’s correlation coefficient 0.85; ICC 0.68 to 0.84) generally fall in the moderate to excellent range[39,40,80-85].
A lack of sensitivity to change using the KL scale has been reported[41], and although it was not created to follow change in OA severity over time, but rather to be used as a screening tool for epidemiological studies, it is frequently used for this purpose[74,86]. There are only five grades, and the scale is not linear. Differentiating between grades zero and one, and one and two can be especially difficult[74,79,87]. To illustrate this point, the border between “possible osteophytic lipping (grade one)” and “definite osteophytes (grade two)” is very subjective and the “narrowing of joint” in the grade three description can include joints with almost no joint narrowing to joints with almost no joint space left[74]. In order to increase its sensitivity to change, Felson et al[74] proposed two changes to the KL scale: grade two to include the requirement of both osteophytes and JSN, and a new grade, two/osteophyte, which describes a knee with osteophytes but no JSN. They do admit that further changes, while addressing some of the problems, might also add to the confusion created because of different definitions of the scale.
KL grades are moderately to poorly correlated with cartilage lesions (Spearman’s correlation r = 0.55, P < 0.01) and cartilage volume (Pearson’s correlation r = -0.30 to -0.49 depending on location, P < 0.01) as measured from MRI[44,88]. Correlations of KL grade to cartilage damage seen at arthroscopy are similar to those measured from MRI (Pearson’s correlation r = 0.49, CI: 0.38 to 0.59), with a higher association for the medial compartment[89,90]. These results suggest that the KL scale, with its emphasis on osteophytes, has significant limitations for the grading of knee OA severity.
Global scales other than the KL scale tend to focus on one feature of knee OA. Ahlback[65] published descriptions of six stages of knee OA based on the combination of JSN and bone attrition only[65,91]. Stages zero to two describe JSN only, with progressive bone attrition described in stages three to five. Ahlback and Rydberg[92] described the stages in a further publication with altered wording. Thirty five years after the initial description, two studies showed that intra-rater (Cohen’s weighted kappa 0.17 to 0.35; Cohen’s kappa 0.15 to 0.76) and inter-rater reliability (Cohen’s weighted kappa 0.18 to 0.45; Cohen’s kappa -0.01 to 0.21) of the Ahlback scale were variable but tended to be poor[91,93]. Dieppe et al[94] subsequently improved the reliability by using a template showing typical bone contour, to be laid over a knee radiograph.
Sundaram et al[68] created a seven-point radiographic scale to assess the entire TF joint for knee OA after tibial dome osteotomy. Their grading system was very similar to the KL scale in that osteophytes were considered the initial presentation of the disease, with JSN being identified at grade three. Psychometric testing was not performed on this scale.
Finally, Brandt et al[66] created a JSN-weighted scale that they contrasted to the KL scale. Secondary features included subchondral sclerosis, geodes and osteophytes. Brandt scale scores were compared to cartilage damage seen at arthroscopy; the Pearson’s correlation coefficient was r = 0.56 (CI: 0.46 to 0.65)[89]. This scale has been used to classify research participants for orthopaedic surgical outcomes research[95].
Composite scales score several features of OA individually, then add them to create a total score[96-100]. Felson et al[101] studied several radiographic features of OA and found that a combination of one or two features (osteophytes alone, or JSN and a bony feature such as a cyst, sclerosis or small osteophyte), each scored individually, correlated best with clinical symptoms of pain and crepitus, lending support to the usefulness of composite scales. Altman et al[26] also discovered that a sum of the individual scores for JSN, bone spurs, sclerosis, attrition and alignment was more sensitive to change over time than each individual score alone. Unlike global scales, composite scales are able to follow the course of several separate OA features, and can respond to change in individuals with a variety of radiographic presentations.
Two scales were designed to follow the development of knee OA in individuals with anterior cruciate ligament tears[96,97]. Satku et al[97] scale grades osteophytes, peaking of the tibial spine, JSN and subchondral sclerosis or cysts in several locations in the knee, each on a scale of zero to one or two, to give a total score of 14. Kannus et al[96] created a complicated scale that measured osteophytes, subchondral sclerosis, flattening of the femoral condyles, subchondral cysts, ligament calcification, JSN and angular deformity at a variety of locations within the knee. Individual scores were out of three to 12, for a total score of 100[96]. Lower scores denoted more severe disease. It was reported to have good to excellent intra-rater reliability (Cohen’s kappa 0.70) and inter-rater reliability (Pearson’s correlation 0.94; Spearman’s correlation 0.90)[102].
McAlindon et al[99] created a scale to investigate the association between knee pain, disability, knee strength and radiographic score. They scored JSN, osteophytes and sclerosis in several compartments of both knees to sum to a possible score of 30[99]. Intra-rater reliability was moderate (Cohen’s kappa of 0.57)[99]. Another scale was created by Merchant et al[98] to follow individuals after ankle or lower leg injuries to investigate the onset of knee OA changes. A “normal” joint was given a score of ten and points were subtracted for osteophytes, JSN, degenerative cysts and subchondral sclerosis observed in both TF compartments[98]. Psychometric testing was not reported.
The compartmental grading scale for knee OA (CG) was created in 1999 by Derek et al[100], who wished to create a scale that was correlated with changes in alignment and deformity caused by OA. The CG scores femoral osteophytes (out of three), JSN (out of three), tibial erosion (out of four) and subluxation (out of three) for a total possible score of 13 (Figure 3). Only the most-affected TF compartment is scored. Tibial osteophytes are excluded in order to prevent over-weighting the scale with osteophytes and because tibial osteophytes frequently decrease in size as OA worsens and the knee subluxes. Tibial erosion is included because it is common and may contribute to joint instability as it progresses. Similarly subluxation, a feature unique to the CG, is incorporated because it also contributes to joint instability and disability. The CG is highly correlated to frontal-plane alignment (Pearson’s correlation r = 0.77, P < 0.001). Sclerosis is not included because bone density is highly variable between people and is affected by obesity and variations in image quality. Equal weight is given to osteophytes, JSN and subluxation, and slightly more weight to tibial erosion. This approach was intended to reduce the emphasis of one feature (i.e., osteophytes) over another and provide for a balanced opportunity for sensitivity to change in those with different presentations of OA.
Initial results showed an inter-rater reliability (Cohen’s weighted kappa) of 0.92 using anteroposterior full-extension radiographs[100]. The CG has been used for research[103] and is a component of the Knee Surgery Triage tool, which incorporates disability evaluation and radiographic grading to guide clinicians in surgical decision-making[104].
Apart from the KL scale, the most common method to assess knee OA severity is to assign grades to individual features of OA such as osteophytes, JSN and sclerosis[26,82,105-110]. An atlas is used to guide interpretation of each feature. Even though each individual feature only describes one aspect of OA, individual feature scales are often used to monitor change over time. The most-often used individual OA feature scale was described by Altman et al[26].
The most commonly-used individual OA feature scale is the OA Research Society International (OARSI) atlas, which was created by Altman et al[26] (the San Francisco Conference Group) in 1987 (Figure 3). For the knee, five OA features were assessed [JSN, spur formation, loss of bone stock (attrition), subchondral bony sclerosis and frontal-plane alignment] and each scored from zero to three. Medial and lateral TF compartments were assessed separately (except for alignment), giving nine individual scores. A total score was not calculated. Initial intra-rater reliability scores (measured with ICCs) for each feature varied from 0.40 to 1.0, although it is important to note that only three radiographs were used for this analysis[26]. Inter-rater reliability scores (measured with ICCs) were slightly lower, varying between 0.32 and 0.86, with JSN having the best reliability. In all cases medial compartment scores were more reliable than lateral compartment scores. JSN and bone spurs were most sensitive to change over time.
In order to standardize the interpretation of radiographs, OARSI published another radiographic atlas in 1995 showing the spectrum of severity of three osteoarthritic features (JSN, marginal osteophytes and subchondral sclerosis), each scored from zero to three[111]. An updated atlas, available electronically, was published in 2007, emphasizing OA changes of medial and lateral femoral and tibial plateau osteophytes, medial and lateral JSN, medial tibial attrition, medial tibial sclerosis and lateral femoral sclerosis[112]. A modified version of the OARSI JSN scale was also created by Felson et al[13], whereby if JSN had increased over time, but not enough to warrant the next grade on the zero to three scale, a one-half grade was assigned. This modification enhanced sensitivity to change[13].
Grades assessed using the OARSI atlas have moderate to good reliability, with JSN more reliable than osteophytes[107]. Intra-rater reliability (Cohen’s kappa 0.57 to 0.91 for osteophytes, 0.77 to 0.83 for sclerosis and 0.68 to 0.80 or ICC 0.79 to 0.95 for JSN) is somewhat higher than inter-rater reliability (Cohen’s kappa 0.33 to 0.88 for osteophytes, 0.77 for sclerosis, and 0.48 to 0.70 or ICC 0.66 to 0.87 for JSN)[39,78,84,107,113,114].
Comparison of the OARSI atlas to findings from arthroscopy has been performed[115]. Osteophytes show moderate sensitivity (49% to 67%) compared to arthroscopy however the other OA features show fair to poor sensitivity (3% to 46%). Specificity of all features is good to excellent (73% to 100%) relative to arthroscopic findings.
Thomas et al[110] and Cooper et al[105] created ordinal scales for individual features of knee OA, similar to the OARSI scale. Thomas et al[110] scored osteophytes, JSN, sclerosis and cysts, each on a scale of zero to three. Cooper et al[105] scored these same four features, plus abnormality of the bony contour, each on a scale of zero to two. Neither scale has been used extensively. More extensive use was made of an atlas produced by Spector et al[30,34,109,116,117] which scored TF osteophytes, sclerosis, JSN and cortical collapse, each on a scale of zero to one or three. Intra-rater reliability (Cohen’s kappa 0.41 to 0.96) and inter-rater reliability (Cohen’s kappa 0.30 to 0.90) for osteophytes and JSN scored according to this scale ranged from fair to excellent[40,118].
Scott et al[82] published an atlas similar to the OARSI atlas which scored eight individual features of knee OA (medial and lateral osteophytes, medial and lateral JSN, medial and lateral subchondral sclerosis, osteophytes of the tibial spines and chondrocalcinosis) each on a scale from zero to one or three. Both medial and lateral TF compartments were included. This atlas was created for the Baltimore Longitudinal Study of Aging and is now referred to as the Scott Feature Based Scoring System[119]. It has been used in epidemiological studies and as an outcome measure[120-122]. Intra-rater reliability (ICC 0.80 to 0.89) and inter-rater reliability (ICC 0.40 to 0.87) have been tested for osteophytes, JSN and sclerosis scored with this system and ranged from fair to excellent[82,85].
The nottingham logically derived line drawing atlas (LDLDA) consisted of line drawings rather than photographs of radiographs[107]. JSN and osteophytes were scored on a scale of zero to three. The authors felt that line drawings could overcome some issues with the OARSI atlas[26], such as differences in magnification between radiographs and more than one OA feature shown on a particular radiograph. The LDLDA has been used to describe the participant sample in epidemiological studies[123], and as an outcome measure[124]. Also tested were variations of the scoring system described in the LDLDA, using grading scores from minus one to three, four and five[125], and from minus three to three, minus four to four, and minus five to five[126]. The authors expected that sensitivity to change might be enhanced with some of these variations, but did not actually test this hypothesis[125,126]. Finally, one of the modified scales was tested using an acetate overlay placed directly on the radiograph, to aid in determining the grades[127]. Reliability for each of these modified scales was as good as or better than the original scale[125-127].
Two scales used computer software to quantitatively assess knee radiographs for OA changes[81,128]. The knee images digital analysis was an interactive software tool created for the cohort hip and cohort knee study[128,129]. Joint space width, osteophyte area, subchondral bone density, joint angle and tibial eminence height were measured using continuous scales[128,129]. While intra- and inter-rater reliability were excellent, only good-quality radiographs could be fully analyzed by the software, and careful participant positioning was particularly important[129,130].
Knee OA computer-aided diagnosis was a fully automated diagnostic system that measured joint space area, minimum joint space width, osteophyte area and TF angle on continuous scales[81]. It was created for the research on OA against disability (ROAD) study[81,131,132]. The intra-rater reliability (ICC) for all parameters was 1.0[81]. Sensitivity to change has not been investigated, but the authors claimed that quantitative radiograph analysis could be as sensitive as quantitative MRI.
The accurate and reliable assessment of knee OA severity as seen on a radiograph is important for diagnosis and monitoring of disease progression. Since 1957, many global, composite and individual feature scales have been developed towards these goals. Global scales, while commonly used, may not be as valid or sensitive to change as other types of scales. Composite grading scales have the advantage that they can be responsive to different presentations of knee OA. Individual OA feature scales are often used to monitor the progression of knee OA, but only respond to changes in a particular OA feature.
The consistent use of one scale is useful to enable comparison of participant groups in research studies and the identification of risk factors. The KL grading scale has been most-commonly used in epidemiological and outcomes research to group and describe participants; however the KL scale has not always been applied consistently, limiting comparison between studies. The OARSI JSN scale is also commonly used, especially to monitor change in JSN, which is used as a proxy for worsening knee OA. However, the selective use of individual feature scales does not allow a variety of presentations of knee OA to be described and monitored. To overcome the above shortcomings, the use of a composite scale is suggested. Several individual features of OA are included, but a single total score gives an indication of the overall severity of arthritic change in the joint.
Many of the existing scales have not had adequate psychometric testing. Reliability, validity (concurrent, content) and sensitivity to change (responsiveness) need to be documented for a scale to be used confidently. However, in recent work, the authors, in collaboration with investigators from the multicenter OA study, evaluated the psychometric properties of the KL, OARSI and CG scales using MRI as a gold standard[133] (Unpublished observations). The findings indicate comparable reliability, validity and sensitivity to change. However the CG scale, which is not subject to the ceiling effects exhibited by the other two scales, suggested responsiveness to more severe joint changes. Further studies are required to establish this. Researchers using scales which do not have adequate testing should perform and report appropriate psychometric assessments as part of their study. In conclusion, the variation in grading scales indicates that a single method is not yet established that will meet the requirements of all needs. Careful consideration of the different grading scales is recommended before one is chosen for a clinical or research application.
The use of grading scales for clinical use is not widespread. Radiologists practicing in the clinical realm typically describe knee OA changes seen on radiographs and make a conclusion about the presence or absence and severity of disease, but do not use a specific grading scale. This practice can reduce the objectiveness of radiologists’ observations and make it difficult to detect change over time and compare reports by different radiologists. We recommend that grading scales be used to ensure consistency in interpreting and reporting radiographic knee OA for clinical use.
P- Reviewer: Garip Y, Singh A, Tawonsawatruk T S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Loeser RF, Goldring SR, Scanzello CR, Goldring MB. Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum. 2012;64:1697-1707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1550] [Cited by in RCA: 2084] [Article Influence: 160.3] [Reference Citation Analysis (2)] |
| 2. | Salaffi F, De Angelis R, Grassi W. Prevalence of musculoskeletal conditions in an Italian population sample: results of a regional community-based study. I. The MAPPING study. Clin Exp Rheumatol. 2005;23:819-828. [PubMed] |
| 3. | Guillemin F, Rat AC, Mazieres B, Pouchot J, Fautrel B, Euller-Ziegler L, Fardellone P, Morvan J, Roux CH, Verrouil E. Prevalence of symptomatic hip and knee osteoarthritis: a two-phase population-based survey. Osteoarthritis Cartilage. 2011;19:1314-1322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 132] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 4. | Andrianakos AA, Kontelis LK, Karamitsos DG, Aslanidis SI, Georgountzos AI, Kaziolas GO, Pantelidou KV, Vafiadou EV, Dantis PC. Prevalence of symptomatic knee, hand, and hip osteoarthritis in Greece. The ESORDIG study. J Rheumatol. 2006;33:2507-2513. [PubMed] |
| 5. | Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1034] [Cited by in RCA: 1050] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 6. | Jordan JM, Helmick CG, Renner JB, Luta G, Dragomir AD, Woodard J, Fang F, Schwartz TA, Abbate LM, Callahan LF. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34:172-180. [PubMed] |
| 7. | Jiang L, Rong J, Zhang Q, Hu F, Zhang S, Li X, Zhao Y, Tao T. Prevalence and associated factors of knee osteoarthritis in a community-based population in Heilongjiang, Northeast China. Rheumatol Int. 2012;32:1189-1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Muraki S, Oka H, Akune T, Mabuchi A, En-yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H. Prevalence of radiographic knee osteoarthritis and its association with knee pain in the elderly of Japanese population-based cohorts: the ROAD study. Osteoarthritis Cartilage. 2009;17:1137-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 298] [Article Influence: 18.6] [Reference Citation Analysis (1)] |
| 9. | Cho HJ, Chang CB, Kim KW, Park JH, Yoo JH, Koh IJ, Kim TK. Gender and prevalence of knee osteoarthritis types in elderly Koreans. J Arthroplasty. 2011;26:994-999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Tufan A, Meulenbelt I, Bijsterbosch J, Kroon HM, Bierma-Zeinstra SM, Nelissen RG, Kloppenburg M. Familial influence on tibiofemoral alignment. Ann Rheum Dis. 2010;69:542-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 989] [Cited by in RCA: 1049] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 12. | Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N, Torner J, Cooke TD, Hietpas J, Lynch J. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69:1940-1945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 315] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 13. | Felson DT, Nevitt MC, Yang M, Clancy M, Niu J, Torner JC, Lewis CE, Aliabadi P, Sack B, McCulloch C. A new approach yields high rates of radiographic progression in knee osteoarthritis. J Rheumatol. 2008;35:2047-2054. [PubMed] |
| 14. | Cerejo R, Dunlop DD, Cahue S, Channin D, Song J, Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46:2632-2636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 217] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 15. | Chapple CM, Nicholson H, Baxter GD, Abbott JH. Patient characteristics that predict progression of knee osteoarthritis: a systematic review of prognostic studies. Arthritis Care Res (Hoboken). 2011;63:1115-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 94] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 16. | Felson DT, Niu J, Gross KD, Englund M, Sharma L, Cooke TD, Guermazi A, Roemer FW, Segal N, Goggins JM. Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative. Arthritis Rheum. 2013;65:355-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 202] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 17. | Brouwer GM, van Tol AW, Bergink AP, Belo JN, Bernsen RM, Reijman M, Pols HA, Bierma-Zeinstra SM. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56:1204-1211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 396] [Cited by in RCA: 448] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 18. | Cicuttini F, Wluka A, Hankin J, Wang Y. Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology (Oxford). 2004;43:321-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 159] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 19. | Nourbakhsh M, Motififard M, Shemshaki H, Etemadifar Mr, Zarezade A, Farajzadegan Z, Mazoochian F. Efficacy of tibial proximal osteotomy in correction of lower limb alignment indexes in patients with osteoarthritis in medial compartment of knee. Med Arh. 2012;66:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 20. | Werner FW, Ayers DC, Maletsky LP, Rullkoetter PJ. The effect of valgus/varus malalignment on load distribution in total knee replacements. J Biomech. 2005;38:349-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 207] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 21. | Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153-156. [PubMed] |
| 22. | Koeck FX, Beckmann J, Luring C, Rath B, Grifka J, Basad E. Evaluation of implant position and knee alignment after patient-specific unicompartmental knee arthroplasty. Knee. 2011;18:294-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 23. | Zhang GQ, Chen JY, Chai W, Liu M, Wang Y. Comparison between computer-assisted-navigation and conventional total knee arthroplasties in patients undergoing simultaneous bilateral procedures: a randomized clinical trial. J Bone Joint Surg Am. 2011;93:1190-1196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 24. | NIH Consensus Statement on total knee replacement December 8-10, 2003. J Bone Joint Surg Am. 2004;86-A:1328-1335. [PubMed] |
| 25. | Wong J, Steklov N, Patil S, Flores-Hernandez C, Kester M, Colwell CW, D’Lima DD. Predicting the effect of tray malalignment on risk for bone damage and implant subsidence after total knee arthroplasty. J Orthop Res. 2011;29:347-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 26. | Altman RD, Fries JF, Bloch DA, Carstens J, Cooke TD, Genant H, Gofton P, Groth H, McShane DJ, Murphy WA. Radiographic assessment of progression in osteoarthritis. Arthritis Rheum. 1987;30:1214-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 261] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 27. | Cicuttini FM, Jones G, Forbes A, Wluka AE. Rate of cartilage loss at two years predicts subsequent total knee arthroplasty: a prospective study. Ann Rheum Dis. 2004;63:1124-1127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 192] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 28. | Fransen M, McConnell S. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev. 2008;4:CD004376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 181] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 29. | Guermazi A, Hunter DJ, Roemer FW. Plain radiography and magnetic resonance imaging diagnostics in osteoarthritis: validated staging and scoring. J Bone Joint Surg Am. 2009;91 Suppl 1:54-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Spector TD, Hart DJ, Doyle DV. Incidence and progression of osteoarthritis in women with unilateral knee disease in the general population: the effect of obesity. Ann Rheum Dis. 1994;53:565-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 184] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 31. | Hashikawa T, Osaki M, Ye Z, Tomita M, Abe Y, Honda S, Takamura N, Shindo H, Aoyagi K. Factors associated with radiographic osteoarthritis of the knee among community-dwelling Japanese women: the Hizen-Oshima Study. J Orthop Sci. 2011;16:51-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Hunter DJ, Niu J, Felson DT, Harvey WF, Gross KD, McCree P, Aliabadi P, Sack B, Zhang Y. Knee alignment does not predict incident osteoarthritis: the Framingham osteoarthritis study. Arthritis Rheum. 2007;56:1212-1218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 107] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 33. | Li RT, Lorenz S, Xu Y, Harner CD, Fu FH, Irrgang JJ. Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:2595-2603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 185] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 34. | Spector TD, Cicuttini F, Baker J, Loughlin J, Hart D. Genetic influences on osteoarthritis in women: a twin study. BMJ. 1996;312:940-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 455] [Cited by in RCA: 439] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 35. | Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13:769-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 682] [Cited by in RCA: 807] [Article Influence: 40.4] [Reference Citation Analysis (0)] |
| 36. | Vrezas I, Elsner G, Bolm-Audorff U, Abolmaali N, Seidler A. Case-control study of knee osteoarthritis and lifestyle factors considering their interaction with physical workload. Int Arch Occup Environ Health. 2010;83:291-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 37. | Abadie E, Ethgen D, Avouac B, Bouvenot G, Branco J, Bruyere O, Calvo G, Devogelaer JP, Dreiser RL, Herrero-Beaumont G. Recommendations for the use of new methods to assess the efficacy of disease-modifying drugs in the treatment of osteoarthritis. Osteoarthritis Cartilage. 2004;12:263-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 96] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 38. | Mazzuca SA, Brandt KD. Is knee radiography useful for studying the efficacy of a disease-modifying osteoarthritis drug in humans? Rheum Dis Clin North Am. 2003;29:819-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 39. | Gossec L, Jordan JM, Mazzuca SA, Lam MA, Suarez-Almazor ME, Renner JB, Lopez-Olivo MA, Hawker G, Dougados M, Maillefert JF. Comparative evaluation of three semi-quantitative radiographic grading techniques for knee osteoarthritis in terms of validity and reproducibility in 1759 X-rays: report of the OARSI-OMERACT task force. Osteoarthritis Cartilage. 2008;16:742-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 76] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 40. | Spector TD, Hart DJ, Byrne J, Harris PA, Dacre JE, Doyle DV. Definition of osteoarthritis of the knee for epidemiological studies. Ann Rheum Dis. 1993;52:790-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 179] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 41. | Amin S, LaValley MP, Guermazi A, Grigoryan M, Hunter DJ, Clancy M, Niu J, Gale DR, Felson DT. The relationship between cartilage loss on magnetic resonance imaging and radiographic progression in men and women with knee osteoarthritis. Arthritis Rheum. 2005;52:3152-3159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 163] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 42. | Emrani PS, Katz JN, Kessler CL, Reichmann WM, Wright EA, McAlindon TE, Losina E. Joint space narrowing and Kellgren-Lawrence progression in knee osteoarthritis: an analytic literature synthesis. Osteoarthritis Cartilage. 2008;16:873-882. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 136] [Cited by in RCA: 122] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 43. | Dieppe PA, Cushnaghan J, Shepstone L. The Bristol ‘OA500’ study: progression of osteoarthritis (OA) over 3 years and the relationship between clinical and radiographic changes at the knee joint. Osteoarthritis Cartilage. 1997;5:87-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 177] [Article Influence: 6.3] [Reference Citation Analysis (1)] |
| 44. | Link TM, Steinbach LS, Ghosh S, Ries M, Lu Y, Lane N, Majumdar S. Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology. 2003;226:373-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 356] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 45. | Sanghi D, Avasthi S, Mishra A, Singh A, Agarwal S, Srivastava RN. Is radiology a determinant of pain, stiffness, and functional disability in knee osteoarthritis? A cross-sectional study. J Orthop Sci. 2011;16:719-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 46. | Cooke TD, Sled EA. Optimizing limb position for measuring knee anatomical axis alignment from standing knee radiographs. J Rheumatol. 2009;36:472-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 47. | Kraus VB, Vail TP, Worrell T, McDaniel G. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum. 2005;52:1730-1735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 251] [Article Influence: 12.6] [Reference Citation Analysis (1)] |
| 48. | Cooke TD, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement. J Rheumatol. 2007;34:1796-1801. [PubMed] |
| 49. | Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215-227. [PubMed] |
| 50. | Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage. 1997;5:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 189] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 51. | Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745-749. [PubMed] |
| 52. | Chang CB, Choi JY, Koh IJ, Seo ES, Seong SC, Kim TK. What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthritis Cartilage. 2010;18:530-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 55] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 53. | Felson DT, Cooke TD, Niu J, Goggins J, Choi J, Yu J, Nevitt MC. Can anatomic alignment measured from a knee radiograph substitute for mechanical alignment from full limb films? Osteoarthritis Cartilage. 2009;17:1448-1452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 54. | Schmitt H, Kappel H, Moser MT, Cardenas-Montemayor E, Engelleiter K, Kuni B, Clarius M. Determining knee joint alignment using digital photographs. Knee Surg Sports Traumatol Arthrosc. 2008;16:776-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 55. | Siu D, Cooke TD, Broekhoven LD, Lam M, Fisher B, Saunders G, Challis TW. A standardized technique for lower limb radiography. Practice, applications, and error analysis. Invest Radiol. 1991;26:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 80] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 56. | Hunt MA, Fowler PJ, Birmingham TB, Jenkyn TR, Giffin JR. Foot rotational effects on radiographic measures of lower limb alignment. Can J Surg. 2006;49:401-406. [PubMed] |
| 57. | Moncrieff MJ, Livingston LA. Reliability of a digital-photographic-goniometric method for coronal-plane lower limb measurements. J Sport Rehabil. 2009;18:296-315. [PubMed] |
| 58. | Hinman RS, May RL, Crossley KM. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Rheum. 2006;55:306-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 192] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 59. | McDaniel G, Mitchell KL, Charles C, Kraus VB. A comparison of five approaches to measurement of anatomic knee alignment from radiographs. Osteoarthritis Cartilage. 2010;18:273-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 60. | Sheehy L, Felson D, Zhang Y, Niu J, Lam YM, Segal N, Lynch J, Cooke TD. Does measurement of the anatomic axis consistently predict hip-knee-ankle angle (HKA) for knee alignment studies in osteoarthritis? Analysis of long limb radiographs from the multicenter osteoarthritis (MOST) study. Osteoarthritis Cartilage. 2011;19:58-64. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 87] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 61. | Issa SN, Dunlop D, Chang A, Song J, Prasad PV, Guermazi A, Peterfy C, Cahue S, Marshall M, Kapoor D. Full-limb and knee radiography assessments of varus-valgus alignment and their relationship to osteoarthritis disease features by magnetic resonance imaging. Arthritis Rheum. 2007;57:398-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 76] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 62. | van Raaij TM, Brouwer RW, Reijman M, Bierma-Zeinstra SM, Verhaar JA. Conventional knee films hamper accurate knee alignment determination in patients with varus osteoarthritis of the knee. Knee. 2009;16:109-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 63. | Cooke TD. Static knee alignment and its association with radiographic knee osteoarthritis. Osteoarthritis Cartilage. 2007;15:844-845; author reply 844-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 64. | Nguyen C, Bryant JT, Cooke TDV, Chow D. Alignment and geometry of the normal knee in stance. J Bone Joint Surg Brit. 1989;71-B:346. |
| 65. | Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh). 1968;277:Suppl 277: 7-27772. [PubMed] |
| 66. | Brandt KD, Fife RS, Braunstein EM, Katz B. Radiographic grading of the severity of knee osteoarthritis: relation of the Kellgren and Lawrence grade to a grade based on joint space narrowing, and correlation with arthroscopic evidence of articular cartilage degeneration. Arthritis Rheum. 1991;34:1381-1386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 191] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 67. | Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9311] [Cited by in RCA: 8893] [Article Influence: 130.8] [Reference Citation Analysis (0)] |
| 68. | Sundaram NA, Hallett JP, Sullivan MF. Dome osteotomy of the tibia for osteoarthritis of the knee. J Bone Joint Surg Br. 1986;68:782-786. [PubMed] |
| 69. | Kellgren J, Jeffrey MR, Ball J. The epidemiology of chronic rheumatism: atlas of standard radiographs of arthritis. Oxford: Blackwell Scientific; 1963; . |
| 70. | The Atlas of Standard Radiographs of Arthritis. Rheumatology (Oxford). 2005;44 Suppl 4:iv46-iv72. [PubMed] |
| 71. | Lawrence J. Rheumatism in populations. London: W.M. Heinemann Medical Books 1977; . |
| 72. | Croft P. An introduction to the Atlas of Standard Radiographs of Arthritis. Rheumatology (Oxford). 2005;44 Suppl 4:iv42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 73. | Bellamy N, Bennett PH, Burch TA. New York symposium on population studies in rheumatic diseases: new diagnostic criteria. Bulletin Rheum Dis. 1967;17:453-458. |
| 74. | Felson DT, Niu J, Guermazi A, Sack B, Aliabadi P. Defining radiographic incidence and progression of knee osteoarthritis: suggested modifications of the Kellgren and Lawrence scale. Ann Rheum Dis. 2011;70:1884-1886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 120] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 75. | Spector TD, Cooper C. Radiographic assessment of osteoarthritis in population studies: whither Kellgren and Lawrence? Osteoarthritis Cartilage. 1993;1:203-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 127] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 76. | Felson DT, Zhang Y, Hannan MT, Naimark A, Weissman BN, Aliabadi P, Levy D. The incidence and natural history of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1995;38:1500-1505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 469] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 77. | Schiphof D, Boers M, Bierma-Zeinstra SM. Differences in descriptions of Kellgren and Lawrence grades of knee osteoarthritis. Ann Rheum Dis. 2008;67:1034-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 229] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 78. | Dowsey MM, Nikpour M, Dieppe P, Choong PF. Associations between pre-operative radiographic changes and outcomes after total knee joint replacement for osteoarthritis. Osteoarthritis Cartilage. 2012;20:1095-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 67] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 79. | Schiphof D, de Klerk BM, Kerkhof HJ, Hofman A, Koes BW, Boers M, Bierma-Zeinstra SM. Impact of different descriptions of the Kellgren and Lawrence classification criteria on the diagnosis of knee osteoarthritis. Ann Rheum Dis. 2011;70:1422-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 80. | Kessler S, Guenther KP, Puhl W. Scoring prevalence and severity in gonarthritis: the suitability of the Kellgren & amp; Lawrence scale. Clin Rheumatol. 1998;17:205-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 81. | Oka H, Muraki S, Akune T, Mabuchi A, Suzuki T, Yoshida H, Yamamoto S, Nakamura K, Yoshimura N, Kawaguchi H. Fully automatic quantification of knee osteoarthritis severity on plain radiographs. Osteoarthritis Cartilage. 2008;16:1300-1306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 82. | Scott WW, Lethbridge-Cejku M, Reichle R, Wigley FM, Tobin JD, Hochberg MC. Reliability of grading scales for individual radiographic features of osteoarthritis of the knee. The Baltimore longitudinal study of aging atlas of knee osteoarthritis. Invest Radiol. 1993;28:497-501. [PubMed] |
| 83. | Spector TD, Dacre JE, Harris PA, Huskisson EC. Radiological progression of osteoarthritis: an 11 year follow up study of the knee. Ann Rheum Dis. 1992;51:1107-1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 103] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 84. | Szebenyi B, Hollander AP, Dieppe P, Quilty B, Duddy J, Clarke S, Kirwan JR. Associations between pain, function, and radiographic features in osteoarthritis of the knee. Arthritis Rheum. 2006;54:230-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 161] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 85. | Günther KP, Sun Y. Reliability of radiographic assessment in hip and knee osteoarthritis. Osteoarthritis Cartilage. 1999;7:239-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 79] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 86. | McAlindon TE, Felson DT, Zhang Y, Hannan MT, Aliabadi P, Weissman B, Rush D, Wilson PW, Jacques P. Relation of dietary intake and serum levels of vitamin D to progression of osteoarthritis of the knee among participants in the Framingham Study. Ann Intern Med. 1996;125:353-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 263] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 87. | Shamir L, Ling SM, Scott WW, Bos A, Orlov N, Macura TJ, Eckley DM, Ferrucci L, Goldberg IG. Knee x-ray image analysis method for automated detection of osteoarthritis. IEEE Trans Biomed Eng. 2009;56:407-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 163] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 88. | Harada Y, Tokuda O, Fukuda K, Shiraishi G, Motomura T, Kimura M, Matsunaga N. Relationship between cartilage volume using MRI and Kellgren-Lawrence radiographic score in knee osteoarthritis with and without meniscal tears. AJR Am J Roentgenol. 2011;196:W298-W304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 89. | Kijowski R, Blankenbaker D, Stanton P, Fine J, De Smet A. Arthroscopic validation of radiographic grading scales of osteoarthritis of the tibiofemoral joint. AJR Am J Roentgenol. 2006;187:794-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 105] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 90. | Wada M, Baba H, Imura S, Morita A, Kusaka Y. Relationship between radiographic classification and arthroscopic findings of articular cartilage lesions in osteoarthritis of the knee. Clin Exp Rheumatol. 1998;16:15-20. [PubMed] |
| 91. | Galli M, De Santis V, Tafuro L. Reliability of the Ahlbäck classification of knee osteoarthritis. Osteoarthritis Cartilage. 2003;11:580-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 59] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 92. | Ahlbäck S, Rydberg J. [X-ray classification and examination technics in gonarthrosis]. Lakartidningen. 1980;77:2091-2093, 2096. [PubMed] |
| 93. | Weidow J, Cederlund CG, Ranstam J, Kärrholm J. Ahlbäck grading of osteoarthritis of the knee: poor reproducibility and validity based on visual inspection of the joint. Acta Orthop. 2006;77:262-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 94. | Dieppe PA, Reichenbach S, Williams S, Gregg P, Watt I, Jüni P. Assessing bone loss on radiographs of the knee in osteoarthritis: a cross-sectional study. Arthritis Rheum. 2005;52:3536-3541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 95. | Choy WS, Lee SK, Kim KJ, Kam BS, Yang DS, Bae KW. Two continuous femoral nerve block strategies after TKA. Knee Surg Sports Traumatol Arthrosc. 2011;19:1901-1908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 96. | Kannus P, Järvinen M, Paakkala T. A radiological scoring scale for evaluation of post-traumatic osteoarthritis after knee ligament injuries. Int Orthop. 1988;12:291-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 97. | Satku K, Kumar VP, Ngoi SS. Anterior cruciate ligament injuries. To counsel or to operate? J Bone Joint Surg Br. 1986;68:458-461. [PubMed] |
| 98. | Merchant TC, Dietz FR. Long-term follow-up after fractures of the tibial and fibular shafts. J Bone Joint Surg Am. 1989;71:599-606. [PubMed] |
| 99. | McAlindon TE, Cooper C, Kirwan JR, Dieppe PA. Determinants of disability in osteoarthritis of the knee. Ann Rheum Dis. 1993;52:258-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 362] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 100. | Derek T, Cooke TDV, Kelly BP, Harrison L, Mohamed G, Khan B. Radiographic grading for knee osteoarthritis. A revised scheme that relates to alignment and deformity. J Rheumatol. 1999;26:641-644. [PubMed] |
| 101. | Felson DT, McAlindon TE, Anderson JJ, Naimark A, Weissman BW, Aliabadi P, Evans S, Levy D, LaValley MP. Defining radiographic osteoarthritis for the whole knee. Osteoarthritis Cartilage. 1997;5:241-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 124] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 102. | Michael JW, Wurth A, Eysel P, König DP. Long-term results after operative treatment of osteochondritis dissecans of the knee joint-30 year results. Int Orthop. 2008;32:217-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 103. | Lynn SK, Costigan PA. Effect of foot rotation on knee kinetics and hamstring activation in older adults with and without signs of knee osteoarthritis. Clin Biomech (Bristol, Avon). 2008;23:779-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 104. | Harrison M, Hopman W, Hope J, Brean M. Development of a novel triage tool for knee surgery. Osteoarthritis Cartilage. 2013;21:S140. |
| 105. | Cooper C, Cushnaghan J, Kirwan JR, Dieppe PA, Rogers J, McAlindon T, McCrae F. Radiographic assessment of the knee joint in osteoarthritis. Ann Rheum Dis. 1992;51:80-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 58] [Reference Citation Analysis (0)] |
| 106. | Hellio Le Graverand MP, Mazzuca S, Duryea J, Brett A. Radiographic grading and measurement of joint space width in osteoarthritis. Rheum Dis Clin North Am. 2009;35:485-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 107. | Nagaosa Y, Mateus M, Hassan B, Lanyon P, Doherty M. Development of a logically devised line drawing atlas for grading of knee osteoarthritis. Ann Rheum Dis. 2000;59:587-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 69] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 108. | Neumann G, Hunter D, Nevitt M, Chibnik LB, Kwoh K, Chen H, Harris T, Satterfield S, Duryea J. Location specific radiographic joint space width for osteoarthritis progression. Osteoarthritis Cartilage. 2009;17:761-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 109. | Spector T, Cooper C, Cushnighan J, Hart DJ, Dieppe PA. A radiographic atlas of knee osteoarthritis. London: Springer Verlag 1992; . |
| 110. | Thomas RH, Resnick D, Alazraki NP, Daniel D, Greenfield R. Compartmental evaluation of osteoarthritis of the knee. A comparative study of available diagnostic modalities. Radiology. 1975;116:585-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 114] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 111. | Altman RD, Hochberg M, Murphy WA, Wolfe F, Lequesne M. Atlas of individual radiographic features in osteoarthritis. Osteoarthritis Cartilage. 1995;3 Suppl A:3-70. [PubMed] |
| 112. | Altman RD, Gold GE. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthritis Cartilage. 2007;15 Suppl A:A1-56. [PubMed] |
| 113. | Boegård T, Rudling O, Petersson IF, Jonsson K. Correlation between radiographically diagnosed osteophytes and magnetic resonance detected cartilage defects in the tibiofemoral joint. Ann Rheum Dis. 1998;57:401-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 95] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 114. | Lanyon P, O’Reilly S, Jones A, Doherty M. Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis. 1998;57:595-601. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 135] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 115. | Kijowski R, Blankenbaker DG, Stanton PT, Fine JP, De Smet AA. Radiographic findings of osteoarthritis versus arthroscopic findings of articular cartilage degeneration in the tibiofemoral joint. Radiology. 2006;239:818-824. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 69] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 116. | Braga L, Renner JB, Schwartz TA, Woodard J, Helmick CG, Hochberg MC, Jordan JM. Differences in radiographic features of knee osteoarthritis in African-Americans and Caucasians: the Johnston county osteoarthritis project. Osteoarthritis Cartilage. 2009;17:1554-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 57] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 117. | O’Reilly SC, Muir KR, Doherty M. Effectiveness of home exercise on pain and disability from osteoarthritis of the knee: a randomised controlled trial. Ann Rheum Dis. 1999;58:15-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 275] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 118. | Cicuttini FM, Baker J, Hart DJ, Spector TD. Association of pain with radiological changes in different compartments and views of the knee joint. Osteoarthritis Cartilage. 1996;4:143-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 137] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 119. | Hurley ST, Hatfield Murdock GL, Stanish WD, Hubley-Kozey CL. Is there a dose response for valgus unloader brace usage on knee pain, function, and muscle strength? Arch Phys Med Rehabil. 2012;93:496-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 120. | Lynn SK, Reid SM, Costigan PA. The influence of gait pattern on signs of knee osteoarthritis in older adults over a 5-11 year follow-up period: a case study analysis. Knee. 2007;14:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 121. | Lethbridge-Cejku M, Scott WW, Reichle R, Ettinger WH, Zonderman A, Costa P, Plato CC, Tobin JD, Hochberg MC. Association of radiographic features of osteoarthritis of the knee with knee pain: data from the Baltimore Longitudinal Study of Aging. Arthritis Care Res. 1995;8:182-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 116] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 122. | Hubley-Kozey CL, Hatfield GL, Astephen Wilson JL, Dunbar MJ. Alterations in neuromuscular patterns between pre and one-year post-total knee arthroplasty. Clin Biomech (Bristol, Avon). 2010;25:995-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 123. | Kerna I, Kisand K, Laitinen P, Tamm AE, Kumm J, Lintrop M, Tamm AO. Association of ADAM12-S protein with radiographic features of knee osteoarthritis and bone and cartilage markers. Rheumatol Int. 2012;32:519-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 124. | Jenkinson CM, Doherty M, Avery AJ, Read A, Taylor MA, Sach TH, Silcocks P, Muir KR. Effects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trial. BMJ. 2009;339:b3170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 125. | Wilkinson CE, Neame R, Prabu A, Carr AJ, Doherty M. Further development of a logically dervided line drawing atlas (LDLDA) for grading knee osteoarthritis (OA). Arthritis Rheum. 2001;44:S227. |
| 126. | Wilkinson CE, Carr AJ, Doherty M. Does increasing the grades of the knee osteoarthritis line drawing atlas alter its clinimetric properties? Ann Rheum Dis. 2005;64:1467-1473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 127. | Wilkinson CE, Carr AJ, Doherty M. Does grading improve by overlaying an acetate line drawing atlas directly over a radiograph? Rheumatology. 2004;43 Suppl 2:65. |
| 128. | Marijnissen AC, Vincken KL, Vos PA, Saris DB, Viergever MA, Bijlsma JW, Bartels LW, Lafeber FP. Knee Images Digital Analysis (KIDA): a novel method to quantify individual radiographic features of knee osteoarthritis in detail. Osteoarthritis Cartilage. 2008;16:234-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 91] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 129. | Kinds MB, Marijnissen AC, Vincken KL, Viergever MA, Drossaers-Bakker KW, Bijlsma JW, Bierma-Zeinstra SM, Welsing PM, Lafeber FP. Evaluation of separate quantitative radiographic features adds to the prediction of incident radiographic osteoarthritis in individuals with recent onset of knee pain: 5-year follow-up in the CHECK cohort. Osteoarthritis Cartilage. 2012;20:548-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 130. | Kinds MB, Vincken KL, Hoppinga TN, Bleys RL, Viergever MA, Marijnissen AC, Welsing PM, Lafeber FP. Influence of variation in semiflexed knee positioning during image acquisition on separate quantitative radiographic parameters of osteoarthritis, measured by Knee Images Digital Analysis. Osteoarthritis Cartilage. 2012;20:997-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 131. | Muraki S, Oka H, Akune T, En-yo Y, Yoshida M, Suzuki T, Yoshida H, Ishibashi H, Tokimura F, Yamamoto S. Independent association of joint space narrowing and osteophyte formation at the knee with health-related quality of life in Japan: a cross-sectional study. Arthritis Rheum. 2011;63:3859-3864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 132. | Muraki S, Oka H, Akune T, En-yo Y, Yoshida M, Nakamura K, Kawaguchi H, Yoshimura N. Association of occupational activity with joint space narrowing and osteophytosis in the medial compartment of the knee: the ROAD study (OAC5914R2). Osteoarthritis Cartilage. 2011;19:840-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 133. | Sheehy L, Cooke TDV, McLean L, Niu J, Lynch J, Segal NA, Singh J, Culham E. Reliability of the uni-compartmental scale for the radiographic evaluation of knee osteoarthritis: Data from the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2013;21 Suppl:S201. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |