Published online Nov 19, 2019. doi: 10.5498/wjp.v9.i7.99
Peer-review started: May 27, 2019
First decision: August 2, 2019
Revised: August 16, 2019
Accepted: October 14, 2019
Article in press: October 14, 2019
Published online: November 19, 2019
Processing time: 179 Days and 4.9 Hours
Treatment for offenders with mental disorders is a key concern in public mental health. Provision of adequate psychiatric treatment is important for the offender and their community. An approach used in Japan to address this issue is administrative involuntary hospitalization. Under this scheme, a person at risk for harming themselves or others because of a mental disorder can be involuntarily hospitalized in a designated psychiatric hospital. However, this scheme does not include tracking of these patients after discharge. Although some data for administrative involuntary hospitalizations are available, it remains unclear what happens to these patients after discharge.
To evaluate follow-up of patients under administrative involuntary hospitalization after discharge and obtain data for later comparisons with outcomes.
We used a retrospective design and conducted a national survey of administrative involuntary hospitalizations. Questionnaires were distributed to 939 facilities across Japan. The questionnaire collected data for selected involuntary hospitalization cases in the hospital on June 30, 2010 (census date), and the prognoses of each patient on a specified date in 2011 and 2012. We also asked about the treatment provided to each patient. We stratified patients by prognosis (good or poor), and used logistic regression analysis to examine the relationship between treatment and prognosis.
We received completed questionnaires from 292 facilities (response rate 31.1%); 105 facilities had no relevant patients. Our analysis included data for 394 patients with valid data. Official statistics indicated 1503 patients were under administrative involuntary hospitalization as at June 30, 2012, meaning the capture rate was 27.2%. Approximately a fourth (104/394) at 1 year, and a third (137/294) at 2 years after the census had unknown prognosis. Treatment content included multi-disciplinary team meetings (78.2% of patients), counseling by public workers (59.9%), and discussion with external specialists (32.5%). Overall, 116 patients were categorized as having a good prognosis at 1 year, and 168 had a poor prognosis. At the 2-year point, 102 patients had a good prognosis and 150 had a poor prognosis. “Discussion with external specialists” was positively associated with a good prognosis at both 1 year (P = 0.016) and 2 years (P = 0.036).
We found that facilities in Japan currently have limited ability to track the prognoses of patients who were hospitalized involuntarily. Discussion with external specialists is associated with a good prognosis.
Core tip: In Japan, involuntary hospitalization by the prefectural governor’s order is applied to psychiatric patients with risks for harming themselves or others. A certain amount of them cannot be followed up the practitioners. Good prognosis can be associated with discussion with external specialist before discharge.
- Citation: Shiina A, Sato A, Iyo M, Fujii C. Outcomes of administrative involuntary hospitalization: A national retrospective cohort study in Japan. World J Psychiatr 2019; 9(7): 99-106
- URL: https://www.wjgnet.com/2220-3206/full/v9/i7/99.htm
- DOI: https://dx.doi.org/10.5498/wjp.v9.i7.99
How offenders with mental disorders should be treated is a concern for the general public and for forensic mental health specialists[1,2]. In the case of offenses directly driven by psychiatric symptoms, it is doubtful if legally punishing the offender effectively prevents recidivism. Rather, proper psychiatric treatment should be provided for the offender and the community in which they will be reintegrated[3].
Japan has two different schemes that address this issue. First, an administrative involuntary hospitalization scheme was established in 1950. This scheme has been succeeded by the Mental Health and Welfare Act (amended in 2013), without any major alteration. Under this scheme, if a person is recognized to be at risk for harming themselves or others because of a mental disorder, the police and prosecutor report the case to the prefectural governor. The governor can then order the person to be hospitalized in a designated psychiatric hospital, based on an assessment by two designated psychiatrists that involuntary hospitalization is necessary. On the other hand, there are scarce legislation regarding the content of treatment under the involuntary hospitalization by the prefectural governor’s order. According to a local survey we conducted before, considerable proportion of psychiatrists believe that qualified treatment, such as electro convulsive therapy, long acting injection of antipsychotic drugs, use of clozapine, confrontation of the offense, and home nursing before discharge, are beneficial for many patients. In reality, however, clozapine is rarely used to such patients mainly because of the issue of informed consent[4].
Second, when a person has committed a serious crime (e.g., murder or arson) and is deemed to be in a state of insanity or diminished responsibility at the time of the offense, the prosecutor makes an allegation to the court. If the court panel (comprising a judge and a psychiatrist) agree, the person is sent to a special hospital according to the Medical Treatment and Supervision Act. This legislation was enacted 14 years ago[5], and has frequently been discussed by forensic mental health researchers and policy makers. Confrontation to their offense and prevention of recidivism are included in standard care program in this scheme. As well, the process about gaining the consent to treatment from inpatient is described in the guidelines. Hundreds of patients are subject to this scheme, many of whom can be discharged into society without reoffending[5]. People subject to the Medical Treatment and Supervision Act are under supervision by the probation office, and their prognoses are statistically clarified. According to an official government report, of the 2247 patients who were permitted to be discharged by the court panel up to 2017, only 1.8% committed further serious crimes[6].
In contrast, the administrative involuntary hospitalization scheme has not been modified since the Medical Treatment and Supervision Act came into force. Therefore, the main people subject to the administrative involuntary hospitalization scheme are those who have committed relatively non-serious crimes under the dominant influence of mental disorders. The court is not involved in decision-making regarding their admission or discharge. In addition, there is no way to track the prognosis of patients discharged from a designated hospital. According to a government report, 753 patients were hospitalized by order of the prefectural governor in June 2015 nationwide; of these, 45 patients remained under administrative involuntary hospitalization after 1 year[7]. However, it was unclear where discharged patients went.
Many practitioners are concerned about the incomplete follow-up of patients who were hospitalized by prefectural government order. To date, some researchers have reported statistical data regarding administrative involuntary hospitalization. For example, the corresponding author conducted a local survey in 2011 to clarify the clinical prognosis of patients who had been hospitalized under this scheme[4]. The results showed that many cases could not be followed up after discharge. Some practitioners suggested a new tracking system to follow patients was needed, similar to that used for the Medical Treatment and Supervision Act, especially because these patients tend to withdraw from medical treatment[8].
On July 26, 2016, an ex-employee intruded a residence for people with disabilities and killed 19 residents; this act was motivated by his prejudiced ideology[9]. This incident was considered the worst massacre committed by an offender in Japan since World War II. Public attention about the forensic mental health system was ignited after it was revealed that this person had been ordered to be involuntarily hospitalized by the prefectural governor a few months before the case occurred, as well as the fact that he was cannabis abuser.
The government submitted a bill for amendment of the Mental Health and Welfare Act following the publication of a report by the special team that examined the incident[10]. The amended bill contained a new scheme covering official follow-up of ex-inpatients who had been under administrative involuntary hospitalization. However, this bill was criticized by politicians and lawyers who were concerned about the risk for unnecessary censoring of patients. As the Prime Minister dissolved the Diet (Lower House) in 2017 because of political conflict not relevant to this issue, the bill remained unapproved[11]. Instead, the Japan Ministry of Health, Labour and Welfare published guidelines based on a similar scheme to strengthen support for patients with mental disorders after discharge. The corresponding author was involved in developing these guidelines[12,13].
Reform of administrative involuntary hospitalization is expected to improve the quality of medical treatment for offenders with mental disorders. A key indicator of functional execution of this scheme will be the follow-up rate of patients, because many criminal acts are committed by psychiatric patients who have quit or received insufficient psychiatric treatment[4]. Therefore, we conducted a national survey to evaluate the current quality of administrative involuntary hospitalization, with the intention of providing data for later comparison with outcomes.
This study aimed to examine the extent to which mental health service providers could track the prognoses of ex-inpatients who had been hospitalized under order of the prefectural governor, and examine the content of the medical treatment they actually received. The data collected in this study are expected to be compared with data gathered in a further study.
The target population for this study was all psychiatric hospitals that accepted patients who were hospitalized by order of the prefectural governor. They included public psychiatric hospitals and designated psychiatric hospitals administered by the private sector. We listed these hospitals based on official reports, and included the 939 facilities that accept administrative involuntary hospitalization as the study sample.
We sent a questionnaire to the administrators of each hospital, and asked them to complete and return the form by mail. We gathered data for patients staying in the hospital on June 30, 2010 (census date) by order of the prefectural governor. If there were over five eligible patients, we collected data for only five patients to avoid placing too much burden on the hospital administrators. Questionnaire items included the prognoses of each patient on a specific day (June 30) in 2011 and 2012. We also asked about the content of treatment provided to each patient. Detail of the questionnaire is shown in the Supplementary document.
To investigate the association between the content of services provided to each patient and their medical prognosis, we first stratified the data for prognoses. We classified patients who had regularly visited an outpatient unit (at either the hospital of admission or another hospital) as a “good” prognosis because withdrawal from regulatory visiting hospital is known as a major risk factor of relapse for many psychiatric patients. Patients who had stayed at any hospital or who were deceased were deemed as having a “poor” prognosis. Other patients, including those with an unknown prognosis were excluded from further analyses. Specific answers describing the patient’s prognosis were classified as either good (e.g., staying at a health center for older adults, occasional telephone consultation with a hospital, or treatment completion) or poor (e.g., escaped from hospital, accidental withdrawal from outpatient treatment, arrested, detained, or incarcerated).
Next, we used logistic regression analysis to examine the impact of the treatment provided to patients during hospitalization on their prognosis, as an exploratory analysis. We set the binary value “prognosis” (as defined above) as the dependent variable. Independent variables were: “multi-disciplinary team meeting while admitted,” “counseling by public workers while admitted,” “discussion with persons other than the psychiatrist in charge before dismissal of the prefectural governor’s order,” and “discussion with specialists external to the hospital before dismissal of the prefectural governor’s order.” We used stepwise logistic regression analysis with increasing variables. Statistical analyses were performed using SPSS for Windows, Version 24 (IBM Corp., Armonk, NY, United States). The level of significance was set at P < 0.05.
Because this study did not include any intervention with patients, there was no possible harm to patients. All data gathered in this study were those previously obtained by the participating psychiatric hospitals. In addition, we did not gather any personal information pertaining to patients. The study protocol was approved by the Ethics Committee of the Graduate School of Medicine at Chiba University on June 6, 2016 (no. 237). We registered this study with the Clinical Trials Registry of the University Hospital Medical Information Network (UMIN, Tokyo, Japan), with the unique trial number UMIN000027318.
We sent questionnaire forms to 939 facilities; 292 facilities returned a completed form, giving a response rate of 31.1%. Of these, 105 facilities had no applicable patients. One patient was reported in 187 facilities, two in 95 facilities, three in 57 facilities, four in 40 facilities, and five or more in 30 facilities. Therefore, we gathered data for 409 patients. An official report indicated that 1503 patients were hospitalized under order of a prefectural governor as at June 30, 2012[6], meaning the capture rate was 27.2%.
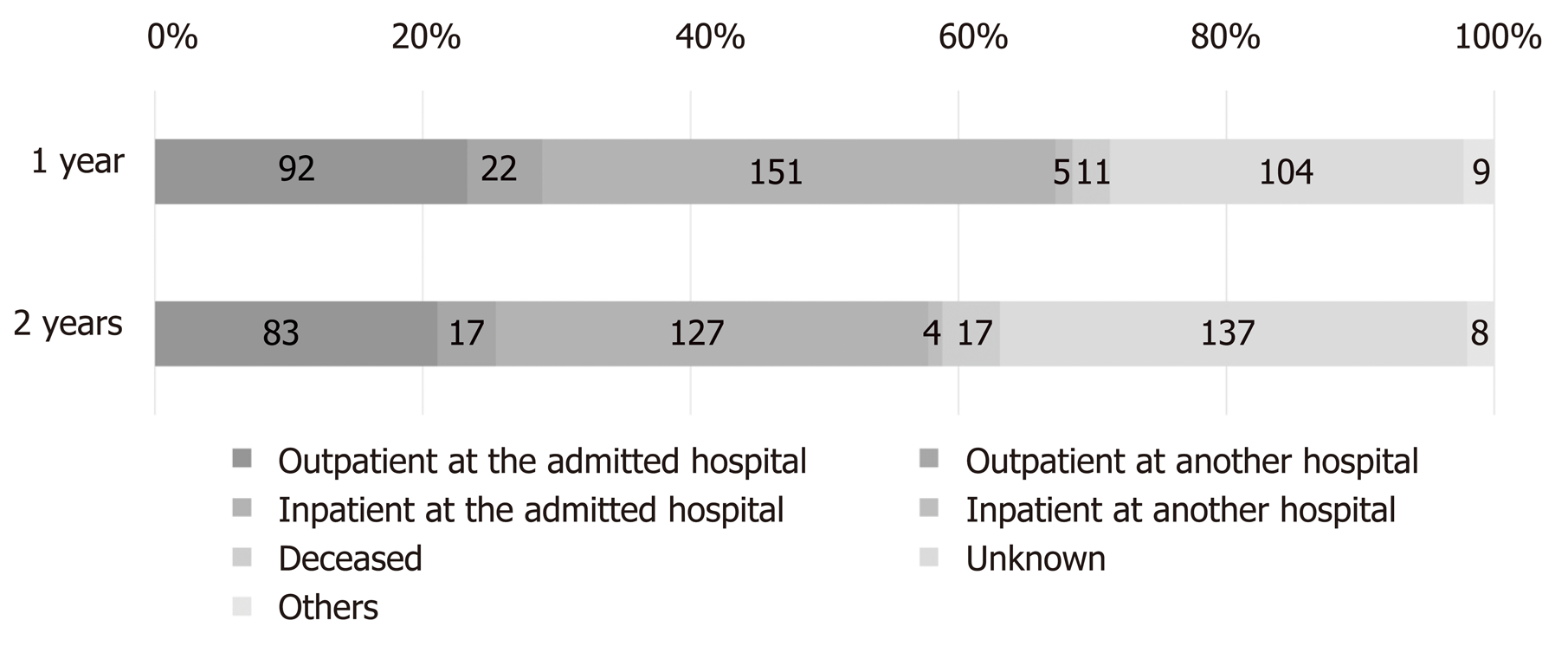
Fifteen of the 409 patients had invalid information. Of the remaining 394 patients, 151 (38.3%) had stayed at the hospital of admission, 92 (23.4%) had regularly visited an outpatient unit at the hospital of admission, five (1.3%) had stayed at another hospital, 22 (5.6%) had regularly visited an outpatient unit at another hospital, and 11 (2.8%) were deceased. In addition, 104 (26.4%) had an unknown prognosis, and nine (2.3%) had a prognosis other than those listed above at 1 year after the census.
We also examined the 2-year prognosis. Of the 294 patients, 127 (32.3%) had stayed at the hospital of admission, 83 (21.1%) had regularly visited an outpatient unit at the hospital of admission, four (1.0%) had stayed at another hospital, 17 (4.3%) had regularly visited an outpatient unit at another hospital, and 17 (4.3%) were deceased. The 2-year prognosis was unknown for 137 (34.9%) patients, and eight (2.0%) had a prognosis other than those listed above; of these, two were recorded as having been arrested or incarcerated. A summary of patients’ prognosis at 1 and 2 years after the starting point is shown in Figure 1.
Regarding living conditions after discharge, 147 (36.0%) patients were living with family members, 77 (18.9%) were single, and 51 (12.5%) were in a facility. In addition, 95 (23.3%) were still in a hospital and 31 (7.6%) had moved hospitals. We requested information about a key person at discharge for all sampled patients. A family member was suggested as the key person for 293 (72.0%) patients. For nine (2.2%) patients, a person other than a family member was deemed the most suitable key person. In 32 (7.9%) cases, professionals took the role of key person for the patient. Forty-one patients had no particular key persons identified.
The responses from the participating hospitals indicated that multi-disciplinary team meetings were conducted for 319 (78.2%) patients. Counseling delivered by public workers was conducted for 243 (59.9%) patients. In 222 (56.3%) cases, discussions with persons other than the psychiatrist in charge were held before dismissal of the prefectural governor’s order. However, discussion with specialists external to the hospital was only conducted in 127 (32.5%) cases.
After discharge, 58 (16.9%) patients received a nurse visit service. Day- or night-care after discharge was implemented for 35 (10.2%) patients. Outpatient care services for daily life in the community were reported for 44 (12.9%) patients, and residential care services were implemented for 30 (8.8%) patients.
Regarding collaboration with other facilities/agencies, 249 (63.7%) cases had some collaboration with the prefectural government after discharge. In 102 (26.1%) cases, other hospitals were involved in the patients’ care after discharge. Public nursing centers were involved in 42 (10.8%) cases. Police concern after discharge was reported in 54 (13.8%) cases, but only two (0.5%) cases had contact with drug control offices after discharge. Involvement of other service providers was reported for 71 (18.2%) patients.
According to the criteria defined in the Methods section, 116 patients (29.4%) were categorized as having a good prognosis at 1 year, and the remaining 168 (42.6%) had a poor prognosis. In addition, 102 patients (25.9%) had a good 2-year prognosis and 150 (38.1%) had a poor prognosis.
The logistic regression analysis suggested that only “discussion with specialists external to the hospital before dismissal of the prefectural governor’s order” was positively associated with a good prognosis at both 1 year [B = 0.020, standard error (SE) = 0.008, Wald = 5.766, df = 1, P = 0.016, Exp(B) = 1.020] and 2 years (B = 0.015, SE = 0.007, Wald = 4.387, df = 1, P = 0.036, Exp(B) = 1.015) after the census.
In this national survey, we examined whether psychiatric facilities accepting administrative involuntary hospitalizations could track the prognosis of patients after discharge. We also examined the services that were provided to support patients’ mental health in the community. The results clarified that facilities did not know the prognoses of approximately one-fourth of these patients within 1 year, and one-third within 2 years. The overall results were consistent with those of a local survey previously conducted by the corresponding author[4]. The response rate of this study was 31.1%. Considering that implementation of this survey relied on voluntary cooperation of each hospital, this response rate is acceptable.
This result should be cautiously interpreted because “unknown” prognoses do not necessarily mean undesirable treatment outcomes. For example, some facilities mainly providing psychiatric emergency care transfer patients in the early stage of inpatient treatment to another hospital that is located near to each patient’s hometown. In these cases, the facility accepting the patient may not initially know the patients’ prognosis. Therefore, hospitals providing qualified psychiatric emergency services rarely track each patient’s prognosis. It is therefore possible that many patients whose prognosis is not clarified lived without trouble in the community independently from the hospital in which they received inpatient care.
We excluded patients with an unknown prognosis from further analysis to examine the association between treatment and prognosis. Because these patients were involuntarily hospitalized to receive treatment for mental disorders, continuous treatment should be important to maintain their mental health, even after dismissal of the order. We considered patients who had regularly visited an outpatient clinic as having a good prognosis. In contrast, longitudinal hospitalization or death was considered proof of a poor prognosis. In addition, unexpected withdrawal from outpatient treatment may predict the relapse of psychiatric illness.
The logistic regression analysis suggested that discussion with specialists who were external to the hospital in which the patient was admitted was associated with a good prognosis 1 and 2 years after the census point. In Japan, there is no official scheme of collaborative discussion with external specialists in psychiatric treatment. Some medical practitioners are willing to consult with external specialists spontaneously. The concrete content of discussion with specialists was not clarified in this survey. In general, consultation with specialists outside the hospital is time consuming and costly. Thus, in cases where such consultation was performed, the patient and practitioners surely discussed deeply whether the patient could adapt to life in the community. In some cases, discharge plan might be rearranged after the discussion. We believe delicate and sincere consideration for community treatment among supporters may have a positive impact of the outcome of discharged patients. In the future, it may be beneficial that collaborative discussion with external specialists is conducted more frequently especially in complicated cases.
The present study suggested that 4.3% of patients admitted under administrative involuntary hospitalization were deceased within 2 years. Even considering the poor mortality rate among patients with mental disorders[14], this percentage seems to be high, especially as the crude death rate of forensic patients was estimated as 0.325% per year in a meta-analytical review of international datasets[15]. When a person commits suicide, the police usually contact hospitals that might have been connected with that person. Therefore, psychiatric hospitals are usually aware when an ex-patient is deceased by suicide. In this study, it is unlikely that cases of suicide were included among those with unknown prognosis. Psychiatric patients also have higher risk for physical illnesses than healthy controls[16]. We did not ask the reason for death in each deceased case. Further investigation is needed to draw any conclusions regarding this point.
Overall, it was difficult to evaluate the effectiveness of the current system of administrative involuntary hospitalization by order of the prefectural governor. There are several outcome measures in forensic mental health, none of which have been decisively approved[17]. For example, Edwards et al[18] investigated the outcomes of patients admitted to a medium secure unit in England; the mean duration of admission was 26 mo, and approximately 10% of the patients were convicted of another offence within 2 years. Compared with this result, the outcomes in the present study appear to be better, with few patients reported to have been arrested and at least one-fourth of the patients had regularly visited an outpatient clinic over 2 years. However, the characteristics of the patients in this study may differ from those of other studies because administrative involuntary hospitalization orders in Japan do not cover patients who have committed serious crimes. Therefore, the present study could not definitively evaluate the quality of care in the current situation in Japan. However, we will be able to examine whether the quality of care improves by comparing the present result with data gathered in the next few years.
The present study is a retrospective survey using the existing data in each participating hospital. Therefore, there are limitations to derive some conclusions from the results. Each patient’s past medical history was not included into analysis. Sampling biases could not be avoided. A prospective cohort with larger and non-biased sampling is necessary to confirm the finding of this study.
In conclusion, we investigated the prognoses of patients under administrative involuntary hospitalization. At 2 years after the census, one-third of the patients had stayed at the ordered psychiatric hospital, one-fourth had regularly visited an outpatient clinic, and one-third had an uncertain prognosis. Discussion with specialists external to the admitting hospital was associated with a good prognosis. These results should be considered as a standard when the system of hospitalization by the prefectural governor’s order is amended.
In Japan, patients with mental disorder having a risk for harming self or others are hospitalized by the prefectural governor’s order.
We have to know the outcome of patients who were hospitalized involuntarily.
To clarify the performance and outcome of the scheme of involuntary hospitalization by the prefectural governor’s order.
Retrospective cohort by examining medical record of hospitals accepting involuntary hospitalization.
A total of 394 subjects were examined. Approximately a fourth at 1 year, and a third at 2 years after the census had unknown prognosis. Approximately a third was identified as good prognosis. Discussion with external specialists before discharge were associated with good prognosis.
Psychiatric hospitals in Japan have limited ability to track the prognoses of patients who were hospitalized involuntarily by the prefectural governor’s order.
Constructive discussion with external specialists before discharge is possible to improve the outcome of the patients with mental disorder. To confirm this hypothesis, a prospective cohort study is necessary.
Manuscript source: Unsolicited manuscript
Specialty type: Psychiatry
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ng QX, Seeman MV, Wang YP S-Editor: Yan JP L-Editor: A E-Editor: Zhang YL
| 1. | Mullen PE. Forensic mental health. Br J Psychiatry. 2000;176:307-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 48] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Ogloff JR, Roesch R, Eaves D. International perspective on forensic mental health systems. Int J Law Psychiatry. 2000;23:429-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Allnutt S, Samuels A, O'driscoll C. The insanity defence: from wild beasts to M'Naghten. Australas Psychiatry. 2007;15:292-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Shiina A, Iyo M, Yoshizumi A, Hirabayashi N. Involuntary hospitalization for offenders with mental disorders in Japan. Proceedings of the 8th European Congress on violence in clinical psychiatry. 2013 Oct 23-26; Gent, Belgium; 2013: 377-380. |
| 5. | Fujii C, Fukuda Y, Ando K, Kikuchi A, Okada T. Development of forensic mental health services in Japan: working towards the reintegration of offenders with mental disorders. Int J Ment Health Syst. 2014;8:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Ministry of Health, Labour and Welfare. The current situation of Medical Treatment and Supervision Act. Available from: https://www.mhlw.go.jp/file/05-Shingikai-12201000-Shakaiengokyokushougaihokenfukushibu-Kikakuka/shiryou2_15.pdf [in Japanese]. |
| 7. | Ministry of Health, Labour and Welfare. The data of mental health and welfare in Japan. 2016. Available from: https://www.ncnp.go.jp/nimh/keikakuold/old/archive/vision/data.html [in Japanese]. |
| 8. | Shiina A, Iyo M, Yoshizumi A, Hirabayashi N. Recognition of change in the reform of forensic mental health by clinical practitioners: a questionnaire survey in Japan. Ann Gen Psychiatry. 2014;13:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Asahi Digital. “Watashi ha kyuseishu” “Nihon no tame” Yogisha kyojutsu Sagamihara sassho. [“I am Messiah” “For Japan” says the suspect of Sagamihara case.]. Available from: http://web.archive.org/web/20170623150601/http://www.asahi.com/articles/ASJ8K2JC3J8KULOB001.html [in Japanese]. |
| 10. | Ministry of Health, Labour and Welfare. The official report of the team for evaluation and recurrence prevention of the Sagamihara residence case. 2016; Available from: http://www.mhlw.go.jp/stf/shingi2/0000145268.html [in Japanese]. |
| 11. | Sagamihara mass murder spotlights support measures after compulsory hospitalization. Available from: https://mainichi.jp/english/articles/20180725/p2a/00m/0na/015000c. |
| 12. | Ministry of Health, Labour and Welfare. The guideline of administrative involuntary hospitalization. [published on 2018 March 27]. Available from: http://www.m.chiba-u.ac.jp/class/shakai/jp/syakaifukki/doc/02.pdf [in Japanese]. |
| 13. | Ministry of Health, Labour and Welfare. The guideline of supporting patients with mental disorders after discharge by municipalities. [published on 2018 March 27]. Available from: http://www.m.chiba-u.ac.jp/class/shakai/jp/syakaifukki/doc/04.pdf [in Japanese]. |
| 14. | Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry. 2015;72:334-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1534] [Cited by in RCA: 1943] [Article Influence: 194.3] [Reference Citation Analysis (0)] |
| 15. | Fazel S, Fimińska Z, Cocks C, Coid J. Patient outcomes following discharge from secure psychiatric hospitals: systematic review and meta-analysis. Br J Psychiatry. 2016;208:17-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 126] [Cited by in RCA: 71] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 16. | DE Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, Detraux J, Gautam S, Möller HJ, Ndetei DM, Newcomer JW, Uwakwe R, Leucht S. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10:52-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1508] [Cited by in RCA: 1548] [Article Influence: 110.6] [Reference Citation Analysis (0)] |
| 17. | Chambers JC, Yiend J, Barrett B, Burns T, Doll H, Fazel S, Jenkinson C, Kaur A, Knapp M, Plugge E, Sutton L, Fitzpatrick R. Outcome measures used in forensic mental health research: a structured review. Crim Behav Ment Health. 2009;19:9-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Edwards J, Steed P, Murray K. Clinical and forensic outcome 2 years and 5 years after admission to a medium secure unit. J Forensic Psychiatry. 2002;13:68-87. [RCA] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 37] [Article Influence: 1.6] [Reference Citation Analysis (0)] |