Published online Sep 22, 2015. doi: 10.5498/wjp.v5.i3.315
Peer-review started: March 6, 2015
First decision: April 10, 2015
Revised: April 30, 2015
Accepted: August 4, 2015
Article in press: August 7, 2015
Published online: September 22, 2015
Processing time: 205 Days and 20.5 Hours
AIM: To summarize research regarding the motor abilities of children and adolescents who suffer from a common psychiatric condition.
METHODS: In order to outline the current knowledge regarding the motor abilities of children and adolescents with autism spectrum disorders (ASD), attention deficit hyperactivity disorder (ADHD), disruptive behavior disorders (DBD) and depression, a comprehensive systematic literature search was carried out using PubMed, Medline and ERIC databases. The databases were searched for relevant English language articles published between January 1990 and April 2014. Only studies that conducted a quantitative evaluation of motor ability and concerned individuals aged 0-18 years were included. A separate search was conducted for each disorder (ASD, ADHD, DBD, depression) in conjunction with each of the following keywords: (psycho/perceptuo) motor/movement skill(s), (psycho/perceptuo) motor/movement abilities, (psycho/perceptuo) motor/movement impairment, (psycho/perceptuo) motor/movement problem(s), motor function, motor coordination, motor performance, motor deficit(s). To detect supplementary relevant literature, the reference lists of the retrieved articles were examined.
RESULTS: The search strategy yielded 51 studies meeting the inclusion criteria. In total, 28 studies were included that examined the motor abilities of children and adolescents with ASD. All studies indicated that they performed below average on various standardized motor assessment instruments. The overall prevalence rate for impairment in motor abilities ranged from 33% to 100%. Twenty-seven studies examined the motor abilities of children and adolescents with ADHD. Depending on the type of motor assessment tool and the cut-off points used by different researchers, prevalence rates of impairment in motor abilities are highly variable and ranged from 8% to 73%. Remarkably, there is a paucity of research addressing the motor abilities of individuals with DBD or depression. Furthermore, methodological problems, such as measurement and comorbidity issues, complicate the generalization of the findings.
CONCLUSION: Research suggests that motor impairment is highly prevalent in some psychiatric conditions, particularly ASD and ADHD. However, future work is necessary to draw sound conclusions.
Core tip: This systematic review provides a comprehensive overview of current available research regarding the motor abilities of children and adolescents with autism spectrum disorders, disruptive behavior disorders, attention deficit hyperactivity disorder and depression. Although motor impairment is not considered to be a major diagnostic feature of any of these psychiatric conditions, the motor ability literature disputes the fact that these individuals possess normal motor abilities. However, future work is necessary to draw sound conclusion. Based on a critical analysis of current evidence, recommendations for future research are proposed.
- Citation: Damme TV, Simons J, Sabbe B, West DV. Motor abilities of children and adolescents with a psychiatric condition: A systematic literature review. World J Psychiatr 2015; 5(3): 315-329
- URL: https://www.wjgnet.com/2220-3206/full/v5/i3/315.htm
- DOI: https://dx.doi.org/10.5498/wjp.v5.i3.315
Motor abilities are frequently affected in children and adolescents suffering from psychiatric conditions[1-3]. Although motor disorders can occur in isolation, many researchers have established that co-occurring motor problems are very common in pediatric mental health disorders, especially Autism Spectrum Disorders (ASD)[4-6] and Attention Deficit Hyperactivity Disorder (ADHD)[7,8].
A child’s development depends upon the continuous interaction of different functional areas, which can be described by motor, psychological, cognitive, linguistic and social aspects[9]. It is widely accepted that from early childhood through adolescence movement plays an essential role in several facets of children’s lives. A childhood, rich in play and varied motor activities, strengthens the foundations for other developmental domains and vice versa. Although motor abilities are particularly important when performing several activities of daily life (including getting dressed, writing, playing, sports, etc.), the relation between motor abilities and other developmental domains is not trivial. Presence of motor impairment can limit the social opportunities of children and can result in significant difficulties in academic life[10-12]. Moreover, several studies indicate that poor motor ability has far-reaching implications for psychosocial and emotional functioning[12-22]. Longitudinal research has demonstrated an increased risk of psychiatric disorders in children and adolescents with motor difficulties, particularly affective disorders such as anxiety and depression[17,18,23-25]. Furthermore, the association of motor impairment with ADHD seems to have a poor prognostic outcome[13,24], thus reflecting important clinical consequences.
In addition to being related to mental health issues, motor ability plays an important part in fitness and physical activity outcome[26,27]. Studies concerning the general population indicated that children with good motor skills are more likely to become fit adolescents[28] and maintain adequate fitness levels into adulthood[29]. Motor ability seems to be an important determinant of physical activity and physical fitness[30]. Due to the high prevalence of motor impairment in children with developmental and emotional disorders, these clinical populations are at risk of developing an inactive lifestyle[1,26]. Numerous studies have shown that children with motor impairment have lower fitness levels compared to their peers[27]. Emck et al[2] reported an association between certain combinations of impaired motor skills and physical fitness levels in children with different psychiatric conditions. Results from the study of Pan[31] showed that adolescents with ASD had significant lower levels of cardiovascular endurance, upper-body muscular strength and endurance and lower body flexibility is comparison to adolescents without ASD. On average, children suffering from developmental coordination disorder (DCD) are less physically active than others and report lower levels of participation in both free and organized active play. Moreover, it has been argued that, as a result, these children are at risk for obesity and poor health-related fitness in general, with potentially serious health consequences in later life[1,32].
Despite the fact that the specific impact of poor motor abilities on mental and physical health is no longer under-recognized, it is often assumed that children will grow out of their clumsiness. However, increasing evidence demonstrates that these problems remain relatively stable through adolescence and adulthood[11,21]. Therefore, it is essential that motor impairment is recognized and assessed. Early detection is a prerequisite for early intervention and perhaps this can lead to the prevention of secondary adverse outcomes of motor impairment, such as physical inactivity and academic difficulties.
Although consistent definitions of key terms are a necessity for discussing and understanding research concerning motor abilities, over the years a wide variety of terms have been used by various disciplines. For instance, terminologies like motor proficiency, motor coordination, motor skills, motor ability, movement problems, movement skills, etc., have been used. While important differences exist between these conceptualizations, they are not always clearly defined in research. Consequently, the variety in nomenclature can be somewhat misleading. In this review, the focus lies on motor abilities as defined by Burton et al[33]. In their taxonomy, motor abilities refer to a person’s potential movement competency. Motor abilities are not directly observable, but are derived from a set of movement tasks. Motor abilities measure the general traits or capacities that underlie performance of a wide variety of motor skills. For example, balance can be derived from a set of tasks, such as walking on a line, standing on a balance beam or standing on one leg.
The area of association between impairment in motor abilities and child psychiatric disorders is complex and appears to be, once again, attracting the attention of researchers in psychiatry. To date, several researchers[1,34-38] have published a review concerning motor problems in children with a psychiatric disorder. However, these reviews often seem to be confined to one psychiatric disorder or a specific motor skill. Moreover, a limited age range has often been applied. Because motor abilities may differ between childhood and adolescence, a completed picture across age groups is warranted. To our knowledge, the review of Emck et al[1], is the only one covering multiple disorders, but only studies concerning gross motor function in children were included. Due to the renewed interest and on-going debate in this field, we want to provide an update on the existing information. With regard to the psychiatric conditions outlined in this review, the approach of Emck et al[1] was followed. However, we extended upon this work by also including adolescents, differentiating between ADHD and behavioral disorders and including studies investigating both fine and gross motor ability.
In conclusion, the aim of this review is threefold. The first objective of the study is to summarize current research regarding the motor abilities of four common pediatric psychiatric disorders, more specifically ASD, ADHD, disruptive behavior disorders (DBD) and Depression. The second objective of the study is to outline the full spectrum of motor abilities, including both fine and gross motor skills in children as well as in adolescents. The final objective is to suggest further areas of research related to motor abilities in these populations.
A comprehensive, systematic literature search was carried out using PubMed, Education Resources Information Center (ERIC) and Medline databases on April 18, 2014. A separate search was conducted for each disorder (ASD, ADHD, DBD and depression) in conjunction with each of the following keywords: (psycho/perceptuo) motor/movement skill(s), (psycho/perceptuo) motor/movement abilities, (psycho/perceptuo) motor/movement impairment, (psycho/perceptuo) motor/movement problem(s), motor function, motor coordination, motor performance, motor deficit(s).
In order to locate every study that potentially could be relevant and to capture a rigorous set of articles, we decided to use this broad range of keywords. To detect additionally relevant studies, we examined the reference lists of the retrieved articles. The following inclusion criteria were predetermined: (1) the study included children or adolescents diagnosed with one or a combination of the following psychiatric disorders: ASD, ADHD, DBD and depression; (2) the article was published between January 1990 and April 17, 2014; (3) the study was published in an English peer-reviewed journal; and (4) the study involved a quantitative evaluation of motor abilities measured by a reliable standardized instrument. According to Burton et al[33], each motor assessment instrument “that produces composite or summary scores for groups of related movement tasks can be considered to be a motor ability test when the interpretation of the scores are intended to extend beyond the specific skills included in the assessment”. For this review, only studies compliant with this definition were included. As mentioned previously, this variety in conceptualizations can be confusing. For instance, the Test of Gross Motor Development, 2nd edition (TGMD-2[39]) can fulfill the role of either a motor ability assessment instrument, or a fundamental movement skill assessment instrument, depending on the inferred interpretation of the results.
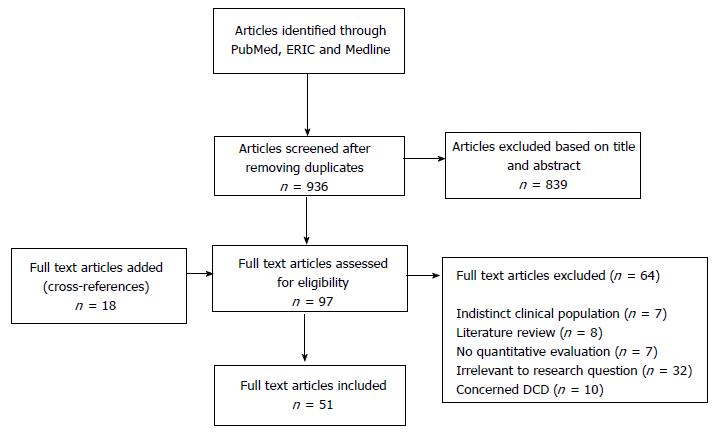
The initial search, conducted by the first and last author, yielded 1422 publications. After screening these titles and abstracts and removing duplicates, 97 studies were identified as potentially relevant. Other 18 articles, retrieved by cross-referencing, were added. A total of 115 full text articles were independently assessed for eligibility by two researchers (first and last author). Disagreements were resolved by discussion. Seven studies were excluded because the clinical populations were not clearly defined. Publications that did not meet criteria 3 included eight literature reviews. Other seven of the originally selected studies did not conduct a quantitative evaluation of motor abilities and were excluded. Furthermore, 32 studies were excluded because they lacked relevance to the research question, focused on motor development or addressed other, more specific motor domains such as gait, handwriting and postural control. Finally, ten studies were withheld because they addressed only populations with DCD. The systematic review process is demonstrated in Figure 1.
The search strategy and inclusion criteria resulted in a total of 51 studies that were acceptable for this literature review. The articles were grouped and analyzed, according to the four diagnostic categories (ADHD, DBD, ASD and depression). An overview of the included studies is presented in the Table 1. Because some studies addressed more than one diagnostic category, the studies are alphabetically organized in Table 1.
| Ref. | Research population(s) | Comparison/control group(s) | Motor assessment instrument(s) | Main findings |
| Berkeley et al[40] (2001) | HFA (n = 15) Age: 6-8 yr Gender: Male and female IQ: Not specified | Norm population | TGMD | 73% cored in the poor to very poor category, illustrating an overall fundamental motor delay. 80% scored ≤ -1.5 SD on the locomotor subscale and 53% scored in the poor/very poor category on the object control subscale |
| Beyer[78] (1999) | ADHD (n = 56) Age: 7-12 yr Gender: Male IQ > 70 | Learning disabilities (n = 56) | BOTMP (Without subscale running speed) | Children with ADHD performed worse on bilateral coordination, strength, visual-motor integration, upper-limb speed and dexterity. Both groups performed equally poorly on the subscales balance, upper limb coordination and response speed |
| Brossard-Racine et al[79] (2011) | ADHD (n = 40) Age: 6-11 yr Gender: Male and female IQ > 80 | Norm population | Movement ABC VMI-V | 50% of the children obtained a score below pc 5 on the Movement ABC, another 20% scored below pc 15 An important subset of the population (85%) exhibited manual dexterity problems 55% of the children obtained a score < -1.5 SD on the VMI |
| Brossard-Racine et al[80] (2012) | ADHD (n = 49) Age: 6-11 yr Gender: Male and female IQ > 80 | Norm population | Movement ABC VMI-V | Motor difficulties were highly present at baseline (73%) but resolved in 18% of the cases after treatment with stimulant medication. Motor impairment persisted in 55% of the population. The severity of the behavioral symptoms was associated with balance skills. No significant differences emerged between the ADHD subtypes |
| After controlling for IQ, the ASD group scored significantly lower than the other 4 groups. Children with DCD and ADHD + DCD also obtained significantly lower scores than the children from the TD group and the ADHD only group | ||||
| Dewey et al[51] (2007) | ASD (n = 49) DCD (n = 46) ADHD (n = 27) ADHD + DCD (n = 38) Age: 5-18 yr Gender: Male and female IQ: Full range | TD (n = 78) | BOTMP-SF | |
| Doyle et al[81] (1995) | ADHD-C (n = 38) Age: 7-12 yr Gender: Male and female IQ: Full range | Norm population | BOTMP-SF | 82% of the children with ADHD exhibited gross motor skills above the norms of the BOTMP-SF Less than 10% of the children had significant motor skill difficulties. Fine motor skills were considered a relative deficit in comparison to gross motor skills |
| Emck et al[2] (2011) | PDD (n = 39) Emotional disorders (n = 17) Behavioral disorders (n = 44) Age: 6-12 yr Gender: Male and female IQ: Not mentioned | Norm population | TGMD-2 | All clinical groups differed significantly from the norm population. Children from the emotional disorders group obtained a higher total score, in comparison to children from the PDD and behavioral disorders groups. Similarly, these groups differed on the locomotion subscale, but no differences emerged for the object control scale |
| Fliers et al[64] (2008) | ADHD (n = 486) Age: 5-19 yr Gender: Male and female IQ > 70 | Controls (n = 269) | DCD-Q Groningen motor Observation scale | Motor coordination problems were demonstrated in one third of children with ADHD (33%-34% boys and 29% girls) Fine and gross motor skills, coordination skills and motor control were related to the inattentive rather than to the hyperactive/impulsive symptoms |
| Fliers et al[65] (2010) | ADHD (n = 32) Age: 6-17 yr Gender: Male and female IQ > 70 | Unaffected siblings (n = 18) Controls (n = 50) | Movement ABC | In total, 63% of the children with ADHD demonstrated motor impairment (29% < pc 15 and 34% < pc5). Children with ADHD performed worse than the unaffected siblings and controls, especially on manual dexterity |
| Ghaziuddin et al[41] (1998) | Autism (n = 12), AS (n = 12), PDD-NOS (n = 12) Age: 8-15 yr Gender: Male and female IQ ≥ 60 | Norm population | BOTMP | Motor problems were present in all groups Differences between the subgroups emerged (Asperger > PDD-NOS > Autism), but after controlling for IQ, the relationship between motor scores and diagnosis was no longer significant |
| Goulardins et al[66] (2013) | ADHD-C (n = 34) Age: 7-11 yr Gender: Male IQ > 70 | Age- and gender matched TD (n = 32) | Motor Development scale | The motor quotients in all areas were lower in the ADHD group in comparison to the TD group However, 88% of the ADHD group scored within the normal range |
| Green et al[47] (2002) | AS (n = 11) Age: 6-10 yr Gender: Male VIQ > 80, TIQ > 70 | SDD-MF (n = 9) | Movement ABC | Children with Asperger syndrome performed worse on all subscales in comparison to SDD-MF, but only the subscale ball skills yielded a significant difference. All the children with Asperger syndrome scored below pc 15, of which 82% had a score beneath pc 5 |
| Green et al[4] (2009) | ASD/autism (n = 101) Age: 9-10 yr Gender: Male and female IQ: Full range | Norm population | Movement ABC DCD-Q | In the ASD group, 79% scored below pc 5 and 10% scored below pc 15. Only 11% scored in the average range (> pc 15). 97% of the children with a low IQ scored beneath pc 5 in comparison to 70% of the children with a higher IQ. The DCD-Q performed moderately well as a screening instrument for motor problems |
| Harvey et al[82] (1997) | ADHD (n = 19) Age: 7-12 yr Gender: Male and female IQ: 80-100 | Norm population | TGMD | Fundamental gross motor performance of children with ADHD is substantially below average, as 61.6% of the children obtained a score ≤ pc 25 |
| Harvey et al[67] (2007) | ADHD (n = 22) Age: 6-12 yr Gender: Male and female IQ > 70 | Age- and gender matched TD (n = 22) | TGMD-2 | Significant differences on the locomotor and object control subscales were revealed between children with and without ADHD. The performance of children with ADHD was classified in the “poor” and “very poor” category, in contrast to the TD children, whose performance was categorized as “average”. Older children obtained higher scores than younger children. No significant effect of stimulant medication was found |
| Hilton et al[52] (2007) | AS (n = 51) Age: 6-12 yr Gender: Male and female IQ ≥ 70 | TD (n = 56) | Movement ABC | Significant differences between children with Asperger syndrome (65% < pc5, 25% < pc 15, 10% no impairment) and control group (100% no impairment) were established. Individuals with Asperger syndrome were most impaired on manual dexterity. A strong relationship exists between motor impairment and severity of the autistic symptoms |
| Hilton et al[5] (2012) | ASD: Concordant pairs (n = 29), Discordant pairs (n = 48) Age: 4-17 yr Gender: Males and females IQ: Not specified | Norm population | BOT-2 DCD-Q | Motor skills of the ASD-affected children were substantially impaired, in contrast to the motor skills of the unaffected siblings, which were essentially normal. 40% of the individuals with ASD scored < -1SD and 43% scored < -2SD from the population mean. Motor skills highly correlated with IQ and autistic severity |
| Jasmin et al[42] (2009) | ASD (n = 35) Age: 3-4 yr Gender: Male IQ: full range | Norm population | PDMS-II | In the ASD group, 63% showed a gross motor delay, 53% a fine motor delay and 57% an overall motor delay. In comparison to the population norms, the mean gross motor and total motor score were situated in the very poor range (-2SD). The mean fine motor score was categorized as poor (-1.5SD) |
| Kooistra et al[85] 2005 | ADHD (n = 29), RD (n = 63), ADHD + RD (n = 47), ADHD + ODD (n = 19), ADHD + RD + ODD (n = 21) Age: 8-16 yr Gender: Male and female IQ > 75 | TD (n = 112) | BOTMP VMI-III | All groups performed significantly worse on the BOTMP (total and subscales) in comparison to the control group, except for the children in the ADHD-only group, whose performance did not differ from the control group (apart from their visual-motor skills). Motor impairment in children with ADHD increased as a function of co-occurring disorders |
| Kooistra et al[68] (2009) | ADHD (n = 47) Age: 7-10 yr Gender: Male and female IQ > 80 | FASD (n = 30) Controls (n = 39) | Movement ABC Clinical observations of motor and postural control | Significant differences between the groups were revealed on all scales, with the exception of the subscale Ball Skills. On the Movement ABC both children with ADHD and FASD exhibited more motor problems than controls. 38% of the ADHD group obtained a score below pc5 and 26% obtained a score < pc15 on the Movement ABC |
| Kopp et al[53] (2010) | ASD and/or ADHD (n = 100) Age: 3-18 yr Gender: Female IQ: Full range | Age- and IQ matched controls (n = 57) | Movement ABC EB-test | Children with ASD and/or ADHD showed more motor coordination problems than controls. 25% of the ASD group and 32% of the ADHD group met the diagnostic criteria for DCD |
| Liu et al[54] (2013) | ASD (n = 30) Age: 3-16 yr Gender: Male and female IQ: 70-100 | Age-matched TD (n = 30) | Movement ABC-2 | Children with ASD scored significantly lower than TD on all subscales and total motor score. All TD children scored within the normal range. In contrast to the TD group, 80% of the ASD group scored in the below average range, of which 77% obtained a score below pc5 |
| Liu et al[55] (2014) | ASD (n = 21) Age: 5-10 yr Gender: Male and female IQ: Not mentioned | Age–matched TD (n = 21) Norm population | TGMD-2 | Significant differences between the ASD and TD group were established for all measures. Whereas 96% of the TD group scored within the normal range, 81% of the ASD group scored in the below average range. On the locomotor subscale, 27% of the ASD group was categorized as poor and 40% as very poor. On the object control scale, 27% were categorized as poor and 33% as very poor |
| Lopata et al[43] 2007 | AS (n = 17) Age: 6-13 yr Gender: Male IQ: Within normal range | Norm population | BOTMP VMI-V | The children with AS performed significantly poor, in comparison to the norm populations. On the BOTMP, the mean composite scores for gross and fine motor skills were approximately -2SD below the population mean. The mean score on the VMI was -1SD below the population mean. No significant differences were found between fine and gross motor skills |
| Manjiviona et al[44] 1995 | AS (n = 12) HFA (n = 9) Age: 7-17 yr Gender: Male and female IQ: Normal range | Norm population | Test of motor impairment-henderson revision | Approximately 67% of the children with HFA and 50% of the children with AS showed clinically significant deficits in motor skills. No differences between the HFA and AS groups emerged |
| Meyer et al[69] (2006) | ADHD (n = 264): ADHD-HI = 74, ADHD-PI = 94, ADHD-C = 96 Age: 6-13 yr Gender: Male and female IQ > 80 | Controls (n = 264) | Grooved Pegboard Test Maze Coordination Test Finger Tapping Test | Children with ADHD performed poorer on the Grooved Pegboard Test and the Maze Coordination Test, but not on the Finger Tapping Test. Children with the ADHD-C subtype were the most impaired. The deficiencies in motor control were mainly confined to a younger age group (6-9 yr) |
| Miller et al[45] (2000) | Autism (n = 14) HFA (n = 26) Age: 6-12 yr Gender: Male and female IQ > 70 | Norm population | Movement ABC | No significant differences appeared between the autism and HFA group. After controlling for IQ, a trend towards more motor impairment in the autism group emerged. Mean total motor scores were situated -1.33 SD below the population means. After controlling for IQ, the HFA group obtained a mean score -1SD and the autism group -1.66SD from the population mean |
| Miyahara et al[48] (1997) | AS (n = 26) Age: 6-15 yr Gender: Male and female IQ > 70 | Learning disability (n = 16) | Movement ABC | 85% of the children with Asperger and 88% of the children with learning disabilities obtained a score below -2SD from the population mean. No group differences were established, except for the subscale manual dexterity. No relationship was found between intellectual and motor functioning |
| Noterdaeme et al[46] (2010) | AS (n = 57) HFA (n = 55) Age: 6-19 yr Gender: Male and female IQ > 80 | Norm population | Standard neurological examination | Motor problems were identified in 53% of children with AS and 47% of children with HFA |
| Pan et al[56] (2009) | ASD (n = 28) ADHD (n = 29) Age: 6-10 yr Gender: Male and female IQ: Average | Controls (n = 34) | TGMD-2 | Both the ASD and ADHD group scored significantly lower than the control group on overall gross motor development as well as on the subscales. The ASD group performed worse than the ADHD group on both subscales. Only 16% of the children with ASD/ADHD showed clinical levels of impairment |
| Pan[31] (2014) | ASD (n = 31): AS = 7, HFA = 24 Age: 10-17 yr Gender: Male IQ: Within normal range | Controls (n = 31) | BOT-2 | The ASD group scored significantly lower than the control group on all subscales, composites and total motor score. The mean manual coordination composite was the lowest, followed by the strength and agility composite |
| Papadopoulos et al[57] (2012) | HFA (n = 23), LFA (n = 8), AS (n = 22) Age: 6-13 yr Gender: Male and female IQ: Full range | TD (n = 20) | Movement ABC | Based on the population norms, 63% of the HFA group, 100% of the LFA group and 28% of the AS group scored below pc 5. Another 18% of the HFA group and 5% of the AS group scored in the borderline range (< pc15). All the TD children obtained a score within the normal range (> pc15). Comparisons between the groups revealed that the HFA group performed worse than the AS group, whereas no difference emerged between the AS en TD group |
| Papadopoulos et al[86] (2013) | ADHD-C without ASD (n = 16) Age: 7-14 yr Gender: Male IQ: Within normal range | TD (n = 16) | Movement ABC-2 | Children with ADHD-C, without comorbidity with ASD, did not display motor difficulties. Higher levels of inattention, but not hyperactivity/impulsivity were associated with poorer total score and performance on the field of ball skills |
| Piek et al[70] (1999) | ADHD-C (n = 16) ADHD-PI (n = 16) Age: 8-11 yr Gender: Male VIQ > 80 | Age matched controls (n = 16) | Movement ABC | Children with ADHD performed significantly poorer than the controls (ADHD-C = 31% < pc5 and 25% < pc15; ADHD-PI = 31% < pc5 and 37% < pc15). Children with ADHD-PI showed a poorer result on Manual Dexterity, whereas children with ADHD-C performed worse on balance |
| Pitcher et al[71] 2003 | ADHD-PI (n = 50) ADHD-C (n = 38) ADHD-HI (n = 16) Age: 7-12 yr Gender: Male VIQ: Full range | Controls (n = 39) | Movement ABC Purdue Pegboard | In comparison to the control group, the ADHD-PI and ADHD-C groups performed significantly worse on the subscales Manual Dexterity and Ball Skills and total score of the Movement ABC. The ADHD-HI did not differ significantly from the control group. The ADHD-PI group performed worse on the Purdue Pegboard in comparison to the controls. No differences were established between any other groups |
| Provost et al[49] (2006) | ASD (n = 19) Age: 21-41 mo Gender: Male and female IQ: Full range | DD without motor problems (n = 18) DD with motor problems (n = 19) | PDMS-2 BSID-II (motor scale) | None of the children with ASD obtained a score within the normal range on the PDMS-2 (84% < -2SD, 16% < -1SD). Motor scores of children with ASD did not differ significantly from those of children with DD and motor problems |
| Schlooz et al[58] (2012) | ASD (n = 12) Age: 9-12 yr Gender: Male IQ: Within normal range | TD (n = 12) Tourette Syndrome (n = 12) | VMI-IV | The ASD group performed worse than the pooled control group on the VMI copy task. Their scores on the visual perception and motor coordination subscales did not differ from the controls |
| Schurink et al[59] 2012 | PDD-NOS (n = 28) Age: 7-12 yr Gender: Male and female IQ > 70 | Age- and gender matched TD (n = 28) | Movement ABC | Compared to the TD group, children with PDD-NOS obtained poor motor scores. In the PDD-NOS group 43% obtained a score below pc 5, 21% showed borderline motor problems and 36% showed no motor problems |
| Sharoun et al[72] (2013) | ADHD (n = 58) Age: 9-11 yr Gender: Male and female IQ: Not mentioned | Controls (n = 58) | 7 motor skill assessments (fine and gross motor tasks) | Children with ADHD showed poorer fine motor skills in comparison to the control group. Results indicate that impairments were observed in tasks requiring more complex motor skills, whereas performance was similar in the less complex tasks |
| Siaperas et al[60] 2011 | AS (n = 50) Age: 7-14 yr Gender: Male IQ > 70 | Age matched controls (n = 50) | Movement ABC-2 | Children with AS showed significant impairment in motor performance. Significant group differences were revealed for all three subscales and the total score |
| Skirbekk et al[73] 2011 | ADHD (n = 39) Anxiety disorder (n = 41) ADHD + Anxiety disorder (n = 25) Age: 7-13 yr Gender: Male and female IQ > 70 | Controls (n = 36) | Movement ABC | All clinical groups showed similar profiles of motor impairment and exhibited a higher total impairment score on the Movement ABC in comparison to the control group. 46% of the children with anxiety disorders, 26% of the ADHD group and 36% of the ADHD + anxiety disorder scored below pc5 |
| Staples et al[61] (2010) | ASD (n = 25) Age: 9-12 yr Gender: Male and female IQ: Full range | Chronological age matched TD (n = 25) Movement skill matched TD (n = 22) Mental age matched TD (n = 19) | TGMD-2 | The movement skills of children with ASD reflect deficits, in addition to delays. The group matched on chronological age performed significantly better on the TGMD-2. Children with ASD perform similarly to children approximately half their age. The motor skills of children with ASD are more impaired, than would be expected, given their cognitive level |
| Tseng et al[74] (2004) | ADHD-C (n = 42) Age: 6-11 yr Gender: Male and female IQ: (above) average | Age-, gender- and handedness matched controls (n = 42) | BOTMP | Significant differences in fine and gross motor skills were revealed between children with and without ADHD. Attention, impulse control and parent rating of activity level were the best predictors of gross motor skills in children with ADHD. Attention and impulse control were the best predictors for fine motor skills |
| Vasserman et al[83] (2014) | ADHD-C (n = 48) ADHD-PI (n = 53) Age: 5-18 yr Gender: Male and female IQ: Full range | Norm population | Any Pegboard task (Purdue Pegboard, Grooved Pegboard…) | In total, 51% of the children with ADHD showed fine motor deficits. Impairment in fine motor skills was more prevalent in the ADHD-PI group (60%) in comparison to the ADHD-C group (40%) |
| Verret et al[75] (2010) | ADHD with stimulant medication (n = 24) ADHD without stimulant medication (n = 19) Age: 7-12 yr Gender: Male and female IQ > 70 | Controls (n = 27) | TGMD-2 | Both groups of children with ADHD obtained lower scores on the locomotor subscale. 47% of the children with ADHD obtained a total score below pc 25, in comparison to 21% of the control group. No differences in performance between the children with or without stimulant medication were established |
| Volker et al[62] 2010 | HFA (n = 60) Age: 6-14 yr Gender: Male and female IQ > 70 | TD (n = 46) Matched ASD subsample (n = 27) | Bender Gestalt-II VMI-V | HFA performed worse on all scales in comparison to the TD group. After controlling for IQ, only differences in performance on scales with a pronounced motor component remained significant |
| Watemberg et al[84] (2007) | ADHD (n = 96): ADHD only = 43, ADHD + DCD = 53 Age: 6-12 yr Gender: Male and female IQ: Not mentioned | Norm population | Movement ABC | DCD was detected in 55% of the children with ADHD. DCD is most prevalent in children with ADHD-PI (63%) and ADHD-C (59%) in comparison to ADHD-HI (11%) |
| Wang et al[76] (2011) | ADHD (n = 25) Age: 4-8 yr Gender: Male and female IQ: 61-112 | Age- and gender matched controls (n = 24) | Movement ABC | Compared to the control group, children in the ADHD group exhibited poorer motor ability on all three subscales. In the ADHD group, 36% had significant motor problems (< pc5) and 28% were borderline cases (< pc15) |
| Whyatt et al[63] (2012) | ASD (n = 18) Age: 7-10 yr Gender: Male and female IQ > 80 | Age-matched receptive vocabulary control group (n = 19) Age-matched non verbal IQ control group (n = 22) | Movement ABC-2 | The ASD group showed overall motor impairment relative to both control groups. Performance comparisons indicate significant impairment in the area of ball skills and manual control in the ASD group; comparable levels of balance control were found in the ASD en control groups |
| Wisdom et al[50] (2007) | ASD (n = 30) Age: 3-13 yr Gender: Male and female IQ: Full range | DCD (n = 22) Receptive-expressive language disorder (n = 30) | Mc Carron Assessment of Neuromuscular Development | Significant group differences emerged for fine and gross motor coordination. The language disorder group was the least impaired (-1SD). The DCD group obtained a mean score of -2SD. The ASD obtained the poorest results, with a mean score below -3SD. The DCD and ASD groups appear to differ more in severity than in kind |
| Yochman et al[77] (2006) | ADHD (n = 49) Age: 4-6 yr Gender: Male and female IQ: Within normal range | Age- and gender matched TD (n = 48) | Miller Assessment for Preschoolers VMI-IV | The scores of the ADHD group were significantly lower than those of the TD group. The group differences remained significant, after controlling for IQ. 47% of the children with ADHD showed fine motor and gross motor problems, 45% showed visual motor problems and 22% exhibited problems with visuomotor integration |
In total, 28 studies were included that examined the motor abilities of children and adolescents with ASD. All studies indicated that they performed below average on various standardized motor assessment instruments. Several studies compared the performance of individuals with ASD to the population norms of the motor assessment instrument[2,4-6,40-50]. These studies showed that impairment in motor abilities is highly prevalent in this population. Quite a few studies that compared the motor abilities of individuals with ASD to those of typically developing peers, confirmed these results[31,51-63]. Overall prevalence rates for impairment in motor abilities ranged from 33% to 100%. However, it is essential to keep in mind that these results are highly depending on the cut-off scores, diagnoses and instruments that have been used.
Overall results indicate that both fine and gross motor skills are affected, as individuals with ASD display a range of measurable motor impairments. More specifically, problems with coordination, balance, ball skills, locomotion, object control, manual dexterity and fine and gross motor delays have been identified. Although some studies suggest that the area of manual dexterity is most impaired[31,52], a specific motor profile is yet to be investigated.
With regard to the potential differences between several disorders within the autism spectrum, no consensus has been reached. Ghaziuddin et al[41] found significant differences in motor abilities of children with Asperger Syndrome, Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS) and Autism. However, after controlling for IQ, the differences no longer yielded significance. In a study of Papadopoulos et al[57], children with high functioning autism (HFA) performed significantly worse on the Movement ABC in comparison to children with Asperger Syndrome. Miller et al[45] examined the differences in motor abilities between children with autism and HFA. Initially, no significant differences were established, but after controlling for IQ, a trend towards a larger impairment in the autism group emerged.
Whereas Miyahara et al[48] found no relationship between intellectual functioning and motor abilities in ASD, two studies performed by Hilton et al[5,52] indicated a strong association. Moreover, they established a relationship between symptom severity and motor ability.
In sum, it can be concluded that impairment in motor abilities in children and adolescents with ASD is more prevalent than in the general population. Additionally, these problems appear at early age and persist into adolescence.
In total, 27 studies were included that examined the motor abilities of children and adolescents with ADHD. Among the studies being reviewed, impairment in motor abilities is commonly reported, with most studies indicating that individuals with ADHD perform worse in comparison to typically developing peers[51,53,56,64-77] or norm populations[2,78-84]. Depending on the type of motor assessment tool and the cut-off points used by different researchers, prevalence rates of impairment in motor abilities are highly variable, ranging from 8% to 73%.
Despite the fact that most studies indicated that individuals with ADHD obtained lower scores in comparison to their peers; scores of individuals with ADHD were often situated within the normal range. Moreover, three of the included studies did not find any difference in motor ability between children with or without ADHD, when including a group of children with ADHD only. In order to create such ADHD only subgroups, these studies ruled out comorbidity with ASD, oppositional defiant disorder (ODD), reading disorder (RD) or DCD[51,85,86].
In three studies, the influence of stimulant medication on motor ability was also assessed. Whereas Harvey et al[67] found no significant effect of stimulant medication, results from the study of Brossard-Racine et al[80] showed that motor difficulties resolved in 18% of the cases, after a three months treatment period. Verret et al[75] established no differences in motor ability between children who were or were not on stimulant medication.
Six studies examined whether differences in motor abilities could be identified within the ADHD subtypes. The results from these studies suggest that the type and degree of motor impairment differs between subtypes. Two studies established an overall larger motor impairment in the ADHD-inattentive subtype (ADHD-I) and ADHD-combined type (ADHD-C) in comparison to the ADHD-hyperactive impulsive subtype (ADHD-HI)[71,84]. Furthermore, Fliers et al[64] stated that fine and gross motor skills, coordination and motor control were related to the inattentive, rather than to the hyperactivity and impulsivity symptoms. With regard to the type of impairment, there is some evidence suggesting that impairment in fine motor skills is more prevalent in the ADHD-I subtype[70,71,83]. However, the results of the study of Meyer et al[69] contrasted these findings, as the ADHD-C subtype was most impaired on Pegboard tasks.
In conclusion, the literature on this topic supports the view that the prevalence of motor impairment is substantial in individuals with ADHD. However, some inconsistencies have been pointed out. More research is needed to draw solid conclusions concerning the motor abilities of children and adolescents with ADHD.
There is a paucity of research investigating the motor abilities of individuals with DBD. In this systematic review, only two studies were included that examined the motor abilities of children with behavioral disorders. However, these studies did not investigate a group solely comprised of children with a DBD. The study of Emck et al[2] assessed the gross motor skills of children with different psychiatric disorders, including a group of behavioral disorders comprised of children with ADHD, ODD and conduct disorder (CD). The results showed that the scores of these children on the Test of Gross Motor Development, 2nd edition (TGMD-2[39]) significantly differed from the norm population, reflecting marked delays in motor development for about three years. Kooistra et al[85] examined to what extent the presence of ODD puts a child with ADHD at risk for motor impairment. Scores on the bruininks-oseretsky test of motor proficiency (BOTMP[87]) of children with ADHD, RD, ODD or various combinations of these, were compared to scores of typically developing controls. The results show that children in the ADHD + ODD group and the ADHD + RD + ODD group scored significantly lower on the BOTMP than controls.
As no separate analyses were conducted to differentiate between several behavioral disorders, the motor abilities of individuals with DBD remain largely unknown. Consequently, the prevalence rate of impairment in motor abilities in this population could not be estimated.
Remarkably, little information is available about the motor abilities of children and adolescents with a depression. Following the search strategy, only one study was included that directly examined the motor abilities of children with emotional disorders. The previous mentioned study of Emck et al[2] also investigated a group of children with emotional disorders. Children from this group performed significantly worse on the TGMD-2 in comparison to the norm population, but performed better in comparison to the other clinical groups of children with Pervasive Developmental Disorders and children with behavioral disorders. However, the emotional disorders group was comprised of children with anxiety disorders and/or depression/dysthymic disorder. As no further analyses were conducted to differentiate between these diagnoses and only gross motor skills of children were examined, no conclusions can be drawn regarding the motor abilities of children and adolescents with a depression.
The aim of this study was to map out existing research documenting motor ability of children and adolescents with four common psychiatric disorders. The major results of this literature review indicated that: (1) Children and adolescents with ADHD or ASD are at risk for impairment in motor abilities; (2) evidence regarding the motor abilities of children and adolescents with DBD or depression is lacking; (3) impairment in motor abilities is common in these child psychiatric disorders, but not universal; and (4) methodological issues complicate the generalization of the findings.
Although impairment in motor ability is not considered to be a major diagnostic feature of any of the discussed psychiatric disorders, the motor ability literature disputes the assumption that these children possess normal motor abilities. As motor impairment may be an important feature, it is essential that it is properly defined and assessed. However, to date, no consensus has been reached upon a golden standard, not for the motor assessment instruments being used, nor for the cut-off scores that are being applied. It is very likely that the discrepancies in the findings from the above-mentioned studies can largely be explained by these methodological variances.
A wide variety of motor assessment instruments have been used across the studies. The Movement ABC or Movement ABC-2 was administered in the majority of the included studies (n = 21). The different versions of the Bruininks-Oseretsky Test of Motor Proficiency (BOTMP/BOTMP-SF/BOT-2) were administered in nine studies. Other frequently used motor assessment instruments included the first or second edition of the TGMD (n = 8) and the different versions of the VMI (n = 7). Apart from the fact that these instruments are valid standardized assessments measuring motor abilities, correlations among these instruments are only low to moderate[88,89]. Thus indicating that they measure different traits or aspects of motor abilities, notwithstanding that these instruments are being used for the same purposes.
In addition, the understanding of the field is further complicated by the use of different cut-off points. The decision of whether or not a person exhibits clinically significant impairment in motor ability is often based upon a certain percentile cut-off score. Whereas some researchers used percentile 5 as a cut-off point[31,42,43,46,48,53,60,73,84], others have used percentile 15[41,44,51,64,67,81,83,85]. Some researchers reported more detailed information and specified the results using both cut-off points[4,5,47,49,52,54,55,57,59,65,66,68,70,71,76,79,80]. Consequently, directly comparing the results of studies with a different methodology would be inappropriate.
Each of the motor assessment instruments used in the included studies can be described as norm-referenced tests. A norm-reference test involves the comparison of a child’s individual test results to those obtained by a representative sample of peers. However, the utility of an assessment instrument is contingent upon its reliability and validity. Tests developed and validated in one population, are potentially not appropriate for administration in another population. Some studies have shown that important cultural differences exist[90,91]. For instance, individuals from diverse cultures use different strategies when performing the test items from the Movement ABC[90]. Just over half of the studies included in this review (n = 29) compared the motor abilities of a clinical population to those of a control group. Of the studies that did not include a control group, the majority used a test that provided appropriate population norms. Only a few studies compared the motor abilities of a clinical population to potentially unsuitable population norms without incorporating a control group of typically developing peers[48,63,81,84].
From the above outlined overview, it is clear that the main focus of the motor ability research is directed towards children between the ages of 5 and 13 years old. Of the 51 included studies, 30 evaluated motor ability in this age category. Other 15 studies investigated a broader age range, of which 13 studies included both primary school children and adolescents and two studies included both young children and primary school children. Other three studies examined the motor abilities of individuals across the full age range, from early childhood through adolescence. Remarkably, only three of the included studies in this review specifically addressed the motor abilities of young children under the age of 6. Most research for this age category focuses on motor development and the achievement of motor milestones. A plausible explanation for this scarcity can be found in the fact that this kind of research fell beyond the scope of this review.
Despite it is relevant and valuable to track the trajectory of motor abilities over time, longitudinal research is lacking. As a consequence, the natural outcome of impairment in motor abilities in the addressed diagnostic categories is largely undetermined. Some studies investigated the steadiness of motor impairment in children with DCD and indicated that the motor status of these children is relatively stable[11,21,92]. In a study by Van Waelvelde et al[93] the stability of Movement ABC scores in children with ASD, ADHD or DCD was examined. Their findings indicated that poor motor performance at preschool age was not always a stable condition, but appeared to be so in children with ASD. However, in these studies, the re-examination of motor abilities was conducted after a period of 1.5-2 years. Consequently, these studies do not provide information regarding the course from early childhood into adolescence, nor do they offer sufficient information regarding the trajectory of motor abilities of individuals with different psychiatric conditions.
In this review, none of the included studies exclusively addressed motor ability in adolescents and no longitudinal studies were included. Consequently, it is impossible to infer whether or not differences in motor ability exist between children or adolescents who suffer from a psychiatric condition.
Several aspects were identified that potentially could influence motor ability. Some studies indicated that the degree and type of impairment seems to be modified by several factors, including symptom severity, medication status, subtypes, gender, comorbidity and IQ. However, it appears that the role of these factors is neglected in the majority of the reviewed studies.
Only a handful of studies examined differences in motor ability between various clinical groups. To date, little is known about whether and how motor impairment varies in type across distinctive diagnostic categories. Identifying motor profiles that are specific to a diagnosis serve a clinical purpose. Specifying the nature, degree and areas of motor problems can perhaps lead to distinguishing profiles between several disorders. Although there is a need to investigate comprehensive motor profiles, only a few studies attempted to differentiate between several motor areas.
Based on the above-discussed issues, there are several reasons to conclude that further research is needed. Whereas the motor abilities of individuals with ASD or ADHD are quite extensively been investigated, some findings are inconsistent, providing mixed results. Furthermore, little research is available addressing the motor abilities of individuals with DBD or Depression and this gap deserves to be filled. Future studies should address or account for factors influencing motor ability, such as IQ and symptom severity, in a systematic manner. Previous research has demonstrated a potential beneficial influence of stimulant medication on motor abilities[80]. Therefore, it is preferable to use a sample that is not on stimulant medication. In addition, diagnostic processes and study designs should include comorbidity issues, as there is a high probability of overlap between different developmental disorders. Finally, investigating detailed motor profiles across different psychiatric disorders is valuable, as it can provide an indication of where unique motor problems emerge. However, it is required to administer the same motor assessment instrument, in order to be able to make comparisons across groups. Moreover, preference should go to extensively used instruments, such as the BOT-2 or the MABC-2, that assess a wide range of motor abilities.
Several researchers suggested that impairment in motor abilities is highly prevalent in children and adolescents with a psychiatric condition. As discussed previously, impairment in motor abilities can have a significant influence on physical and mental health. Therefore, it is important that all children with a psychiatric condition should receive a complete developmental evaluation, including the assessment of motor abilities. The choice of a suitable motor assessment instrument is a complex matter and depends upon several factors. Age, purpose of assessment, cultural similarity between norm and test group, number of items in relation to the available time, etc., are aspects that should be taken into account when deciding upon which instrument to use[33,94]. In general, complementary use of different assessment instruments is recommended. Moreover, knowledge about the frequency and degree of motor impairment among individuals with a psychiatric condition is important when evaluating the need for treatment. Lastly, acknowledging each child’s individual capacities is essential to provide parents and teachers the opportunity to modify the demands of daily life to a level the child is able to cope with.
This systematic review has several limitations. To minimize bias, multiple databases were searched and hand searches were conducted. Although clear research questions were addressed, an extensive and sensitive search was conducted and predefined eligibility criteria for inclusion were used, the possibility of publication bias remains. Studies published in languages other than English were excluded. As with all systematic reviews the findings and interpretations are limited by the quality and quantity of the available evidence. Therefore, conflicting or inconsistent findings may result from differences in population (symptom severity, comorbidity, medication status, etc.) and variability in the assessments instruments that were used to assess motor ability.
Motor abilities are frequently affected in children and adolescents who suffer from a psychiatric condition. The presence of motor impairment can have a significant effect on physical as well as mental health.
Within the field of child psychiatry, the assessment of motor abilities has become increasingly important. In recent years, numerous studies have been published addressing motor abilities of children and adolescents suffering from a psychiatric condition.
This review provides a comprehensive overview and critically analyzes current knowledge regarding the motor abilities of individuals with attention deficit hyperactivity disorder (ADHD), autism spectrum disorders (ASD), disruptive behavior disorders (DBD) and depression. Particular attention has been paid to the full spectrum of motor abilities, including both fine and gross motor skills in children as well as in adolescents.
Several studies indicate that motor impairment is highly prevalent in some pediatric mental health disorders. It is important that all children with a psychiatric condition receive a complete developmental evaluation, including the assessment of motor abilities.
Motor abilities refer to an individual’s potential motor competency. Motor abilities measure the general traits or capacities that underlie performance of a wide variety of motor skills. Consequently, an individuals’ motor ability is not directly observable, but is derived from a set of movement tasks.
This is a comprehensive systematyc review aimed to summarize the current literature about the motor abilities of children and adolescents suffering from a common psychiatric condition. In summary, the authors found that children and adolescents with ADHD or ASD are at risk for impairment in motor abilities and impairment in motor abilities is common in these child psychiatric disorders. They also stated that evidence regarding the motor abilities of children and adolescents with DBD or depression is quite lacking. The paper is generally well-written.
P- Reviewer: Hosak L, Miettunen J, Serafini G S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Emck C, Bosscher R, Beek P, Doreleijers T. Gross motor performance and self-perceived motor competence in children with emotional, behavioural, and pervasive developmental disorders: a review. Dev Med Child Neurol. 2009;51:501-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Emck C, Bosscher RJ, Van Wieringen PC, Doreleijers T, Beek PJ. Gross motor performance and physical fitness in children with psychiatric disorders. Dev Med Child Neurol. 2011;53:150-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Simons J, Verscheure B, Vandenbussche I, Adriaenssens P, Delbroek H. Motorische ontwikkeling bij kinderen en adolescenten met een psychiatrische stoornis [Motor development of children and adolescents with a psychiatric disorder]. Tijdschrift voor Ortho-pedagogiek, Kinderpsychiatrie en Klinische Kinderpsychologie. 2013;38:75-83. |
| 4. | Green D, Charman T, Pickles A, Chandler S, Loucas T, Simonoff E, Baird G. Impairment in movement skills of children with autistic spectrum disorders. Dev Med Child Neurol. 2009;51:311-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 367] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 5. | Hilton CL, Zhang Y, Whilte MR, Klohr CL, Constantino J. Motor impairment in sibling pairs concordant and discordant for autism spectrum disorders. Autism. 2012;16:430-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 121] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 6. | Lane A, Harpster K, Heathcock J. Motor characteristics of young children referred for possible autism spectrum disorder. Pediatr Phys Ther. 2012;24:21-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 7. | Barkley RA. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. New York: Guilford Press 2005; . |
| 8. | Kaplan BJ, Wilson BN, Dewey D, Crawford SG. DCD may not be a discrete disorder. Hum Mov Sci. 1998;17:471-490. [RCA] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 215] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 9. | Wagner MO, Bös K, Jascenoka J, Jekauc D, Petermann F. Peer problems mediate the relationship between developmental coordination disorder and behavioral problems in school-aged children. Res Dev Disabil. 2012;33:2072-2079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Dewey D, Kaplan BJ, Crawford SG, Wilson BN. Developmental coordination disorder: associated problems in attention, learning, and psychosocial adjustment. Hum Mov Sci. 2002;21:905-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 270] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 11. | Losse A, Henderson SE, Elliman D, Hall D, Knight E, Jongmans M. Clumsiness in children--do they grow out of it? A 10-year follow-up study. Dev Med Child Neurol. 1991;33:55-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 398] [Cited by in RCA: 324] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 12. | Tseng MH, Howe TH, Chuang IC, Hsieh CL. Cooccurrence of problems in activity level, attention, psychosocial adjustment, reading and writing in children with developmental coordination disorder. Int J Rehabil Res. 2007;30:327-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Piek JP, Rigoli D, Pearsall-Jones JG, Martin NC, Hay DA, Bennett KS, Levy F. Depressive symptomatology in child and adolescent twins with attention-deficit hyperactivity disorder and/or developmental coordination disorder. Twin Res Hum Genet. 2007;10:587-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 81] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 14. | Piek JP, Bradbury GS, Elsley SC, Tate L. Motor coordination and Social-Emotional behaviour in Preschool - aged children. IJDDE. 2008;55:143-151. [DOI] [Full Text] |
| 15. | Francis M, Piek J. The effects of perceived social support and self-worth on depressive symptomatology in children with and without developmental coordination disorder (DCD). Proceedings of the 38th APS Annual Conference;. New York: Guilford Press 2003; 70-74. |
| 16. | Schoemaker MM, Kalverboer AF. Social and affective problems of children who are clumsy: How early do they begin? Adapt Phys Activ Q. 1994;11:130-140. |
| 17. | Sigurdsson E, Van Os J, Fombonne E. Are impaired childhood motor skills a risk factor for adolescent anxiety? Results from the 1958 U.K. birth cohort and the National Child Development Study. Am J Psychiatry. 2002;159:1044-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 84] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Lingam R, Jongmans MJ, Ellis M, Hunt LP, Golding J, Emond A. Mental health difficulties in children with developmental coordination disorder. Pediatrics. 2012;129:e882-e891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 150] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 19. | Skinner RA, Piek JP. Psychosocial implications of poor motor coordination in children and adolescents. Hum Mov Sci. 2001;20:73-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 352] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 20. | Chen YW, Tseng MH, Hu FC, Cermak SA. Psychosocial adjustment and attention in children with developmental coordination disorder using different motor tests. Res Dev Disabil. 2009;30:1367-1377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Stephenson EA, Chesson RA. ‘Always the guiding hand’: parents’ accounts of the long-term implications of developmental co-ordination disorder for their children and families. Child Care Health Dev. 2008;34:335-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 22. | Pearsall-Jones JG, Piek JP, Rigoli D, Martin NC, Levy F. Motor disorder and anxious and depressive symptomatology: a monozygotic co-twin control approach. Res Dev Disabil. 2011;32:1245-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Shaffer D, Schonfeld I, O’Connor PA, Stokman C, Trautman P, Shafer S, Ng S. Neurological soft signs. Their relationship to psychiatric disorder and intelligence in childhood and adolescence. Arch Gen Psychiatry. 1985;42:342-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 115] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 24. | Rasmussen P, Gillberg C. Natural outcome of ADHD with developmental coordination disorder at age 22 years: a controlled, longitudinal, community-based study. J Am Acad Child Adolesc Psychiatry. 2000;39:1424-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 470] [Cited by in RCA: 449] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 25. | Hellgren L, Gillberg IC, Bågenholm A, Gillberg C. Children with deficits in attention, motor control and perception (DAMP) almost grown up: psychiatric and personality disorders at age 16 years. J Child Psychol Psychiatry. 1994;35:1255-1271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 89] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 26. | Wrotniak BH, Epstein LH, Dorn JM, Jones KE, Kondilis VA. The relationship between motor proficiency and physical activity in children. Pediatrics. 2006;118:e1758-e1765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 351] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 27. | Rivilis I, Hay J, Cairney J, Klentrou P, Liu J, Faught BE. Physical activity and fitness in children with developmental coordination disorder: a systematic review. Res Dev Disabil. 2011;32:894-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 215] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 28. | Barnett LM, Van Beurden E, Morgan PJ, Brooks LO, Beard JR. Does childhood motor skill proficiency predict adolescent fitness? Med Sci Sports Exerc. 2008;40:2137-2144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 193] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 29. | Stodden D, Langendorfer S, Roberton MA. The association between motor skill competence and physical fitness in young adults. Res Q Exerc Sport. 2009;80:223-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 130] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 30. | Lopes VP, Rodrigues LP, Maia JA, Malina RM. Motor coordination as predictor of physical activity in childhood. Scand J Med Sci Sports. 2011;21:663-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 208] [Cited by in RCA: 207] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 31. | Pan CY. Motor proficiency and physical fitness in adolescent males with and without autism spectrum disorders. Autism. 2014;18:156-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 32. | Cairney J, Veldhuizen S. Is developmental coordination disorder a fundamental cause of inactivity and poor health-related fitness in children? Dev Med Child Neurol. 2013;55 Suppl 4:55-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 33. | Burton AW, Miller DE. Movement skill assessment. Champaign, IL: Human Kinetics 1998; . |
| 34. | Fournier KA, Hass CJ, Naik SK, Lodha N, Cauraugh JH. Motor coordination in autism spectrum disorders: a synthesis and meta-analysis. J Autism Dev Disord. 2010;40:1227-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 646] [Cited by in RCA: 687] [Article Influence: 49.1] [Reference Citation Analysis (0)] |
| 35. | Miyahara M. Meta review of systematic and meta analytic reviews on movement differences, effect of movement based interventions, and the underlying neural mechanisms in autism spectrum disorder. Front Integr Neurosci. 2013;7:16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 36. | Downey R, Rapport MJ. Motor activity in children with autism: a review of current literature. Pediatr Phys Ther. 2012;24:2-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 37. | Harvey WJ, Reid G. Attention-deficit/hyperactivity disorder: A review of research on movement skill performance and physical fitness. Adapt Phys Activ Q. 2003;20:1-25. |
| 38. | Gowen E, Hamilton A. Motor abilities in autism: a review using a computational context. J Autism Dev Disord. 2013;43:323-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 234] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 39. | Ulrich DA. Test of gross motor development-2 (TGMD-2). Austin: Prod-Ed 2000; . |
| 40. | Berkeley SL, Zittel LL, Pitney LV, Nichols SE. Locomotor and object control skills of children diagnosed with autism. Adapt Phys Activ Q. 2001;18:405-416. |
| 41. | Ghaziuddin M, Butler E. Clumsiness in autism and Asperger syndrome: a further report. J Intellect Disabil Res. 1998;42:43-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 189] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 42. | Jasmin E, Couture M, McKinley P, Reid G, Fombonne E, Gisel E. Sensori-motor and daily living skills of preschool children with autism spectrum disorders. J Autism Dev Disord. 2009;39:231-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 186] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 43. | Lopata C, Hamm EM, Volker MA, Sowinski JE. Motor and visuomotor skills of children with Asperger’s disorder: preliminary findings. Percept Mot Skills. 2007;104:1183-1192. [PubMed] |
| 44. | Manjiviona J, Prior M. Comparison of Asperger syndrome and high-functioning autistic children on a test of motor impairment. J Autism Dev Disord. 1995;25:23-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 155] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 45. | Miller JN, Ozonoff S. The external validity of Asperger disorder: lack of evidence from the domain of neuropsychology. J Abnorm Psychol. 2000;109:227-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 86] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 46. | Noterdaeme M, Wriedt E, Höhne C. Asperger’s syndrome and high-functioning autism: language, motor and cognitive profiles. Eur Child Adolesc Psychiatry. 2010;19:475-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 47. | Green D, Baird G, Barnett AL, Henderson L, Huber J, Henderson SE. The severity and nature of motor impairment in Asperger’s syndrome: a comparison with specific developmental disorder of motor function. J Child Psychol Psychiatry. 2002;43:655-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 194] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 48. | Miyahara M, Tsujii M, Hori M, Nakanishi K, Kageyama H, Sugiyama T. Brief report: motor incoordination in children with Asperger syndrome and learning disabilities. J Autism Dev Disord. 1997;27:595-603. [PubMed] |
| 49. | Provost B, Lopez BR, Heimerl S. A comparison of motor delays in young children: autism spectrum disorder, developmental delay, and developmental concerns. J Autism Dev Disord. 2007;37:321-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 233] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 50. | Wisdom SN, Dyck MJ, Piek JP, Hay D, Hallmayer J. Can autism, language and coordination disorders be differentiated based on ability profiles? Eur Child Adolesc Psychiatry. 2007;16:178-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 51. | Dewey D, Cantell M, Crawford SG. Motor and gestural performance in children with autism spectrum disorders, developmental coordination disorder, and/or attention deficit hyperactivity disorder. J Int Neuropsychol Soc. 2007;13:246-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 207] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 52. | Hilton C, Wente L, LaVesser P, Ito M, Reed C, Herzberg G. Relationship between motor skill impairment and severity in children with Asperger syndrome. Res Autism Spectr Disord. 2007;1:339-349. [DOI] [Full Text] |
| 53. | Kopp S, Beckung E, Gillberg C. Developmental coordination disorder and other motor control problems in girls with autism spectrum disorder and/or attention-deficit/hyperactivity disorder. Res Dev Disabil. 2010;31:350-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 54. | Liu T, Breslin CM. Fine and gross motor performance of the MABC-2 by children with autism spectrum disorder and typically developing children. Res Autism Spectr Disord. 2013;7:1244-1249. [DOI] [Full Text] |
| 55. | Liu T, Hamilton M, Davis L, ElGarhy S. Gross motor performance by children with Autism Spectrum Disorder and typically developing children on TGMD-2. J Child Adolesc Behav. 2014;2:123. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 56. | Pan CY, Tsai CL, Chu CH. Fundamental movement skills in children diagnosed with autism spectrum disorders and attention deficit hyperactivity disorder. J Autism Dev Disord. 2009;39:1694-1705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 57. | Papadopoulos N, McGinley J, Tonge B, Bradshaw J, Saunders K, Murphy A, Rinehart N. Motor proficiency and emotional/behavioural disturbance in autism and Asperger’s disorder: another piece of the neurological puzzle? Autism. 2012;16:627-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 58. | Schlooz WAJM, Hulstijn W. Atypical visuomotor performance in children with PDD. Res Autism Spectr Disord. 2012;6:326-336. [DOI] [Full Text] |
| 59. | Schurink J, Hartman E, Scherder E, Houwen S, Visscher C. Relationship between motor and executive functioning in school-age children with pervasive developmental disorder not otherwise specified. Res Autism Spectr Disord. 2012;6:726-732. [DOI] [Full Text] |
| 60. | Siaperas P, Ring HA, McAllister CJ, Henderson S, Barnett A, Watson P, Holland AJ. Atypical movement performance and sensory integration in Asperger’s syndrome. J Autism Dev Disord. 2012;42:718-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 61. | Staples KL, Reid G. Fundamental movement skills and autism spectrum disorders. J Autism Dev Disord. 2010;40:209-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 188] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 62. | Volker MA, Lopata C, Vujnovic RK, Smerbeck AM, Toomey JA, Rodgers JD, Schiavo A, Thomeer ML. Comparison of the Bender Gestalt-II and VMI-V in samples of typical children and children with high-functioning autism spectrum disorders. J Psychoeduc Assess. 2010;28:187-200. [RCA] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 63. | Whyatt CP, Craig CM. Motor skills in children aged 7-10 years, diagnosed with autism spectrum disorder. J Autism Dev Disord. 2012;42:1799-1809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 128] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 64. | Fliers E, Rommelse N, Vermeulen SH, Altink M, Buschgens CJ, Faraone SV, Sergeant JA, Franke B, Buitelaar JK. Motor coordination problems in children and adolescents with ADHD rated by parents and teachers: effects of age and gender. J Neural Transm. 2008;115:211-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 146] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 65. | Fliers EA, de Hoog ML, Franke B, Faraone SV, Rommelse NN, Buitelaar JK, Nijhuis-van der Sanden MW. Actual motor performance and self-perceived motor competence in children with attention-deficit hyperactivity disorder compared with healthy siblings and peers. J Dev Behav Pediatr. 2010;31:35-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 66. | Goulardins JB, Marques JC, Casella EB, Nascimento RO, Oliveira JA. Motor profile of children with attention deficit hyperactivity disorder, combined type. Res Dev Disabil. 2013;34:40-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 67. | Harvey WJ, Reid G, Grizenko N, Mbekou V, Ter-Stepanian M, Joober R. Fundamental movement skills and children with attention-deficit hyperactivity disorder: peer comparisons and stimulant effects. J Abnorm Child Psychol. 2007;35:871-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 68. | Kooistra L, Ramage B, Crawford S, Cantell M, Wormsbecker S, Gibbard B, Kaplan BJ. Can attention deficit hyperactivity disorder and fetal alcohol spectrum disorder be differentiated by motor and balance deficits? Hum Mov Sci. 2009;28:529-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 69. | Meyer A, Sagvolden T. Fine motor skills in South African children with symptoms of ADHD: influence of subtype, gender, age, and hand dominance. Behav Brain Funct. 2006;2:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 70. | Piek JP, Pitcher TM, Hay DA. Motor coordination and kinaesthesis in boys with attention deficit-hyperactivity disorder. Dev Med Child Neurol. 1999;41:159-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 217] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 71. | Pitcher TM, Piek JP, Hay DA. Fine and gross motor ability in males with ADHD. Dev Med Child Neurol. 2003;45:525-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 264] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 72. | Scharoun SM, Bryden PJ, Otipkova Z, Musalek M, Lejcarova A. Motor skills in Czech children with attention-deficit/hyperactivity disorder and their neurotypical counterparts. Res Dev Disabil. 2013;34:4142-4153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 73. | Skirbekk B, Hansen BH, Oerbeck B, Wentzel-Larsen T, Kristensen H. Motor impairment in children with anxiety disorders. Psychiatry Res. 2012;198:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 74. | Tseng MH, Henderson A, Chow SM, Yao G. Relationship between motor proficiency, attention, impulse, and activity in children with ADHD. Dev Med Child Neurol. 2004;46:381-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 75. | Verret C, Gardiner P, Béliveau L. Fitness level and gross motor performance of children with attention-deficit hyperactivity disorder. Adapt Phys Activ Q. 2010;27:337-351. [PubMed] |
| 76. | Wang HY, Huang TH, Lo SK. Motor ability and adaptive function in children with attention deficit hyperactivity disorder. Kaohsiung J Med Sci. 2011;27:446-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 77. | Yochman A, Ornoy A, Parush S. Perceptuomotor functioning in preschool children with symptoms of attention deficit hyperactivity disorder. Percept Mot Skills. 2006;102:175-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 78. | Beyer R. Motor proficiency of boys with attention deficit hyperactivity disorder and boys with learning disabilities. Adapt Phys Activ Q. 1999;16:403-414. |
| 79. | Brossard-Racine M, Majnemer A, Shevell M, Snider L, Bélanger SA. Handwriting capacity in children newly diagnosed with Attention Deficit Hyperactivity Disorder. Res Dev Disabil. 2011;32:2927-2934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 80. | Brossard-Racine M, Shevell M, Snider L, Bélanger SA, Majnemer A. Motor skills of children newly diagnosed with Attention Deficit Hyperactivity Disorder prior to and following treatment with stimulant medication. Res Dev Disabil. 2012;33:2080-2087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 81. | Doyle S, Wallen M, Whitmont S. Motor skills in Australian children with attention deficit hyperactivity disorder. Occup Ther Int. 1995;2:229-240. [RCA] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 82. | Harvey WJ, Reid G. Motor performance of children with attention-deficit hyperactivity disorder: A preliminary investigation. Adapt Phys Activ Q. 1997;14:189-202. |
| 83. | Vasserman M, Bender HA, Macallister WS. Motor skills development in children with inattentive versus combined subtypes of ADHD. Appl Neuropsychol Child. 2014;3:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 84. | Watemberg N, Waiserberg N, Zuk L, Lerman-Sagie T. Developmental coordination disorder in children with attention-deficit-hyperactivity disorder and physical therapy intervention. Dev Med Child Neurol. 2007;49:920-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 85. | Kooistra L, Crawford S, Dewey D, Cantell M, Kaplan BJ. Motor correlates of ADHD: contribution of reading disability and oppositional defiant disorder. J Learn Disabil. 2005;38:195-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 86. | Papadopoulos N, Rinehart N, Bradshaw JL, McGinley JL. Brief report: children with ADHD without co-morbid autism do not have impaired motor proficiency on the movement assessment battery for children. J Autism Dev Disord. 2013;43:1477-1482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 87. | Bruininks RH. Bruininks-Oseretsky Test of Motor Proficiency. Circle Pines, MN: American Guidance Service 1978; . |
| 88. | Logan SW, Robinson LE, Rudisill ME, Wadsworth DD, Morera M. The comparison of school-age children’s performance on two motor assessments: the Test of Gross Motor Development and the Movement Assessment Battery for Children. Phys Educ Sport Pedagog. 2014;19:48-59. [DOI] [Full Text] |
| 89. | Spironello C, Hay J, Missiuna C, Faught BE, Cairney J. Concurrent and construct validation of the short form of the Bruininks-Oseretsky Test of Motor Proficiency and the Movement-ABC when administered under field conditions: implications for screening. Child Care Health Dev. 2010;36:499-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 90. | Ruiz L, Graupera JL, Gutiérrez M, Miyahara M. The assessment of motor coordination in children with the Movement. ABC test: A comparative study among Japan, USA and Spain. Int J App Sport Sci. 2003;15:22-35. |
| 91. | Miyahara M, Tsujii M, Hanai T, Jongmans M, Barnett A, Henderson S, Hori M, Nakanishi K, Kageyama H. The Movement Assessment Battery for Children: A preliminary investigation of its usefulness in Japan. Hum Mov Sci. 1998;17:679-697. [RCA] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 62] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 92. | Pless M, Carlsson M, Sundelin C, Persson K. Preschool children with developmental coordination disorder: a short-term follow-up of motor status at seven to eight years of age. Acta Paediatr. 2002;91:521-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 93. | Van Waelvelde H, Oostra A, Dewitte G, Van Den Broeck C, Jongmans MJ. Stability of motor problems in young children with or at risk of autism spectrum disorders, ADHD, and or developmental coordination disorder. Dev Med Child Neurol. 2010;52:e174-e178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 94. | Cools W, Martelaer KD, Samaey C, Andries C. Movement skill assessment of typically developing preschool children: a review of seven movement skill assessment tools. J Sports Sci Med. 2009;8:154-168. [PubMed] |