Published online May 19, 2025. doi: 10.5498/wjp.v15.i5.104995
Revised: February 19, 2025
Accepted: April 8, 2025
Published online: May 19, 2025
Processing time: 110 Days and 1 Hours
Patients with middle and advanced hepatocellular carcinoma (HCC) frequently experience significant anxiety and depression, severely affecting their quality of life.
To examine the anxiety and depression status of patients with middle and advanced HCC, the influencing factors, and the correlation between these psychological factors and quality of life.
We collected baseline data from 100 patients with HCC, assessing anxiety and depression levels using the Hamilton Anxiety Rating Scale (HAMA) and Ha
Results indicated that 64% of patients exhibited anxiety and 65% showed de
Anxiety and depression are prevalent among patients with middle and advanced HCC, impacting quality of life. This underscores the need for psychological health considerations in liver cancer treatment and establishing psychological interventions is essential.
Core Tip: Patients middle and advanced hepatocellular carcinoma (HCC) often experience significant anxiety and depression, which may severely affect their quality of life. This study assessed the anxiety and depression status of patients middle and advanced HCC and their influencing factors, analyzing the correlation between these psychological factors and quality of life. According to the results, a large number of advanced HCC patients suffer from depression and anxiety, which are nega
- Citation: Hendi M, Zhang B, Lv JM, Cai XJ. Factors influencing anxiety and depression in advanced hepatocellular carcinoma patients and their impact on quality of life. World J Psychiatry 2025; 15(5): 104995
- URL: https://www.wjgnet.com/2220-3206/full/v15/i5/104995.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i5.104995
Hepatocellular carcinoma (HCC) is a prevalent malignant tumor, ranking sixth globally and fifth in China for incidence[1]. It is among the top three causes of cancer mortality and poses a significant global health challenge. HCC represents 75% to 80% of liver cancer cases, with incidence and death rates differing greatly by region due to risk factors like alcoholic and non-alcoholic cirrhosis, viral hepatitis (especially hepatitis B and C), and fatty liver[2]. Therapeutic approaches consist of surgical removal, Transcatheter arterial chemoembolization (TACE), percutaneous ethanol injection, chemotherapy, ablative therapy, and liver transplantation. Surgery can fully cure early-stage HCC, but about 70% of patients are diagnosed at intermediate or advanced stages, where surgery is not an option[3]. HCC ranks as the fifth most common cancer in men and the seventh in women. Furthermore, men are three times more likely to develop HCC than women, regardless of race or geographic location. This disease is often associated with high mortality rates and poor prognosis in its advanced stages, presenting significant psychological challenges for patients during their diagnosis and treatment. Patients middle and advanced HCC not only endure physical suffering from the disease but also frequently face anxiety and depression, severely impacting their quality of life[4].
The definitive diagnosis of HCC requires multimodal approaches including diagnostic imaging modalities (computed tomography and magnetic resonance imaging), serological biomarkers such as alpha-fetoprotein assessment, and histopathological confirmation through percutaneous tissue sampling. Among these diagnostic methods, histopathological examination of biopsy specimens obtained via needle puncture continues to represent the most authoritative diagnostic criterion in clinical practice[5]. Staging considers tumor size, number, vascular invasion, liver function, and symptoms, with the Barcelona Clinic Liver Cancer (BCLC) system being the most effective for treatment guidance[1,6]. Early-stage HCC is classified as stages 0 and A, while stages B, C, and D represent intermediate to late stages. Therapy is customized based on the tumor’s features, liver performance, and overall health. Current studies are investigating improved ultrasound, deoxycholine, and circulating tumor DNA tests for diagnostic purposes[7].
Anxiety and depression are common psychological issues among cancer patients. Studies have shown that the prevalence of anxiety and depression in liver cancer patients is higher than in the general population. A study by Klankaew et al[8] found that approximately 80% of patients with advanced liver cancer exhibited varying degrees of anxiety and depression symptoms[8]. Moreover, anxiety and depression not only affect patients’ mental health but are also closely related to physical symptoms, treatment adherence, and prognosis[9]. Patients often experience profound anxiety and depression when confronting the uncertainties of their illness, pain, treatment side effects, and declining quality of life. Therefore, understanding the influencing factors of these psychological states is crucial for improving the overall health and quality of life of liver cancer patients[10].
Liver cancer’s development is complex, involving various biological pathways and is linked to chronic hepatitis, cirrhosis, and metabolic diseases[11]. Hepatitis B and C infections significantly increase liver cancer risk by causing inflammation and fibrosis, leading to mutations[12]. The growing prevalence of non-alcoholic fatty liver disease and metabolic syndrome also contributes to the rising incidence of liver cancer[13,14]. Liver cancer is linked to abnormal activation of signaling pathways like Wnt/β-catenin, phosphatidylinositol 3-kinase/protein kinase B, mitogen-activated protein kinase, and p53, leading to unchecked cell growth and increased angiogenesis[15]. Genetic polymorphisms, particularly in the DPYD gene, also play a crucial role. Variants like DPYD*2A and DPYD*2B can reduce DPD enzyme activity, affecting drug metabolism and potentially increasing toxicity and liver dysfunction[16].
Research has indicated that multiple factors may influence the psychological health status of liver cancer patients. First, the social support system of patients has been shown to play a crucial role in psychological adjustment. Zhao et al[17] noted that good social support can effectively alleviate psychological stress and enhance patients’ coping abilities. Additionally, psychological interventions (such as counseling and cognitive behavioral therapy) have demonstrated positive effects in improving patients’ emotional states[18]. The disease context and progression that patients face may also exacerbate anxiety and depression. For example, the severity of the disease, the presence of comorbidities, and the choice of treatment options can significantly impact psychological well-being.
Lifestyle habits are also important factors to consider. According to research by Liu et al[19], long-term unhealthy lifestyle habits (such as smoking, excessive drinking, and lack of exercise). Improving lifestyle not only enhances the physical health of patients but may also have a positive impact on their psychological state. Lately, more research has concentrated on the connection between mental health and quality of life. According to research by Balikji et al[20], depression and anxiety detrimentally affect quality of life, particularly in the context of chronic disease development. The psychological state of patients directly affects their engagement in daily life and their satisfaction with life, thus it is essential to emphasize a comprehensive assessment of multiple factors, including mental health, in order to improve patient prognosis and quality of life.
Hamilton Anxiety Rating Scale (HAMA) can effectively reflect the severity of anxiety states and shows a good correlation with scores from other anxiety symptom assessment tools[21]. Hamilton Depression Rating Scale (HAMD) is the most commonly used scale for assessing depression in clinical settings, primarily used to evaluate the severity of depressive symptoms in patients with depressive disorders, making it one of the most widely used symptom assessment tools in the world[22]. Additionally, we use the Functional Assessment of Cancer Therapy-Hepatobiliary Questionnaire (FACT-Hep) scale to assess the quality of life of patients; this questionnaire has been widely applied in studies involving liver cancer patients and can comprehensively reflect patients’ physical, social/family, psychological, functional, and liver-related tumor-specific conditions[23].
In summary, the purpose of this study is to analyze the anxiety and depression status of patients with advanced liver cancer and their influencing factors, as well as to explore the correlation between these psychological factors and quality of life. The aim is to provide a theoretical basis for clinical treatment and psychological intervention to help improve the quality of life of patients with advanced liver cancer.
This study involved 105 patients diagnosed with advanced HCC at our hospital from November 2023 to November 2024.
All investigators underwent standardized training. Surveys were conducted using a combination of paper and electronic questionnaires. During the survey process, principles of informed consent were strictly followed. Researchers performed logical checks on the returned questionnaires and completed quality assessments. Questionnaires that did not meet quality standards (e.g., errors, non-standard responses, or multiple missing items) were re-evaluated and verified to ensure data quality. Questionnaires with multiple unanswered questions or irreparable issues were treated as invalid. The estimated time for questionnaire completion was 10 to 15 minutes. The research team provided guidance while patients filled out the questionnaires. Data were collected via paper questionnaires and subsequently entered into a computer system by designated personnel. To ensure data accuracy, all collected data underwent double entry. A total of 105 questionnaires were distributed, and 100 valid questionnaires were returned, resulting in a response rate of 95.23%. All questionnaires were completed in one sitting.
Inclusion criteria: (1) Diagnosis of liver cancer conforms to the standards outlined in the “Guidelines for the Diagnosis and Treatment of Primary Liver Cancer” (2019 edition); (2) Cognitively normal, having read the questionnaire instruc
Exclusion criteria: (1) Presence of other malignant tumors; (2) Consciousness disturbances preventing questionnaire completion; (3) Individuals unwilling to cooperate in completing the questionnaire for personal reasons; (4) Functional impairment of vital organs such as the heart, brain, liver, or kidneys; and (5) Women who are pregnant or nursing.
The ethics committee reviewed and approved this study. All participants signed an informed consent form, ensuring they were aware of the study’s purpose, procedures, and privacy protection measures.
Demographic and clinical data collection: A retrospective analysis was conducted to gather participant information, including demographic data such as age, gender, and alcohol consumption, as well as disease-related data including BCLC stage, number of tumors, history of liver resection, TACE, and hepatic artery infusion chemotherapy (HAIC).
Anxiety and depression[24]: HAMA was used to assess the severity of anxiety symptoms, consisting of 14 items scored on a 0-4 scale: < 14 indicates possibly anxiety; 14-21 indicates mild anxiety; 22-28 indicates moderate anxiety; ≥ 29 indicates severe anxiety. HAMA meets psychometric standards, with a Cronbach’s alpha of 0.93. The HAMD is the most commonly used scale for assessing depressive states, comprising 24 items, most scored on a 0-4 scale, with a few on a 0-2 scale: ≤ 8 indicates possibly depression; 9-20 indicates mild depression; 21-35 indicates moderate depression; > 35 indicates severe depression. HAMD meets psychometric standards, with a Cronbach’s alpha of 0.87.
Quality of life assessment: FACT-Hep questionnaire was developed by the Outcomes Research and Education Center in the United States to assess the quality of life in liver cancer patients. It covers five dimensions: Physical, social/family, psychological, functional, and liver-related tumor-specific conditions, consisting of 45 items with a total score of 180. A higher score indicates better quality of life[23]. A FACT-Hep score < 120 is considered indicative of poor quality of life. The Chinese version of the FACT-Hep questionnaire has shown good test-retest reliability, with all module and total scale scores exceeding 0.7. The overall Cronbach’s alpha was 0.863, indicating good reliability and validity[25].
Social support level[26]: The Social Support Rating Scale (SSRS) was employed to assess social support levels among patients with HCC. This scale includes 10 items that are grouped into three categories: Subjective support (items 1, 3, 4, 5), objective support (items 2, 6, 7), and the use of support (items 8, 9, 10). The scores for items 6 and 7 depend on how many support sources the participant chooses, with ‘none’ earning 0 points; points are awarded for each additional source chosen. The other items are scored individually. Total scores can range from 0 to 66, with scores of ≤ 22 indicating low support, 23-44 indicating moderate support, and 45-66 indicating high support. In this study, the overall Cronbach’s alpha coefficient for the scale was 0.730, indicating satisfactory internal consistency.
The statistical analysis utilized SPSS Statistics version 26.0. Means and standard deviations were used to summarize continuous variables, while counts and percentages were used for categorical variables. Multivariate logistic regression identified independent risk factors for anxiety and depression in liver cancer patients, reporting odds ratios (ORs) with 95% confidence intervals (CIs). The regression model employed two-sided tests with a significance level set at P < 0.05. Moreover, Pearson correlation analysis was performed to examine the relationships between HAMA scores, HAMD scores, and FACT-Hep scores in patients with liver cancer.
A total of 100 patients with intermediate to advanced liver cancer were included in the study, of which 91 were male (91%). Among them, 82 patients (82%) were classified as BCLC stage C, 86 patients (86%) had multiple tumors, 38 patients (38%) had a history of liver resection, and 87 patients (87%) underwent TACE/HAIC.
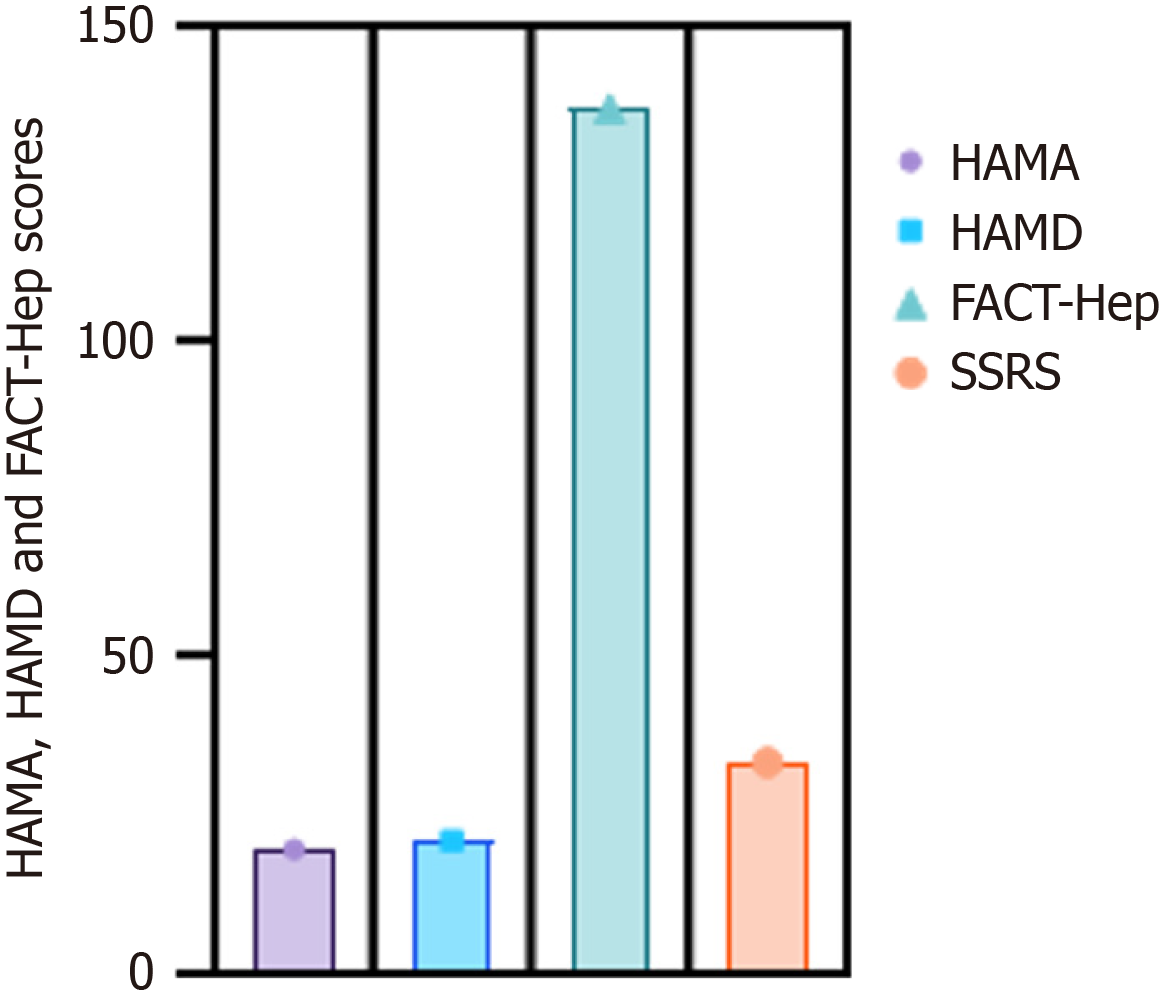
In this study, 105 questionnaires were distributed, and 100 valid questionnaires were returned, resulting in a response rate of 95.23%. The average total HAMA score was 19.53 ± 3.27, the average total HAMD score was 20.89 ± 3.85, the average total SSRS score was 33.29 ± 6.98, and the average total FACT-Hep score was 136.76 ± 7.62, as shown in Figure 1.
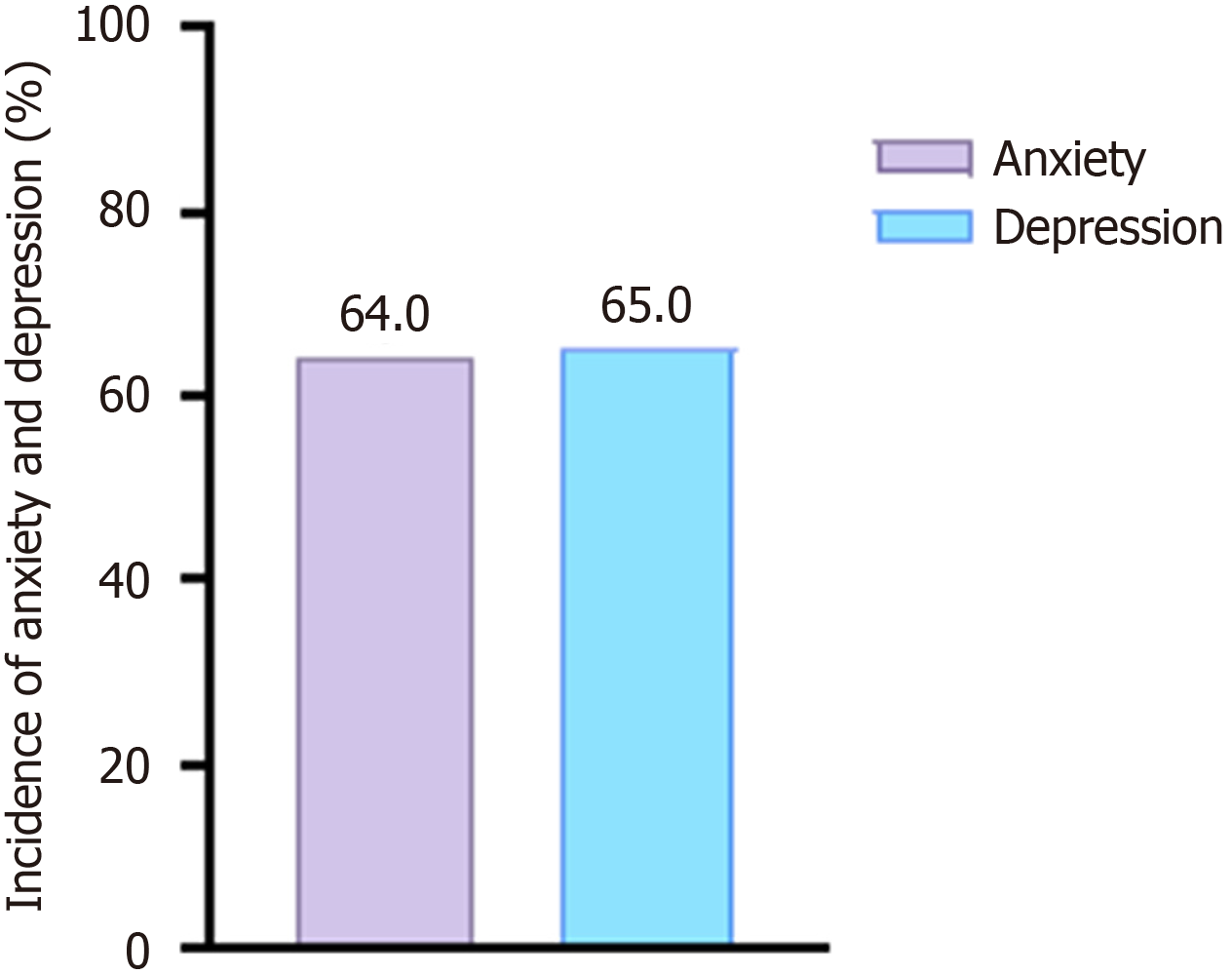
Among the 100 patients with advanced liver cancer, 64 experienced anxiety, resulting in an incidence rate of 64.0% (64/100), with FACT-Hep scores of 119.65 ± 10.73. A total of 65 patients experienced depression, resulting in an incidence rate of 65.0% (65/100), with FACT-Hep scores of 114.62 ± 10.85. The incidence of anxiety (64.0%) and depression (65.0%) is shown in Figure 2.
The results of the univariate analysis for each depression-related factor are displayed in Table 1. The univariate analysis revealed notable differences in education level, living alone, KPS scores, HAMA scores, HAMD scores, history of liver resection and TACE/HAIC, BCLC stage C, number of tumors, social support level, and FACT-Hep scores between depressed and non-depressed patients (P < 0.05).
| Variable | Without depression (n = 35) | Depression (n = 65) | P value |
| Age (years) | 0.617 | ||
| < 60 | 15 (42.9) | 29 (44.6) | |
| ≥ 60 | 20 (57.1) | 36 (55.4) | |
| Sex | 0.253 | ||
| Male | 32 (91.4) | 59 (90.8) | |
| Female | 3 (8.6) | 6 (9.2) | |
| Education | < 0.001 | ||
| Primary | 18 (51.5) | 50 (76.9) | |
| Secondary | 9 (25.7) | 7 (10.8) | |
| Senior high school | 6 (17.1) | 5 (7.7) | |
| College or above | 2 (5.7) | 3 (4.6) | |
| Live alone | < 0.001 | ||
| Yes | 17 (48.6) | 51 (78.5) | |
| No | 18 (51.4) | 14 (21.5) | |
| KPS score | < 0.001 | ||
| 60-80 | 19 (54.3) | 48 (73.8) | |
| > 80 | 16 (45.7) | 17 (26.2) | |
| HAMA score | < 0.001 | ||
| < 14 | 17 (48.5) | 19 (29.2) | |
| 14-21 | 11 (31.4) | 12 (18.5) | |
| ≥ 22 | 7 (20.1) | 34 (52.3) | |
| HAMD score | < 0.001 | ||
| ≤ 8 | 15 (42.8) | 20 (30.8) | |
| 9-20 | 8 (22.8) | 8 (12.3) | |
| ≥ 21 | 12 (34.3) | 37 (56.9) | |
| Previous liver resection | < 0.001 | ||
| Yes | 8 (22.9) | 30 (46.2) | |
| No | 27 (77.1) | 35 (53.8) | |
| TACE/HAIC | < 0.001 | ||
| Yes | 25 (71.4) | 62 (95.4) | |
| No | 10 (28.6) | 3 (4.6) | |
| BCLC stage | < 0.001 | ||
| B | 12 (34.3) | 6 (9.2) | |
| C | 23 (65.7) | 59 (90.8) | |
| Number of tumors | 0.028 | ||
| Single | 9 (25.7) | 5 (7.7) | |
| Multiple | 26 (74.3) | 60 (92.3) | |
| FACT-Hep scores | < 0.001 | ||
| Good | 12 (34.3) | 6 (9.2) | |
| Poor | 23 (65.7) | 59 (90.8) | |
| FACT-Hep scores, mean ± SD | 136.5 ± 11.36 | 114.62 ± 10.85 | 0.039 |
| Social support | 0.017 | ||
| Low support | 15 (42.9) | 35 (53.8) | |
| Moderate support | 9 (25.7) | 19 (29.2) | |
| High support | 11 (31.4) | 11 (17.0) | |
| History of smoking | 0.215 | ||
| Yes | 16 (45.7) | 35 (53.8) | |
| No | 19 (54.3) | 30 (46.2) | |
| History of drinking | 0.743 | ||
| Yes | 20 (57.1) | 40 (61.5) | |
| No | 15 (42.9) | 25 (38.5) |
The results of the univariate analysis for each factor linked to anxiety levels are displayed in Table 2. Significant differences were found between anxious and non-anxious patients concerning age, gender, education level, living alone, KPS scores, HAMA scores, HAMD scores, history of liver resection and TACE/HAIC, BCLC stage C, number of tumors, social support level, FACT-Hep scores, and alcohol consumption (P < 0.05).
| Variable | Without anxiety (n = 36) | Anxiety (n = 64) | P value |
| Age (years) | 0.041 | ||
| < 60 | 15 (41.7) | 21 (32.8) | |
| ≥ 60 | 21 (58.3) | 43 (67.2) | |
| Sex | 0.013 | ||
| Male | 29 (80.6) | 62 (96.9) | |
| Female | 7 (19.4) | 2 (3.1) | |
| Education | < 0.001 | ||
| Primary | 17 (47.2) | 49 (76.6) | |
| Secondary | 9 (25.1) | 8 (12.5) | |
| Senior high school | 7 (19.4) | 5 (7.8) | |
| College or above | 3 (8.3) | 2 (3.1) | |
| Live alone | < 0.001 | ||
| Yes | 19 (52.8) | 50 (78.1) | |
| No | 17 (47.2) | 14 (21.9) | |
| KPS score | < 0.001 | ||
| 60-80 | 20 (55.6) | 47 (73.4) | |
| > 80 | 16 (44.4) | 17 (26.6) | |
| HAMA score | < 0.001 | ||
| < 14 | 17 (47.2) | 19 (29.7) | |
| 14-21 | 11 (30.6) | 12 (18.7) | |
| ≥ 22 | 8 (22.2) | 33 (51.6) | |
| HAMD score | < 0.001 | ||
| ≤ 8 | 15 (41.7) | 15 (23.4) | |
| 9-20 | 8 (22.2) | 8 (12.5) | |
| ≥ 21 | 13 (36.1) | 41 (64.1) | |
| Previous liver resection | < 0.001 | ||
| Yes | 8 (22.2) | 30 (46.9) | |
| No | 28 (77.8) | 34 (53.1) | |
| TACE/HAIC | < 0.001 | ||
| Yes | 25 (69.4) | 62 (96.9) | |
| No | 11 (30.6) | 2 (3.1) | |
| BCLC stage | < 0.001 | ||
| B | 13 (36.1) | 5 (7.8) | |
| C | 23 (63.9) | 59 (92.2) | |
| Number of tumors | < 0.001 | ||
| Single | 10 (27.8) | 4 (6.3) | |
| Multiple | 26 (72.2) | 60 (93.7) | |
| FACT-Hep scores | < 0.001 | ||
| Good | 13 (36.1) | 5 (7.8) | |
| Poor | 23 (63.9) | 59 (92.2) | |
| FACT-Hep scores, mean ± SD | 138.7 ± 11.42 | 119.65 ± 10.73 | 0.015 |
| Social support | < 0.001 | ||
| Low support | 14 (38.9) | 33 (51.6) | |
| Moderate support | 8 (22.2) | 20 (31.2) | |
| High support | 14 (38.9) | 11 (17.2) | |
| History of smoking | 0.571 | ||
| Yes | 19 (52.8) | 33 (51.6) | |
| No | 17 (47.2) | 31 (48.4) | |
| History of drinking | 0.039 | ||
| Yes | 17 (47.2) | 36 (56.3) | |
| No | 19 (52.8) | 28 (43.7) |
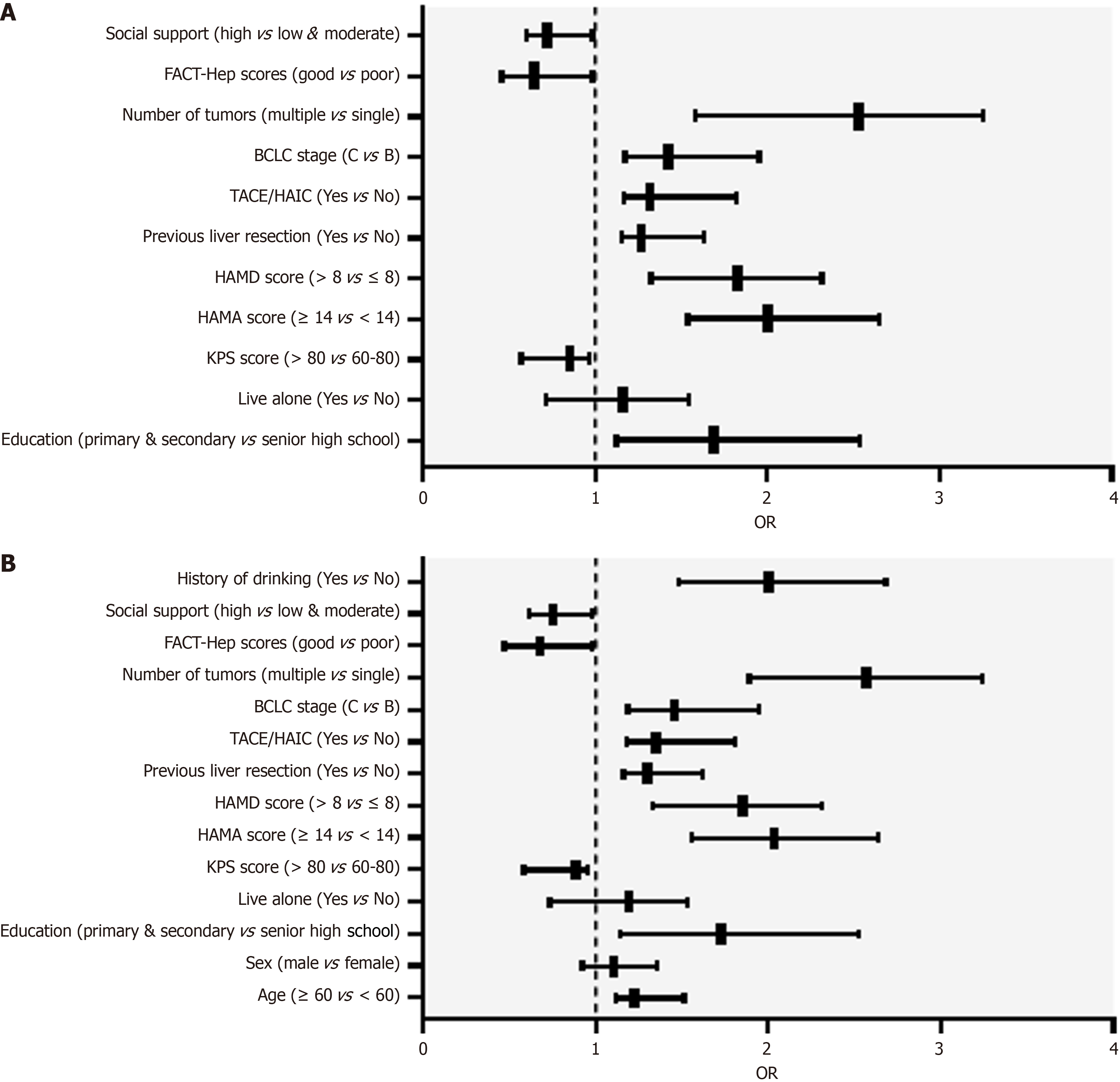
Depression was treated as the dependent variable (no depression = 0, depression = 1), and variables listed in Table 1 were employed as independent variables. A multivariate logistic regression analysis was executed to pinpoint independent factors affecting depression in patients with HCC. The results indicated that higher FACT-Hep scores were associated with a lower risk of depression (OR = 0.643, 95%CI: 0.458-0.985), and patients with high levels of social support had a lower likelihood of depression compared to those with low support (OR = 0.722, 95%CI: 0.603-0.987). Higher HAMA and HAMD scores were associated with an increased risk of depression (OR = 2.003, 95%CI: 1.539-2.651) and (OR = 1.826, 95%CI: 1.324-2.318). A history of liver resection (OR = 1.267, 95%CI: 1.152-1.634) and TACE/HAIC (OR = 1.318, 95%CI: 1.167-1.826) were identified as independent risk factors for depression; BCLC stage C (OR = 1.423, 95%CI: 1.175-1.953) and multiple tumors (OR = 2.528, 95%CI: 1.582-3.256) were also independent risk factors for depression, as shown in Table 3 and Figure 3A.
| Variable | OR | 95%CI | P value |
| Education (primary & secondary vs senior high school) | 1.693 | 1.124-2.538 | 0.028 |
| Live alone (yes vs no) | 1.163 | 0.718-1.544 | 0.951 |
| KPS score (> 80 vs 60-80) | 0.856 | 0.573-0.969 | 0.012 |
| HAMA score (≥ 14 vs < 14) | 2.003 | 1.539-2.651 | < 0.001 |
| HAMD score (> 8 vs ≤ 8) | 1.826 | 1.324-2.318 | < 0.001 |
| Previous liver resection (yes vs no) | 1.267 | 1.152-1.634 | 0.017 |
| TACE/HAIC (yes vs no) | 1.318 | 1.167-1.826 | < 0.001 |
| BCLC stage (C vs B) | 1.423 | 1.175-1.953 | < 0.001 |
| Number of tumors (multiple vs single) | 2.528 | 1.582-3.256 | 0.034 |
| FACT-Hep scores (good vs poor) | 0.643 | 0.458-0.985 | < 0.001 |
| Social support (high vs low & moderate) | 0.722 | 0.603-0.987 | < 0.001 |
In this study, anxiety was designated as the dependent variable (coded as 0 for no and 1 for yes) based on the outcomes of the univariate analysis presented in Table 2. Statistically significant variables from this analysis were employed as independent variables. A multivariate logistic regression analysis was conducted to ascertain the independent factors influencing anxiety among patients with HCC. The findings revealed that elevated FACT-Hep scores were significantly associated with a reduced risk of anxiety (OR = 0.678, 95%CI: 0.473-0.978). Additionally, KPS scores exceeding 80 were identified as a protective factor against anxiety (OR = 0.888, 95%CI: 0.584-0.957). Furthermore, patients with higher levels of social support demonstrated a lower likelihood of experiencing anxiety compared to those with lower levels of support (OR = 0.752, 95%CI: 0.615-0.977).
Conversely, factors such as age over 60 years (OR = 1.228, 95%CI: 1.114-1.514) and a history of alcohol consumption (OR = 2.007, 95%CI: 1.483-2.684) were identified as independent risk factors for anxiety. Additionally, higher HAMA and HAMD scores increased the risk of anxiety (OR = 2.038, 95%CI: 1.554-2.636 and OR = 1.856, 95%CI: 1.336-2.308, respectively). A history of liver resection (OR = 1.299, 95%CI: 1.163-1.622), lower education level (OR = 1.728, 95%CI: 1.139-2.523), and undergoing TACE/HAIC (OR = 1.353, 95%CI: 1.182-1.811) were also identified as independent risk factors for anxiety. Furthermore, BCLC stage C (OR = 1.455, 95%CI: 1.187-1.943) and multiple tumors (OR = 2.567, 95%CI: 1.893-3.244) were significant independent risk factors for anxiety, as shown in Table 4 and Figure 3B.
| Variable | OR | 95%CI | P value |
| Age (≥ 60 vs < 60) | 1.228 | 1.114-1.514 | < 0.001 |
| Sex (male vs female) | 1.104 | 0.925-1.353 | 0.773 |
| Education (primary & secondary vs senior high school) | 1.728 | 1.139-2.523 | 0.028 |
| Live alone (yes vs no) | 1.193 | 0.736-1.534 | 0.951 |
| KPS score (> 80 vs 60-80) | 0.888 | 0.584-0.957 | 0.012 |
| HAMA score (> 14 vs ≤ 14) | 2.038 | 1.554-2.636 | < 0.001 |
| HAMD score (> 8 vs ≤ 8) | 1.856 | 1.336-2.308 | < 0.001 |
| Previous liver resection (yes vs no) | 1.299 | 1.163-1.622 | 0.017 |
| TACE/HAIC (yes vs no) | 1.353 | 1.182-1.811 | < 0.001 |
| BCLC stage (C vs B) | 1.455 | 1.187-1.943 | < 0.001 |
| Number of tumors (multiple vs single) | 2.567 | 1.893-3.244 | 0.034 |
| FACT-Hep scores (good vs poor) | 0.678 | 0.473-0.978 | < 0.001 |
| Social support (high vs low & moderate) | 0.752 | 0.615-0.977 | < 0.001 |
| History of drinking (yes vs no) | 2.007 | 1.483-2.684 | < 0.001 |
Pearson correlation analysis revealed a negative correlation between HAMA and HAMD scores and FACT-Hep scores in liver cancer patients. The correlation coefficient between HAMA scores and FACT-Hep scores was r = -0.671, while the correlation coefficient between HAMD scores and FACT-Hep scores was r = -0.575, as shown in Table 5 and Supplementary Figure 1. This indicates that higher levels of anxiety and depression are associated with lower quality of life in patients with liver cancer.
| Variable | FACT-Hep scores | |
| r | P value | |
| HAMA score | -0.671 | < 0.001 |
| HAMD score | -0.575 | < 0.001 |
Most liver cancer patients are already in the intermediate to advanced stage when they seek medical attention. Although there are various treatment options available, the effectiveness of these treatments is uncertain, and the cure rate is low[27]. Evaluating treatment outcomes solely based on cure rates and survival rates has certain limitations; therefore, quality of life has become an important indicator for assessing the effectiveness of clinical treatments for liver cancer. At the intermediate to advanced stage, liver cancer may be accompanied by symptoms such as hypercalcemia and spontaneous hypoglycemia, severely affecting the patient’s physical function[28]. Additionally, the side effects of chemotherapy are significant, and adverse reactions such as gastrointestinal symptoms and bone marrow suppression can greatly increase the suffering of patients, leading to a decline in their quality of life[29]. Although these physical symptoms can be alleviated through targeted medical interventions or nursing care to improve comfort, significant improvements in quality of life cannot be achieved. In recent years, research on the psychological health and quality of life of cancer and chronic disease patients has become an international research hotspot[30]. In China, although several studies have explored the factors influencing negative emotions and quality of life among liver cancer patients, the research is still not comprehensive enough.
This study found that the overall psychological health status of patients with intermediate to advanced HCC is poor. Among the 100 patients, 64 (64.0%) exhibited symptoms of anxiety, and 65 (65.0%) showed symptoms of depression, with these prevalence rates significantly higher than those in the general population. According to the literature, depression and anxiety contribute to less favorable outcomes in individuals with HCC[31]. A meta-analysis found that the preva
Our findings indicate that depression and anxiety are negatively correlated with social support and quality of life. The decrease in FACT-Hep scores is closely related to an increase in anxiety and depression, indicating that good quality of life helps alleviate psychological health issues. Consistent with other studies, social support is regarded as a crucial element for enhancing an individual’s mental well-being[32]. Furthermore, our multivariate logistic regression analysis shows that higher HAMA and HAMD scores are associated with a higher risk of depression and anxiety, while high social support and high KPS scores are protective factors. This aligns with the findings of Chu et al[33], who found that lower anxiety and depression levels were linked to higher resilience and social support.
Regarding the mechanisms and molecular genetics of liver cancer, the occurrence of liver cancer is closely related to factors such as chronic liver disease, hepatitis virus infection, and metabolic syndrome. Another study indicated that gallic acid significantly inhibited the proliferation of SMMC-7721 liver cancer cells and stimulated the apoptotic process. Although the individual effect of exosomes derived from human umbilical cord mesenchymal stem cells was not significant, the effect was markedly enhanced after their combined application. Meanwhile, the expression levels of key enzymes such as hexokinase, phosphofructokinase, pyruvate kinase, lactate dehydrogenase, tumor necrosis factor-alpha, interleukin-1beta, catalase, superoxide dismutase, and glutathione peroxidase were significantly reduced in malignant liver cells, while the expression of interleukin 6 and malondialdehyde was elevated. Pathway enrichment analysis emphasized that the metabolism of selenium compounds and the metabolism of cysteine and methionine are key pathways[34]. These pathophysiological changes not only affect the physiological health of patients but may also exacerbate their psychological burden by influencing the neuroendocrine system and immune response[35]. For example, chronic inflammation may lead to psychological health issues, which in turn can affect the physiological state of patients, creating a vicious cycle[36] (Supplementary Figure 2).
In summary, this study highlights the importance of psychological health for patients with intermediate to advanced HCC, especially against the backdrop of high rates of anxiety and depression. Future research should focus on how to reduce anxiety and depression levels in HCC patients through improving social support, enhancing quality of life, and providing psychological interventions. Additionally, further exploration of the relationship between liver cancer-related biomarkers and psychological health may provide new insights into understanding the psychological well-being of liver cancer patients.
This study is subject to several limitations. Initially, using self-reported questionnaires for evaluating patients might result in recall bias and fail to encompass all elements of psychological health. Secondly, employing a cross-sectional design restricts the ability to analyze causal links between variables. Future studies should work to overcome these limitations. Further research is needed to explore the potential confounding connection between anxiety symptoms and a family history of HCC. In addition, in our study, male patients accounted for 91% of the sample proportion, which is significantly higher than the existing literature reported that the prevalence of male HCC is about male:female = 3:1. This discrepancy may be due to sample selection bias: Our single-center study reflects only the demographic characteristics of patients with liver cancer in our hospital, and the sample size of our study was relatively small, with only 100 patients. The incidence of liver cancer is associated with some confounding factors such as hepatitis virus infection and alcohol abuse, and the prevalence of alcohol abuse is significantly higher in men than in women, the risk of chronic hepatitis virus infection is higher, and the risk of occupational exposure (such as exposure to harmful chemicals) may affect the accuracy of the results. Finally, the fact that this study was carried out at a single center in China restricts the applicability of the findings to HCC patients in China. Future research should include more objective assessments and undertake large-scale, prospective studies, as well as randomized controlled trials, to evaluate the efficacy of specific interventions designed to alleviate anxiety and depression in patients with HCC.
The findings suggest that a significant portion of patients with intermediate to advanced HCC have symptoms of depression and anxiety. Higher levels of social support and quality of life are associated with lower levels of depression and anxiety. Higher HAMA and HAMD scores, a history of liver resection, BCLC stage C, and multiple tumors are risk factors for depression in patients with intermediate to advanced HCC. Meanwhile, KPS scores are negatively correlated with anxiety. Independent risk factors for anxiety include being over 60 years old, a history of alcohol consumption, higher HAMA and HAMD scores, a history of liver resection, BCLC stage C, and multiple tumors. The anxiety and depression scores of liver cancer patients are negatively correlated with quality of life. Therefore, encouraging patients to engage in active self-care, enhancing psychological counseling, and providing psychological therapy and behavioral interventions for those with anxiety and depression can help improve their recovery, psychological comfort, and quality of life.
| 1. | Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, Zhu AX, Murad MH, Marrero JA. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2107] [Cited by in RCA: 3031] [Article Influence: 433.0] [Reference Citation Analysis (3)] |
| 2. | Zhonghao J, Fan Y. New advances in the treatment of intermediate and advanced hepatocellular carcinoma. Front Oncol. 2024;14:1430991. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Koshy A. Evolving Global Etiology of Hepatocellular Carcinoma (HCC): Insights and Trends for 2024. J Clin Exp Hepatol. 2025;15:102406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 4. | Li M, Yu B, He H, Li N, Gao R. Impact of psychological resilience and social support on psycho-social adjustment in postoperative patients with primary hepatocellular carcinoma: mediating effects of fear of progression. Front Psychol. 2024;15:1461199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Adhoute X, Penaranda G, Raoul JL, Le Treut P, Bollon E, Hardwigsen J, Castellani P, Perrier H, Bourlière M. Usefulness of staging systems and prognostic scores for hepatocellular carcinoma treatments. World J Hepatol. 2016;8:703-715. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Shun SC, Chen CH, Sheu JC, Liang JD, Yang JC, Lai YH. Quality of life and its associated factors in patients with hepatocellular carcinoma receiving one course of transarterial chemoembolization treatment: a longitudinal study. Oncologist. 2012;17:732-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Xu RH, Wei W, Krawczyk M, Wang W, Luo H, Flagg K, Yi S, Shi W, Quan Q, Li K, Zheng L, Zhang H, Caughey BA, Zhao Q, Hou J, Zhang R, Xu Y, Cai H, Li G, Hou R, Zhong Z, Lin D, Fu X, Zhu J, Duan Y, Yu M, Ying B, Zhang W, Wang J, Zhang E, Zhang C, Li O, Guo R, Carter H, Zhu JK, Hao X, Zhang K. Circulating tumour DNA methylation markers for diagnosis and prognosis of hepatocellular carcinoma. Nat Mater. 2017;16:1155-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 478] [Cited by in RCA: 635] [Article Influence: 79.4] [Reference Citation Analysis (0)] |
| 8. | Klankaew S, Temthup S, Nilmanat K, Fitch MI. The Effect of a Nurse-Led Family Involvement Program on Anxiety and Depression in Patients with Advanced-Stage Hepatocellular Carcinoma. Healthcare (Basel). 2023;11:460. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Chen JJ, Huang SS, Li IF, Lin KP, Tsay SL. Prognostic association of demographic and clinical factors with the change rates of symptoms and depression among patients with hepatocellular carcinoma. Support Care Cancer. 2019;27:4665-4674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Han T, Zhou Y, Li D. Relationship between hepatocellular carcinoma and depression via online database analysis. Bioengineered. 2021;12:1689-1697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 11. | Zheng Y, Ming P, Zhu C, Si Y, Xu S, Chen A, Wang J, Zhang B. Hepatitis B virus X protein-induced SH2 domain-containing 5 (SH2D5) expression promotes hepatoma cell growth via an SH2D5-transketolase interaction. J Biol Chem. 2019;294:4815-4827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Sharma KK, Mohsin M, Mittal P, Ali Z, Fatma N, Upadhyay P, Gupta R, Verma A, Kumar G. Diagnosis of the Initial Stage of Hepatocellular Carcinoma: A Review. Curr Pharm Des. 2024;30:1708-1724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Hirai H, Taketa K. Lectin affinity electrophoresis of alpha-fetoprotein. Increased specificity and sensitivity as a marker of hepatocellular carcinoma. J Chromatogr. 1992;604:91-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Jitpraphawan O, Ruamtawee W, Treewatchareekorn M, Sethasine S. Diagnostic and prognostic performances of GALAD score in staging and 1-year mortality of hepatocellular carcinoma: A prospective study. World J Gastroenterol. 2024;30:2343-2353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (2)] |
| 15. | Zhang P, Feng J, Wu X, Chu W, Zhang Y, Li P. Bioinformatics Analysis of Candidate Genes and Pathways Related to Hepatocellular Carcinoma in China: A Study Based on Public Databases. Pathol Oncol Res. 2021;27:588532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 16. | Gao X, Wang X, Zhang S. Bioinformatics identification of crucial genes and pathways associated with hepatocellular carcinoma. Biosci Rep. 2018;38:BSR20181441. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Zhao X, Jin A, Hu B. How Do Perceived Social Support and Community Social Network Alleviate Psychological Distress During COVID-19 Lockdown? The Mediating Role of Residents' Epidemic Prevention Capability. Front Public Health. 2022;10:763490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Rasing SPA, Stikkelbroek YAJ, Riper H, Dekovic M, Nauta MH, Dirksen CD, Creemers DHM, Bodden DHM. Effectiveness and Cost-Effectiveness of Blended Cognitive Behavioral Therapy in Clinically Depressed Adolescents: Protocol for a Pragmatic Quasi-Experimental Controlled Trial. JMIR Res Protoc. 2019;8:e13434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Liu Z, Song C, Suo C, Fan H, Zhang T, Jin L, Chen X. Alcohol consumption and hepatocellular carcinoma: novel insights from a prospective cohort study and nonlinear Mendelian randomization analysis. BMC Med. 2022;20:413. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 25] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 20. | Balikji J, Hoogbergen MM, Garssen J, Verster JC. Mental Resilience, Mood, and Quality of Life in Young Adults with Self-Reported Impaired Wound Healing. Int J Environ Res Public Health. 2022;19:2542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 21. | Liu S, Cheng Y, Xie Z, Lai A, Lv Z, Zhao Y, Xu X, Luo C, Yu H, Shan B, Xu L, Xu J. A Conscious Resting State fMRI Study in SLE Patients Without Major Neuropsychiatric Manifestations. Front Psychiatry. 2018;9:677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Jin G, Li L, Liu J, Wang B, Zhan B. Depression and the risk factors for isolated infectious disease fever patients in the hospital during the COVID-19. Pak J Med Sci. 2023;39:474-478. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 23. | Heffernan N, Cella D, Webster K, Odom L, Martone M, Passik S, Bookbinder M, Fong Y, Jarnagin W, Blumgart L. Measuring health-related quality of life in patients with hepatobiliary cancers: the functional assessment of cancer therapy-hepatobiliary questionnaire. J Clin Oncol. 2002;20:2229-2239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 212] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 24. | Wu G, Jiang Z, Pu Y, Chen S, Wang T, Wang Y, Xu X, Wang S, Jin M, Yao Y, Liu Y, Ke S, Liu S. Serum short-chain fatty acids and its correlation with motor and non-motor symptoms in Parkinson's disease patients. BMC Neurol. 2022;22:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 43] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 25. | Yang Q, Yu X, Zhang W. Health variations among breast-cancer patients from different disease states: evidence from China. BMC Health Serv Res. 2020;20:1033. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Zou Z, Wang Z, Herold F, Kramer AF, Ng JL, Hossain MM, Chen J, Kuang J. Validity and reliability of the physical activity and social support scale among Chinese established adults. Complement Ther Clin Pract. 2023;53:101793. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 27. | Dai X, Jiang W, Ma L, Sun J, Yan X, Qian J, Wang Y, Shi Y, Ni S, Yao N. A metabolism-related gene signature for predicting the prognosis and therapeutic responses in patients with hepatocellular carcinoma. Ann Transl Med. 2021;9:500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 28. | Liu W, Pan Y, Zhu H, Zhou Y, Zhang H, Liu L, Liu Q, Ji G. CircRNA_0008194 functions as a ceRNA to promote invasion of hepatocellular carcinoma via inhibiting miR-190a/AHNAK signaling pathway. J Clin Lab Anal. 2022;36:e24286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Zhou H, Nong Y, Zhu Y, Liang Y, Zhang J, Chen H, Zhu P, Zhang Q. Serum untargeted lipidomics by UHPLC-ESI-HRMS aids the biomarker discovery of colorectal adenoma. BMC Cancer. 2022;22:314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 30. | Chen LC, Lin HY, Hung SK, Chiou WY, Lee MS. Role of modern radiotherapy in managing patients with hepatocellular carcinoma. World J Gastroenterol. 2021;27:2434-2457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (5)] |
| 31. | Tan DJH, Quek SXZ, Yong JN, Suresh A, Koh KXM, Lim WH, Quek J, Tang A, Tan C, Nah B, Tan E, Keitoku T, Muthiah MD, Syn N, Ng CH, Kim BK, Tamaki N, Ho CSH, Loomba R, Huang DQ. Global prevalence of depression and anxiety in patients with hepatocellular carcinoma: Systematic review and meta-analysis. Clin Mol Hepatol. 2022;28:864-875. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 32. | Lu L, Wang X, Wang X, Guo X, Pan B. Association of Covid-19 pandemic-related stress and depressive symptoms among international medical students. BMC Psychiatry. 2022;22:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 33. | Chu Y, Zhang Y, Wang S, Dai H. Resilience mediates the influence of hope, optimism, social support, and stress on anxiety severity among Chinese patients with cervical spondylosis. Front Psychiatry. 2022;13:997541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 34. | Zhang Q, Han L, Luo X, Bao Y, Wang S, Li T, Huo J, Meng X. Enhancing inhibitory effect in SMMC-7721 hepatoma cells through combined treatment of gallic acid and hUC-MSCs-Exos. Int Immunopharmacol. 2025;144:113704. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 35. | Zhou Z, Li Y, Hao H, Wang Y, Zhou Z, Wang Z, Chu X. Screening Hub Genes as Prognostic Biomarkers of Hepatocellular Carcinoma by Bioinformatics Analysis. Cell Transplant. 2019;28:76S-86S. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 83] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 36. | Moghimi A, Bani Hosseinian N, Mahdipour M, Ahmadpour E, Miranda-Bedate A, Ghorbian S. Deciphering the Molecular Complexity of Hepatocellular Carcinoma: Unveiling Novel Biomarkers and Therapeutic Targets Through Advanced Bioinformatics Analysis. Cancer Rep (Hoboken). 2024;7:e2152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |