Published online Apr 19, 2025. doi: 10.5498/wjp.v15.i4.104450
Revised: January 23, 2025
Accepted: February 19, 2025
Published online: April 19, 2025
Processing time: 95 Days and 2.1 Hours
Depression is a disorder characterized by significant and persistent depressed mood, cognitive impairment, impaired voluntary activity, working memory, and somatic symptoms.
To determine the efficacy of Qi-based mindfulness therapy (QMT) in treating anxiety, depression, and sleep disturbances in individuals with mild-to-moderate depression.
A self-controlled before–after trial was conducted. The study invited online participants for recruitment between May and July 2023. Participants (n = 18) aged 18-65 years with mild-to-moderate depression, who were receiving QMT training for 4 weeks, were included. The primary efficacy indicators were the 17 Hamilton Depression Rating Scale and Hamilton Anxiety Scale scores. The secondary outcome indicators included the Zung Self-rating Depression Scale, the self-rating Anxiety Scale, and the Insomnia Severity Index. Pre- and post-intervention assessments were conducted. The patients’ symptoms related to depression, anxiety, and insomnia were reassessed 4 weeks after the post-intervention evaluation.
Patients who underwent the QMT intervention for 4 weeks exhibited a statistically significant reduction in scores on the 17 Hamilton Depression Rating Scale, Hamilton Anxiety Scale, the Zung Self-Rating Depression Scale, the Self-Rating Anxiety Scale, and the Insomnia Severity Index relative to their pre-intervention scores (all P < 0.05).
QMT training for 4 weeks is an effective nonpharmacological treatment for symptoms of depression, anxiety, and insomnia among patients with mild-to-moderate depression.
Core Tip: Depression is a disorder characterized by significant and persistent depressed mood, cognitive impairment, impaired voluntary activity, working memory, and somatic symptoms. Alexander Ma developed Qi-based mindfulness therapy based on mindfulness training and traditional Chinese medicine theory for Qi. This study determined the efficacy of Qi-based mindfulness therapy for depression, anxiety, and sleep disturbances in patients with mild-to-moderate depression.
- Citation: Li QW, Yang Y, Gao XJ, Ma A, Sun W. Effect of Qi-based mindfulness therapy for mild-to-moderate depression. World J Psychiatry 2025; 15(4): 104450
- URL: https://www.wjgnet.com/2220-3206/full/v15/i4/104450.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i4.104450
Depression is a disorder characterized by significant and persistent depressed mood, cognitive impairment, impaired voluntary activity, impaired working memory, and somatic symptoms[1,2]. Long-term depression is accompanied by insomnia, which exacerbates the condition and ultimately contributes to suboptimal treatment outcomes[3]. According to the United Nations Health Agency, depression is the foremost cause of disability on a global scale, with an estimated 300 million affected individuals[4]. The current clinical treatment primarily involves medication according to the guidelines for diagnosing and treating depressive disorders in China[5,6]. However, previous studies have disclosed that the therapeutic efficacy of antidepressants is relatively low in patients with mild-to-moderate depressive disorders[6,7]. Therefore, in clinical practice, when the patient’s depressive symptoms are moderately to mildly controlled by medications, the use of nonpharmacological interventions alone or in combination with medications is often necessary. Mindfulness-based cognitive therapy is a stereotypical, psychological, and behavioral intervention technique[8], which is effective in improving the severity of depression and anxiety symptoms, and its treatment principles are consistent with standard cognitive behavioral therapy[9]. Several studies have shown that mindfulness-based interventions can significantly reduce the relapse rate among patients with major depression[10]. This therapy significantly improves the symptoms of patients with chronic refractory depression, in addition to having a long-lasting effect that alleviates residual symptoms of depressive disorders and successfully and efficiently reduces the risk of relapse[11]. It should be noted that traditional mindfulness therapies often involve longer operation times, requiring patients to commit to extended periods of practice. This can lead to decreased patient cooperation as the treatment duration increases. Furthermore, long-term medication may increase the stigma associated with mental illness and other negative emotions, thereby impairing the therapeutic effect for some patients and failing to meet clinical needs in terms of efficacy and side effects. The present study aimed to identify the efficacy of a novel nonpharmacological, safe, short-operation-time, and effective treatment with minimized adverse effects.
Alexander Ma developed Qi-based mindfulness therapy (QMT) based on mindfulness training and traditional Chinese medicine theory for Qi. According to the traditional Chinese medicine theory, Qi is the foundation of all life processes. Primarily, Qi has the following functions: (1) Increasing resistance and preventing disease; (2) Repairing body damage and curing chronic disease; (3) Elevating positive emotions while diminishing negative ones; (4) Improving sleep quality and overcoming insomnia; (5) Improving brain function and increasing concentration and creativity; and (6) Allowing individuals to feel relaxed and content. The sense of Qi can be improved through the practice of meditation. A practitioner with a Qi sense is more relaxed and happier. The Qi sense can help patients improve their mood and sleep quality. Additionally, QMT emphasizes self-awareness by recognizing negative emotions and thoughts and immediately ceasing them by concentrating on the sense of Qi. This study aimed to determine the efficacy of QMT for depression, anxiety, and sleep disturbances in patients with mild-to-moderate depression.
This was a small-scale analysis based on a self-controlled before–after trial on QMT intervention for mild-to-moderate depression. The study was based on voluntary recruitment and was conducted in several provinces in China. Written informed consent was obtained from all patients before study participation. The Ethics Committee of Peking University Sixth Hospital approved the protocol and the informed consent statement.
The patients were recruited through hospital-based advertisements in the outpatient department from May 1 to June 1, 2023. The inclusion criteria were as follows: (1) Age 18-65 years; (2) Meeting the diagnostic criteria of the major depressive disorder (MDD) according to the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition); (3) Not taking psychiatric drugs in the last month; (4) Less than 72 points on the Zung Self-Rating Depression Scale (SDS) and less than 24 points on the 17 Hamilton Depression Rating Scale (HAMD); (5) High school education or above; and (6) Voluntarily agreed with the investigation and signed a written informed consent form before the start of the clinical trial.
The exclusion criteria were as follows: (1) Presence of severe psychiatric disorders, including schizophrenia spectrum, bipolar disorder, obsessive–compulsive disorder, dementia and neurocognitive disorders, drug use disorders, and other psychotic disorders; (2) Depression caused by nervous system disease (stroke and Parkinson’s disease); (3) Presence of severe organic diseases or other conditions making the individuals unsuitable for participating in the study (at the investigator’s discretion); and (4) Taking antidepressant drugs or antipsychotic drugs 2 weeks before the trial.
The participants attended a 4-week-long QMT training program. The intervention methods consisted of 4 weeks of QMT training. During week 1, the participants were engaged in various forms of Qi-based meditation, relaxation exercises, and concentration training. The minimum daily practice time was 20 minutes. In the second week, they focused on the sense of Qi in the “dantian” region, and the minimum daily practice time was 30 minutes. In week 3, they focused on practicing self-awareness, recognizing negative emotions and thoughts, and immediately ceasing them by directing their attention to the sense of Qi. In week 4, the primary objective was to engage in habit optimization practice, namely substituting habitual thought processes with universal wisdom and continuously refining character traits and behavior patterns. The universal wisdom includes dualism, impermanence, thorough integrity and non-downfall, being yourself, and cultivating merit. The minimum daily practice time was 45 minutes. The subjects were clocked daily to verify that the exercise tasks were completed. Additionally, the participants attended a 10-minutes lecture on depressive disorders. Professional therapists administered QMT after having completed standardized training to ensure the consistency of treatment quality.
The primary efficacy indicators were the HAMD-17 and Hamilton Anxiety Scale (HAMA) scores. The secondary outcome indicators were the SDS, the Self-Rating Anxiety Scale (SAS), and the Insomnia Severity Index (ISI). Pre- and post-intervention assessments were conducted.
HAMD-17: We utilized the HAMD-17 version, which is a standardized tool for measuring the severity of depressive symptoms. The evaluation process involved two professionals who conducted a thorough and structured interview to ensure accuracy. A score of less than 7 points indicated no depression, 14 points and above indicated the presence of depression, 21 points and above suggested obvious depression, and 29 points and above indicated severe depression.
HAMA: The HAMA is extensively used in clinical practice. Ideally, the assessment should involve two professionals conducting a structured interview. In this study, we utilized the HAMA-14 version. A score of less than 7 points indicated no anxiety, 14 points and above indicated the presence of anxiety, 21 points and above suggested obvious anxiety, and 29 points and above indicated severe anxiety.
SDS: This scale was designed by Zung in 1965. The SDS has 20 items, and each item has 1 to 4 points. The total score ranges from 20 to 80, with a higher score indicating more serious depressive symptoms.
SAS: The SAS was used to assess an individual’s anxiety degree. The SAS consists of 20 projects, each divided into four levels. The SAS standard score is the total score of each item multiplied by 1.25. The SAS standard score of 50 or above represents anxiety state. Higher scores indicate more severe anxiety.
ISI: The ISI is a commonly used and extensively validated instrument to screen for insomnia and assess its severity level. Higher scores on the ISI indicate greater insomnia severity.
Sample size estimation was based on the results of previous studies examining the effects of mindfulness-based cognitive therapy for anxiety and depression symptoms. In small samples of adults with mild-to-moderate depression, the safety and efficacy of QMT are comparable to those observed in research on anxiety and depression[12]. G*power was used for calculation. With a large effect size of 0.4, an error probability of 0.05, and power of 0.9, the required sample size was 15.
Categorical data were expressed as frequencies (percentages), and continuous variables were expressed as mean ± SD. Quantitative data were analyzed using the χ2-test. For end points including HAMD, HAMA, SAS, SDS, and ISI, one-way analysis of variance was used for analysis. The differences between different intervention time points were analyzed using the Bonferroni post-hoc test. GraphPad Prism 9.3 statistical software was used for all analyses. P < 0.05 was considered statistically significant.
A total of 43 subjects were pre-screened by the general practitioners. Of these, 21 patients failed to meet the inclusion/exclusion criteria. The remaining 22 patients were included in the study, and 18 patients completed the study and had valid measurements.
A total of 18 eligible participants [12 (66.7%) women, 36.5 ± 7.6 years old, body mass index: 22.8 ± 4.6 kg/m2] were included. The demographic data at baseline and after QMT intervention are presented in Table 1.
| Female | Male | Age | BMI |
| 12 (66.7) | 6 (33.3) | 36.5 ± 7.5 | 22.7 ± 4.5 |
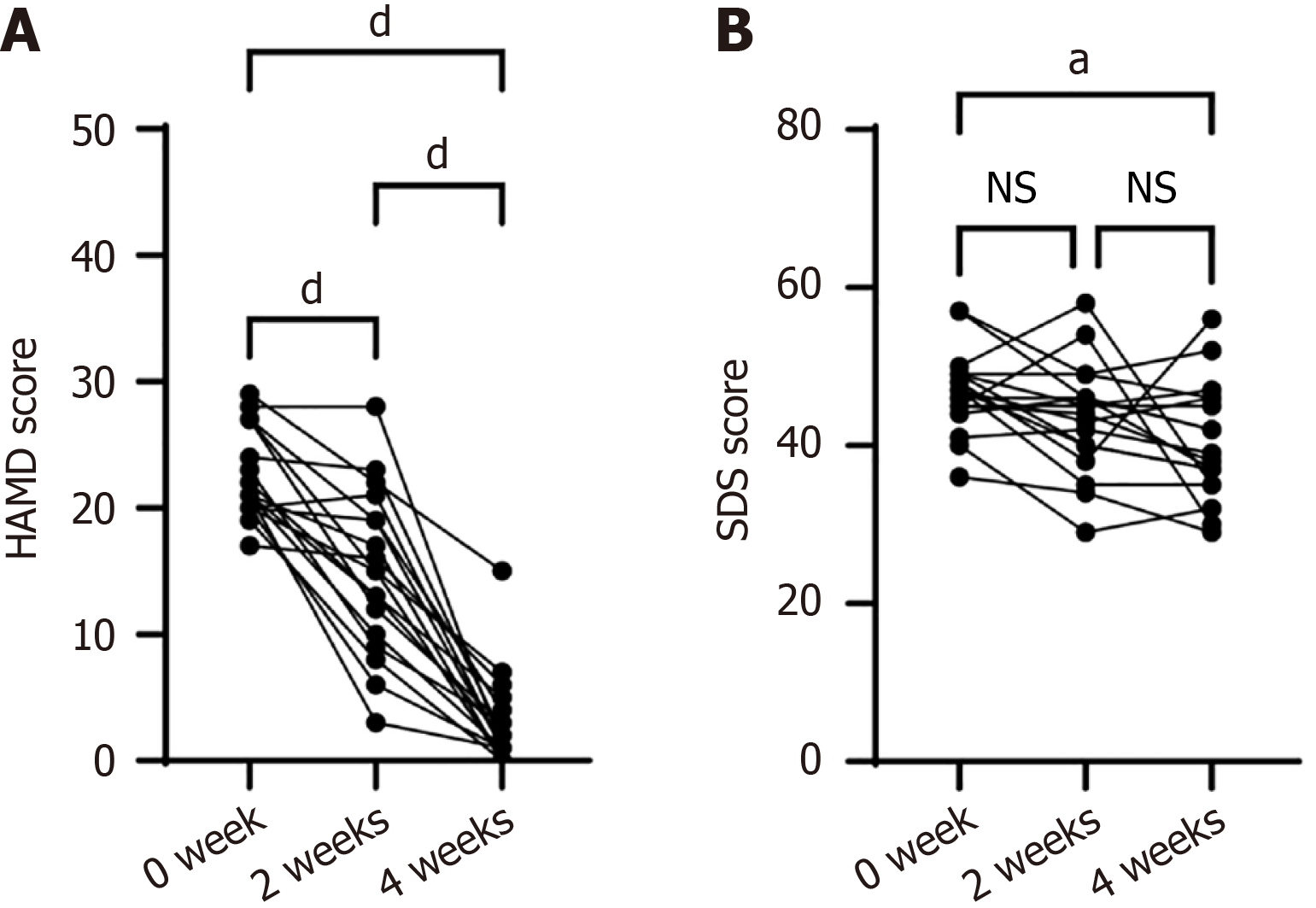
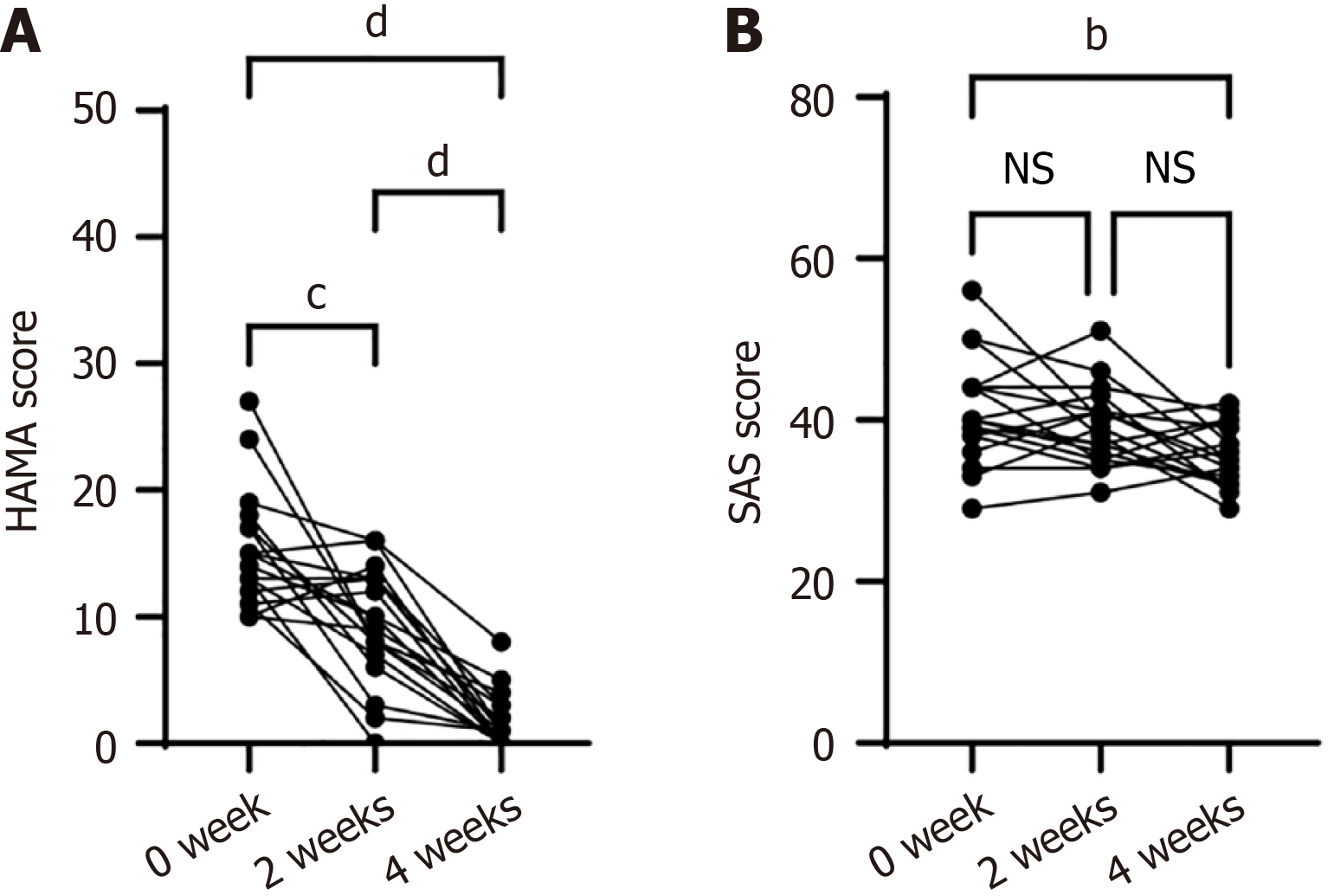
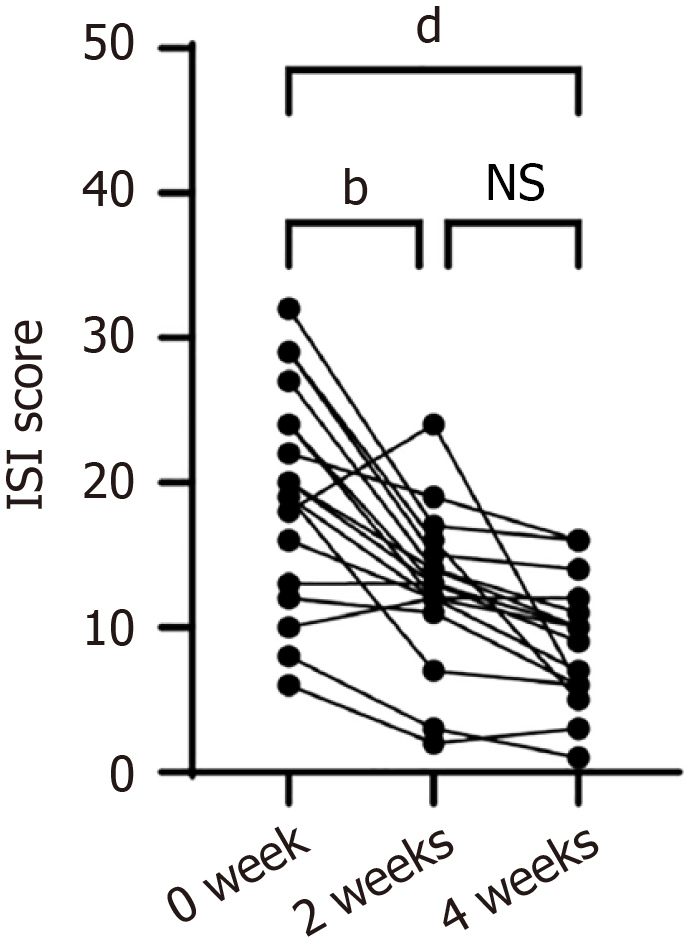
QMT treatment demonstrated significant improvements in depression severity, as measured by the HAMD and the SDS, compared with pretest baseline scores. The HAMD results indicated a considerable decrease in depression levels between pretest and posttest measurements [F (2, 51) = 78.70, P < 0.0001, 0-week vs 2-week, P < 0.0001; 0-week vs 4-week, P < 0.0001] (Figure 1A). Additionally, there was a significant decrease in the SDS scores [F (2, 51) = 4.40, P < 0.05] from baseline to the post-intervention point at 4 weeks (0-week vs 4-week, P < 0.05) (Figure 1B). Furthermore, anxiety questionnaires indicated a significant reduction in emotional regulation related to anxiety between the pretest and posttest phases. Namely, there was a significant decrease in anxiety symptoms, as measured by the HAMA [F (2, 51) = 52.39, P < 0.0001], comparing baseline with the post-intervention points at 2 and 4 weeks (0-week vs 2-week, P = 0.0001; 0-week vs 4-week, P < 0.0001) (Figure 2A). Additionally, there was a significant decrease in the SAS scores [F (2, 51) = 5.15, P < 0.01] from baseline to the post-intervention point at 4 weeks (0-week vs 4-week, P < 0.01) (Figure 2B). Finally, regarding insomnia symptoms, the results of the ISI indicated a significant reduction in insomnia symptoms, with a notable decrease in the ISI score from baseline to the post-intervention point at 4 weeks [F (2, 51) = 8.29, P < 0.001]. The ISI scores significantly decreased from baseline to the post-intervention point at 4 weeks (0-week vs 4-week, P < 0.001) (Figure 3).
There was no significant difference in the incidence of adverse events.
MDD is a prevalent clinical psychological disease associated with stress. It continues to impose a significant burden on individuals and society and is a potential risk factor threatening mental health. The prognosis of this disorder is limited, especially in sensitive patients with mild-to-moderate depressive disorder. For patients with mild-to-moderate depressive disorder, the use of antidepressant medications is a current clinical option. However, antidepressants have numerous side effects, so there is an urgent need for applying alternative, nonpharmacological interventions. Antidepressants are currently available in clinical practice as a treatment option for patients diagnosed with mild-to-moderate depressive disorder. However, the prognosis is limited, particularly for those who are more susceptible to medication-induced symptoms[13,14]. Effective management of mild-to-moderate depression symptoms is a way to prevent progression to severe depression.
In this study, we investigated the improvement in the symptoms of patients with mild-to-moderate depression with a new type of QMT therapy. Preliminarily, we developed a set of QMT operation processes, and the results confirmed the efficacy of QMT. The data showed that the SDS and SAS scores were significantly reduced after 2 weeks of treatment, but the patients’ depression and anxiety self-assessment symptoms persisted. However, after 4 weeks of treatment, the patients’ depression and anxiety self-assessment symptoms improved significantly.
The current study showed that the HAMD and HAMA scores improved to different degrees after 2 and 4 weeks of treatment. The HAMD and HAMA scores decreased significantly after 4 weeks, and similar findings have been reported in the national literature. The ISI is a reliable, valid, brief self-report instrument to quantify perceived insomnia severity and a useful tool for measuring outcomes after insomnia treatment. We observed an improvement in the ISI to different degrees after 2 and 4 weeks of treatment, and the ISI scores decreased significantly after 4 weeks. The findings are consistent with prior research regarding the positive impact of mindfulness-based interventions on sleep quality[15]. The above findings suggest that the symptoms of depression, anxiety, and insomnia in patients with mild-to-moderate depression can be improved through QMT treatment.
The degree of reduction of anxiety, depression, and sleep disorders varies among different patients possibly due to the following reasons. First, the severity of depression, anxiety, and insomnia differs among individuals, leading to variations in treatment effectiveness. Second, there are differences in patients’ learning abilities; different patients may exhibit slight variations in their proficiency in learning and applying the QMT. These differences in learning proficiency can contribute to disparate treatment outcomes. Therefore, in future clinical practice, it is necessary to enhance individualized treatment approaches using QMT.
Previous studies have suggested that the mechanisms underlying mindfulness-based intervention include changes in brain mechanisms associated with psychological cognitive functions[16-18]. In depressed patients, there is a significant association between cognitive and emotional responses due to excessive attention to negative emotions, decreased attention, reduction of self-adjusting function, cognitive maladaptation, and rumination, which reduces the meta-awareness abilities of the patients. Depression can be alleviated by repeating and strengthening positive thinking meditation, body scanning, and thought exercise training to improve positive thinking levels. QMT exercises helped the patients identify negative thoughts and emotions and develop a new, correct, positive mindset. The participants were encouraged to confront difficulties and establish adaptive behavior patterns, which improved their health-related quality of life.
As the patients’ level of mindfulness meditation progresses, they become more attuned to abnormal perceptual patterns, negative thought patterns, and feelings. Additionally, they allocate less attention to negative information and more towards positive information. Moreover, the individual encounters challenges less frequently through rumination and avoidance, which ultimately contributes to the alleviation of depressive symptoms and the prevention of major depression. According to the traditional Chinese medicine theory, Qi circulation is a form of vital energy that sustains the body’s normal functioning[19]. Qi stagnation and qi deficiency are associated with depression[20], anxiety[21] and insomnia[22]. QMT helped the participants overcome negative emotions by acquiring a Qi sense and gaining more energy. The Qi sense is easier to train concentration than breathing. Concentrating on Qi sense can reduce patients’ automated thought processes and promote physical and mental relaxation.
Mindfulness-based intervention has the potential to induce modifications in brain function or brain structure[23,24], including brain areas responsible for learning, memory, attention, and emotion, prefrontal cortex, cingulate gyrus, and hippocampus. It has been indicated that mindfulness-based intervention can reduce the HAMD-17 scores. Other studies have revealed that mindfulness treatment can reduce hippocampal atrophy and enhance functional connectivity within the default mode network[25]. Additionally, these interventions have been associated with improved memory and memory functions. In future research, functional magnetic resonance imaging and electroencephalography should be combined to elucidate the patterns of how QMT affects different brain regions, particularly those related to emotion and insomnia, such as the prefrontal cortex and the lateral orbitofrontal cortex.
It was found that mindfulness-based intervention caused a decrease in connectivity of the anterior cingulate gyrus, which is associated with regulating emotions, left dorsomedial prefrontal cortex, right superior temporal gyrus, left middle occipital gyrus, and left inferior temporal gyrus. Additionally, the treatment can cause increased connectivity with the right inferior temporal gyrus, right inferior frontal gyrus, right temporomandibular junction, and inferior parietal lobe. Hölzel et al[26] found that after mindfulness-based intervention training, the concentration of hippocampus, posterior cingulate cortex, temporoparietal junction, and cerebellar gray matter increased. The changes in these brain regions suggest that improving depressive symptoms and preventing depression recurrence by mindfulness-based intervention may occur through the attentional control network system and emotion regulation areas of the brain.
Our results indicate that QMT is an effective treatment in reducing anxiety and depression symptom severity among a broad range of treatment-seeking individuals. Additionally, our study provides more evidence for the involvement of neural mechanisms in the effective treatment of depression by QMT therapy. Advancements and innovations in this study include the introduction of QMT to China for the first time and the development of a standardized operation procedure. QMT is a simple, noninvasive, and effective treatment method for a range of depressive disorders. Additionally, in our small-sample trial on QMT, the patients’ noted that it was easier to concentrate when doing QMT and that QMT was more relaxing than the traditional mindfulness practice. Therefore, our study provides empirical evidence for improving sleep quality through relaxation training. In summary, the effect of symptom intervention in patients with mild-to-moderate depression using QMT in this study is comparable to that of mindfulness-based intervention. Additionally, the positive patient acceptance and significant clinical improvement in sleep quality and depressive symptoms suggest that QMT could be a viable nonpharmacological intervention technique for clinical promotion.
Our study has several limitations. First, this study had a small sample size, so the effect of the exercise interventions requires further research on a larger sample size. Second, the subjects with mild-to-moderate depression without a history of medication were recruited online. QMT was associated with a more pronounced recovery effect in patients who consistently interacted with their surroundings, had high self-awareness and social support, and exhibited good social functioning. In the future, MDD patients with a medication history should receive QMT training to evaluate treatment efficacy. Third, the long-term implications of the study’s findings cannot be assessed due to the observational design employed in our study. Finally, we lacked objective data on the diagnostic tests used in this study.
The results of this study indicate that QMT may effectively improve depressive symptoms and subjective sleep quality in patients with mild-to-moderate depression. This study supports QMT as a nonpharmacological intervention for the management of depressive symptoms and insomnia in patients with depression.
| 1. | Harvey PO, Le Bastard G, Pochon JB, Levy R, Allilaire JF, Dubois B, Fossati P. Executive functions and updating of the contents of working memory in unipolar depression. J Psychiatr Res. 2004;38:567-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 232] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 2. | Levens SM, Gotlib IH. Updating positive and negative stimuli in working memory in depression. J Exp Psychol Gen. 2010;139:654-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 169] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 3. | Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, Jansson-Fröjmark M, Palagini L, Rücker G, Riemann D, Baglioni C. Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med Rev. 2019;43:96-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 681] [Article Influence: 97.3] [Reference Citation Analysis (0)] |
| 4. | Herrman H, Kieling C, McGorry P, Horton R, Sargent J, Patel V. Reducing the global burden of depression: a Lancet-World Psychiatric Association Commission. Lancet. 2019;393:e42-e43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 247] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 5. | Fournier JC, DeRubeis RJ, Hollon SD, Dimidjian S, Amsterdam JD, Shelton RC, Fawcett J. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1410] [Cited by in RCA: 1275] [Article Influence: 85.0] [Reference Citation Analysis (0)] |
| 6. | Cladder-Micus MB, Speckens AEM, Vrijsen JN, T Donders AR, Becker ES, Spijker J. Mindfulness-based cognitive therapy for patients with chronic, treatment-resistant depression: A pragmatic randomized controlled trial. Depress Anxiety. 2018;35:914-924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 7. | Kim J, Shin C, Han KM, Lee MS, Jeong HG, Pae CU, Patkar AA, Masand PM, Han C. Investigating the effectiveness of a smart mental health intervention (inMind) for stress reduction during pharmacological treatment for mild to moderate major depressive disorders: Study protocol for a randomized control trial. Front Psychiatry. 2023;14:1034246. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Ghawadra SF, Lim Abdullah K, Choo WY, Danaee M, Phang CK. The effect of mindfulness-based training on stress, anxiety, depression and job satisfaction among ward nurses: A randomized control trial. J Nurs Manag. 2020;28:1088-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Mirchandaney R, Barete R, Asarnow LD. Moderators of Cognitive Behavioral Treatment for Insomnia on Depression and Anxiety Outcomes. Curr Psychiatry Rep. 2022;24:121-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 38] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 10. | Bondolfi G, Jermann F, der Linden MV, Gex-Fabry M, Bizzini L, Rouget BW, Myers-Arrazola L, Gonzalez C, Segal Z, Aubry JM, Bertschy G. Depression relapse prophylaxis with Mindfulness-Based Cognitive Therapy: replication and extension in the Swiss health care system. J Affect Disord. 2010;122:224-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 120] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 11. | Foroughi A, Sadeghi K, Parvizifard A, Parsa Moghadam A, Davarinejad O, Farnia V, Azar G. The effectiveness of mindfulness-based cognitive therapy for reducing rumination and improving mindfulness and self-compassion in patients with treatment-resistant depression. Trends Psychiatry Psychother. 2020;42:138-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Strege MV, Swain D, Bochicchio L, Valdespino A, Richey JA. A Pilot Study of the Effects of Mindfulness-Based Cognitive Therapy on Positive Affect and Social Anxiety Symptoms. Front Psychol. 2018;9:866. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Oliva V, Lippi M, Paci R, Del Fabro L, Delvecchio G, Brambilla P, De Ronchi D, Fanelli G, Serretti A. Gastrointestinal side effects associated with antidepressant treatments in patients with major depressive disorder: A systematic review and meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 102] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 14. | Yang NN, Lin LL, Li YJ, Li HP, Cao Y, Tan CX, Hao XW, Ma SM, Wang L, Liu CZ. Potential Mechanisms and Clinical Effectiveness of Acupuncture in Depression. Curr Neuropharmacol. 2022;20:738-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 68] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 15. | Rusch HL, Rosario M, Levison LM, Olivera A, Livingston WS, Wu T, Gill JM. The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Ann N Y Acad Sci. 2019;1445:5-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 216] [Article Influence: 36.0] [Reference Citation Analysis (0)] |
| 16. | Allen JG, Romate J, Rajkumar E. Mindfulness-based positive psychology interventions: a systematic review. BMC Psychol. 2021;9:116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 17. | Bloom PA, Pagliaccio D, Zhang J, Bauer CCC, Kyler M, Greene KD, Treves I, Morfini F, Durham K, Cherner R, Bajwa Z, Wool E, Olafsson V, Lee RF, Bidmead F, Cardona J, Kirshenbaum JS, Ghosh S, Hinds O, Wighton P, Galfalvy H, Simpson HB, Whitfield-Gabrieli S, Auerbach RP. Mindfulness-based real-time fMRI neurofeedback: a randomized controlled trial to optimize dosing for depressed adolescents. BMC Psychiatry. 2023;23:757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Noda S, Shirotsuki K, Nakao M. Low-intensity mindfulness and cognitive-behavioral therapy for social anxiety: a pilot randomized controlled trial. BMC Psychiatry. 2024;24:190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 19. | Chiang HC, Yang ST, Lee KC, Huang PY, Hsu M, Chang HH. From theory to clinic: key components of qi deficiency in traditional Chinese medicine. Altern Ther Health Med. 2012;18:28-36. [PubMed] |
| 20. | Xinzhu W, Yuanchun H. Qi stagnation and qi deficiency are associated with depression in college students. Front Public Health. 2024;12:1444237. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Yaqi W, Weibo Z, Yixing W, Haihong Z, Yaoyao Z, Yun Y, Taotao WU, Bin L, Ji W. Traditional Chinese Medicine constitution among patients with allergic rhinitis and its correlation with anxiety and depression. J Tradit Chin Med. 2023;43:1252-1258. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Liu C, Qu J, Chen L, Liu R. Analysis of Sleep Quality and TCM Constitution Characteristics in 258 Outpatients: A Cross-Sectional Study Based on Outpatient Cases. Appl Bionics Biomech. 2022;2022:2952531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Goldin PR, Thurston M, Allende S, Moodie C, Dixon ML, Heimberg RG, Gross JJ. Evaluation of Cognitive Behavioral Therapy vs Mindfulness Meditation in Brain Changes During Reappraisal and Acceptance Among Patients With Social Anxiety Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2021;78:1134-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 24. | Nakamura H, Tawatsuji Y, Fang S, Matsui T. Explanation of emotion regulation mechanism of mindfulness using a brain function model. Neural Netw. 2021;138:198-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Sezer I, Pizzagalli DA, Sacchet MD. Resting-state fMRI functional connectivity and mindfulness in clinical and non-clinical contexts: A review and synthesis. Neurosci Biobehav Rev. 2022;135:104583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 92] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 26. | Hölzel BK, Carmody J, Vangel M, Congleton C, Yerramsetti SM, Gard T, Lazar SW. Mindfulness practice leads to increases in regional brain gray matter density. Psychiatry Res. 2011;191:36-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1205] [Cited by in RCA: 792] [Article Influence: 56.6] [Reference Citation Analysis (0)] |