Published online Mar 19, 2025. doi: 10.5498/wjp.v15.i3.99364
Revised: December 18, 2024
Accepted: January 8, 2025
Published online: March 19, 2025
Processing time: 220 Days and 10.8 Hours
Schizophrenia is a chronic psychiatric condition with complex symptomatology, including debilitating auditory hallucinations. Transcranial direct current stimu
To evaluate the therapeutic efficacy of tDCS in schizophrenia.
Adhering to PRISMA guidelines, we systematically searched PubMed, Embase, Web of Science, and the Cochrane Library on September 19, 2023, for randomized controlled trials examining the efficacy of tDCS in schizophrenia, with no language or time restrictions. We included studies that compared tDCS with a control condition and reported clinically relevant outcomes. Data extraction and quality assessments were performed by independent evaluators using the Coch
Nine studies comprising 425 participants (tDCS group: 219, control group: 206) were included. The meta-analysis demonstrated a significant reduction in au
tDCS significantly reduces auditory hallucinations in schizophrenia, suggesting its potential as an effective adjunctive treatment for managing this disabling symptom. The findings highlight the practical significance of tDCS in clinical settings, particularly for patients with treatment-resistant auditory hallucinations.
Core Tip: This work rigorously follows the PRISMA guidelines and includes nine studies with a total of 425 participants, highlighting a significant reduction in auditory hallucination scores post-transcranial direct current stimulation treatment. Given the pressing need for effective adjunctive treatments for schizophrenia, especially for symptoms as challenging as auditory hallucinations, our findings offer valuable insights into innovative therapeutic strategies.
- Citation: Zou SJ, Shi JN. Therapeutic efficacy of transcranial direct current stimulation in treating auditory hallucinations in schizophrenia: A meta-analysis. World J Psychiatry 2025; 15(3): 99364
- URL: https://www.wjgnet.com/2220-3206/full/v15/i3/99364.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i3.99364
Schizophrenia, a multifaceted and often debilitating psychiatric disorder, manifests through a spectrum of symptoms affecting cognitive, emotional, and behavioral domains, including hallucinations, delusions, disorganized thinking, and social withdrawal. Among these, auditory hallucinations are particularly prevalent and profoundly disabling, con
Auditory hallucinations are a core feature of schizophrenia, affecting approximately 60%-80% of patients and contributing to significant distress and functional impairment. These hallucinations are often resistant to conventional pharmacological treatments and are closely associated with poor prognosis, including an increased risk of hospitalization and suicidality. Therefore, targeting auditory hallucinations specifically through non-invasive neuromodulation techniques like tDCS may offer a valuable therapeutic avenue. By focusing on auditory hallucinations, this review addresses a symptom that is both highly prevalent and particularly debilitating in the schizophrenia population, with the potential for substantial clinical impact. Recent studies[7-9] have increasingly focused on refining neuromodulation techniques, such as tDCS, to address treatment-resistant auditory hallucinations in schizophrenia. Notably, emerging evidence highlights the potential for optimizing stimulation parameters, such as frequency and session duration, to enhance therapeutic outcomes. Additionally, comparative studies between different forms of transcranial stimulation, such as tACS and high-frequency transcranial random noise stimulation, are being explored as promising adjunctive treatments, suggesting that tailored stimulation protocols could lead to more consistent and effective results. The aim of this systematic review and meta-analysis is to critically evaluate and synthesize the current body of evidence on the therapeutic efficacy of tDCS in schizophrenia. Specifically, this review seeks to assess tDCS’s potential as an adjunctive or standalone intervention for alleviating symptoms, particularly auditory hallucinations, and to delineate its role within the broader treatment framework of schizophrenia. Additionally, the review aims to identify key factors influencing tDCS efficacy, highlight research gaps, and provide recommendations for optimizing future clinical protocols and trials.
During our systematic review, we diligently adhered to the PRISMA criteria to ensure the rigor and credibility of our research methodology[10]. A literature search was performed on September 19, 2023, utilizing four major electronic databases: PubMed, Embase, Web of Science, and the Cochrane Library, to encompass a comprehensive range of articles relevant to our meta-analysis without time constraints. Our search strategy was carefully crafted, utilizing the following key terms: "Transcranial Direct Current Stimulation", "Schizophrenia", "Auditory Hallucinations", "tDCS", "Hallucinations", "Psychosis", and "Mental Health". These terms were selected to comprehensively cover the Patient, Intervention, Comparison, Outcome (PICO) framework and ensure the exhaustive retrieval of relevant studies. This strategic selection of keywords was instrumental in ensuring the exhaustive retrieval of relevant studies, thereby fortifying the foundation of our meta-analysis. Furthermore, to enhance the comprehensiveness of our literature search, we imposed no restrictions based on language, thereby broadening the scope of our study inclusion. Additionally, we undertook a manual screening of the reference lists of pertinent articles to identify any further records that could potentially contribute to our analysis.
Inclusion criteria: Study design: We incorporated randomized controlled studies (RCTs) that assessed the efficacy of tDCS in persons diagnosed with schizophrenia. Participants: The selected studies included subjects diagnosed with schizophrenia, regardless of age, gender, or subtype, to represent a comprehensive range of the patient population. Interventions: Only studies that explicitly examined the application of tDCS as an intervention for schizophrenia were included. Comparators: Studies were considered if they compared tDCS with a control condition, which may encompass sham stimulation, standard care, or alternative therapeutic approaches, to evaluate the relative efficacy of tDCS. Outcomes: Research must concentrate on clinically important outcomes directly associated with auditory hallucinations, as measured by validated psychiatric assessment tools.
Exclusion criteria: Non-RCT studies: Observational studies, case reports, reviews, commentaries, and editorials were eliminated to prioritize data from RCT, which offer superior evidence quality. Non-Schizophrenia Participants: Studies including people with disorders other than schizophrenia, like schizoaffective disorder or bipolar disorder, were eliminated to provide a concentrated emphasis on schizophrenia. Alternative interventions: Studies that did not primarily focus on tDCS or that combined tDCS with other neuromodulatory approaches without a distinct distinction of effects were eliminated. Insufficient data: Studies without adequate data on the relevant outcomes for meta-analysis were omitted. Duplicate publications: In cases of several studies concerning the same research population, only the most complete or current publication was used to prevent data duplication.
In the meta-analysis, two independent assessors performed literature scanning and data extraction, guaranteeing comprehensive cross-verification. Discrepancies identified were addressed through dialogue, with the possibility of engaging a third-party reviewer if required. The extracted data included critical information such as the study's authors, publication year, participant sample size, age, and particulars of the tDCS intervention, including timing, frequency, and intensity. The outcome measures emphasized included mean scores, standard deviations of scale evaluations, and any recorded adverse reactions. In instances where relevant data was lacking in the published reports, the original investigators were contacted via email to get the necessary information, hence improving the thoroughness and precision of our research.
To evaluate the methodological integrity of the studies incorporated into our meta-analysis, we utilized the Cochrane Collaboration's tool for assessing risk of bias[11]. This thorough evaluation was performed independently by two reviewers, who examined several essential domains, including random sequence generation, allocation concealment, participant and staff blinding, outcome data completeness, selective outcome reporting, and the detection of any additional biases that might compromise the study's validity. Each domain was classified according to the risk of bias it presented, labeled as low, unclear, or high. When reviewers' evaluations differed, a positive discourse was undertaken to achieve consensus, and a third reviewer's viewpoint was solicited when necessary to address outstanding disputes.
χ2 statistics and the I2 index were utilized to evaluate study heterogeneity, with I2 values under 50% and P values ≤ 0.10 signifying minimal heterogeneity, hence validating the application of a fixed-effect model for effect size computation. I2 values of 50% or greater, or P values below 0.10, indicated substantial heterogeneity, requiring the application of a random-effects model. Sensitivity analyses were performed by systematically omitting studies to evaluate their influence on the overall outcomes. Publication bias was assessed using funnel plot symmetry and Egger's test, with all analyses conducted in Stata version 17 to ensure methodological rigor.
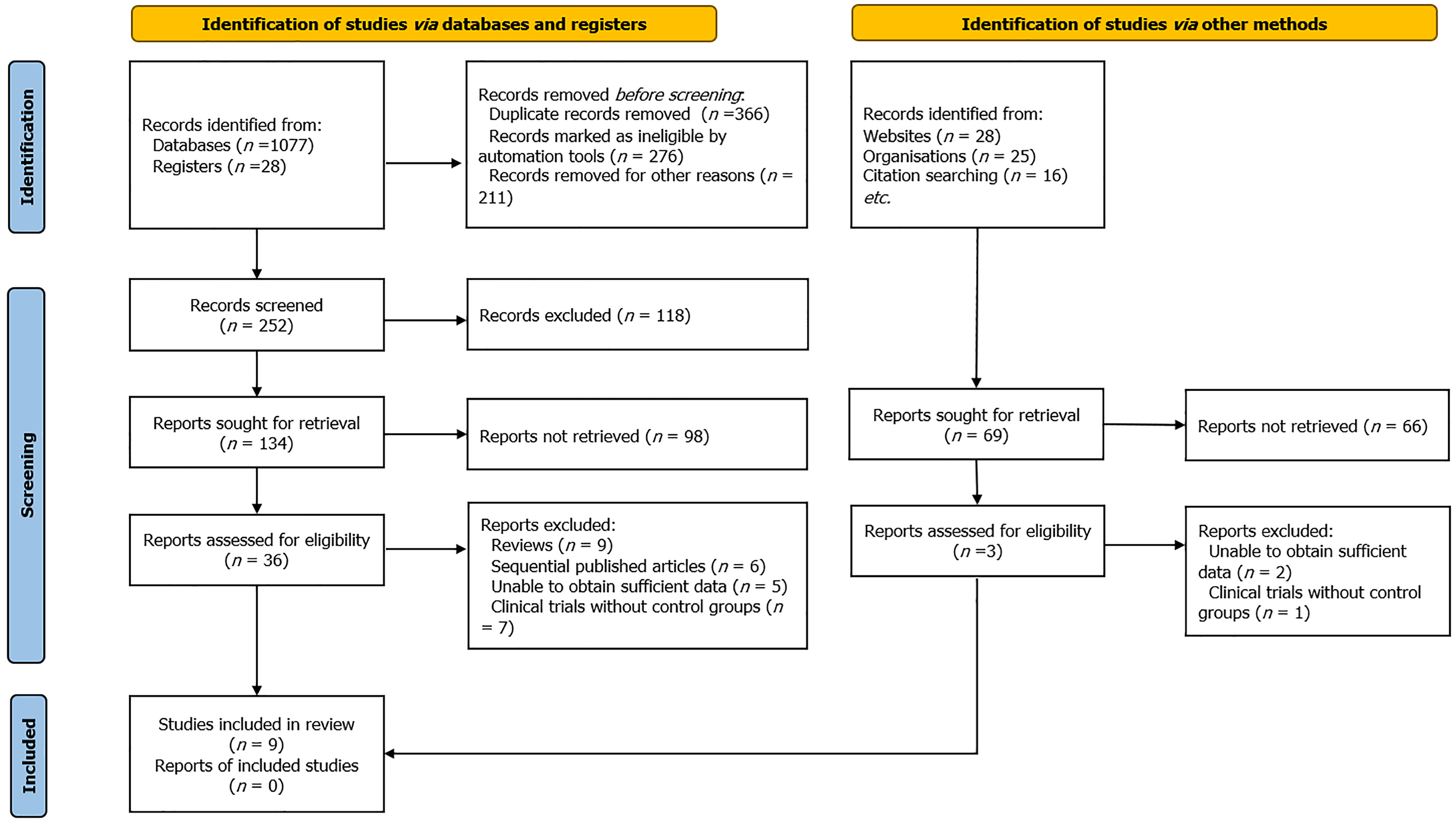
Initially, our systematic review and meta-analysis conducted an extensive search across various electronic databases, resulting in 1174 possibly pertinent papers. By employing a deduplication method, we optimized this collection to guarantee the inclusion of only unique research. A comprehensive evaluation of titles and abstracts ensued, directed by rigorous inclusion and exclusion criteria that included study design, participant demographics, assessed outcomes, and research quality. The preliminary screening yielded the identification of 39 articles for further analysis. Multiple researchers conducted independent assessments of the complete texts of these papers to ensure an impartial rating procedure. This phase resulted in the deletion of 30 papers for several reasons: Review articles (n = 11), sequentially published studies (n = 6), insufficient data (n = 6), and clinical trials lacking control groups (n = 7). As a result, nine publications met all the stringent criteria established in our study protocol and were incorporated into the final meta-analysis, guaranteeing a thorough and comprehensive synthesis of the available evidence[12-20] (Figure 1).
The meta-analysis consolidated results from nine research conducted over eight years to assess the effectiveness of tDCS in treating schizophrenia. The studies combined included 425 participants: 219 in the tDCS treatment groups and 206 in the control groups. A uniform stimulation technique was noted, featuring an intensity of 2 × 20 mA for several minutes across the majority of trials, with a period primarily set at five days, except for one study that prolonged the intervention to 20 days. The application frequency of tDCS was predominantly twice daily, with a singular study implementing it once daily. Electrode placement focused on the dorsolateral prefrontal cortex (anode) and the temporoparietal junction (cathode), areas associated with the pathophysiology of schizophrenia. The results were predominantly evaluated utilizing the Auditory Hallucination Rating Scale, a tool specifically designed for one of the most significant symptoms of schizophrenia (Table 1).
| Ref. | Year | Country | Sample size (T/C) | Electrode position | Stimulation intensity (mA × min) | Stimulation duration (days) | Stimulation frequency/day | Outcome measures |
| Bose et al[12] | 2018 | India | 62/13 | A: F3 FP1; C: T3 P3 | 2 × 20 | 5 | 2 | AHRS |
| Brunelin et al [13] | 2012 | France | 15/15 | A: F3 FP1; C: T3 P5 | 2 × 20 | 5 | 2 | AHRS |
| Chang et al [14] | 2018 | China | 30/30 | A: F3 FP1; C: T3 P7 | 2 × 20 | 5 | 2 | AHRS |
| Fröhlich et al [15] | 2016 | United States | 13/13 | A: F3 FP1; C: T3 P9 | 2 × 20 | 5 | 1 | AHRS |
| Kantrowitz et al [16] | 2019 | United States | 47/42 | A: F3 FP1; C: T3 P11 | 2 × 20 | 5 | 2 | AHRS |
| Koops et al [17] | 2018 | Norway | 26/18 | A: F3 FP1; C: T3 P13 | 2 × 20 | 5 | 2 | AHRS |
| Lindenmayer et al [18] | 2019 | United States | 15/13 | A: F3 FP1; C: T3 P15 | 2 × 20 | 20 | 2 | AHRS |
| Mondino et al [19] | 2016 | France | 45973 | A: F3 FP1; C: T3 P17 | 2 × 20 | 5 | 2 | AHRS |
| Valiengo et al [20] | 2020 | Brazil | 50/50 | A: F3 FP1; C: T3 P19 | 2 × 20 | 5 | 2 | AHRS |
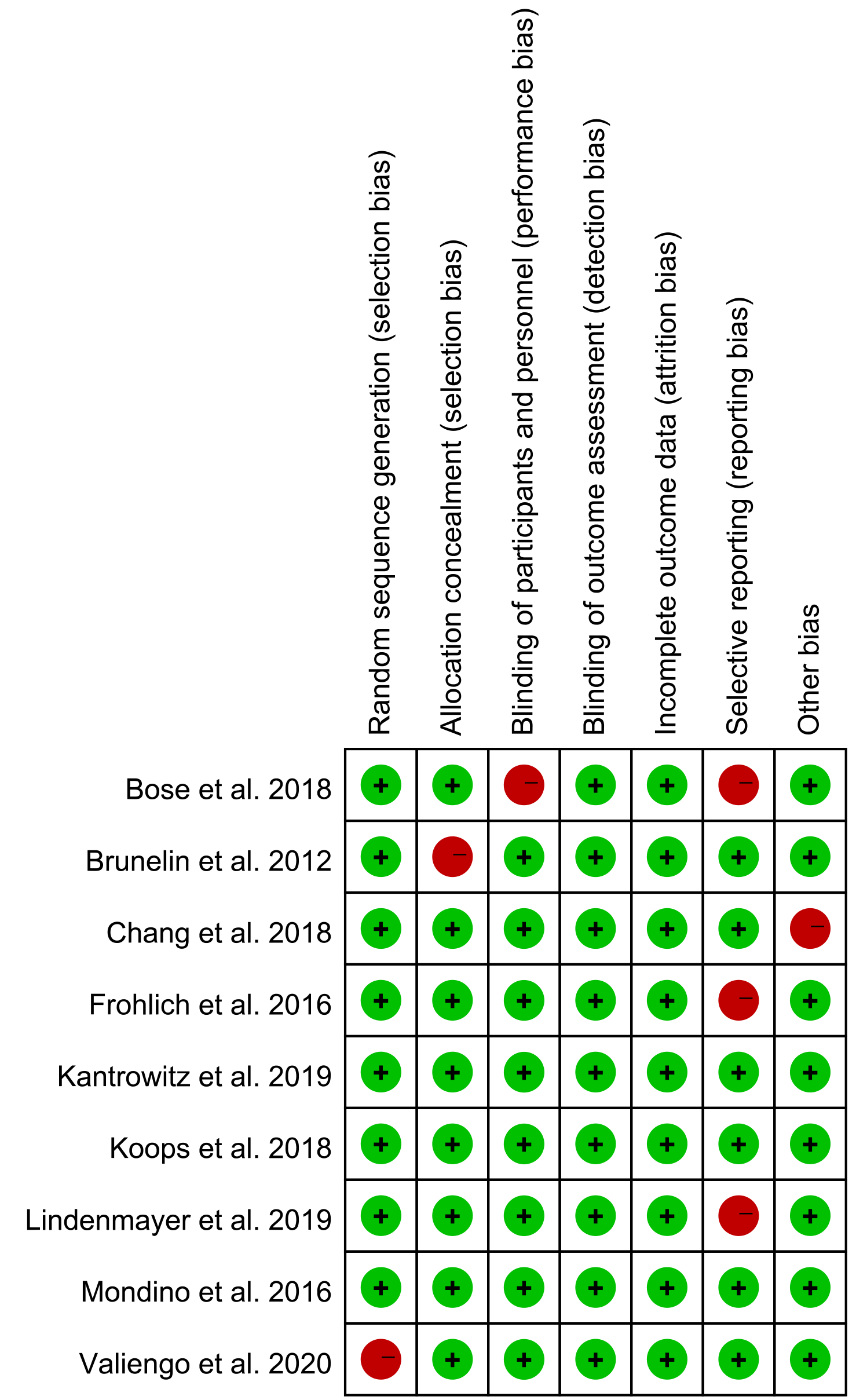
Our meta-analysis utilized the Cochrane risk of bias tool, which indicated that the majority of studies had a low risk in critical categories. The production of random sequences and allocation concealment were generally sufficient; nonetheless, few studies exhibited a lack of clarity, presenting a moderate risk of selection bias. Although the blinding of participants and professionals was inconsistent, potentially leading to performance bias, the blinding of outcome assessment was predominantly robust, indicating low detection bias. Attrition bias was minimal, with selective reporting almost nonexistent, suggesting dependable results. Nevertheless, other research indicated bias hazards, necessitating careful interpretation of the data (Figure 2).
The meta-analysis carefully assessed and integrated nine studies, demonstrating statistical heterogeneity (P = 0.092, I2 = 41.3%), which necessitated the application of a random-effects model for the study. The findings revealed a statistically significant disparity in auditory hallucination scores between the experimental group, which underwent tDCS, and the control group. The weighted mean difference (WMD) was -2.18, with a 95% confidence interval of -4.0 to -0.29, and a P value of less than 0.01, signifying that tDCS is an efficacious treatment for auditory hallucinations in individuals with schizophrenia. This effect size indicates a clinically significant decrease in the severity of auditory hallucinations, which are among the most disruptive and demanding symptoms for patients with schizophrenia. The statistical significance of these results highlights the possibility of tDCS as a therapeutic intervention (Figure 3).
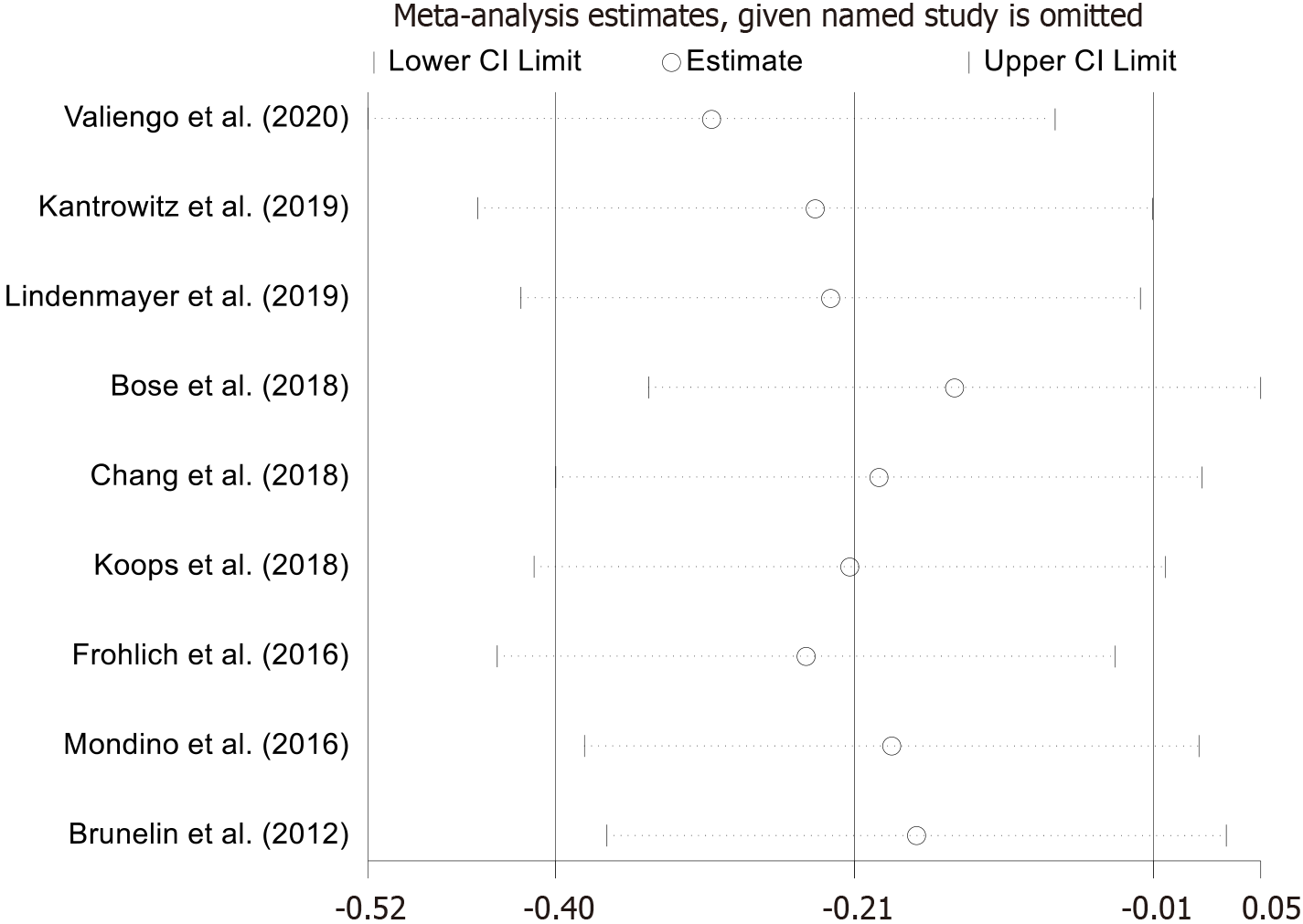
The meta-analysis conducted a sensitivity analysis to assess the robustness of the overall impact size, given the significant heterogeneity observed among the included studies. We sought to ascertain the impact of individual studies on the overall outcomes by methodically excluding each study from the pooled analysis and examining the resultant effect size. The outcomes of this method validated the consistency and reliability of the findings, with no individual study unduly influencing the meta-analytic summary. This enhances the trustworthiness of the aggregate data and fortifies the integrity of our conclusions. The consistent stability of these results, irrespective of the excluded study, confirms the robustness of the major outcomes demonstrated in this analysis (Figure 4).
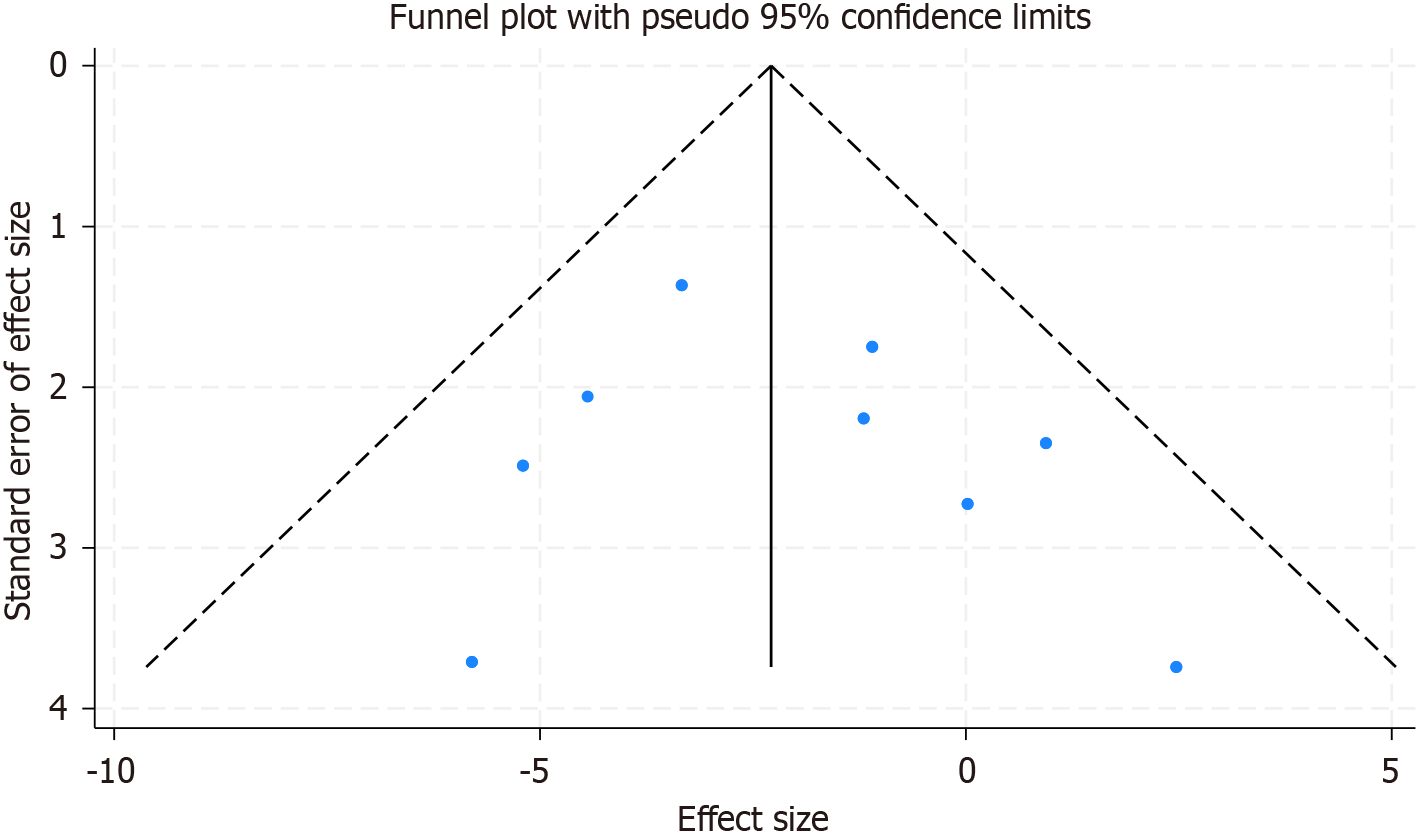
An assessment of publication bias was performed as part of our meta-analysis to guarantee the thoroughness and precision of the research results. Symmetrical funnel plots were created for the studies included, indicating a lack of publication bias upon eye examination (Figure 5). Additionally, Egger's linear regression test was utilized to objectively evaluate the existence of publication bias across many factors. The test outcomes indicated no substantial publication bias (P > 0.05 for all), so affirming the dependability of our meta-analytic findings.
Schizophrenia is a multifaceted psychiatric disorder characterized by positive, negative, and cognitive symptoms, with many patients showing inadequate response to conventional antipsychotics or suffering from severe side effects[21,22]. As a non-invasive neuromodulation technique, tDCS has emerged as a promising adjunctive therapy, particularly for refractory auditory hallucinations and cognitive impairments, by modulating cortical activity and promoting neuroplasticity[23,24]. This systematic review and meta-analysis aims to evaluate the efficacy of tDCS as a therapeutic modality for schizophrenia, clarifying its potential as a standalone or adjunctive treatment and informing future research. The results of this meta-analysis provide compelling evidence for the efficacy of tDCS as a therapeutic intervention for managing auditory hallucinations in schizophrenia. With a significant pooled effect size (WMD: -2.18), tDCS was shown to meaningfully reduce the severity of this debilitating symptom, which profoundly impacts patients' daily functioning and quality of life. Theoretically, our findings contribute to the growing body of neuromodulation research, demonstrating that tDCS modulates cortical excitability in key regions, such as the dorsolateral prefrontal cortex and temporoparietal junction, which are implicated in auditory perception disturbances. Practically, tDCS offers a non-invasive, safe alternative or adjunct to conventional pharmacotherapy, particularly for patients refractory to antipsychotics. Clinically, it provides a promising treatment with minimal side effects, enhancing the potential for improved outcomes and quality of life. Furthermore, the consistency and generalizability of these results across diverse study populations support tDCS as a viable, personalized treatment option in schizophrenia management.
The processes behind the efficacy of tDCS may be complex, according to its capacity to influence cortical excitability and connection. Neuroimaging research indicates that schizophrenia is linked to dysregulation in particular brain networks, including those involving the auditory cortex and the dorsolateral prefrontal cortex, which are regions associated with the pathophysiology of auditory hallucinations. tDCS, by administering a modest electrical current, may affect neuroplasticity in these regions, hence diminishing the abnormal neuronal activity that underlies hallucinations[25]. The neurological foundation of tDCS's effects may be elucidated by examining synaptic plasticity's involvement. tDCS may restore the equilibrium of excitatory and inhibitory neurotransmission in brain areas linked to schizophrenia by promoting long-term potentiation and long-term depression[26]. The alterations in synaptic efficiency may facilitate symptom alleviation and yield enduring effects beyond the stimulus duration.
The sensitivity analysis highlights the strength of our conclusions. By illustrating that the outcomes were not dependent on any one study, we validate the reliability of tDCS as an intervention across various research contexts and patient demographics. This consistency enhances the generalizability of our findings and indicates that tDCS may be advantageous for a wide array of patients experiencing auditory hallucinations. Publication bias, a common issue in meta-analyses, was mitigated using funnel plot analysis and Egger's regression test. The lack of substantial publication bias enhances the credibility of our research and indicates that our findings accurately reflect the existing evidence.
While this meta-analysis provides valuable insights into the potential of tDCS as a treatment for schizophrenia, several limitations must be acknowledged. First, the variability in tDCS protocols across studies, including differences in stimulation parameters, may affect the consistency and generalizability of the results. Additionally, small sample sizes in some studies limit statistical power, while short follow-up durations restrict our understanding of the long-term efficacy of tDCS. Furthermore, participant heterogeneity in terms of medication status and disease stage could have influenced treatment outcomes, highlighting the need for more controlled research in this area. Another significant limitation is the inconsistency in electrode positioning, which is crucial for the targeted brain regions and the effectiveness of tDCS. Variations in electrode placement could lead to stimulation of different brain areas, contributing to heterogeneity in treatment outcomes. Our meta-analysis did not account for these variations, which may impact the reliability of the findings. Future studies should aim to standardize tDCS protocols, including electrode positioning, to ensure more reliable and comparable results. Additionally, research should focus on elucidating the neural mechanisms underlying tDCS effects, establishing optimal stimulation parameters, and exploring the long-term impact of tDCS on symptom reduction. Addressing these gaps will strengthen the evidence base for tDCS as a therapeutic intervention for schizophrenia and guide its integration into multimodal treatment strategies.
This meta-analysis indicates that tDCS effectively reduces auditory hallucinations in schizophrenia, showing promise as an adjunct to pharmacotherapy. While short-term benefits are evident, long-term efficacy and sustainability remain unclear. Future research should optimize stimulation parameters, assess broader symptom impacts, and evaluate cost-effectiveness. Despite promising results, limitations such as small sample sizes and methodological variability highlight the need for further high-quality, large-scale trials to confirm tDCS’s role in clinical practice.
We thank the study participants for their invaluable contributions and support.
| 1. | Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, Malaspina D, Owen MJ, Schultz S, Tsuang M, Van Os J, Carpenter W. Definition and description of schizophrenia in the DSM-5. Schizophr Res. 2013;150:3-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 444] [Article Influence: 37.0] [Reference Citation Analysis (0)] |
| 2. | Gebreegziabhere Y, Habatmu K, Mihretu A, Cella M, Alem A. Cognitive impairment in people with schizophrenia: an umbrella review. Eur Arch Psychiatry Clin Neurosci. 2022;272:1139-1155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 126] [Article Influence: 42.0] [Reference Citation Analysis (0)] |
| 3. | Lefaucheur JP, Antal A, Ayache SS, Benninger DH, Brunelin J, Cogiamanian F, Cotelli M, De Ridder D, Ferrucci R, Langguth B, Marangolo P, Mylius V, Nitsche MA, Padberg F, Palm U, Poulet E, Priori A, Rossi S, Schecklmann M, Vanneste S, Ziemann U, Garcia-Larrea L, Paulus W. Evidence-based guidelines on the therapeutic use of transcranial direct current stimulation (tDCS). Clin Neurophysiol. 2017;128:56-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 829] [Cited by in RCA: 1198] [Article Influence: 133.1] [Reference Citation Analysis (0)] |
| 4. | Gupta T, Kelley NJ, Pelletier-Baldelli A, Mittal VA. Transcranial Direct Current Stimulation, Symptomatology, and Cognition in Psychosis: A Qualitative Review. Front Behav Neurosci. 2018;12:94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Lindenmayer JP, Fitapelli B. Noninvasive direct current stimulation for schizophrenia: a review. Curr Opin Psychiatry. 2021;34:253-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Moffa AH, Brunoni AR, Nikolin S, Loo CK. Transcranial Direct Current Stimulation in Psychiatric Disorders: A Comprehensive Review. Psychiatr Clin North Am. 2018;41:447-463. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Zhang R, Ren J, Zhang C. Efficacy of transcranial alternating current stimulation for schizophrenia treatment: A systematic review. J Psychiatr Res. 2023;168:52-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Mondino M, Janin D, Galvao F, Brunelin J. High-Frequency Transcranial Random Noise Stimulation for Auditory Hallucinations of Schizophrenia: A Case Series. Biomedicines. 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Jiang WL, Cai DB, Sun CH, Yin F, Goerigk S, Brunoni AR, Zhao XW, Mayes TL, Zheng W, Xiang YT. Adjunctive tDCS for treatment-refractory auditory hallucinations in schizophrenia: A meta-analysis of randomized, double-blinded, sham-controlled studies. Asian J Psychiatr. 2022;73:103100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 10. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 40406] [Article Influence: 10101.5] [Reference Citation Analysis (2)] |
| 11. | Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA; Cochrane Bias Methods Group; Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18487] [Cited by in RCA: 24818] [Article Influence: 1772.7] [Reference Citation Analysis (3)] |
| 12. | Bose A, Shivakumar V, Agarwal SM, Kalmady SV, Shenoy S, Sreeraj VS, Narayanaswamy JC, Venkatasubramanian G. Efficacy of fronto-temporal transcranial direct current stimulation for refractory auditory verbal hallucinations in schizophrenia: A randomized, double-blind, sham-controlled study. Schizophr Res. 2018;195:475-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 13. | Brunelin J, Mondino M, Gassab L, Haesebaert F, Gaha L, Suaud-Chagny MF, Saoud M, Mechri A, Poulet E. Examining transcranial direct-current stimulation (tDCS) as a treatment for hallucinations in schizophrenia. Am J Psychiatry. 2012;169:719-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 374] [Article Influence: 28.8] [Reference Citation Analysis (0)] |
| 14. | Chang CC, Tzeng NS, Chao CY, Yeh CB, Chang HA. The Effects of Add-on Fronto-Temporal Transcranial Direct Current Stimulation (tDCS) on Auditory Verbal Hallucinations, Other Psychopathological Symptoms, and Insight in Schizophrenia: A Randomized, Double-Blind, Sham-Controlled Trial. Int J Neuropsychopharmacol. 2018;21:979-987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 15. | Fröhlich F, Burrello TN, Mellin JM, Cordle AL, Lustenberger CM, Gilmore JH, Jarskog LF. Exploratory study of once-daily transcranial direct current stimulation (tDCS) as a treatment for auditory hallucinations in schizophrenia. Eur Psychiatry. 2016;33:54-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 16. | Kantrowitz JT, Sehatpour P, Avissar M, Horga G, Gwak A, Hoptman MJ, Beggel O, Girgis RR, Vail B, Silipo G, Carlson M, Javitt DC. Significant improvement in treatment resistant auditory verbal hallucinations after 5 days of double-blind, randomized, sham controlled, fronto-temporal, transcranial direct current stimulation (tDCS): A replication/extension study. Brain Stimul. 2019;12:981-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 17. | Koops S, Blom JD, Bouachmir O, Slot MI, Neggers B, Sommer IE. Treating auditory hallucinations with transcranial direct current stimulation in a double-blind, randomized trial. Schizophr Res. 2018;201:329-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Lindenmayer JP, Kulsa MKC, Sultana T, Kaur A, Yang R, Ljuri I, Parker B, Khan A. Transcranial direct-current stimulation in ultra-treatment-resistant schizophrenia. Brain Stimul. 2019;12:54-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 19. | Mondino M, Jardri R, Suaud-Chagny MF, Saoud M, Poulet E, Brunelin J. Effects of Fronto-Temporal Transcranial Direct Current Stimulation on Auditory Verbal Hallucinations and Resting-State Functional Connectivity of the Left Temporo-Parietal Junction in Patients With Schizophrenia. Schizophr Bull. 2016;42:318-326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 145] [Cited by in RCA: 150] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 20. | Valiengo LDCL, Goerigk S, Gordon PC, Padberg F, Serpa MH, Koebe S, Santos LAD, Lovera RAM, Carvalho JB, van de Bilt M, Lacerda ALT, Elkis H, Gattaz WF, Brunoni AR. Efficacy and Safety of Transcranial Direct Current Stimulation for Treating Negative Symptoms in Schizophrenia: A Randomized Clinical Trial. JAMA Psychiatry. 2020;77:121-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 85] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 21. | Stępnicki P, Kondej M, Kaczor AA. Current Concepts and Treatments of Schizophrenia. Molecules. 2018;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 323] [Article Influence: 46.1] [Reference Citation Analysis (1)] |
| 22. | Marder SR, Umbricht D. Negative symptoms in schizophrenia: Newly emerging measurements, pathways, and treatments. Schizophr Res. 2023;258:71-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 43] [Reference Citation Analysis (0)] |
| 23. | Herrera-Melendez AL, Bajbouj M, Aust S. Application of Transcranial Direct Current Stimulation in Psychiatry. Neuropsychobiology. 2020;79:372-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 24. | Nieuwdorp W, Koops S, Somers M, Sommer IE. Transcranial magnetic stimulation, transcranial direct current stimulation and electroconvulsive therapy for medication-resistant psychosis of schizophrenia. Curr Opin Psychiatry. 2015;28:222-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 25. | Chhabra H, Shivakumar V, Agarwal SM, Bose A, Venugopal D, Rajasekaran A, Subbanna M, Kalmady SV, Narayanaswamy JC, Debnath M, Venkatasubramanian G. Transcranial direct current stimulation and neuroplasticity genes: implications for psychiatric disorders. Acta Neuropsychiatr. 2016;28:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Koops S, van den Brink H, Sommer IE. Transcranial direct current stimulation as a treatment for auditory hallucinations. Front Psychol. 2015;6:244. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |