Published online Mar 19, 2025. doi: 10.5498/wjp.v15.i3.99152
Revised: November 20, 2024
Accepted: December 30, 2024
Published online: March 19, 2025
Processing time: 139 Days and 20.1 Hours
Effective health management for high-risk stroke populations is essential. The hospital-community-home (HCH) collaborative health management (CHM) model leverages resources from hospitals, communities, and families. By inte
To explore the effects of the HCH-CHM model on stroke risk reduction in high-risk populations.
In total, 110 high-risk stroke patients screened in the community from January 2019 to January 2023 were enrolled, with 52 patients in the control group receiving routine health education and 58 in the observation group receiving HCH-CHM model interventions based on routine health education. Stroke awareness scores, health behavior levels, medication adherence, blood pressure, serum biochemical markers (systolic/diastolic blood pressure, total cholesterol, and triglyceride), and psychological measures (self-rating anxiety/depression scale) were evaluated and compared between groups.
The observation group showed statistically significant improvements in stroke awareness scores and health behavior levels compared to the control group (P < 0.05), with notable enhancements in lifestyle and dietary habits (P < 0.05) and reductions in postintervention systolic blood pressure, diastolic blood pressure, total cholesterol, triglyceride, self-rating anxiety scale, and self-rating depression scale scores (P < 0.05).
The HCH-CHM model had a significant positive effect on high-risk stroke populations, effectively increasing disease awareness, improving health behavior and medication adherence, and appropriately ameliorating blood pressure, serum biochemical marker levels, and negative psychological symptoms.
Core Tip: High-risk stroke groups often present with obesity, advanced age, multiple comorbidities, low disease awareness, and limited prevention and treatment knowledge. They also suffer considerable burden from the disease. Hence, timely and effective health management interventions are essential. This study examines the impact of the hospital-community-family collaborative health management model on individuals at high-risk for stroke. Compared with routine health education, the hospital-community-family collaborative health management model demonstrates a substantial intervention effect, effectively raising patients’ disease awareness, enhancing their health behaviors and medication adherence, and improving their blood pressure, serum biochemical marker levels, and psychological well-being. These findings offer valuable insights and new strategies for optimizing the management of high-risk stroke populations.
- Citation: Wang J, Zhao CX, Tian J, Li YR, Ma KF, Du R, Li MK, Hu R. Effect of hospital-community-home collaborative health management on symptoms, cognition, anxiety, and depression in high-risk individuals for stroke. World J Psychiatry 2025; 15(3): 99152
- URL: https://www.wjgnet.com/2220-3206/full/v15/i3/99152.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i3.99152
Stroke, or ischemia apoplexy, is typically ischemic (up to 87%) and ranks as the second leading cause of disability and death globally[1]. The disease is preventable, with declining risks of new occurrences and recurrences, and targeted changes in risk factors, such as smoking, obesity, overeating, malnutrition, and inactivity, can have a meaningful preventive effect[2,3]. In 2020, stroke affected nearly 20 million adults in China, resulting in almost 2.5 million deaths. This not only had major physical and mental impacts on patients but also increased the medical burden on patients and their families[4]. Generally, prevention is considered more effective than treatment for stroke, and providing effective, scientific health management can optimize patient management and outcomes[5]. Additionally, high-risk populations for stroke are often characterized by obesity, advanced age, multiple comorbidities, and limited awareness of the disease and its prevention, underscoring the need for timely and effective health management interventions[6,7].
Health management is a proactive strategy that facilitates the development of scientific and individualized health plans for patients based on disease risk factors and previous case data, helping to prevent or delay disease progression by improving habits and behaviors[8,9]. Currently, health management is applied across various medical scenarios to aid prevention and treatment. For example, health education for patients with diabetic foot has improved their un
This retrospective study enrolled 110 high-risk stroke patients screened from the community between January 2019 and January 2023. Patients were grouped based on health education intervention methods, with 52 patients in the control group receiving only routine health education, and 58 patients in the observation group receiving the HCH-CHM model intervention based on routine health education.
High-risk stroke patients identified through echocardiography or carotid ultrasound examination were enrolled[16]. These individuals presented with hypertension, diabetes, and dyslipidemia, with a smoking history (either continuous smoking or cumulative smoking for 6 months or longer), a family or previous history of stroke, prior transient ischemic attacks, and atrial fibrillation. They were also classified as significantly overweight or obese and exhibited a lack of physical activity. Excluded patients included those with impaired mobility or on long-term bed rest; aphasia, attention disturbances, or swallowing disorders; mental illness; an inability to participate in health management owing to environmental, physical, or mental conditions; pregnant or lactating women; cognitive dysfunction or communication barriers; and those severely ill or requiring critical care.
The control group received routine health education as follows: (1) Creating basic patient information files; (2) In
In addition, to these measures, the observation group received further intervention via the HCH-CHM model, as follows: (1) A multidisciplinary health management team was established, comprising the hospital, community medical institutions, and families, with 10 medical staff from the community service center and 6 hospital chief physicians. The community service center was responsible for health management, and hospital doctors provided relevant technical guidance and answered questions during the management process; (2) To enable HCH-collaborative stroke health risk assessments, hospital physicians managed quality control, and community healthcare workers conducted residents’ health risk assessments. These assessments covered patient information, lifestyle, family history of stroke, and relevant physical and laboratory tests. Family members helped patients develop action plans and provided timely feedback to medical staff; (3) The HCH-collaborative health education intervention was implemented by establishing comprehensive electronic information files and conducting monthly face-to-face follow-ups through home visits. Interventions were tailored to patients’ situations to monitor blood pressure and other indicators and assess risk factors. Family members were guided to support patients in health management, encouraging healthy lifestyle changes and providing targeted health education; (4) Patient management was reinforced using the regional intelligent reporting management system for disease control and prevention, promoting five major prescriptions and providing individual counseling to explain health management and stroke self-management methods, facilitating dynamic personalized health management; and (5) Face-to face follow-ups were enhanced through outpatient services, home and telephone visits, and online communication, collecting data on residents’ living conditions, symptoms, medication use, and cardiocerebrovascular events. Using follow-up and risk assessment data, patients received individualized guidance on knowledge, skills, and psychological counseling to promote healthier lifestyles and disease prevention.
Stroke awareness: Patients’ awareness of stroke prevention was assessed with the stroke prevention knowledge questionnaire, covering risk factors, prevention knowledge, early symptom recognition, and emergency treatment. The questionnaire has 20 items (5 per dimension) with a total score of 100, where higher scores indicate better stroke prevention awareness.
Healthy behavior: Patient’s health behavior levels were evaluated using the Health-Promoting Lifestyle Profile, which includes subscales for health responsibility, exercise, nutrition, stress management, interpersonal relationships, and self-actualization, totaling 52 items. Responses were rated on a four-point scale, including “never” (1 point), “sometimes” (2 points), “always” (3 points), and “all the time” (4 points), with higher scores indicating better health behavior.
Standardized medication use: Adherence to prescribed antiplatelet drugs (APDs), statins, antihypertensive drugs (AHTDs), and hypoglycemic agents was evaluated.
Blood pressure and serum biochemical indices: Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured before and after the intervention using a blood pressure monitor. Additionally, fasting venous blood (3 mL) collected before and after intervention was centrifuged for serum analysis, measuring total cholesterol (TC) and triglyceride (TG) levels with an automatic biochemical analyzer.
Psychological emotions: Patients’ anxiety and depression levels were assessed before and after the intervention using the self-rating anxiety scale (SAS) and self-rating depression scale (SDS). Each scale includes 20 items, with a total score of 80, where higher scores indicate greater anxiety and depression severity.
The measurement data were described using mean ± SE, and between-group and within-group comparisons were conducted using independent sample t-tests and paired t-tests, respectively. Categorical data were presented as ratios (percentage), with comparisons between groups made using the χ2-test. The collected experimental data were analyzed using SPSS 21.0, with statistical significance reported at the P < 0.05 Level.
We comparatively analyzed patients’ general data, including age, sex, weight, education level, and the presence of hypertension, diabetes, and hyperlipidemia. We found no significant between-group differences (P > 0.05, Table 1).
| Patient data | Control group (n = 52) | Observation group (n = 58) | χ2/t | P value |
| Age, years | 59.27 ± 9.45 | 61.29 ± 10.73 | 1.043 | 0.300 |
| Sex | 0.736 | 0.391 | ||
| Male | 29 (55.77) | 37 (63.79) | ||
| Female | 23 (44.23) | 21 (36.21) | ||
| Weight, kg | 58.69 ± 8.69 | 59.67 ± 9.18 | 0.573 | 0.568 |
| Educational level | 0.666 | 0.717 | ||
| Junior high school and below | 14 (26.92) | 12 (20.69) | ||
| Senior high school | 22 (42.31) | 28 (48.28) | ||
| University or above | 16 (30.77) | 18 (31.03) | ||
| Hypertension | 2.628 | 0.105 | ||
| With | 30 (57.69) | 42 (72.41) | ||
| Without | 22 (42.31) | 16 (27.59) | ||
| Diabetes | 1.014 | 0.314 | ||
| With | 15 (28.85) | 22 (37.93) | ||
| Without | 37 (71.15) | 36 (62.07) | ||
| Hyperlipidemia | 0.822 | 0.365 | ||
| With | 26 (50.00) | 24 (41.38) | ||
| Without | 26 (50.00) | 34 (58.62) |
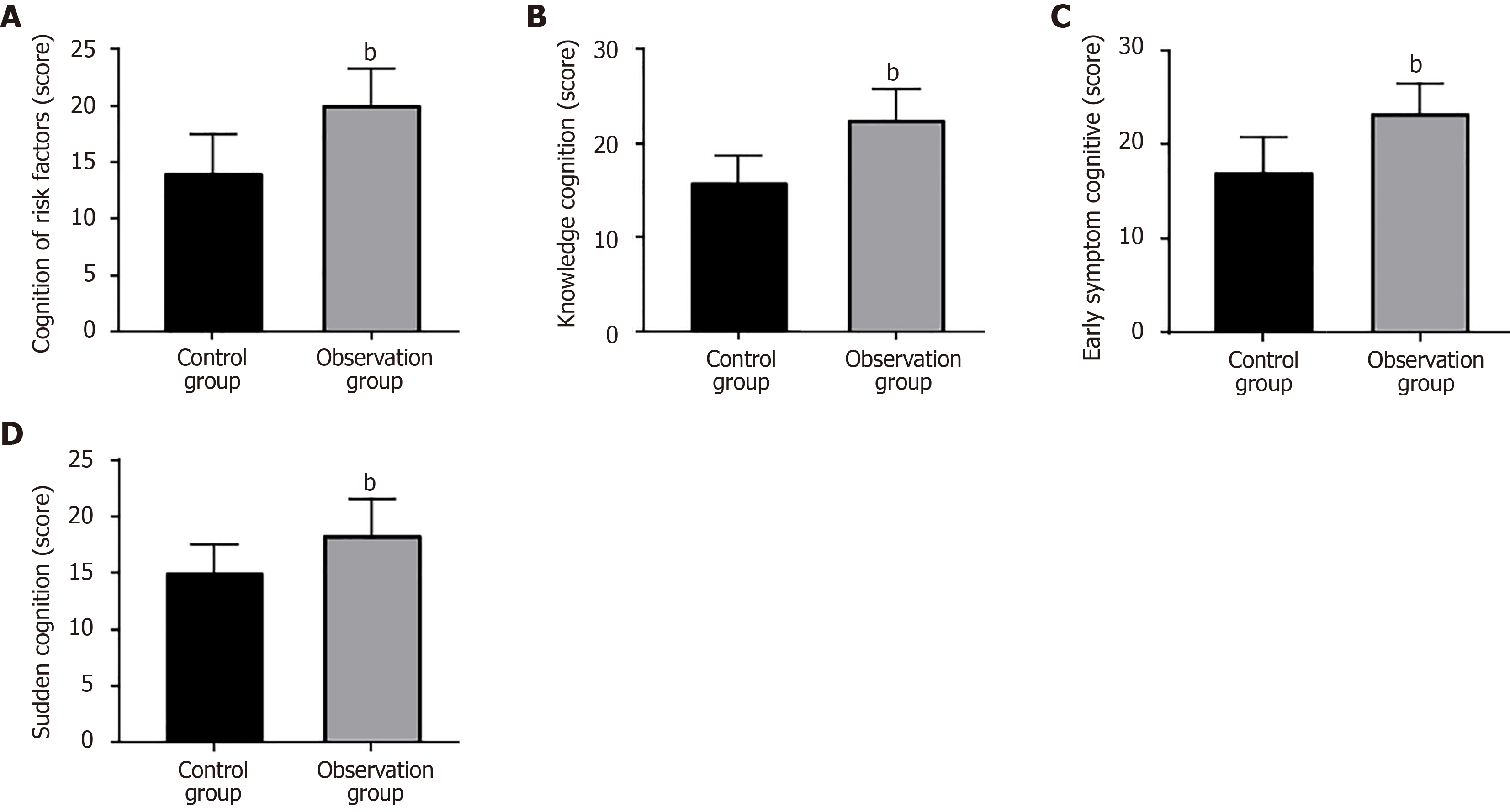
We evaluated the impact of the two intervention methods on disease awareness in high-risk stroke populations, focusing on risk factor knowledge, prevention knowledge, early symptom recognition, and emergency treatment. The observation group scored higher across all these areas, with statistically significant differences (P < 0.05, Figure 1 and Table 2).
| Dimensions | Control group (n = 52) | Observation group (n = 58) | t | P value |
| Risk factor cognition | 13.96 ± 3.51 | 19.9 ± 3.38 | 9.036 | < 0.001 |
| Prevention knowledge cognition | 15.75 ± 2.93 | 22.36 ± 3.39 | 10.880 | < 0.001 |
| Early symptom cognition | 16.94 ± 3.84 | 23.14 ± 3.25 | 9.169 | < 0.001 |
| Emergency treatment cognition | 14.90 ± 2.58 | 18.19 ± 3.31 | 5.766 | < 0.001 |
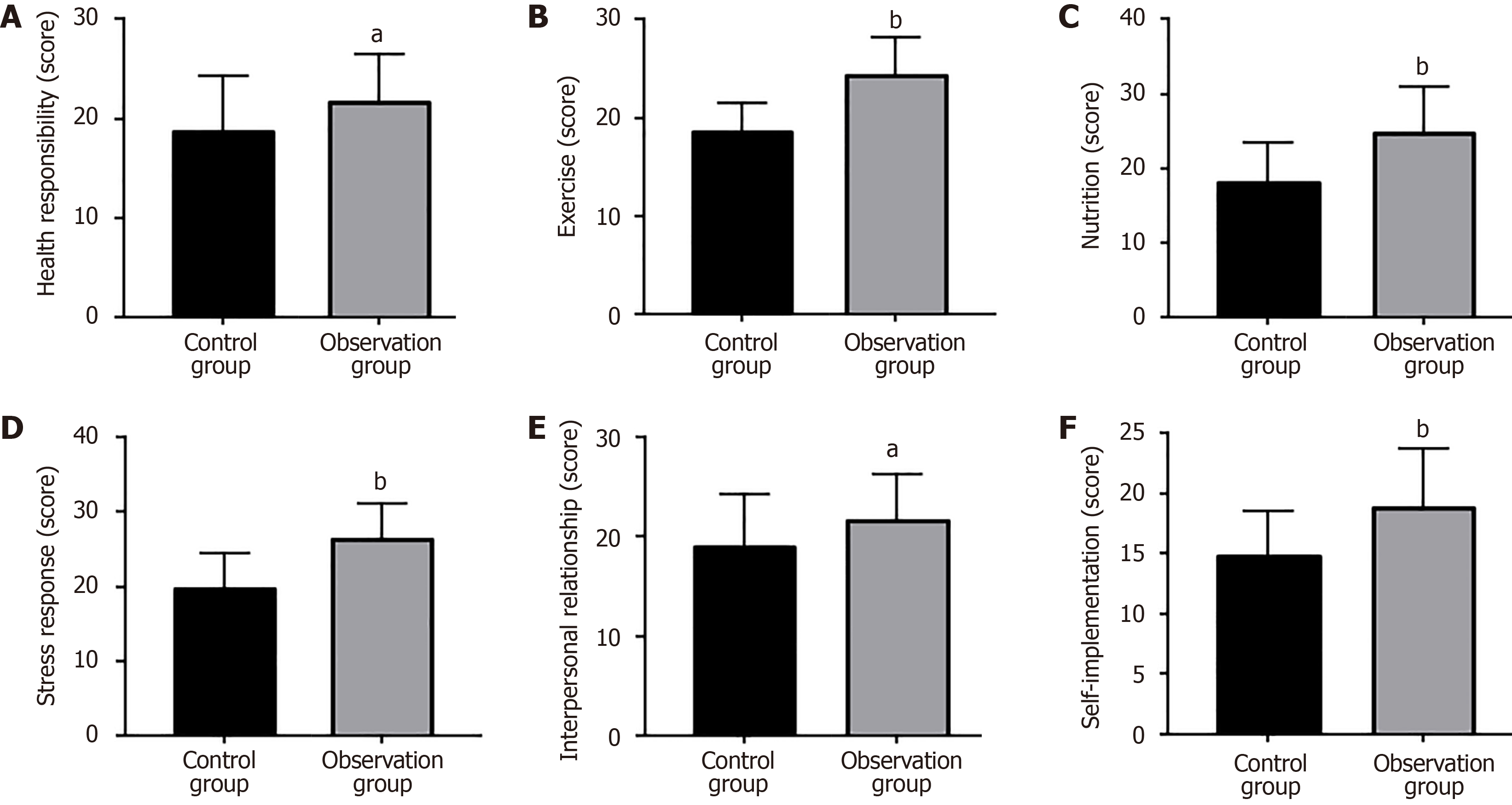
The influence of the two management models on health behaviors in high-risk stroke patients was assessed across six domains: Health responsibility, exercise, nutrition, stress management, interpersonal relationships, and self-actualization. The observation group scored significantly higher than the control group in all domains (P < 0.05, Figure 2 and Table 3).
| Dimensions | Control group (n = 52) | Observation group (n = 58) | t | P value |
| Health responsibility | 18.67 ± 5.68 | 21.60 ± 4.84 | 2.920 | 0.004 |
| Exercise | 18.60 ± 2.97 | 24.38 ± 3.78 | 8.846 | < 0.001 |
| Nutrition | 18.12 ± 5.38 | 24.71 ± 6.17 | 5.939 | < 0.001 |
| Stress management | 19.79 ± 4.71 | 26.33 ± 4.72 | 7.263 | < 0.001 |
| Interpersonal relationships | 19.04 ± 5.30 | 21.69 ± 4.62 | 2.802 | 0.006 |
| Self-actualization | 14.73 ± 3.80 | 18.81 ± 4.90 | 4.839 | < 0.001 |
We assessed the effectiveness of the two management models on patients’ standardized use of APDs, statins, AHTDs, and hypoglycemic agents. The observation group showed significantly better standardized medication adherence across all categories compared to the control group (P < 0.05, Table 4).
| Standardized medication | Control group (n = 52) | Observation group (n = 58) | χ2 | P value |
| Antiplatelet drugs | 42 (80.77) | 55 (94.83) | 5.200 | 0.023 |
| Statins | 40 (76.92) | 54 (93.10) | 5.775 | 0.016 |
| Antihypertensive drugs | 41 (78.85) | 57 (98.28) | 10.650 | 0.001 |
| Hypoglycemic agents | 42 (80.77) | 56 (96.55) | 7.027 | 0.008 |
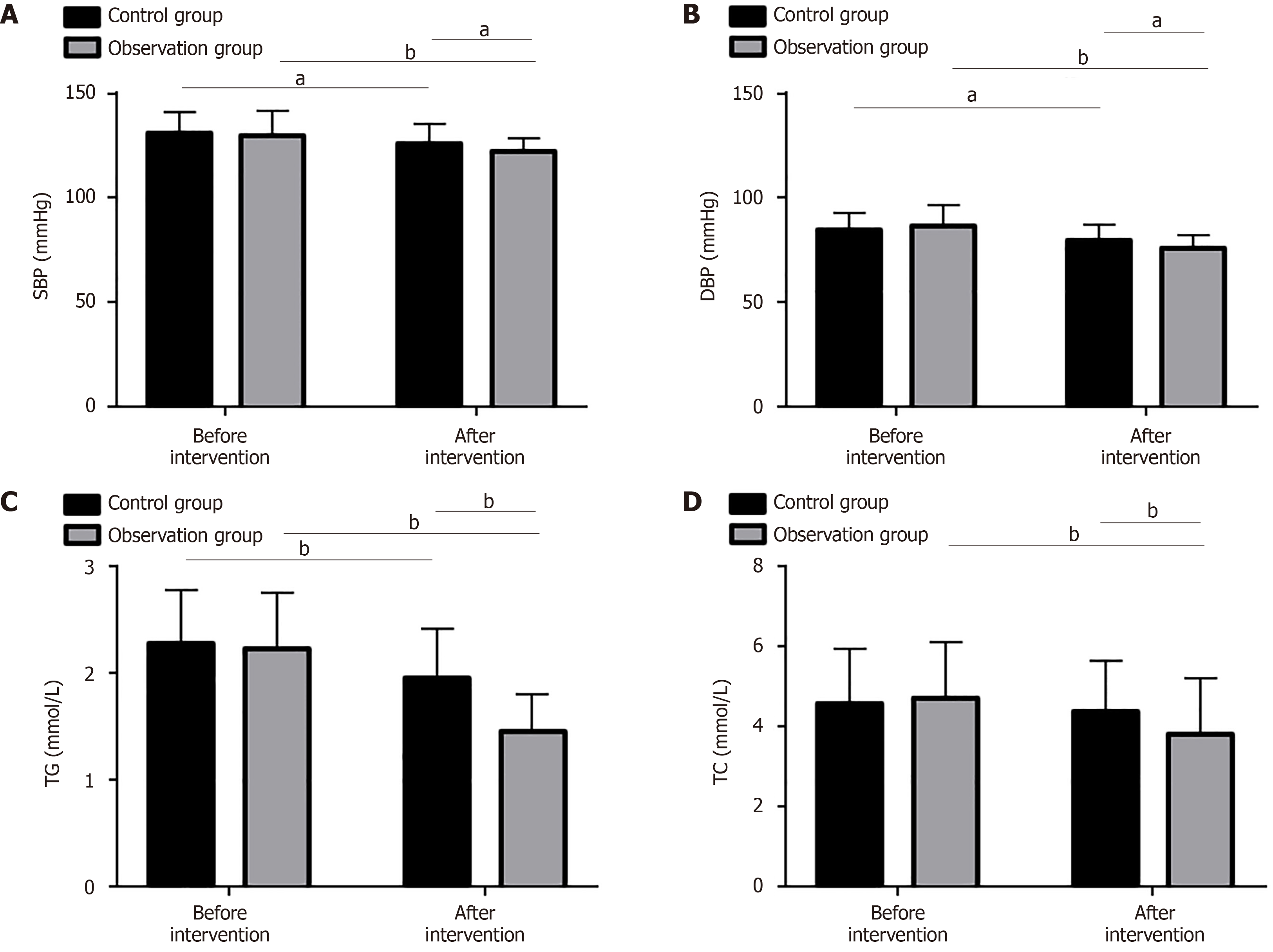
We investigated the effects of the two management interventions on blood pressure and serum biochemical indices, measuring SBP, DBP, TG, and TC levels in both groups. No significant between-group differences were noted before intervention. After intervention, the observation group showed statistically significant reductions in SBP, DBP, TG, and TC levels, which were lower than those in the control group (P < 0.05, Figure 3 and Table 5).
| Indicators | Control group (n = 52) | Observation group (n = 58) | t | P value |
| SBP | ||||
| Before intervention | 130.83 ± 10.53 | 129.57 ± 12.31 | 0.574 | 0.568 |
| After intervention | 125.87 ± 9.70 | 122.41 ± 6.26 | 2.245 | 0.027 |
| DBP | ||||
| Before intervention | 84.87 ± 8.13 | 86.52 ± 9.92 | 0.947 | 0.346 |
| After intervention | 79.54 ± 7.66 | 76.03 ± 6.22 | 2.649 | 0.009 |
| TG | ||||
| Before intervention | 2.28 ± 0.50 | 2.23 ± 0.52 | 0.513 | 0.609 |
| After intervention | 1.95 ± 0.46 | 1.45 ± 0.35 | 6.454 | < 0.001 |
| TC | ||||
| Before intervention | 4.58 ± 1.37 | 4.72 ± 1.39 | 0.531 | 0.597 |
| After intervention | 4.38 ± 1.27 | 3.80 ± 1.40 | 2.266 | 0.025 |
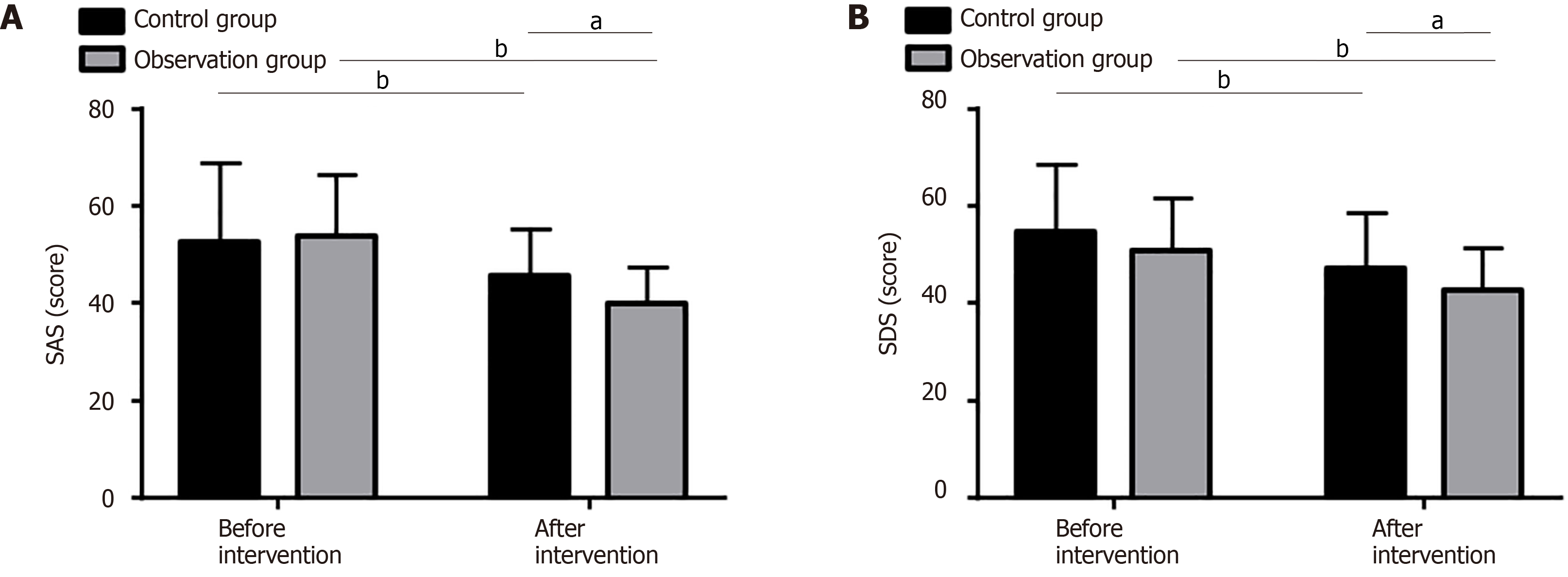
Psychological and emotional changes in the two high-risk groups were evaluated using the SAS and SDS scales. No significant between-group differences were found before intervention (P > 0.05). However, postintervention scores on both scales decreased significantly, with the observation group showing even lower SAS and SDS scores (P < 0.05, Figure 4 and Table 6).
| Indicators | Control group (n = 52) | Observation group (n = 58) | t | P value |
| SAS score | ||||
| Before intervention | 52.58 ± 16.35 | 53.74 ± 12.70 | 0.418 | 0.677 |
| After intervention | 45.58 ± 9.69 | 39.76 ± 7.60 | 3.523 | < 0.001 |
| SDS score | ||||
| Before intervention | 54.77 ± 13.81 | 50.74 ± 10.89 | 1.708 | 0.091 |
| After intervention | 46.96 ± 11.61 | 42.47 ± 8.82 | 2.298 | 0.024 |
As a sudden cerebrovascular disease, stroke has a high rate of disability and mortality[17,18]. This study focused on high-risk stroke populations, analyzing the influence of the HCH-CHM model on this group to provide insights for the clinical management of patients with elevated stroke risk.
Regarding disease awareness, the observation group showed significantly higher scores compared with the control group in areas such as risk factor knowledge, prevention knowledge, early symptom recognition, and emergency treatment awareness. This suggests that the HCH-CHM model effectively enhances disease awareness across these areas, likely attributed to its integration of health risk assessment and follow-up data, which guides patients in disease knowledge and skills[19]. Similarly, research by Shi et al[20] demonstrated that the HCH-CHM model effectively raised disease awareness among patients with hypertension, lowering their blood pressure and reducing anxiety and de
In terms of standardized medication adherence, the observation group demonstrated significantly better adherence to APDs, statins, AHTDs, and hypoglycemic agents compared with the control group, showing the HCH-CHM model’s efficacy in promoting standardized medication use among high-risk stroke populations. Gao et al[23] also reported that the HCH-CHM model significantly improved medication compliance in children with epilepsy, consistent with our findings. In the comparative analysis of blood pressure and serum biochemical indices, we found that postintervention levels of SBP, DBP, TG, and TC in the observation group were significantly lower than those in the control group, suggesting that the HCH-CHM model effectively improves blood pressure and serum indices, aiding in restoring metabolic balance in high-risk patients. The HCH-CHM model’s ability to help establish comprehensive electronic patient files holding pathological data and monitor biochemical indices contributes to timely and targeted interventions, leading to scientific management of these indices[24]. Research by Guo et al[25] showed that HCH-CHM intervention signi
From a psychological perspective, the observation group’s SAS and SDS scores decreased markedly after intervention, being lower than those in the control group, thereby highlighting the HCH-CHM model’s positive impact on alleviating negative emotions in high-risk stroke populations. This effect may stem from the model’s emphasis on psychological support from the multidisciplinary health management team and families. Feng et al[26] also found that using the HCH-CHM model in home rehabilitation for disabled elderly patients with stroke improved medical compliance and alleviated negative emotions, aligning with our results. Additionally, the HCH-CHM model combined with motor imagery therapy has shown major benefits in motor function, balance, daily living activities, and quality of life in patients with cerebral infarction[27].
This study has several limitations. First, its single-center design may limit the applicability of the results to other healthcare environments or patient demographics. Future multicenter studies could help validate these findings across diverse populations and settings. Second, the study did not include long-term follow-up data, which could further clarify the HCH-CHM model’s long-term clinical benefits. Finally, additional data on factors such as sleep and quality of life would expand our understanding of the HCH-CHM model’s potential clinical advantages. Future research will address these areas to further enhance the current findings.
In conclusion, the HCH-CHM model demonstrates strong intervention effects in high-risk stroke populations by improving disease awareness, enhancing health behaviors, supporting standardized medication use, effectively regulating blood pressure and serum biochemical indices, and alleviating negative emotions. These results offer valuable insights for optimizing the management of high-risk stroke populations.
| 1. | Saini V, Guada L, Yavagal DR. Global Epidemiology of Stroke and Access to Acute Ischemic Stroke Interventions. Neurology. 2021;97:S6-S16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 560] [Article Influence: 140.0] [Reference Citation Analysis (0)] |
| 2. | Guzik A, Bushnell C. Stroke Epidemiology and Risk Factor Management. Continuum (Minneap Minn). 2017;23:15-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 213] [Article Influence: 26.6] [Reference Citation Analysis (0)] |
| 3. | Aigner A, Grittner U, Rolfs A, Norrving B, Siegerink B, Busch MA. Contribution of Established Stroke Risk Factors to the Burden of Stroke in Young Adults. Stroke. 2017;48:1744-1751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 161] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 4. | Tu WJ, Wang LD; Special Writing Group of China Stroke Surveillance Report. China stroke surveillance report 2021. Mil Med Res. 2023;10:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 206] [Article Influence: 103.0] [Reference Citation Analysis (0)] |
| 5. | Oh CW, Lee SH, Nam TM, Jang JH, Kim YZ, Kim KH, Kim DH, Ko NG, Kim SH. Comparative Analysis of Stroke Patients with and without Sequelae: A Cross-Sectional Analysis Using the KOREA National Health and Nutrition Examination Survey (2016-2019). J Clin Med. 2021;10:4122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 6. | Li RC, Xu WD, Lei YL, Bao T, Yang HW, Huang WX, Tang HR. The risk of stroke and associated risk factors in a health examination population: A cross-sectional study. Medicine (Baltimore). 2019;98:e17218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Wang H, Wu M, Tu Q, Li M. Risk factors for stroke in a population of central China: A cross-sectional study. Medicine (Baltimore). 2022;101:e31946. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 8. | Melchart D, Eustachi A, Wellenhofer-Li Y, Doerfler W, Bohnes E. Individual Health Management - A Comprehensive Lifestyle Counselling Programme for Health Promotion, Disease Prevention and Patient Education. Forsch Komplementmed. 2016;23:30-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Stonbraker S, Richards S, Halpern M, Bakken S, Schnall R. Priority Topics for Health Education to Support HIV Self-Management in Limited-Resource Settings. J Nurs Scholarsh. 2019;51:168-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Makiling M, Smart H. Patient-Centered Health Education Intervention to Empower Preventive Diabetic Foot Self-care. Adv Skin Wound Care. 2020;33:360-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Bezerra PMM, Vieira TI, Dos Santos FG, Ribeiro ILA, de Sousa SA, Valença AMG. The impact of oral health education on the incidence and severity of oral mucositis in pediatric cancer patients: a systematic review and meta-analysis. Support Care Cancer. 2022;30:8819-8829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Chang HL, Huang HL, Chung YC. [Effects of a Hybrid Health Education Program on Pain and Knee Angle in Elderly Patients After Total Knee Replacement Surgery]. Huli Zazhi. 2023;70:45-55. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Paluch AE, Bajpai S, Ballin M, Bassett DR, Buford TW, Carnethon MR, Chernofsky A, Dooley EE, Ekelund U, Evenson KR, Galuska DA, Jefferis BJ, Kong L, Kraus WE, Larson MG, Lee IM, Matthews CE, Newton RL Jr, Nordström A, Nordström P, Palta P, Patel AV, Pettee Gabriel K, Pieper CF, Pompeii L, Rees-Punia E, Spartano NL, Vasan RS, Whincup PH, Yang S, Fulton JE; Steps for Health Collaborative. Prospective Association of Daily Steps With Cardiovascular Disease: A Harmonized Meta-Analysis. Circulation. 2023;147:122-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 60] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 14. | Flach C, Muruet W, Wolfe CDA, Bhalla A, Douiri A. Risk and Secondary Prevention of Stroke Recurrence: A Population-Base Cohort Study. Stroke. 2020;51:2435-2444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 199] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 15. | Mazurek MO, Parker RA, Chan J, Kuhlthau K, Sohl K; ECHO Autism Collaborative. Effectiveness of the Extension for Community Health Outcomes Model as Applied to Primary Care for Autism: A Partial Stepped-Wedge Randomized Clinical Trial. JAMA Pediatr. 2020;174:e196306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 16. | Wang Y, Han S, Qin H, Zheng H, Jiang B, Cao Y, Gao Y, Guan L, Jia Q, Jiang Y, Jiao Y, Li S, Li Y, Li Z, Liu W, Ru X, Sun D, Sun H, Wang P, Wang T, Zong L, Guo L, Xie X, Xu Y, Xu Y, Yang X, Yang Y, Zhou M, Wang W; Chinese Stroke Association Stroke Council Guideline Writing Committee. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of the management of high-risk population. Stroke Vasc Neurol. 2020;5:270-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | Boursin P, Paternotte S, Dercy B, Sabben C, Maïer B. [Semantics, epidemiology and semiology of stroke]. Soins. 2018;63:24-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 18. | Hong C, Pencina MJ, Wojdyla DM, Hall JL, Judd SE, Cary M, Engelhard MM, Berchuck S, Xian Y, D'Agostino R Sr, Howard G, Kissela B, Henao R. Predictive Accuracy of Stroke Risk Prediction Models Across Black and White Race, Sex, and Age Groups. JAMA. 2023;329:306-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 45] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 19. | Han Y, Hu Y, Yu C, Guo Y, Pei P, Yang L, Chen Y, Du H, Sun D, Pang Y, Chen N, Clarke R, Chen J, Chen Z, Li L, Lv J; China Kadoorie Biobank Collaborative Group. Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur Heart J. 2021;42:3374-3384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 211] [Article Influence: 52.8] [Reference Citation Analysis (0)] |
| 20. | Shi W, Cheng L, Li Y. Influence of "Hospital-Community-Family" Integrated Management on Blood Pressure, Quality of Life, Anxiety and Depression in Hypertensive Patients. Comput Math Methods Med. 2022;2022:1962475. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 21. | Lo SHS, Chang AM, Chau JPC. Stroke Self-Management Support Improves Survivors' Self-Efficacy and Outcome Expectation of Self-Management Behaviors. Stroke. 2018;49:758-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 54] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 22. | Jiang J, Gu X, Cheng CD, Li HX, Sun XL, Duan RY, Zhu Y, Sun L, Chen FK, Bao ZY, Zhang Y, Shen JH. The Hospital-Community-Family-Based Telemedicine (HCFT-AF) Program for Integrative Management of Patients With Atrial Fibrillation: Pilot Feasibility Study. JMIR Mhealth Uhealth. 2020;8:e22137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Gao Y, Tang X, Wen Y, Qian D, Pan X, Zhang L. Effects of the hospital-community-family ternary linkage continuous nursing model on compliance, cognitive function, resilience, and quality of life for children with epilepsy: a retrospective study. Transl Pediatr. 2022;11:239-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 24. | Felton WL 3rd, Kornstein SG, Gondwe T, Huynh C, Wallenborn JT, Henry J. Evaluation of an Electronic Health Record Alert to Improve Screening and Management of Cardiovascular Disease and Stroke Factors in a High-Risk Population. South Med J. 2022;115:232-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 25. | Guo L, Zhang M, Namassevayam G, Wei M, Zhang G, He Y, Guo Y, Liu Y. Effectiveness of health management among individuals at high risk of stroke: An intervention study based on the health ecology model and self-determination theory (HEM-SDT). Heliyon. 2023;9:e21301. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 26. | Feng W, Yu H, Wang J, Xia J. Application effect of the hospital-community integrated service model in home rehabilitation of stroke in disabled elderly: a randomised trial. Ann Palliat Med. 2021;10:4670-4677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 27. | Li WW, Li M, Guo XJ, Liu FD. Application of a hospital-community-family trinity rehabilitation nursing model combined with motor imagery therapy in patients with cerebral infarction. World J Clin Cases. 2023;11:621-628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |