Published online Mar 19, 2025. doi: 10.5498/wjp.v15.i3.103252
Revised: January 6, 2025
Accepted: January 18, 2025
Published online: March 19, 2025
Processing time: 82 Days and 19.4 Hours
Postpartum stress urinary incontinence (SUI) symptoms affect a patient’s daily activities and quality of life and increase the negative emotions that they experience. At present, there is no research on the effect of fractional CO2 laser treatment combined with Kegel exercise on postpartum SUI and postpartum depression and anxiety.
To investigate the effect of lattice CO2 laser treatment combined with Kegel exercise on mild to moderate postpartum SUI and its influence on postpartum depression and anxiety.
Using a retrospective study, data from 82 cases of mild to moderate postpartum SUI in Huzhou Maternal & Child Health Care Hospital from January to April 2024 were retrospectively collected. The cases were divided into groups according to the different treatment methods, namely Group S (41 cases, only receiving lattice CO2 laser treatment) and Group L (41 cases, receiving lattice CO2 laser combined with Kegel exercise treatment). The baseline data of the two groups were compared. In addition, we analyzed and compared the scores of the international commission on urinary incontinence questionnaire short form (ICI-Q-SF), incontinence quality of life questionnaire (I-QOL), Edinburgh postnatal depression scale (EPDS), and postpartum specific anxiety scale (PSAS) before treatment, at the end of treatment, and 3 months after the end of treatment between the two groups. Furthermore, the clinical efficacy and adverse reactions of the two groups were analyzed and compared at the end of treatment and 3 months after the end of treatment.
There was no significant difference in the baseline data and the ICI-Q-SF, I-QOL, EPDS, and PSAS scores between the two groups before treatment. However, at the end of treatment, the ICI-Q-SF, I-QOL, EPDS, and PSAS scores between Groups L and S were significantly different. The overall effective rate of treatment in Group L was significantly higher than that in Group S. During the 3-month follow-up after treatment, it was found that the ICI-Q-SF, EPDS, and PSAS scores of Group L were still lower than those of Group S. In comparison, the I-QOL score and total effective rate of treatment were still higher in Group L than those in Group S, and this difference was significant. There was no significant difference in the adverse reactions between Group L and Group S.
The combination of dot lattice CO2 laser and Kegel exercise has a significant therapeutic effect on mild to moderate postpartum SUI. It can prolong the duration of therapeutic effects, improve a patient’s quality of life, and alleviate postpartum depression and anxiety.
Core Tip: Postpartum stress urinary incontinence (SUI) has a serious impact on women's lives and work, resulting in many women suffering from postpartum depression and anxiety due to the symptoms of postpartum SUI. This study focuses on the increase of Kegel exercise in combination with fractional CO2 laser treatment, which was found to prolong the duration of the treatment effects on postpartum SUI and play a positive role in alleviating postpartum depression and anxiety in patients.
- Citation: Lou ZX, Huang SY, Wan ZQ, Chen Y, Shan HY, Wang LY. Effect of lattice CO2 laser combined with Kegel exercise mild moderate stress urinary incontinence and postpartum depression anxiety. World J Psychiatry 2025; 15(3): 103252
- URL: https://www.wjgnet.com/2220-3206/full/v15/i3/103252.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i3.103252
Postpartum stress urinary incontinence (SUI) is caused by an increase in hormone levels during pregnancy and the excessive expansion of the pelvic floor during vaginal delivery, which results in the weakening of urethral and pelvic floor support and reduction of urinary control[1]. Postpartum SUI is mainly characterized by the involuntary outflow of urine from the urethral opening during prolonged standing or walking, running, coughing, or sneezing. This can seriously impact a woman’s postpartum quality of life and work. As a result, many women who are affected by postpartum SUI experience postpartum depression, anxiety, and other negative emotions[2].
When the vaginal wall is irradiated by a laser, it can stimulate the regeneration of elastic fibers and collagen, reconstruct the pelvic floor structure, and thereby provide better support for the urethra. At the same time, laser treatment has the advantage of being rapid and minimally invasive, and patients with SUI experience fewer adverse reactions in the treatment of vaginal relaxation, atrophy, and pelvic organ prolapse[3]. The CO2 laser with a wavelength of 10600 nm is a common type of lattice laser that is used. Previous studies have found that lattice CO2 laser treatment can promote collagen synthesis, reshape pelvic connective tissue, and restore pelvic tissue function[4]. However, over time its effectiveness decreases, and it is usually necessary to repeat laser treatment every six months to one year to consolidate the laser treatment effectiveness. This undoubtedly inconveniences patients to a certain extent. If other non-surgical treatments can be used to consolidate the treatment effect, it can save the patient the cost of one laser treatment.
Kegel exercises (pelvic movement, pelvic floor muscle training) are a first-line non-surgical intervention for postpartum SUI. After correctly mastering the training techniques, patients can exercise at home on their own. Its efficacy is closely related to the standard, compliance, and cooperation of training[5]. However, Kegel exercises that are incorrectly performed may lead to the worsening of postpartum SUI symptoms and the occurrence of pain[6], thereby increasing the pain and psychological burden of patients. Therefore, in this study, when patients with mild to moderate postpartum SUI were treated with CO2 laser once a month at the hospital, medical staff guided them to correctly perform Kegel exercises.
This study analyzes the therapeutic effect of dot matrix CO2 laser treatment combined with Kegel exercise on mild to moderate postpartum SUI. We also explore its influence on postpartum depression and anxiety in patients to provide more options for the clinical treatment of postpartum SUI.
This was a retrospective study that collected data from 82 cases of mild to moderate postpartum SUI in Huzhou Maternal & Child Health Care Hospital from January to April 2024. The cases were divided according to the different treatment methods, namely, Group S and Group L. Group S was treated solely with lattice CO2 laser therapy, and Group L was treated with lattice CO2 laser combined with Kegel exercise; there are 41 cases in each group.
The inclusion criteria were as follows: (1) Singleton was full-term and delivered vaginally; (2) Follow-up from six months to one year postpartum revealed SUI in line with the mild to moderate diagnostic criteria[7], i.e., there was no urine leakage under normal conditions, but there was involuntary urine outflow when the abdominal pressure suddenly increased, such as sneezing and coughing. According to the grading results of a 1 hour urine pad test, mild included 2 g ≤ urine leakage < 5 g, and moderate was 5 g ≤ urine leakage < 10 g; (3) No contraindications for laser therapy; (4) Good compliance and normal cognition; and (5) The patient provided written informed consent.
The exclusion criteria were as follows: (1) There was severe perineal injury present; (2) An incomplete pelvic floor structure; (3) The existence of reproductive tract tumors; (4) The presence of infectious diseases, such as vaginitis and urinary tract infection; (5) Severe mental disorders; (6) Previous history of pelvic floor and pelvic surgery; and (7) Individuals who terminate or change the treatment plan during the research process.
Patients in Group S were treated with lattice CO2 laser therapy. Experienced medical personnel operated the dot lattice CO2 laser therapy device (HL-1G, Beijing Hertz Medical Technology Co., Ltd.) for laser treatment. The machine parameter settings were: A single pulse mode was adopted, with a low energy level and 80-120 mJ/pixel (depending on the patient’s comfort level), a laser wavelength of 10600 nm, a spot diameter of 75-100 μm, and a spot density of 3.6%-6.4%. The specific operation steps were as follows: The patient assumed the lithotomy position, and after routine disinfection, a dry cotton ball was used to keep the vagina dry. A 360-degree laser hand tool sleeve was gently inserted into the vagina until there was resistance-i.e., it reached the cervix-and then stopped. Thereafter the laser was engaged and a pulse emitted, pulled back 1 cm, and emitted again; this was repeated until the hand tool was retracted to the vaginal orifice. The above operation was performed twice. Using a 45-degree laser hand tool, the previous operation on the anterior wall of the vagina was reinforced. Laser treatment was performed once a month for three sessions, with the entire treatment course lasting for three months. After each treatment, sexual activity should be prohibited for one week, and vigorous exercise should be avoided.
Patients in Group L received lattice CO2 laser treatment in the hospital and were guided by medical staff to perform the Kegel exercise. First, the patient was provided with a Kegel exercise manual and allowed to complete various training exercises by watching the Kegel exercise manual on-site and following live-action demonstrations to guide their movements. For example: Guide the patient to choose the correct sitting, lying, or standing posture, ensuring that they are in a comfortable position and keeping their body relaxed, especially their pelvic floor muscles. Guide the patient to correctly locate the pelvic floor muscles and emphasize normal breathing, specifically to avoid holding their breath and not inhaling or exhaling vigorously. The patients were guided to concentrate on completing the combined exercise of levator ani and relaxation, where relaxation was performed 4-6 seconds after each levator ani to contract the pelvic floor muscles. In addition, in the process of trying to urinate, the patients were guided to suddenly stop, keep the contraction state for a few seconds, and then gradually increase the retention time, from the initial few seconds to more than 10 seconds, and then slowly relax the pelvic floor muscles. Guide patients to perform the entire training process with deep breathing. In the hospital, medical staff are able to supervise and correct patients’ incorrect movements; however, when the patient returns home, they perform the exercise according to the voice training version provided by the hospital. Medical personnel followed up via telephone or WeChat group inquiries and supervised the patient to perform three Kegel exercise sessions at home every day (divided into early, middle, and late timeslots); each session was performed for not less than 30 min, and the whole treatment course consisted of 3 months. After the patient completed the treatment course, the patient was encouraged to continue performing appropriate Kegel exercises at home.
Each indicator was evaluated before treatment, at the end of treatment (completion of the entire course of treatment), and 3 months after the end of treatment: (1) Clinical effect: The international commission on urinary incontinence questionnaire short form (ICI-Q-SF) was used to evaluate the patients’ urinary incontinence symptoms. The scale includes the frequency, amount, and impact of urinary leakage on daily life, with a total score of 21 points. The higher the score, the more severe the urinary incontinence symptoms[8]; The urinary incontinence quality of life questionnaire (I-QOL) was used to evaluate the patient’s quality of life. The questionnaire includes behavioral restrictions, psychological influences, and social disorders, with a total of 22 items across 3 criteria. The total score was calculated as (total score-22)/88 × 100, and the higher the score, the better the quality of life[9]; Efficacy assessment[10], i.e., Significantly effective: The patient has no urinary leakage when standing, walking, coughing, or sneezing and the urinary incontinence symptoms have disappeared; Effective: The patient’s urinary leakage symptoms have been reduced, and the frequency of urinary incontinence has decreased by more than 50% compared to before treatment; and Invalid: There was no significant change in the patient’s urinary leakage symptoms, and the reduction in urinary incontinence frequency does not exceed 50% compared to before treatment. Total effective rate (%) = (number of Significantly Effective cases + number of Effective cases)/total cases × 100; (2) Postpartum depression: The Edinburgh postnatal depression scale (EPDS) was used to evaluate the postpartum depression status of patients. The scale includes 10 items with a total score ranging from 0-30, where the higher the score, the more severe the postpartum depression[11]; (3) Postpartum anxiety: The postnatal specific anxiety scale (PSAS) was used to evaluate the patient’s postpartum anxiety status. The scale includes 51 items with a total score ranging from 51-204 points. The higher the score, the more severe the postpartum anxiety level[12]; and (4) Adverse reactions: The incidence of adverse reactions during the treatment and follow-up period was recorded and counted. These mainly included vaginal bleeding, sexual intercourse pain, vulvar pruritus, increased secretion, urgent urinary incontinence, etc.
Statistical analysis was performed using SPSS 27.0 software, and the measurement data was first verified using the S-W method to conform to normal distribution. Data are expressed as the mean ± SD, and two groups were compared using a t-test. Count data was expressed as a percentage, and comparisons between the two groups were performed using the χ2 test. Differences with a P < 0.05 were considered statistically significant.
The age, body mass index, education level, fertility history, and postpartum SUI severity of the two groups were analyzed and compared. The results revealed no statistically significant differences (P > 0.05) (Table 1).
| Baseline data | Group S (n = 41) | Group L (n = 41) | t/χ2 value | P value |
| Age (years) | 28.19 ± 3.25 | 28.34 ± 3.39 | 0.205 | 0.838 |
| Body mass index (kg/m2) | 23.45 ± 2.61 | 23.86 ± 2.83 | 0.682 | 0.497 |
| Degree of education | 0.201 | 0.645 | ||
| High school or below | 16 (60.98) | 18 (43.90) | ||
| College degree or above | 25 (39.02) | 23 (56.10) | ||
| Reproductive history | 0.195 | 0.659 | ||
| Primipara | 22 (53.66) | 20 (48.78) | ||
| Multipara | 19 (46.34) | 21 (51.22) | ||
| Severity of postpartum SUI | 0.210 | 0.647 | ||
| Slight | 27 (65.85) | 25 (60.98) | ||
| Moderate | 14 (34.15) | 16 (39.02) |
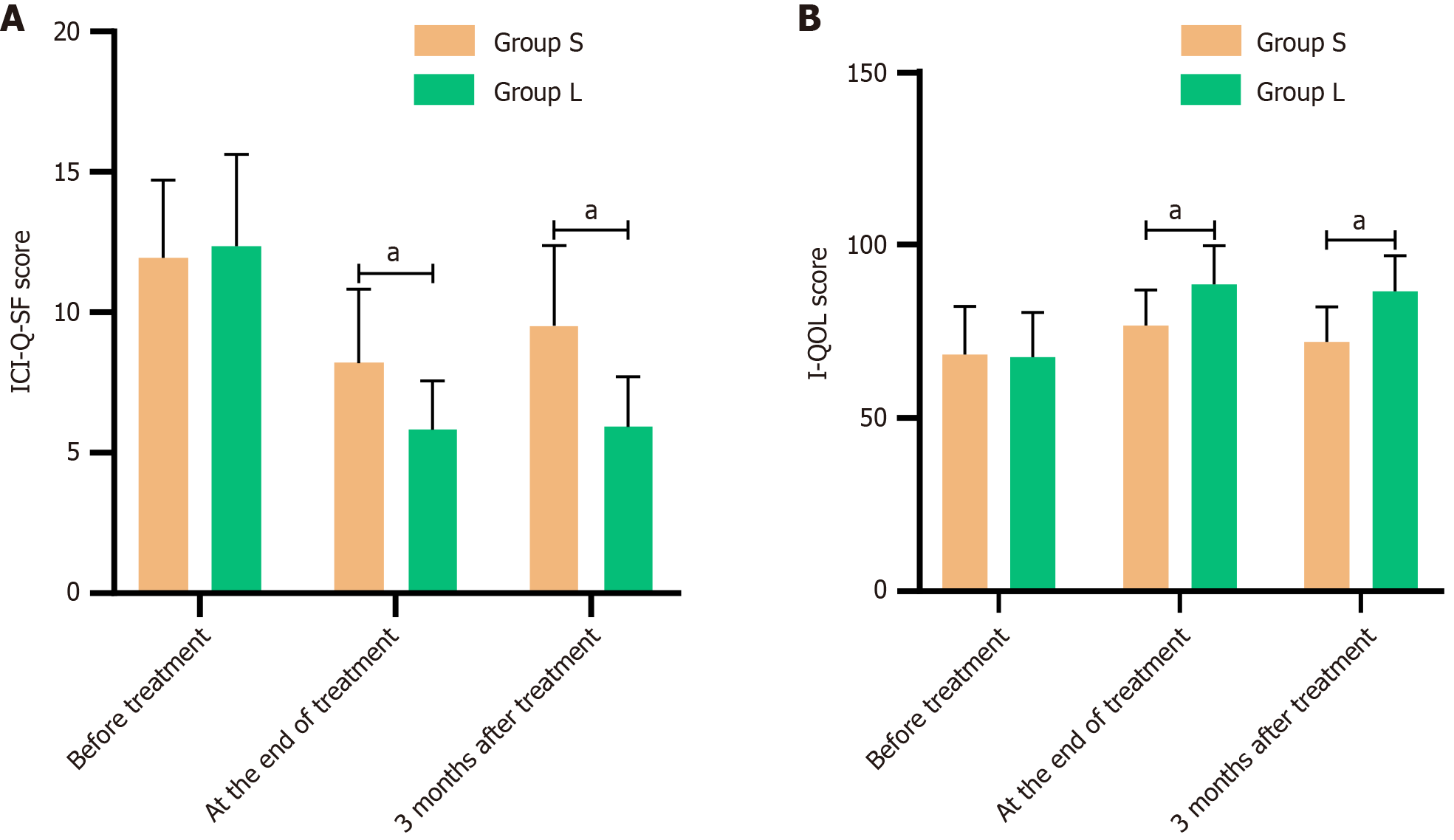
For the comparison of the ICI-Q-SF and I-QOL scores between Group L and Group S before treatment, the difference was not statistically significant (P > 0.05). However, at the end of treatment, the ICI-Q-SF score of Group L was lower than that of Group S, while the I-QOL score was higher than that of Group S, and these differences were statistically significant (P < 0.05). Three months after the end of treatment, the ICI-Q-SF score of Group L was still lower than that of Group S, and the I-QOL score remained higher than that of Group S, and these differences were also statistically significant (P < 0.05) (Table 2 and Figure 1).
| Group | n | ICI-Q-SF scores | I-QOL scores | ||||
| Before treatment | At the end of treatment | 3 months after treatment | Before treatment | At the end of treatment | 3 months after treatment | ||
| Group S | 41 | 11.94 ± 2.76 | 8.19 ± 2.63 | 9.53 ± 2.85 | 68.32 ± 13.91 | 76.64 ± 10.32 | 71.98 ± 10.05 |
| Group L | 41 | 12.35 ± 3.28 | 5.82 ± 1.74 | 5.92 ± 1.79 | 67.56 ± 12.85 | 88.58 ± 11.16 | 86.59 ± 10.16 |
| t value | 0.612 | 4.812 | 6.868 | 0.257 | 5.034 | 6.546 | |
| P value | 0.541 | < 0.001 | < 0.001 | 0.798 | < 0.001 | < 0.001 | |
The total effective rate at the end of treatment in Group L was significantly higher than that in Group S (P < 0.05). Furthermore, the maintenance rate of the total effective rate in Group L remained significantly higher than that in Group S 3 months after the end of treatment (P < 0.05) (Table 3).
| Group | n | At the end of treatment | Total efficiency | 3 months after treatment | Total efficiency | ||||
| Significant effect | Effective | Invalid | Significant effect | Effective | Invalid | ||||
| Group S | 41 | 15 (36.58) | 13 (31.71) | 13 (31.71) | 28 (68.29) | 13 (31.71) | 12 (29.27) | 16 (39.02) | 25 (60.98) |
| Group L | 41 | 21 (51.22) | 15 (36.59) | 5 (12.19) | 36 (87.81) | 21 (51.22) | 13 (31.71) | 7 (17.07) | 34 (82.93) |
| χ2 value | 1.783 | 0.217 | 4.556 | 4.556 | 3.216 | 0.058 | 4.895 | 4.895 | |
| P value | 0.182 | 0.641 | 0.033 | 0.033 | 0.076 | 0.81 | 0.027 | 0.027 | |
For the comparison of the EPDS and PSAS scores between Group L and Group S before treatment, the difference was not statistically significant (P > 0.05). However, at the end of treatment, the EPDS and PSAS scores of Group L were significantly lower than those of Group S, and the differences were statistically significant (P < 0.05). Three months after the end of treatment, the EPDS and PSAS scores of Group L were also significantly lower than those of Group S, and the differences were statistically significant (P < 0.05) (Table 4 and Figure 2).
| Group | n | EPDS scores | PSAS scores | ||||
| Before treatment | At the end of treatment | 3 months after treatment | Before treatment | At the end of treatment | 3 months after treatment | ||
| Group S | 41 | 9.89 ± 2.64 | 8.46 ± 1.35 | 8.65 ± 1.46 | 141.92 ± 27.85 | 92.57 ± 17.83 | 96.95 ± 18.16 |
| Group L | 41 | 9.94 ± 2.72 | 7.49 ± 1.08 | 7.51 ± 1.17 | 143.18 ± 26.96 | 71.63 ± 15.92 | 73.82 ± 16.73 |
| t value | 0.084 | 3.593 | 3.902 | 0.208 | 5.609 | 5.998 | |
| P value | 0.933 | 0.001 | < 0.001 | 0.836 | < 0.001 | < 0.001 | |
There were six instances of adverse reactions in Group L during the treatment process and 3 months after the end of treatment, including one case of dyspareunia, three cases of vulva pruritus, and two cases of urgent urinary incontinence. There were eight incidents of adverse reactions in Group S during the treatment process and 3 months after the end of treatment, including one case of vaginal bleeding, two cases of dyspareunia, two cases of vulva pruritus, two cases of increased secretion, and one case of urgent urinary incontinence. In the comparison of the incidence of adverse reactions between the two groups, the difference was not statistically significant (P > 0.05) (Table 5).
| Group | n | Vaginal bleeding | Coital pain | Vulvar itching | Increased secretion | Urge incontinence |
| Group S | 41 | 1 (2.44) | 2 (4.88) | 2 (4.88) | 2 (4.88) | 1 (2.44) |
| Group L | 41 | 0 (0.00) | 1 (2.44) | 3 (7.32) | 0 (0.00) | 2 (4.88) |
| χ2 value | 1.012 | 0.346 | 0.213 | 2.635 | 0.346 | |
| P value | 0.314 | 0.556 | 0.644 | 0.105 | 0.556 |
Postpartum SUI is a common pelvic floor muscle dysfunction that can seriously impact a woman’s physical and mental health[13]. At present, in clinical practice, it is widely believed that postpartum SUI mainly originates from the traction of the pelvic floor structure during the delivery of the fetus by the mother, as well as the mechanical compression on the pelvic floor tissues caused by factors such as weight gain and uterine enlargement during pregnancy that can result in pelvic floor relaxation[14]. Furthermore, this can lead to weakened support around the urethra, reducing the ability to control urine flow, which ultimately results in urinary incontinence[15]. Therefore, taking effective measures to improve a patient’s pelvic floor muscle strength is an important measure to alleviate SUI symptoms.
The main component of the pelvic floor support structure is collagen. Previous studies have shown that, during pregnancy, changes in hormone levels in women can reduce the metabolism of connective tissue and decrease the production of collagen. This affects the function of the detrusor or pelvic floor muscles and urethral stability to an extent, thereby promoting the development of SUI[16]. Therefore, reconstructing pelvic floor collagen can help improve pelvic floor muscle strength, maintain the detrusor or pelvic floor muscles and urethra stability, and improve postpartum SUI symptoms in women. The photothermal effect of dot lattice CO2 laser technology can stimulate the production of heat shock protein factors and promote collagen production through laser emission energy. It can reshape vaginal connective tissue and increase the contraction force of vaginal epithelial collagen fibers and urethral support without damaging the vaginal connective tissue, thereby improving urethral closure pressure and alleviating postpartum SUI symptoms[17]. Alcalay et al[18] performed dot lattice CO2 laser therapy on 52 patients with mild to moderate SUI and found through follow-up that dot matrix CO2 laser therapy effectively improved patients’ clinical symptoms and vaginal tissue composition and structure, but it lacked a corresponding control group. Behnia-Willison et al[19] evaluated the SUI-related symptoms of 58 female patients before and after lattice CO2 laser treatment, and 80% of participants exhibited an improvement in symptoms after completing three laser treatments. However, during the follow-up evaluation, it was found that the treatment effect was slightly weakened. Dabaja et al[20] found that the ICI-Q-SF scores of patients with SUI showed significant improvement after lattice CO2 laser treatment but returned to baseline levels 6 months after treatment. This suggests that the duration of the treatment effect using dot lattice CO2 laser therapy alone to treat postpartum SUI is not long.
Kegel exercise can effectively improve the strength and control ability of pelvic floor muscles, enhance the urethral sphincter contraction function, increase bladder closure, and have a therapeutic effect on postpartum urinary incontinence, urinary frequency, urinary urgency, and other symptoms[21]. This study used a combination of lattice CO2 laser and Kegel exercise therapy (Group L) to treat patients with mild to moderate postpartum SUI and compared the results to patients who received lattice CO2 laser therapy alone (Group S) as a control. The results showed that the ICI-Q-SF score in Group L was significantly lower than that in Group S at the end of treatment, while the I-QOL score was significantly higher than that in Group S, and the overall effective rate of clinical treatment was higher than that of Group S. Furthermore, the ICI-Q-SF score of Group L remained lower than that of Group S, and the I-QOL score was still higher than that of Group S 3 months after the end of treatment, indicating that the overall clinical effect remained good. This demonstrates that the combination of lattice CO2 laser therapy and Kegel exercise for the treatment of mild to moderate postpartum SUI provides an improved curative effect and maintains the duration of treatment effect, and it does not increase the incidence of adverse reactions in the treatment process.
Cause analysis: Lattice CO2 laser intervention can help submucosal neovascularization, promote collagen deposition and proliferation of elastic fibers, promote epithelial cell proliferation, induce histological changes in the vaginal epithelium and lamina propria, and improve and maintain vaginal tissue function. Through the incorporation of Kegel exercises, the coordination between the bladder and pelvic floor muscles can be further enhanced, the bladder capacity and control ability can be improved, and the occurrence of urinary intention and urgency can be reduced[22]. Therefore, the combined application of dot lattice CO2 laser therapy and Kegel exercise can enhance the stimulation of pelvic floor muscles, improve the contraction strength and endurance of the pelvic floor muscles, and play a role in consolidating the therapeutic effect.
SUI symptoms can affect a patient’s daily activities and quality of life, increase their depression, anxiety, and other negative emotions[23], and even increase the risk of suicidal ideation[24]. Liu and Hu[25] found that, through Kegel exercises, not only can SUI symptoms be improved, but the incidence of depression in patients can also be reduced. In this study, the EPDS score for postpartum depression and the PSAS score for postpartum specific anxiety in Group L were significantly lower than those in Group S at the end of treatment, and the EPDS and PSAS scores of Group L remained lower than those of Group S at 3 months after the end of treatment. The reason for this may be that the efficacy of receiving lattice CO2 laser treatment alone was limited and the duration of effect maintenance was short, thus causing some patients to have difficulty recovering to their prenatal state. This often increases the psychological burden in daily life because of embarrassing situations, such as urinary leakage and unpleasant odors, that are difficult to talk about, which increases negative emotions such as postpartum depression and anxiety. In contrast, the combination of dot lattice CO2 laser therapy and Kegel exercise further improved the treatment efficacy and maintained the duration of efficacy, thereby effectively controlling urinary incontinence in patients and alleviating SUI symptoms. After effective treatment, the patient’s clinical symptoms should have significantly improved, and the treatment effect should last for a long time, which is conducive to reducing the psychological pressure and negative emotions induced by this dysfunction. This enhances their ability to address the dysfunction correctly, increase self-confidence, and embrace daily life and work optimistically. Furthermore, it positively promotes the patient’s healthy psychology and maintains their good emotional state. In addition, after the patient completes the treatment course, Kegel exercises can still be performed at home according to their own needs, thereby preventing the recurrence of SUI to an extent. This is important in further improving the long-term quality of life and promoting the patient’s mental health.
This study also has some limitations: (1) Although this study confirms the significant and stable efficacy of dot lattice CO2 laser therapy in combination with Kegel exercise treatment for mild to moderate postpartum SUI, an extended follow-up period is required. This would provide strong evidence for the long-term efficacy and safety of dot lattice CO2 laser therapy in combination with Kegel exercise treatment for mild to moderate postpartum SUI; and (2) This study conducted research at a single center with a small sample size and limited representativeness. Therefore, a larger multicenter cohort is required to support the conclusions.
The combination treatment of dot lattice CO2 laser therapy and Kegel exercise has a significant therapeutic effect on mild to moderate postpartum SUI, which can improve treatment efficacy and maintain the efficacy duration, thereby enhancing patients’ quality of life and alleviating the postpartum depression and anxiety caused by SUI symptoms.
| 1. | Molinet Coll C, Martínez Franco E, Altimira Queral L, Cuadras D, Amat Tardiu L, Parés D. Hormonal Influence in Stress Urinary Incontinence During Pregnancy and Postpartum. Reprod Sci. 2022;29:2190-2199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 2. | Siddiqui NY, Wiseman JB, Cella D, Bradley CS, Lai HH, Helmuth ME, Smith AR, Griffith JW, Amundsen CL, Kenton KS, Clemens JQ, Kreder KJ, Merion RM, Kirkali Z, Kusek JW, Cameron AP; LURN. Mental Health, Sleep and Physical Function in Treatment Seeking Women with Urinary Incontinence. J Urol. 2018;200:848-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 3. | Gambacciani M, Torelli MG, Martella L, Bracco GL, Casagrande AG, Albertin E, Tabanelli S, Viglietta M, D'Ambrogio G, Garone G, Cervigni M. Rationale and design for the Vaginal Erbium Laser Academy Study (VELAS): an international multicenter observational study on genitourinary syndrome of menopause and stress urinary incontinence. Climacteric. 2015;18 Suppl 1:43-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 4. | González Isaza P, Jaguszewska K, Cardona JL, Lukaszuk M. Long-term effect of thermoablative fractional CO(2) laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J. 2018;29:211-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 80] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 5. | Gonzales AL, Barnes KL, Qualls CR, Jeppson PC. Prevalence and Treatment of Postpartum Stress Urinary Incontinence: A Systematic Review. Female Pelvic Med Reconstr Surg. 2021;27:e139-e145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Balk EM, Adam GP, Corsi K, Mogul A, Trikalinos TA, Jeppson PC. Adverse Events Associated with Nonsurgical Treatments for Urinary Incontinence in Women: a Systematic Review. J Gen Intern Med. 2019;34:1615-1625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Urogynocology Subgroup; Chinese Society of Obstetrics and Gynocology; Chinese Medical Association. [Update of guideline on the diagnosis and treatment of female stress urinary incontinence (2017)]. Zhonghua Fu Chan Ke Za Zhi. 2017;52:289-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Abrams P, Avery K, Gardener N, Donovan J; ICIQ Advisory Board. The International Consultation on Incontinence Modular Questionnaire: www.iciq.net. J Urol. 2006;175:1063-6; discussion 1066. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 330] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 9. | Bushnell DM, Martin ML, Summers KH, Svihra J, Lionis C, Patrick DL. Quality of life of women with urinary incontinence: cross-cultural performance of 15 language versions of the I-QOL. Qual Life Res. 2005;14:1901-1913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 82] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Li J, Li H, Zhou Y, Xie M, Miao Y, Wang L, Zhao Y, Ying T, Hu Y, Chen Y, Chen Y, Sun X, Wang J. The Fractional CO(2) Laser for the Treatment of Genitourinary Syndrome of Menopause: A Prospective Multicenter Cohort Study. Lasers Surg Med. 2021;53:647-653. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 11. | Yu J, Zhang Z, Deng Y, Zhang L, He C, Wu Y, Xu X, Yang J. Risk factors for the development of postpartum depression in individuals who screened positive for antenatal depression. BMC Psychiatry. 2023;23:557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 12. | Fallon V, Halford JCG, Bennett KM, Harrold JA. The Postpartum Specific Anxiety Scale: development and preliminary validation. Arch Womens Ment Health. 2016;19:1079-1090. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 100] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 13. | Caruso FB, Schreiner L, Todescatto AD, Crivelatti I, Oliveira JM. Risk Factors for Urinary Incontinence in Pregnancy: A Case Control Study. Rev Bras Ginecol Obstet. 2020;42:787-792. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Ptak M, Ciećwież S, Brodowska A, Starczewski A, Nawrocka-Rutkowska J, Diaz-Mohedo E, Rotter I. The Effect of Pelvic Floor Muscles Exercise on Quality of Life in Women with Stress Urinary Incontinence and Its Relationship with Vaginal Deliveries: A Randomized Trial. Biomed Res Int. 2019;2019:5321864. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Yang X, Wang X, Gao Z, Li L, Lin H, Wang H, Zhou H, Tian D, Zhang Q, Shen J. The Anatomical Pathogenesis of Stress Urinary Incontinence in Women. Medicina (Kaunas). 2022;59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 16. | Ostrzenski A. The new etiology and surgical therapy of stress urinary incontinence in women. Eur J Obstet Gynecol Reprod Biol. 2020;245:26-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Salvatore S, Leone Roberti Maggiore U, Athanasiou S, Origoni M, Candiani M, Calligaro A, Zerbinati N. Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause. 2015;22:845-849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 176] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 18. | Alcalay M, Ben Ami M, Greenshpun A, Hagay Z, Schiff E. Fractional-Pixel CO(2) Laser Treatment in Patients With Urodynamic Stress Urinary Incontinence: 1-Year Follow-Up. Lasers Surg Med. 2021;53:960-967. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Behnia-Willison F, Nguyen TTT, Mohamadi B, Vancaillie TG, Lam A, Willison NN, Zivkovic J, Woodman RJ, Skubisz MM. Fractional CO(2) laser for treatment of stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol X. 2019;1:100004. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Dabaja H, Lauterbach R, Matanes E, Gruenwald I, Lowenstein L. The safety and efficacy of CO(2) laser in the treatment of stress urinary incontinence. Int Urogynecol J. 2020;31:1691-1696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Alagirisamy P, Sidik SM, Rampal L, Ismail SIF. Effectiveness of a Pelvic Floor Muscle Exercise Intervention in Improving Knowledge, Attitude, Practice, and Self-Efficacy among Pregnant Women: A Randomized Controlled Trial. Korean J Fam Med. 2022;43:42-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 22. | Woodley SJ, Lawrenson P, Boyle R, Cody JD, Mørkved S, Kernohan A, Hay-Smith EJC. Pelvic floor muscle training for preventing and treating urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev. 2020;5:CD007471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 115] [Article Influence: 23.0] [Reference Citation Analysis (6)] |
| 23. | Gallego-Gómez C, Rodríguez-Gutiérrez E, Torres-Costoso A, Martínez-Vizcaíno V, Martínez-Bustelo S, Quezada-Bascuñán CA, Ferri-Morales A. Urinary incontinence increases risk of postpartum depression: systematic review and meta-analysis. Am J Obstet Gynecol. 2024;231:296-307.e11. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Pan T, Zhang Z, He T, Zhang C, Liang J, Wang X, Di X, Hong Y, Bai P. The association between urinary incontinence and suicidal ideation: Findings from the National Health and Nutrition Examination Survey. PLoS One. 2024;19:e0301553. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | Liu D, Hu WL. SLK Triple Therapy Improves Maternal and Fetal Status and Promotes Postpartum Pelvic Floor Function in Chinese Primiparous Women. Med Sci Monit. 2019;25:8913-8919. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |