Published online Mar 19, 2025. doi: 10.5498/wjp.v15.i3.102529
Revised: December 20, 2024
Accepted: January 17, 2025
Published online: March 19, 2025
Processing time: 128 Days and 9.4 Hours
Catatonic syndrome is a mental health issue, as well as a medical, neurological, and toxic condition. There are few published data on catatonic syndrome in African countries and none in Sudan, the third-largest African country.
To assess the prevalence and presenting symptoms of catatonic syndrome in an acute psychiatric inpatient population in four governmental psychiatric hospitals in Sudan.
A cross-sectional study was conducted in four psychiatric hospitals in the capital, Khartoum, in Sudan. The data were collected using an interviewer-administered questionnaire tool, which included sociodemographic data (age, sex, educational level, marital status, and residence). Signs and symptoms of catatonic syndrome were assessed using the Bush–Francis Catatonia Rating Scale (BFCRS) and the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) diagnostic criteria. χ² tests were used to compare categorized variables. Mul
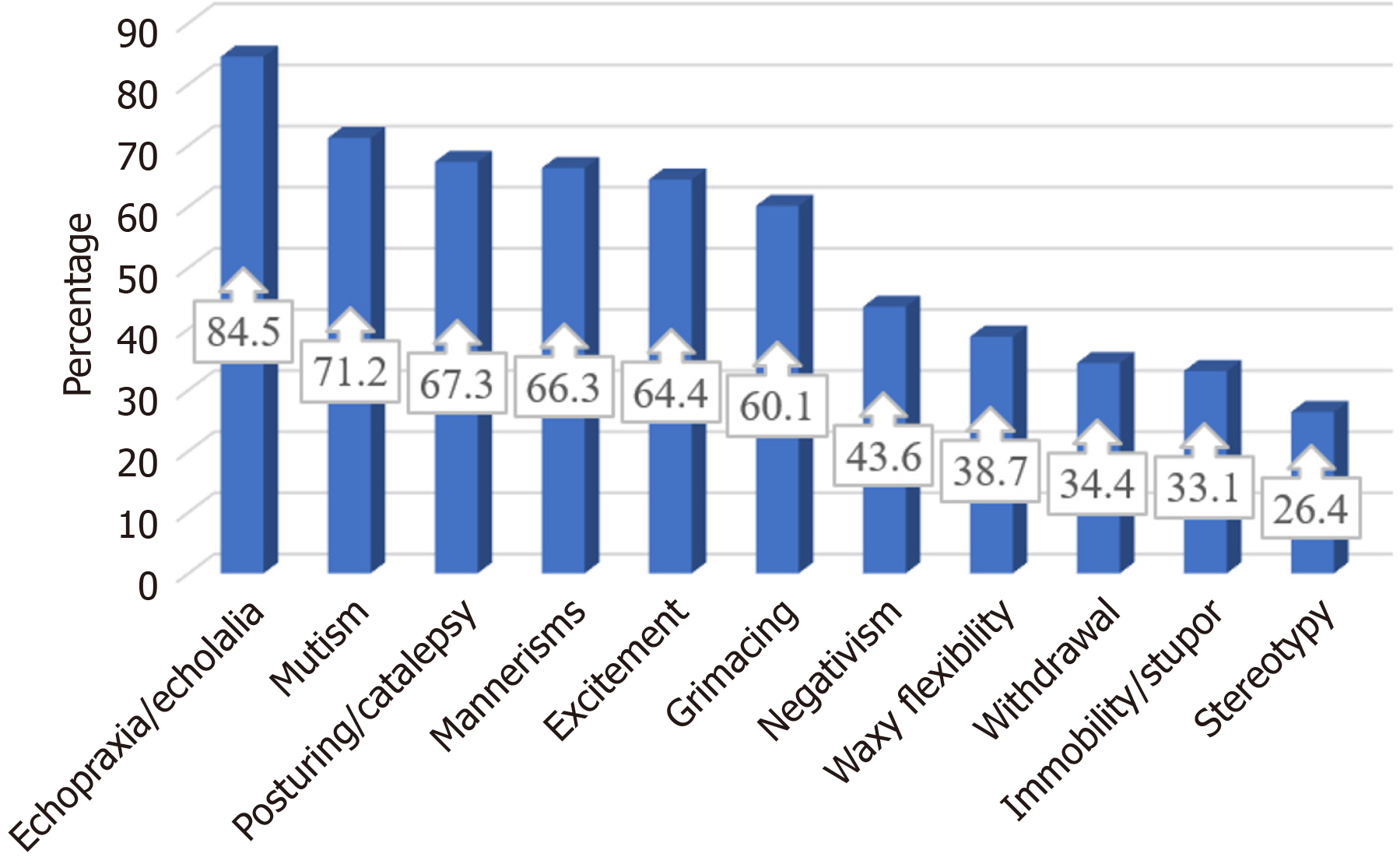
Of the 384 patients, 50.0% and 49.3% were males and females, respectively, and their median age was 30.0 years. One hundred and sixty-three (42.4%) patients had catatonic syndrome according to the BFCRS criteria. Of these patients, 104 fulfilled the DSM-5 criteria, with a 27.1% prevalence of catatonic syndrome. Echopraxia/echolalia (84.5%), mutism (71.2%), posturing/catalepsy (67.3%), and mannerisms (66.3%) were the main manifestations among patients with catatonic syndrome. There was no significant difference in age, sex, marital status, or job between patients with and those without catatonic syndrome. Of the 163 patients with catatonic syndrome, 31.3% had bipolar disorder, 28.2% had schizophrenia, and 19.6% had major depressive disorder.
Catatonic syndrome is highly prevalent in an acute psychiatric inpatient population in Sudan regardless of age or sex. Echopraxia/echolalia (84.5%) and mutism were the main manifestations among the patients with catatonic syndrome.
Core Tip: This study highlights the prevalence of catatonia in Sudan and investigates the characteristics thereof. Echo
- Citation: Idrees MB, Elmahdi AM, Alharbi HY, Adam I. Catatonia in an acute adult inpatient population in mental health units in Khartoum, Sudan: A cross-sectional study. World J Psychiatry 2025; 15(3): 102529
- URL: https://www.wjgnet.com/2220-3206/full/v15/i3/102529.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i3.102529
Catatonic syndrome is a complex neuropsychiatric syndrome that presents a challenging mixture of abnormal motor, behavioral symptoms, and systemic manifestations[1]. Its causes can be both psychiatric and organic; therefore, organic causes need to be ruled out first[2]. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), catatonic syndrome is a mental disorder and is diagnosed when the clinical picture includes at least three of the following: stupor, catalepsy, waxy flexibility, mutism, negativism, posturing, mannerisms, agitation, stereotypy, gri
Two subtypes of catatonic syndrome have been described: retarded and excited; the former is associated with signs reflecting a lack of movement, including immobility, staring, mutism, rigidity, withdrawal, and refusal to eat, with more bizarre features such as posturing, grimacing, negativism, waxy flexibility, echolalia, or echopraxia, stereotypy, ver
Moreover, catatonic syndrome is associated with other disorders, underscoring the necessity of rapid diagnosis and treatment. If catatonic syndrome is not fully diagnosed[5], patients could have life-threatening complications; therefore, urgent treatment is required. In particular, catatonic syndrome appears to be a risk factor for the development of neuroleptic malignant syndrome[6], which has a mortality rate of approximately 10%[7]. Additionally, the immobility and refusal to eat or drink associated with catatonic syndrome can give rise to potentially serious medical complications, such as dehydration, malnutrition, deep vein thrombosis, pulmonary embolism, and muscle contractures[8,9].
The awareness of catatonic syndrome among general medical doctors and even psychiatrists is relatively poor, and it is often seen as a historical diagnosis[10]. It is important to be aware of catatonic syndrome and to have a high index of suspicion when longstanding psychiatric medications have been stopped during medical management or when patients have reduced oral intake. As these patients are likely under the care of a medical team rather than a psychiatrist, it is essential to increase physician awareness of catatonic syndrome and encourage prompt treatment[5].
There are several proposed classifications of catatonic syndrome[11]. Several scales have been developed to quantify catatonic signs[11], such as the Bush–Francis Catatonia Rating Scale (BCFRS) and the DSM-5, which have been the most recently used to diagnose catatonic syndrome[11].
Recent reports have shown varied prevalence and features of catatonic syndrome among adults in different regions of the world[12–17]. However, few of these publications on catatonic syndrome have been conducted in African countries[18–20]. None were conducted in Sudan, the third-largest country in Africa. Therefore, this study aimed to determine the prevalence and identify the presenting symptoms of catatonic syndrome in an acute psychiatric inpatient population in Khartoum, the capital of Sudan.
A cross-sectional hospital-based study was conducted in four governmental psychiatric hospitals in Sudan (Taha Baasher, Khartoum North, Tegani Elmahi, and Khartoum–Omdurman) between March and June 2022. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines[21].
Patients (males and females) admitted with acute mental illness to a psychiatric ward were assessed for catatonic and clinical symptomatology. The assessments occurred on the first day of admission to the hospital or the first day of symptom appearance.
Patients were included in the sample only once if they were readmitted to the acute ward within the study period and stayed there for more than 24 hours.
Adults were aged ≥ 18 years, including male and female psychiatric patients who presented to a psychiatric hospital emergency room. Inpatient admissions resulted directly from outpatient services, emergency psychiatry services, or transfers from other clinical specialties, such as neurology, neurosurgery, and private psychiatric clinics. The principal investigator/author and four research assistants recruited consenting participants from all new admissions. The research assistants were psychiatry residents with at least 2 years of experience. The principal investigator further trained the research assistants in using the BFCSI/BFCRS and DSM-5 to assess catatonia, elicit signs, and capture the collected data on a data sheet (examining the first 7 patients together).
The data were collected using an interviewer-administered questionnaire, gathering sociodemographic data (age, sex, educational level, and marital status). The second section contains signs and symptoms of catatonic syndrome, scored according to the BFCRS and DSM-5 diagnostic criteria. The BFCRS was used to recognize and score the catatonic signs and symptoms of stupor, catalepsy, waxy flexibility, mutism, negativism, posturing, mannerisms, agitation, stereotypy, grimacing, echolalia, or echopraxia[3], and it measures the severity of 23 catatonic signs. The instrument was used to score (on a 0–3-point scale) the first 14 items of the BFCRS. If two or more of the BFCRS signs were present, a diagnosis of catatonic syndrome was considered. Moreover, if three or more signs were present, the diagnosis of catatonic syndrome was considered as per the DSM-5 diagnostic criteria. The mental illness was diagnosed by the treating psychiatrist at the hospital, regardless of the presence or absence of symptoms or signs of catatonic syndrome.
According to the four hospitals’ records, 1012 patients presented with acute mental illness 4 months before the current study. Thus, a three-sample interval was assumed by dividing the expected number of patients (1012/384) by three. Eligible patients were interviewed every three intervals until the required sample size of 384 patients was reached.
OpenEpi Menu Software Version 3.01[22] was used to compute the required sample size, which was 384 patients. Given previous studies[18-20,23] that determined the optimal sample size, the maximum event occurrence (the prevalence of catatonic syndrome, i.e., even if it is 50.0%) was assumed to be 50.0% using the equation n = Z2pq/d2, where q = (1 − p), Z1 − α = 95%CI = 1.96, and d = margin of error of 5% = 0.05.
The data were analyzed using a licensed SPSS Version 24. Age was assessed for normality using the Shapiro–Wilk test, and was not normally distributed. Hence, it was expressed as the median (interquartile range) and compared between patients with and without catatonia using a non-parametric test. χ² tests were used to compare the categorized variables. A two-sided P < 0.05 was statistically significant. Multivariate analysis was not performed because none of the variables were found to be different between patients with and without catatonic syndrome.
Three hundred and eighty-four patients were enrolled in the study. Of these, 50.0% and 49.3% were males and females, respectively. The median (interquartile range) age was 30.0 (24.0-40.0) years. Of the 384 enrolled patients, 78 (20.3%) had no formal education, and 146 (38.0%) had a primary education. Around half (47.1%) of the patients were married, and 45.8% were unemployed (Table 1).
| Variable | Frequency | Proportion | |
| Gender | Male | 198 | 51.6% |
| Female | 186 | 48.4% | |
| Education level | No formal education | 78 | 20.3% |
| Primary | 146 | 38.0% | |
| Secondary | 108 | 28.1% | |
| University and above | 52 | 13.5% | |
| Marital status | Single | 156 | 40.6% |
| Married | 181 | 47.1% | |
| Divorced | 32 | 8.3% | |
| Widowed | 15 | 3.9% | |
| Job | Student | 48 | 12.5% |
| Employee | 55 | 14.3% | |
| Laborer | 105 | 27.3% | |
| Not working | 176 | 45.8% |
One hundred and sixty-three (42.4%) patients had catatonic syndrome according to the BFCRS criteria. Of these, 104 patients fulfilled the DSM-5 criteria, with a prevalence of catatonic syndrome of 27.1%.
Echopraxia/echolalia (84.5%), mutism (71.2%), posturing/catalepsy (67.3%), mannerisms (66.3%), excitement (64.4%), and grimacing (60.1%) were the main manifestations among the patients with catatonic syndrome (Figure 1). None of the patients had malignant catatonic syndrome.
There was no significant difference in the median (interquartile range) of the age [28.5 (22.0-40.0) years vs 30.0 (25-42.0) years, P = 0.226] between patients with catatonic syndrome and those without catatonic syndrome. There was no significant difference in sex, marital status, and job between patients with catatonic syndrome and patients without catatonic syndrome (Table 2). Of 163 patients with catatonic syndrome, 51 (31.3%) had bipolar disorder, 46 (28.2%) had schizophrenia, 32 (19.6%) had major depressive disorder, 16 (9.8%) had substance-induced psychosis, 11 (6.7%) had substance-induced bipolar disorder, and 7 (4.3%) had a missing or unknown diagnosis.
| Variable | Patients with catatonic syndrome (n = 163) | Patients without catatonic syndrome (n = 221) | P value | |
| Sex | Male | 76 (46.6) | 122 (55.2) | 0.999 |
| Female | 87 (53.4) | 99 (44.4) | ||
| Education level | No formal education | 41 (25.2) | 37 (16.7) | 0.099 |
| Primary | 63 (38.7) | 83 (37.6) | ||
| Secondary | 37 (22.7) | 71 (32.1) | ||
| University | 22 (13.5) | 30 (13.6) | ||
| Marital status | Single | 74 (45.4) | 82 (37.1) | 0.068 |
| Married | 74 (45.4) | 107 (48.4) | ||
| Divorced | 7 (4.3) | 25 (11.3) | ||
| Widowed | 8 (4.9) | 7 (3.2) | ||
| Job | Student | 27 (16.6) | 21 (9.5) | 0.076 |
| Employee | 20 (12.3) | 35 (15.8) | ||
| Laborer | 36 (22.1) | 69 (31.2) | ||
| Not working | 80 (49.1) | 96 (43.4) |
The current study showed that 42.4% and 27.1% of the patients had catatonic syndrome, according to the BFCRS and the DSM-5, respectively. The prevalence of catatonic syndrome did not diverge between females and males, and there was no age distinction between patients with and without catatonic syndrome. Our results, which showed that 42.4% of the patients had catatonia, were slightly higher than the results of Cuevas-Esteban et al[23], who reported that 39.6% of the patients (106) admitted to an acute geriatric psychiatry ward in Spain had catatonic syndrome, which was assessed via BFCRS.
The prevalence (42.4% and 27.1%) of catatonic syndrome in the current study was higher than that reported in several countries[4,12,13,17,19] (Table 3). For example, the prevalence of catatonic syndrome was 18.3% using the BFCSI and 6.6% using the DSM-5 among 241 adults aged > 16 years in a mental hospital in South Africa[19]. An incidence of 10.6 episodes of catatonic syndrome per 100000 person-years was observed in electronic healthcare records in London[12]. In India, the prevalence of catatonic syndrome was 16.3% and 10.6%, respectively, according to the diagnostic cut-offs defined by the BFCRS and Northoff Catatonia Scale[13]. Moreover, the prevalence rates per the International Classification of Diseases-10 and DSM-5 criteria were 19% and 5.3%, respectively[13]. In an acute inpatient setting in Poland, the prevalence of catatonic syndrome was 8.5% and 5.0%, according to the BFCRS and DSM-5, respectively[16]. In Hungary, the prevalence of catatonic syndrome was 8.5% and 5.0%, according to the BFCRS and the DSM-5, respectively[16]. In Australia, 5.5% of older patients (age > 65 years) referred to a consultation-liaison psychiatry service had catatonia[17]. Moreover, the prevalence of catatonic syndrome in the current study was higher than the pooled prevalence (9.0%) of catatonic syndrome reported in a meta-analysis that included 74 studies from 1935 to 2017[4]. In Belgium, using the BFCRS, 50.8%, and using the DSM-5, 16.9%, of 101 acute inpatients had catatonic syndrome[14]. The difference in the prevalence of catatonic syndrome in various studies could be explained by the patients enrolled in these studies and by the diagnostic tools used to diagnose catatonic syndrome, which the DSM-5 gives low prevalence[13,19].
| Ref. | Country | Prevalence of catatonic syndrome using the Bush–Francis Catatonia Rating Scale | Prevalence of catatonic syndrome using manual of mental disorders, fifth edition |
| This study | Sudan | 42.4% | 27.1% |
| [23] | Spain | 39.6% | - |
| [19] | South Africa | 18.3% | 6.6% |
| [13] | India | 16.3% | 5.3% |
| [16] | Poland | 8.5% | 5.0% |
| [16] | Hungary | 8.5% | 5.0% |
| [14] | Belgium | 50.8% | 16.9% |
In the current study, the prevalence of catatonic syndrome was identical between males and females. This corroborates findings observed in electronic healthcare records in London[12].
The most common symptoms elicited by the BFCSI were echopraxia/echolalia, mutism, posturing/catalepsy, mannerisms, and excitement. In Australia, immobility, rigidity, and posturing were commonly encountered catatonic signs in those scoring ≥2 on the Bush–Francis Catatonia Screening. Moreover, 5.5% of older patients (age > 65 years) referred to a consultation-liaison psychiatry service had catatonic syndrome[17]. Staring (52.5%) and withdrawal (45.0%) were the most common signs of catatonic syndrome noted in India, according to the BFCRS[13]. Excitement (64.3%), verbigeration (61.9%), and negativism (59.5%) were the most prevalent manifestations of catatonic syndrome in Spain[23].
Our results have shown that bipolar disorder, schizophrenia, and major depressive disorder are the main mental illnesses among patients with catatonic syndrome. This is consistent with the results of a previous meta-analysis, which showed that the prevalence of catatonic syndrome was higher in bipolar disorder, even more than in schizophrenia[4]. Bipolar disorder and schizophrenia are the leading mental illnesses in patients with catatonic syndrome in South Africa[19]. Conversely, depression and delirium (48.6% and 66.7%, respectively) were the most frequent psychiatric syndromes among patients with catatonic syndrome in Spain[23].
This cross-sectional study could not detect the direction of associations, and the outcome was not evaluated. Some pertinent limitations include the possibility of false positives, incorrect diagnoses made by treating psychiatrists (particularly as they were not study team members), selection bias, variability among raters, and generalizability. Assessment of catatonia at only one point during admission may have falsely deflated the prevalence rate.
Catatonic syndrome is highly prevalent in an acute psychiatric inpatient population in Sudan regardless of age or sex. Echopraxia/echolalia (84.5%) and mutism were the main manifestations among the patients with catatonic syndrome.
| 1. | Fornaro M. Catatonia: a narrative review. Cent Nerv Syst Agents Med Chem. 2011;11:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: Our current understanding of its diagnosis, treatment and pathophysiology. World J Psychiatry. 2016;6:391-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 149] [Cited by in RCA: 191] [Article Influence: 21.2] [Reference Citation Analysis (9)] |
| 3. |
American Psychiatric Association; DSM-5 Task Force.
Diagnostic and statistical manual of mental disorders: |
| 4. | Solmi M, Pigato GG, Roiter B, Guaglianone A, Martini L, Fornaro M, Monaco F, Carvalho AF, Stubbs B, Veronese N, Correll CU. Prevalence of Catatonia and Its Moderators in Clinical Samples: Results from a Meta-analysis and Meta-regression Analysis. Schizophr Bull. 2018;44:1133-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 110] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 5. | Doran E, Sheehan JD. Acute catatonia on medical wards: a case series. J Med Case Rep. 2018;12:206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Sienaert P, van Harten P, Rhebergen D. The psychopharmacology of catatonia, neuroleptic malignant syndrome, akathisia, tardive dyskinesia, and dystonia. Handb Clin Neurol. 2019;165:415-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Strawn JR, Keck PE Jr, Caroff SN. Neuroleptic malignant syndrome. Am J Psychiatry. 2007;164:870-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 258] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 8. | Clinebell K, Azzam PN, Gopalan P, Haskett R. Guidelines for preventing common medical complications of catatonia: case report and literature review. J Clin Psychiatry. 2014;75:644-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 9. | Peritogiannis V, Rizos DV. Catatonia Due to General Medical Conditions in Psychiatric Patients: Implications for Clinical Practice. Psychiatry Int. 2023;4:18-27. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Wortzel JR, Maeng DD, Francis A, Oldham MA. Prevalent Gaps in Understanding the Features of Catatonia Among Psychiatrists, Psychiatry Trainees, and Medical Students. J Clin Psychiatry. 2021;82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 11. | Zingela Z, Stroud L, Cronje J, Fink M, van Wyk S. Assessment of catatonia and inter-rater reliability of three instruments: a descriptive study. Int J Ment Health Syst. 2021;15:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Rogers JP, Pollak TA, Begum N, Griffin A, Carter B, Pritchard M, Broadbent M, Kolliakou A, Ke J, Stewart R, Patel R, Bomford A, Amad A, Zandi MS, Lewis G, Nicholson TR, David AS. Catatonia: demographic, clinical and laboratory associations. Psychol Med. 2023;53:2492-2502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 32] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 13. | Subramaniyam BA, Muliyala KP, Hari Hara S, Kumar Reddi VS. Prevalence of catatonic signs and symptoms in an acute psychiatric unit from a tertiary psychiatric center in India. Asian J Psychiatr. 2019;44:13-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Stuivenga M, Morrens M. Prevalence of the catatonic syndrome in an acute inpatient sample. Front Psychiatry. 2014;5:174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 15. | Hirjak D, Brandt GA, Fritze S, Kubera KM, Northoff G, Wolf RC. Distribution and frequency of clinical criteria and rating scales for diagnosis and assessment of catatonia in different study types. Schizophr Res. 2024;263:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 16. | Takács R, Asztalos M, Ungvari GS, Antosik-Wójcińska AZ, Gazdag G. The prevalence of catatonic syndrome in acute psychiatric wards. Psychiatr Pol. 2019;53:1251-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Kaelle J, Abujam A, Ediriweera H, Macfarlane MD. Prevalence and symptomatology of catatonia in elderly patients referred to a consultation-liaison psychiatry service. Australas Psychiatry. 2016;24:164-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Worku B, Fekadu A. Symptom profile and short term outcome of catatonia: an exploratory clinical study. BMC Psychiatry. 2015;15:164. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Zingela Z, Stroud L, Cronje J, Fink M, Van Wyk S. A prospective descriptive study on prevalence of catatonia and correlates in an acute mental health unit in Nelson Mandela Bay, South Africa. PLoS One. 2022;17:e0264944. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Yitayih Y, Tesfaye E, Adorjan K. The Presentation and Treatment Response of Catatonia in Patients Admitted to the Psychiatric Inpatient Unit at Jimma University Medical Center, Ethiopia. Psychiatry J. 2020;2020:8739546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5754] [Cited by in RCA: 9926] [Article Influence: 583.9] [Reference Citation Analysis (0)] |
| 22. | Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Version. Available from: https://www.openepi.com/Menu/OE_Menu.htm. |
| 23. | Cuevas-Esteban J, Iglesias-González M, Rubio-Valera M, Serra-Mestres J, Serrano-Blanco A, Baladon L. Prevalence and characteristics of catatonia on admission to an acute geriatric psychiatry ward. Prog Neuropsychopharmacol Biol Psychiatry. 2017;78:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |