Published online Mar 19, 2025. doi: 10.5498/wjp.v15.i3.100959
Revised: November 25, 2024
Accepted: January 22, 2025
Published online: March 19, 2025
Processing time: 178 Days and 18.6 Hours
Military personnel frequently face unique psychological challenges due to high-stress environments, which increase the risk of mental health issues like anxiety and depression. Acceptance and commitment therapy (ACT) has shown potential in addressing these issues by enhancing psychological flexibility and resilience.
To systematically evaluate the effectiveness of ACT in improving the mental health of military personnel. Through a scoping review and meta-analysis, we quantitatively assess the impact of ACT on psychological outcomes, guiding future research and clinical practice.
Relevant literature was searched systematically from database inception to June 30, 2023, across multiple databases, including PubMed, Web of Science, Cochrane Library, and Embase. The Joanna Briggs Institute's (JBI) scoping review guidelines were used as the methodological framework. Meta-analysis was performed using a random-effects model, and publication bias was assessed through Egger's regression test and Begg's funnel plot.
Twenty-six studies were included, highlighting the application of ACT in addressing PTSD, chronic pain, anxiety, and depression among military per
This study underscores the potential of ACT as an effective intervention for improving the mental health of military personnel. Future research should focus on large-scale, multi-center RCTs to further validate these findings, particularly within diverse military populations.
Core Tip: The study assesses acceptance and commitment therapy (ACT)'s impact on military mental health, offering a new intervention perspective. It confirms ACT reduces post-traumatic stress disorder (PTSD) symptoms and increases resilience. Findings highlight ACT's significant reduction of PTSD and improvement in coping skills. Strict assessments ensure the study's reliability and robustness. The research supports mental health interventions in military settings, encouraging tailored treatment advancements.
- Citation: Wang JQ, Wang XZ, Wang WX. Acceptance and commitment therapy for enhancing mental health in military personnel: A comprehensive review and meta-analysis. World J Psychiatry 2025; 15(3): 100959
- URL: https://www.wjgnet.com/2220-3206/full/v15/i3/100959.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i3.100959
As the particular group bearing these significant duties, military personnel often operate under high stress and pressure[1]. They are frequently subjected to harsh living conditions, intensive training, extended working hours, and various hazardous factors, predisposing them to mental and physical health issues such as post-traumatic stress disorder (PTSD), depression, insomnia, and chronic pain[2]. Hence, exploring and providing adequate mental health support and intervention measures to ensure military personnel's health and combat readiness has emerged as a pressing issue[3]. As China's role in the international community becomes increasingly prominent, the country faces more complex and variable international security challenges[4]. In this context, the responsibilities of the Chinese military in consolidating national defense security and executing overseas non-war military tasks have become more crucial[5].
Acceptance and commitment therapy (ACT), based on mindfulness techniques and a third-generation cognitive-behavioral therapy (CBT), employs six core therapeutic processes—acceptance, cognitive defusion, being present, self-as-context, values clarification, and committed action—to enhance psychological flexibility and help individuals lead meaningful, value-driven lives[6].
Compared with other therapies, ACT is particularly sensitive to the context of psychological phenomena and their psychological functions. It employs a variety of flexible and effective therapeutic techniques to enhance psychological flexibility and has become a central feature of the third wave of CBT. As one of the most frequently cited psychological interventions in recent years, it holds significant importance for individuals in high-stress environments, such as the military. In the broader field of mental health, particularly in the treatment of PTSD, anxiety, and depression, ACT has demonstrated significant efficacy[7]. However, research on the application methods, effectiveness assessments, and intervention outcomes of ACT in the unique population of military personnel shows considerable heterogeneity[8]. ACT's unique advantages in military mental health interventions are primarily reflected in the design of its core processes. Military personnel often face complex and diverse psychological stressors, such as traumatic experiences following high-intensity missions and the psychological burden of heightened alertness. ACT employs processes like acceptance, cognitive defusion, and self-observation to help military personnel accept these painful experiences, reduce psychological struggle, and focus more effectively on important life and mission goals. Unlike traditional CBT, ACT does not require individuals to change or control negative emotions but emphasizes coexisting with these emotions peacefully. This approach is particularly suitable for service members with comorbidities like PTSD and chronic pain, which increase treatment complexity. The theoretical basis of ACT posits that emotions and feelings are unavoidable, and the focus should be on coexisting with them. This principle helps service members maintain psychological stability in un
Against this backdrop, our study employs the scoping review framework published by the Joanna Briggs Institute (JBI) in 2020 to systematically analyze and evaluate the literature on the application of ACT within military populations. This approach aims to thoroughly understand the actual effects and potential value of ACT in mental health interventions for military personnel, particularly its capacity to improve psychological health issues such as PTSD, anxiety, and depression[14].
This research's scientific significance and clinical value lie in its novel attempt to comprehensively assess ACT's effectiveness in mental health interventions for military personnel through systematic evaluation and meta-analysis. Specifically, we focus on how ACT aids military personnel in coping with and managing psychological health challenges, facilitates psychological recovery, and enhances overall quality of life. Research indicates that the mental health of military personnel not only affects themselves but also directly or indirectly impacts the quality of life and mental well-being of their family members. Consequently, interventions aimed at improving the psychological health of service members often benefit their families as well, helping them better cope with the stressors associated with military life[15,16]. Moreover, our findings will provide a scientific basis for developing and implementing mental health intervention strategies within the military while delivering tangible welfare improvements for military personnel and their families. Through a comprehensive analysis of existing research, this study aims to reveal ACT's effectiveness in psychological interventions for military personnel, offering direction and foundation for future research and practice.
This scoping review is guided by the methodological framework of the JBI evidence synthesis manual, published in 2020[17].
A comprehensive search was conducted across databases including PubMed, Web of Science, Cochrane Library, Embase, PsycINFO, CNKI (China National Knowledge Infrastructure), Wanfang Medical Journal Database, VIP Chinese Science and Technology Periodical Database, and the China Biological Medicine Database, covering the period up to June 30, 2023. Search terms in English included "acceptance and commitment therapy, ACT therapy, ACT treatment" with "veteran*, soldier*, army, navy, marine, troop, air force, armed, peacekeeper*, defense". In Chinese, search terms included "military personnel, troops, officers, soldiers, warriors" and "acceptance and commitment therapy (ACT), ACT therapy". Taking the PubMed database as an example, the specific search strategy is as follows: (((((((veteran*[Title/ Abstract]) OR (soldier*[Title/Abstract])) OR (army[Title/Abstract]) OR (navy[Title/Abstract]) OR (marine[Title/Abstract]) OR (troop[Title/Abstract]) OR (air force[Title/Abstract]) OR (armed[Title/Abstract]) OR (peacekee
Inclusion criteria were determined based on the JBI's participants, concept, context principle for scoping reviews. Participants (P) included active or retired military personnel; the concept (C) encompassed ACT in all forms, including online and face-to-face; the context (C) referred to settings where military personnel received ACT treatment, including outpatient clinics, military activity centers, community settings, and home-based interventions. Study types included qualitative research, randomized controlled trials (RCTs), quasi-experiments, and mixed-methods studies. Exclusion criteria were: (1) Non-Chinese and non-English literature; (2) Inaccessible full texts or duplicates; and (3) Research proposals, guidelines, and opinions. The primary focus of this study was to explore the application, scope, evaluation criteria, and intervention effects of ACT among military personnel.
This study adopts the JBI guidelines instead of the PRISMA framework, as the JBI guidelines are specifically designed for scoping reviews and are well-suited to systematically overview the breadth and scope of research within a given field. In contrast, PRISMA focuses more on assessing the strength of evidence for specific intervention effects. The JBI guidelines align better with the objectives of our study, facilitating a comprehensive analysis of ACT’s application in military mental health interventions. To enhance transparency in study selection, we also established clear criteria for handling comorbidities. If a study involves military personnel with comorbid conditions (e.g., PTSD combined with chronic pain, anxiety disorders, or other mental health issues) that do not significantly affect the core outcomes of ACT intervention, the study will be included. The rationale for including such studies is based on ACT's inherent flexibility, which makes it suitable for interventions addressing comorbid mental health issues. However, studies in which comorbidities are likely to significantly alter the effects of ACT (e.g., severe mental illness or substance use disorders) will be excluded to reduce heterogeneity and ensure comparability of results.
First, the retrieved literature will be imported into EndNote 20 software for deduplication, a crucial step in the literature screening process. Next, two researchers trained in evidence-based nursing will conduct the initial screening. These researchers will carefully read the titles and abstracts of the articles and screen them based on predefined inclusion and exclusion criteria. After the initial screening, the full texts of eligible articles will be obtained for a second round of screening. If any disagreements arise between the two researchers during the screening process, a third researcher, also trained in evidence-based nursing, will be brought in for discussion to reach a consensus on the inclusion or exclusion of the articles.
During the data extraction phase, the information collected will include author details, publication year, country or region of the study, study type (e.g., experimental study, survey study), sample size, age range of the study population, specifics of the intervention subjects, detailed description of the study content, intervention measures used, primary outcome measures (key indicators used to assess study results), and main intervention outcomes (significant effects of the intervention). This comprehensive and meticulous data extraction will provide a solid data foundation for subsequent literature analysis, ensuring the scientific rigor and reliability of the research.
To further assess ACT's effectiveness in mental health interventions among military personnel, this study's meta-analysis focused on RCTs, quasi-experimental, and mixed-methods studies to ensure the reliability and validity of the research findings. Data extraction primarily targeted quantifiable indicators of mental health improvement, such as changes in anxiety and depression symptom scores, along with other quantifiable outcomes related to the mental health of military personnel. Accurate recording of mean scores, standard deviations, and total sample sizes for both experimental and control groups was crucial. These data are vital for subsequent statistical analyses to assess the magnitude and direction of effects across studies and their statistical significance, ensuring high-quality and reliable research outcomes.
Meta-analysis was performed using R software, with effect sizes represented by R-values and their 95%CI. Cochran's Q test and I2 statistics were employed to assess heterogeneity across included studies. Additionally, sensitivity analysis was conducted to evaluate the stability of the research findings, incorporating funnel plots and Egger's test to assess the potential for publication bias. The significance level for all statistical tests was set at P < 0.05.
In the data analysis phase, a random-effects model was used to combine mean differences (MDs) between experimental and control groups. Tau2, I2 statistics, and χ² tests further assessed study heterogeneity. These steps ensured an accurate evaluation of the intervention's impact on rumination outcomes while maintaining the reliability and stability of the results.
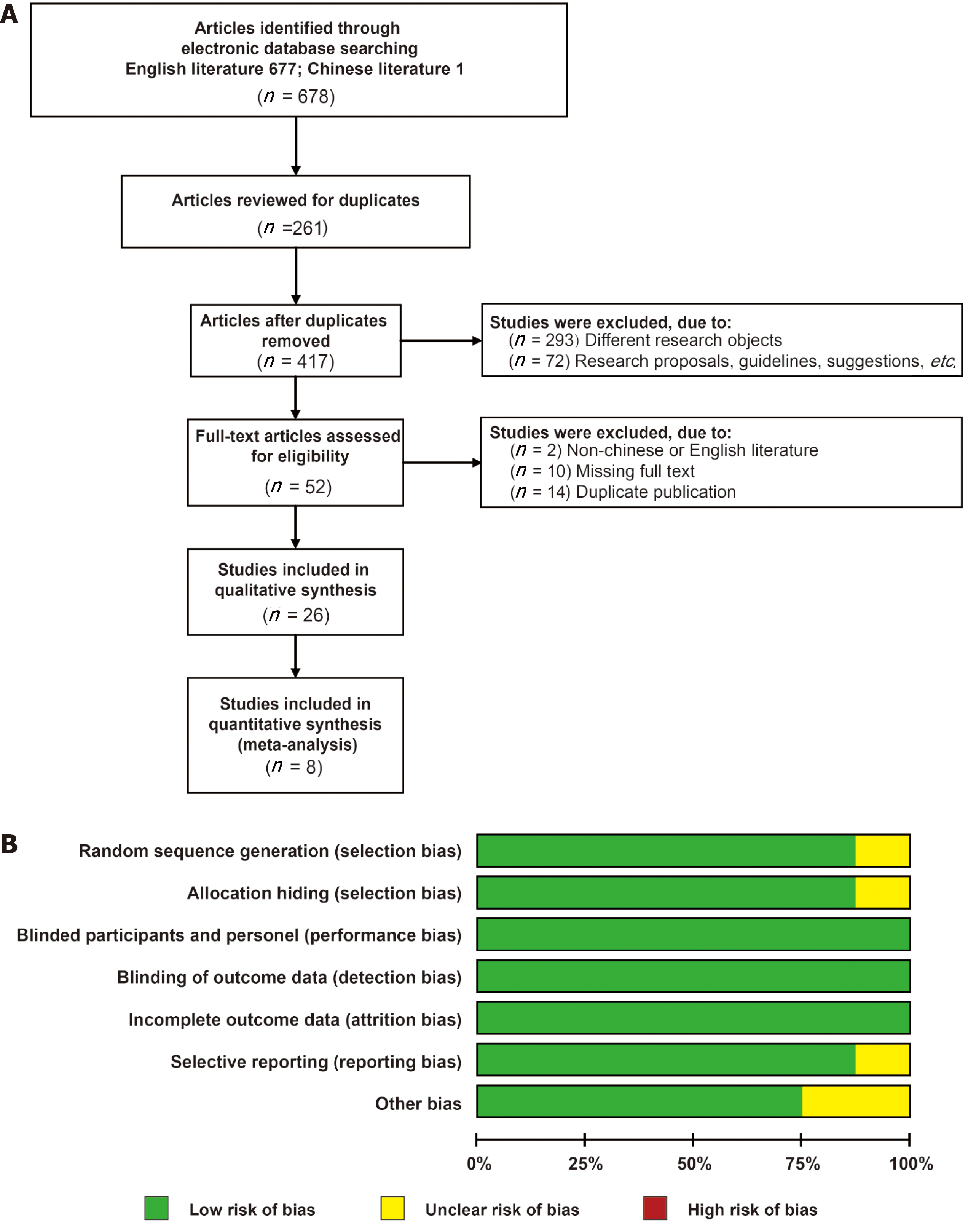
During the search process, 678 articles were identified through database searches, comprising 677 articles in English and 1 in Chinese. After deduplication, 417 articles remained. Screening of titles and abstracts based on predefined criteria led to the exclusion of 365 articles; upon full-text review of the remaining 52 articles, 26 were ultimately included for analysis, with 8 being incorporated into a quantitative meta-analysis (Figure 1A). Among the included studies, 25 originated from the United States and 1 from New Zealand. The designs of these studies included 9 RCTs, 15 quasi-experimental studies, and 2 mixed-methods studies. The sample sizes ranged from 12 to 981 participants, with study durations spanning from one day to six months. Detailed characteristics of the studies are presented in Table 1.
| Included literature | Country/region | Research design | Sample size (example, experimental group/control group) | Age (years, experimental group/control group) | Intervene object | Research content | Experimental group intervention | Control group Intervention measure | Main evaluation index | Main intervention effect |
| Reyes et al[24] | United States | Quasi-experiment | 23 | 31.22 ± 5.53 | College veteran | PTSD | The smart phone ACT intervention (listen to the assigned audio at least once a day, watch the assigned video once a week (for 4 weeks) and write about the viewing experience) was assessed at baseline, weekend 2, and weekend 4 | PCL-5; AAQ-II; MAAS; CD-RISC | Resilience, mindfulness, mental activity and symptoms of traumatic stress disorder were all improved | |
| Kelly et al[31] | United States | RCT | 21/19 | 54.9 ± 10.7/56.8 ± 13.3 | Veteran | PTSD | Twelve weekly 50min individual counseling ACT sessions, each with a specific topic, were assessed at baseline, at the end of treatment (12 weeks), and at 3 months | PCT therapy (person-centered therapy) for 50 minutes 12 times a week | MAAS; AAQ-II; PCL-5; CSQ-8; VLQ; SAS-SR; MOS-SSS; Q-LES-Q-SF | Improving the quality of social relations and participation in social activities can effectively improve the symptoms of traumatic stress disorder |
| Ramirez et al[28] | United States | Quasi-experiment | 311 | 37.6 ± 8.06 | Active serviceman | PTSD | Act-led outpatient treatment program for trauma: 6 weeks, 12 hours of group therapy per week, 2 individual sessions of 60 to 90 minutes | PCL-5; AAQ-II; VLQ; PHQ-9; GAD; ISI; CFQ; BASIS-24 | Improved mental activity, cognitive dissociation degree, traumatic stress disorder symptoms were effectively improved, but did not improve sleep | |
| Reyes et al[32] | United States | Quasi-experiment | 23 | 31.22 ± 5.53 | College veteran | PTSD | The smartphone ACT intervention was assessed over a 4-week period (including audio-guided mindfulness meditation and video lessons based on ACT principles, listening to the assigned audio at least once a day, watching the assigned video once a week and writing about the viewing experience) at baseline, weekend 2, and weekend 4 | CD-RISC; PCL-5; AAQ-II; MASS; RRS; ISS | Improve mindfulness, improve traumatic stress disorder, reduce experiential avoidance, and reduce rumination | |
| Gobin et al[34] | United States | RCT | 54/50 | Male: 34.7 ± 8.9; Female: 33.8 ± 7.3 | Veteran | PTSD (emphasis on the difference between male and female effects) | Conduct 12 one-hour individual sessions using the ACT manual developed by a professional therapist | PCT Therapy (Human-Centered Therapy) | BSI-18; SF-12; PCL-M | There was a significant advantage in the treatment effect of ACT in women, but no difference in the treatment effect in men |
| Meyer et al[35] | United States | Quasi-experiment | 43 | 45.26 ± 8.6 | Veteran | PTSD, alcohol use disorder | Once a week for a total of 12 ACT individual outpatient treatments | PCL-5; AAQ-II; AUDIT; DAST;PHQ-9; QOL-BREF | Improved traumatic stress disorder, reduced depressive symptoms and suicidal ideation, and reduced alcohol dependence; Quality of life improved | |
| Jacobs et al[36] | United States | Quasi-experiment | 12 | 68 ± 6.59 | Senior veterans over 60 years old | PTSD | 12 ACT courses | GDS-15; GAD-7; AAQ-II | Anxiety and psychoactivity were improved, and depressive symptoms were significantly improved | |
| Lang et al[37] | United States | RCT | 80/80 | 65 ± 81.83/63 ± 78.8 | Veteran | PTSD/anxiety/depression | Structured treatment according to the ACT manual, 11-hour treatment per week for a total of 12 times, at baseline, in the middle of treatment, after treatment, 3 months, 6 months, and 9 months | A total of 12 PCT treatments were performed once a week for 1 hour | PCL-MBSI-18; AUDIT; SDS; ISIAAQ-II; CSQ-8; PHQ-9; QOL-BREF | There was no difference between mental activity and anxiety and depression. There was a statistically significant difference in insomnia improvement in the ACT group |
| Kelly et al[38] | United States | Quasi-experiment | 19 | 56 ± 7 | Veteran | PTSD combined with tobacco addiction | ACT treatment for post-traumatic stress disorder combined with tobacco addiction (ACT-PT), 9 times a week for 50 minutes each time, the fifth time to encourage smoking cessation, plus 8 weeks of nicotine patch therapy, measured at baseline, end of treatment, 1 month, and 3 months | PCL-5; FTND; Number of cigarettes smoked; QSU; CSQ-8 | The symptoms of traumatic stress disorder were improved, the impulse to smoke was reduced, and the amount of smoking was significantly reduced | |
| Dindo et al[39] | United States | RCT | 27/12 | 37.7 ± 6.3/34.7 ± 5.8 | Veteran | Chronic pain | Each of the 1-day workshops included 4-hour ACT intervention, 2-hour behavior change training, and follow-up after 3 months | Routine psychiatric care | PCL-C; AAQ-II; BPI; DASS-21 | Improvement: anxiety depression, mental activity; Pain improvement was less than in the control group |
| Herbert et al[40] | United States | Quasi-experiment | 126 | 51.88 ± 13.14 | Veteran | Chronic pain | Face-to-face or video teleconferencing, 60 minutes ACT therapy per session 8 times per week | PCL-C; BPI; CPAQ; PASS-20 PHQ-9 | The improvement of pain and depression with PTSD was better, and the improvement of pain without PTSD was not significant | |
| Udell et al[41] | United States | Quasi-experiment | 242/310 | No statistical difference | Seaman | Pain | An improved pain treatment program based on ACT conceptual skills, 3 times per week for 1.5 hours per session, 6 sessions for 2 weeks. And receive standard care | Standard treatment services (physical, psychological, medical) | AAQ-II; PRS; GAD-7 | Effective pain relief; The psychoactive effect of anxiety and depression is small |
| Huddleston et al[42] | United States | Mixed study | 25 | Veteran | Depression and anxiety combined with migraine | A five-day, 5-hour workshop that included ACT and migraine education was followed for 3 months | AAQ-II; HRSA; IDAS; CPAQ | Effectively improve migraine, anxiety depression, mental activity | ||
| Dindo et al[43] | United States | RCT | 40/35 | 62.2 ± 10.1/63.0 ± 10.7 | Veteran | Pain associated with anxiety and depression after orthopedic surgery | ACT (5-hour workshop led by 2 psychologists, issue of ACT manual) + usual treatment, 3 months follow-up | Routine treatment: analgesia, education before and after operation | Stop pain time; Duration of opiate withdrawal; CPAQ; CPVI | The duration of pain cessation and opioid use decreased, and pain acceptance increased |
| Herbert et al[44] | United States | RCT | 64/65 | Veteran | Chronic pain (difference between remote and face-to-face intervention) | Telemedicine: 8-week ACT Manual Chronic Pain Intervention with 3-month and 6-month follow-up | Face to face ACT | BPI; PASS-20; CPAQ; PHQ-9; PSQI | Both groups had good effects on pain and anxiety. There was no significant effect on improving sleep | |
| Cosio[29] | United States | Quasi-experiment | 50/46 | No statistical difference | Veteran | Chronic pain | Twelve one-hour sessions using the ACT manual over a 10-week period | Cognitive Behavioral therapy is administered once or twice a week for 12 sessions | BPI; CPCI; BSI-18 | There was no significant difference in pain improvement between the two groups |
| Cosio and Schafer[45] | United States | Quasi-experiment | 50 | 29-79 | Veteran | Chronic pain | Twelve pain summation management sessions with ACT manual therapy, each one hour, for 10 weeks | BPI; CPCI; BSI-18 | Effective pain relief | |
| Grau et al[46] | United States | Quasi-experiment | 831 | Mean age 49.1 | Veteran | Depression | And received at least two ACT-D (Acceptance and Commitment Therapy for Depression) treatments | AAQ-II; PHQ-9 | Depression improved, and depression with PTSD was less effective | |
| Barnes et al[30] | United States | RCT | 35/35 | The median was 42/49 | Veteran | Suicide prevention | ACT (3 to 6 independent treatments) + conventional treatment,1 month, 3 months follow-up | Conventional treatment: Psychotropic drug therapy and individual and group psychotherapy; And all mental health services available after discharge | CSSRS; CSQ-8; AAQ-II | Suicide intention decreased and intervention acceptance was good |
| Kumpula et al[48] | United States | Quasi-experiment | 665/844/271 | 51.8/51.9/55.7 | Veteran | Suicide prevention | After 12 courses of ACT-D, BDI-II evaluation was performed before, during and at the end of treatment | Cognitive behavioral therap; Interpersonal Therapy | BDI-II | ACT was less effective at reducing suicidal intentions than the other two treatments |
| Walser(et al[49] | United States | Quasi-experiment | 981 | 50.5 | Veteran | Suicide prevention | At least 10 sessions of ACT-D therapy for 6 months with weekly 90 minutes phone consultations | BDI-II; AAQ-II; FFMQ | Suicidal intention decreased, mindfulness increased | |
| Karlin et al[50] | United States | Quasi-experiment | 731 | 51 ± 12.4 | Veteran | Depression | ACT-D: Part I a 3-day workshop personal experience; The second part was a weekly telephone consultation for 6 months | BDI-II WHOQOL-BREF | Depression and quality of life were significantly improved in the older group (> 65) and the younger group | |
| Afari et al[51] | United States | RCT | 45/43 | 56 ± 10.3/58.1 ± 9.5 | Male veteran | Lose weight | Four weekly 2-hour session ACT intervention sessions measuring baseline, 3-month, 6-month data | Behavioral weight loss intervention | Weight; BES; AAQ-W | The two interventions had the same effect on weight loss, and the effect of ACT on overeating control was weaker than behavioral weight loss |
| Heffner et al[52] | United States | RCT | 25/24 | 47.9 ± 13.3/54.8 ± 16.1 | Veteran | Give up smoking | Web-based ACT program: Vet Flexiquit, a 6-session online course and a 6-week SMS program | Smoke-free Veterans Program: Smoke free VET | Smoking quantity; FTND | There was no difference between the two groups, and combined treatment was recommended |
| Dindo et al[53] | United States | Mixed study | 31 | Rural veteran | Restoration of social function | A 1-day (5-hour) community ACT group workshop +5 thematic qualitative interviews were assessed 1 month and 3 months later | PCL-5; AAQ-II; OQ-45; M2C-Q | Pain, post-traumatic stress disorder symptoms, social inclusion, and psychoactivity were improved | ||
| Harvey et al[21] | New Zeeland | Quasi-experiment | 69/31 | Active serviceman | Alcohol use disorder | A 1-week ACT short course, intervention day 1, assessment 1 month later | Non-intervention population included in the study | AUDIT; BPAQ; PSS-10; GAD-7 | Emotional management, aggression, alcohol consumption, anxiety, stress, etc., were effectively improved |
Furthermore, this study evaluated the quality of the literature included in the quantitative meta-analysis using the Cochrane risk of bias tool standards (Figure 1B). Potential biases in each study, including random sequence generation, allocation concealment, blinding, and outcome assessment, were classified as low, high, or unclear risk. Studies with apparent deficiencies in randomization or allocation concealment were categorized as high risk of selection bias; cases with missing information or insufficient data to determine bias risk were considered unclear, whereas studies with proper randomization, allocation concealment, and adequately implemented blinding were assessed as low risk. This systematic evaluation ensures that each included study undergoes a comprehensive and fair quality review.
The ACT treatment model incorporates six therapeutic processes, with intervention contents tailored to different therapeutic themes. The primary intervention themes of ACT in military personnel include: (1) Improving symptoms of PTSD in military personnel: Focusing on enhancing resilience, improving social relationships, reducing interaction difficulties[18], integrating exposure therapy within the psychological flexibility framework, comparing the effectiveness of ACT with other methods, and integrating treatment for comorbidities (such as smoking cessation, alcohol use disorders) through continuous adaptation using the plan-do-study-act quality improvement model; (2) Pain management research in military personnel: Investigating the effectiveness of ACT in alleviating chronic pain, examining the influence of PTSD on the efficacy of ACT in pain management, preventing chronic pain post-orthopedic surgery, comparing the effects of telehealth vs face-to-face ACT interventions in pain reduction, contrasting the effectiveness of ACT with other behavioral therapies in pain management, and incorporating it as a behavioral medicine component in comprehensive chronic pain treatment; (3) Reducing anxiety and depression in military personnel, lowering suicide tendencies in veterans, and comparing the anti-depressive efficacy of ACT among elderly and young veterans; and (4) Other applications in military personnel include weight control, smoking cessation, aiding veterans in regaining social functionality, improving sleep, and managing alcohol use disorders.
Modes of ACT intervention in military personnel mainly include: (1) Remote ACT interventions via smartphone apps or online platforms; (2) Group therapy or workshops; (3) Individual therapy; and (4) A combination of group and individual therapy.
Based on the application of ACT in military personnel, the outcome indicators are categorized into five groups (Table 1): (1) PTSD symptom assessments such as PCL-5 and evaluations under the theoretical framework of ACT, like psychological flexibility and mindfulness; (2) Depression and anxiety-related scale assessments, along with sleep quality evaluation scales; (3) Pain intensity and pain acceptance level assessment scales; and (4) Satisfaction, social, and quality of life-related assessment scales. E. Evaluations of other application effects such as dependency on tobacco and alcohol, binge eating severity, and effectiveness in reintegration into society.
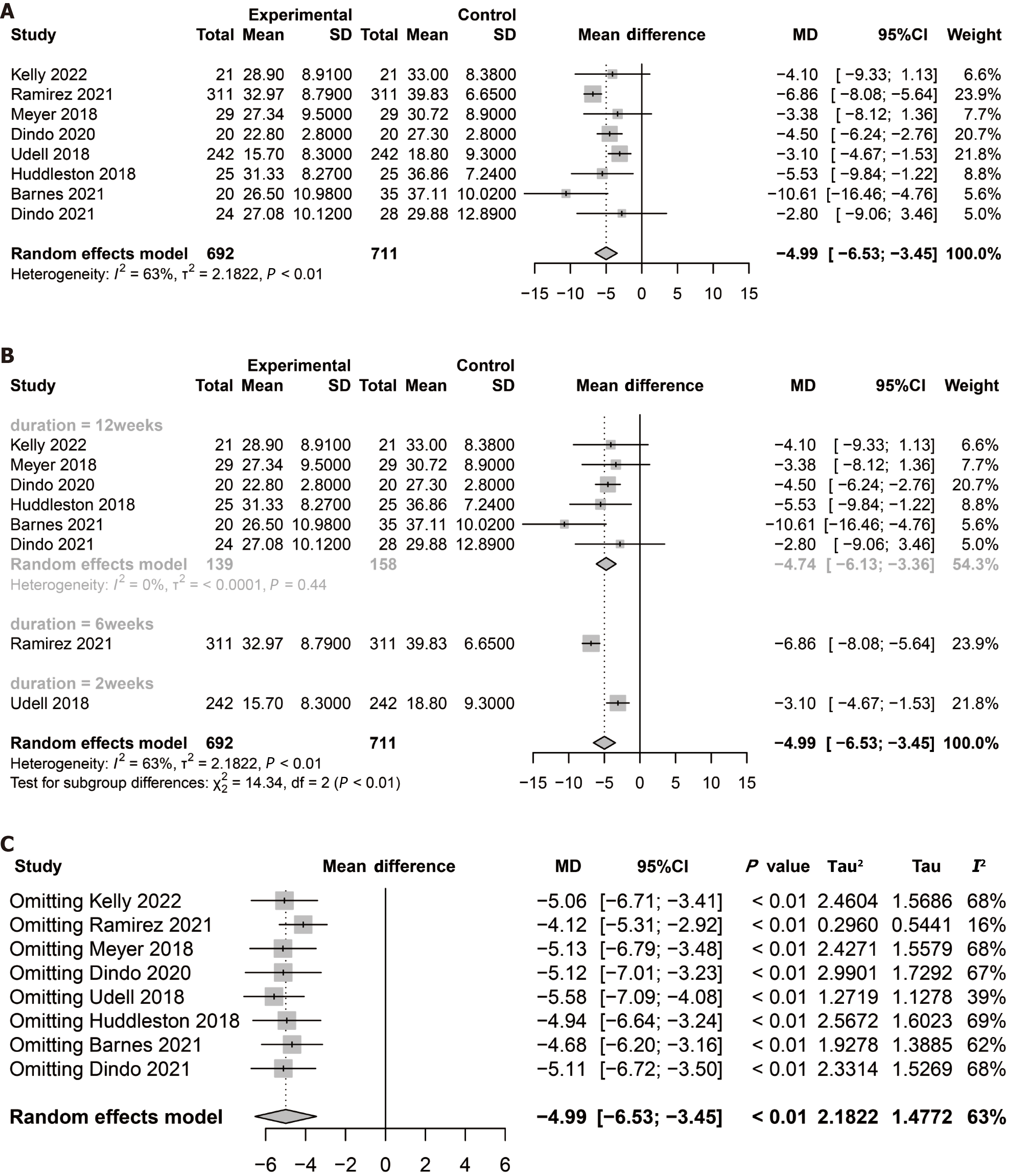
In this meta-analysis, we synthesized several studies to evaluate the impact of ACT on enhancing the mental health of military personnel (Figure 2A). The analysis included a total sample size of 1403 participants (692 in the experimental group and 711 in the control group), encompassing eight studies published between 2018 and 2022. This analysis aimed to explore the effectiveness of ACT within a military context, focusing on its potential value in improving mental health and examining the consistency of effects across different studies.
The results from the random-effects model, as displayed in the forest plot, indicate that the experimental group showed statistically significant improvements compared to the control group, with a MD of -4.99 and a 95%CI of (-6.53 to -3.45). This negative value indicates a significant improvement in mental health in the experimental group compared to the control group, suggesting that ACT can markedly reduce psychological stress in military personnel. It implies that those who received the intervention experienced a noticeable alleviation of stress, which may translate into better performance in executing military tasks and maintaining daily psychological well-being. Clinically, this result is highly significant as it supports the integration of ACT as an effective component of mental health interventions for military personnel.
However, it is essential to note the considerable heterogeneity (I2 = 63%) among the studies, which may limit the comparability of the results. Sources of heterogeneity could include differences in study design, specifics of the inter
This study's subgroup analysis evaluates the impact of different intervention durations on ACT's effectiveness in mental health interventions for military personnel (Figure 2B). The subgroups were based on the length of the intervention period, categorized into 12 weeks, 6 weeks, and 2 weeks. The results indicate that for the 12-week intervention, the random-effects model demonstrated a significant positive effect of ACT, with a combined MD of -4.74 and a 95%CI of (-6.13 to -3.36), suggesting a substantial improvement in mental health status. Notably, the heterogeneity for this subgroup was 0%, indicating high consistency in the study outcomes.
Results also showed significant improvements for the separate analyses of the 6-week and 2-week intervention periods. The significance test for differences between subgroups (P < 0.01) highlighted that the length of the intervention period is a crucial factor affecting treatment outcomes. This finding underscores the importance of considering the duration of ACT interventions to maximize their benefits on the mental health of military personnel.
These insights are vital for future research directions, especially when considering how to optimize ACT interventions to enhance their positive impact on the mental health of military personnel. Further research is needed to explore the effects of different intervention durations on treatment outcomes and how to adjust treatment plans based on military personnel's specific needs.
In the meta-analysis of this study, we conducted a sensitivity analysis of ACT's effects on military personnel's mental health. Sensitivity analysis assessed the impact of each study on the overall effect size by sequentially excluding each study (Figure 2C and Table 2). Forest plot results indicate that after the exclusion of any study, all MD values remained negative, and the 95%CIs did not include zero, signifying that ACT has a significant positive impact on improving the mental health of military personnel. After excluding any study, the P-values remained below 0.0001, further substantiating the significance of ACT's effects. Although the τ2 and τ values varied with the exclusion of different studies, these variations did not significantly affect the stability of the pooled effect size. Heterogeneity fluctuated across different sensitivity analyses but generally indicated moderate to high levels (47.2%-75.6%), suggesting some degree of variability among studies. The pooled estimate has a MD of -4.99 with a 95%CI of (-6.53 to -3.45) and an I² of 63%, indicating a significant improvement in the mental health of military personnel following ACT. This is reflected in the reduction of anxiety and stress symptoms, as well as the enhancement of psychological resilience. In clinical practice, this effect can help military personnel cope more effectively with task-related stress and improve their quality of life. Despite design and sample variations in individual studies, the overall effect remains robust and reliable.
| Deleted document | Pooled effect size of remaining literature (Pooled MD) | 95%CI for the remaining literature |
| Kelly et al[31] | -5.0595 | -6.7125 to -3.4065 |
| Ramirez et al[28] | -4.1187 | -5.3140 to -2.9234 |
| Meyer et al[35] | -5.1322 | -6.7874 to -3.4769 |
| Dindo et al[39] | -5.1192 | -7.0131 to -3.2253 |
| Udell et al[41] | -5.5820 | -7.0866 to -4.0773 |
| Huddleston et al[42] | -4.9395 | -6.2009 to -3.1573 |
| Barnes et al[30] | -4.6791 | -6.2009 to -3.1573 |
| Dindo et al[53] | -5.1108 | -6.7211 to -3.5005 |
Therefore, despite some heterogeneity, it can be concluded that ACT is a compelling psychological intervention for enhancing the mental health of military personnel, with robust effects across various studies. This finding is significant for guiding future therapeutic practices and research.
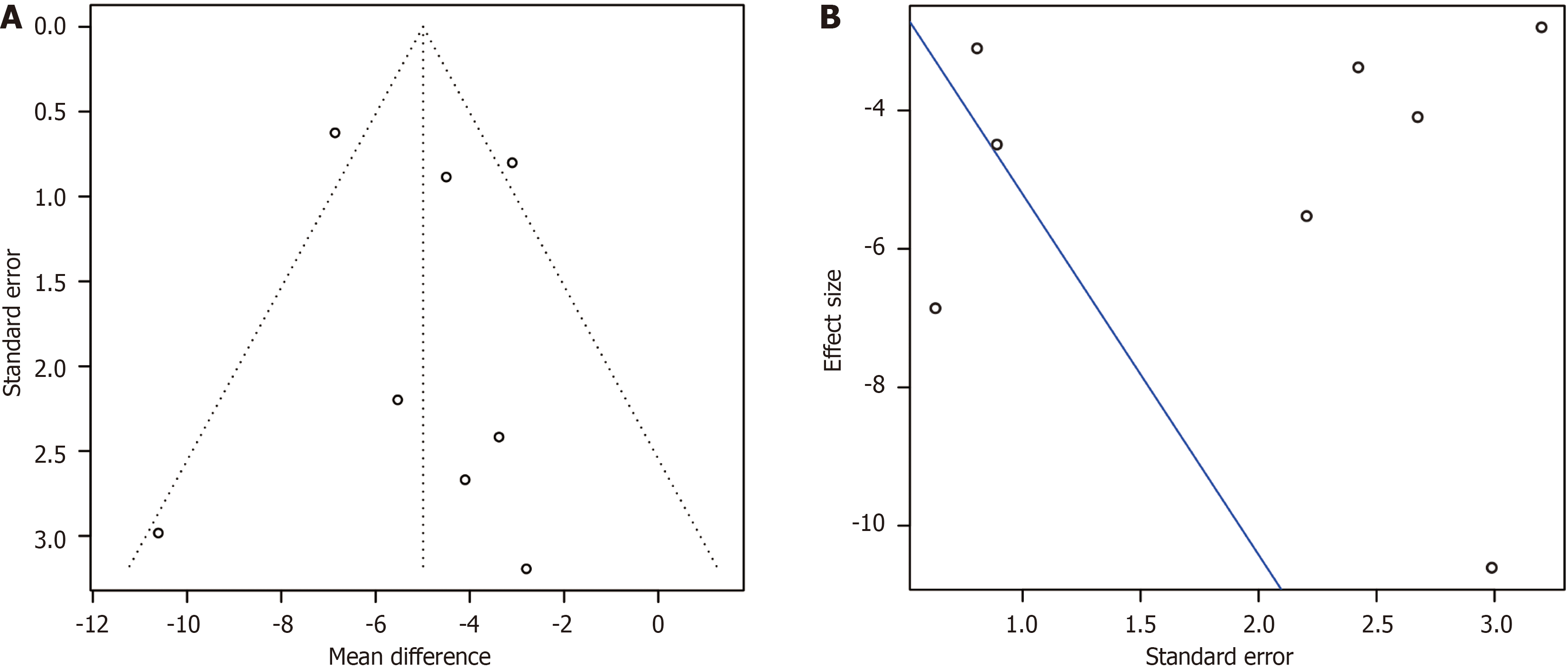
In our meta-analysis exploring the effect of ACT on improving mental health in military personnel, we conducted a publication bias assessment to evaluate the robustness of the results (Figure 3). Through visual inspection of a funnel plot and statistical examination using Egger's regression test, we assessed the reliability of our study findings.
The funnel plot (Figure 3A) illustrates the relationship between the effect sizes of individual studies and their standard errors. While there are deviations in the effect sizes of a few studies from the expected effect size, most of the studies cluster around the center, demonstrating a degree of symmetry that reduces the likelihood of publication bias. This indicates consistency in the study outcomes, enhancing the credibility of the meta-analysis conclusions.
For Egger's regression test (Figure 3B) results, we observed an estimated regression coefficient (b) of -5.5197 with a 95%CI ranging from -8.7432 to -2.2961. Although this suggests that effect size estimates might decrease with more minor standard errors, the t-value of 0.2803 with a corresponding P-value of 0.7887 indicates this trend is not statistically significant. This means we lack sufficient evidence to suggest the presence of publication bias.
In summary, the publication bias assessment results of this meta-analysis support the robust and credible estimation of ACT's effectiveness in enhancing the mental health of military personnel. Despite some heterogeneity among the studies, the overall findings still point to ACT as an effective psychological intervention method for improving the mental health of military personnel.
This study included 26 articles, of which 25[19] originated from the United States and one[20] from New Zealand. This distribution highlights the relatively limited research on the application of ACT in military personnel, with an uneven geographic distribution and no studies conducted domestically. The literature predominantly comprises quasi-experimental studies, with only nine RCTs[9], and some studies facing challenges such as small sample sizes, short intervention durations, and a lack of adequate controls, necessitating improvements in overall research quality[21]. Additionally, research is scarce on intervention methods and settings, such as differences in the effectiveness of digital, electronic, and internet-based remote treatments vs face-to-face manual ACT interventions[10], distinctions between group and individual therapies, and choices regarding the number and duration of intervention sessions. These factors significantly influence the cost and acceptance among military personnel, impacting the widespread application of such interventions[22]. The study population primarily consisted of veterans[23], with studies indicating concerning levels of mental health among Chinese veterans, including high rates of PTSD, depression, and anxiety, with a strong interconnection between these symptoms[24]. However, research on the mental health of Chinese military personnel has stalled in recent years. Therefore, there is an urgent need to draw upon international research findings to initiate the application of ACT in psychological interventions for Chinese veterans[25].
Recent years have seen ACT demonstrating promising outcomes in treating mental illnesses and behavioral disorders, offering a more flexible approach compared to traditional methods by tailoring practices to the specific circumstances of patients[26,27]. This has led to better comorbidity management, making ACT widely applied in addressing PTSD, depression, and non-suicidal self-injury behaviors[28]. Among the studies included in this research, it was consistently reported that military personnel have a good acceptance and satisfaction level towards ACT, marking it as a practical choice for addressing their psychological issues[29]. Notably, ACT has shown significant effectiveness in alleviating symptoms of PTSD among military personnel[30], particularly among female military personnel[31] though its su
Additionally, behaviors such as smoking and excessive alcohol consumption may serve as maladaptive coping mechanisms for PTSD, where ACT's effectiveness in addressing PTSD along with substance use disorders or chronic pain showcases an advantage over other therapies[33]. ACT has been found to be helpful in treating various conditions, including depression, anxiety, and chronic pain[34]. Military personnel with PTSD often exhibit significant interpersonal issues and social withdrawal, whereas ACT has filled the gap left by other therapies in restoring social functions and improving quality of life[35].
Pain is a common complaint among veterans seeking primary healthcare and one of the most frequently reported symptoms post-service[36]. ACT has been significantly effective in alleviating chronic pain in military personnel[37], enhancing pain acceptance[38], and reducing the use of post-surgical analgesics[38]. However, compared to other intervention methods, the superiority of ACT's effects is not consistently clear or may even appear weaker[39].
Anxiety and depression levels are notably higher in veterans than in civilians, often co-occurring with other physical symptoms and suicidal tendencies[40]. ACT has shown significant effectiveness in reducing anxiety and depression[41], and suicidal inclinations in veterans[42], proving to be equally effective in older populations[43] without demonstrating superiority over CBT and other treatments[44].
Furthermore, ACT has not shown a distinct advantage in smoking cessation or weight reduction among military personnel[45], and its effectiveness in improving sleep remains inconclusive[46].
In summary, while ACT has demonstrated positive effects in addressing various psychological issues in military personnel, further exploration is needed in integrating it with other psychological therapies and tailoring intervention choices.
The devastating impact of modern high-tech warfare and the harsh realities of combat can profoundly affect the psychological well-being of active service members and veterans, often leading to chronic mental health issues, functional decline, difficulties in reintegration into the community, and poor quality of life[47]. This underscores the urgent necessity of implementing and researching ACT psychological interventions within China. Given the findings from the included literature, practical applications of ACT should emphasize its advantages in treating PTSD combined with other psychological and behavioral disorders. This involves integrating ACT with other treatment plans for comprehensive management, training professional therapists, standardizing treatment protocols, and tailoring intervention programs to different military populations, such as selecting appropriate ACT protocols or manuals and setting reasonable content and session durations.
Research on ACT has varied significantly regarding sample sizes, intervention durations (ranging from one day to several months), and assessment metrics. There is a need for large-scale, multi-center RCTs to confirm the effectiveness of ACT locally[48].
In our meta-analysis investigating ACT's effectiveness in mental health interventions for military personnel, we systematically evaluated ACT's impact on improving mental health among this group. The quantitative analysis revealed that ACT significantly enhances the mental health of military personnel. Under the random-effects model, the pooled MD was -4.99 with a 95%CI of (-6.53 to -3.45), indicating a significant improvement in mental health metrics for the experimental group compared to the control group. Sensitivity analysis further confirmed the stability of this finding. The positive effects of ACT interventions were maintained regardless of the exclusion of any individual study, suggesting that no single study significantly influenced the overall conclusion. Based on the analysis results, we observed high heterogeneity (I2 = 63%), which mainly stems from differences in study design, intervention duration and delivery methods, and the psychological health status of participants. Further analysis revealed that the design variations between RCTs and quasi-experimental studies significantly impacted the robustness of the effect estimates. Studies with longer intervention durations (exceeding 12 weeks) showed a notable difference in effect size compared to short-term interventions, potentially exacerbating heterogeneity. Additionally, differences in outcomes between face-to-face and remote interventions were observed. The baseline psychological health levels of participants (such as a history of PTSD) also contributed to effect variability. Differences in the focus and intensity of intervention content (e.g., PTSD psychological adjustment vs psychological resilience training under everyday military stress) and the complexity of the military environment (such as the cultural atmosphere, management styles, and task pressures across different military bases) further increased heterogeneity. Future studies could use stratified or subgroup analyses to explore the impact of these characteristics more accurately, enhancing the interpretability of meta-analysis results.
Despite high heterogeneity (I2 = 63%), this analytical approach demonstrates the robust positive impact of ACT on the mental health of military personnel. Tests for publication bias also affirmed the robustness of these findings, with neither funnel plots nor Egger's regression test indicating significant publication bias, thereby enhancing the credibility of our conclusions. This suggests that, despite diversity in study design and sample selection, our meta-analysis accurately reflects the actual effectiveness of ACT in mental health interventions for military personnel. Integrating these data, we can emphasize in our discussion the potential of ACT as an intervention measure for improving the psychological well-being of military populations, especially given the unique psychological challenges and stressors they face. ACT offers potent psychological support in this context. Our findings encourage clinicians and mental health policymakers to consider including ACT in mental health interventions for military personnel (Figure 4).
This study confirms ACT's efficacy within the scientific research domain and underscores its significant value in clinical practice. As a flexible psychological intervention, ACT offers effective treatment avenues for a variety of mental health challenges faced by military personnel. Its core therapeutic processes—acceptance, cognitive defusion, and committed action—provide military personnel with new coping strategies, aiding them in better managing and accepting psychological traumas, thereby engaging in more meaningful lives. These findings offer mental health professional potent therapeutic tools and provide a scientific basis for the development and implementation of mental health intervention programs within the military. Furthermore, the results support the broader and more systematic application of ACT in military training and psychological rehabilitation, contributing to enhanced psychological resilience and overall well-being among military personnel.
Despite providing compelling evidence of ACT's effectiveness in mental health interventions for military personnel, this study has limitations. First, the included studies exhibit high heterogeneity, possibly due to differences in study design, sample size, intervention duration, and intensity. For instance, in the selected literature for this study, the number of military populations from non-Western backgrounds was insufficient. This limitation raises concerns about the generalizability of the findings on a global scale, making it difficult to ascertain whether ACT would be equally effective in psychological interventions for military personnel who grew up in different cultural and regional contexts. After all, there are significant differences between Western and non-Western settings in terms of values, military management styles, and perceptions of mental health issues. This shortcoming may lead to hesitations in applying the study's findings in some regions. Second, while a random-effects model was used in the meta-analysis to mitigate the impact of heterogeneity, quality issues in some studies could still affect the accuracy and reliability of the overall results. Additionally, the publication bias, assessed through Egger's regression test and Begg's funnel plot, cannot be entirely ruled out as a potential influence on the outcomes. Future research requires more rigorous and standardized study designs to enhance the quality and credibility of the findings.
Considering these limitations and the current study's findings, future research should focus on several key areas. Firstly, future research should focus on large-sample, multicenter RCTs to further validate the effectiveness of ACT in military mental health interventions. Additionally, original studies should be conducted to explore the specific applicability and intervention outcomes of ACT in diverse military populations. Methodological research will be crucial for optimizing the implementation strategies of ACT in military settings, providing a basis for enhancing its efficacy. Broad systematic review studies should also comprehensively analyze the intervention mechanisms of ACT and its implementation across various environments, further solidifying the theoretical foundation and empirical support for ACT in the field of military mental health.
Secondly, exploring the effects of ACT in different military environments and populations, while considering the influence of culture, environmental factors, and task specificity, will aid in developing more tailored and effective intervention strategies. Future research should pay greater attention to the applicability of ACT in diverse military environments and cultural contexts, with a focus on its global relevance for military mental health interventions. It is recommended to address common psychological health needs among military personnel from different countries and regions, particularly issues related to post-traumatic stress, stress from overseas deployment, and cultural adaptation. This involves delving into the mechanisms of ACT's core processes (such as acceptance and cognitive defusion) in mitigating cross-cultural psychological stress to enhance its theoretical support.
Methodologically, it is advisable to control for cultural variables in the design of multicenter RCTs and compare the effects across military populations from different countries, ensuring methodological transparency and generalizability of the findings. Additionally, research should examine the effectiveness of various implementation methods, such as in-person interventions vs remote telehealth platforms, assessing resource utilization efficiency and the degree to which military personnel engage with ACT content. Exploring optimal implementation schemes tailored to different in
Through systematic evaluation and meta-analysis, this study assessed the application effectiveness of ACT in improving mental health among military personnel. The findings reveal that ACT significantly improves PTSD, post-surgical or chronic pain, anxiety, depression, weight control, smoking cessation, and alcohol use disorders. These results align with existing literature on the effectiveness of ACT in the general population, further affirming ACT's applicability in a particular group—military personnel. Notably, the study finds ACT particularly effective in treating PTSD, which is of significant practical importance for a group frequently exposed to traumatic events. Additionally, the study highlights the potential of ACT in promoting mental health among military personnel, providing scientific evidence for its broader application in future military mental health interventions.
| 1. | Morse JL, Fishbein JN, Wooldridge JS, Herbert MS, Afari N. Posttraumatic Stress Disorder and Weight Loss in Male and Female Active-duty Service Members: A Weight Management Study. Mil Med. 2025. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Stegerhoek P, Kooijman K, Ziesemer K, IJzerman H, Kuijer PPFM, Verhagen E. Risk factors for adverse health in military and law enforcement personnel; an umbrella review. BMC Public Health. 2024;24:3151. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Seidaliyeva U, Ilipbayeva L, Taissariyeva K, Smailov N, Matson ET. Advances and Challenges in Drone Detection and Classification Techniques: A State-of-the-Art Review. Sensors (Basel). 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 4. | Wise PH, Shiel A, Southard N, Bendavid E, Welsh J, Stedman S, Fazal T, Felbab-Brown V, Polatty D, Waldman RJ, Spiegel PB, Blanchet K, Dayoub R, Zakayo A, Barry M, Martinez Garcia D, Pagano H, Black R, Gaffey MF, Bhutta ZA; BRANCH Consortium. The political and security dimensions of the humanitarian health response to violent conflict. Lancet. 2021;397:511-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Khorram-Manesh A, Burkle FM, Goniewicz K, Robinson Y. Estimating the Number of Civilian Casualties in Modern Armed Conflicts-A Systematic Review. Front Public Health. 2021;9:765261. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 6. | Schieffler DA, Matta SE. Evidence to Support the Use of S-Adenosylmethionine for Treatment of Post-Concussive Sequelae in the Military. Mil Med. 2022;187:e1182-e1192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Sherman H, Frye-Cox N, Lucier-Greer M. Combat Deployment Experiences and Soldier Mental Health: Examining the Factor Structure of a Combat Experiences Scale. Mil Med. 2023;188:e1156-e1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Bessey AF, Black KJ, Britt TW. A bidirectional examination of mental health symptoms and perceptions of leader support: Which comes first? Mil Psychol. 2023;35:119-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Mureșanu IA, Grad DA, Mureșanu DF, Dobran SA, Hapca E, Strilciuc Ș, Benedek I, Capriș D, Popescu BO, Perju-Dumbravă L, Cherecheș RM. Evaluation of post-traumatic stress disorder (PTSD) and related comorbidities in clinical studies. J Med Life. 2022;15:436-442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 10. | Voth M, Chisholm S, Sollid H, Jones C, Smith-MacDonald L, Brémault-Phillips S. Efficacy, Effectiveness, and Quality of Resilience-Building Mobile Health Apps for Military, Veteran, and Public Safety Personnel Populations: Scoping Literature Review and App Evaluation. JMIR Mhealth Uhealth. 2022;10:e26453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Yan X, Wang X, Chen Y, Xu X, Peng L, Xu Y. Feasibility and effects of mindfulness-based stress reduction (MBSR) for improving resilience, posttraumatic stress disorder symptoms and posttraumatic growth among military medical college students. Acta Psychol (Amst). 2024;251:104556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Zorzela L, Loke YK, Ioannidis JP, Golder S, Santaguida P, Altman DG, Moher D, Vohra S; PRISMAHarms Group. PRISMA harms checklist: improving harms reporting in systematic reviews. BMJ. 2016;352:i157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 325] [Cited by in RCA: 388] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 13. | Zhao C, Zhao Z, Levin ME, Lai L, Shi C, Hu J, Chen W, Ren Z. Efficacy and acceptability of mobile application-delivered acceptance and commitment therapy for posttraumatic stress disorder in China: A randomized controlled trial. Behav Res Ther. 2023;171:104440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Hong B, Yang S, Hyeon S, Kim S, Lee J. Third-wave cognitive behavioral therapies for caregivers of cancer patients: a scoping review. BMC Complement Med Ther. 2023;23:360. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Shen YC, Heissel J, Bacolod M. Core Mental Health Clinician Capacity and Use Rates in the US Military. JAMA Netw Open. 2024;7:e2434246. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Corry NH, Radakrishnan S, Williams CS, Woodall KA, Stander VA. Longitudinal association of health behaviors and health-related quality of life with military spouse readiness. BMC Public Health. 2024;24:1341. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Makris T, Dorstyn DS. Third-wave psychotherapies to promote mental health in epilepsy: An updated systematic review. Epilepsy Behav. 2022;134:108766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | McCracken LM, Vowles KE. Acceptance and commitment therapy and mindfulness for chronic pain: model, process, and progress. Am Psychol. 2014;69:178-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 388] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 19. | Walser RD, O'Connell M. Acceptance and commitment therapy and the therapeutic relationship: Rupture and repair. J Clin Psychol. 2021;77:429-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Crump L, LaChapelle D. "Don't need [therapy]! Not necessary, that's what we're for!": Does content from fibromyalgia Facebook peer support groups emulate psychological flexibility principles? PEC Innov. 2023;2:100144. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Harvey ST, Henricksen A, Bimler D, Dickson D. Addressing anger, stress, and alcohol-related difficulties in the military: an ACT intervention. Mil Psychol. 2017;29:464-476. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Smith-MacDonald L, Lusk J, Lee-Baggley D, Bright K, Laidlaw A, Voth M, Spencer S, Cruikshank E, Pike A, Jones C, Bremault-Phillips S. Companions in the Abyss: A Feasibility and Acceptability Study of an Online Therapy Group for Healthcare Providers Working During the COVID-19 Pandemic. Front Psychiatry. 2021;12:801680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Ruisch JE, Nederstigt AHM, van der Vorst A, Boersma SN, Vink MT, Hoeboer CM, Olff M, Sobczak S. Treatment of post-traumatic stress disorder in people with dementia: a structured literature review. Psychogeriatrics. 2023;23:523-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Reyes AT, Song H, Bhatta TR, Kearney CA. Exploring the relationships between resilience, mindfulness, and experiential avoidance after the use of a mindfulness- and acceptance-based mobile app for posttraumatic stress disorder. Perspect Psychiatr Care. 2022;58:776-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Rowe-Johnson MK, Browning B, Scott B. Effects of acceptance and commitment therapy on trauma-related symptoms: A systematic review and meta-analysis. Psychol Trauma. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Bluett EJ, Homan KJ, Morrison KL, Levin ME, Twohig MP. Acceptance and commitment therapy for anxiety and OCD spectrum disorders: an empirical review. J Anxiety Disord. 2014;28:612-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 170] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 27. | Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, Currie M, Qureshi R, Mattis P, Lisy K. Systematic reviews of etiology and risk, in Joanna Briggs Institute reviewer’s manual. 2020. [DOI] [Full Text] |
| 28. | Ramirez MW, Woodworth CA, Evans WR, Grace GA, Schobitz RP, Villarreal SA, Howells CJ, Gissendanner RD, Katko NJ, Jones KN. A trauma-focused intensive outpatient program integrating elements of exposure therapy with acceptance and commitment therapy: Program development and initial outcomes. J Contextual Behav Sci. 2021;21:66-72. |
| 29. | Cosio D. Practice-based evidence for outpatient, acceptance and commitment therapy for veterans with chronic, non-cancer pain. J Contextual Behav Sci. 2016;5:23-32. |
| 30. | Barnes SM, Borges LM, Smith GP, Walser RD, Forster JE, Bahraini NH. Acceptance and commitment therapy to promote recovery from suicidal crises: A randomized controlled acceptability and feasibility trial of ACT for life. J Contextual Behav Sci. 2021;20:35-45. |
| 31. | Kelly MM, Reilly ED, Ameral V, Richter S, Fukuda S. A Randomized Pilot Study of Acceptance and Commitment Therapy to Improve Social Support for Veterans with PTSD. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 32. | Reyes AT, Bhatta TR, Muthukumar V, Gangozo WJ. Testing the acceptability and initial efficacy of a smartphone-app mindfulness intervention for college student veterans with PTSD. Arch Psychiatr Nurs. 2020;34:58-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 33. | Thoma N, Pilecki B, McKay D. Contemporary Cognitive Behavior Therapy: A Review of Theory, History, and Evidence. Psychodyn Psychiatry. 2015;43:423-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 92] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 34. | Gobin RL, Strauss JL, Golshan S, Allard CB, Bomyea J, Schnurr PP, Lang AJ. Gender Differences in Response to Acceptance and Commitment Therapy Among Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn Veterans. Womens Health Issues. 2019;29:267-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Meyer EC, Walser R, Hermann B, La Bash H, DeBeer BB, Morissette SB, Kimbrel NA, Kwok OM, Batten SV, Schnurr PP. Acceptance and Commitment Therapy for Co-Occurring Posttraumatic Stress Disorder and Alcohol Use Disorders in Veterans: Pilot Treatment Outcomes. J Trauma Stress. 2018;31:781-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 36. | Jacobs ML, Luci K, Hagemann L. Group-based Acceptance and Commitment Therapy (ACT) for Older Veterans: Findings from a Quality Improvement Project. Clin Gerontol. 2018;41:458-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 37. | Lang AJ, Schnurr PP, Jain S, He F, Walser RD, Bolton E, Benedek DM, Norman SB, Sylvers P, Flashman L, Strauss J, Raman R, Chard KM. Randomized controlled trial of acceptance and commitment therapy for distress and impairment in OEF/OIF/OND veterans. Psychol Trauma. 2017;9:74-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 38. | Kelly MM, Sido H, Forsyth JP, Ziedonis DM, Kalman D, Cooney JL. Acceptance and commitment therapy smoking cessation treatment for veterans with posttraumatic stress disorder: a pilot study. J Dual Diagn. 2015;11:50-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 39. | Dindo L, Johnson AL, Lang B, Rodrigues M, Martin L, Jorge R. Development and evaluation of an 1-day Acceptance and Commitment Therapy workshop for Veterans with comorbid chronic pain, TBI, and psychological distress: Outcomes from a pilot study. Contemp Clin Trials. 2020;90:105954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 40. | Herbert MS, Malaktaris AL, Dochat C, Thomas ML, Wetherell JL, Afari N. Acceptance and Commitment Therapy for Chronic Pain: Does Post-traumatic Stress Disorder Influence Treatment Outcomes? Pain Med. 2019;20:1728-1736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 41. | Udell CJ, Ruddy JL, Procento PM. Effectiveness of Acceptance and Commitment Therapy in Increasing Resilience and Reducing Attrition of Injured US Navy Recruits. Mil Med. 2018;183:e603-e611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 42. | Huddleston C, Martin L, Woods K, Dindo L. One-Day Behavioral Intervention for Distressed Veterans with Migraine: Results of a Multimethod Pilot Study. Mil Med. 2018;183:e184-e192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 43. | Dindo L, Zimmerman MB, Hadlandsmyth K, StMarie B, Embree J, Marchman J, Tripp-Reimer T, Rakel B. Acceptance and Commitment Therapy for Prevention of Chronic Postsurgical Pain and Opioid Use in At-Risk Veterans: A Pilot Randomized Controlled Study. J Pain. 2018;19:1211-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 76] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 44. | Herbert MS, Afari N, Liu L, Heppner P, Rutledge T, Williams K, Eraly S, VanBuskirk K, Nguyen C, Bondi M, Atkinson JH, Golshan S, Wetherell JL. Telehealth Versus In-Person Acceptance and Commitment Therapy for Chronic Pain: A Randomized Noninferiority Trial. J Pain. 2017;18:200-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 45. | Cosio D, Schafer T. Implementing an acceptance and commitment therapy group protocol with veterans using VA's stepped care model of pain management. J Behav Med. 2015;38:984-997. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 46. | Grau PP, Sripada RK, Ganoczy D, Weinstein JH, Pfeiffer PN. Outcomes of Acceptance and Commitment Therapy for depression and predictors of treatment response in Veterans Health Administration patients. J Affect Disord. 2023;323:826-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 47. | Donahue ML, Fruge JE, Andresen FJ, Twohig MP. Acceptance and commitment therapy (ACT) among US veterans: A systematic review. J Contextual Behav Sci. 2024;100731. |
| 48. | Kumpula MJ, Wagner HR, Dedert EA, Crowe CM, Day KT, Powell K, Batdorf WH, Shabana H, Kim E, Kimbrel NA. An Evaluation of the Effectiveness of Evidence-Based Psychotherapies for Depression to Reduce Suicidal Ideation among Male and Female Veterans. Womens Health Issues. 2019;29 Suppl 1:S103-S111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 49. | Walser RD, Garvert DW, Karlin BE, Trockel M, Ryu DM, Taylor CB. Effectiveness of Acceptance and Commitment Therapy in treating depression and suicidal ideation in Veterans. Behav Res Ther. 2015;74:25-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 50. | Karlin BE, Walser RD, Yesavage J, Zhang A, Trockel M, Taylor CB. Effectiveness of acceptance and commitment therapy for depression: comparison among older and younger veterans. Aging Ment Health. 2013;17:555-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 51. | Afari N, Herbert MS, Godfrey KM, Cuneo JG, Salamat JS, Mostoufi S, Gasperi M, Ober K, Backhaus A, Rutledge T, Wetherell JL. Acceptance and commitment therapy as an adjunct to the MOVE! programme: a randomized controlled trial. Obes Sci Pract. 2019;5:397-407. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 52. | Heffner JL, Kelly MM, Reilly ED, Reece SG, Claudio T, Serfozo E, Baker K, Watson NL, Karekla M. An Avatar-Led Web-Based and SMS Text Message Smoking Cessation Program for Socioeconomically Disadvantaged Veterans: Pilot Randomized Controlled Trial. JMIR Form Res. 2023;7:e44503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 53. | Dindo L, Roddy MK, Boykin D, Woods K, Rodrigues M, Smith TL, Gonzalez RD, True G. Combination outreach and wellness intervention for distressed rural veterans: results of a multimethod pilot study. J Behav Med. 2021;44:440-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |