Published online Jan 19, 2025. doi: 10.5498/wjp.v15.i1.100685
Revised: October 28, 2024
Accepted: November 26, 2024
Published online: January 19, 2025
Processing time: 117 Days and 8 Hours
Bipolar disorder (BD) is a severe mental illness characterized by significant mood swings. Effective drug treatment modalities are crucial for managing BD.
To analyze the current status and future trends of global research on BD drug treatment over the last decade.
The Web of Science Core Collection database spanning from 2015 to 2024 was utilized to retrieve literature related to BD drug treatment. A total of 2624 articles were extracted. Data visualization and analysis were conducted using CiteSpace, VOSviewer, Pajek, Scimago Graphica, and R-studio bibliometrix to identify research hotspots, key contributors, and future trends.
The United States, China, and the United Kingdom have made the most significant contributions to research on BD drug treatment and formed notable research collaboration networks. The University of Pittsburgh, Massachusetts General Hospital, and the University of Michigan have been identified as the major research institutions in this field. The Journal of Affective Disorders is the most influential journal. A keyword analysis revealed research hotspots related to clinical symptoms, drug efficacy, and genetic mechanisms. A citation analysis identified the management guidelines published by Yatham et al in 2018 as the most cited paper.
This study provides a detailed overview of the field of BD drug treatment, highlighting key contributors, research hotspots, and future directions. The study findings can be employed as a reference for future research and policymaking, which may enable further development and optimization of BD pharmacotherapy.
Core Tip: This study employs advanced bibliometric tools, including CiteSpace, VOSviewer, and the bibliometrix package in R, to analyze the evolution of pharmacotherapy for bipolar disorder over the past decade. It identifies key contributors, research hotspots, and future trends, emphasizing significant international collaborations, particularly among institutions in the United States, China, and the United Kingdom. The findings highlight key areas such as clinical symptoms, drug efficacy, and genetic mechanisms, providing valuable insights for scholars and policymakers. This work offers clear guidance for innovation in bipolar disorder pharmacotherapy and serves as a critical reference for future research.
- Citation: Chen BF, Liu L, Lin FZ, Zeng HM, Huang HQ, Zhang CF, Liu CC, Chen X, Peng J, Wang YF, Wang ZL, Chen B, Liu DL, Liu Y, Li ZZ, Zeng XX. Comprehensive bibliometric analysis of pharmacotherapy for bipolar disorders: Present trends and future directions. World J Psychiatry 2025; 15(1): 100685
- URL: https://www.wjgnet.com/2220-3206/full/v15/i1/100685.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i1.100685
Bipolar disorder (BD) is a mental illness characterized by severe mood swings, including episodes of mania and major depression, and it typically follows a recurrent course. BD is commonly categorized into two subtypes: Bipolar I disorder (BD-I) and bipolar II disorder (BD-II)[1]. In BD-I, there should be at least one manic episode, which involves elevated mood, emotional instability, impulsivity, and excessive energy, with or without one or more episodes of major depression. BD-II is characterized by at least one major depressive episode accompanied by hypomania, without full-blown manic episodes[2,3]. The lifetime prevalence of BD is approximately 1%-2%, with two peak periods of onset at ages 15-24 and 45-54[4]. Although the exact etiology of BD remains unclear, it is generally believed to result from an interplay between genetic and environmental factors. Multiple studies have shown that first-degree relatives of BD probands have a 7.9-fold higher risk and second-degree relatives have a 3.3-fold higher risk, compared to families without any probands. Additionally, twin studies indicate a heritability of 70%-80% for BD[5,6]. Social and environmental factors significantly impact the development of BD, with childhood abuse (particularly emotional abuse), stressful life events (such as disability or divorce), and substance abuse (including alcohol and cannabis) increasing the risk of developing BD[7-9].
Currently, the treatment of BD primarily involves pharmacotherapy combined with various psychological inter
Bibliometrics is the study of the development of scientific research and academic communication through the quantitative analysis of literature and citation data. It is an important tool to evaluate the credibility and impact of academic research[15]. As it involves quantitative, multi-dimensional analysis and long-term trend observation of data, it reflects the status of communication and collaboration within the academic community, identifies new research frontiers, hot topics, and academic trends, and provides researchers with directions and inspiration for working in their respective fields[16]. Although a substantial body of research on the pharmacological treatment of BD is available, there is a lack of bibliometric analyses specifically focused on BD and its pharmacological treatments. This study uses bibliometric methods to conduct a global analysis of the current state and future trends in BD pharmacological treatment over the last decade. It aims to identify research hotspots and future directions in the field of BD, in order to provide a more comprehensive and in-depth understanding of its pharmacological treatment.
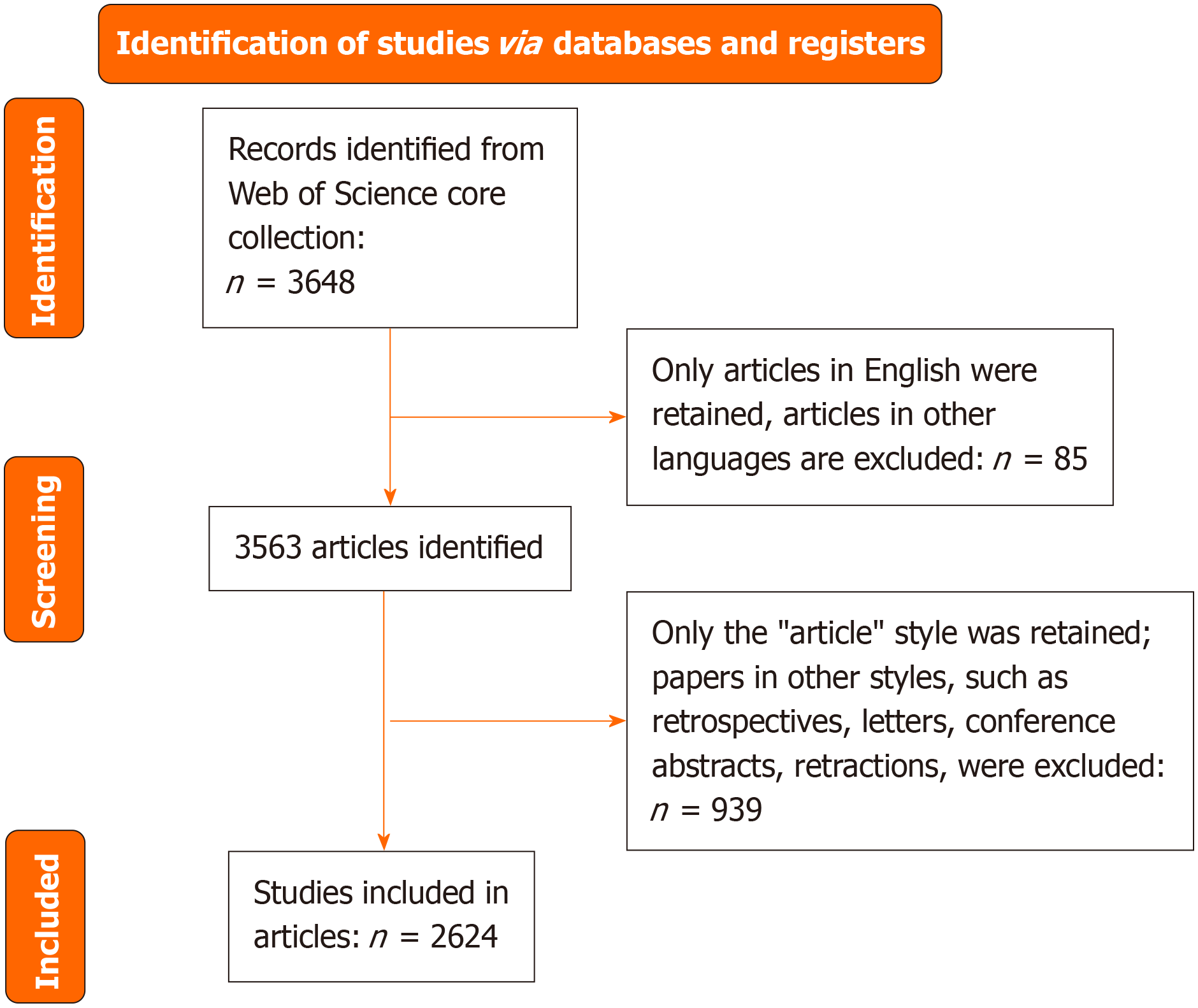
We conducted a comprehensive search of the literature on BP using the Web of Science Core Collection database, spanning from 2015 to 2024. The search formula was set as (((TS = (“bipolar disorder” OR “bipolar I disorder” OR “bipolar II disorder”)) AND (TS = (“medication” OR “drug treatment” OR “drug therapy” OR “pharmacotherapy”)) AND (PY = (2015-2024))). We were able to identify 3648 documents, from which we excluded 85 non-English articles and 939 documents not classified as “article”. Consequently, we ultimately included 2624 articles (Figure 1). The filtered data were exported as text files and visualized using CiteSpace (version 6.1.R6), VOSviewer (version 1.6.20), Pajek (version 32.5.18), Scimago Graphica (version 1.0.39.0), the bibliometrix package in R-studio, and Excel (Office 2021).
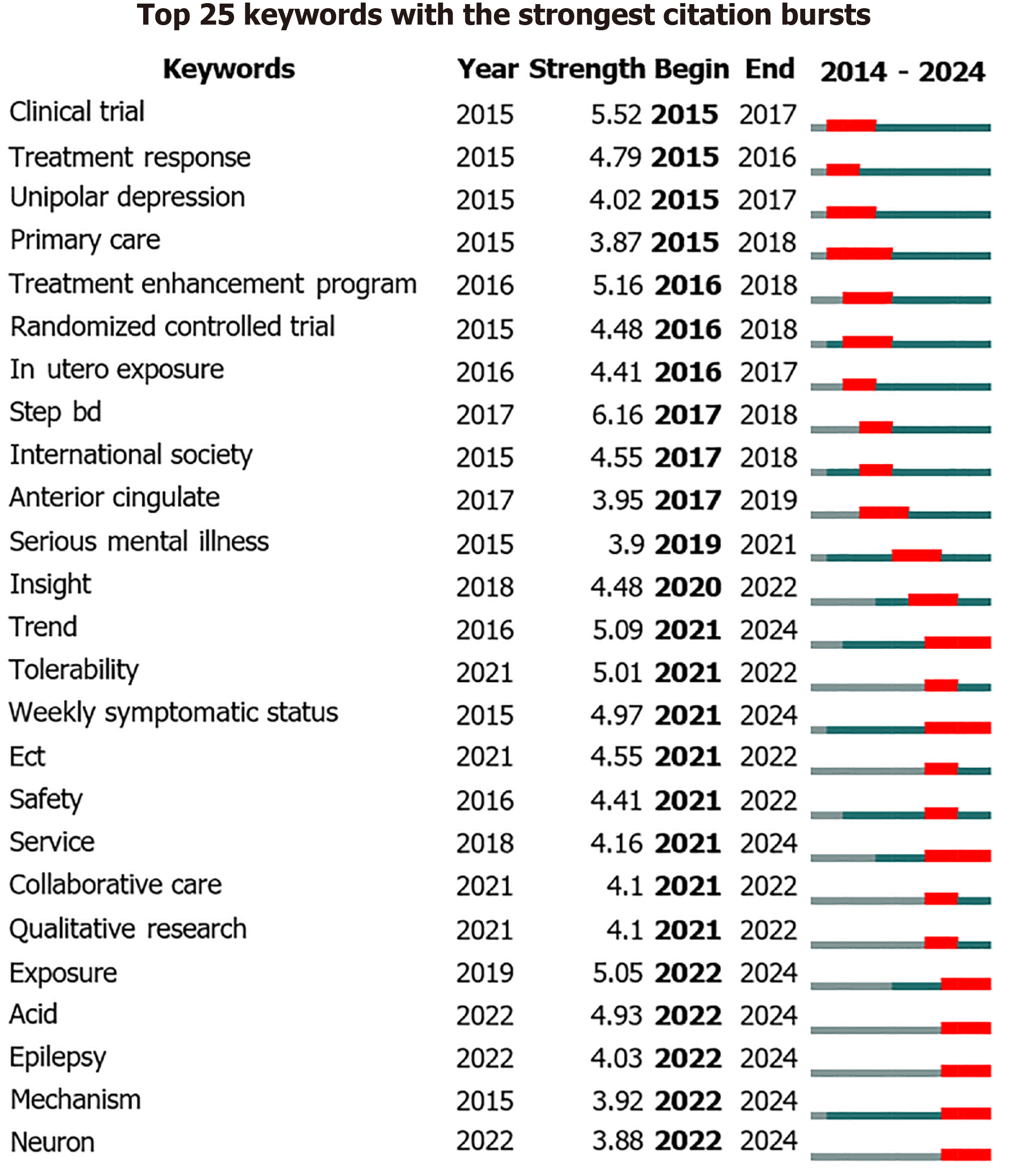
CiteSpace is a visualization analysis tool that operates within a Java environment. It leverages bibliometrics, co-occurrence analysis, and cluster analysis to study and visualize hotspots and research frontiers within specific knowledge domains[17]. First, we imported the data into CiteSpace to create citation burst charts for the top 15 cited articles and keyword burst charts for the top 25 keywords appearing in the included articles. “Year” indicates the starting year of the citation or keyword appearance, “Strength” represents the intensity of the citation or keyword occurrence, “Begin” denotes the starting year of the citation or keyword burst, and “End” indicates the ending year. Each line segment represents a period, with red bars indicating the duration of a strong citation burst[18,19].
VOSviewer is an application that runs on a Java environment and can be used to create, visualize, and explore maps based on any type of network data, primarily for bibliometric network analysis[20,21]. We utilized VOSviewer to generate visualizations of author collaboration networks, institutional collaboration networks, overlay maps of research field distributions, and keyword co-occurrence networks. Pajek is a powerful tool for adjusting various complex network diagrams. To enhance the clarity of nodes, concentrate similar clusters, and improve the overall aesthetics of the scientific network diagrams, we combined Pajek with VOSviewer to adjust the visual effects of scientific network diagrams[22]. In the adjusted diagrams, we can intuitively see that nodes of the same color belong to the same cluster and exhibit a certain degree of collaboration. The size of the nodes is related to the frequency of the occurrence of the relevant content, while the lines between the nodes indicate a certain degree of correlation[23-25].
Scimago Graphica is a user-friendly, free, no-code tool that does not rely on a Java environment and allows for the creation of complex visualizations through simple drag-and-drop interactions[26]. We used Scimago Graphica for assessing global collaborations, analyzing country citation strength, and comparing link strength. The upper right corner of the diagrams lists labels explaining the information represented by the nodes, lines, and colors, making them simple, clear, and aesthetically pleasing.
The R-studio bibliometrix package is a bibliometric analysis software tool developed by Massimo Aria and others. It inputs a code within the R language environment to run bibliometrix, an open-source tool used for a comprehensive scientific mapping analysis of scientific literature[27].
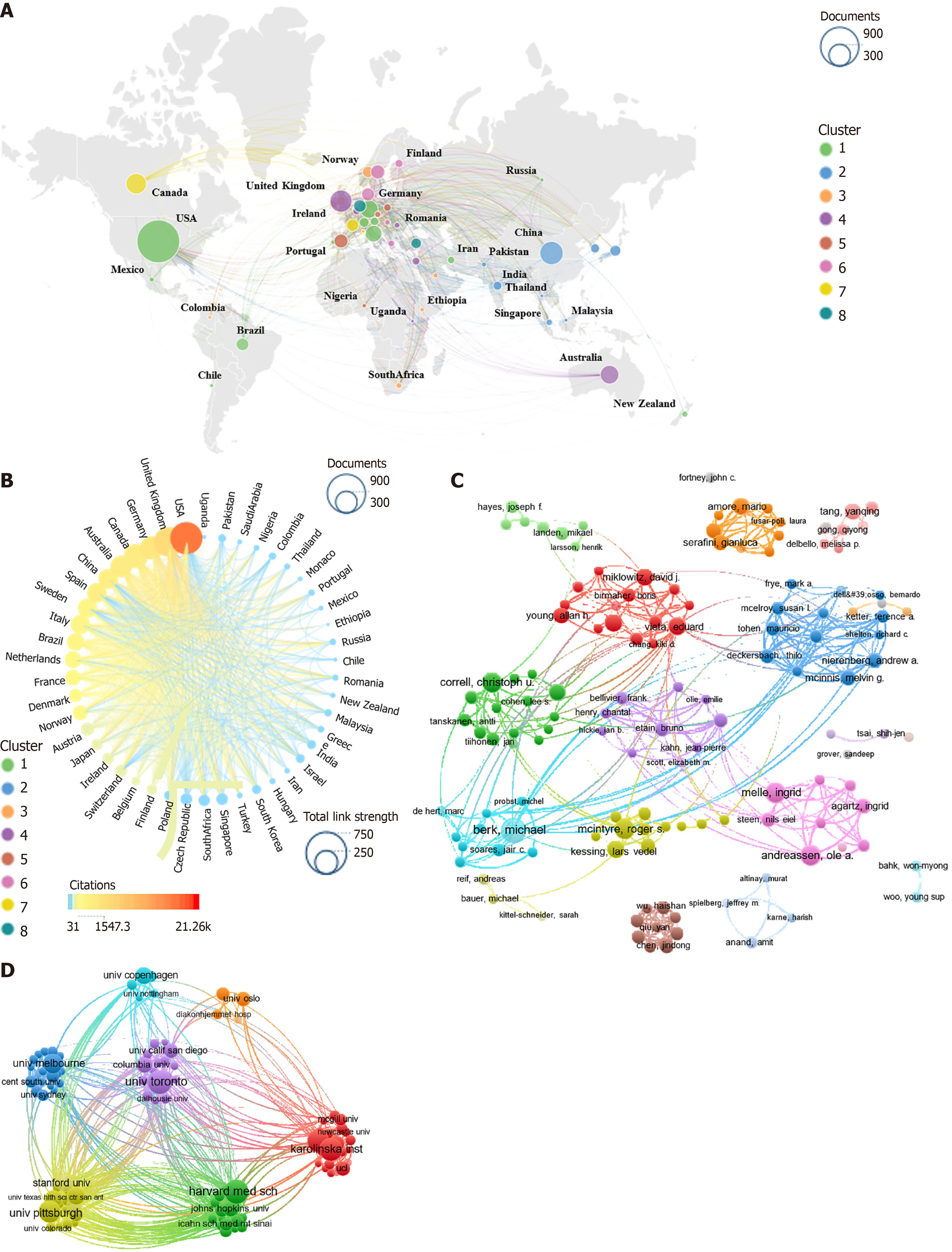
A global map of publications related to BD and its pharmacotherapy is presented (Figure 2A). The size of the circles indicates the volume of publications, while different colors represent various country clusters. Over the past decade, North America, East Asia, and Western Europe have made significant contributions to advances in BD pharmacotherapy. Australia has also played a notable role in this field. All countries involved in this research field are categorized into eight major clusters based on the extent of their collaboration. The green cluster, led by the United States, has the highest productivity, followed by the blue cluster, led by China. We further examined countries/regions based on the strength of their collaborative links and revealed the total citation frequency of different countries (Figure 2B). The size of the circles represents the strength of a country’s collaborative links, while the color intensity indicates the total citation frequency. A positive correlation was noted between the size of the circles and the intensity of the color. The United States leads in both the collaborative link strength and total citation frequency, followed by the United Kingdom, Germany, and Canada. In total, 20 countries were found to have a total citation frequency exceeding 31000.
This study analyzes the collaboration networks and productivity of authors through co-authorship mapping (Figure 2C). The size of the circles represents the number of publications. Different colors denote different clusters of authors. A total of 133 authors with more than five publications each were grouped into over ten author clusters based on their collaborations. The dark blue cluster, led by McInnis MG and Nierenberg AA, is the primary author cluster. The red cluster led by Vieta E and the dark green cluster led by Correll CU are also identified as key author clusters in the field over the last decade. 120 institutions with more than ten publications each were grouped into seven main institutional clusters based on their collaborations (Figure 2D). The yellow cluster, led by the University of Pittsburgh, has been the dominant institutional cluster in this field over the past decade. This cluster comprises 19 institutions, including, but not limited to, Massachusetts General Hospital and the University of Michigan. The purple cluster led by the University of Toronto and the green cluster led by Harvard Medical School also demonstrated exceptional productivity.
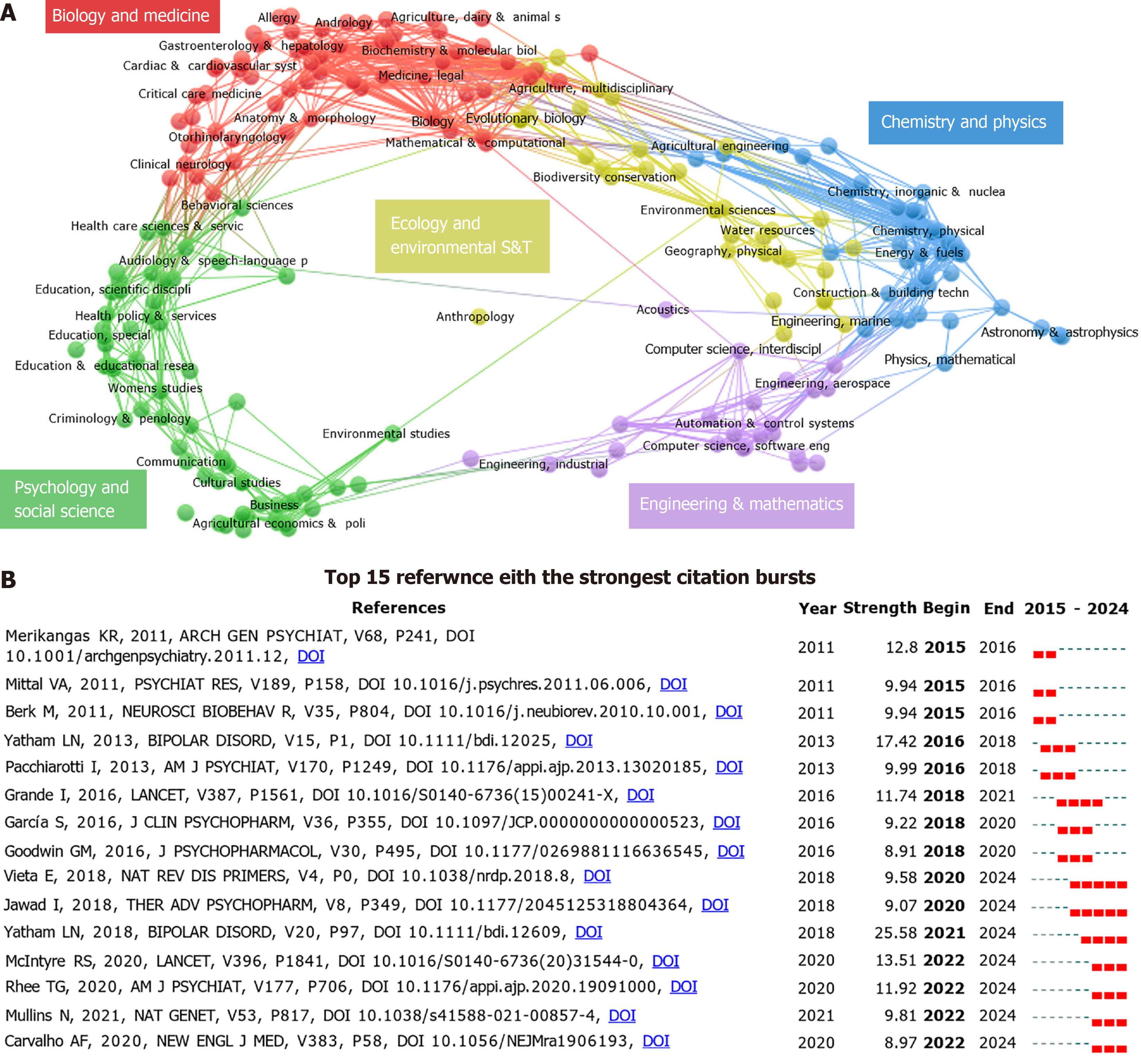
Table 1 lists the top ten journals in the field over the past decade based on publication volume, total citation frequency, and co-citation frequency. The publication volume indicates the productivity of a journal, the total citation frequency reflects the quality and level of attention a journal receives, and the co-citation frequency shows the relevance of journal content within the field[28]. The top three journals by publication volume are the Journal of Affective Disorders (documents = 270), Bipolar Disorders (documents = 79), and Frontiers in Psychiatry (documents = 77). The first two journals are also among the top three for total citation frequency and co-citation frequency. Over the past decade, five main research directions, represented by red, blue, green, purple, and yellow clusters, have emerged in the fields of BD and pharmacotherapy. The labels indicate the main content of these research directions. Nodes of the same color belong to sub-disciplines or research directions within that field (Figure 3A). The red cluster represents “biology and medicine”, blue represents “chemistry and physics”, green represents “psychology and social science”, purple represents “engineering & mathematics”, and yellow represents “ecology and environmental S&T”. “Biology and medicine” and “psychology and social science” are the primary research directions in this field.
| Documents, journal | Documents, counts | Total citations, journal | Total citations, counts | Co-citations, journal | Co-citations, counts | |
| 1 | Journal of Affective Disorders | 270 | Journal of Affective Disorders | 4267 | Journal of Affective Disorders | 5901 |
| 2 | Bipolar Disorders | 79 | Bipolar Disorders | 2380 | American Journal of Psychiatry | 4453 |
| 3 | Frontiers in Psychiatry | 77 | JAMA Psychiatry | 1549 | Bipolar Disorders | 4348 |
| 4 | Psychiatry Research | 67 | Journal of Clinical Psychiatry | 974 | Journal of Clinical Psychiatry | 3753 |
| 5 | BMC Psychiatry | 64 | BMC Psychiatry | 855 | Archives of General Psychiatry | 2987 |
| 6 | Journal of Clinical Psychiatry | 47 | Scizophrenia Research | 803 | Biological Psychiatry | 2735 |
| 7 | Journal of Psychiatry Research | 45 | Psychological Medicine | 789 | British Journal of Psychology | 2527 |
| 8 | Scizophrenia Research | 41 | European Neuropsychopharmacology | 741 | Schizophrenia Bulletin | 2406 |
| 9 | Psychological Medicine | 38 | Psychiatric Services | 728 | Molecular Psychiatry | 1841 |
| 10 | ACTA Psychiatrica Scandinavica | 38 | Psychiatry Research | 679 | Psychiatry Research | 1728 |
Deep interpretation and analysis of citations and literature can help scholars identify the most prominent research directions and future hotspots and trends in the field. Supplementary Table 1 lists the top ten most cited papers in the field over the past decade. The most frequently cited paper is the 2018 guidelines on the management of BD patients by Yatham et al[29] published in Bipolar Disorders, with a total of 933 citations. This is followed by a systematic review and meta-analysis of the field by Vancampfort et al[30] published in World Psychiatry in 2015, with a total of 790 citations. Classic papers tend to have sustained citation data, while flash-in-the-pan articles are cited frequently but only for a limited time. Therefore, understanding the flash-in-the-pan articles at different periods can enhance our understanding and knowledge of the frontiers and hotspots in a particular field[31]. We used CiteSpace to create a burst detection map of citations and identified the 15 most significant burst articles in the field (Figure 3B). The first burst article appeared in 2011, authored by Merikangas et al[32]. Most of the citation bursts occurred in 2018 and later, with the strongest citation burst associated with the guidelines by Yatham et al[29]. Currently, seven papers are still in a burst phase. These seven can be defined as the current flash-in-the-pan articles in the field.
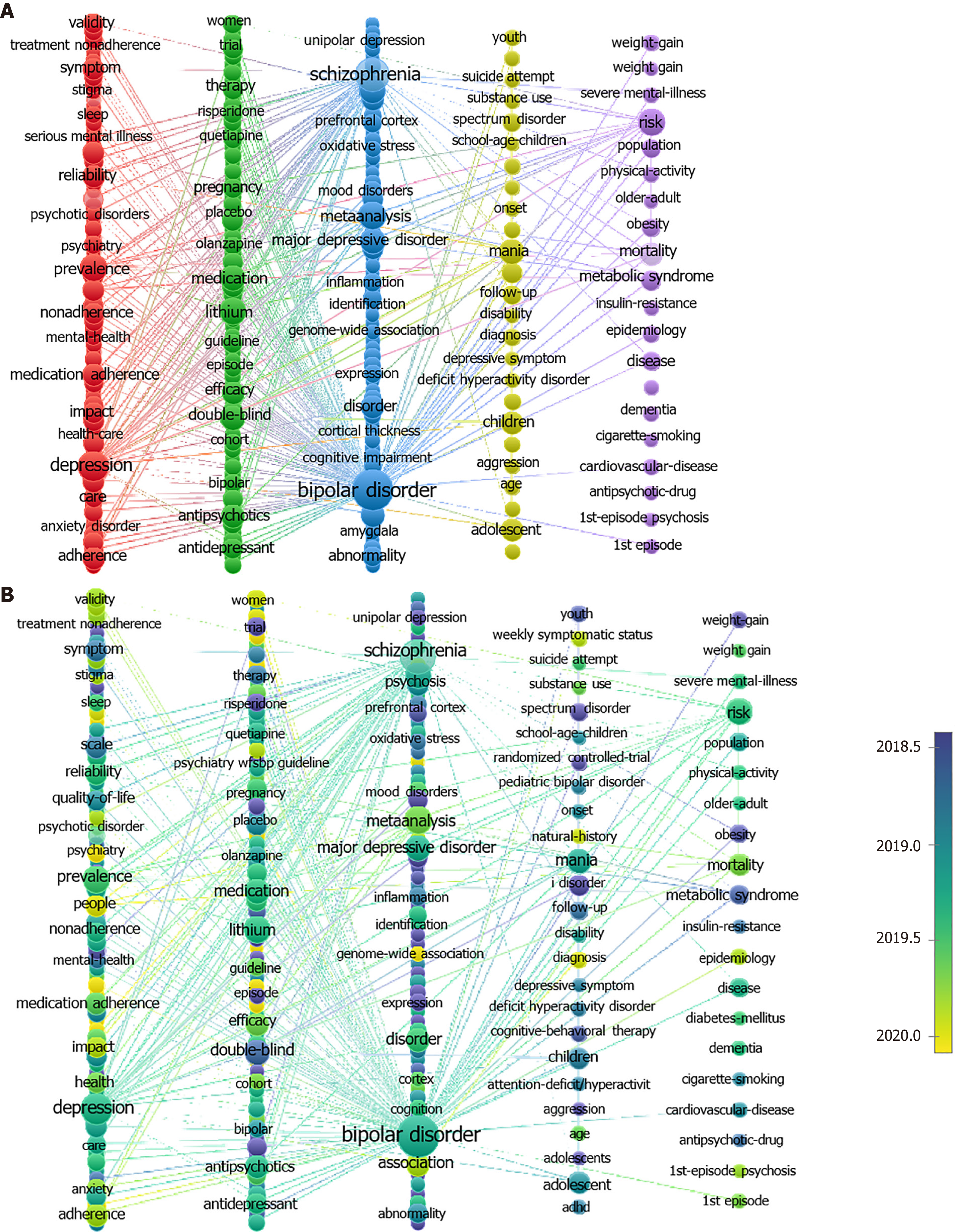
Keywords reflect hotspots within a field and their interconnections[33]. This study used VOSviewer to identify 250 keywords from 2624 documents, each with an occurrence strength of at least 20, and plotted a keyword network clustering diagram (Figure 4A). The 250 keywords were divided into five clusters, with the size of the circles representing the frequency of keyword occurrences. Keywords belonging to the same research direction were marked with the same color. The red cluster represents “clinical symptoms and health research”, with high-frequency keywords, such as “depression”, “comorbidity”, and “medication adherence”. The green cluster represents “pharmacotherapy and efficacy research”, with high-frequency keywords, such as “lithium”, “medication”, and “antipsychotics”. The blue cluster represents “gene expression and mechanism research”, with representative keywords like “abnormality”, “expression”, and “inflammation”. The yellow cluster represents “age factors and differences research”, with high-frequency keywords, such as “adolescent”, “children”, and “age”. The purple cluster represents “risk factors and epidemiology research”, with representative keywords like “risk”, “mortality”, and “metabolic syndrome”.
By overlaying time on the keyword clustering diagram, one can gain insights into changes in research directions within a field, helping scholars explore cutting-edge technology and future trends in that domain. As shown in Figure 4B, colors can reveal the average years of occurrence for different keywords, with earlier keywords appearing in blue, such as “unipolar depression”, “metabolic syndrome”, and “risperidone” and later keywords appearing in yellow, such as “psychiatry”, “genome-wide association”, and “1st-episode psychosis”. The frequent appearance of keywords in a specific period is known as a citation burst, often indicating research inclinations and concentrated trends in a specific period within a field. Figure 5 lists the top 25 keywords with the strongest citation bursts lasting at least one year. “Primary care” is the keyword with the highest sustained attention. Keywords like “primary care”, “trend”, “weekly symptomatic status”, and “service” are currently experiencing citation bursts.
The significant productivity of North America, East Asia, and Western Europe highlights their extensive involvement in this research field. Australia has also made a substantial impact in this area. To emphasize the collaborative nature of international research in this field, we grouped the countries into eight major clusters. The United States-led green cluster is the most important one, highlighting the dominance of the United States in this research field because of its highly extensive scientific resources and research infrastructure and its significant contribution in both the quantity and quality of publications on BD pharmacotherapy. There is a positive correlation between the intensity of international collaboration and citation frequency (Figure 2B). The United States is a global leader in both collaboration intensity and total citations, followed by the United Kingdom, Germany, and Canada. Hence, it can be suggested that a highly collaborative research environment often yields more impactful studies. This insight is crucial for understanding the dynamics of global research collaboration and its impact on scientific progress. It further indicates that transnational collaboration among countries not only facilitates the sharing of resources and the leveraging of complementary strengths, but also significantly expedites the creation and spread of new knowledge, thereby injecting a potent impetus into the innovation of BD treatments.
Authors and institutions play key roles in advancing research. Figure 2C shows more than ten collaboration clusters comprising 133 authors with over five publications each, with the dark blue cluster led by McInnis MG and Nierenberg AA being the most significant. These clusters highlight the key researchers driving development in this field. Similarly, an analysis of institutions showed that the yellow cluster led by the University of Pittsburgh, with Massachusetts General Hospital and the University of Michigan as the other participants, is the dominant institutional cluster (Figure 2D). This result underscores the importance of institutional collaboration in promoting research productivity and impact. Inter-institutional collaboration empowers researchers from diverse fields to collaborate closely in exploring BD treatment. By integrating multidisciplinary perspectives, it stimulates the creation of innovative treatment methods and strategies. This collaborative approach not only boosts research efficiency but also markedly enhances the quality and influence of the research outcomes.
The analysis of journals and research areas provides additional insights into the structure of the field. Table 1 lists the top journals ranked by publication volume, total citations, and co-citations. The Journal of Affective Disorders leads all these categories, underscoring its critical role in disseminating high-quality and impactful research on the pharmacotherapy of BD. Figure 3A displays five major research directions, with “biology and medicine” and “psychology and social science” being the most important ones, indicating the multidisciplinary nature of the field. This diversity suggests that extensive interdisciplinary connections and exchanges are necessary to understand and treat BD. Therefore, future research should focus on interdisciplinary collaboration, integrating insights from psychology, neuroscience, genetics, and psychiatry. This approach will drive innovation and expedite the application of research findings in clinical practice.
Citation and literature analyses further refine our understanding of key contributions and emerging trends in the field. Supplementary Table 1 lists the most cited papers of the past decade. The 2018 paper by Yatham et al[29] on management guidelines for patients with BD was identified as the most cited one. Systematic reviews and meta-analyses are also widely used in this field, as illustrated by the 2015 paper of Vancampfort et al[30], highlighting the reliance of this field on comprehensive evidence. The identification of citation bursts, especially the most notable burst related to Yatham et al’s guidelines[29], indicates shifts in the research focus and the emergence of new frontiers in BD research. These seven papers still experiencing citation bursts indicate current hot topics and areas of intense research activity. In 2018, Vieta et al[34] conducted a comprehensive discussion on BD, delving into its clinical symptoms and assessment methods and exploring both pharmacological and psychosocial treatment approaches. In the same year, Jawad et al[35] investigated the non-adherence to BD treatment medications, analyzed its causes and impacts on patients, and emphasized the necessity and methods for improving medication adherence. In 2018, the Canadian Network for Mood and Anxiety Treatments and the International Society for Bipolar Disorder collaborated to release an updated version of the guidelines for managing patients of BD, incorporating the latest advancements in treatment[29]. In 2020, McIntyre et al[36] combined epidemiological data to detail the connections and differences between BD-I and BD-II by thoroughly studying the pathogenesis and treatment strategies of BD, thereby providing a basis for clinical diagnosis. Carvalho et al[37] elucidated the genetic and neurobiological characteristics of BD. Rhee et al[38] reviewed the trends in BD pharmacotherapy from 1997 to 2016 and compared the efficacy of second-generation antipsychotics, lithium, and mood stabilizers, laying the groundwork for future drug research. In 2021, Mullins et al[39] conducted a genome-wide association study on over 40000 patients of BD and identified 64 BD-related genetic loci, deepening the understanding of the biological etiology of BD and providing new perspectives for future treatments.
We divided 250 keywords into five clusters (Figure 4A). The red cluster (clinical symptoms and health research) reveals that the prevalence of metabolic syndrome, obesity, smoking, and type 2 diabetes is higher among patients with BD, potentially leading to their premature death[40]. Research on the clinical treatment of BD is still mainly focused on pharmacotherapy. A national study on the consistency of multimodal treatment guidelines for BD indicated that, compared to pharmacotherapy, psychosocial therapy has seen only a limited implementation in daily clinical practice for BD. Hence, more effort is needed to implement non-pharmacological guideline recommendations for BD[41]. The Taiwanese Society of Biological Psychiatry and Neuropsychopharmacology provided the latest interpretations of the consensus on biological treatment for acute, maintenance, and mixed phases of BD in 2023, discussed various treatment plans for BD, evaluated the related efficacy, and summarized extensive research evidence and clinical experience to recommend grades for various clinical treatment plans of BD[42]. The International Society for International Society for Bipolar Disorder conducted an anonymous survey in 2023 on the preferences and attitudes of clinicians toward using lithium for the global maintenance treatment of BD. The survey revealed that these preferences and attitudes may be influenced by patients’ beliefs and clinical environments[43]. The formulation of various clinical guidelines and the conduct of different surveys continue to drive the development of clinical treatment modalities for BD, providing more comprehensive and advanced evidence and concepts for both clinicians and patients. We believe that more extensive clinical guidelines and clinical surveys will be carried out in the future.
The green cluster (drug therapy and efficacy research) indicates that pharmacotherapy is currently the optimal solution for patients with BD. Therefore, it has received significant attention from scholars and clinicians. Researchers in this field tend to extensively study pharmacotherapy[41]. A meta-analysis aimed at understanding BD treatment practices indicated that anticonvulsants, second-generation antipsychotics, and antidepressants are the most prescribed drugs for mood stabilization. However, because of data gaps, it is not possible to conduct cross-regional and cross-ethnic studies[44]. In the past decade, lithium and valproate remained the pharmacological foundations for BD treatment. However, the patterns of BD pharmacotherapy are continuously evolving. To evaluate the advantages and disadvantages of this evolution, Lähteenvuo et al[45] conducted a detailed cohort study on the actual effectiveness of antipsychotics and mood stabilizers in BD. They not only explored the relative efficacy and safety of antipsychotics and mood stabilizers, but also specifically studied first-episode patients, further revealing the high safety and stability of lithium treatment. According to current scientific knowledge in this field, the first-line treatment drugs for BD mainly include mood stabilizers (such as lithium), anticonvulsants (such as valproate and lamotrigine), and atypical antipsychotics (such as quetiapine, aripiprazole, asenapine, lurasidone, and cariprazine)[40]. Some novel drugs or therapies have also been reported, such as levothyroxine and neurosteroids[46,47]. However, the adverse reactions and severe side effects of these drugs still need further resolution[48].
The blue cluster (gene expression and mechanism research) shows the significant progress made in the study of gene expression and mechanisms in the pharmacotherapy of BD in recent years. Lithium, the most classic treatment drug for BD, has been shown to regulate the survival and function of nerve cells by affecting the glycogen synthase kinase 3β pathway[49]. Additionally, gene expression studies on BD revealed the specific mechanisms through which drugs act at the neuronal level. For example, antipsychotics can influence the plasticity and survival of nerve cells by regulating the synthesis and release of neurotransmitters. They can also regulate the expression of genes related to neuroinflammation, thus exerting anti-inflammatory effects[50]. Additionally, future studies should delve deeper into the relationship between gene expression and drug response, aiming to develop personalized treatment plans tailored to individual patients’ genetic profiles and specific conditions. This will optimize clinical outcomes and improve patient satisfaction with treatment.
The yellow cluster (age factors and differentiation studies) confirms that BD patients of different age groups respond differently to drugs. Young patients (under 18 years of age) show different drug efficacy and side effects from those of adult patients when using antidepressants. Research in this direction often relates to hormones and inflammation markers, as biological age and sex significantly affect gonadal hormones, stress hormones, and inflammation markers[51]. For young patients, especially those experiencing their first episode, a combination of mood stabilizers and antipsychotics is usually adopted. For older patients, monotherapy, such as lithium or lamotrigine alone, is often recommended to reduce the risk of drug interactions and side effects[52,53]. Given the differences in drug efficacy and side effects among BD patients of various age groups, future research should focus on conducting age-specific studies. This will allow for the development of tailored drug therapies and treatment models that cater to the unique needs of patients across different age brackets, ultimately enhancing clinical outcomes.
The purple cluster (risk factors and epidemiology research) shows that the risk factors for BD mainly include genetic, biological, and psychosocial factors. Among these, genetics is the most significant risk factor, with surveys indicating that BD has a high familial aggregation[5]. Biological factors are mainly associated with neurotransmitter dysfunctions (such as serotonin, norepinephrine, and dopamine) and structural changes in the brain. Additionally, life stress, stressful events, and negative life experiences can trigger or exacerbate the condition[54]. Epidemiological studies have indicated that the global lifetime prevalence of BD is approximately 2.4%, with the onset typically occurring around the age of 25 years. BD has a high relapse rate (up to 90%), especially if not properly treated after an acute episode[32,55]. Hence, we call for future epidemiological researchers in this field to focus more on interdisciplinary cooperation, including efforts from psychiatry, psychology, neuroscience, and genetics, to comprehensively understand and treat BD.
Earlier appearing keywords include “unipolar depression”, “metabolic syndrome”, and “risperidone”, while later appearing keywords include “psychiatry”, “genome-wide association”, and “1st-episode psychosis” (Figure 4B). Hence, it can be suggested that past research tended to focus on comparing BD with unipolar depression, metabolic issues in BD patients (such as obesity and diabetes), and the application of early drugs such as risperidone[56-58]. In contrast, recent research focuses include the overall development of the impact of psychiatry on BD treatment, the identification of genes associated with BD through genome-wide association study, and first-episode psychosis patients[59-61].
Keywords such as “primary care”, “trend”, “weekly symptomatic status”, and “service” are currently experiencing a surge (Figure 5), indicating that the field is undergoing significant developments and changes. The frequent appearance of the keyword “primary care” reflects that BD treatment is increasingly being integrated into primary healthcare systems. Moreover, the integration of BD treatment into primary care systems should be a priority for future research and clinical practice. Studies should explore effective strategies for diagnosing and managing BD in primary care settings, enabling earlier identification and treatment of patients, thereby reducing the disease burden and healthcare costs[62]. The surge of “trend” and “weekly symptomatic status” suggests that researchers are closely monitoring the epidemiological trends and treatment effects of BD. Future research should focus on large-scale, long-term epidemiological studies for an improved understanding of the incidence, treatment patterns, and long-term prognosis of BD. This also highlights the importance of real-time monitoring of BD symptoms and treatment effects. In the future, researchers in this field should develop and apply digital health tools to track the symptom changes and drug responses of patients in real time. The data so collected may help in devising better treatment plans and improved treatment outcomes[45,63]. Additionally, the surge of the keyword “service” indicates that more attention is being paid to the research of integrated care models, which involves the merging of mental health services with other medical services to provide comprehensive care to patients with BD[64,65].
BD-I typically involves manic episodes, whereas BD-II involves at least one major depressive episode along with hypomania[66]. Both BD-I and BD-II have chronic courses, although the former often manifests more severely and usually requires hospitalization[67]. BD-II also presents with more severe characteristics, such as more frequent mixed episodes and more severe complications[68]. In addition, numerous studies have confirmed that, compared to BD-I, BD-II carries a higher risk of suicide, which may be related to the longer depressive cycles and mixed states in BD-II[69,70]. Therefore, there are significant differences in the pharmacological treatment of BD-I and BD-II.
For BD-I patients, the primary focus is often on treating mania, whereas for BD-II patients, antidepressant treatment is predominant[71,72]. For BD-I, lithium is the most common mood stabilizer. For BD-II depression, lamotrigine is the most common mood stabilizer, as it can also prevent depressive episodes[73]. Terao et al[67] showed that lamotrigine is more effective in stabilizing mood and preventing relapse than in alleviating mania in BD-I. It is also more effective for the long-term treatment of BD-II[67,74]. Hence, it can be suggested that lamotrigine is more suitable for the treatment of BD-II than it is for BD-I.
There are also differences in the combination of drugs used to treat BD-I and BD-II. In BD-I treatment, the combination of mood stabilizers and antipsychotics is most common, such as the use of olanzapine and lithium combined with valproate, while in BD-II, the combination of mood stabilizers and antidepressants is most common, such as the combined use of lamotrigine and quetiapine[10,75-77]. In contrast to BD-I, research on the efficacy of pharmacological treatment for BD-II is scarce. Since BD-II has a higher frequency of onset than BD-I, many drugs used for BD-I cannot be used alone for BD-II. In addition, the guidelines provide limited recommendations specifically for BD-II[29]. Swartz and Thase[78] and Datto et al[79] have evaluated the pharmacological treatment of BD-II and shown that quetiapine can effectively improve depressive and anxiety symptoms in BD-II, although the response is slower compared to that for BD-I. In addition, pramipexole and lithium show promise as second-line drugs for treating BD-II depression[80]. Hence, it is clear that current research on the pharmacological treatment of BD-II is highly limited and lacks effective clinical evidence to verify the efficacy and safety of related drugs.
Due to differences in data formats, we only included studies from the Web of Science. Therefore, not all studies may be included. In addition, this research is limited to a single region, and therefore has only been conducted using English literature. It is possible that incorporating non-English literature or research from other regions could yield different results. Aside from this, bibliometric analysis, the quantity of key annotated bibliographies, citation normalization, and the qualitative assessment of bibliographic content, innovation, and impact are crucial but have not been the focus of further investigation. Despite its importance, this remains an area for future research.
This study utilized bibliometric methods to analyze the global research trends and current status of drug treatment for BD over the past decade, providing valuable insights for future research in BD pharmacotherapy. The United States, China, and the United Kingdom have made the most significant contributions to research in this field and have established important collaborative research networks. The University of Pittsburgh, Massachusetts General Hospital, and the University of Michigan have been identified as the leading research institutions in this area. International and inter-institutional collaboration is vital for innovating BD treatments. Going forward, we must enhance such cooperation to tackle BD treatment challenges together and provide patients with safer, more effective therapies. The Journal of Affective Disorders is recognized as the most influential journal in this field. Keyword analysis revealed research hotspots related to clinical symptoms, drug efficacy, and genetic mechanisms. Overall, this study offers a new perspective on addressing the multifaceted challenges associated with this complex disorder.
| 1. | Harrison PJ, Geddes JR, Tunbridge EM. The Emerging Neurobiology of Bipolar Disorder. Focus (Am Psychiatr Publ). 2019;17:284-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Lee CY, Zeng JH, Lee SY, Lu RB, Kuo PH. SNP Data Science for Classification of Bipolar Disorder I and Bipolar Disorder II. IEEE/ACM Trans Comput Biol Bioinform. 2021;18:2862-2869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Smith DJ, Whitham EA, Ghaemi SN. Bipolar disorder. Handb Clin Neurol. 2012;106:251-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Rowland TA, Marwaha S. Epidemiology and risk factors for bipolar disorder. Ther Adv Psychopharmacol. 2018;8:251-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 237] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 5. | O'Connell KS, Coombes BJ. Genetic contributions to bipolar disorder: current status and future directions. Psychol Med. 2021;51:2156-2167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 6. | Scaini G, Valvassori SS, Diaz AP, Lima CN, Benevenuto D, Fries GR, Quevedo J. Neurobiology of bipolar disorders: a review of genetic components, signaling pathways, biochemical changes, and neuroimaging findings. Braz J Psychiatry. 2020;42:536-551. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 7. | Palmier-Claus JE, Berry K, Bucci S, Mansell W, Varese F. Relationship between childhood adversity and bipolar affective disorder: systematic review and meta-analysis. Br J Psychiatry. 2016;209:454-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 145] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 8. | Marwaha S, Winsper C, Bebbington P, Smith D. Cannabis Use and Hypomania in Young People: A Prospective Analysis. Schizophr Bull. 2018;44:1267-1274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 9. | Janiri D, Moccia L, Montanari S, Simonetti A, Conte E, Chieffo D, Monti L, Kotzalidis GD, Janiri L, Sani G. Primary emotional systems, childhood trauma, and suicidal ideation in youths with bipolar disorders. Child Abuse Negl. 2023;146:106521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Harrison PJ, Cipriani A, Harmer CJ, Nobre AC, Saunders K, Goodwin GM, Geddes JR. Innovative approaches to bipolar disorder and its treatment. Ann N Y Acad Sci. 2016;1366:76-89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 11. | Marzani G, Price Neff A. Bipolar Disorders: Evaluation and Treatment. Am Fam Physician. 2021;103:227-239. [PubMed] |
| 12. | Sheikh M, Qassem M, Triantis IF, Kyriacou PA. Advances in Therapeutic Monitoring of Lithium in the Management of Bipolar Disorder. Sensors (Basel). 2022;22:736. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 13. | Penninx BWJH, Lange SMM. Metabolic syndrome in psychiatric patients: overview, mechanisms, and implications. Dialogues Clin Neurosci. 2018;20:63-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 347] [Article Influence: 49.6] [Reference Citation Analysis (0)] |
| 14. | Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. 2018;20:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1964] [Cited by in RCA: 2413] [Article Influence: 344.7] [Reference Citation Analysis (0)] |
| 15. | Ellegaard O, Wallin JA. The bibliometric analysis of scholarly production: How great is the impact? Scientometrics. 2015;105:1809-1831. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1309] [Cited by in RCA: 772] [Article Influence: 77.2] [Reference Citation Analysis (0)] |
| 16. | Hicks D, Wouters P, Waltman L, de Rijcke S, Rafols I. Bibliometrics: The Leiden Manifesto for research metrics. Nature. 2015;520:429-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1012] [Cited by in RCA: 822] [Article Influence: 82.2] [Reference Citation Analysis (0)] |
| 17. | Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci U S A. 2004;101 Suppl 1:5303-5310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1484] [Cited by in RCA: 1310] [Article Influence: 62.4] [Reference Citation Analysis (0)] |
| 18. | Chen C. CiteSpace II: Detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci. 2006;57:359-377. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2009] [Cited by in RCA: 2057] [Article Influence: 108.3] [Reference Citation Analysis (0)] |
| 19. | Chen R, Wang Z, Zhang L. Research trends on alphavirus receptors: a bibliometric analysis. Front Cell Infect Microbiol. 2024;14:1388360. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4505] [Cited by in RCA: 5141] [Article Influence: 321.3] [Reference Citation Analysis (0)] |
| 21. | van Eck NJ, Waltman L. Text mining and visualization using VOSviewer. 2011 Preprint. Available from: arXiv:1109.2058. [DOI] [Full Text] |
| 22. | Dohleman BS. Exploratory social network analysis with Pajek. Psychometrika. 2006;71:605-606. [DOI] [Full Text] |
| 23. | Newman ME. Fast algorithm for detecting community structure in networks. Phys Rev E Stat Nonlin Soft Matter Phys. 2004;69:066133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3224] [Cited by in RCA: 1081] [Article Influence: 51.5] [Reference Citation Analysis (0)] |
| 24. | Noack A. Modularity clustering is force-directed layout. Phys Rev E Stat Nonlin Soft Matter Phys. 2009;79:026102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 25. | Waltman L, van Eck NJ, Noyons EC. A unified approach to mapping and clustering of bibliometric networks. J Informetr. 2010;4:629-635. [RCA] [DOI] [Full Text] [Cited by in Crossref: 781] [Cited by in RCA: 518] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 26. | Hassan-montero Y, De-moya-anegón F, Guerrero-bote VP. SCImago Graphica: a new tool for exploring and visually communicating data. EI Profesional de la Información. 2022;31:e310502. [DOI] [Full Text] |
| 27. | Aria M, Cuccurullo C. bibliometrix: An R-tool for comprehensive science mapping analysis. J Informetr. 2017;11:959-975. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1736] [Cited by in RCA: 2270] [Article Influence: 283.8] [Reference Citation Analysis (0)] |
| 28. | Yang LJ, Han LX, Liu NX. A new approach to journal co-citation matrix construction based on the number of co-cited articles in journals. Scientometrics. 2019;120:507-517. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 29. | Yatham LN, Kennedy SH, Parikh SV, Schaffer A, Bond DJ, Frey BN, Sharma V, Goldstein BI, Rej S, Beaulieu S, Alda M, MacQueen G, Milev RV, Ravindran A, O'Donovan C, McIntosh D, Lam RW, Vazquez G, Kapczinski F, McIntyre RS, Kozicky J, Kanba S, Lafer B, Suppes T, Calabrese JR, Vieta E, Malhi G, Post RM, Berk M. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20:97-170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1142] [Cited by in RCA: 1122] [Article Influence: 160.3] [Reference Citation Analysis (0)] |
| 30. | Vancampfort D, Stubbs B, Mitchell AJ, De Hert M, Wampers M, Ward PB, Rosenbaum S, Correll CU. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry. 2015;14:339-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 707] [Cited by in RCA: 843] [Article Influence: 84.3] [Reference Citation Analysis (0)] |
| 31. | PRICE DJ. NETWORKS OF SCIENTIFIC PAPERS. Science. 1965;149:510-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1774] [Cited by in RCA: 907] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 32. | Merikangas KR, Jin R, He JP, Kessler RC, Lee S, Sampson NA, Viana MC, Andrade LH, Hu C, Karam EG, Ladea M, Medina-Mora ME, Ono Y, Posada-Villa J, Sagar R, Wells JE, Zarkov Z. Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Arch Gen Psychiatry. 2011;68:241-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1693] [Cited by in RCA: 1754] [Article Influence: 125.3] [Reference Citation Analysis (0)] |
| 33. | Zhong D, Li Y, Huang Y, Hong X, Li J, Jin R. Molecular Mechanisms of Exercise on Cancer: A Bibliometrics Study and Visualization Analysis via CiteSpace. Front Mol Biosci. 2021;8:797902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 79] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 34. | Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, Gao K, Miskowiak KW, Grande I. Bipolar disorders. Nat Rev Dis Primers. 2018;4:18008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 353] [Cited by in RCA: 530] [Article Influence: 75.7] [Reference Citation Analysis (0)] |
| 35. | Jawad I, Watson S, Haddad PM, Talbot PS, McAllister-Williams RH. Medication nonadherence in bipolar disorder: a narrative review. Ther Adv Psychopharmacol. 2018;8:349-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 106] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 36. | McIntyre RS, Berk M, Brietzke E, Goldstein BI, López-Jaramillo C, Kessing LV, Malhi GS, Nierenberg AA, Rosenblat JD, Majeed A, Vieta E, Vinberg M, Young AH, Mansur RB. Bipolar disorders. Lancet. 2020;396:1841-1856. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 568] [Article Influence: 113.6] [Reference Citation Analysis (0)] |
| 37. | Carvalho AF, Firth J, Vieta E. Bipolar Disorder. N Engl J Med. 2020;383:58-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 195] [Cited by in RCA: 334] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 38. | Rhee TG, Olfson M, Nierenberg AA, Wilkinson ST. 20-Year Trends in the Pharmacologic Treatment of Bipolar Disorder by Psychiatrists in Outpatient Care Settings. Am J Psychiatry. 2020;177:706-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 166] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 39. | Mullins N, Forstner AJ, O'Connell KS, Coombes B, Coleman JRI, Qiao Z, Als TD, Bigdeli TB, Børte S, Bryois J, Charney AW, Drange OK, Gandal MJ, Hagenaars SP, Ikeda M, Kamitaki N, Kim M, Krebs K, Panagiotaropoulou G, Schilder BM, Sloofman LG, Steinberg S, Trubetskoy V, Winsvold BS, Won HH, Abramova L, Adorjan K, Agerbo E, Al Eissa M, Albani D, Alliey-Rodriguez N, Anjorin A, Antilla V, Antoniou A, Awasthi S, Baek JH, Bækvad-Hansen M, Bass N, Bauer M, Beins EC, Bergen SE, Birner A, Bøcker Pedersen C, Bøen E, Boks MP, Bosch R, Brum M, Brumpton BM, Brunkhorst-Kanaan N, Budde M, Bybjerg-Grauholm J, Byerley W, Cairns M, Casas M, Cervantes P, Clarke TK, Cruceanu C, Cuellar-Barboza A, Cunningham J, Curtis D, Czerski PM, Dale AM, Dalkner N, David FS, Degenhardt F, Djurovic S, Dobbyn AL, Douzenis A, Elvsåshagen T, Escott-Price V, Ferrier IN, Fiorentino A, Foroud TM, Forty L, Frank J, Frei O, Freimer NB, Frisén L, Gade K, Garnham J, Gelernter J, Giørtz Pedersen M, Gizer IR, Gordon SD, Gordon-Smith K, Greenwood TA, Grove J, Guzman-Parra J, Ha K, Haraldsson M, Hautzinger M, Heilbronner U, Hellgren D, Herms S, Hoffmann P, Holmans PA, Huckins L, Jamain S, Johnson JS, Kalman JL, Kamatani Y, Kennedy JL, Kittel-Schneider S, Knowles JA, Kogevinas M, Koromina M, Kranz TM, Kranzler HR, Kubo M, Kupka R, Kushner SA, Lavebratt C, Lawrence J, Leber M, Lee HJ, Lee PH, Levy SE, Lewis C, Liao C, Lucae S, Lundberg M, MacIntyre DJ, Magnusson SH, Maier W, Maihofer A, Malaspina D, Maratou E, Martinsson L, Mattheisen M, McCarroll SA, McGregor NW, McGuffin P, McKay JD, Medeiros H, Medland SE, Millischer V, Montgomery GW, Moran JL, Morris DW, Mühleisen TW, O'Brien N, O'Donovan C, Olde Loohuis LM, Oruc L, Papiol S, Pardiñas AF, Perry A, Pfennig A, Porichi E, Potash JB, Quested D, Raj T, Rapaport MH, DePaulo JR, Regeer EJ, Rice JP, Rivas F, Rivera M, Roth J, Roussos P, Ruderfer DM, Sánchez-Mora C, Schulte EC, Senner F, Sharp S, Shilling PD, Sigurdsson E, Sirignano L, Slaney C, Smeland OB, Smith DJ, Sobell JL, Søholm Hansen C, Soler Artigas M, Spijker AT, Stein DJ, Strauss JS, Świątkowska B, Terao C, Thorgeirsson TE, Toma C, Tooney P, Tsermpini EE, Vawter MP, Vedder H, Walters JTR, Witt SH, Xi S, Xu W, Yang JMK, Young AH, Young H, Zandi PP, Zhou H, Zillich L; HUNT All-In Psychiatry, Adolfsson R, Agartz I, Alda M, Alfredsson L, Babadjanova G, Backlund L, Baune BT, Bellivier F, Bengesser S, Berrettini WH, Blackwood DHR, Boehnke M, Børglum AD, Breen G, Carr VJ, Catts S, Corvin A, Craddock N, Dannlowski U, Dikeos D, Esko T, Etain B, Ferentinos P, Frye M, Fullerton JM, Gawlik M, Gershon ES, Goes FS, Green MJ, Grigoroiu-Serbanescu M, Hauser J, Henskens F, Hillert J, Hong KS, Hougaard DM, Hultman CM, Hveem K, Iwata N, Jablensky AV, Jones I, Jones LA, Kahn RS, Kelsoe JR, Kirov G, Landén M, Leboyer M, Lewis CM, Li QS, Lissowska J, Lochner C, Loughland C, Martin NG, Mathews CA, Mayoral F, McElroy SL, McIntosh AM, McMahon FJ, Melle I, Michie P, Milani L, Mitchell PB, Morken G, Mors O, Mortensen PB, Mowry B, Müller-Myhsok B, Myers RM, Neale BM, Nievergelt CM, Nordentoft M, Nöthen MM, O'Donovan MC, Oedegaard KJ, Olsson T, Owen MJ, Paciga SA, Pantelis C, Pato C, Pato MT, Patrinos GP, Perlis RH, Posthuma D, Ramos-Quiroga JA, Reif A, Reininghaus EZ, Ribasés M, Rietschel M, Ripke S, Rouleau GA, Saito T, Schall U, Schalling M, Schofield PR, Schulze TG, Scott LJ, Scott RJ, Serretti A, Shannon Weickert C, Smoller JW, Stefansson H, Stefansson K, Stordal E, Streit F, Sullivan PF, Turecki G, Vaaler AE, Vieta E, Vincent JB, Waldman ID, Weickert TW, Werge T, Wray NR, Zwart JA, Biernacka JM, Nurnberger JI, Cichon S, Edenberg HJ, Stahl EA, McQuillin A, Di Florio A, Ophoff RA, Andreassen OA. Genome-wide association study of more than 40,000 bipolar disorder cases provides new insights into the underlying biology. Nat Genet. 2021;53:817-829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 609] [Cited by in RCA: 867] [Article Influence: 216.8] [Reference Citation Analysis (0)] |
| 40. | Nierenberg AA, Agustini B, Köhler-Forsberg O, Cusin C, Katz D, Sylvia LG, Peters A, Berk M. Diagnosis and Treatment of Bipolar Disorder: A Review. JAMA. 2023;330:1370-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 134] [Reference Citation Analysis (0)] |
| 41. | Renes JW, Regeer EJ, Hoogendoorn AW, Nolen WA, Kupka RW. A nationwide study on concordance with multimodal treatment guidelines in bipolar disorder. Int J Bipolar Disord. 2018;6:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 42. | Cheng CM, Chang WH, Lin YT, Chen PS, Yang YK, Bai YM; TSBPN Bipolar Taskforce. Taiwan consensus on biological treatment of bipolar disorder during the acute, maintenance, and mixed phases: The 2022 update. Asian J Psychiatr. 2023;82:103480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 43. | Hidalgo-Mazzei D, Mantingh T, Pérez de Mendiola X, Samalin L, Undurraga J, Strejilevich S, Severus E, Bauer M, González-Pinto A, Nolen WA, Young AH, Vieta E. Clinicians' preferences and attitudes towards the use of lithium in the maintenance treatment of bipolar disorders around the world: a survey from the ISBD Lithium task force. Int J Bipolar Disord. 2023;11:20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 44. | Singh B, Yocum AK, Strawbridge R, Burdick KE, Millett CE, Peters AT, Sperry SH, Fico G, Vieta E, Verdolini N, Godin O, Leboyer M, Etain B, Tso IF, Coombes BJ, McInnis MG, Nierenberg AA, Young AH, Ashton MM, Berk M, Williams LJ, Keramatian K, Yatham LN, Overs BJ, Fullerton JM, Roberts G, Mitchell PB, Andreassen OA, Andreazza AC, Zandi PP, Pham D, Biernacka JM, Frye MA; FACE-BD Collaborators, The Global Bipolar Cohort Collaborative. Patterns of pharmacotherapy for bipolar disorder: A GBC survey. Bipolar Disord. 2024;26:22-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 34] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 45. | Lähteenvuo M, Paljärvi T, Tanskanen A, Taipale H, Tiihonen J. Real-world effectiveness of pharmacological treatments for bipolar disorder: register-based national cohort study. Br J Psychiatry. 2023;223:456-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 46. | Zamar A, Lulsegged A, Kouimtsidis C. A new approach for the treatment of subthreshold bipolar disorders: Targeted high dose levothyroxine and repetitive transcranial magnetic stimulation for mitochondrial treatment. Front Psychiatry. 2022;13:976544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 47. | Serretti A. A Critical View on New and Future Antidepressants. Clin Psychopharmacol Neurosci. 2024;22:201-210. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 48. | Smith CM, Santalucia M, Bunn H, Muzyk A. Sublingual Dexmedetomidine for the Treatment of Agitation in Patients with Schizophrenia and Bipolar Disorder. Clin Psychopharmacol Neurosci. 2023;21:215-221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 49. | Won E, Kim YK. An Oldie but Goodie: Lithium in the Treatment of Bipolar Disorder through Neuroprotective and Neurotrophic Mechanisms. Int J Mol Sci. 2017;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 137] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 50. | Catts VS, Lai YL, Weickert CS, Weickert TW, Catts SV. A quantitative review of the postmortem evidence for decreased cortical N-methyl-D-aspartate receptor expression levels in schizophrenia: How can we link molecular abnormalities to mismatch negativity deficits? Biol Psychol. 2016;116:57-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 103] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 51. | Lyu N, Zhao Q, Fu B, Li J, Wang H, Yang F, Liu S, Huang J, Zhang X, Zhang L, Li R. Hormonal and inflammatory signatures of different mood episodes in bipolar disorder: a large-scale clinical study. BMC Psychiatry. 2023;23:449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 52. | Jing P, Su J, Zheng C, Mei X, Zhang X. A retrospective study of psychotropic drug treatments in bipolar disorder at acute and maintenance episodes. Front Psychiatry. 2023;14:1057780. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 53. | Arnold I, Dehning J, Grunze A, Hausmann A. Old Age Bipolar Disorder-Epidemiology, Aetiology and Treatment. Medicina (Kaunas). 2021;57:587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 54. | Zhong Y, Chen Y, Su X, Wang M, Li Q, Shao Z, Sun L. Global, regional and national burdens of bipolar disorders in adolescents and young adults: a trend analysis from 1990 to 2019. Gen Psychiatr. 2024;37:e101255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 55. | McLaren KD, Marangell LB. Special considerations in the treatment of patients with bipolar disorder and medical co-morbidities. Ann Gen Hosp Psychiatry. 2004;3:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 56. | Forty L, Smith D, Jones L, Jones I, Caesar S, Cooper C, Fraser C, Gordon-Smith K, Hyde S, Farmer A, McGuffin P, Craddock N. Clinical differences between bipolar and unipolar depression. Br J Psychiatry. 2008;192:388-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 57. | Volkow ND, O'Brien CP. Issues for DSM-V: should obesity be included as a brain disorder? Am J Psychiatry. 2007;164:708-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 120] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 58. | Swann AC. The strong relationship between bipolar and substance-use disorder. Ann N Y Acad Sci. 2010;1187:276-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 59. | Miziou S, Tsitsipa E, Moysidou S, Karavelas V, Dimelis D, Polyzoidou V, Fountoulakis KN. Psychosocial treatment and interventions for bipolar disorder: a systematic review. Ann Gen Psychiatry. 2015;14:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 60. | Chen R, Yang Z, Liu J, Cai X, Huo Y, Zhang Z, Li M, Chang H, Luo XJ. Functional genomic analysis delineates regulatory mechanisms of GWAS-identified bipolar disorder risk variants. Genome Med. 2022;14:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 61. | Baeza I, de la Serna E, Mezquida G, Cuesta MJ, Vieta E, Amoretti S, Lobo A, González-Pinto A, Díaz-Caneja CM, Corripio I, Valli I, Puig O, Mané A, Bioque M, Ayora M, Bernardo M, Castro-Fornieles J; PEPs group. Prodromal symptoms and the duration of untreated psychosis in first episode of psychosis patients: what differences are there between early vs. adult onset and between schizophrenia vs. bipolar disorder? Eur Child Adolesc Psychiatry. 2024;33:799-810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 62. | Koirala P, Anand A. Diagnosing and treating bipolar disorder in primary care. Cleve Clin J Med. 2018;85:601-608. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 63. | Patrick RE, Heintz HL, Skurla MD, Forester BP. A Comprehensive Review of the Evaluation, Diagnosis, and Treatment of Older Adult Bipolar Disorder. Curr Treat Options Psych. 2020;7:508-530. [DOI] [Full Text] |
| 64. | Coventry P, Lovell K, Dickens C, Bower P, Chew-Graham C, McElvenny D, Hann M, Cherrington A, Garrett C, Gibbons CJ, Baguley C, Roughley K, Adeyemi I, Reeves D, Waheed W, Gask L. Integrated primary care for patients with mental and physical multimorbidity: cluster randomised controlled trial of collaborative care for patients with depression comorbid with diabetes or cardiovascular disease. BMJ. 2015;350:h638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 185] [Cited by in RCA: 188] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 65. | van der Lee AP, Hoogendoorn A, Kupka R, Haan L, Beekman AT. Discontinuity of psychiatric care among patients with bipolar disorder in the Netherlands. Int J Soc Psychiatry. 2024;207640241278291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 66. | Tondo L, Vázquez GH, Baldessarini RJ. Depression and Mania in Bipolar Disorder. Curr Neuropharmacol. 2017;15:353-358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 100] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 67. | Terao T, Ishida A, Kimura T, Yarita M, Hara T. Preventive Effects of Lamotrigine in Bipolar II Versus Bipolar I Disorder. J Clin Psychiatry. 2017;78:e1000-e1005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 68. | Dell'Osso B, Holtzman JN, Goffin KC, Portillo N, Hooshmand F, Miller S, Dore J, Wang PW, Hill SJ, Ketter TA. American tertiary clinic-referred bipolar II disorder compared to bipolar I disorder: More severe in multiple ways, but less severe in a few other ways. J Affect Disord. 2015;188:257-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 69. | Holma KM, Haukka J, Suominen K, Valtonen HM, Mantere O, Melartin TK, Sokero TP, Oquendo MA, Isometsä ET. Differences in incidence of suicide attempts between bipolar I and II disorders and major depressive disorder. Bipolar Disord. 2014;16:652-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 129] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 70. | Novick DM, Swartz HA, Frank E. Suicide attempts in bipolar I and bipolar II disorder: a review and meta-analysis of the evidence. Bipolar Disord. 2010;12:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 221] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 71. | Geddes JR, Miklowitz DJ. Treatment of bipolar disorder. Lancet. 2013;381:1672-1682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 523] [Cited by in RCA: 483] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 72. | Solé B, Jiménez E, Torrent C, Reinares M, Bonnin CDM, Torres I, Varo C, Grande I, Valls E, Salagre E, Sanchez-Moreno J, Martinez-Aran A, Carvalho AF, Vieta E. Cognitive Impairment in Bipolar Disorder: Treatment and Prevention Strategies. Int J Neuropsychopharmacol. 2017;20:670-680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 182] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 73. | Prabhavalkar KS, Poovanpallil NB, Bhatt LK. Management of bipolar depression with lamotrigine: an antiepileptic mood stabilizer. Front Pharmacol. 2015;6:242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 45] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 74. | Sharma V, Khan M, Corpse C. Role of lamotrigine in the management of treatment-resistant bipolar II depression: a chart review. J Affect Disord. 2008;111:100-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 75. | Persson C, Kardell M, Karanti A, Isgren A, Annerbrink K, Landen M. [Prescribed drug use for bipolar disorder type I and II in clinical practice]. Läkartidningen. 2017;114:D77T. [PubMed] |
| 76. | Hooshmand F, Do D, Shah S, Gershon A, Park DY, Kim H, Yuen LD, Dell'Osso B, Wang PW, Ketter TA, Miller S. Differential prevalence and demographic and clinical correlates of antidepressant use in American bipolar I versus bipolar II disorder patients. J Affect Disord. 2018;234:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 77. | Brancati GE, Nunes A, Scott K, O'Donovan C, Cervantes P, Grof P, Alda M. Differential characteristics of bipolar I and II disorders: a retrospective, cross-sectional evaluation of clinical features, illness course, and response to treatment. Int J Bipolar Disord. 2023;11:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 78. | Swartz HA, Thase ME. Pharmacotherapy for the treatment of acute bipolar II depression: current evidence. J Clin Psychiatry. 2011;72:356-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 34] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 79. | Datto C, Pottorf WJ, Feeley L, LaPorte S, Liss C. Bipolar II compared with bipolar I disorder: baseline characteristics and treatment response to quetiapine in a pooled analysis of five placebo-controlled clinical trials of acute bipolar depression. Ann Gen Psychiatry. 2016;15:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 80. | Johnson DE, McIntyre RS, Mansur RB, Rosenblat JD. An update on potential pharmacotherapies for cognitive impairment in bipolar disorder. Expert Opin Pharmacother. 2023;24:641-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |