Published online Aug 19, 2024. doi: 10.5498/wjp.v14.i8.1224
Revised: May 28, 2024
Accepted: July 10, 2024
Published online: August 19, 2024
Processing time: 109 Days and 19.7 Hours
Psychological problems affect economic development. However, there is a huge gap between mental health service resources and mental health service needs. Existing mental health service technology and platforms cannot meet all the diverse mental health needs of people. Smart medicine is a new medical system based online that can effectively improve the quality and efficiency of medical services and make mental health services accessible.
To explore the level of intelligent medical use among young and middle-aged people and its correlation with psychological factors.
Convenience sampling was used to select 200 young and middle-aged patients with medical experience at the Third People's Hospital of Chengdu between January 2022 and January 2023 as the research subjects. The general condition Questionnaire, Eysenck Personality Questionnaire, Symptom Checklist-90, General Health Questionnaire, and Smart Medical Service Use Intention Questionnaire were used to collect data. Pearson’s correlation was used to analyze the correlation between the participants’ willingness to use smart medical services and their personality characteristics, psychological symptoms, and mental health.
The results revealed that the mental health of young and middle-aged people was poor, and some had psychological problems such as anxiety, depression, and physical discomfort. Familiarity, acceptance, and usage of smart healthcare in this population are at a medium level, and these levels correlate with psychological characteristics. Acceptance was positively correlated with E, and negatively correlated with P, anxiety, fear, anxiety/insomnia, and social dysfunction. The degree of use was negatively correlated with P, obsessive-compulsive symptoms, depression, anxiety, hostility, paranoia, and somatic symptoms.
The familiarity, acceptance, and usage of smart medical services among the middle-aged and young groups are related to various psychological characteristics.
Core Tip: Smart healthcare refers to making full use of limited medical manpower and equipment resources based on advanced Internet + and Internet of Things technologies and giving full play to the medical technology advantages of large hospitals to create a regional medical information platform for health records and realize the interaction between patients and medical personnel, medical institutions, and medical equipment. A new medical system that provides information and mobile and remote medical services for disease diagnosis, monitoring, and treatment.
- Citation: Zhang H, Liu Y, Gu R. Correlation between psychological traits and the use of smart medical services in young and middle-aged adults: An observational study. World J Psychiatry 2024; 14(8): 1224-1232
- URL: https://www.wjgnet.com/2220-3206/full/v14/i8/1224.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i8.1224
The development of "Internet +" promotes the integration of cloud computing and other network technologies with the medical industry, and the term "smart medical" frequently appears in people's vision[1]. Smart healthcare is a medical service model centered on patient data that advocates patient-centered care and provides convenient and quick communication channels for medical staff and patients. Through intelligent medical treatment, medical staff can obtain patient case reports and medical records at any time to quickly diagnose diseases and make treatment plans; at the same time, patients can know their own health status any time[2]. Related studies show that smart healthcare can optimize the medical environment and provide convenient medical services for the older adult population[3]. However, studies also indicate that the current awareness and usage rate of smart healthcare is relatively low, and therefore, targeted measures are needed to increase the usage rate of smart healthcare[4]. Therefore, targeted measures should be taken to improve the utilization rate of smart medical care[4]. In addition, smart medical care focuses not only on patient treatment but also on patient mental health. Relevant studies have indicated that smart medical products can provide special services according to the physiological characteristics and psychological needs of patients with chronic diseases, reduce their psychological pressure, and enhance their confidence in life[5]. However, research on smart healthcare has mainly focused on the utilization rate and psychological needs of vulnerable groups; there has been no exploration of the utilization and mental health status of young and middle-aged groups[6,7]. As the backbone of society, young and middle-aged people are under pressure from work, family, society and other aspects, and are more prone to negative emotions, which should be paid more attention to. Research has found that middle-aged and young adults have a higher incidence of depression, anxiety, and acute or transient mental disorders[8]. Based on this knowledge, this study considers young and middle-aged groups as research objects to explore the status quo of their willingness to use smart medical services and their correlation with psychological characteristics, aiming at improving the popularity and utilization rate of smart medical services.
Convenience sampling was used to select 200 young and middle-aged patients with medical experience at the Third People's Hospital of Chengdu between January 2022 and January 2023 as the research subjects.
Inclusion criteria: No major physiological diseases; The clinical data were complete.
Exclusion criteria: Dropouts.
General condition questionnaire: The self-designed questionnaire included questions on sex, age, marital status, education level, monthly family income per capita, household registration type, and medical insurance type.
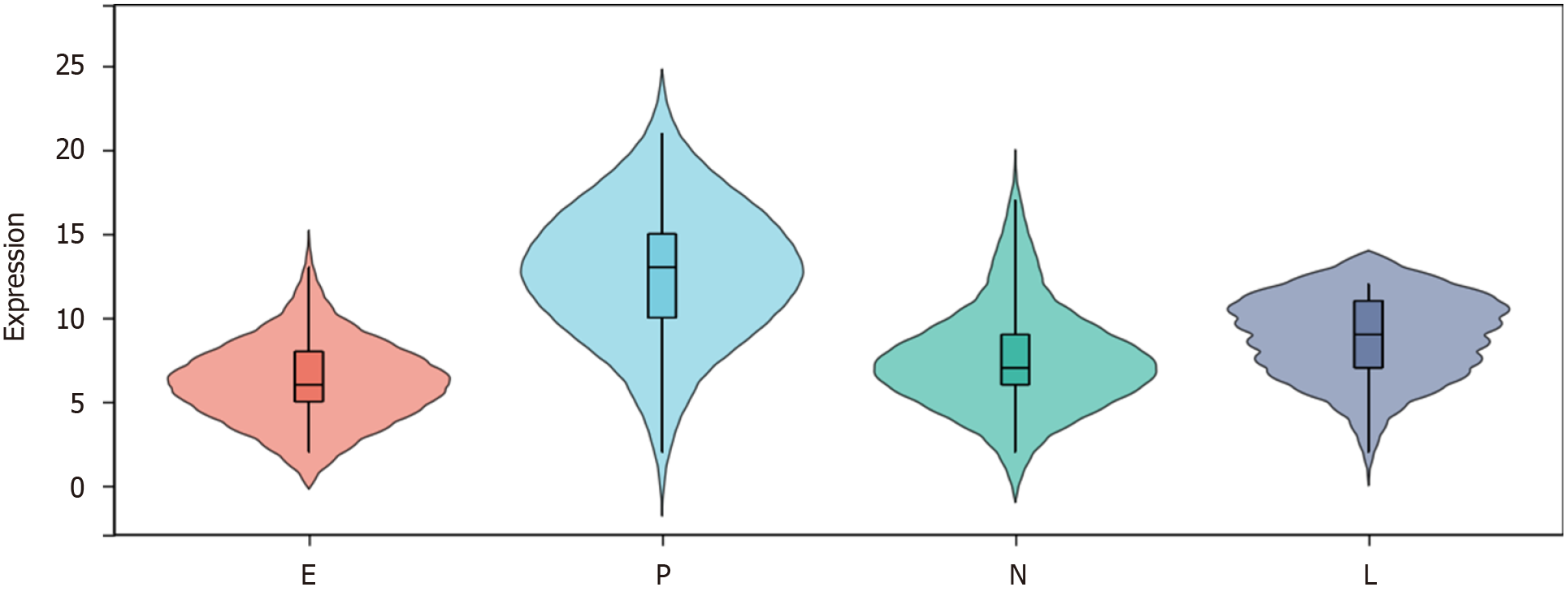
Eysenck Personality Questionnaire for adults: The scale is an effective personality measurement tool compiled by the British psychologist Eysenck[9]. It involves the affirmation and negation of social life, self-consciousness, and emotion and is commonly used to analyze the traits or structure of personality. The scale includes four subscales: extroversion (E), psychoticism (P), neuroticism (N), and lying (L), with 21, 23, 24, and 20 items in each subscale, respectively, for a total of 88 items. The scale uses “yes” or “no” to evaluate the relevant questions, with one point for correct answers and no points for incorrect answers. The reliability and validity of the scale ranged from 0.74 to 0.78[10].
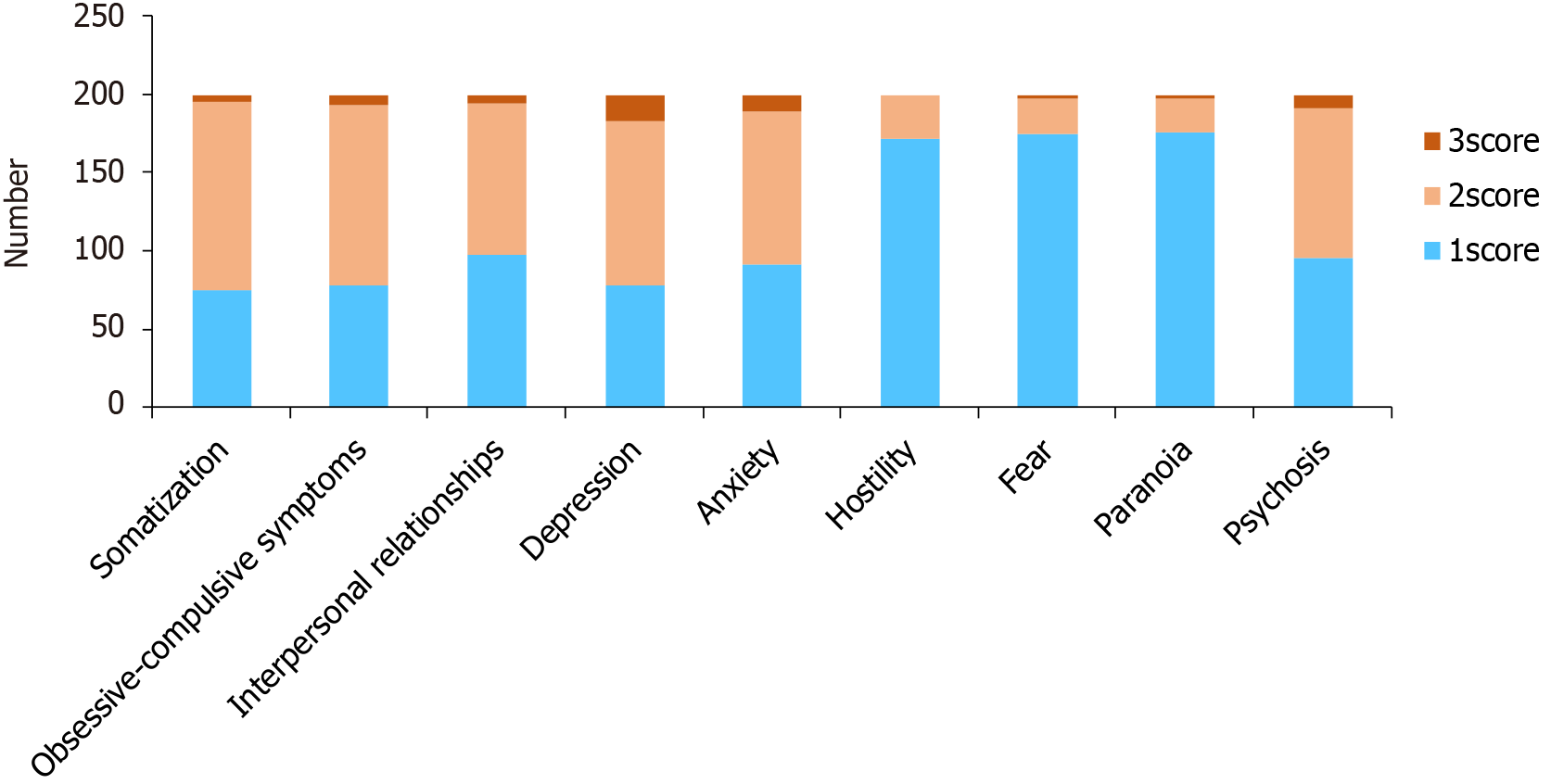
Symptom Checklist-90: This scale was adapted from the Hopkins symptoms checklist compiled by Derogatis[11]. The psychological symptoms and their severity were evaluated from the perspectives of feeling, emotion, thinking, consciousness, behavior, living habits, interpersonal relationships, diet, and sleep. The scale has nine factors and a total of 90 items. The scale uses a 5-point scoring method, ranging from "none" to "severe.” The factor score is the total score of each item in a factor/number of items in a factor. The scores range from 1 to 5, with higher scores indicating more severe symptoms. The scale’s reliability and validity were 0.871[12].
General Health Questionnaire: The scale was developed by Goldberg[13], including 28 items and four factors including somatic symptoms, anxiety/insomnia, social dysfunction, and severe depression. A four-stage scale is used, ranging from 0 for "never" to 3 for "often,” with 7 questions for each scale. The score range for each scale was 0-21, and the total score range was 0-84. A high score indicates a lower level of mental health, and a total score of more than 21 indicates poor mental health. Scale for the reliability and validity of 0.872[14].
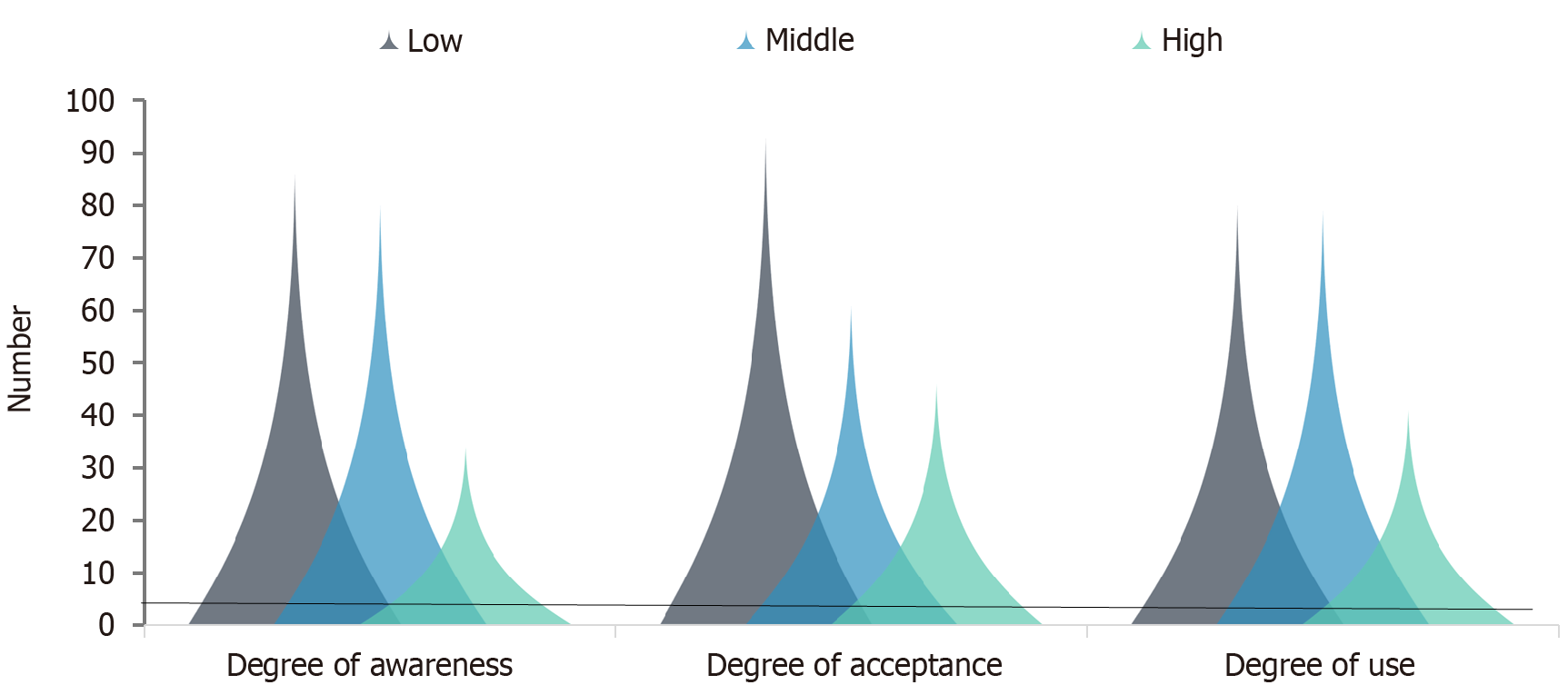
Smart medical services use intention questionnaire: A questionnaire on the willingness to use smart medical services was created with reference to relevant questions in the literature on the status quo of smart medical service use[15] to understand the willingness of middle-aged and young people to use smart medical services. It mainly includes the three dimensions of smart healthcare awareness, acceptance, and usage, with a total of 12 items. A 5-point scale was used, with a score of 5 for strongly agreeing and 1 for strongly disagreeing, with higher scores indicating a stronger intention to use.
Quality control: After the questionnaire was designed, a two-dimensional code was generated and posted on the platform, and the research subjects completed the questionnaire in an anonymous form. Two staff members were responsible for the release of the questionnaires and statistics of the results.
Statistical software (SPSS 27.0) was used to process the data from 200 young and middle-aged people. The measurement data were expressed as mean ± SD, and the count data were expressed as rate (%). Pearson’s correlation was used to analyze the correlation between young and middle-aged people's willingness to use smart medical services and their personality characteristics, psychological symptoms, and mental health status. P < 0.05 was considered statistically significant.
There were 123 males (61.50%) and 77 females (38.50%) with an average age of (34.35 ± 2.42) years (range, 30-39 years). There were 165 married cases (82.50%) and 35 unmarried cases (17.50%) patients. 69 cases (34.50%) had a junior high school education or below, and 131 patients (65.50%) had a junior high school education or above. Of these, 57 cases (28.50%) had a per capita monthly household income of < 3000 yuan, 143 cases (71.50%) had a per capita monthly household income of ≥ 3000 yuan. There were 97 cases (48.50%) with agricultural household registration and 103 cases (51.50%) without agricultural household registration. There were 21 cases (10.50%) without medical insurance, 131 cases (65.50%) with new rural cooperative medical insurance/medical insurance for urban and rural residents, 43 cases (21.50%) with urban medical insurance, and 5 cases (2.50%) with free medical insurance and commercial medical insurance.
The scores of Eysenck Personality Questionnaire (EPQ) scale were: 6.15 ± 2.21, 12.64 ± 3.77, 7.57 ± 2.85 and 8.84 ± 2.31, respectively (Figure 1).
The score of somatization dimension was 1.64 ± 0.50, obsessive-compulsive symptom dimension was 1.74 ± 0.55, interpersonal relationship dimension was: 1.53 ± 0.53, depression dimension was 1.90 ± 0.65, anxiety dimension was 1.59 ± 0.59. The scores of hostility, fear, paranoia, and psychosis were: 1.08 ± 0.27, 1.07 ± 0.31, 1.08 ± 0.31 and 1.57 ± 0.59, respectively. Except for the hostile dimension, which was scored from 1 to 2, the scores of the other dimensions ranged from 1 to 3; the specific distribution is shown in Figure 2.
The somatic symptom scores ranged from 1 to 13, with an average of 6.72 ± 2.30. Anxiety/insomnia scores ranged from 1 to 16, with an average of 7.53 ± 3.18. The social dysfunction scores ranged from 2 to 10, with an average of 5.85 ± 1.31. The scores for major depression ranged from 2 to 8, with an average score of 5.08 ± 1.14.
The average scores of cognition, acceptance, and usage were: 13.70 ± 3.54, 13.64 ± 3.42 and 13.16 ± 3.59 respectively. To fully understand the willingness of young and middle-aged people to use smart healthcare, the scores for each dimension were divided into P50 and P75. In the cognitive dimension, scores of < 14 points indicated low familiarity, 14-17 points indicated medium familiarity and > 17 points indicated medium and high familiarity. Acceptance dimension: < 14 points indicated a low level of acceptance, 14-16 points indicated a medium level of acceptance, and > 16 points indicated a high level of acceptance. Dimensions of use: < 13 indicates a low level of use, 13-16 indicates a medium level of use, and > 16 indicates a high level of use. See Figure 3 for the specific distribution of familiarity, acceptance and usage among 200 young and middle-aged people.
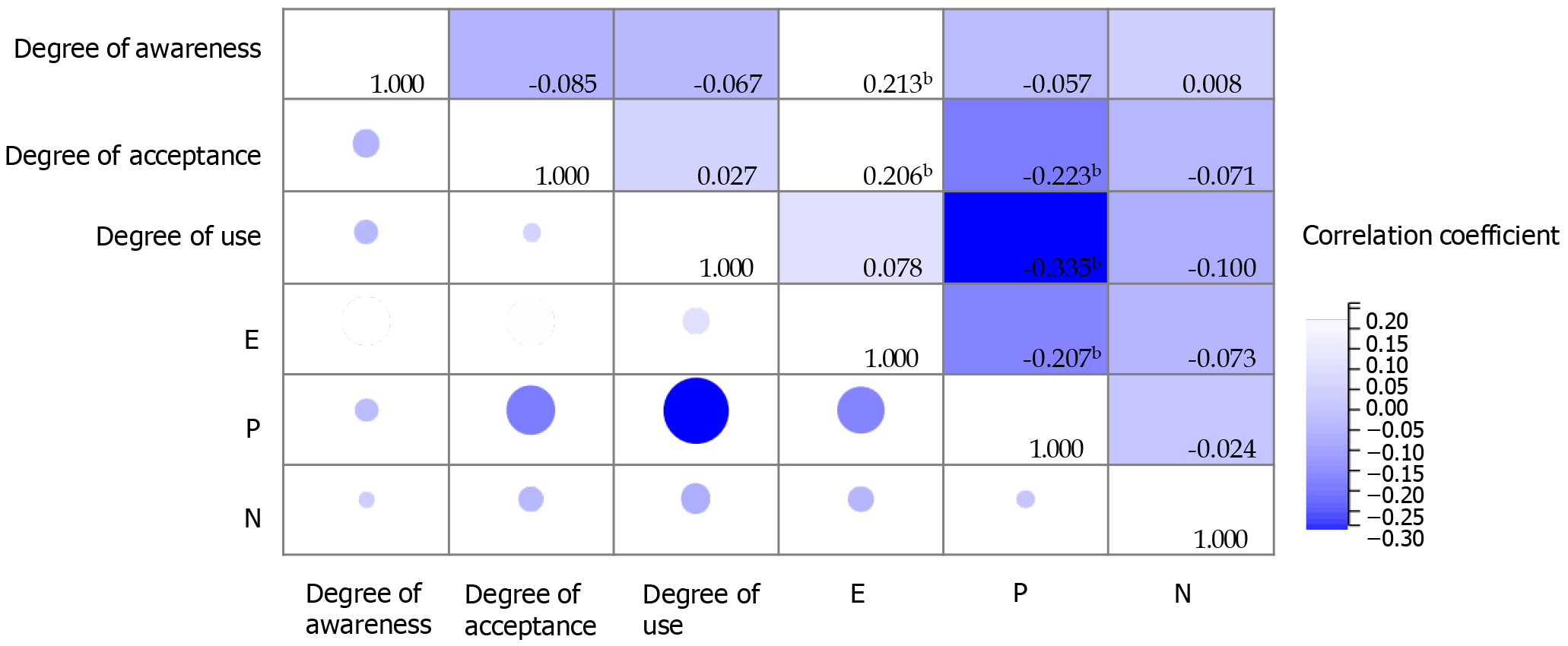
Awareness of intelligent medical services among young and middle-aged people was positively correlated with E (P < 0.05), and negatively correlated with somatization, obsessive-compulsive symptoms, interpersonal relationships, depression, fear, paranoia, psychotic dimensions, somatic symptoms, anxiety/insomnia, and severe depression (P < 0.05). Acceptance was positively correlated with E (P < 0.05), and negatively correlated with P, anxiety, fear, anxiety/insomnia, and social dysfunction (P < 0.05). The degree of use was negatively correlated with P, obsessive-compulsive symptoms, depression, anxiety, hostility, paranoid dimensions, and somatic symptoms (P < 0.05) (Figure 4, Tables 1 and 2).
| Degree of awareness | Degree of acceptance | Degree of use | |
| Somatization | -0.367b | -0.038 | -0.056 |
| Obsessive-compulsive symptoms | -0.266b | -0.032 | -0.161a |
| Interpersonal relation | -0.222b | -0.126 | -0.080 |
| Depression | -0.208b | -0.062 | -0.153a |
| Anxiety | -0.138 | -0.154a | -0.141a |
| Hostility | -0.137 | -0.105 | -0.162a |
| Fear | -0.174a | -0.200b | -0.016 |
| Paranoia | -0.206b | -0.042 | -0.161a |
| Psychosis | -0.202b | 0.064 | -0.054 |
Smart healthcare is a medical service model centered on patient data and has a wide range of application scenarios, including telemedicine applications such as remote consultation, remote surgery, and emergency rescue, as well as smart guidance, mobile medical care, smart campus management, and AI-assisted diagnosis and treatment. It has important research significance and development potential in many fields[16,17]. However, smart healthcare started late in China, and owing to an imbalance in regional development, the smart healthcare system has not been fully popularized in some regions and groups.
Intelligent medical treatment has been developed based on modern scientific and technological means, and its audience consists mostly of young and middle-aged groups. This study shows that familiarity, acceptance, and use of smart medical care among young and middle-aged people are at a medium level, and only 20% of the participants have high cognition, high acceptance, and high willingness to use it. The reasons are as follows. First, young and middle-aged people generally have high technological literacy and Internet use experience, and their acceptance of new technologies and services is high. Intelligent medical services provide a more convenient, efficient, and personalized medical service experience through digital, automated, and intelligent technical means, which is in line with the pursuit of a high-quality and efficient life for middle-aged and young people[18]. Second, young and middle-aged people face greater work and life pressures and pay more attention to health management and disease prevention.
Smart medical services can provide comprehensive health monitoring, disease prevention, remote diagnosis and treatment, and other functions to help patients manage their health status better and relieve the strain and inconvenience of medical resources[19]. However, the willingness of young and middle-aged people to use smart medical services is also affected by certain factors. On one hand, they are concerned about privacy leakage and data insecurity. However, the poor service quality of some smart medical systems may reduce their willingness to use the same[20,21]. Therefore, to promote continuous development, it is necessary to strengthen information protection and improve the service quality of smart healthcare.
The mental health status of young and middle-aged people is a complex and multi-dimensional issue of widespread concern around the world. Lanz et al[22] found that middle-aged and young people have the highest levels of stress and future anxiety and the poorest mental health status. This current study explores the psychological characteristics of 200 middle-aged and young people using EPQ, Symptom Checklist-90 (SCL-90), and General Health Questionnaire (GHQ-28). The results indicate that the mental health status of the participants was poor, specifically manifested as high scores on the EPQ dimensions of psychoticism and neuroticism, high scores on the SCL-90 dimensions of somatization, obsessive-compulsive symptoms, and depression, and high scores on the GHQ-28 dimensions of anxiety/insomnia and somatic symptoms. The results suggested that the participants were under a lot of pressure and were prone to anxiety, emotional instability, and physical discomfort, which is consistent with the above research results. This could be attributed to a number of reasons: first, middle-aged and young people are usually at a critical stage of career development and face considerable work pressures. Long working hours, high work pressure, and uncertainty about career development may all lead to anxiety and depression. Massamba et al[23] explored the work and psychosocial factors of 1736 white-collar workers and found that nearly 40% of them faced high levels of work pressure, and high levels of effort were accompanied by low returns, resulting in an imbalanced state and the potential for health problems. Second, this group also has to shoulder the responsibility of taking care of the family, raising children, and supporting older adults, which may bring economic and psychological pressure to bear and lead to psychological problems. Kim et al[24] pointed out in their study that during the epidemic period, schools were closed and parents had to devote themselves to taking care of their children and the elderly at home, which intensified parents' psychological pressure and affected their mental health. Furthermore, middle-aged and young people may face interpersonal tensions in relationship and social anxiety problems. They may feel they need to constantly adapt to different social environments and establish and maintain relationships with different groups of people, and this pressure may lead to the occurrence of psychological problems. Mistretta et al[25] pointed out that depressive symptoms in the middle-aged group are related to social processes and interpersonal tension. Additionally, due to long-term fatigue and irregular sleep patterns, some middle-aged people have physical diseases or health problems, which may also have a negative impact on their mental health[26]. Therefore, it is necessary to understand the mental health status of the middle-aged and young group and take measures to reduce their stress.
This study indicates that the willingness to use smart medical services in young and middle-aged populations is correlated with psychological characteristics. Specifically, the degree of awareness was positively correlated with extraversion and negatively correlated with somatization, obsessive-compulsive symptoms, interpersonal relationships, depression, fear, paranoia, psychotic dimensions, somatic symptoms, anxiety/insomnia, and severe depression. Acceptance was positively correlated with extraversion and negatively correlated with psychoticism, anxiety, fear, anxiety/insomnia, and social dysfunction. The degree of use was negatively correlated with psychoticism, obsessive-compulsive symptoms, depression, anxiety, hostility, paranoia, and somatic symptoms.
First, some psychological characteristics, such as openness, curiosity, and innovation ability, may encourage people’s acceptance and use of smart medical services. These psychological characteristics make people more willing to try new technologies, thereby increasing their likelihood of using smart medical services[27]. Second, when people experience negative emotions such as anxiety, depression, and psychoticism, their thinking mode may become narrow, and it is difficult to comprehensively and objectively evaluate new products or services, which leads to their biased cognition of smart medical services and a reduced utilization rate[28]. In addition, individuals with sensitive interpersonal relation
In addition, somatization, obsessive-compulsive disorder, and paranoia all reflect an individual's mental state, which will also impact the acceptance of things in young and middle-aged groups[30]. However, smart healthcare can promote mental health among young and middle-aged people by providing convenient mental health services, personalized mental health management, integrating mental health and physical health services, and promoting social interaction and emotional support.
This study has some limitations: First, the sample size is relatively small, and the results may be biased; second, the survey scales used in this study are dependent on the respondents' self-report and assessment. This means the results could be affected by individual subjective perceptions, ability to understand the questions, and ability to express themselves clearly, which could impact the objectivity and accuracy of the data. Therefore, future studies can increase the sample size and consider the limitations of the scales in the survey, and combine other research methods for comprehensive analysis to improve the reliability of the data.
This study explored young and middle-aged people’s willingness to use smart medical services and its correlation with psychological characteristics. The results revealed that the mental health of young and middle-aged people was poor, and some had psychological problems such as anxiety, depression, and physical discomfort. Familiarity, acceptance, and usage of smart healthcare in this population are at a medium level, and these levels correlate with psychological characteristics. Therefore, we should pay more attention to the mental health of young and middle-aged groups and improve mental health services through intelligent medical service systems to reduce their psychological stress and promote the development of intelligent medical services.
| 1. | Ghersi I, Mariño M, Miralles MT. Smart medical beds in patient-care environments of the twenty-first century: a state-of-art survey. BMC Med Inform Decis Mak. 2018;18:63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Jiang J, Zhang J, Sun J, Wu D, Xu S. User's image perception improved strategy and application of augmented reality systems in smart medical care: A review. Int J Med Robot. 2023;19:e2497. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Xu Z, Shi D, Tu Z. Research on Diagnostic Information of Smart Medical Care Based on Big Data. J Healthc Eng. 2021;2021:9977358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Maulik PK, Devarapalli S, Kallakuri S, Praveen D, Jha V, Patel A. Systematic Medical Appraisal, Referral and Treatment (SMART) Mental Health Programme for providing innovative mental health care in rural communities in India. Glob Ment Health (Camb). 2015;2:e13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Nourse R, Lobo E, McVicar J, Kensing F, Islam SMS, Kayser L, Maddison R. Characteristics of Smart Health Ecosystems That Support Self-care Among People With Heart Failure: Scoping Review. JMIR Cardio. 2022;6:e36773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 6. | Huang Q, Li Y, Wu X, Ge S, Qu Z, Wang A, Tang X. The willingness and influencing factors to choose smart senior care among old adults in China. BMC Geriatr. 2022;22:967. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Zhang Q, Li M, Wu Y. Smart home for elderly care: development and challenges in China. BMC Geriatr. 2020;20:318. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 8. | Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, Il Shin J, Kirkbride JB, Jones P, Kim JH, Kim JY, Carvalho AF, Seeman MV, Correll CU, Fusar-Poli P. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27:281-295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1834] [Cited by in RCA: 1510] [Article Influence: 503.3] [Reference Citation Analysis (1)] |
| 9. | Li H, Zou Y, Wang J, Yang X. Role of Stressful Life Events, Avoidant Coping Styles, and Neuroticism in Online Game Addiction among College Students: A Moderated Mediation Model. Front Psychol. 2016;7:1794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 10. | Wei Y, Li H, Wang H, Zhang S, Sun Y. Psychological Status of Volunteers in a Phase I Clinical Trial Assessed by Symptom Checklist 90 (SCL-90) and Eysenck Personality Questionnaire (EPQ). Med Sci Monit. 2018;24:4968-4973. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Xu YJ, Wang Q, Su L, Dai XY, Zhu XY. Analysis of Scores of SCL-90 of Patients with Traumatic Subdural Effusion. Fa Yi Xue Za Zhi. 2020;36:223-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Yu Y, Wan C, Zhao X, Huebner ES, Tan J, Xu C, Zhang J. Undergraduate students' norms for the Chinese version of the symptom check-List-90-R (SCL-90-R). BMC Public Health. 2020;20:1588. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Richard C, Lussier MT, Gagnon R, Lamarche L. GHQ-28 and cGHQ-28: implications of two scoring methods for the GHQ in a primary care setting. Soc Psychiatry Psychiatr Epidemiol. 2004;39:235-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Hjelle EG, Bragstad LK, Zucknick M, Kirkevold M, Thommessen B, Sveen U. The General Health Questionnaire-28 (GHQ-28) as an outcome measurement in a randomized controlled trial in a Norwegian stroke population. BMC Psychol. 2019;7:18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Lu L, Zhang J, Xie Y, Gao F, Xu S, Wu X, Ye Z. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR Mhealth Uhealth. 2020;8:e18907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 244] [Article Influence: 48.8] [Reference Citation Analysis (0)] |
| 16. | Chia-Jung H, Tzu-Chi H, Pei-Chang H. The Application of Smart Medical Care in Community Health Maintenance from User Experience: A Preliminary Study in College Students. Stud Health Technol Inform. 2021;284:328-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Richter I, Mielke C, Haux R. Development of a Role Model for the Use of Smart Home Based Data in Medical Care. Stud Health Technol Inform. 2021;281:679-683. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Yao R, Zhang W, Evans R, Cao G, Rui T, Shen L. Inequities in Health Care Services Caused by the Adoption of Digital Health Technologies: Scoping Review. J Med Internet Res. 2022;24:e34144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 151] [Article Influence: 50.3] [Reference Citation Analysis (0)] |
| 19. | Winter A, Stäubert S, Ammon D, Aiche S, Beyan O, Bischoff V, Daumke P, Decker S, Funkat G, Gewehr JE, de Greiff A, Haferkamp S, Hahn U, Henkel A, Kirsten T, Klöss T, Lippert J, Löbe M, Lowitsch V, Maassen O, Maschmann J, Meister S, Mikolajczyk R, Nüchter M, Pletz MW, Rahm E, Riedel M, Saleh K, Schuppert A, Smers S, Stollenwerk A, Uhlig S, Wendt T, Zenker S, Fleig W, Marx G, Scherag A, Löffler M. Smart Medical Information Technology for Healthcare (SMITH). Methods Inf Med. 2018;57:e92-e105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 20. | Zhang L, Hu X. Analysis of the Smart Medical Service Model in Super-Aged Society-UR Agency as an Example. J Healthc Eng. 2022;2022:8368057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 21. | Almalawi A, Khan AI, Alsolami F, Abushark YB, Alfakeeh AS. Managing Security of Healthcare Data for a Modern Healthcare System. Sensors (Basel). 2023;23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 22. | Lanz M, Caliciuri R, Iafrate R, Regalia C, Rosnati R, Sorgente A. Covid-Related Stress in the Financial, Relational and Health Domains. Which Longitudinal Effects on Present and Future Perception? Psychol Rep. 2023;332941231161790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 23. | Massamba VK, Talbot D, Milot A, Trudel X, Dionne CE, Vézina M, Mâsse B, Gilbert-Ouimet M, Dagenais GR, Pearce N, Brisson C. Association between psychosocial work-related factors at midlife and arterial stiffness at older age in a prospective cohort of 1736 white-collar workers. BMJ Open. 2023;13:e073649. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Kim KW, Wallander JL, Wiebe D. Associations among COVID-19 Family Stress, Family Functioning, and Child Health-Related Quality of Life through Lifestyle Behaviors in Children. Children (Basel). 2024;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 25. | Mistretta EG, Davis MC, Yeung E. Family Strain Predicts Subsequent Depressive Symptoms in Middle-aged Adults: Hope Mediates and Self-compassion Moderates the Relation. J Soc Clin Psychol. 2020;39:25-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 26. | Kumar A. Some things aren't better left unsaid: Interpersonal barriers to gratitude expression and prosocial engagement. Curr Opin Psychol. 2022;43:156-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Joshanloo M. Reciprocal relationships between personality traits and psychological well-being. Br J Psychol. 2023;114:54-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 28. | Choi Y, Choi SH, Yun JY, Lim JA, Kwon Y, Lee HY, Jang JH. The relationship between levels of self-esteem and the development of depression in young adults with mild depressive symptoms. Medicine (Baltimore). 2019;98:e17518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 29. | Cain NM, De Panfilis C, Meehan KB, Clarkin JF. A Multisurface Interpersonal Circumplex Assessment of Rejection Sensitivity. J Pers Assess. 2017;99:35-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Forresi B, Michelini G, Sapuppo W, Costa G, Castellini G, Livellara S, Gregori Grgič R. Anger, personality traits and psychopathological symptoms in subjects exposed to negative interpersonal actions in workplaces: an observational study in a large sample attending a Center for Occupational Stress. Int Arch Occup Environ Health. 2022;95:1763-1773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |