Published online Jul 19, 2024. doi: 10.5498/wjp.v14.i7.1127
Revised: June 3, 2024
Accepted: June 19, 2024
Published online: July 19, 2024
Processing time: 68 Days and 2.1 Hours
Studies have shown a strong bidirectional association between diabetes and depression, with diabetes increasing the risk of developing depression and vice versa. Depression among patients with diabetes is associated with poor glycemic control, complications, and poor self-care.
To explore the present state of research globally concerning diabetes and depression, to aid understanding the current research landscape and identify potential future areas of research.
A bibliometric approach was used, utilizing the Scopus database to gather pertinent research articles released from 2004 to 2023. Analyses encompassed publication patterns, significant contributors, research focal points, prevalent themes, and the most influential articles, aimed at discerning emerging research subjects.
A total of 3229 publications that met the search criteria were identified. A significant increase in the number of publications related to diabetes and depression has been observed in the past two decades. The most productive nation was the USA (n = 1015; 31.43%), followed by China (n = 325; 10.07%), the UK (n = 236; 7.31%), and Germany (n = 218; 6.75%). Three principal themes in research on depression and diabetes were delineated by the analysis. First, the exploration of the elevated prevalence and etiology of this comorbidity; second, the focus on interventions, particularly randomized controlled trials, aimed at enhancing diabetes management among individuals with depression; and finally, the investigation of the involved risk factors and biological mechanisms under
There has been a recent surge of interest in the relationship between diabetes and depression. This could aid researchers to identify areas lacking in the literature and shape future research.
Core Tip: Although there have been numerous studies examining research productivity in diabetes or depression separately, there is a notable absence of a bibliometric analysis concentrating on the intersection of both conditions. Conducting bibliometrics in this regard will enable us to pinpoint the primary countries, institutions, journals, and research themes involved. Such insights will provide more comprehensive understanding of the present research landscape and offer guidance for future inquiries. By analyzing publication patterns across time, we can anticipate burgeoning areas of interest, thereby aiding in research funding allocations, program formulation, and policy development.
- Citation: Al-Jabi SW. Emerging global interest: Unraveling the link between diabetes mellitus and depression. World J Psychiatry 2024; 14(7): 1127-1139
- URL: https://www.wjgnet.com/2220-3206/full/v14/i7/1127.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i7.1127
Depression and diabetes mellitus (DM) have a complicated link in which one can both cause and predispose patients to the other[1-3]. Studies point to a strong correlation[4,5] between the incidence of diabetes and depression, especially type 2 DM (T2DM). However, the two diseases are negatively correlated. Individuals with severe depression may suffer from diabetes three times more frequently than the general population[6]. Common molecular pathways involving inflammation, autonomic dysfunction, changes to the central nervous system, and hypothalamic–pituitary–adrenal (HPA) axis activation are linked to these disorders[1,5,7,8].
T2DM and depression are inversely related to biological processes, including low-grade inflammation, hyperglycemia, and (micro)vascular dysfunction[8]. Depression and T2DM are related to molecular changes that impact the sympathetic nervous system, the HPA axis, and subclinical inflammation[2].
Patients with diabetes who have comorbid depression are more likely to have poor glycemic control, to use healthcare more frequently, to have more complications, and to die[3]. Patients with T2DM who have poor glycemic control are at risk of experiencing more complications from their disease and becoming depressed[9]. An emotional state brought on by having diabetes and the responsibility of self-management, diabetes distress, on its own, raises complications associated with the disease and is associated with worse health outcomes[6].
Depression and anxiety may arise from the psychological burden of diabetes and from the detrimental effects of problems on quality of life[1,5]. T2DM, depression, and anxiety are complexly related to psychosocial factors, including stress, lifestyle, socioeconomic background, and genetic background[1,5].
In individuals with diabetes, both pharmacological and individual psychological depression therapies are effective; however, the current treatment options are limited and have conflicting effects on glycemic outcomes[1,7]. Improving outcomes associated with diabetes appears to be best achieved by collaborative care programs that simultaneously manage both conditions[3]. It is advised to routinely screen diabetic patients for depression and distress, and psychological therapies tailored to diabetes may help depressed patients better manage their condition[6,10].
While research on diabetes and depression is growing, a gap exists in the bibliometric analysis of this specific link. This comprehensive approach to publication patterns can reveal key trends, influential institutions, and impactful research areas[11,12]. Bibliometrics helps us understand where the field stands and what future directions hold. In contrast, systematic reviews summarize existing research[13,14]. Notably, despite numerous studies on research productivity in either diabetes[15-23] or depression[24-31], a bibliometric analysis focusing on the co-occurrence of both conditions is lacking.
Bibliometrics in this context would allow us to identify leading countries, institutions, journals, and research themes. This knowledge will provide a deeper understanding of the current research landscape and guide future investigations. By analyzing publication trends over time, we can predict emerging areas of interest and inform research funding decisions, and program and policy development.
The research draws upon data retrieved from the Scopus database, which offers distinct advantages over other databases[32-35]. First, Scopus provides broad global and regional coverage of scientific journals, conference proceedings, and books, ensuring the inclusion of high-quality data. Second, Scopus furnishes comprehensive author and institution profiles through advanced profiling algorithms and manual curation, ensuring accuracy and completeness. Third, Scopus serves as a vital bibliometric data source for various large-scale analyses in research evaluations, scientific landscape studies, policy assessments, and university rankings. Fourth, Scopus data are accessible for specific academic research endeavors, facilitating investigations into areas such as researcher mobility, network visualizations, and spatial bibliometrics. Finally, Scopus offers individual profiles for authors, institutions, and publications, making it highly user-friendly for practical applications.
A literature search on depression and DM was conducted on April 13, 2024. The Scopus online advanced search function was utilized to identify relevant studies published between January 2004 and December 2023. Synonyms for both DM and depression were included in the search strategy.
Step 1: Several previous systematic reviews and meta-analyses on DM were consulted to identify relevant search terms[36-43]. These terms were subsequently incorporated into the article title. The title included: diabetic, diabetes, type 2 DM, type 1 DM, T2DM, T1DM, glycemic control, glycaemic control, elevated blood glucose, and elevated blood sugar.
Step 2: The first step involved narrowing the publications to only those containing the terms "depression and linked terms" in their titles. To accomplish this, we utilized several previous systematic reviews and meta-analyses on DM[36-43] to generate keywords, which were then used in the Scopus search engine to fulfill the study objective. The "Article Title" field was populated with the following terms: Depress* OR "seasonal affective" OR dysthym* OR "affective disorder" OR "mood disorder*" OR "bipolar disorder".
To avoid any misinterpretation, we excluded publications related to depressed heart disease or depressed cardiac disease. Consequently, keywords were used instead of conducting a title/abstract search. The title search yielded a minimal number of false-positive results, rendering it a dependable approach[44-46]. Conversely, a title/abstract search may generate numerous false positives, focusing not primarily on DM and depression but on other subjects.
Step 3: The research limits its scope to peer-reviewed scientific journal articles, excluding books, book chapters, retracted articles, and errata.
The current research environment was mapped using numerical data from the collected articles. This analysis focused on publication trends, the types of documents included, where they were published (journals), and who produced them (countries, institutions, and funding agencies). Additionally, consideration was given to how often the articles were cited by others to measure their influence.
The search approach was utilized, and the collected data were exported to a "CSV" file format in Microsoft Excel. VOSviewer 1.6.20 (Leiden University, Leiden, The Netherlands) was used to illustrate the network characteristics among countries and co-occurring terms found in titles and abstracts, providing a visual representation of the results[47,48]. VOSviewer can be used to construct knowledge networks rooted in scientific principles, illustrating the evolution of research fields and facilitating the anticipation of future research trends and international collaborations. The co-occurrence analysis of VOSviewer categorizes terms into distinct clusters, each represented by a unique color. Through a term co-occurrence network, maps were generated to identify the most frequently occurring terms in titles and abstracts, thereby delineating research hotspots as thematic clusters.
After being exported from Scopus, the data were imported into Microsoft Word from Microsoft Office Excel. VOSviewer version 1.6.20 and Microsoft Excel 2013 were used to create the figures. Frequencies and percentages were used to present descriptive statistics. The top 10 rankings in each category were taken into consideration after bibliometric analysis was transformed into rankings incorporating countries, cited publications, funding agencies, journals, and institutions. A space was added between ranking numbers when bibliometric analysis produced the same ranking number.
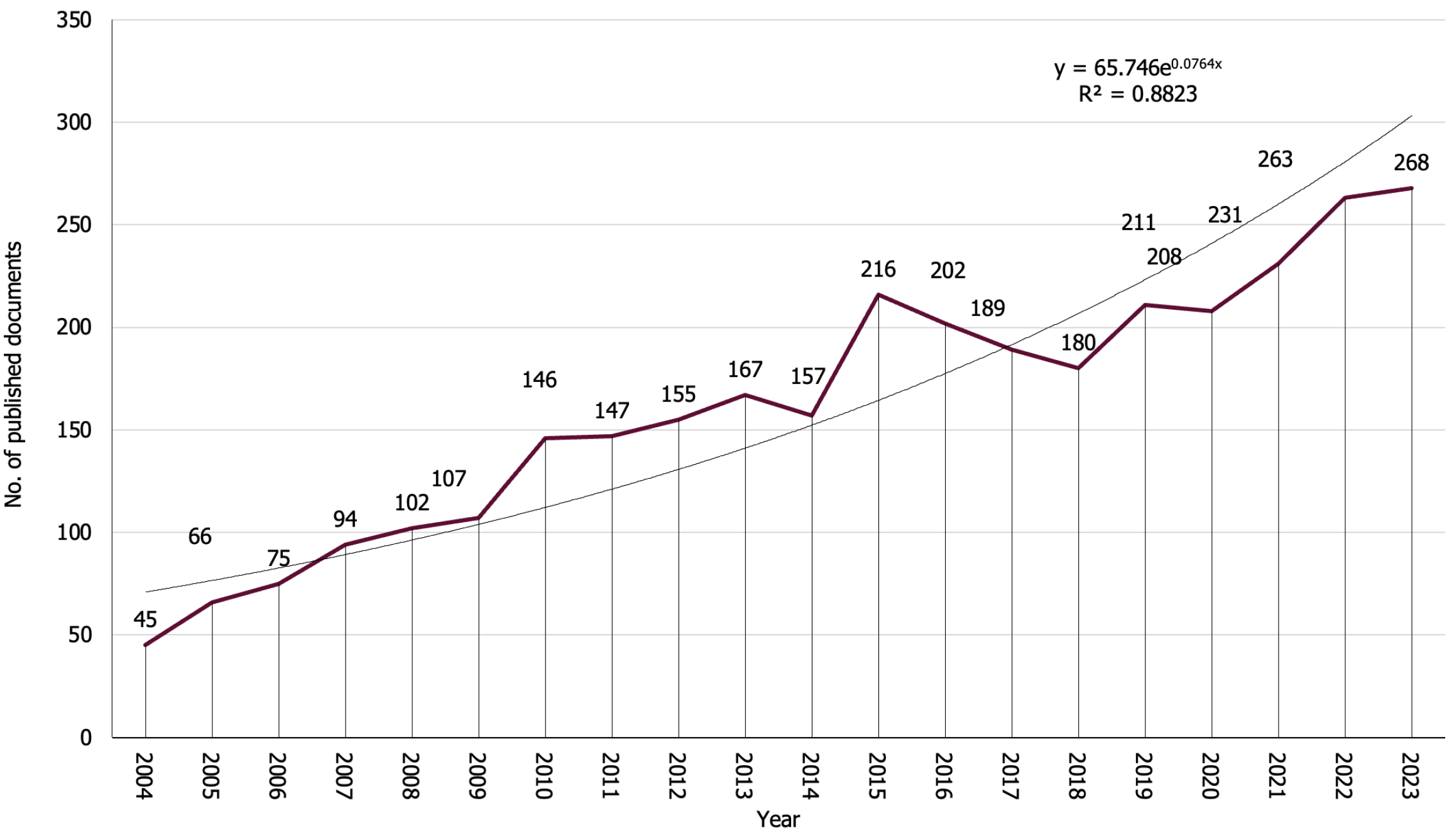
Between 2004 and 2023, 3229 publications that met the search criteria were identified. Of these, 2711 (83.96%) were original research articles, 286 (8.86%) reviews, 90 (2.79%) letters to the editor, and 142 (4.40%) were categorized under other classifications, such as notes or editorials. Over the past decade, there has been a notable surge in publications concerning the correlation between DM and depression. In 2004, there were 45 articles published on this topic, which escalated to 268 by 2023. Particularly since 2010, the rate of publication growth has accelerated significantly, with an average of over 195 articles being published each year (Figure 1). Linear regression analysis confirmed this pattern, revealing a modest positive correlation (R2 = 0.8823, P < 0.001) between the yearly count of publications and their respective publication years.
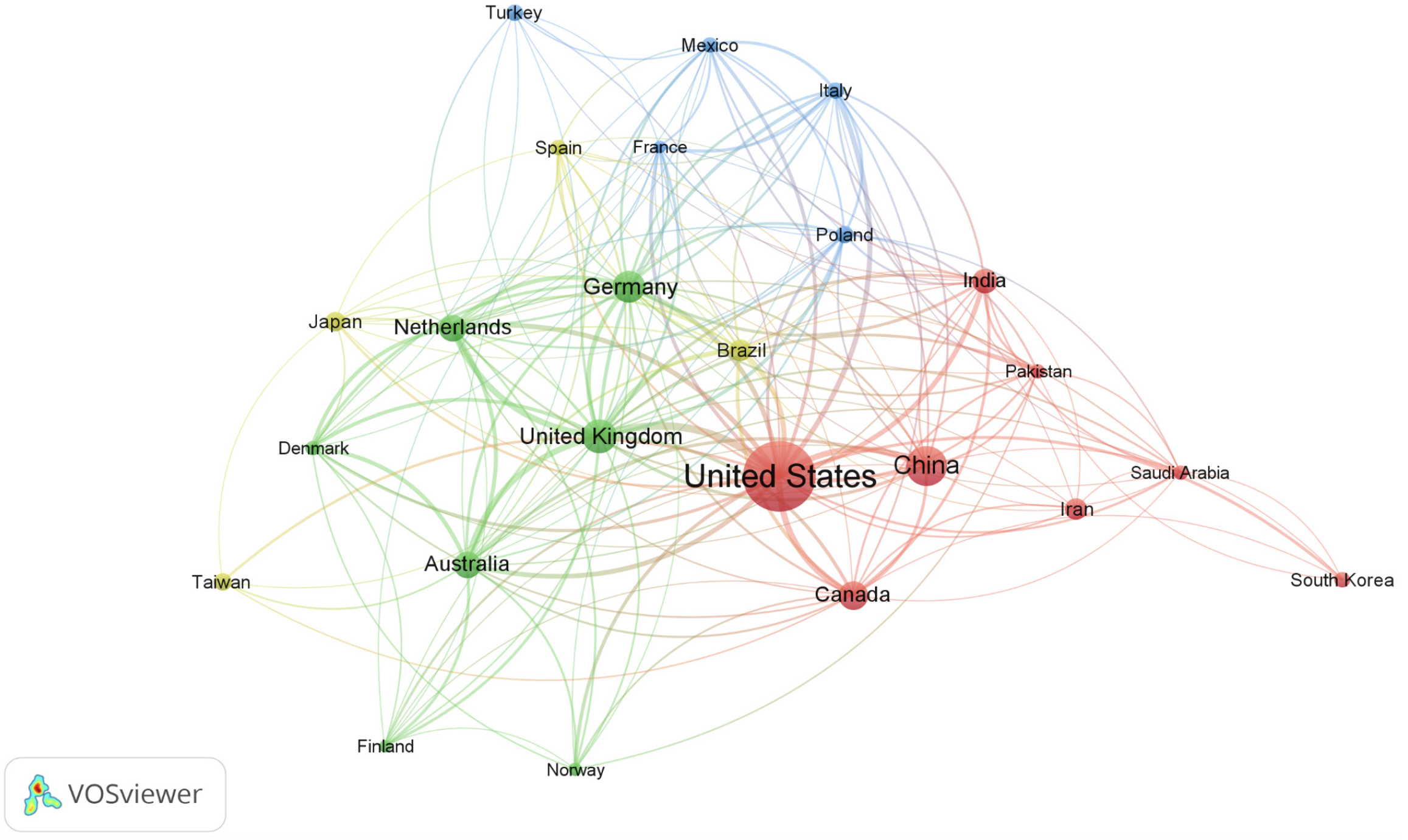
Scientific research on DM and depression has involved the participation of 160 countries. The top 10 countries in this research generated a combined total of 2249 publications, constituting 69.65% of all analyzed publications (Table 1). The findings showed that the USA (n = 1015; 31.43%) was the most productive nation, followed by China (n = 325; 10.07%), the UK (n = 236; 7.31%), and Germany (n = 218; 6.75%). Figure 2 illustrates a network visualization map that depicts research collaborations among 24 countries, each contributing a minimum of 30 articles. The size of the nodes and the thickness of the connecting lines signify the extent of cross-country collaboration, with the USA demonstrating the most robust collaboration.
| Ranking | Country | No. of documents | % |
| 1st | USA | 1015 | 31.43 |
| 2nd | China | 325 | 10.07 |
| 3rd | UK | 236 | 7.31 |
| 4th | Germany | 218 | 6.75 |
| 5th | Canada | 175 | 5.42 |
| 6th | Netherlands | 153 | 4.74 |
| 7th | Australia | 150 | 4.65 |
| 8th | India | 130 | 4.03 |
| 9th | Iran | 102 | 3.16 |
| 10th | Brazil | 98 | 3.03 |
Table 2 presents a comprehensive compilation of the top 10 most productive institutions engaged in research on DM and depression from 2004 to 2023. These distinguished academic and research entities collectively made significant contributions, constituting 12.54% of the total number of published articles (n = 405) within this domain. The University of Washington in the USA showcased its prominence as the foremost contributor, generating 87 articles (2.69%). Tilburg University in Netherlands contributed 63 articles (1.95%), while McGill University in Canada produced 54 articles (1.67%). Notably, the USA had four listed institutions, the Netherlands three, Canada two, and the UK one institution among the top-ranked contributors.
| Ranking | Institute | Country | No. of documents | % |
| 1st | University of Washington | USA | 87 | 2.69 |
| 2nd | Tilburg University | Netherlands | 63 | 1.95 |
| 3rd | Université McGill | Canada | 54 | 1.67 |
| 4th | Universiteit van Amsterdam | Netherlands | 53 | 1.64 |
| 5th | VA Medical Center | USA | 52 | 1.61 |
| 6th | Harvard Medical School | USA | 51 | 1.58 |
| 7th | Amsterdam UMC - Vrije Universiteit Amsterdam | Netherlands | 50 | 1.55 |
| 8th | King's College London | UK | 44 | 1.36 |
| 9th | University of Michigan, Ann Arbor | USA | 43 | 1.33 |
| 10th | Institut Universitaire en Santé Mentale Douglas | Canada | 42 | 1.30 |
A total of 1302 publications, representing 40.32% of the retrieved articles, received financial support. Table 3 lists the top 10 funding agencies associated with publications relevant to DM and depression. These agencies contributed 20.04% (n = 647) of the articles. The National Institute of Diabetes and Digestive and Kidney Diseases in the United States (n = 189; 5.85%) emerged as the foremost funding source, followed by the National Institutes of Health in the USA (n = 153; 4.74%) and the National Institute of Mental Health in the USA (n = 125; 3.87%). The USA featured prominently with five funding agencies on the list, while China, Canada, Germany, Australia, and Brazil each had one agency represented in this list.
| Ranking | Funding agency | Country | No. of documents | % |
| 1st | National Institute of Diabetes and Digestive and Kidney Diseases | USA | 189 | 5.85 |
| 2nd | National Institutes of Health | USA | 153 | 4.74 |
| 3rd | National Institute of Mental Health | USA | 125 | 3.87 |
| 4th | National Natural Science Foundation of China | China | 91 | 2.82 |
| 5th | National Institute on Aging | USA | 70 | 2.17 |
| 6th | Canadian Institutes of Health Research | Canada | 44 | 1.36 |
| 7th | Bundesministerium für Bildung und Forschung | Germany | 31 | 0.96 |
| 7th | National Heart, Lung, and Blood Institute | USA | 31 | 0.96 |
| 9th | National Health and Medical Research Council | Australia | 27 | 0.84 |
| 10th | Conselho Nacional de Desenvolvimento Científico e Tecnológico | Brazil | 26 | 0.81 |
The top 10 most active journals together published 595 articles related to DM and depression, constituting 18.43% of all publications (Table 4). Diabetes Care emerged as the primary contributor, publishing the greatest number of papers (n = 139), accounting for 4.30% of the total publications. Similarly, Diabetic Medicine secured the second position with 96 papers (2.97%), followed by the Journal of Affective Disorders with 67 papers (2.07%) and Diabetes Research and Clinical Practice with 65 papers (2.01%).
| Ranking | Journal | Frequency | % | IF1 |
| 1st | Diabetes Care | 139 | 4.30 | 16.2 |
| 2nd | Diabetic Medicine | 96 | 2.97 | 3.5 |
| 3rd | Journal of Affective Disorders | 67 | 2.07 | 6.6 |
| 4th | Diabetes Research and Clinical Practice | 65 | 2.01 | 5.1 |
| 5th | Journal of Diabetes and Its Complications | 47 | 1.46 | 3.0 |
| 5th | Plos One | 47 | 1.46 | 3.7 |
| 7th | Diabetologia | 35 | 1.08 | 8.2 |
| 8th | Journal of Psychosomatic Research | 34 | 1.05 | 4.7 |
| 9th | General Hospital Psychiatry | 33 | 1.02 | 7.0 |
| 10th | BMC Psychiatry | 32 | 0.99 | 4.4 |
A citation analysis of the retrieved publications revealed an average of 26.74 citations per article. The overall citation impact was further characterized by an h-index of 126 and a total cumulative citation count of 86355. The citation distribution was uneven. While 472 (14.6%) of the articles received no citations, 165 (5.11%) were highly cited, receiving > 100 citations each. The citation counts ranged from 0 to 1179. Table 5 details the top 10 publications associated with DM and depression, which together garnered 7632 citations. These top publications had citation counts ranging from 546 to 1179[49-58].
| Ref. | Title | Year | Source title | Cited by |
| Mezuk et al[54] | Depression and type 2 diabetes over the lifespan: A meta-analysis | 2008 | Diabetes Care | 1179 |
| Ali et al[57] | The prevalence of co-morbid depression in adults with Type 2 diabetes: A systematic review and meta-analysis | 2006 | Diabetic Medicine | 935 |
| Roy and Lloyd[51] | Epidemiology of depression and diabetes: A systematic review | 2012 | Journal of Affective Disorders | 809 |
| Lin et al[55] | Relationship of depression and diabetes self-care, medication adherence, and preventive care | 2004 | Diabetes Care | 795 |
| Knol et al[53] | Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis | 2006 | Diabetologia | 751 |
| Gonzalez et al[56] | Depression and diabetes treatment nonadherence: A meta-analysis | 2008 | Diabetes Care | 743 |
| Golden et al[49] | Examining a bidirectional association between depressive symptoms and diabetes | 2008 | JAMA | 694 |
| Katon et al[58] | The pathways study: A randomized trial of collaborative care in patients with diabetes and depression | 2004 | Archives of General Psychiatry | 609 |
| Bixler et al[50] | Excessive daytime sleepiness in a general population sample: The role of sleep apnea, age, obesity, diabetes, and depression | 2005 | Journal of Clinical Endocrinology and Metabolism | 571 |
| Nouwen et al[52] | Type 2 diabetes mellitus as a risk factor for the onset of depression: A systematic review and meta-analysis | 2010 | Diabetologia | 546 |
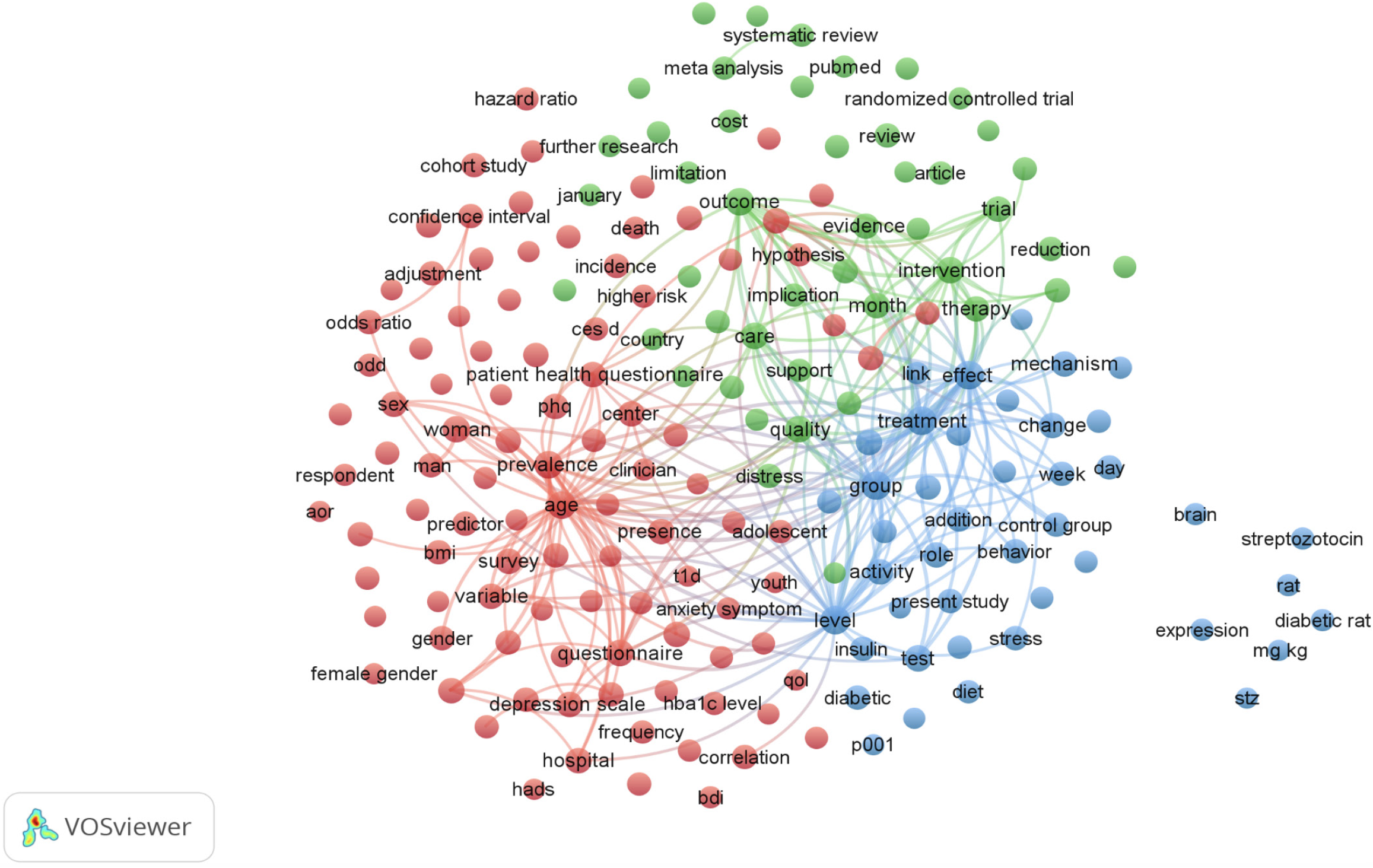
A visualization map based on frequent terms in the retrieved articles revealed three main research themes (Figure 3). The red cluster highlights a focus on understanding how depression and diabetes cooccur, with a growing interest in prevalence and contributing factors. This finding aligns with the emphasis on epidemiology and risk factors observed in this cluster. The green cluster centers on randomized controlled trials (RCTs) investigating how depression hinders diabetes management. These RCTs tested interventions such as psychotherapy, medication, or lifestyle changes to improve depression symptoms in diabetic patients, aiming for better diabetes control. Finally, the blue cluster explores the interplay of risk factors and mechanisms. This research examined how factors such as self-care decline, shared risk factors (obesity, inactivity), and potential biological and social mechanisms influence the two-way relationship between diabetes and depression.
The purpose of this study was to use bibliometric analysis to clarify the trends in research on depression and diabetes from 2004 to 2023. A total of 3229 relevant publications were obtained from Scopus. Subsequently, the bibliometric mapping program VOSviewer was used to show the primary characteristics and general landscape of the field's evolution. The overall publication output during the previous 20 years showed a dynamic trend that peaked in 2023. Additionally, we examined global collaboration, contributions to organizations, financing sources, journal publishing, and citations. Future directions for diabetes and depression research are also considered in the discussion.
The primary causes of the upward trend in the number of articles describing the links between depression and diabetes were as follows. The bidirectional relationship between depression and diabetes is a significant area of research that has contributed to the increasing trend of publications[4,59-62]. Several factors, such as a decrease in self-care, obesity and sedentary lifestyles, which are common risk factors, and the impact of depression on diabetes treatment have been related to depression and diabetes[60,61,63]. The bidirectional relationship between T2DM and depression has prompted interest in understanding the shared molecular processes of hyperglycemia, vascular dysfunction, and low-grade inflammation[8]. Clinical trials with large sample sizes, meta-analyses, and extensive national and cross-country clinical investigations are a few examples of how research methodologies have progressed to support the increase in publications[60]. The conditions of research in this field have been revealed through the use of bibliometric and visual analysis, highlighting popular topics and potential future research directions[64].
We noticed that over time, the countries with the most publications on the links between diabetes and depression were the USA, China, and the UK. The USA had the most citations, field-weighted citation impact, and publications globally concerning endocrinology, diabetes, and metabolism[65]. The USA plays a prominent role in diabetes research and has the most active research facilities and researchers[64]. Diabetes research in China has attracted increasing amounts of attention due to the high prevalence of diabetes worldwide[66,67]. The country has made significant progress in diabetes research, both in terms of volume and publishing effect[68]. Additionally, the UK is significantly adding to the corpus of research in the fields of endocrinology, diabetes, and metabolism[65]. It is one of the countries with the greatest number of publications and citations in this field[65].
Actively studied topics can be identified via term clustering and co-occurrence analysis. Three subjects have been thoroughly researched during the last 20 years. The first cluster emphasizes the growing attention given to the prevalence and contributing factors of the coexistence of depression and diabetes. This result supports the focus on epidemiology and risk factors that this cluster identified. RCTs examining how depression affects diabetes management made up the second cluster. These RCTs aimed for better diabetes control and assessed treatments, including psychotherapy, medication, or lifestyle modifications, for minimizing depression symptoms in diabetic patients. The third cluster investigated how risk factors and mechanisms interact. The present study investigated the possible biological and social mechanisms affecting the two-way relationship between diabetes and depression, as well as shared risk factors (obesity and inactivity).
The co-occurrence of depression and diabetes is an important issue, and there is increasing interest in their prevalence and contributing risk factors. There is evidence pointing to common biological processes between T2D and depression, and depression is twice as common in those with this disease as in the general public[8,60]. In those with T2DM, comorbid conditions, dysglycemia, gender, anxiety, educational level, socioeconomic status, and pharmaceutical treatments are among the factors that contribute to the onset of cognitive impairments, depression, and psychosocial problems[69]. Lifestyle decisions and social factors are important co-occurrence predictors, as are behavioral indicators, life outcomes, and demographic characteristics[70,71].
Another area attracting much interest is RCTs that look at how depression affects diabetes management. Cognitive behavioral therapy (CBT) helps people with T2DM better manage their depressive symptoms and diabetes[72-78]. CBT has been shown to improve glycemic control, quality of life, and self-care behavior in people with T2DM and to greatly decrease depressive symptoms and diabetes-related distress[73-75,77,78]. In adults with type 1 DM (T1DM) or T2DM, CBT-based therapies have been shown to improve glycemic control and depression symptoms in numerous RCTs[74,76-78]. Treatments such as CBT have been demonstrated in RCTs to lower both diabetes control and depressive symptoms, confirming the reciprocal relationship between depression and diabetes[72-78]. Researchers have investigated the longitudinal relationships between depression and diabetes regimen distress (RD) through RCTs. The results show a covarying link in which changes in RD and depression symptoms occur together over time[79]. RCTs have shown that CBT improves depressive symptoms, anxiety, stress associated with diabetes, glycemic control, quality of life, and self-care behavior in patients with T1DM or T2DM, advancing our knowledge of the possible advantages of CBT in diabetes[75-78]. We should exercise caution when interpreting RCT findings due to the heterogeneity in CBT delivery methods, follow-up duration, outcomes, and long-term effects[73,75]. Considering the great variety of included studies and other limitations, more studies with a large number of studies are necessary to validate the findings[74]. The feasibility and efficacy of collaborative care models for depression in diabetes patients in low- and middle-income countries are yet unknown, which emphasizes the need for ethical issues while carrying out RCTs in various geographic locations[80]. A multicenter single-blind RCT emphasized the need for ethical issues when carrying out RCTs on comorbid depression and diabetes in diverse populations[80]. Its goal is to determine the efficacy of fluoxetine and mindfulness in primary care settings.
Researchers are currently investigating potential biological and social factors that influence the inverse relationship between diabetes and depression. Numerous studies have demonstrated a bidirectional relationship between diabetes and depression, influenced by both biological and social factors. Biological processes such as hyperglycemia, vascular dysfunction, and inflammation are linked to T2D and depression, with depression being twice as common in T2D patients as in the general population[8,81]. It is possible that inflammation, sleep problems, a sedentary lifestyle, poor eating habits, and activation of the HPA axis are at the root of both disorders[81]. The somatic-affective aspect of depression primarily links diabetes and depression, and the use of somatic health care independently links both disorders[82,83]. Common biological and behavioral processes, such as inflammation, autonomic dysfunction, sleep disturbance, an inactive lifestyle, poor eating habits, environmental and cultural risk factors, and activation of the HPA axis, are linked to depression and diabetes[7].
Future research directions for exploring the links between diabetes and depression are likely to focus on mechanistic studies to understand the molecular mechanisms underlying the bidirectional relationship[59]. To determine whether treating patients with comorbid conditions will enhance their quality of life and medical outcomes, lengthy, outcome-oriented RCTs are required[60]. Future research should focus on identifying promising preventive interventions and creating creative, cost-effective interventions to prevent depression, T2DM, and cardiovascular diseases[84].
This innovative study established the first baseline data on research activities investigating the link between DM and depression. However, some limitations are important to consider. First, relying solely on Scopus for document retrieval may have excluded relevant publications from local, unindexed journals. While Scopus is a vast database, numerous health-related publications, particularly from non-English-speaking countries, might not be indexed. This can introduce bias toward countries with well-represented journals or English-language publications, potentially underestimating overall research productivity. Second, the analysis was restricted to publications retrieved from Scopus, potentially limiting its comprehensiveness. However, Scopus remains the most accessible database for analyzing research activity and identifying hotspots on specific topics. Finally, the search terms were confined to "DM and depression" and related terms within titles only. This approach might have missed relevant publications that used these terms as keywords or within the body of the text.
This study examined the development, patterns, and areas of inquiry related to depression in diabetes patients. An examination of 3229 publications released between 2004 and 2023 revealed a significant increase in research efforts during the previous 20 years, highlighting the significance of treating this common psychological disorder in individuals with diabetes. Due to their substantial contributions to diabetes research and the significant influence of their publications in the field, the USA, China, and the UK emerged as the top three countries with the highest volume of publications regarding the relationship between depression and diabetes. The analysis delineated three principal themes in research on depression and diabetes: (1) Exploring the elevated prevalence and etiology of this comorbidity; (2) focusing on interventions, particularly RCTs, aimed at enhancing diabetes management among individuals with depression; and (3) investigating the involved risk factors and biological mechanisms underlying this bidirectional relationship. This research sheds light on the growing recognition of the influence of depression on treatment adherence and health outcomes within this demographic group. This study has contributed to advancing knowledge in this field by charting a course for future research on depression treatments for individuals with diabetes.
The author thanks An-Najah National University for all its administrative assistance during the implementation of the project. In addition, the author thanks Dr. Waleed Sweileh and Dr. Sa’ed H Zyoud for helping and validating the research strategy.
| 1. | Torzsa P, Hargittay C, Torzsa G, Tripolszky B, Rihmer Z, Gonda X. A 2-es típusú cukorbetegség kapcsolata a szorongásos és az affektív zavarokkal. LAM. 2023;33:339-345. [DOI] [Full Text] |
| 2. | Tabák AG, Akbaraly TN, Batty GD, Kivimäki M. Depression and type 2 diabetes: a causal association? Lancet Diabetes Endocrinol. 2014;2:236-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 122] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 3. | Oladeji BD, Gureje O. The comorbidity between depression and diabetes. Curr Psychiatry Rep. 2013;15:390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Manigault KR. The bidirectional relationship between depression & diabetes. US Pharm. 2016;41:26-29. |
| 5. | Endomba FT, Guillaume M, Lemogne C, Chauvet-Gélinier J. Mise au point sur les liens entre diabète et dépression. Médecine des Maladies Métaboliques. 2024;18:204-213. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Kreider KE. Diabetes Distress or Major Depressive Disorder? A Practical Approach to Diagnosing and Treating Psychological Comorbidities of Diabetes. Diabetes Ther. 2017;8:1-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 7. | Holt RI, de Groot M, Lucki I, Hunter CM, Sartorius N, Golden SH. NIDDK international conference report on diabetes and depression: current understanding and future directions. Diabetes Care. 2014;37:2067-2077. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 103] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | van Sloten T, Schram M. Understanding depression in type 2 diabetes: a biological approach in observational studies. F1000Res. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Siddiqui S. Depression in type 2 diabetes mellitus--a brief review. Diabetes Metab Syndr. 2014;8:62-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Mukherjee N, Chaturvedi SK. Depressive symptoms and disorders in type 2 diabetes mellitus. Curr Opin Psychiatry. 2019;32:416-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 11. | Ellegaard O, Wallin JA. The bibliometric analysis of scholarly production: How great is the impact? Scientometrics. 2015;105:1809-1831. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1309] [Cited by in RCA: 773] [Article Influence: 77.3] [Reference Citation Analysis (0)] |
| 12. | Thompson DF, Walker CK. A descriptive and historical review of bibliometrics with applications to medical sciences. Pharmacotherapy. 2015;35:551-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 243] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 13. | Sweileh WM, Wickramage K, Pottie K, Hui C, Roberts B, Sawalha AF, Zyoud SH. Bibliometric analysis of global migration health research in peer-reviewed literature (2000-2016). BMC Public Health. 2018;18:777. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 114] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 14. | Møller AM, Myles PS. What makes a good systematic review and meta-analysis? Br J Anaesth. 2016;117:428-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 15. | Chen H, Wei F, Chen X, Chen K. Global Research Trends in Gestational Diabetes Mellitus from 2000 to 2020: A Bibliometric Study. Z Geburtshilfe Neonatol. 2022;226:197-204. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Cheng K, Guo Q, Yang W, Wang Y, Sun Z, Wu H. Mapping Knowledge Landscapes and Emerging Trends of the Links Between Bone Metabolism and Diabetes Mellitus: A Bibliometric Analysis From 2000 to 2021. Front Public Health. 2022;10:918483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 69] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 17. | Jiang C, Hu Y, Wang S, Chen C. Emerging trends in DNA and RNA methylation modifications in type 2 diabetes mellitus: a bibliometric and visual analysis from 1992 to 2022. Front Endocrinol (Lausanne). 2023;14:1145067. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Kong L, Deng B, Guo M, Chen M, Wang X, Zhang M, Tang H, Wang Q, Yang L, Xiong Z. A systematic bibliometric analysis on the clinical practice of CGM in diabetes mellitus from 2012 to 2022. Front Endocrinol (Lausanne). 2023;14:1229494. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Li X, Su X, Xia F, Qiu J, Zhang J, Wu H, Xie X, Xu M. Bibliometric and visual analysis of diabetes mellitus and pyroptosis from 2011 to 2022. Eur J Med Res. 2023;28:235. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 20. | Li Y, Peng L, Gu W. The published trend of studies on COVID-19 and diabetes: bibliometric analysis. Front Endocrinol (Lausanne). 2023;14:1248676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 21. | Yuan K, Zhang X, Wu B, Zeng R, Hu R, Wang C. Research trends between diabetes mellitus and bariatric surgery researches: Bibliometric analysis and visualization from 1998 to 2023. Obes Rev. 2024;25:e13730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 22. | Zhang L, Bao B, Guo J, Qin Z, Huang H, Chen L, Liu B. Current status and prospects of diabetes mellitus induced erectile dysfunction: A bibliometric and visualization study. Front Endocrinol (Lausanne). 2023;14:1168744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 23. | Zhang W, Zhang S, Dong C, Guo S, Jia W, Jiang Y, Wang C, Zhou M, Gong Y. A bibliometric analysis of RNA methylation in diabetes mellitus and its complications from 2002 to 2022. Front Endocrinol (Lausanne). 2022;13:997034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Chen L, Ren T, Tan Y, Li H. Global trends of research on depression in breast cancer: A bibliometric study based on VOSviewer. Front Psychol. 2022;13:969679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 25. | He T, Wu Z, Zhang X, Liu H, Wang Y, Jiang R, Liu C, Hashimoto K, Yang C. A Bibliometric Analysis of Research on the Role of BDNF in Depression and Treatment. Biomolecules. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 26. | Jingili N, Oyelere SS, Ojwang F, Agbo FJ, Nyström MBT. Virtual Reality for Addressing Depression and Anxiety: A Bibliometric Analysis. Int J Environ Res Public Health. 2023;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 27. | Li KL, Chen YM, Wang XQ, Hu HY. Bibliometric Analysis of Studies on Neuropathic Pain Associated With Depression or Anxiety Published From 2000 to 2020. Front Hum Neurosci. 2021;15:729587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 28. | Ying H, Zhang X, He T, Feng Q, Wang R, Yang L, Duan J. A bibliometric analysis of research on heart failure comorbid with depression from 2002 to 2021. Heliyon. 2023;9:e13054. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 29. | Al-Jabi SW. Current global research landscape on COVID-19 and depressive disorders: Bibliometric and visualization analysis. World J Psychiatry. 2021;11:253-264. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 24] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 30. | Al-Jabi SW. Global research trends and mapping knowledge structure of depression in dialysis patients. World J Psychiatry. 2023;13:593-606. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Reference Citation Analysis (0)] |
| 31. | Zyoud SH, Shakhshir M, Abushanab AS, Koni A, Shahwan M, Jairoun AA, Al-Jabi SW. Bibliometric mapping of the landscape and structure of nutrition and depression research: visualization analysis. J Health Popul Nutr. 2023;42:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 32. | Baas J, Schotten M, Plume A, Côté G, Karimi R. Scopus as a curated, high-quality bibliometric data source for academic research in quantitative science studies. Quant Sci Stud. 2020;1:377-386. [RCA] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 188] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 33. | Bakhmat N, Kolosova O, Demchenko O, Ivashchenko I, Strelchuk V. Application of international scientometric databases in the process of training competitive research and teaching staff: Opportunities of Web of Science (WoS), Scopus, Google Scholar. J Theor Appl Inf Technol. 2022;100:4914-4924. |
| 34. | Martín-Martín A, Thelwall M, Orduna-Malea E, Delgado López-Cózar E. Google Scholar, Microsoft Academic, Scopus, Dimensions, Web of Science, and OpenCitations' COCI: a multidisciplinary comparison of coverage via citations. Scientometrics. 2021;126:871-906. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 435] [Cited by in RCA: 199] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 35. | Mongeon P, Paul-Hus A. The journal coverage of Web of Science and Scopus: A comparative analysis. Scientometrics. 2016;106:213-228. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1180] [Cited by in RCA: 825] [Article Influence: 82.5] [Reference Citation Analysis (0)] |
| 36. | Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2579] [Cited by in RCA: 2562] [Article Influence: 106.8] [Reference Citation Analysis (0)] |
| 37. | Arsh A, Afaq S, Carswell C, Bhatti MM, Ullah I, Siddiqi N. Effectiveness of physical activity in managing co-morbid depression in adults with type 2 diabetes mellitus: A systematic review and meta-analysis. J Affect Disord. 2023;329:448-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 38. | Buchberger B, Huppertz H, Krabbe L, Lux B, Mattivi JT, Siafarikas A. Symptoms of depression and anxiety in youth with type 1 diabetes: A systematic review and meta-analysis. Psychoneuroendocrinology. 2016;70:70-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 299] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 39. | Chow YY, Verdonschot M, McEvoy CT, Peeters G. Associations between depression and cognition, mild cognitive impairment and dementia in persons with diabetes mellitus: A systematic review and meta-analysis. Diabetes Res Clin Pract. 2022;185:109227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 46] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 40. | Huang Y, Wei X, Wu T, Chen R, Guo A. Collaborative care for patients with depression and diabetes mellitus: a systematic review and meta-analysis. BMC Psychiatry. 2013;13:260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 116] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 41. | Tegegne KD, Gebeyehu NA, Kassaw MW. Depression and determinants among diabetes mellitus patients in Ethiopia, a systematic review and meta-analysis. BMC Psychiatry. 2023;23:209. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 42. | van der Feltz-Cornelis C, Allen SF, Holt RIG, Roberts R, Nouwen A, Sartorius N. Treatment for comorbid depressive disorder or subthreshold depression in diabetes mellitus: Systematic review and meta-analysis. Brain Behav. 2021;11:e01981. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 63] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 43. | van Dooren FE, Nefs G, Schram MT, Verhey FR, Denollet J, Pouwer F. Depression and risk of mortality in people with diabetes mellitus: a systematic review and meta-analysis. PLoS One. 2013;8:e57058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 243] [Cited by in RCA: 293] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 44. | Sweileh WM. Global research activity on antimicrobial resistance in food-producing animals. Arch Public Health. 2021;79:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 45. | Sweileh WM. Health-related publications on people living in fragile states in the alert zone: a bibliometric analysis. Int J Ment Health Syst. 2020;14:70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 46. | Zyoud SH, Shakhshir M, Abushanab AS, Koni A, Shahwan M, Jairoun AA, Al-jabi SW. Global research trends on the links between insulin resistance and obesity: A visualization analysis. Transl Med Commun. 2022;7:18. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 47. | Arruda H, Silva ER, Lessa M, Proença D Jr, Bartholo R. VOSviewer and Bibliometrix. J Med Libr Assoc. 2022;110:392-395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 176] [Reference Citation Analysis (0)] |
| 48. | van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4505] [Cited by in RCA: 5142] [Article Influence: 321.4] [Reference Citation Analysis (0)] |
| 49. | Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Diez Roux AV, Lee HB, Lyketsos C. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751-2759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 676] [Cited by in RCA: 630] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 50. | Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A. Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab. 2005;90:4510-4515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 484] [Cited by in RCA: 491] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 51. | Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142 Suppl:S8-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 881] [Cited by in RCA: 770] [Article Influence: 59.2] [Reference Citation Analysis (0)] |
| 52. | Nouwen A, Winkley K, Twisk J, Lloyd CE, Peyrot M, Ismail K, Pouwer F; European Depression in Diabetes (EDID) Research Consortium. Type 2 diabetes mellitus as a risk factor for the onset of depression: a systematic review and meta-analysis. Diabetologia. 2010;53:2480-2486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 558] [Cited by in RCA: 510] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 53. | Knol MJ, Twisk JW, Beekman AT, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49:837-845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 632] [Cited by in RCA: 619] [Article Influence: 32.6] [Reference Citation Analysis (0)] |
| 54. | Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. 2008;31:2383-2390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1207] [Cited by in RCA: 1077] [Article Influence: 63.4] [Reference Citation Analysis (0)] |
| 55. | Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, Ciechanowski P, Ludman EJ, Bush T, Young B. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27:2154-2160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 685] [Cited by in RCA: 697] [Article Influence: 33.2] [Reference Citation Analysis (0)] |
| 56. | Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, Safren SA. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. 2008;31:2398-2403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 627] [Cited by in RCA: 697] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 57. | Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2006;23:1165-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 824] [Cited by in RCA: 830] [Article Influence: 43.7] [Reference Citation Analysis (0)] |
| 58. | Katon WJ, Von Korff M, Lin EH, Simon G, Ludman E, Russo J, Ciechanowski P, Walker E, Bush T. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry. 2004;61:1042-1049. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 522] [Cited by in RCA: 481] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 59. | Zhuang QS, Shen L, Ji HF. Quantitative assessment of the bidirectional relationships between diabetes and depression. Oncotarget. 2017;8:23389-23400. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 60. | Alzoubi A, Abunaser R, Khassawneh A, Alfaqih M, Khasawneh A, Abdo N. The Bidirectional Relationship between Diabetes and Depression: A Literature Review. Korean J Fam Med. 2018;39:137-146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 62] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 61. | Adriaanse M, Pouwer F. Diabetes, Depression, and Cardiovascular Risk. In: Alvarenga M, Byrne D, editors. Handbook of Psychocardiology. Singapore: Springer, 2015: 831-847. [DOI] [Full Text] |
| 62. | Yu M, Zhang X, Lu F, Fang L. Depression and Risk for Diabetes: A Meta-Analysis. Can J Diabetes. 2015;39:266-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 168] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 63. | Granon B, Leroy A. Depression and diabetes. Correspondances en MHND. 2023;27:178-181. |
| 64. | Zou X, Sun Y. Bibliometrics Analysis of the Research Status and Trends of the Association Between Depression and Insulin From 2010 to 2020. Front Psychiatry. 2021;12:683474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 65. | Hassan W, Duarte AE, Kamdem JP, da Rocha JBT. Bibliometric analysis of endocrinology, diabetes and metabolism research in South Asia from (2012-2021): Comparison with five developed countries. Diabetes Metab Syndr. 2023;17:102760. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 66. | Chan JCN, Chow EYK, Luk AOY. Diabetes in China and the Western Pacific Region. In: Dagogo-Jack S, editor. Diabetes Mellitus in Developing Countries and Underserved Communities. Cham: Springer, 2017: 63-83. [DOI] [Full Text] |
| 67. | Zhao X, Guo L, Yuan M, He X, Lin Y, Gu C, Li Q, Zhao L, Tong X. Growing Trend of China's Contribution to Global Diabetes Research: A Systematic Literature Review. Medicine (Baltimore). 2016;95:e3517. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 68. | Wu Z, Jin T, Weng J. A thorough analysis of diabetes research in China from 1995 to 2015: current scenario and future scope. Sci China Life Sci. 2019;62:46-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 69. | Randväli M, Toomsoo T, Šteinmiller J. The Main Risk Factors in Type 2 Diabetes for Cognitive Dysfunction, Depression, and Psychosocial Problems: A Systematic Review. Diabetology. 2024;5:40-59. [DOI] [Full Text] |
| 70. | Alva ML. Co-occurrence of diabetes and depression in the U.S. PLoS One. 2020;15:e0234718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 71. | Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, Thornton PL, Haire-Joshu D. Social Determinants of Health and Diabetes: A Scientific Review. Diabetes Care. 2020;44:258-279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 750] [Cited by in RCA: 899] [Article Influence: 179.8] [Reference Citation Analysis (0)] |
| 72. | Mansour N, Labib N, Khalil M, Esmat S. Brief Cognitive Behavioral Therapy for Patients with Comorbid Depression and Type 2 Diabetes in an Urban Primary Care Facility: Randomized Controlled Trial. Open Access Maced J Med Sci. 2022;10:60-67. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 73. | Vlachou E, Ntikoudi A, Owens DA, Nikolakopoulou M, Chalimourdas T, Cauli O. Effectiveness of cognitive behavioral therapy-based interventions on psychological symptoms in adults with type 2 diabetes mellitus: An update review of randomized controlled trials. J Diabetes Complications. 2022;36:108185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 74. | Yang X, Li Z, Sun J. Effects of Cognitive Behavioral Therapy-Based Intervention on Improving Glycaemic, Psychological, and Physiological Outcomes in Adult Patients With Diabetes Mellitus: A Meta-Analysis of Randomized Controlled Trials. Front Psychiatry. 2020;11:711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 75. | Sukarno A, Bahtiar MN. The Effectiveness of Cognitive Behavior Therapy on Psychological Stress, Physical Health, and Self-Care Behavior among Diabetes Patients: A Systematic Review. Health Educ Health Promot. 2022;10:531-537. |
| 76. | Li Y, Storch EA, Ferguson S, Li L, Buys N, Sun J. The efficacy of cognitive behavioral therapy-based intervention on patients with diabetes: A meta-analysis. Diabetes Res Clin Pract. 2022;189:109965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 77. | Li C, Xu D, Hu M, Tan Y, Zhang P, Li G, Chen L. A systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy for patients with diabetes and depression. J Psychosom Res. 2017;95:44-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 78. | Jenkinson E, Knoop I, Hudson JL, Moss-Morris R, Hackett RA. The effectiveness of cognitive behavioural therapy and third-wave cognitive behavioural interventions on diabetes-related distress: A systematic review and meta-analysis. Diabet Med. 2022;39:e14948. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 79. | Hessler D, Fisher L, Strycker LA, Arean PA, Bowyer V. Causal and bidirectional linkages over time between depression and diabetes regimen distress in adults with type 2 diabetes. Diabetes Res Clin Pract. 2015;108:360-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 80. | Chandra M, Raveendranathan D, Johnson Pradeep R, Patra S, Rushi, Prasad K, Brar JS. Managing Depression in Diabetes Mellitus: A Multicentric Randomized Controlled Trial Comparing Effectiveness of Fluoxetine and Mindfulness in Primary Care: Protocol for DIAbetes Mellitus ANd Depression (DIAMAND) Study. Indian J Psychol Med. 2020;42:S31-S38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 81. | Holt RI, de Groot M, Golden SH. Diabetes and depression. Curr Diab Rep. 2014;14:491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 283] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 82. | Wiltink J, Michal M, Wild PS, Schneider A, König J, Blettner M, Münzel T, Schulz A, Weber M, Fottner C, Pfeiffer N, Lackner K, Beutel ME. Associations between depression and diabetes in the community: do symptom dimensions matter? Results from the Gutenberg Health Study. PLoS One. 2014;9:e105499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 83. | Mayberry LS, Nelson LA, Gonzalez JS. Adults with type 2 diabetes benefit from self-management support intervention regardless of depressive symptoms. J Diabetes Complications. 2021;35:108024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 84. | Bădescu SV, Tătaru C, Kobylinska L, Georgescu EL, Zahiu DM, Zăgrean AM, Zăgrean L. The association between Diabetes mellitus and Depression. J Med Life. 2016;9:120-125. |