Published online Jul 19, 2024. doi: 10.5498/wjp.v14.i7.1053
Revised: June 7, 2024
Accepted: June 14, 2024
Published online: July 19, 2024
Processing time: 65 Days and 19.9 Hours
Having a gynecological tumor or undergoing treatment can be a traumatic experience for women, as it affects their self-image and sexual relationships and can lead to psychological reactions. Psychological adjustment following cancer occurrence remains a key issue among the survivors.
To examine the current status of quality of life (QoL), anxiety, and depression in patients with gynecological cancer and to analyze the factors associated with it.
Data for 160 patients with gynecological malignancies treated at Shanxi Bethune Hospital from June 2020 to June 2023 were collected and analyzed retrospectively. Patients’ QoL was assessed using the European Organization for Research on Treatment of Cancer Quality of Life Questionnaire Core 30 and the Functional Assessment of Cancer Therapy-General Questionnaire. Their emotional status was evaluated using the Self-Rating Anxiety/Depression Scale. The associated factors of anxiety and depression were analyzed.
The overall QoL score of the patients 6 months after surgery was 76.39 ± 3.63 points. This included low levels of social and emotional function and severe fatigue and pain. The scores for physiological, functional, emotional, social, and family well-being exhibited an upward trend following surgery compared with those before surgery. One month after surgery, some patients experienced anxiety and depression, with an incidence of 18.75% and 18.13%, respectively. Logistic analysis revealed that good sleep was a protective factor against anxiety and depression in patients with gynecological tumors, whereas physical pain was a risk factor.
Patients with gynecological malignancies often experience anxiety and depression. By analyzing the factors that affect patients’ QoL, effective nursing measures can be administered.
Core Tip: Patients diagnosed with cancer experience various emotions. Up to now, numerous papers exploring the association and risk factors between various types of cancer and depressive/anxiety episodes have been published. However, the results of these studies remain inconsistent. The aim of this study was to evaluate the relationship between depression and anxiety mood in gynecological cancer and its risk factors.
- Citation: Shang HX, Ning WT, Sun JF, Guo N, Guo X, Zhang JN, Yu HX, Wu SH. Investigation of the quality of life, mental status in patients with gynecological cancer and its influencing factors. World J Psychiatry 2024; 14(7): 1053-1061
- URL: https://www.wjgnet.com/2220-3206/full/v14/i7/1053.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i7.1053
Gynecological malignancies are crucial as they affect the lives and health of women, accounting for 14.4% of new cancer cases among women worldwide[1]. The common types are cervical, ovarian, endometrial, and vaginal cancers[2-5], each of which has a specific symptom burden on the survivor’s quality of life (QoL). Over the past few decades, the average life expectancy of patients with gynecologic cancers has increased with the continued development and adoption of interdisciplinary and interprofessional care in clinical practice[6]. Because of the specific location of gynecologic malignancies, surgery usually involves pelvic organ dissection, which results in greater mental stress and psychological pain in these patients compared with patients with other cancer types. This is in addition to the harm and adverse effects caused by surgery and chemoradiotherapy common to all cancer patients[7,8]. Treatment also affects the self-efficacy, QoL, and physical function of cancer patients[9]. Even after treatment, cancer survivors face various difficulties and challenges that affect their QoL, a term that describes the alteration and enhancement of life attributes.
Symptoms such as anxiety, depression, and fatigue are common in all cancer patients[10]. In addition to physical symptoms, patients often struggle with psychological problems[11]. In addition, cancer patients often lack confidence or the ability to effectively manage life after receiving cancer treatment; thus, more information is needed. These cancer-related sequelae may significantly compromise mental health and QoL. Anxiety and depression are a direct threat to the physical and mental health of patients, are very common in clinical practice, and are a major cause of death[12]. Depression and anxiety are more common in patients with cancer than in people without chronic medical conditions; however, the prevalence varies widely[13]. Among patients with cancer, the estimated prevalence of depression is 11%-57%, whereas that of anxiety is 6.5%-23%[14]. Therefore, examining the anxiety and depression status of patients with gynecological cancer and analyzing the influencing factors will be useful for targeted intervention in patients who experience anxiety and depression in clinical practice, avoiding or reducing further physical and mental health damage caused by anxiety or depression, improving patients’ QoL, and prolonging their lives.
Patients with gynecological malignancies admitted to Shanxi Bethune Hospital between June 2020 and June 2023 were enrolled as the research subjects for this retrospective analysis. The inclusion criteria were as follows: (1) Definite diagnosis of a gynecological malignancy; (2) Age > 18 years; (3) Expected survival > 6 months; (4) Karnofsky Performance Status score ≥ 60; (5) Certain cognitive level with no language communication barriers; and (6) Complete clinical data. The exclusion criteria were as follows: (1) Cancer concomitant with other major diseases; (2) Recent major traumatic or life events; (3) Serious mental disorders; and (4) Incomplete clinical data. Of the 171 questionnaires distributed, 160 valid ones were recovered, with a questionnaire recovery rate of 93.6%.
The survey was conducted in the gynecology ward by uniformly trained investigators in the form of face-to-face interviews.
General information questionnaire: The questionnaire was designed by the researcher and patient clinical data were collected, including age, tumor type, ethnicity, education level, annual household income, marital status, number of children born, and working status.
QoL: This survey was conducted on week 1 as well as 1-, 3-, and 6-months after surgery. The European Organization for Research and Treatment on Cancer (EORTC) Quality of Life Questionnaire Core 30 (QLQ-C30) and the Functional Assessment of Cancer Therapy-General Questionnaire (FACT-G) were used to assess QoL. The QLQ-C30 consists of 30 items covering five functional dimensions (physical, role, emotional, cognitive, and social functioning), three symptom dimensions (fatigue, nausea and vomiting, and pain), one global health status, and six single-item measures (dyspnea, insomnia, appetite loss, constipation, diarrhea, and financial problems). Except for global health status, which was measured on a 7-point Likert scale, the items were graded on a 4-point Likert scale. The final score was linearly transformed, with a total score of 0-100 for each category. The higher the score in the functional and global health status dimensions, the better the QoL. Scores for symptom dimensions and single-item measures are inversely associated with QoL. The FACT-G scale is usually used to measure the QoL of ordinary cancer patients, with a total of 27 items from the following four dimensions: Physical (7 items), social/family (7 items), emotional (6 items), and functional well-being (7 items). Each item is graded on a scale of 0-4, with 0 being not at all, 1 being a little bit, 2 being somewhat, 3 being quite a bit, and 4 being very much. Based on the scoring method of the scale, the four dimensions and the total score are calculated and the total score range is 0-108 points. A higher score suggests better QoL for the research subject.
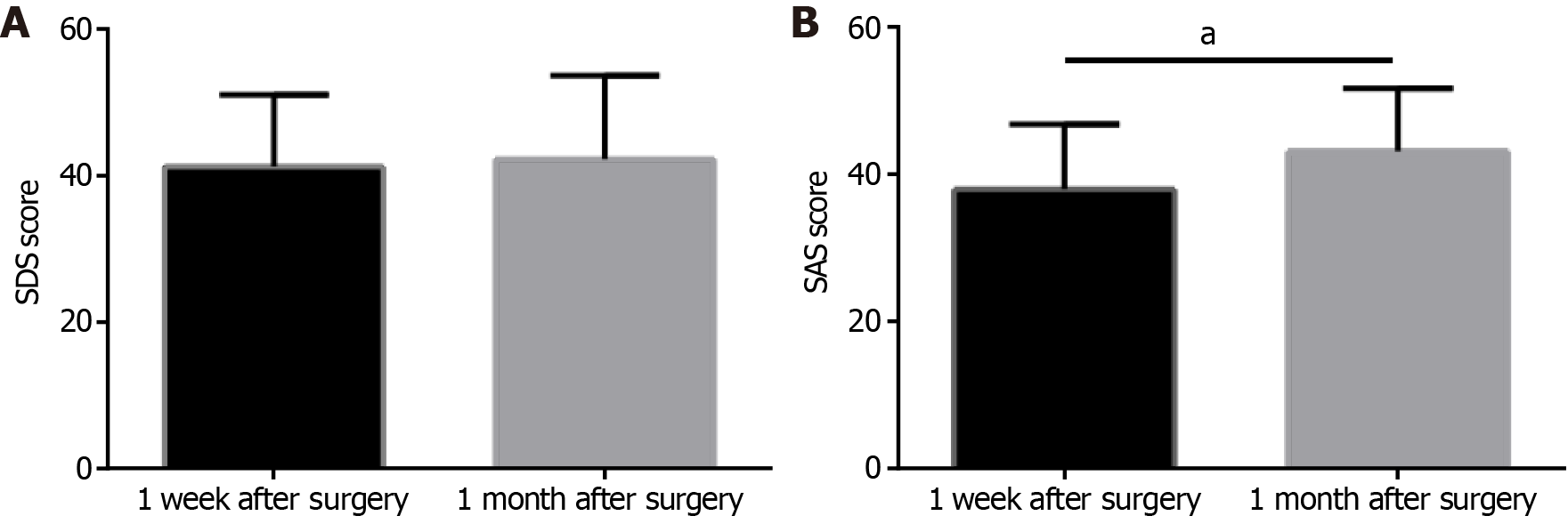
Depression and anxiety: Depression and anxiety in the patients were assessed on week 1 and 6-months after surgery using the self-rating depression scale (SDS) and self-rating anxiety scale (SAS), respectively. Based on the results using Chinese norms, an SDS score of > 53 is considered depression and an SAS score > 50 indicates anxiety, with higher scores of both representing a higher level of anxiety or depression.
SPSS 25.0 was used to analyze the data. Continuous variables (mean ± SD) were comparatively analyzed between groups using a t-test and among groups using one-way analysis of variance. The counting data were expressed as percentages, and the χ2 test was used. Based on univariate analysis, multivariate logistic regression was used to analyze the influencing factors of anxiety and depression. Tests were two-tailed with P < 0.05 indicating statistical significance.
Compared with the indicators before surgery, the scores of physical, role, emotional, cognitive, and social functioning of postsurgical patients with gynecological cancer exhibited an overall increasing trend (mean global health status: 76.39 ± 3.63 points), of which the level of social and emotional functioning was low. For symptom dimensions, pain had the highest score (26.25 ± 6.46 points), followed by insomnia (21.83 ± 4.95 points) and fatigue (21.44 ± 2.73 points). Meanwhile, the score for financial problems was also high (Table 1).
| n = 160 | 1 week after surgery | 1 month after surgery | 3 months after surgery | 6 months after surgery | F | P value |
| Physical functioning | 80.31 ± 4.28 | 84.14 ± 4.52 | 87.04 ± 4.05 | 89.96 ± 5.16 | 133.0 | < 0.0001 |
| Role functioning | 81.77 ± 5.20 | 83.73 ± 4.61 | 86.72 ± 6.34 | 89.84 ± 4.50 | 73.25 | < 0.0001 |
| Emotional functioning | 65.59 ± 4.01 | 68.17 ± 4.27 | 70.61 ± 7.34 | 73.99 ± 7.14 | 58.90 | < 0.0001 |
| Cognitive functioning | 83.87 ± 6.09 | 86.53 ± 5.06 | 87.91 ± 4.68 | 88.74 ± 5.09 | 26.39 | < 0.0001 |
| Social functioning | 64.09 ± 3.77 | 66.20 ± 5.74 | 69.39 ± 2.16 | 70.38 ± 3.60 | 82.90 | < 0.0001 |
| Global health status | 65.49 ± 5.75 | 69.01 ± 4.70 | 72.33 ± 3.37 | 76.39 ± 3.63 | 174.0 | < 0.0001 |
| Fatigue | 18.71 ± 1.17 | 19.58 ± 1.46 | 20.61 ± 2.33 | 21.44 ± 2.73 | 55.82 | < 0.0001 |
| Nausea and vomiting | 10.17 ± 1.94 | 10.13 ± 1.83 | 8.94 ± 1.68 | 7.44 ± 1.27 | 91.87 | < 0.0001 |
| Pain | 23.36 ± 3.55 | 24.38 ± 5.01 | 25.30 ± 3.05 | 26.25 ± 6.46 | 11.02 | < 0.0001 |
| Dyspnea | 8.28 ± 1.03 | 7.97 ± 1.14 | 7.46 ± 0.93 | 6.82 ± 1.09 | 59.47 | < 0.0001 |
| Insomnia | 19.89 ± 3.82 | 21.40 ± 4.43 | 21.81 ± 4.17 | 21.83 ± 4.95 | 7.033 | 0.0001 |
| Appetite loss | 6.33 ± 1.17 | 6.18 ± 1.12 | 5.44 ± 0.81 | 5.64 ± 1.04 | 26.43 | < 0.0001 |
| Constipation | 4.50 ± 0.56 | 4.78 ± 0.47 | 4.25 ± 0.58 | 4.16 ± 0.84 | 31.88 | < 0.0001 |
| Diarrhea | 3.76 ± 0.62 | 3.71 ± 0.77 | 3.54 ± 0.73 | 3.47 ± 0.58 | 6.585 | 0.0002 |
| Financial problems | 50.65 ± 5.60 | 52.54 ± 4.52 | 54.63 ± 5.47 | 54.98 ± 5.01 | 24.26 | < 0.0001 |
In the FACT-G scoring, the physical, functional, emotional, social, and family well-being scores all exhibited a significant upward trend in patients at 1 week, as well as 1-, 3-, and 6-month after surgery compared with before surgery (P < 0.05; Table 2).
| 1 week after surgery | 1 month after surgery | 3 months after surgery | 6 months after surgery | F | P value | |
| Physical well-being | 20.19 ± 1.30 | 21.61 ± 1.47 | 23.69 ± 1.57 | 24.84 ± 1.26 | 351.0 | < 0.0001 |
| Social and family well-being | 13.73 ± 1.40 | 18.17 ± 1.19 | 19.46 ± 1.23 | 20.17 ± 1.29 | 124.3 | < 0.0001 |
| Emotional well-being | 18.24 ± 1.36 | 19.34 ± 1.11 | 20.24 ± 1.31 | 21.28 ± 1.38 | 159.1 | < 0.0001 |
| Functional well-being | 14.58 ± 1.08 | 14.81 ± 1.07 | 16.13 ± 1.25 | 18.66 ± 1.38 | 387.7 | < 0.0001 |
| FACT-G total score | 70.74 ± 2.43 | 73.93 ± 2.24 | 79.52 ± 2.86 | 84.94 ± 2.78 | 934.5 | < 0.0001 |
The SDS score for gynecological cancer patients was 41.31 ± 9.88 one week after surgery and 42.28 ± 11.53 one month after surgery, with no statistical significance (P > 0.05). In contrast, a significant difference was observed in SAS scores at 1 week (37.98 ± 8.92) and 1 month (43.07 ± 8.58) after surgery (P < 0.05; Figure 1).
Among the 160 gynecological cancer patients, 30 (18.75%) had anxiety, 29 (18.13%) had depression, and 17 (10.63%) had both anxiety and depression. Univariate analysis of the influencing factors of anxiety and depression revealed that annual household income, working status, body pain, and sleep duration had a significant impact on anxiety (Table 3), whereas annual household income, body pain, and sleep duration significantly influenced depression (Table 4).
| Anxiety (n = 30) | Non-anxiety (n = 130) | χ2 | P value | |
| Age (years) | 0.401 | 0.527 | ||
| < 45 | 14 | 69 | ||
| ≥ 45 | 16 | 61 | ||
| Tumor type | 0.489 | 0.783 | ||
| Carcinoma of the cervix | 10 | 48 | ||
| Carcinoma of the vulva | 5 | 26 | ||
| Endometrial carcinoma | 15 | 56 | ||
| Ethnicity | 0.036 | 0.849 | ||
| Han | 20 | 89 | ||
| Ethnic minorities | 10 | 41 | ||
| Education level | 0.312 | 0.577 | ||
| High school and below | 17 | 87 | ||
| Bachelor’s degree or above | 13 | 43 | ||
| Residence | 0.041 | 0.839 | ||
| Rural | 16 | 72 | ||
| Urban | 14 | 58 | ||
| Payment mode for medical expenses | 0.173 | 0.677 | ||
| Medical insurance payouts | 22 | 100 | ||
| Out-of-pocket payment | 8 | 30 | ||
| Annual household income (ten thousand CNY) | 9.842 | 0.002 | ||
| < 5 | 20 | 46 | ||
| ≥ 5 | 10 | 84 | ||
| Marital status | 0.390 | 0.532 | ||
| Married | 19 | 90 | ||
| Unmarried, divorced, or widowed | 11 | 40 | ||
| Number of children born | 2.342 | 0.310 | ||
| None | 5 | 39 | ||
| 1 | 16 | 62 | ||
| ≥ 2 | 9 | 29 | ||
| Working status | 6.333 | 0.012 | ||
| Employed | 14 | 92 | ||
| Unemployed or resigned | 16 | 38 | ||
| Body pain | 16.381 | < 0.0001 | ||
| With | 22 | 43 | ||
| Without | 8 | 87 | ||
| Daily sleep duration (hour) | 15.511 | < 0.0001 | ||
| < 6 | 20 | 37 | ||
| ≥ 6 | 10 | 93 |
| Depression (n = 29) | Non-depressive (n = 131) | χ2 | P value | |
| Age (years) | 1.563 | 0.211 | ||
| < 45 | 12 | 71 | ||
| ≥ 45 | 17 | 60 | ||
| Tumor type | 0.064 | 0.969 | ||
| Carcinoma of the cervix | 10 | 48 | ||
| Carcinoma of the vulva | 6 | 25 | ||
| Endometrial carcinoma | 13 | 58 | ||
| Ethnicity | 0.111 | 0.739 | ||
| Han | 19 | 90 | ||
| Ethnic minorities | 10 | 41 | ||
| Education level | 5.985 | 0.014 | ||
| High school and below | 8 | 69 | ||
| Bachelor’s degree or above | 21 | 62 | ||
| Residence | 0.188 | 0.665 | ||
| Rural | 17 | 71 | ||
| Urban | 12 | 60 | ||
| Payment mode for medical expenses | 0.183 | 0.669 | ||
| Medical insurance payouts | 23 | 99 | ||
| Out-of-pocket payment | 6 | 32 | ||
| Annual household income (ten thousand CNY) | 4.410 | 0.036 | ||
| < 5 | 17 | 49 | ||
| ≥ 5 | 12 | 82 | ||
| Marital status | 0.300 | 0.584 | ||
| Married | 21 | 88 | ||
| Single, divorced, or widowed | 8 | 43 | ||
| Number of children born | 0.204 | 0.903 | ||
| None | 8 | 36 | ||
| 1 | 15 | 63 | ||
| ≥ 2 | 6 | 32 | ||
| Working status | 0.063 | 0.801 | ||
| Employed | 19 | 89 | ||
| Unemployed or resigned | 10 | 42 | ||
| Body pain | 30.511 | < 0.0001 | ||
| Yes | 25 | 40 | ||
| No | 4 | 91 | ||
| Daily sleep duration (hour) | 25.011 | < 0.0001 | ||
| < 6 | 22 | 35 | ||
| ≥ 6 | 7 | 96 |
Multivariate regression analysis revealed that body pain was a risk factor for anxiety and depression, whereas sleep duration ≥ 6 h was a protective factor (Table 5).
| Variables | β | SE | Wald | P value | HR | 95%CI |
| Anxiety | ||||||
| Annual household income ≥ 50000 CNY | -0.792 | 0.481 | 2.710 | 0.100 | 0.453 | 0.176-1.163 |
| Employed | -0.853 | 0.500 | 2.915 | 0.088 | 0.426 | 0.160-1.134 |
| Presence of body pain | 1.551 | 0.486 | 10.172 | 0.001 | 4.716 | 1.818-12.232 |
| Sleep duration ≥ 6 hours | -1.581 | 0.496 | 10.147 | 0.001 | 0.206 | 0.078-0.544 |
| Depression | ||||||
| Educational level: Bachelor’s degree or above | 0.461 | 0.563 | 0.671 | 0.413 | 1.586 | 0.526-4.784 |
| Presence of body pain | 2.861 | 0.626 | 20.455 | 0.000 | 16.964 | 4.974-57.857 |
| Sleep duration ≥ 6 hours | -2.278 | 0.572 | 15.861 | 0.000 | 0.103 | 0.033-0.315 |
In general hospitals in China, physical illness often coexists with anxiety and depression[15]. Although anxiety and depression may be early symptoms of physical diseases, they are associated with physical diseases and have various effects on the diseases themselves. The incidence of anxiety was 32.0%-40.0% and that of depression was 25.8%-58.0% in Chinese patients with malignancies. A survey of 3497 adults with anxiety and depression in China revealed statistically higher rates of comorbid anxiety and depression among cancer patients than among adults without cancer (49.69% vs 18.37%; 54.90% vs 17.50%)[16]. This suggests a high incidence of anxiety and depression among patients with malignancies in China. To effectively treat malignancies and enhance the QoL in patients with cancer, considerable attention should be paid to the prevention and treatment of anxiety and depression.
Anxiety, depression, and concurrent anxiety and depression were documented in 30 (18.75%), 29 (18.13%), and 17 (10.63%) of the 160 patients with gynecological cancer in this study, respectively. Six months after surgery, the global health status of these patients was 76.39 ± 3.63, in which the levels of social and emotional functioning were low and the symptoms of fatigue and pain were serious. In terms of the FACT-G scale, the scores of related parameters, such as physical, functional, emotional, social, and family well-being, exhibited an upward trend; however, the average mental health level of patients was relatively low after 1 month of surgery, which may be because of the transition from the ignorance period (incomplete understanding of the condition) to depression period (fully aware of the severity of the condition and developing obvious negative emotions) or the transition from the acceptance period (psychologically forced to accept) to loss period (falling into a pessimistic and desperate state). With continued treatment and time, physical functioning significantly improved at 3 months following surgery, and patients entered the recognition or acceptance period. After 6 months, the patients gradually entered the adaptation period, during which their mental health significantly improved.
In addition, we found that good sleep status was a protective factor for anxiety and depression in patients with gynecological cancer, whereas body pain was a risk factor. Sleep disturbance is a common and significant complaint in patients with cancer, with up to 95% complaining of sleep disturbance/disability during diagnosis, treatment, and even after surviving 10 years[17]. Savard et al[18] conducted a study on cancer survivors and found that 52% had difficulty sleeping, with 58% reporting cancer-induced or exacerbated sleep problems. In a study by Hajj et al[19], higher levels of anxiety and depression were observed in patients with breast cancer with cognitive impairment and poor sleep quality/insomnia. Therefore, good sleep quality and duration are protective factors against anxiety and depression in patients with gynecological cancer. Cancer pain is a multidimensional factor that goes far beyond a nociceptive biochemical signal, with up to half of all cancer patients regularly experiencing pain. Because of its complex etiology, pain manifests as nociceptive, neuropathic, nociceptive, and psychogenic[20,21]. Pain has a significant impact on overall QoL by affecting physical, psychological, and spiritual aspects[22]. In a study of the Austrian population by Unseld et al[23], increased pain levels were strongly associated with psychiatric symptoms in patients with cancer.
This study have several limitations. First, this was a retrospective study, which did not allow the randomization of patients in either group. Thus, the similarity of patients in groups is jeopardized and potentially results in selection bias. Moreover, this study had a small sample size from a single-center study, which may have resulted in differences between both groups. Second, the treatment variability should have been mentioned. This study did not account for variations in treatment modalities, such as surgery type, chemotherapy regimens, or radiation therapy. These treatments can differ in their efficacy, side effects, and impact on QoL, anxiety, and depression. Third, the follow-up time was too short to determine long-term outcomes. A longer follow-up period would provide a more comprehensive understanding of the observed changes in outcomes over time. Fourth, the study solely focused on quantitative measures, such as questionnaires. The absence of qualitative data, such as patient interviews or open-ended questions, limits the opportunity to gain further insight into the patient’s experiences and perspectives regarding QoL, anxiety, and depression. Therefore, well-designed, randomized, and controlled trials with prospective data collection, long-term follow-up, and sample size calculation are required to confirm our findings.
In summary, patients with gynecological malignancies often experience anxiety and depression. By analyzing the factors that affect their QoL, effective nursing measures may be provided to improve QoL. Mental health treatment options for such women should be strengthened to reduce the burden of increased mental symptoms.
| 1. | Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75126] [Cited by in RCA: 64583] [Article Influence: 16145.8] [Reference Citation Analysis (176)] |
| 2. | Perkins RB, Wentzensen N, Guido RS, Schiffman M. Cervical Cancer Screening: A Review. JAMA. 2023;330:547-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 180] [Reference Citation Analysis (0)] |
| 3. | Ali AT, Al-Ani O, Al-Ani F. Epidemiology and risk factors for ovarian cancer. Prz Menopauzalny. 2023;22:93-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 46] [Reference Citation Analysis (0)] |
| 4. | Berek JS, Matias-Guiu X, Creutzberg C, Fotopoulou C, Gaffney D, Kehoe S, Lindemann K, Mutch D, Concin N; Endometrial Cancer Staging Subcommittee, FIGO Women's Cancer Committee. FIGO staging of endometrial cancer: 2023. Int J Gynaecol Obstet. 2023;162:383-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 459] [Article Influence: 229.5] [Reference Citation Analysis (0)] |
| 5. | Egger EK, Ralser DJ, Lindner K, Recker F, Marinova M, Savchenko O, Lau JF, Mustea A. Diagnostic and Therapeutic Approach in a Metastatic Vaginal Adenocarcinoma: A Case Report. Front Immunol. 2021;12:686879. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Paulsen A, Vistad I, Fegran L. Gynecological cancer survivors' experiences with sexual health communication in nurse-led follow-up consultations. Acta Obstet Gynecol Scand. 2024;103:551-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 7. | Aquil A, El Kherchi O, El Azmaoui N, Mouallif M, Guerroumi M, Benider A, Elgot A. Predictors of mental health disorders in women with breast and gynecological cancer after radical surgery: A cross-sectional study. Ann Med Surg (Lond). 2021;65:102278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Klapheke AK, Keegan THM, Ruskin R, Cress RD. Depressive symptoms and health-related quality of life in older women with gynecologic Cancers. J Geriatr Oncol. 2020;11:820-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Sajjad S, Ali A, Gul RB, Mateen A, Rozi S. The effect of individualized patient education, along with emotional support, on the quality of life of breast cancer patients - A pilot study. Eur J Oncol Nurs. 2016;21:75-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Grusdat NP, Stäuber A, Tolkmitt M, Schnabel J, Schubotz B, Wright PR, Schulz H. Routine cancer treatments and their impact on physical function, symptoms of cancer-related fatigue, anxiety, and depression. Support Care Cancer. 2022;30:3733-3744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 41] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 11. | Grassi L, Riba M. Cancer and severe mental illness: Bi-directional problems and potential solutions. Psychooncology. 2020;29:1445-1451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 12. | Wang YH, Li JQ, Shi JF, Que JY, Liu JJ, Lappin JM, Leung J, Ravindran AV, Chen WQ, Qiao YL, Shi J, Lu L, Bao YP. Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies. Mol Psychiatry. 2020;25:1487-1499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 434] [Article Influence: 86.8] [Reference Citation Analysis (0)] |
| 13. | Naser AY, Hameed AN, Mustafa N, Alwafi H, Dahmash EZ, Alyami HS, Khalil H. Depression and Anxiety in Patients With Cancer: A Cross-Sectional Study. Front Psychol. 2021;12:585534. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 113] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 14. | Unseld M, Krammer K, Lubowitzki S, Jachs M, Baumann L, Vyssoki B, Riedel J, Puhr H, Zehentgruber S, Prager G, Masel EK, Preusser M, Jaeger U, Gaiger A. Screening for post-traumatic stress disorders in 1017 cancer patients and correlation with anxiety, depression, and distress. Psychooncology. 2019;28:2382-2388. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 15. | Chen Y, Huang X, Zhang C, An Y, Liang Y, Yang Y, Liu Z. Prevalence and predictors of posttraumatic stress disorder, depression and anxiety among hospitalized patients with coronavirus disease 2019 in China. BMC Psychiatry. 2021;21:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 16. | Yang YL, Liu L, Wang Y, Wu H, Yang XS, Wang JN, Wang L. The prevalence of depression and anxiety among Chinese adults with cancer: a systematic review and meta-analysis. BMC Cancer. 2013;13:393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 120] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | Büttner-Teleagă A, Kim YT, Osel T, Richter K. Sleep Disorders in Cancer-A Systematic Review. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 89] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 18. | Savard J, Simard S, Blanchet J, Ivers H, Morin CM. Prevalence, clinical characteristics, and risk factors for insomnia in the context of breast cancer. Sleep. 2001;24:583-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 291] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 19. | Hajj A, Hachem R, Khoury R, Hallit S, ElJEBBAWI B, Nasr F, El Karak F, Chahine G, Kattan J, Rabbaa Khabbaz L. Clinical and genetic factors associated with anxiety and depression in breast cancer patients: a cross-sectional study. BMC Cancer. 2021;21:872. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 20. | Haroun R, Wood JN, Sikandar S. Mechanisms of cancer pain. Front Pain Res (Lausanne). 2022;3:1030899. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 21. | Mestdagh F, Steyaert A, Lavand'homme P. Cancer Pain Management: A Narrative Review of Current Concepts, Strategies, and Techniques. Curr Oncol. 2023;30:6838-6858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 66] [Reference Citation Analysis (0)] |
| 22. | Rodriguez C, Ji M, Wang HL, Padhya T, McMillan SC. Cancer Pain and Quality of Life. J Hosp Palliat Nurs. 2019;21:116-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 23. | Unseld M, Zeilinger EL, Fellinger M, Lubowitzki S, Krammer K, Nader IW, Hafner M, Kitta A, Adamidis F, Masel EK, Preusser M, Jäger U, Gaiger A. Prevalence of pain and its association with symptoms of post-traumatic stress disorder, depression, anxiety and distress in 846 cancer patients: A cross sectional study. Psychooncology. 2021;30:504-510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |