Published online Jun 19, 2024. doi: 10.5498/wjp.v14.i6.985
Revised: April 23, 2024
Accepted: April 28, 2024
Published online: June 19, 2024
Processing time: 113 Days and 1.4 Hours
Epilepsy and depression have complicated bidirectional relationships. Our study aimed to explore the field of epilepsy comorbid with depression in a bibliometric perspective from 2014-2023.
To improve our understanding of epilepsy and depression by evaluating the relationship between epilepsy and depression, bibliometric analyses were performed.
Epilepsy and depression-related publications from the last decade were retrieved from the Web of Science Core Collection. We conducted bibliometric and visual analysis using VOSviewer and CiteSpace, examining authorships, countries, institutions, journals of publication, co-citations of references, connections between keywords, clusters of keywords, and keywords with citation bursts.
Over the past ten years, we collected 1045 research papers focusing on the field of epilepsy and comorbid depression. Publications on epilepsy and depression have shown a general upward trend over time, though with some fluctuations. The United States, with 287 articles, and the University of Melbourne, contributing 34 articles, were the top countries and institutions, respectively. In addition, in the field of epilepsy and depression, Professor Lee, who has published 30 articles, was the most contributing author. The hot topics pay attention to the quality of life in patients with epilepsy and depression.
We reported that quality of life and stigma in patients with epilepsy comorbid with depression are possible future hot topics and directions in the field of epilepsy and depression research.
Core Tip: A total of 1045 publications explored the development of epilepsy and depression. Our study integrated bibliometric information to analyze the most influential authorships, countries, institutions, journals of publication, co-citations of references, connections between keywords, clusters of keywords, and keywords with citation bursts in the field of epilepsy and depression research. We then identified future hot topics and directions in the field of epilepsy and depression.
- Citation: Chen L, He XH, Li XL, Yang J, Huang H. Bibliometric analysis of research in epilepsy and comorbid depression from 2014 to 2023. World J Psychiatry 2024; 14(6): 985-998
- URL: https://www.wjgnet.com/2220-3206/full/v14/i6/985.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i6.985
Epilepsy, a chronic neurological condition that impacts over 70 million individuals globally, is a group of brain neurons caused by transient abnormal discharge due to central nervous system dysfunction[1,2]. The World Health Organization ranks epilepsy as the second most burdensome neurologic disorder worldwide[3]. Epilepsy can affect both sexes and people of all ages worldwide, leading to social, behavioral, health, and economic consequences and significantly affecting the quality of life of patients[4,5].
Previous research indicates that epilepsy has an annual incidence rate of 0.614%, and compared with that in high-income countries, the incidence of epilepsy in low/middle-income countries is greater[5,6]. People with epilepsy expe
Depressive disorder is a severe and common mood disorder and is one of the most widespread forms of psychiatric disorders worldwide[14,15]. In depressive disorder, hypothalamic pituitary adrenal axis abnormalities are well known. High instances of depression in epilepsy patients are likely linked to hormonal imbalances, which stem from the negative impacts of seizures and interictal epileptiform discharges on the hypothalamic-pituitary-adrenal axis[16]. In addition, the imbalance between GABA-mediated inhibition and excessive glutamatergic neurotransmission is involved in epileptogenesis[17], and disturbed GABA and glutaminergic neurotransmission has also been observed in individuals with depressive disorders[18,19]. Studies have shown that epileptogenesis can promote the production of excitatory amino acids, which leads to the activity of 5-hydroxytryptamine, and this is one of the main causes of depression[20]. A decrease in 5-hydroxytryptamine activity can also further induce epilepsy[21], indicating a bidirectional relationship between epilepsy and depressive disorder. An increasing number of studies have shown that depression in epilepsy patients has a specific biological basis[16,22-25]. Hence, summarizing the historical progression of research in the fields of epilepsy and depressive disorders is essential, and further exploring the mechanisms of epilepsy and depression comorbidity by bibliometric analysis and visualization provides a novel research focus and emerging topics.
Bibliometrics, first introduced in the early 1900s, formed an independent discipline in 1969[26]. This method involves analyzing published content along with its associated metadata as a quantitative approach to characterizing and assessing the evolution and advancement of a discipline or research field. It also includes visualizing the outcomes of the literature analysis through software that performs correlation analysis[27]. Bibliometrics has been widely used in the field of biomedicine because it provides a reliable basis for the diagnosis and treatment of various diseases and is reasonable[28]. Details such as authorships, countries, institutions, journals of publication, and co-citations of references can be obtained in the analysis process. Thus, the development of a field can be obtained through bibliometric analysis. To our knowledge, there has been no published bibliometric analysis focusing on epilepsy and depressive disorder. To fill this gap, we employed bibliometric tools VOSviewer and CiteSpace to determine the evolution and developmental frontiers of epilepsy and depressive disorder.
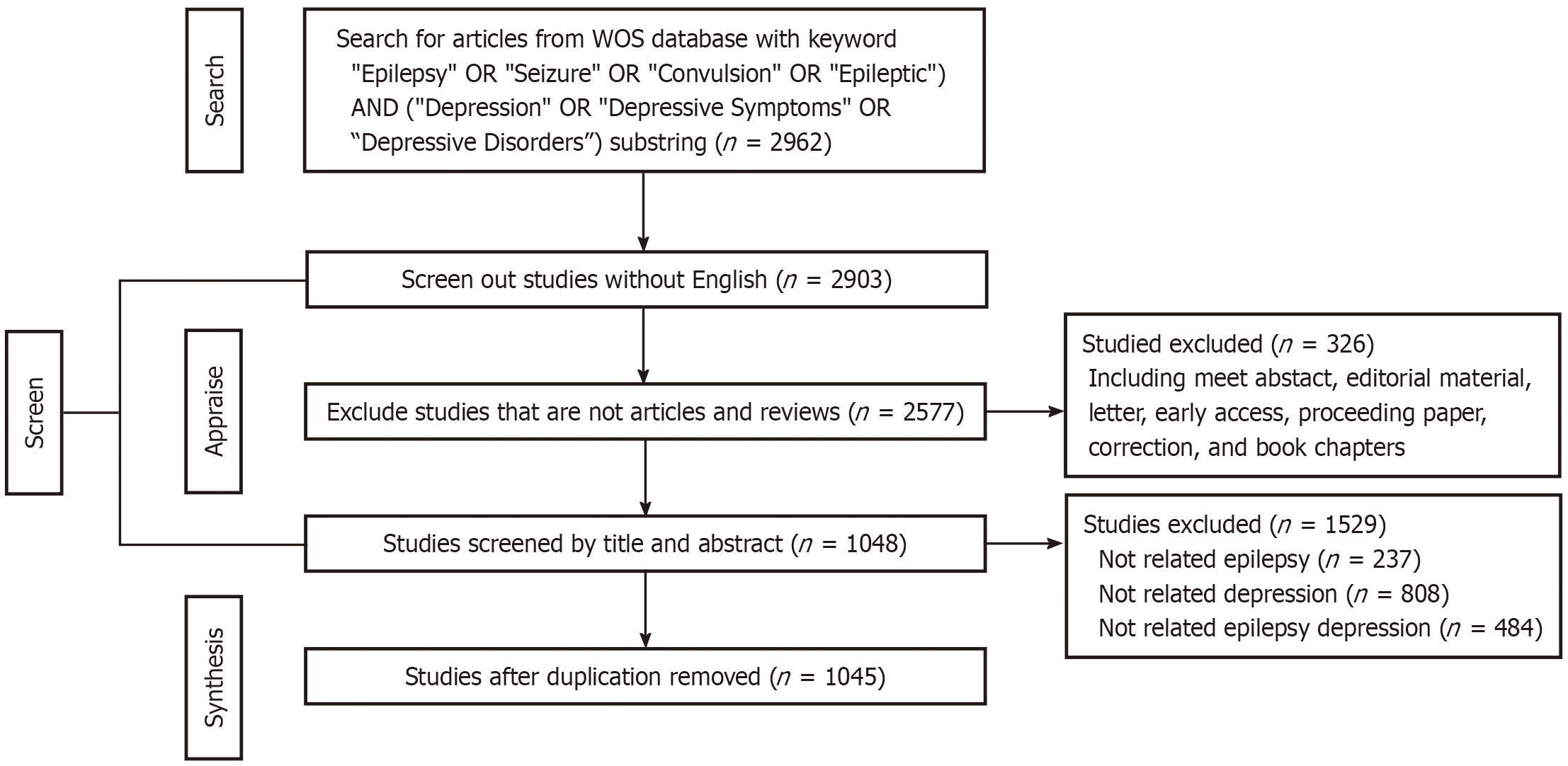
Web of Science (WoS) is one of the most commonly used academic database sources[29]. For this study, data from the past decade were sourced from the WoS Core Collection (WoSCC) database. To minimize bias from daily updates to the database, literature collection from the WoSCC was conducted on a single day, that is, January 4 2024. We used TS = ((“Epilepsy” OR “Seizure” OR “Convulsion” OR “Epileptic”) AND (“Depression” OR “Depressive Symptoms” OR ”Depressive Disorders”)) AND WC = (“neurology” OR “Psychiatry” OR “neuropsychiatry”). The timeframe for the publications analyzed spanned from January 1, 2014, to December 31, 2023, and only original articles and reviews were included in the document types. In total, 2962 publications were incorporated into the study, with 2147 original articles and 440 reviews. Chen and He assessed the titles and abstracts, eliminating any research that was not unrelated to epilepsy and depression. The search strategy is depicted in Table 1 and Figure 1.
| Category | Specific standard requirement |
| Research database | Web of Science core collection |
| Citation indexes | SCI-Expanded |
| Searching period | January 2014 to December 2023 |
| Language | English |
| Searching keywords | (“Epilepsy” OR “Seizure” OR “Convulsion” OR “Epileptic”) AND (“Depression” OR “Depressive Symptoms” OR “Depressive Disorders”) |
| Document types | Articles and reviews |
| Data extraction | Export with full records and cite references in plain text format |
| Sample size | 2962 |
In this research, bibliometric analysis and data visualization were performed using VOSviewer (version 1.6.20) and CiteSpace (version 6.2. R7). Initially, we exported the records obtained from the WoS into plain text files containing full records and references, labeled as download_XX.txt. Subsequently, these files were imported into VOSviewer and CiteSpace for conducting bibliometric and visual analysis. VOSviewer and CiteSpace are pivotal tools employed for bibliometric analysis and the identification of trends within scientific literature. VOSviewer and CiteSpace are adept at conducting comprehensive analyses across various dimensions, including countries, journals, authorships, co-citation journals, fronts, and emerging trends, by examining annual publication numbers, identifying growth trends, exploring the most commonly used keywords, and detecting keywords that have experienced significant spikes in citations over time.
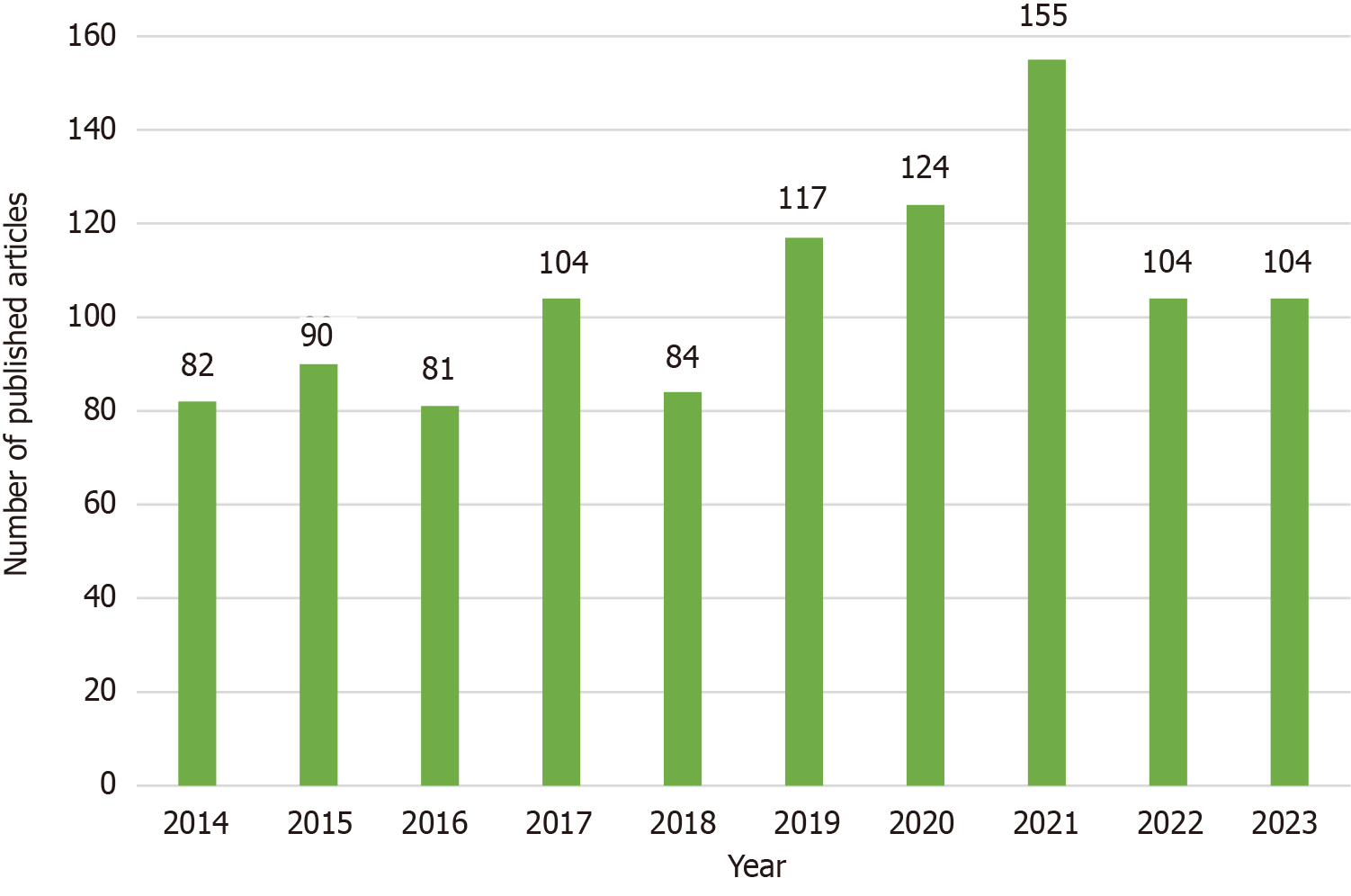
This study utilized 1045 articles authored by 4647 individuals from 1587 institutions across 80 countries. These articles were published in 125 different journals and cited 26513 references from 5305 journals. A total of 1045 articles related to epilepsy and depression were published in a decade, which depicted an increasing trend and some fluctuations (Figure 2). Overall, over the past ten years, the number of published articles in the field of epilepsy and depression has remained steady at over 80 despite a few minor fluctuations, suggesting that academics are becoming increasingly interested in this area of research.
According to Prices’ Law, the minimum number of articles written by a core author in a particular field m = 0.749 × nmax1/2 (nmax is the number of articles by the most productive authors in the field).
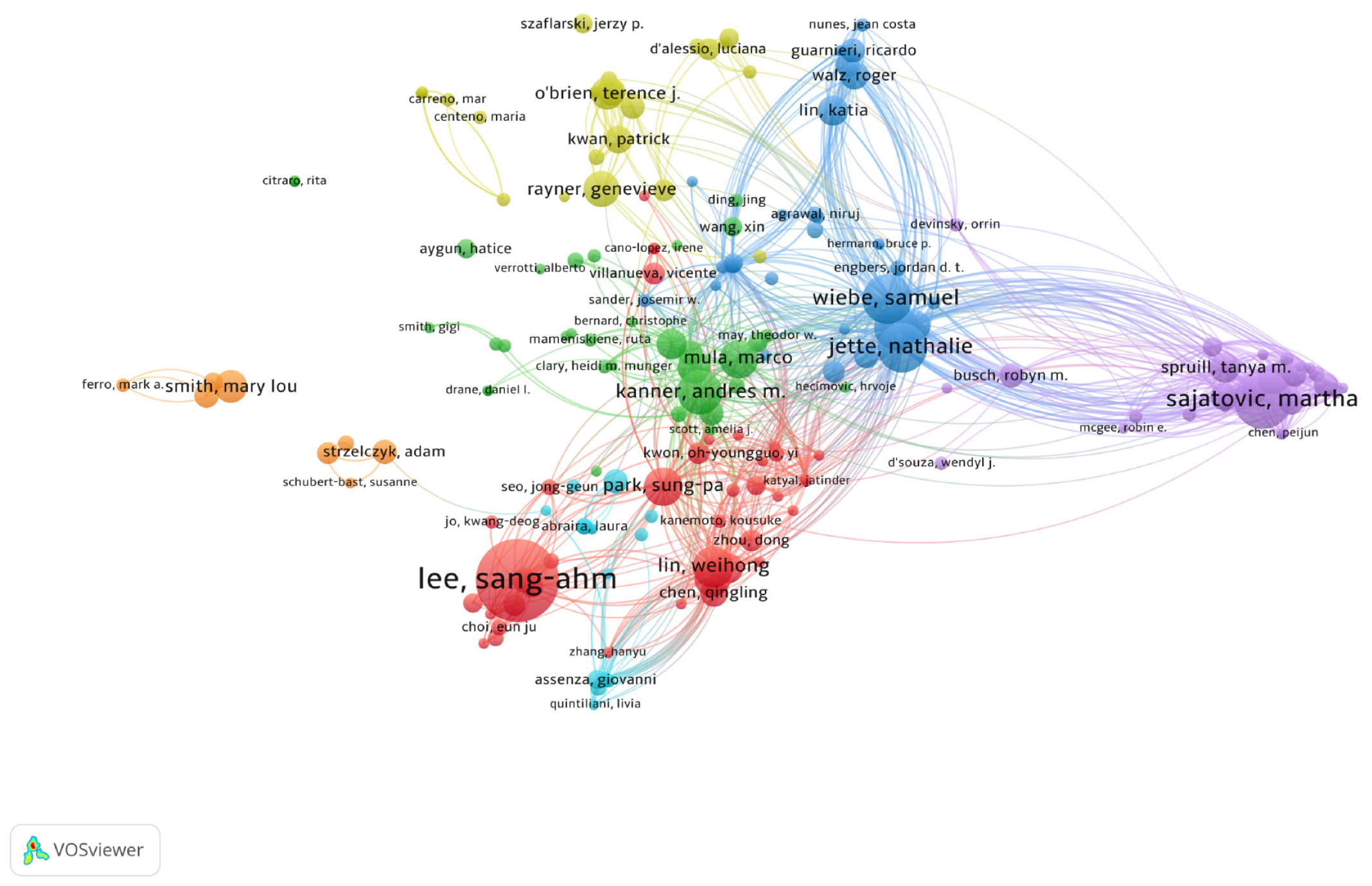
In our research, m = 0.749 × 30 ≈ 4.10. Therefore, authors with more than 4 articles (including 4 articles) are positioned as the core authors in this field. In the last 10 years, a total of 4647 authors contributed to the field of epilepsy and depression, and 182 authors published over 4 articles (Figure 3). Lee S emerged as the most prolific author in this field, who has published 30 articles. Their primary research focus is on comorbid mental health in people with epilepsy. Table 2 shows the highly productive authors who have published more than 15 articles in this field.
| Rank | Author | Documents | Citations | Average citation/publication |
| 1 | Lee S | 30 | 262 | 8.73 |
| 2 | Sajatovic M | 21 | 277 | 13.19 |
| 3 | Jette N | 18 | 698 | 38.78 |
| 3 | Wiebe S | 18 | 577 | 32.06 |
| 4 | Kanner A | 16 | 677 | 42.31 |
| 4 | Patten S | 16 | 553 | 34.56 |
| 5 | Lin W | 15 | 50 | 3.33 |
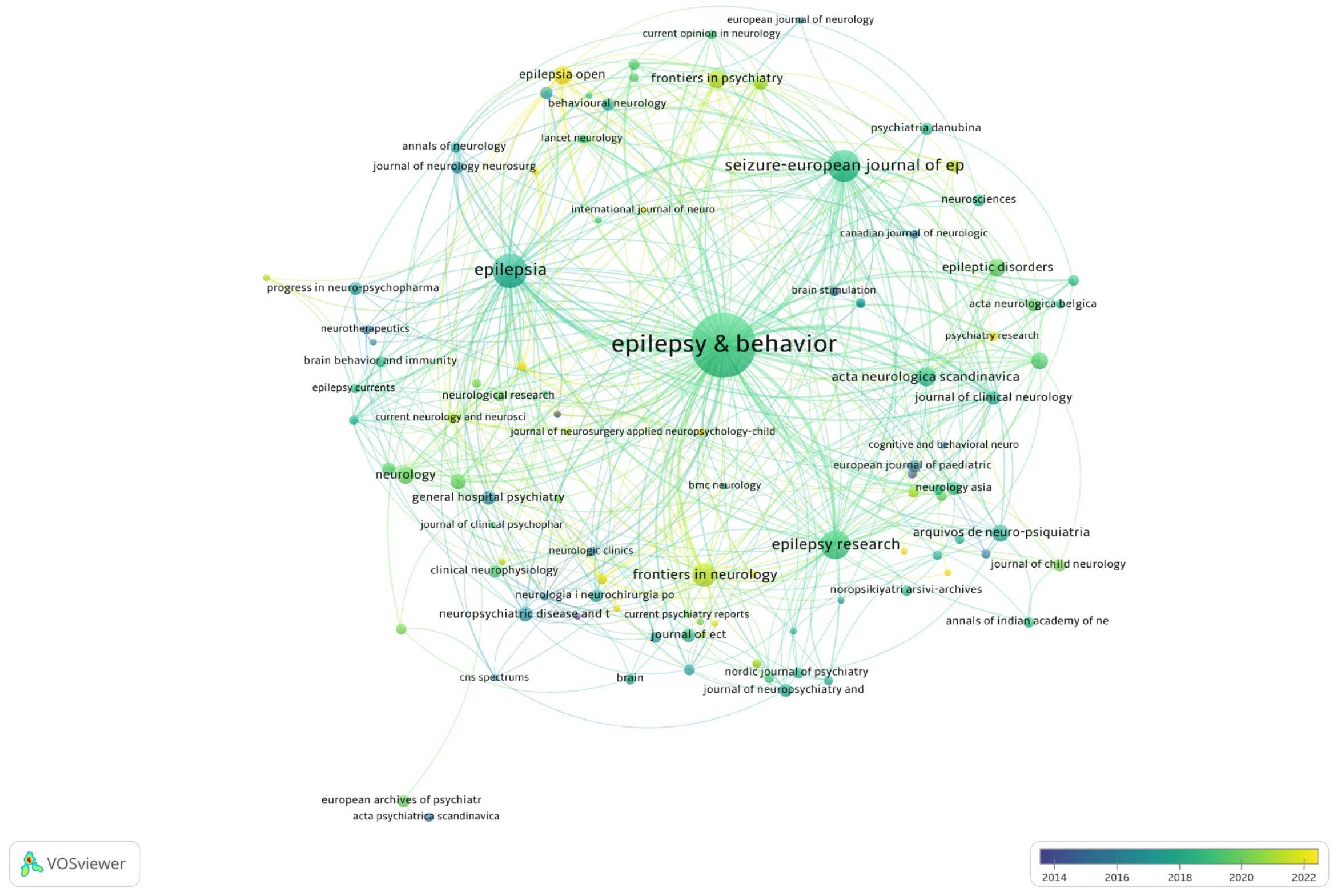
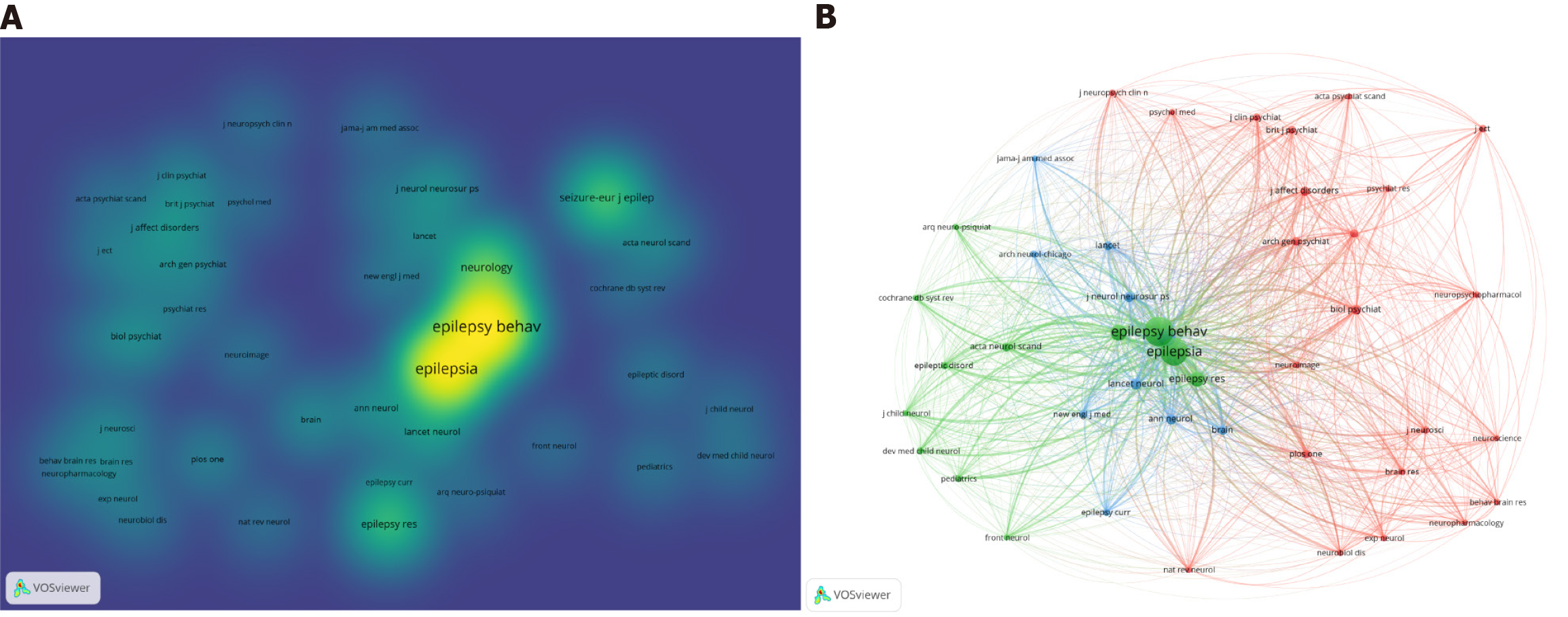
A total of 125 journals were included and visualized by using VOSviewer. As a result, between 2019 and 2021, the number of articles published in the majority of the journals was the greatest (Figure 4), which is consistent with Figure 1. Then, we summarized the journals with the top 10 most publications (Table 3) and found that the top 10 journals published 73.59% of the total publications (n = 769). Among the top 10 journals in epilepsy and depression research, Epilepsy & Behavior was the most active journal, with 481 publications, closely followed by Epilepsia with 80 publications, and the Seizure-European Journal of Epilepsy with 64 publications.
| Rank | Source | Publication | Citations | Average citation/publication |
| 1 | Epilepsy and Behavior | 481 | 6740 | 14.01 |
| 2 | Epilepsia | 80 | 2221 | 27.76 |
| 3 | Seizure-European Journal of Epilepsy | 64 | 1178 | 18.41 |
| 4 | Epilepsy Research | 50 | 554 | 11.08 |
| 5 | Frontiers in Neurology | 28 | 331 | 11.82 |
| 6 | Acta Neurologica Scandinavica | 15 | 219 | 14.60 |
| 7 | Epilepsia Open | 14 | 47 | 3.36 |
| 8 | Frontiers in Psychiatry | 13 | 127 | 9.77 |
| 9 | Neurology | 12 | 233 | 19.42 |
| 10 | Epileptic Disorders | 12 | 88 | 7.33 |
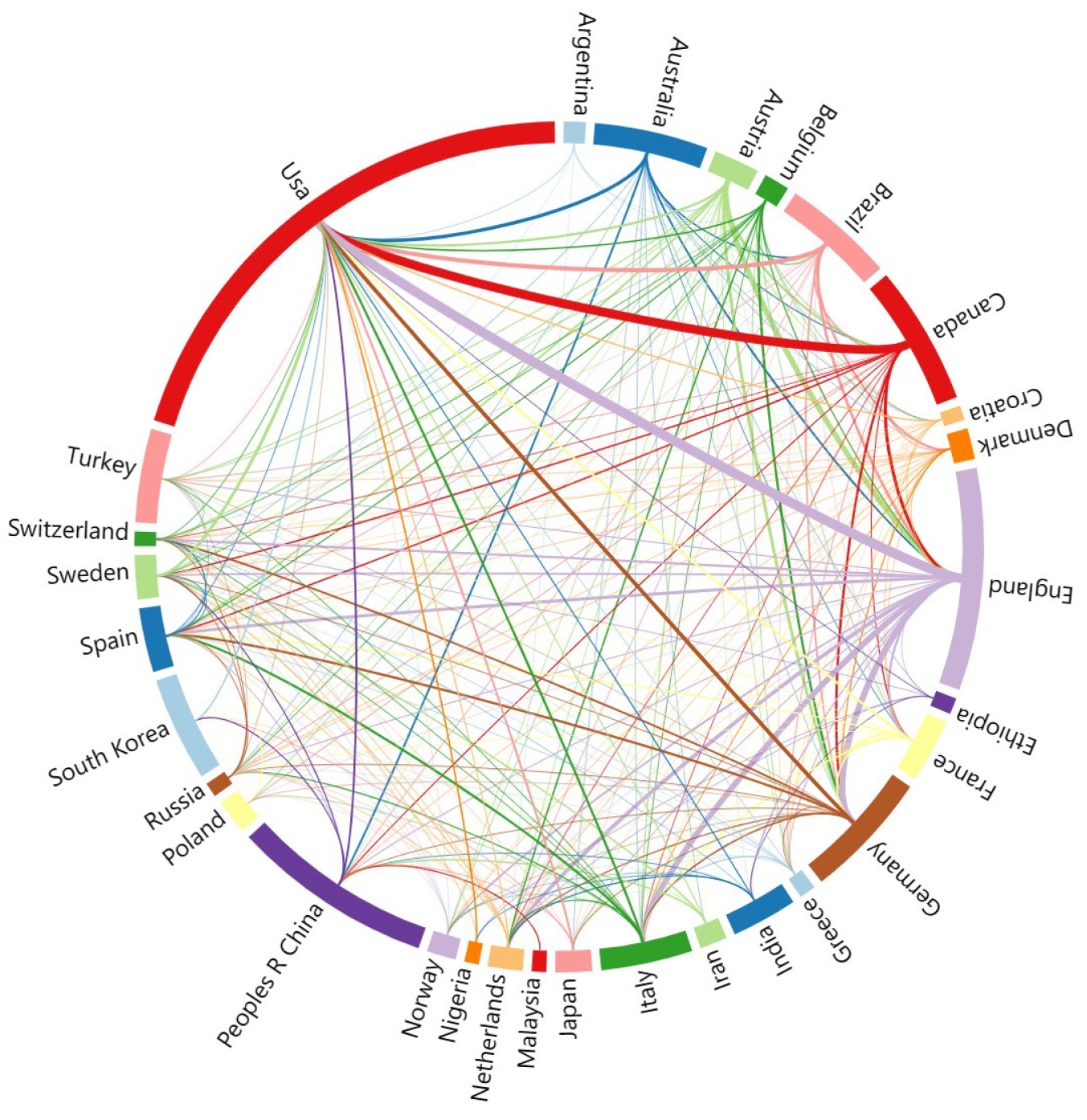
This study utilized 1045 articles authored by 4647 individuals from 1587 institutions across 80 countries. Firstly, the 30 countries with the most publications were visualized using VOSviewer and Microsoft Charticulator. The United States and England demonstrated the highest frequency of collaboration in this field, with Canada also showing significant cooperative involvement (Figure 5). Table 4 details the top five countries and institutions that are leading in publishing research on epilepsy and depression, providing a deeper analysis of those with high productivity. According to Table 4, we found that these five countries published 664 publications (63.54%), and the majority of publications were from the United States (n = 287, 27.46%), which received 5106 citations; however, England has the highest number of citations per paper, with 121 articles receiving 2786 citations, and each publication’s average number of citations was 23.02. Moreover, publications from these top five institutions amounted to 145, accounting for 13.88% of the total, with the University of Melbourne leading with 34 publications, representing 3.25%, followed by the University of Ulsan (n = 34, 3.06%) and the University of Calgary (n = 29, 2.78%).
| Rank | Country | Publications | Citations | Institutions | Publications | Citations |
| 1 | United States | 287 | 5106 | University of Melbourne | 34 | 411 |
| 2 | England | 121 | 2786 | University of Ulsan | 32 | 292 |
| 3 | China | 110 | 1205 | University of Calgary | 29 | 979 |
| 4 | Canada | 76 | 1717 | Case Western Reserve University | 28 | 358 |
| 5 | Germany | 70 | 1366 | Kyungpook National University | 22 | 523 |
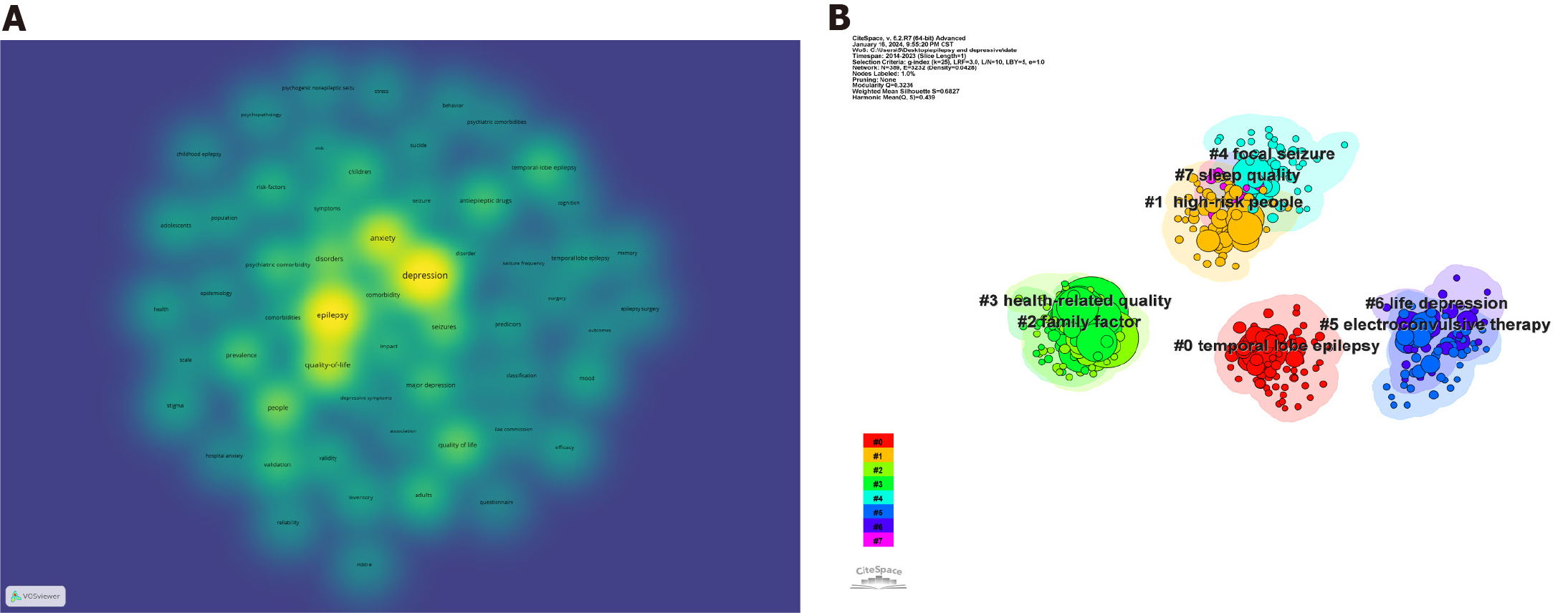
To identify the main areas of interest and emerging trends in epilepsy and depression research, we utilized VOSviewer to generate a map of keyword co-occurrences (Figure 6A). First, we analyzed the frequency of keyword occurrence in epilepsy and depression research. The brighter and wider the yellow range is, the greater the frequency of keyword occurrence. Table 5 lists the common keywords of the top 5 most common keywords: Depression (frequency: 643), epilepsy (frequency: 605), anxiety (frequency: 364), quality of life (frequency: 307), and people (frequency: 198). The five most prominent keywords prevalent in the current research literature underscore the focal areas of scholarly interest and investigation within the field.
| Rank | Keyword | Occurrences | Total link strength |
| 1 | Depression | 643 | 5456 |
| 2 | Epilepsy | 605 | 5011 |
| 3 | Anxiety | 364 | 3235 |
| 4 | Quality-of-life | 307 | 2817 |
| 5 | People | 198 | 1834 |
Then, we conducted a cluster analysis of co-occurring keywords using CiteSpace, resulting in the identification of eight clusters. The average silhouette (S value) of the cluster serves as a metric to assess the quality of clustering. Typically, an S value greater than 0.5 suggests reasonable clustering and an S value exceeding 0.7 indicates highly convincing clustering[30]. All of the clusters achieved an S value over 0.5, indicating that the clustering results were reasonably reliable (Figure 6B, Table 6).
| Cluster-ID | Silhouette | Mean | Included keyword (top 5) |
| 0 | 0.651 | 2017 | Temporal lobe epilepsy; depression-like behavior; mesial temporal lobe epilepsy; rij rat, and absence seizure |
| 1 | 0.623 | 2017 | High-risk people, Lebanese people, taking medication, family cohesion, and negative health events |
| 2 | 0.610 | 2017 | Family factor, psychogenic nonepileptic seizure, psychiatric disorder, emotional functioning, and patient caregiver |
| 3 | 0.819 | 2016 | Health-related quality, neurological disorders, depression inventory, risk factor, electroconvulsive therapy, and drug-resistant epilepsy |
| 4 | 0.630 | 2017 | Focal seizure, eslicarbazepine acetate, an antiepileptic drug, clinical practice finding, and Euro-Esli study |
| 5 | 0.693 | 2016 | Electroconvulsive therapy; magnetic seizure therapy; novel seizure quality index; ictal parameter; and case report |
| 6 | 0.771 | 2016 | Life depression, temporal lobe epilepsy surgery, prospective study, seizure freedom, and retrospective analysis |
| 7 | 0.909 | 2018 | Sleep quality, clinical features, sleep abnormalities, major determinants, and self-reported insomnia |
A total of 26513 references were obtained from 5305 journals. First, we analyzed the five most important publications in epilepsy and depression research (Table 7). As we can see from Table 7, all five highly cited publications are articles. They are both dedicated to studying and assessing the quality of life of people with epilepsy. However, depressive disorders, which affect about one-third of patients with epilepsy, are the most prevalent psychiatric comorbidity and significantly decrease the quality of life in patients[12].
| Rank | Title | Year | Citation |
| 1 | Quality of life of people with epilepsy: A European study | 1997 | 182 |
| 2 | Consensus statement: The evaluation and treatment of people with epilepsy and affective disorders | 2008 | 171 |
| 3 | Depression but not seizure frequency predicts quality of life in treatment-resistant epilepsy | 2004 | 128 |
| 4 | Epilepsy and risk of suicide: A population-based case-control study | 2007 | 112 |
| 5 | A brief questionnaire to screen for quality of life in epilepsy: The QOLIE-10 | 1996 | 111 |
Figure 7 shows that the three most frequently cited journals were Epilepsy Behavior (7234 citations), Epilepsia (6133 citations), and Neurology (1757 citations) (Figure 7A). The journal co-citation consists of three clusters corresponding to the three colors in the figure (Figure 7B). The Journal of Neurology is excellent in JCR1, and the remaining two journals are excellent in JCR2. Among the three clusters, the journals in the green cluster are mainly related to epilepsy research, which is devoted to the most current information available on the behavioral aspects of seizures and epilepsy. The journals in the red cluster focus on psychiatric disorders, which involve the epidemiology, classification, and treatment of psychiatric disorders or the development and validity of measurement instruments. The journals in the blue cluster focus on the overall study of neurological diseases, which is devoted to the study of diseases and conditions of the nervous system.
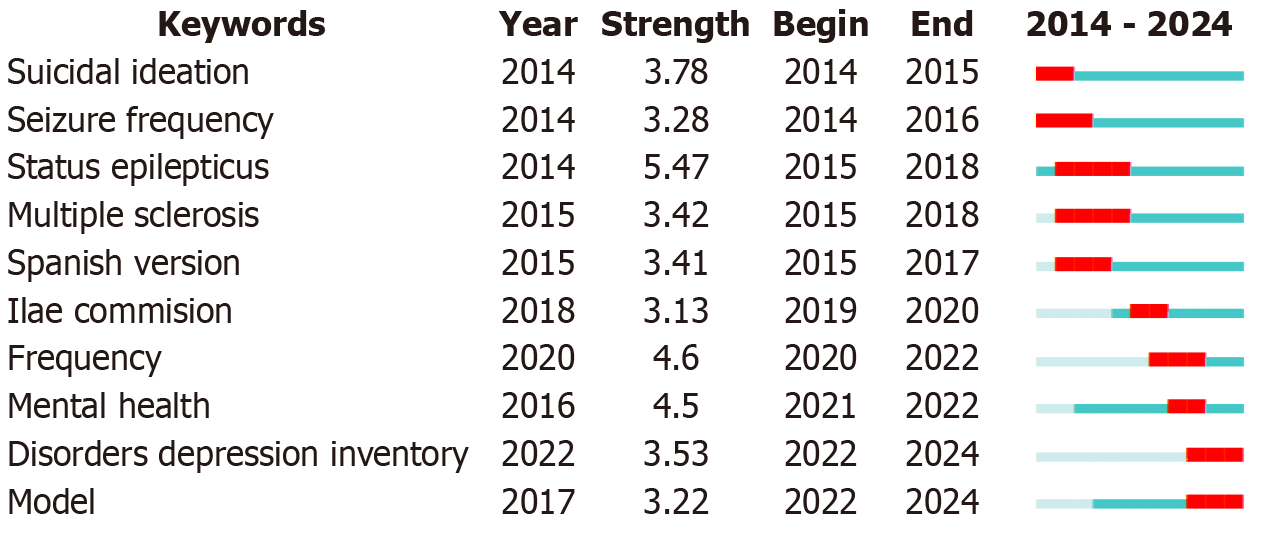
Finally, we created visualizations of the top 10 keywords that exhibited the most significant citation bursts between 2014 and 2023 (Figure 8). The blue line indicates the period, whereas the red line shows the period during which bursts of keyword citations occurred. The most intense explosive word is status epilepticus. The three most recent citation bursts occurred in 2022 (model) and 2022 (disorders depression inventory) and lasted until 2024 and 2021 (mental health); all of these bursts lasted until 2022.
Epilepsy and depression are known to have a bidirectional relationship[31]. Depression, notably the most frequent psychiatric comorbidity among epilepsy patients, greatly diminishes the quality of life[32]. Previous studies revealed that in patients with epilepsy, a nearly 2-fold increase in the risk of developing depression was observed[31]. Furthermore, if people are first diagnosed with depression, the risk of developing epilepsy increases 2.5-fold[33]. In addition, another study demonstrated that epilepsy is not only associated with an increased risk of depression but also with the severity of epilepsy[34]. Although the association between epilepsy and depression has been increasingly established and an increasing number of people have paid attention to the subject of epilepsy and depression in recent years, the dynamics and progress of the epilepsy and depression research field need further elucidation. Therefore, we used bibliometric analysis to study the link between epilepsy and depression.
Our study is the first to employ visualized bibliometric techniques to investigate the field of epilepsy and depression and revealed emerging topics and frontiers via VOSviewer and CiteSpace. Based on our findings, in the last 10 years, we identified 1045 articles authored by 4647 researchers from 1587 institutions across 80 countries, published in 125 different journals, and referencing 26513 citations from 5305 journals. The annual publication output showed steady growth in the research field. Especially from 2020 to 2021, researchers increasingly focused on epilepsy comorbid depression, leading to a record high in the annual number of publications on the topic. According to a previous report, compared to people without epilepsy, patients with epilepsy are more vulnerable to the psychological effects of the coronavirus disease 2019 (COVID-19) pandemic[35]. Thus, we speculated that the increase in publications is closely related to the COVID-19 pandemic. The COVID-19 pandemic has had far-ranging consequences for general physical and mental health[36]. To curb the spread of COVID-19, governments have undertaken measures such as forced house arrests, and mental and physical well-being have significantly decreased[37]. Although there has been no clear evidence thus far that COVID-19 can directly affect seizures, there is evidence that the COVID-19 pandemic has led to an increased risk of depression in epilepsy patients[38].
In our research, we recognized Lee S as the leading scholar in terms of productivity within the field of research on epilepsy and depression. Lee S from South Korea was devoted to studying related comorbid mental health in people with epilepsy, with topics such as anxiety, suicide risk, stigma with epilepsy, and perceived stress. However, Jette N, an author from the United States, had the highest average citation count per publication, who mainly focused on the analysis of epilepsy patients with complex comorbidities, and her articles were published in authoritative journals such as Lancet, Nat Rev Dis Primers, and Neurology. The average number of citations of Jette N was 38.78, which suggested that Jette N was the most influential scholar in epilepsy and depression research. In the author network, we revealed that only the authors who have a number of publications cooperate closely. The overwhelming majority of authors do not have cooperative relationships, which is not conducive to the development of epilepsy and depression research.
In our study, the bibliometric analysis summarized 125 journals from 2014 to 2023. Epilepsy & Behavior published the most papers on epilepsy and depression (46.0% of all articles), followed by Epilepsia (7.7% of all articles) and the Seizure-European Journal of Epilepsy (6.1% of all articles). The majority of the research originated from the United States (27.5% of all papers), followed by England (111.6% of all articles) and the People’s Republic of China (10.5% of all articles). The United States held a dominant position in the field of epilepsy and depression research. The People’s Republic of China is the only developing country in the top 5, and great achievements have been made in the epilepsy and depression research field in the past 10 years. Furthermore, among the five institutions producing the most publications, two were from Korea. It was closely related to Lee S, who was the most productive author who worked for the University of Ulsan. The nations and organizations that publish publications on this topic are not evenly distributed. As a result, more countries and institutions need to collaborate more on epilepsy and depression research for this field to advance.
Our findings highlight the five most cited publications on epilepsy and depression, consisting of 4 original articles and 1 review. In the 5 publications, 3 focused on the quality of life of patients. The article “Consensus statement: The evaluation and treatment of people with epilepsy and affective disorders”, published in Epilepsy Behavior, received the second most citations; this article presents a consensus statement dedicated to addressing depression across various age groups, including children, adolescents, and adults. This study proposes a detailed methodology for the diagnosis of affective disorders in individuals diagnosed with epilepsy, thereby contributing to a more nuanced understanding and manage
Keywords serve as a concise, high-level summary of an article’s content. Frequently occurring keywords help pinpoint the central themes and emerging trends in a research field. Based on the keyword co-occurrence and cluster analysis by VOSviewer, the main current research trends include quality-of-life and high-risk factors in comorbid epilepsy with depression patients, depression in epilepsy patients caused by family factors, anxiety in patients with epilepsy and electroconvulsive therapy (ECT) for depression.
Quality of life is a broad-ranging and complex concept that affects a person’s physical health, psychological state, social relationships, and relationships with salient features of their environment in a complex way[40]. Previous studies have shown that compared to healthy people, patients with epilepsy have less social support, lower rates of employment, and less social engagement[41-43]. These factors reduce quality of life. Siarava et al[44] reported that 1 in 4 patients with epilepsy suffer from major depressive disorder. Studies have confirmed that higher rates of depression and anxiety are present in patients with epilepsy, which affects social cognition, further lowering the quality of life of patients[45,46].
Furthermore, compared to the general population, depression can even lead to suicidal ideation, which may be connected to depression[47,48]. Another important cause of depression in patients with epilepsy is adverse reactions to antiseizure drugs, such as barbiturates, phenytoin, and vigabatrin[49,50]. The presence of depression and the negative impacts of antiseizure drugs significantly affected the quality of life in patients[44].
Epilepsy often results in the loss of dignity. Consequently, patients with epilepsy might attribute their unemployment, absence of friendships, or relationship challenges to their condition. This attributional style has been associated with the development of depression[51]. While psychosocial factors are acknowledged contributors, the elevation in depression rates among individuals with epilepsy, as opposed to those suffering from other neurological and chronic medical conditions, may predominantly be attributed to underlying risk factors. These include genetic predispositions, as well as endocrine and metabolic anomalies, suggesting a complex interplay of biological mechanisms influencing the prevalence of depression in this population[50]. In addition, depression is the most commonly seen psychiatric comorbidity in patients diagnosed with temporal lobe epilepsy, particularly those exhibiting hippocampal sclerosis[52]. Co-occurrence of temporal lobe epilepsy with hippocampal sclerosis and major depression is common in the clinic[53]. Visoná de Figueiredo et al[54] reported that 34.5% of patients with comorbid TEL and depression presented with hippocampal sclerosis as the structural substrate. Therefore, according to a meta-analysis by Cai et al[55], hippocampal sclerosis may be viewed as a significant risk factor for depression in patients with temporal lobe epilepsy.
ECT, a rapidly effective treatment for depression, has evolved over several decades[56]. ECT was employed as a treatment modality in patients with severe depression characterized by suicidal ideation or the presence of psychotic symptoms[57]. Several previous studies have shown that the quality of life of people with depression improved after ECT treatment, and this effect persisted for a long time[58]. Patients with depression who received ECT tended to have greater improvements in health-related quality of life than hospitalized patients with depression who received only antidepressants[59]. Moreover, Güney et al[60] reported that among patients with depression, male and female patients of all ages whose health-related quality of life significantly improved after treatment with ECT.
Moreover, they also found that compared with younger patients, elderly patients experienced greater improvements in mental health and social functioning after ECT, consistent with previous studies[60,61]. Although ECT is an effective treatment for depression, its disadvantage is that it is associated with side effects related to cognitive function, such as impaired learning and memory[62]. Therefore, patients should be informed of the risks and adverse effects associated with ECT, and patients must be thoroughly informed about the potential risks and adverse effects associated with ECT. Providing written information to both patients and their families is crucial, as it compensates for the possibility that patients might not retain verbal explanations over time.
Epilepsy and depression have a bidirectional relationship, and the two conditions often co-occur. To our knowledge, this is the first bibliometric analysis of epilepsy and depression research. This study conducted a bibliometric evaluation of the total scientific contributions in the fields from 2014 to 2023. We identified important publications, authors, journals, institutions, and countries and further analyzed the research network. Our study revealed that quality of life and stigma in patients with epilepsy comorbid with depression are possible future hot topics and directions in the field of epilepsy and depression research.
We thank Dr. Yi Zhou for his valuable academic advice.
| 1. | Löscher W, Potschka H, Sisodiya SM, Vezzani A. Drug Resistance in Epilepsy: Clinical Impact, Potential Mechanisms, and New Innovative Treatment Options. Pharmacol Rev. 2020;72:606-638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 537] [Cited by in RCA: 480] [Article Influence: 96.0] [Reference Citation Analysis (0)] |
| 2. | Chi G, Huang Z, Li X, Zhang K, Li G. Substance P Regulation in Epilepsy. Curr Neuropharmacol. 2018;16:43-50. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fèvre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gonzalez-Medina D, Gosselin R, Grainger R, Grant B, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Laden F, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Levinson D, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mock C, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O’Donnell M, O’Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leòn FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiebe N, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD, AlMazroa MA, Memish ZA. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197-2223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5870] [Cited by in RCA: 6060] [Article Influence: 466.2] [Reference Citation Analysis (0)] |
| 4. | Guerreiro CA. Epilepsy: Is there hope? Indian J Med Res. 2016;144:657-660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Beghi E. The Epidemiology of Epilepsy. Neuroepidemiology. 2020;54:185-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 679] [Article Influence: 113.2] [Reference Citation Analysis (0)] |
| 6. | Fiest KM, Sauro KM, Wiebe S, Patten SB, Kwon CS, Dykeman J, Pringsheim T, Lorenzetti DL, Jetté N. Prevalence and incidence of epilepsy: A systematic review and meta-analysis of international studies. Neurology. 2017;88:296-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 710] [Cited by in RCA: 1202] [Article Influence: 133.6] [Reference Citation Analysis (0)] |
| 7. | Keezer MR, Sisodiya SM, Sander JW. Comorbidities of epilepsy: current concepts and future perspectives. Lancet Neurol. 2016;15:106-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 494] [Article Influence: 54.9] [Reference Citation Analysis (0)] |
| 8. | Ioannou P, Foster DL, Sander JW, Dupont S, Gil-Nagel A, Drogon O’Flaherty E, Alvarez-Baron E, Medjedovic J. The burden of epilepsy and unmet need in people with focal seizures. Brain Behav. 2022;12:e2589. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 64] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 9. | Chu SF, Liao KH, Wei L. Increasing Risk of Dementia Among Patients with Subsequent Epilepsy Within 2 Years Post-Traumatic Brain Injury: A Population-Based Case-Control Study. J Multidiscip Healthc. 2024;17:1447-1457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Costagliola G, Orsini A, Coll M, Brugada R, Parisi P, Striano P. The brain-heart interaction in epilepsy: implications for diagnosis, therapy, and SUDEP prevention. Ann Clin Transl Neurol. 2021;8:1557-1568. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 45] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 11. | Perrone V, Veronesi C, Dovizio M, Ancona DD, Andretta M, Bartolini F, Cavaliere A, Chinellato A, Ciaccia A, Cillo M, De Francesco A, Enieri N, Ferrante F, Gentile S, Procacci C, Ubertazzo L, Vercellone A, Lucatelli D, Procaccini M, Degli Esposti L. Analysis of Patients with Focal Epilepsy and Drug-Resistant Epilepsy in Italy: Evaluation of Their Characteristics, Therapeutic Pathway and the Consumption of Healthcare Resources. Clinicoecon Outcomes Res. 2022;14:513-521. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 12. | Maguire MJ, Marson AG, Nevitt SJ. Antidepressants for people with epilepsy and depression. Cochrane Database Syst Rev. 2021;4:CD010682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Ottman R, Lipton RB, Ettinger AB, Cramer JA, Reed ML, Morrison A, Wan GJ. Comorbidities of epilepsy: results from the Epilepsy Comorbidities and Health (EPIC) survey. Epilepsia. 2011;52:308-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Song J, Kim YK. Animal models for the study of depressive disorder. CNS Neurosci Ther. 2021;27:633-642. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 52] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 15. | Hutka P, Krivosova M, Muchova Z, Tonhajzerova I, Hamrakova A, Mlyncekova Z, Mokry J, Ondrejka I. Association of Sleep Architecture and Physiology with Depressive Disorder and Antidepressants Treatment. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 16. | Butler T, Harvey P, Cardozo L, Zhu YS, Mosa A, Tanzi E, Pervez F. Epilepsy, depression, and growth hormone. Epilepsy Behav. 2019;94:297-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 17. | Łukawski K, Gryta P, Łuszczki J, Czuczwar SJ. Exploring the latest avenues for antiepileptic drug discovery and development. Expert Opin Drug Discov. 2016;11:369-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Vecera CM, C Courtes A, Jones G, Soares JC, Machado-Vieira R. Pharmacotherapies Targeting GABA-Glutamate Neurotransmission for Treatment-Resistant Depression. Pharmaceuticals (Basel). 2023;16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 19. | Benson KL, Bottary R, Schoerning L, Baer L, Gonenc A, Eric Jensen J, Winkelman JW. (1)H MRS Measurement of Cortical GABA and Glutamate in Primary Insomnia and Major Depressive Disorder: Relationship to Sleep Quality and Depression Severity. J Affect Disord. 2020;274:624-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 20. | Josephson CB, Lowerison M, Vallerand I, Sajobi TT, Patten S, Jette N, Wiebe S. Association of Depression and Treated Depression With Epilepsy and Seizure Outcomes: A Multicohort Analysis. JAMA Neurol. 2017;74:533-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 137] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 21. | Mula M. Depression in epilepsy. Curr Opin Neurol. 2017;30:180-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 22. | Zuo C, Cao H, Song Y, Gu Z, Huang Y, Yang Y, Miao J, Zhu L, Chen J, Jiang Y, Wang F. Nrf2: An all-rounder in depression. Redox Biol. 2022;58:102522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 69] [Reference Citation Analysis (0)] |
| 23. | Kanner AM. Depression in epilepsy: prevalence, clinical semiology, pathogenic mechanisms, and treatment. Biol Psychiatry. 2003;54:388-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 334] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 24. | Jhaveri DJ, McGonigal A, Becker C, Benoliel JJ, Nandam LS, Soncin L, Kotwas I, Bernard C, Bartolomei F. Stress and Epilepsy: Towards Understanding of Neurobiological Mechanisms for Better Management. eNeuro. 2023;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 25. | Paredes-Aragón E, Ruiz-Garcia R, Burneo JG. [Depression in patients with epilepsy. Pathophysiological and clinical concepts and therapeutic strategies]. Rev Neurol. 2023;76:137-146. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Cui Y, Mou J, Liu Y. Bibliometric and visualized analysis of research on e-commerce journals. ICEC17: Proceedings of the International Conference on Electronic Commerce; 2017 Aug 17; USA. New York: Association for Computing Machinery, 2017: 1-7. [DOI] [Full Text] |
| 27. | Ninkov A, Frank JR, Maggio LA. Bibliometrics: Methods for studying academic publishing. Perspect Med Educ. 2022;11:173-176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 372] [Article Influence: 124.0] [Reference Citation Analysis (0)] |
| 28. | Xu Y, Cao Z, Chen T, Ren J. Trends in metabolic dysfunction in polycystic ovary syndrome: a bibliometric analysis. Front Endocrinol (Lausanne). 2023;14:1245719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Wu H, Li Y, Tong L, Wang Y, Sun Z. Worldwide research tendency and hotspots on hip fracture: a 20-year bibliometric analysis. Arch Osteoporos. 2021;16:73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 119] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 30. | Wang Y, Huo X, Li W, Xiao L, Li M, Wang C, Sun Y, Sun T. Knowledge Atlas of the Co-Occurrence of Epilepsy and Autism: A Bibliometric Analysis and Visualization Using VOSviewer and CiteSpace. Neuropsychiatr Dis Treat. 2022;18:2107-2119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 31. | Bølling-Ladegaard E, Dreier JW, Kessing LV, Budtz-Jørgensen E, Lolk K, Christensen J. Directionality of the Association Between Epilepsy and Depression: A Nationwide Register-Based Cohort Study. Neurology. 2023;100:e932-e942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 28] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 32. | Sebera F, Dedeken P, Garrez I, Umwiringirwa J, Leers T, Ndacyayisenga JP, Mutungirehe S, Ndayisenga A, Niyonzima O, Umuhoza G, Teuwen DE, Boon PAMJ. Association of depression and epilepsy in Rwanda: A prospective longitudinal study. Epilepsy Behav. 2023;138:108993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 33. | Karceski S. Epilepsy and Depression: How Are They Related? Neurology. 2023;100:e995-e997. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 34. | Qin SK, Yang ZX, Guan ZW, Zhang JH, Ping X, Lu Y, Pei L. Exploring the association between epilepsy and depression: A systematic review and meta-analysis. PLoS One. 2022;17:e0278907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 35. | Hao X, Zhou D, Li Z, Zeng G, Hao N, Li E, Li W, Deng A, Lin M, Yan B. Severe psychological distress among patients with epilepsy during the COVID-19 outbreak in southwest China. Epilepsia. 2020;61:1166-1173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 101] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 36. | Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 236] [Cited by in RCA: 372] [Article Influence: 93.0] [Reference Citation Analysis (0)] |
| 37. | Tashakori-Miyanroudi M, Souresrafil A, Hashemi P, Jafar Ehsanzadeh S, Farrahizadeh M, Behroozi Z. Prevalence of depression, anxiety, and psychological distress in patients with epilepsy during COVID-19: A systematic review. Epilepsy Behav. 2021;125:108410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 38. | Reilly C, Muggeridge A, Cross JH. The perceived impact of COVID-19 and associated restrictions on young people with epilepsy in the UK: Young people and caregiver survey. Seizure. 2021;85:111-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 39. | Barry JJ, Ettinger AB, Friel P, Gilliam FG, Harden CL, Hermann B, Kanner AM, Caplan R, Plioplys S, Salpekar J, Dunn D, Austin J, Jones J; Advisory Group of the Epilepsy Foundation as part of its Mood Disorder. Consensus statement: the evaluation and treatment of people with epilepsy and affective disorders. Epilepsy Behav. 2008;13 Suppl 1:S1-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 161] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 40. | Haraldstad K, Wahl A, Andenæs R, Andersen JR, Andersen MH, Beisland E, Borge CR, Engebretsen E, Eisemann M, Halvorsrud L, Hanssen TA, Haugstvedt A, Haugland T, Johansen VA, Larsen MH, Løvereide L, Løyland B, Kvarme LG, Moons P, Norekvål TM, Ribu L, Rohde GE, Urstad KH, Helseth S; LIVSFORSK network. A systematic review of quality of life research in medicine and health sciences. Qual Life Res. 2019;28:2641-2650. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 487] [Article Influence: 81.2] [Reference Citation Analysis (0)] |
| 41. | Nazir N, Zafar MS, Akram MN, Khokhar M, Yousaf I. Perceived social support and psychological well-being among patients with epilepsy. J Pak Med Assoc. 2023;73:635-637. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 42. | Kariuki SM, Thomas PT, Newton CR. Epilepsy stigma in children in low-income and middle-income countries. Lancet Child Adolesc Health. 2021;5:314-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 43. | Mao L, Wang K, Zhang Q, Wang J, Zhao Y, Peng W, Ding J. Felt Stigma and Its Underlying Contributors in Epilepsy Patients. Front Public Health. 2022;10:879895. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 23] [Reference Citation Analysis (0)] |
| 44. | Siarava E, Hyphantis T, Katsanos AH, Pelidou SH, Kyritsis AP, Markoula S. Depression and quality of life in patients with epilepsy in Northwest Greece. Seizure. 2019;66:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 45. | Yogarajah M, Mula M. Social cognition, psychiatric comorbidities, and quality of life in adults with epilepsy. Epilepsy Behav. 2019;100:106321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 46. | Schachter SC. Quality of life for patients with epilepsy is determined by more than seizure control: the role of psychosocial factors. Expert Rev Neurother. 2006;6:111-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 47. | Tao K, Wang X. The comorbidity of epilepsy and depression: diagnosis and treatment. Expert Rev Neurother. 2016;16:1321-1333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 48. | Altura KC, Patten SB, Fiest KM, Atta C, Bulloch AG, Jetté N. Suicidal ideation in persons with neurological conditions: prevalence, associations and validation of the PHQ-9 for suicidal ideation. Gen Hosp Psychiatry. 2016;42:22-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 44] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 49. | Mula M, Sander JW. Negative effects of antiepileptic drugs on mood in patients with epilepsy. Drug Saf. 2007;30:555-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 169] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 50. | Lambert MV, Robertson MM. Depression in epilepsy: etiology, phenomenology, and treatment. Epilepsia. 1999;40 Suppl 10:S21-S47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 183] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 51. | Malik NI, Fatima R, Ullah I, Atta M, Awan A, Nashwan AJ, Ahmed S. Perceived stigma, discrimination and psychological problems among patients with epilepsy. Front Psychiatry. 2022;13:1000870. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 52. | de Figueiredo NSV, Gaça LB, Assunção-Leme IB, Mazetto L, Garcia MTFC, Sandim GB, Alonso NB, Centeno RS, Filho GMA, Jackowski AP, Júnior HC, Yacubian EMT. A pioneering FreeSurfer volumetric study of a series of patients with mesial temporal lobe epilepsy and hippocampal sclerosis with comorbid depression. Psychiatry Res Neuroimaging. 2021;311:111281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 53. | Briellmann RS, Hopwood MJ, Jackson GD. Major depression in temporal lobe epilepsy with hippocampal sclerosis: clinical and imaging correlates. J Neurol Neurosurg Psychiatry. 2007;78:1226-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 54. | Visoná de Figueiredo NS, Jardim AP, Mazetto L, Corso Duarte JT, Comper SM, Alonso NB, da Silva Noffs MH, Scorza CA, Cavalheiro EA, Centeno RS, de Araújo Filho GM, Yacubian EMT. Do Hippocampal Neurons Really Count for Comorbid Depression in Patients With Mesial Temporal Lobe Epilepsy and Hippocampal Sclerosis? A Histopathological Study. Front Integr Neurosci. 2021;15:747237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 55. | Cai L, He Q, Luo H, Gui X, Wei L, Lu Y, Liu J, Sun A. Is depression in patients with temporal lobe epilepsy related to hippocampal sclerosis? A meta-analysis. Clin Neurol Neurosurg. 2023;225:107602. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 56. | Fox CA, McLoughlin DM. Speed of electroconvulsive therapy for depression: Effects of electrode placement. Acta Psychiatr Scand. 2021;143:444-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 57. | Nordanskog P, Hultén M, Landén M, Lundberg J, von Knorring L, Nordenskjöld A. Electroconvulsive Therapy in Sweden 2013: Data From the National Quality Register for ECT. J ECT. 2015;31:263-267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 71] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 58. | Lex H, Nevers SW, Jensen EL, Ginsburg Y, Maixner DF, Mickey BJ. Long-term quality of life in treatment-resistant depression after electroconvulsive therapy. J Affect Disord. 2021;291:135-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 59. | Li M, Yao X, Sun L, Zhao L, Xu W, Zhao H, Zhao F, Zou X, Cheng Z, Li B, Yang W, Cui R. Effects of Electroconvulsive Therapy on Depression and Its Potential Mechanism. Front Psychol. 2020;11:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 60. | Güney P, Ekman CJ, Hammar Å, Heintz E, Landén M, Lundberg J, Nordanskog P, Nordenskjöld A. Electroconvulsive Therapy in Depression: Improvement in Quality of Life Depending on Age and Sex. J ECT. 2020;36:242-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 61. | McCall WV, Prudic J, Olfson M, Sackeim H. Health-related quality of life following ECT in a large community sample. J Affect Disord. 2006;90:269-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 62. | Porter RJ, Baune BT, Morris G, Hamilton A, Bassett D, Boyce P, Hopwood MJ, Mulder R, Parker G, Singh AB, Outhred T, Das P, Malhi GS. Cognitive side-effects of electroconvulsive therapy: what are they, how to monitor them and what to tell patients. BJPsych Open. 2020;6:e40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |