Published online Jun 19, 2024. doi: 10.5498/wjp.v14.i6.930
Revised: May 8, 2024
Accepted: May 16, 2024
Published online: June 19, 2024
Processing time: 85 Days and 23.8 Hours
Preoperative anxiety is a common emotional problem during the perioperative period and may adversely affect postoperative recovery. Emergence agitation (EA) is a common complication of general anesthesia that may increase patient discomfort and hospital stay and may be associated with the development of postoperative complications. Pre-anesthetic anxiety may be associated with the development of EA, but studies in this area are lacking.
To determine the relationship between pre-anesthetic anxiety and EA after radical surgery in patients with non-small cell lung cancer (NSCLC).
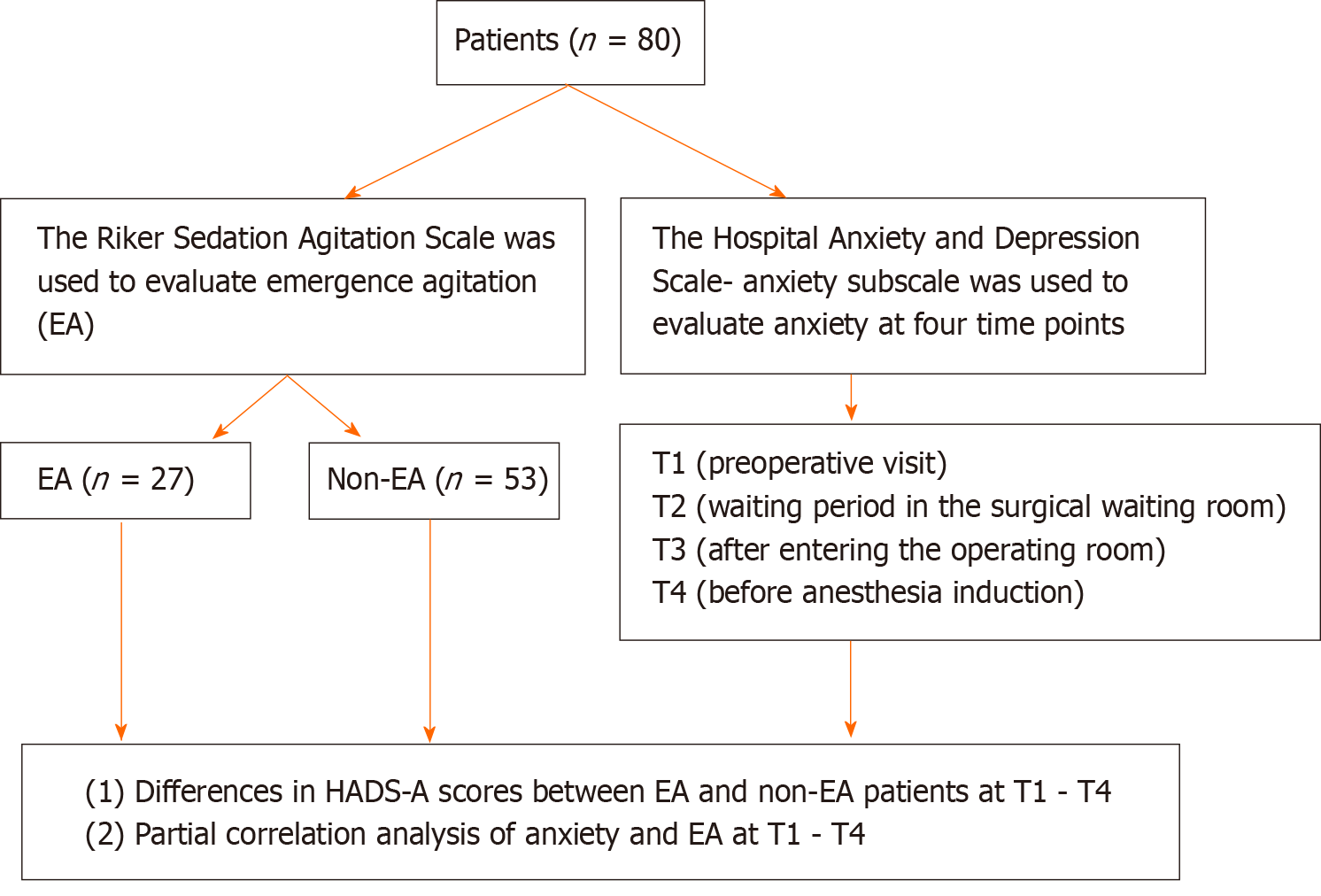
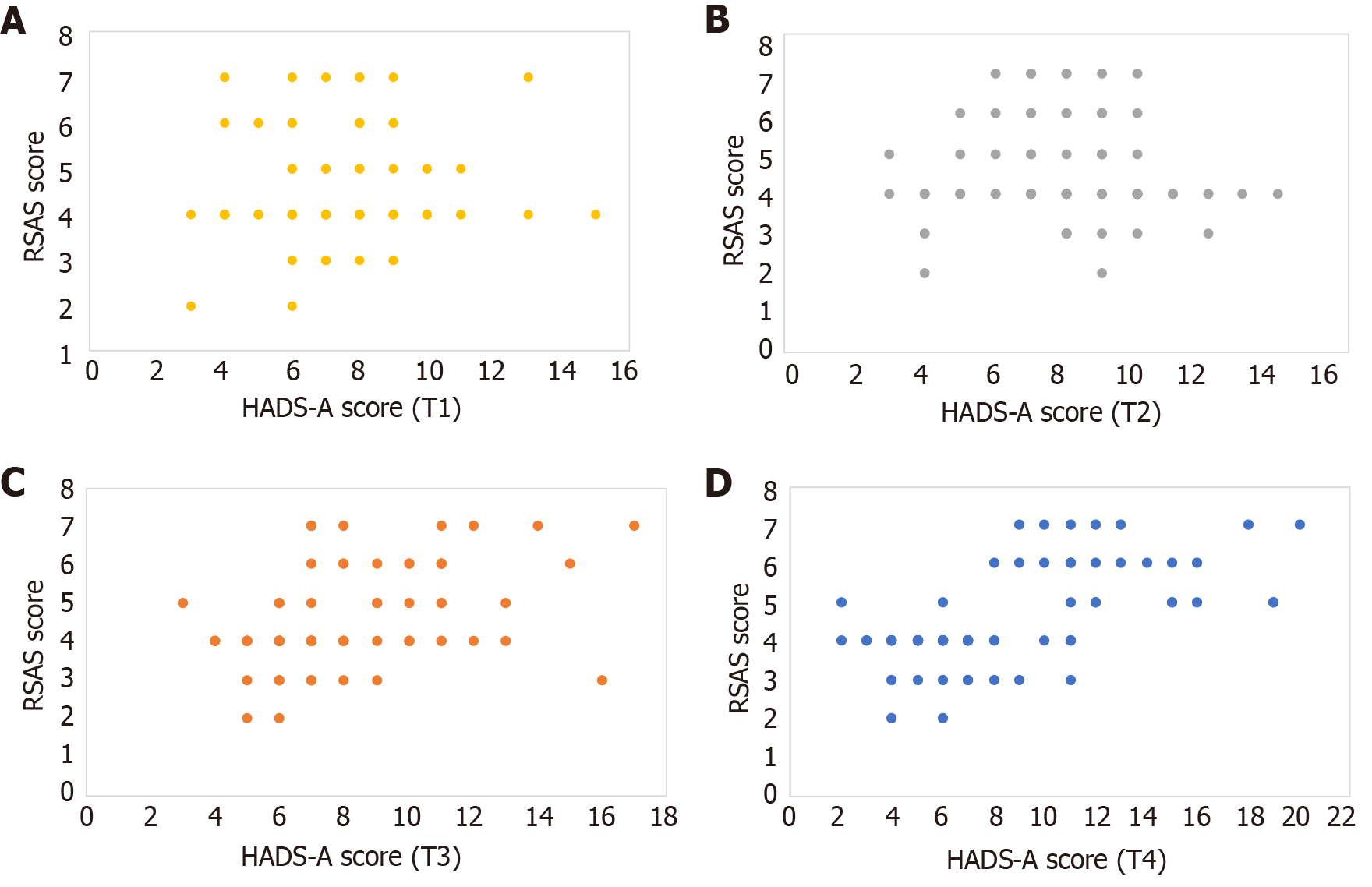
Eighty patients with NSCLC undergoing surgical treatment between June 2020 and June 2023 were conveniently sampled. We used the Hospital Anxiety and Depression Scale’s (HADS) anxiety subscale (HADS-A) to determine patients’ anxiety at four time points (T1-T4): Patients’ preoperative visit, waiting period in the surgical waiting room, after entering the operating room, and before anesthesia induction, respectively. The Riker Sedation-Agitation Scale (RSAS) examined EA after surgery. Scatter plots of HADS-A and RSAS scores assessed the correlation between patients’ pre-anesthesia anxiety status and EA. We performed a partial correlation analysis of HADS-A scores with RSAS scores.
NSCLC patients’ HADS-A scores gradually increased at the four time points: 7.33 ± 2.03 at T1, 7.99 ± 2.22 at T2, 8.05 ± 2.81 at T3, and 8.36 ± 4.17 at T4. The patients’ postoperative RSAS score was 4.49 ± 1.18, and 27 patients scored ≥ 5, indicating that 33.75% patients had EA. HADS-A scores at T3 and T4 were significantly higher in patients with EA (9.67 ± 3.02 vs 7.23 ± 2.31, 12.56 ± 4.10 vs 6.23 ± 2.05, P < 0.001). Scatter plots showed the highest correlation between HADS-A and RSAS scores at T3 and T4. Partial correlation analysis showed a strong positive correlation between HADS-A and RSAS scores at T3 and T4 (r = 0.296, 0.314, P < 0.01).
Agitation during anesthesia recovery in patients undergoing radical resection for NSCLC correlated with anxiety at the time of entering the operating room and before anesthesia induction.
Core Tip: This study explored the relationship between anxiety and awakening agitation at four time points (patients’ preoperative visit, waiting period in the surgical waiting room, after entering the operating room, and before anesthesia induction), and clarified that emergence agitation in patients undergoing radical surgery for non-small cell lung cancer was related to anxiety at the time of entering the operating room and before anesthesia induction. This finding provides new insights into the management of preoperative anxiety and prevention of postoperative agitation, which can help improve postoperative recovery.
- Citation: Yan F, Yuan LH, He X, Yu KF. Correlation between pre-anesthesia anxiety and emergence agitation in non-small cell lung cancer surgery patients. World J Psychiatry 2024; 14(6): 930-937
- URL: https://www.wjgnet.com/2220-3206/full/v14/i6/930.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i6.930
The pathogenesis of lung cancer involves various factors, including smoking, environmental pollution, occupational exposure, exposure to radioactive substances, chronic lung diseases, genetic factors, and decreased immune system function[1,2]. Clinically, treatment strategies for non-small cell lung cancer (NSCLC) are diverse, with surgical resection being the most common and recommended treatment[3]. General anesthesia is commonly used for radical NSCLC surgery and can assist in the smooth implementation of surgery. However, there have been reports indicating the occurrence of emergence agitation (EA) after general anesthesia[4]. EA is an adverse reaction to general anesthesia, characterized by a state of consciousness and behavioral dissociation during the recovery period, manifested as excitement, agitation, disorientation, and inappropriate behavior. It can pose many risks to patients, including falls, bleeding, accidental extubation, and increased hospital costs, adding to the workload of healthcare providers[5].
Excessive stress response, characterized by anxiety, depression, and elevated blood pressure, is the main cause of postoperative EA in patients under general anesthesia. Patients with NSCLC face a higher risk of recurrence and metastasis after undergoing surgical resection[6], often requiring postoperative treatments, such as radiation and chemotherapy. This may lead to psychological stress owing to concerns about the success rate of the surgery and the financial burden, resulting in anxiety, depression, and other negative psychological states. Anxiety is the result of the comprehensive interaction of physiological, psychological, and social factors, which may cause patients to experience intense, excessive, and persistent worries and fears accompanied by physiological panic reactions such as increased heart and respiratory rates[7]. Excessive pre-operative anxiety and tension can increase the risk of developing EA[8].
Several studies have been conducted on children with preoperative anxiety assessment using the modified Yale Anxiety Scale[9,10]. One study has shown a certain positive correlation between preoperative anxiety and postoperative EA[9]. However, owing to the lack of standardized assessment criteria for preoperative anxiety in adults, research in this area is lacking. Furthermore, reports on the relationship between preoperative anxiety and EA mainly involve orthopedic surgery, nasal surgery, and coronary intervention surgery, with few studies focusing on cancer, particularly radical surgery[11,12]. Therefore, this study focused on analyzing the correlation between pre-anesthetic anxiety and EA in patients with NSCLC undergoing surgery under general anesthesia.
Using convenience sampling, 80 patients with NSCLC who underwent surgical treatment between June 2020 and June 2023 were selected.
The inclusion criteria included the following: (1) Definitive diagnosis of NSCLC undergoing surgical treatment; (2) Age ≥ 18 years, any gender; and (3) American Society of Anesthesiologists’ physical status classification[13] of grade I or II.
The exclusion criteria included the following: (1) Patients with psychiatric disorders, history of substance abuse, or drug addiction; (2) Patients requiring rescue interventions such as cardiac arrest or multiple organ dysfunction syndrome during surgery; (3) Patients with severe impairment in liver, kidney, heart, or lung function; (4) Patients with visual or auditory impairments before surgery; (5) Patients with tumor metastasis or concurrent malignant tumors; (6) Patients receiving preoperative adjuvant therapies such as radiation or chemotherapy; and (7) Pregnant or lactating women.
Anxiety: The Hospital Anxiety and Depression Scale (HADS) is used to screen patients for anxiety and depression in general hospital patients[14]. We used the HADS’ anxiety subscale (HADS-A) comprising 7 items to measure patients’ anxiety, with each item rated on a four-point scale from 0 to 3. Specifically, a score of 0 indicates no presence of symptoms and 1 indicates mild presence of symptoms, with little or no impact on the individual being assessed, or a mild impact. A score of 2 indicates a moderate presence of symptoms, with some impact on the individual being assessed, and 3 indicates a severe presence of symptoms, with significant frequency and intensity and a severe impact on the individual being assessed. If the total score is 8 or higher, the patient is considered to have anxiety[11].
We assessed patients’ anxiety levels at four time points, as follows. T1 (preoperative visit): One day before surgery, a preoperative visit was conducted, informed consent was obtained, communication with the patient was conducted, and the HADS-A was administered. T2 (waiting period in the surgical waiting room): Inside the operating room waiting area, the HADS-A was administered after the patients experienced preoperative fasting, in an unfamiliar operating room environment, and with unfamiliar operating room staff. T3 (after entering the operating room): All patients completed the HADS-A when escorted into the operating room by the operating room nurse and anesthesiologist. T4 (before anesthesia induction): The HADS-A was administered when the mask was placed on the patient’s face before anesthesia induction.
Emergence agitation: The Riker Sedation Agitation Scale (RSAS) is used to assess sedation and agitation in post-anesthesia recovery patients. Therefore, we used the RSAS to evaluate patients’ EA status. This scale primarily grades the level of agitation based on the behavioral manifestations of patients during the recovery period, using a seven-point scoring system, with a score of 5 or higher indicating the occurrence of EA[15]. Further details are presented in Table 1.
| Point | Classify | Describe |
| 1 | Can't be awakened | The patient has a mild or no response to stimuli and is unable to communicate or follow instructions |
| 2 | Very calm | The patient responds to somatic stimuli but is unable to communicate and follow instructions |
| 3 | Calm | The patient is drowsy, can be awakened by verbal stimulation or gentle shaking, and can obey simple commands |
| 4 | Quiet cooperation | The patient is quiet, easily aroused, and obeys instructions |
| 5 | Agitation | The patient is anxious or physically agitated, tries to roll over and get up, can be quieted by verbal cues to discourage him or her |
| 6 | Very agitated | The patient requires protective restraint and repeated verbal prompts to discourage |
| 7 | Dangerous agitation | The patient pulls on the endotracheal tube, attempts to remove the internal catheter, rolls over the bed rails, unconsciously assaults healthcare workers, and struggles to roll over in the bed, requiring forcible restriction of his movements |
Before surgery, the doctor established an intravenous access for the patient, monitored vital signs, and induced intravenous anesthesia using Sufentanil Citrate Injection (0.1-5.0 μg/kg, iv), Atracurium Besylate Injection (0.2 mg/kg, iv), and Propofol Medium/Long Chain Fat Emulsion Injection (2 mg/kg, iv). After the patient received oxygen through a face mask, a double-lumen endotracheal tube was placed under direct vision with a disposable adult video laryngoscope using a fiberoptic bronchoscope for precise positioning. Once successfully positioned, the anesthesia machine was connected, and anesthesia was maintained by continuous inhalation of sevoflurane (National Drug Approval H20080681) at a flow rate of 2 L/min. Throughout the surgery, the doctor continuously infused the Sufentanil Citrate Injection (0.15-0.7 μg/kg) based on the patient’s condition, with intermittent additional doses of Atracurium Besylate as needed to maintain muscle relaxation. The patient’s tidal volume was adjusted to 6-8 mL/kg, inspiration-to-expiration ratio was set at 1:2, peak airway pressure was kept below 30 cmH2O, respiratory rate was maintained at 12-20 breaths per minute, central venous pressure was maintained at 5-12 cmH2O, mean arterial pressure was maintained above 65 mmHg, and urine output was ensured to be greater than 0.5 mL/kg/h. Vasopressors were used to maintain blood pressure within 20% of the baseline level. All patients underwent temperature monitoring and management. After surgery, patients were provided with intravenous patient-controlled analgesia with weak opioids and non-steroidal anti-inflammatory drugs, along with multimodal analgesia involving the combined use of various drugs to reduce the dosage of individual medications.
Observation index: (1) HADS-A scores from T1 to T4; (2) RSAS score and incidence of EA; (3) Differences in HADS-A scores between EA and non-EA patients; and (4) After controlling for age and Numerical Rating Scale (NRS) score, partial correlation analysis between anxiety state and EA. NRS is a numerical representation of pain intensity in which the patient is asked to express the intensity of pain with a number (0-10).
We first entered the collected data into Excel for double-checking and analysis; then, we imported it into SPSS 23.0, a statistical software for data analysis. Descriptive statistics using mean ± SD were employed for continuous data, and t-tests were conducted. For categorical data, proportions and frequencies were used and chi-square tests were performed. We created scatter plots of HADS-A and RSAS scores at four time points (T1-T4) to understand whether there was a correlation between pre-anesthesia anxiety levels and EA at these time points. After controlling for the relevant factors, we conducted a partial correlation analysis.
The flow chart of our study is shown in Figure 1.
The HADS-A scores of NSCLC patients gradually increased in all four time points T1~T4, starting from an average of 7.33 ± 2.03 at T1, 7.99 ± 2.22 at T2, 8.05 ± 2.81 at T3, and 8.36 ± 4.17 at T4.
The RSAS score of 80 patients with NSCLC after surgical treatment was 4.49 ± 1.18. A total of 27 patients scored ≥ 5 points, indicating that EA occurred in 33.75% of patients, as shown in Table 2.
| Point | n | % |
| 1 | 0 | 0 |
| 2 | 2 | 2.5 |
| 3 | 8 | 10 |
| 4 | 43 | 53.75 |
| 5 | 10 | 12.5 |
| 6 | 10 | 12.5 |
| 7 | 7 | 8.75 |
| Sum | 80 | 100.00 |
The HADS-A scores at T3 and T4 were significantly higher in patients with EA (P < 0.05), as shown in Table 3.
| Time | EA (n = 27) | non-EA (n = 53) | t | P value |
| T1 | 7.59 ± 2.10 | 7.19 ± 2.41 | -0.739 | 0.462 |
| T2 | 7.63 ± 1.71 | 8.17 ± 2.43 | 1.030 | 0.306 |
| T3 | 9.67 ± 3.02 | 7.23 ± 2.31 | -4.015 | < 0.001 |
| T4 | 12.56 ± 4.10 | 6.23 ± 2.05 | -7.556 | < 0.001 |
A scatter plot of HADS-A scores vs RSAS scores at four time points (Figure 2) showed that the highest correlation between HADS-A and RSAS scores was found at T3 and T4.
After controlling for age and NRS scores, a strong positive correlation was observed between anxiety and EA at T3 and T4, as shown in Table 4.
| Time | Partial correlation analysis | |
| r | P value | |
| T1 | 0.098 | 0.396 |
| T2 | 0.042 | 0.713 |
| T3 | 0.296 | 0.008 |
| T4 | 0.314 | 0.005 |
Anxiety may increase sensitivity to external stimuli by affecting nervous system regulation, making patients more prone to EA. EA also poses risks such as falls and bleeding[5]. Additionally, patients with EA often require physical restraints or medication interventions, which increase the complexity of care and healthcare personnel workload, adding to the healthcare burden[5,16]. Although EA is generally considered short-lived and self-limiting, its long-term effects on patients during their hospital stay and their traditional implications remain unclear.
The relationship between preoperative anxiety and EA has been the focus of interest in both pediatric and adult patients, although relatively more research has been conducted in children[9,17]. Owing to their psychological and physiological development, children exhibit more pronounced fear and anxiety about surgery and anesthesia, which can lead to a higher incidence of EA postoperatively[17]. In a cross-sectional study of 100 pediatric patients undergoing ophthalmic and otolaryngologic surgeries, the overall incidence of EA in children was 30%, with 34.5% in otolaryngologic surgery and 24.4% in ophthalmic surgery. Higher levels of preoperative anxiety were associated with an increased risk of EA (OR = 1.19, 95%CI 1.06-1.33)[18]. Additionally, Gooden et al[19] showed that children with higher preoperative anxiety levels were six times more likely to experience EA than those with lower anxiety levels. Research on the relationship between preoperative anxiety and EA in adult patients is relatively scarce, possibly because adults are generally considered more capable of understanding and coping with surgery and anesthesia processes. However, adult patients may experience preoperative anxiety, which may affect postoperative recovery[20,21]. The assessment and management of preoperative anxiety in adults are equally important; however, more research is needed to explore the relationship between preoperative anxiety and EA in adults, especially in the context of cancer surgery, and effectively managing this issue.
We investigated the anxiety levels of patients with NSCLC during preoperative visits, in the waiting room, after entering the operating room, and before anesthesia induction. We found that patients’ anxiety levels showed an increasing trend, reflecting their growing concerns and fears about surgery as the operation progressed. This is consistent with the study by Kuzminskaitė et al[22], wherein most patients perceive the day of surgery as the most critical and potentially risky moment in their lives, leading to anxiety levels ranging from 11% to 93% and experiencing varying degrees of anxiety before surgery. This anxiety stems from fear of the unknown, concerns about surgical outcomes, and worries about their safety.
Older individuals are also more likely to develop EA. Owing to organ function degeneration, older patients have a lower tolerance to surgery and anesthesia. Postoperative pain is a risk factor for EA[23]. Therefore, after excluding interfering factors such as age and postoperative pain, we found no significant correlation between anxiety levels during preoperative visits or in the preoperative waiting room and the occurrence of EA. However, there was a correlation between anxiety levels after entering the operating room and before anesthesia induction, and EA. This further confirms that preoperative anxiety directly influences the occurrence of EA. The operating room and anesthesia induction process may have a more direct and pronounced impact on patients’ emotions. The unfamiliar environment of the operating room, tense atmosphere before surgery, and effects of anesthetic drugs can trigger more pronounced anxiety in patients, affecting their recovery. Anesthetic agents such as sevoflurane have sedative and hypnotic effects, which may lead to adverse reactions such as agitation during recovery, potentially increasing the risk of emergence agitation when patients experience anxiety while receiving these medications[24].
Therefore, we recommend conducting thorough preoperative visits and patient preparation. During the visit, it is important to actively communicate with the patient and provide detailed information about the anesthesia methods, surgical procedures, and relevant cases to alleviate preoperative anxiety, improve the patient’s emotional state, enhance their positivity for surgery, and prevent emergence agitation due to negative emotions. Before entering the operating room and inducing anesthesia, healthcare professionals can take measures such as deep breathing, relaxation training, and distraction techniques to help patients manage their anxiety. These skills can help patients relax their minds and bodies and reduce their feelings of anxiety.
Anxiety can potentially affect the effectiveness of anesthesia and smooth progression of surgery, and is also associated with EA. By assessing the anxiety levels of patients with NSCLC at multiple time points, we can gain a more comprehensive understanding of the dynamic changes in their anxiety states, confirming that patient EA is related to anxiety levels upon entering the operating room and before anesthesia induction. Compared with existing research, this study may reveal new opportunities for anxiety assessment and intervention timing, offering a fresh perspective for future studies.
| 1. | Chen P, Liu Y, Wen Y, Zhou C. Non-small cell lung cancer in China. Cancer Commun (Lond). 2022;42:937-970. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 351] [Article Influence: 117.0] [Reference Citation Analysis (0)] |
| 2. | Harðardottir H, Jonsson S, Gunnarsson O, Hilmarsdottir B, Asmundsson J, Gudmundsdottir I, Saevarsdottir VY, Hansdottir S, Hannesson P, Gudbjartsson T. [Advances in lung cancer diagnosis and treatment - a review]. Laeknabladid. 2022;108:17-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 3. | Bott MJ, Patel AP, Crabtree TD, Morgensztern D, Robinson CG, Colditz GA, Waqar S, Kreisel D, Krupnicka AS, Patterson GA, Broderick S, Meyers BF, Puri V. Role for Surgical Resection in the Multidisciplinary Treatment of Stage IIIB Non-Small Cell Lung Cancer. Ann Thorac Surg. 2015;99:1921-1928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 4. | Assefa MT, Chekol WB, Melesse DY, Nigatu YA, Bizuneh YB. Incidence and risk factors of emergence delirium in elderly patients after general or spinal anesthesia for both elective and emergency surgery. Ann Med Surg (Lond). 2022;84:104959. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Keffer JH. Quality assurance in home laboratory testing. Clin Lab Med. 1986;6:799-803. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Li Y, Yan B, He S. Advances and challenges in the treatment of lung cancer. Biomed Pharmacother. 2023;169:115891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 143] [Reference Citation Analysis (0)] |
| 7. | Eberhart L, Aust H, Schuster M, Sturm T, Gehling M, Euteneuer F, Rüsch D. Preoperative anxiety in adults - a cross-sectional study on specific fears and risk factors. BMC Psychiatry. 2020;20:140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 99] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 8. | Liu W, Sun R, Gao X, Wang S. Effects of preoperative nasal spray esketamine on separation anxiety and emergence agitation in pediatric strabismus surgery: A randomized clinical trial. Medicine (Baltimore). 2022;101:e32280. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 9. | Ali AB, Khan F. Emergence Delirium and Its Association with Preoperative Anxiety in Paediatric Patients Undergoing Infra Umbilical Surgery Under Combined General and Caudal Anaesthesia: An Observational Study from a Tertiary Care Centre in a South Asian Country. Turk J Anaesthesiol Reanim. 2022;50:129-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Tang X, Zhang M, Yang L, Tao X, Li Y, Wang Y, Wang X, Hu X. Individual cartoon video for alleviating perioperative anxiety and reducing emergence delirium in children: a prospective randomised trial. BMJ Paediatr Open. 2023;7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 11. | Ren A, Zhang N, Zhu H, Zhou K, Cao Y, Liu J. Effects of Preoperative Anxiety on Postoperative Delirium in Elderly Patients Undergoing Elective Orthopedic Surgery: A Prospective Observational Cohort Study. Clin Interv Aging. 2021;16:549-557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Yang KL, Detroyer E, Van Grootven B, Tuand K, Zhao DN, Rex S, Milisen K. Association between preoperative anxiety and postoperative delirium in older patients: a systematic review and meta-analysis. BMC Geriatr. 2023;23:198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 13. | Doyle DJ, Hendrix JM, Garmon EH. American Society of Anesthesiologists Classification. 2023 Aug 17. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed] |
| 14. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28548] [Cited by in RCA: 31822] [Article Influence: 757.7] [Reference Citation Analysis (0)] |
| 15. | Jo JY, Jung KW, Kim HJ, Park SU, Park H, Ku S, Choi SS. Effect of Total Intravenous Anesthesia vs Volatile Induction With Maintenance Anesthesia on Emergence Agitation After Nasal Surgery: A Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg. 2019;145:117-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 16. | Lee SJ, Sung TY. Emergence agitation: current knowledge and unresolved questions. Korean J Anesthesiol. 2020;73:471-485. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 112] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 17. | Zainal Abidin H, Omar SC, Mazlan MZ, Hassan MH, Isa R, Ali S, Hassan SK, Marzuki A. Postoperative Maladaptive Behavior, Preoperative Anxiety and Emergence Delirium in Children Undergone General Anesthesia: A Narrative Review. Glob Pediatr Health. 2021;8:2333794X211007975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Yu H, Sun X, Li P, Deng X. Prevalence and risk factors of emergence agitation among pediatric patients undergo ophthalmic and ENT Surgery: a cross-sectional study. BMC Pediatr. 2023;23:598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 19. | Gooden R, Tennant I, James B, Augier R, Crawford-Sykes A, Ehikhametalor K, Gordon-Strachan G, Harding-Goldson H. [The incidence of emergence delirium and risk factors following sevoflurane use in pediatric patients for day case surgery, Kingston, Jamaica]. Rev Bras Anestesiol. 2014;64:413-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 20. | Aust H, Eberhart L, Sturm T, Schuster M, Nestoriuc Y, Brehm F, Rüsch D. A cross-sectional study on preoperative anxiety in adults. J Psychosom Res. 2018;111:133-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 103] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 21. | Woldegerima Berhe Y, Belayneh Melkie T, Fitiwi Lema G, Getnet M, Chekol WB. The overlooked problem among surgical patients: Preoperative anxiety at Ethiopian University Hospital. Front Med (Lausanne). 2022;9:912743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Kuzminskaitė V, Kaklauskaitė J, Petkevičiūtė J. Incidence and features of preoperative anxiety in patients undergoing elective non-cardiac surgery. Acta Med Litu. 2019;26:93-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Liu Q, Li L, Wei J, Xie Y. Correlation and influencing factors of preoperative anxiety, postoperative pain, and delirium in elderly patients undergoing gastrointestinal cancer surgery. BMC Anesthesiol. 2023;23:78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 20] [Reference Citation Analysis (0)] |
| 24. | Barreto ACTP, Rangel da Rocha Paschoal AC, Barbosa Farias C, Gomes Nogueira Borges PS, Gonelli Albanez da Cunha Andrade R, de Orange FA. [Risk factors associated with anesthesia emergence delirium in children undergoing outpatient surgery]. Braz J Anesthesiol. 2018;68:162-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |