Published online May 19, 2024. doi: 10.5498/wjp.v14.i5.678
Revised: April 13, 2024
Accepted: April 19, 2024
Published online: May 19, 2024
Processing time: 84 Days and 6 Hours
Rectus abdominis separation (DRA) affects pelvic stability and body image. No studies have explored the effects of manual massage on early postpartum DRA and postpartum depression.
To analyze the curative effect of massage on early postpartum DRA and its impact on postpartum depression and thus its ability promote the overall psychosomatic rehabilitation of postpartum women.
Data were retrospectively collected on 70 primiparous women with postpartum DRA who underwent rehabilitation at the Postpartum Rehabilitation Center of Huzhou Maternal and Child Health Hospital from October 2022 to September 2023. The patients were divided into the Group S (35 cases, biomimetic electrical stimulation treatment) and Group L (35 cases, biomimetic electrical stimulation combined with manual massage treatment). Baseline data, the edinburgh po
No significant differences were found in the baseline data, rectus abdominis distance, waist circumference, and VAS and EPDS scores between the two groups before treatment (P > 0.05). After treatment, the distance between rectus abdominis and waist circumference in Group L were significantly smaller than those in Group S (P < 0.05). Furthermore, lower back pain (VAS score) and the EPDS score in Group L were significantly lower than those in Group S (P < 0.05).
Manual massage can significantly reduce early postpartum DRA, waist circumference, and back pain and improve the patient’s mental state and postpartum depression.
Core Tip: Postpartum rectus abdominis separation can cause abdominal distension, difficulty in defecation, and pelvic floor dysfunction. It significantly impacts body image and can lead to negative emotions such as anxiety and inferiority complex in women after childbirth, increasing the incidence of postpartum depression. This study describes the ability of massage in reducing the separation of the rectus abdominis muscle, waist circumference, and lower back pain and improving the patient’s mental state, which helps lower the risk of postpartum depression.
- Citation: Chen Y, Sun XY, Qian C, Zhang XX, Zhou YJ, Zhang HY, Xie ZW. Therapeutic effect of manual massage on early postpartum rectus abdominis separation and postpartum depression. World J Psychiatry 2024; 14(5): 678-685
- URL: https://www.wjgnet.com/2220-3206/full/v14/i5/678.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i5.678
Rectus abdominis separation (DRA) is the abnormal separation of the medial edge of the rectus abdominis muscles on both sides of the abdomen. It usually occurs in middle to late pregnancy and postpartum. The main manifestations include abdominal distension, difficulty in defecation, and pelvic floor dysfunction. No uniform diagnostic criteria for postpartum has been established for DRA. Most scholars regard rectus abdominis distance > 2 cm as DRA[1]. DRA usually resolves moderately within 1-8 wk postpartum[2]. However, without any reasonable therapeutic intervention, approximately 39%-70% of DRA cannot recover spontaneously within 6-8 wk postpartum[3], and approximately 39%-45% of DRA cases persist within half a year[4]. The persistence of DRA can lead to various problems, such as pelvic instability, back pain, abdominal wall hernia, and internal organ prolapse[5]. DRA creates an abdominal bulge, which can greatly affect body image and lead to emotional disorders, such as low mood and feelings of inferiority in women with postpartum DRA, which increase the risk of postpartum depression. Postpartum depression is a type of mood disorder experienced after birth characterized by depression and extreme emotional distress. In severe cases, hallucinations or suicidal tendencies can develop[6]. Therefore, postpartum rehabilitation should not be limited to the recovery of DRA, pelvic floor strength, and other physical effects of childbirth. Attention should also be paid to the psychological recovery of postpartum women, in order to achieve the holistic rehabilitation of mind and body. Current conservative treatment methods for postpartum DRA in China mainly include life guidance, abdominal muscle group autonomous training, and bionic electrical stimulation. However, the therapeutic effects are often poor due to nonstandard movements, poor compliance, and intolerance to electrical stimulation[7]. Manual massage is an important part of traditional Chinese medicine with a long history. However, manual massage has only been recently integrated in postpartum rehabilitation. This study investigated the effect of manual massage on early postpartum DRA and postpartum depression to confirm the benefit of traditional Chinese medicine massage in postpartum rehabilitation.
Data were retrospectively collected on 70 primiparous women with postpartum DRA who underwent rehabilitative treatment at the Postpartum Rehabilitation Center of Huzhou Maternal and Child Health Hospital from October 2022 to September 2023. The patients were divided according to the rehabilitation treatment method received into the Group S, who were treated with biomimetic electrical stimulation, and Group L, who were treated with a combination of bionic electrical stimulation combined and manual massage (n = 35 per group).
The inclusion criteria were as follows: (1) In line with the “expert consensus on the diagnosis and treatment of postpartum DRA” related diagnostic criteria[8], i.e., the pregnant women were 6-8 wk postpartum, lochia has subsided, and the separation distance of rectus abdominis muscle ≥ 2 cm on ultrasound examination; (2) muscle strength of types Ⅰ and Ⅱ pelvic floor muscles ≥ grade 3; (3) singleton, full-term pregnancy with no macrosomia; (4) no serious systemic complications, such as postpartum hemorrhage and incision infection; (5) no contraindication of electrical stimulation; and (6) signed informed consent form by the patient and family members.
The exclusion criteria were as follows: (1) Mental disorder or mental retardation; (2) pelvic floor disorders; (3) diagnosis of epilepsy; (4) implanted with a cardiac pacemaker; (5) previous abdominal surgery; (6) intestinal adhesion or congenital abdominal wall dysplasia; (7) long-term cough, constipation, and other diseases that increase abdominal pressure; (8) presence of malignant tumors; (9) severe heart, liver, and kidney dysfunction; and (10) unwilling to cooperate with the treatment or lost to follow-up.
All patients were guided by the rehabilitation physician to undergo independent training that included routine rehabilitation exercises, such as supine leg lifting, kneeling abdominal contraction, kneeling leg extension, flat abdominal contraction, and standing abdominal contraction.
Group S, the conventional rehabilitation exercise group, underwent biomimetic electrical stimulation treatment using a biological stimulation feedback instrument (Nanjing Medland Medical Technology Co., Ltd.; model specification: MLD B4). Each patient was placed in a supine position. Electrode sheets were placed on the external and internal oblique muscles, rectus abdominis, and transversus abdominis on both sides of the abdomen. Electrode wires were used to connect six channels and three loops. Muscle tremor, passive contraction, and comfortable tingling sensation were taken as the standard while considering the patient’s tolerance. The best current intensity was then determined. Each stimulation lasted for 30 min. The treatment course was one treatment per day for 10 d. The results were reviewed after 1 course of treatment.
Group L underwent a manual massage in addition to routine rehabilitation exercise and bionic electrical stimulation treatment. Each patient was placed in a supine position and asked to relax the body. The abdomen was exposed while the rest of the body was covered and kept warm. The rehabilitation physician poured an appropriate amount of lavender essential oil to the palm and applied it evenly to the abdomen using the Taiji technique. The abdomen was kneaded 5-8 times, and the pericostal and anterior iliac spine muscles 3-5 times along the direction of the navel. The abdomen was pressed 3-5 times along the navel to the rectus abdominis on both sides. The rectus abdominis was lifted 15 times and the belt vein 8-10 times. The abdomen was encircled, with the Shenque point as the center, and the points of Qimen, Tianshu, and Zhongji were pushed back and forth five times. Point kneading technique was performed according to the Shenshu, Zhongwan, Xiawan, Shenque, Qihai, Guanyuan, Zhongji, Qugu, and Huiyin points. The massage techniques of pressing, kneading, plucking, and rolling were adopted. The acupoints and deep muscle groups were stimulated along the meridian direction of the patient. The muscles on both sides of the waist to the middle were massaged for 20 min each time, The treatment course was one treatment per day for 10 d. The results were reviewed after 1 course of treatment.
The following indicators were evaluated before and after treatment: (1) Distance between rectus abdominis muscles: The distance between the rectus abdominis muscles was measured by color Doppler ultrasound (Siemens Production; model specification: Sonoline G50). Each patient was placed in a supine position with both knees bent at 90°. The hands were placed on both sides of the body. The ultrasonic probe was used to measure the distance between the rectus abdominis muscles at three sites (3 cm above the umbilicus, in the middle of the umbilicus, and 3 cm below the umbilicus). Each site was measured twice, and the average measurement was obtained; (2) abdominal circumference: The abdominal circumferences at the middle of the umbilicus and at 3 cm above and below the umbilicus were measured using a soft ruler. Each section was measured twice, and the average was obtained; (3) lower back pain: The visual analog scale (VAS) was used to evaluate lower back pain in the patients. The possible total score ranged from 0 to 10 points. A higher score indicated greater pain severity[9]; and (4) postpartum depression: The edinburgh postpartum depression scale (EPDS) was used to evaluate postpartum depression. The scale consists of 10 items with a possible total score ranging from 0 to 30 points. The higher the score, the more severe the depression[10].
SPSS 23.0 software was used to analyze and process the data. Count data were expressed as number (percentage). The two groups were compared using the χ2 test. Normally distributed measurement data were expressed as mean ± SD. Comparisons between the groups were performed using student’s t-test. P < 0.05 was considered statistically significant.
The differences between Groups S and L in terms of age, body mass index, delivery method, and pelvic floor muscle strength grade were not significant (P > 0.05; Table 1).
| Baseline data | Group S (n = 35) | Group L (n = 35) | t/χ2 | P value |
| Age (yr) | 28.20 ± 3.76 | 29.66 ± 3.04 | 1.786 | 0.078 |
| Body mass index (kg/m2) | 23.05 ± 2.78 | 22.76 ± 2.75 | 0.439 | 0.662 |
| Delivery method | 0.057 | 0.811 | ||
| Cesarean section | 17 (48.57) | 16 (45.71) | ||
| Spontaneous labor | 18 (51.43) | 19 (54.29) | ||
| Pelvic floor muscle strength grading | 0.473 | 0.789 | ||
| Level 3 | 10 (28.57) | 11 (31.43) | ||
| Level 4 | 19 (54.29) | 20 (57.14) | ||
| Level 5 | 6 (17.14) | 4 (11.43) |
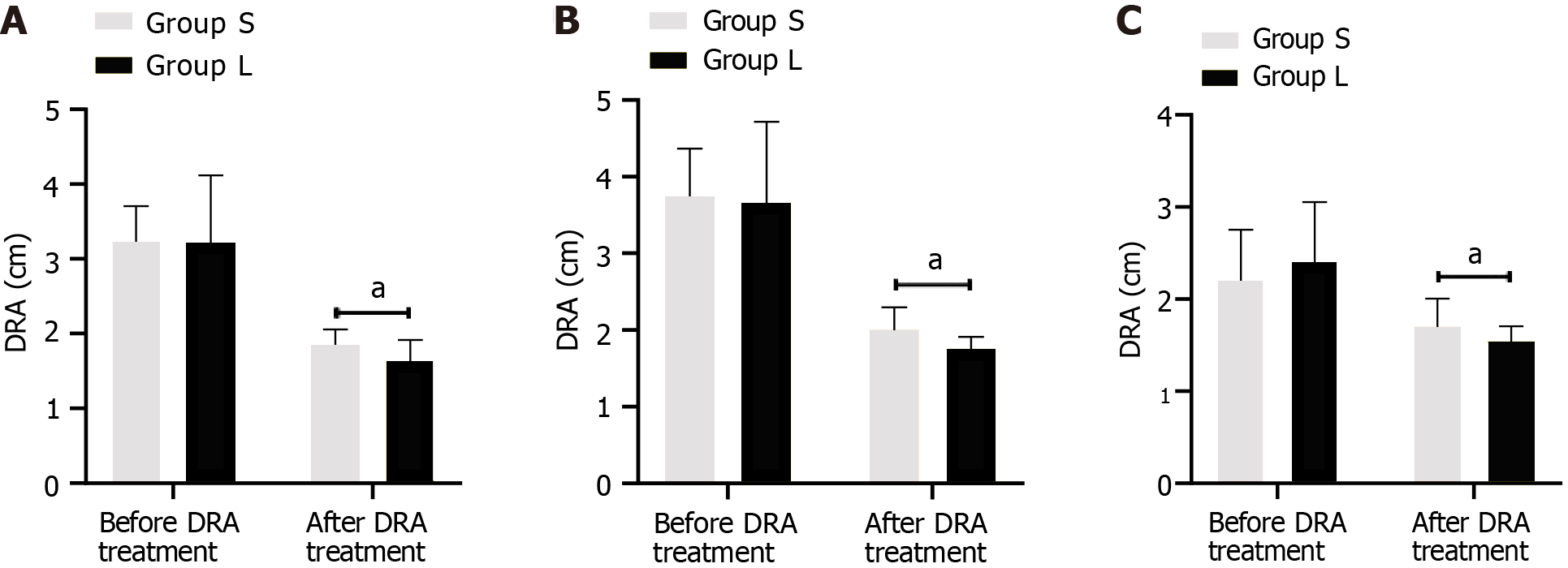
The differences between Groups L and S in the pretreatment distances between the median rectus abdominis, between the rectus abdominis 3 cm above the umbilicus, and between the rectus abdominis 3 cm below the umbilicus in Groups L and S were not significant (P > 0.05). However, the posttreatment distances between the median rectus abdominis, between the rectus abdominis 3 cm above the umbilicus, and between the rectus abdominis 3 cm below the umbilicus in Group L were significantly smaller than those in Group S (P < 0.05; Table 2 and Figure 1).
| Group | n | 3 cm above umbilicus | Navel midline | 3 cm below umbilicus | |||
| Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | ||
| Group S | 35 | 3.24 ± 0.51 | 1.86 ± 0.24 | 3.75 ± 0.66 | 2.01 ± 0.33 | 2.23 ± 0.56 | 1.71 ± 0.32 |
| Group L | 35 | 3.23 ± 0.93 | 1.65 ± 0.31 | 3.67 ± 1.09 | 1.78 ± 0.18 | 2.43 ± 0.66 | 1.55 ± 0.19 |
| t value | 0.056 | 3.169 | 0.371 | 3.777 | 1.367 | 2.486 | |
| P value | 0.996 | 0.002 | 0.711 | < 0.001 | 0.176 | 0.015 | |
No significant differences were observed between Groups S and L in the abdominal circumferences 3 cm above the umbilicus, in the middle of the umbilicus, and 3 cm below the umbilicus before treatment (P > 0.05). However, after treatment, the abdominal circumferences 3 cm above the umbilicus, in the middle of the umbilicus, and 3 cm below the umbilicus in Group L were significantly smaller than those in Group S (P < 0.05; Table 3).
| Group | n | 3 cm above umbilicus | Navel midline | 3 cm below umbilicus | |||
| Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | ||
| Group S | 35 | 83.83 ± 7.08 | 82.86 ± 7.67 | 85.73 ± 7.93 | 84.43 ± 7.73 | 87.26 ± 7.41 | 86.17 ± 7.84 |
| Group L | 35 | 83.29 ± 7.26 | 79.60 ± 4.75 | 84.39 ± 7.36 | 80.90 ± 5.10 | 86.40 ± 7.53 | 82.79 ± 5.43 |
| t value | 0.315 | 2.138 | 0.733 | 2.255 | 0.482 | 2.097 | |
| P value | 0.754 | 0.036 | 0.466 | 0.027 | 0.632 | 0.039 | |
The difference in pretreatment VAS scores for lower back pain between Groups S and L was not significant (P > 0.05). However, after treatment, the lower back pain VAS score in Group L was significantly lower than that in Group S (P < 0.05; Table 4).
| Group | n | Lower back pain VAS score | |
| Before treatment | After treatment | ||
| Group S | 35 | 2.57 ± 1.29 | 1.26 ± 0.74 |
| Group L | 35 | 2.51 ± 1.36 | 0.77 ± 0.59 |
| t value | 0.19 | 3.063 | |
| P value | 0.85 | 0.003 | |
The difference in pretreatment EPDS scores between Groups S and L was not significant (P > 0.05). However, the posttreatment EPDS score in Group L was significantly lower than that in Group S (P < 0.05; Table 5).
| Group | n | EPDS score | |
| Before treatment | After treatment | ||
| Group S | 35 | 9.86 ± 2.37 | 9.03 ± 1.28 |
| Group L | 35 | 9.92 ± 2.41 | 8.24 ± 1.06 |
| t value | 0.105 | 2.812 | |
| P value | 0.917 | 0.006 | |
Physiological changes in the mother during pregnancy, such as elevated progesterone levels and fetal pressure on the uterus, can weaken the elasticity of the skeletal muscle tissue structure and abdominal muscle contraction force, and expand and stretch the bilateral rectus abdominis muscles to both sides, all of which can lead to DRA[11]. The abdominal wall is very important to the human body. If the DRA postpartum cannot be recovered effectively, the abdominal muscles will weaken over time. This muscle weakening has adverse effects on the support of abdominal organs and maintenance of pelvic stability[12]. The long-term persistence of DRA can cause pelvic and lumbar spine injuries and increase lower back pain, which can seriously affect the quality of life and physical and mental health of patients. Therefore, exploring effective treatment methods for early postpartum DRA is of great significance to improving the quality of life post
Biomimetic electrical stimulation promotes abdominal muscle contraction, increase the excitability of the muscles, enhance muscle strength[13], and encourages the convergence of the rectus abdominis muscle toward the abdominal white line. It is commonly used as passive physical therapy for early postpartum DRA. Traditional Chinese medicine classifies postpartum DRA under the category of “tendon meridian.” The disease is located in the abdomen and waist. The abdomen is yin; the waist and back are yang. Treatment should follow the principle of “Yin Ping Yang Mi”[14]. Manual Tuina massage, a traditional Chinese medicine treatment, involves massaging the abdominal muscles through techniques that can promote blood flow, enhance abdominal muscle contraction and elasticity, and maintain the mechanical balance of abdominal muscles. In this study, the distance between the rectus abdominis muscles and abdominal circumference measurements in Group L were significantly smaller than those in Group S after treatment (P < 0.05). This indicates that manual massage as supplement to bionic electrical stimulation therapy can further promote recovery from early postpartum DRA. Biomimetic electrical stimulation awakens muscle proprioceptors and enhances the activity level of separated muscle groups. The combination of massage techniques and back and forth massage performed on the acupoints of Qimen, Tianshu, and Zhongji can retrain the corresponding rectus abdominis muscles inside the acupoints, increase their elasticity and strength, and prevent or treat any muscle atrophy. Meanwhile, massage can also improve blood circulation in the arteries and veins on the abdominal wall and thus improve the distribution of nutrients to the rectus abdominis muscle, thereby enhancing the repair of the rectus abdominis muscles to their normal state. Furthermore, during manual massage, acupoints, such as Shangwan-Shenque-Qugu, are fully lifted and pinched, which help dredge meridians, relieve muscle fatigue, increase ligament elasticity, and improve muscle strength. With the resulting increase in abdominal muscle elasticity and tension, the abdominal shape is gradually improved. At the same time, oil deposition in the body is reduced, thereby inhibiting fat accumulation, improving symptoms of abdominal wall relaxation and swelling, and reducing the abdominal circumference.
Pregnancy and childbirth can both lead to widening and weakening of the lumbar tendon, relaxation of the abdominal skin, and sagging and bulging of the midline, which causes instability in the abdominal core and leads to postpartum lower back pain[15]. Studies have shown that the pathological characteristics of lower back pain in patients with postpartum DRA are mainly caused by abdominal muscle spasm and myofascial incarceration[16]. Tuina can promote analgesic effects by stimulating different levels of targets[17]. Smith et al[18] reported that manual massage can alleviate the pain of childbirth. In the present study, the lower back pain VAS score in Group L was significantly lower than that in Group S (P < 0.05), indicating the enhanced therapeutic effect of manual massage and biomimetic electrical stimulation therapy on lower back pain. This may be related to the therapeutic effects brought about by manual massage through dredging meridians and preserving tendons. Therefore, bionic electrical stimulation therapy combined with manual massage can more effectively promote the healing of inflammation- and pain-causing substances in the body. Meanwhile, this combination treatment can effectively promote abdominal blood circulation, improve muscle tone, reduce stimulation to the lumbar nerves, and relieve symptoms of lower back pain.
The changes in abdominal appearance caused by postpartum DRA can have varying degrees of impact on the emotions of postpartum women, which mainly manifest as lack of interest, low emotions, and depression, among others[19]. This may be related to contemporary women’s pursuit of an ideal body shape. Postpartum DRA induces negative emotions, which will affect patients’ participation in postpartum rehabilitation, which in turn negatively affects the repair of the rectus abdominis muscles, such as further aggravation of the separation and even injury, forming a vicious cycle[20]. In the present study, the posttreatment EPDS score in the Group L was significantly lower than that in the Group S (P < 0.05). This may be related to the relaxation that manual massage can provide. Relaxation can alleviate the postpartum emotional state. Stimulation of the sensory nerve fibers on the skin can relax tense muscles, creating a calming experience. These benefits positively affect mood and improve the overall mental state, in addition to the physical benefits. Manual massage can also improve early postpartum DRA and abdominal circumference indicators and alleviate lower back pain. These positive holistic effects will also help improve the depressive mood in postpartum patients. Kianpour et al[21] found that lavender essential oil can relieve postpartum depression. This is the rationale behind the massage oil used in this study. Typically, essential oil is applied to the patient’s abdomen, and Tai Chi technique is used to massage the abdomen 5-8 times. This technique helps release lavender essential oil molecules, allowing them to float in the air, promoting nasal inhalation. The effect on the limbic system of the brain (the amygdala and hippocampus) in turn has a psychological outcome[22] that promotes positive emotions and alleviates patient anxiety and depression.
This study has some limitations. First, the efficacy of biomimetic electrical stimulation therapy combined with manual massage is significant, but whether long-term DRA will recur remains to be confirmed. Second, the single-center design and small sample size limit the generalizability of the results. Further larger-scale sample involving multiple centers are needed to validate the conclusions derived in this study.
Manual massage has a significant therapeutic effect on early postpartum DRA. Its combination with biomimetic electrical stimulation therapy effectively reduced DRA, waist circumference, and lower back pain. Furthermore, manual massage promoted relaxation, which can alleviate the physical and mental states and improve postpartum depression.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade C, Grade C
Novelty: Grade B, Grade C
Creativity or Innovation: Grade B, Grade B
Scientific Significance: Grade B, Grade C
P-Reviewer: Portero D, Spain; Sharma S, India S-Editor: Qu XL L-Editor: A P-Editor: Zhao S
| 1. | Reinpold W, Köckerling F, Bittner R, Conze J, Fortelny R, Koch A, Kukleta J, Kuthe A, Lorenz R, Stechemesser B. Classification of Rectus Diastasis-A Proposal by the German Hernia Society (DHG) and the International Endohernia Society (IEHS). Front Surg. 2019;6:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 79] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 2. | Fernandes da Mota PG, Pascoal AG, Carita AI, Bø K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther. 2015;20:200-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 129] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 3. | Kamel DM, Yousif AM. Neuromuscular Electrical Stimulation and Strength Recovery of Postnatal Diastasis Recti Abdominis Muscles. Ann Rehabil Med. 2017;41:465-474. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Coldron Y, Stokes MJ, Newham DJ, Cook K. Postpartum characteristics of rectus abdominis on ultrasound imaging. Man Ther. 2008;13:112-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 117] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 5. | Denizoglu Kulli H, Gurses HN. Relationship between inter-recti distance, abdominal muscle endurance, pelvic floor functions, respiratory muscle strength, and postural control in women with diastasis recti abdominis. Eur J Obstet Gynecol Reprod Biol. 2022;279:40-44. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Gopalan P, Spada ML, Shenai N, Brockman I, Keil M, Livingston S, Moses-Kolko E, Nichols N, O'Toole K, Quinn B, Glance JB. Postpartum Depression-Identifying Risk and Access to Intervention. Curr Psychiatry Rep. 2022;24:889-896. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 30] [Reference Citation Analysis (0)] |
| 7. | Hu J, Gu J, Yu Z, Yang X, Fan J, You L, Hua Q, Zhao Y, Yan Y, Bai W, Xu Z, Chen C. Efficacy of Standardized Rehabilitation in the Treatment of Diastasis Rectus Abdominis in Postpartum Women. Int J Gen Med. 2021;14:10373-10383. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Sun X, Li H, Su YY, Li DY, Wang Q. Expert consensus on the diagnosis and treatment of postpartum rectus abdominis separation. Zhongguo Fuchanke Linchuang Zazhi. 2021;22:220-221. [DOI] [Full Text] |
| 9. | Faiz KW. [VAS--visual analog scale]. Tidsskr Nor Laegeforen. 2014;134:323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 92] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 10. | Yu J, Zhang Z, Deng Y, Zhang L, He C, Wu Y, Xu X, Yang J. Risk factors for the development of postpartum depression in individuals who screened positive for antenatal depression. BMC Psychiatry. 2023;23:557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 11. | Gluppe S, Engh ME, Bø K. What is the evidence for abdominal and pelvic floor muscle training to treat diastasis recti abdominis postpartum? A systematic review with meta-analysis. Braz J Phys Ther. 2021;25:664-675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 48] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 12. | Radhakrishnan M, Ramamurthy K. Efficacy and Challenges in the Treatment of Diastasis Recti Abdominis-A Scoping Review on the Current Trends and Future Perspectives. Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Hwang UJ, Jung SH, Kim HA, Kim JH, Kwon OY. Effect of Abdominal Electrical Muscle Stimulation Training With and Without Superimposed Voluntary Muscular Contraction on Lumbopelvic Control. J Sport Rehabil. 2020;29:1137-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Zhai WH, Wang MJ, Zhao YJ, Hu SL, Zhou JM. Treatment of postpartum depression with integrated traditional Chinese and Western medicine nursing and electrical stimulation. World J Clin Cases. 2023;11:7980-7986. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med. 2016;50:1092-1096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 165] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 16. | Sokunbi G, Camino-Willhuber G, Paschal PK, Olufade O, Hussain FS, Shue J, Abjornson C, Zelenty WD, Lebl DR, Cammisa FP, Girardi FP, Hughes AP, Sama AA. Is Diastasis Recti Abdominis Associated With Low Back Pain? A Systematic Review. World Neurosurg. 2023;174:119-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 17. | Liu ZF, Wang HR, Yu TY, Zhang YQ, Jiao Y, Wang XY. Tuina for peripherally-induced neuropathic pain: A review of analgesic mechanism. Front Neurosci. 2022;16:1096734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 18. | Smith CA, Levett KM, Collins CT, Dahlen HG, Ee CC, Suganuma M. Massage, reflexology and other manual methods for pain management in labour. Cochrane Database Syst Rev. 2018;3:CD009290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 19. | Liu Y, Zhu Y, Jiang L, Lu C, Xiao L, Wang T, Chen J, Sun L, Deng L, Gu M, Zheng T, Feng M, Shi Y. Efficacy of electro-acupuncture in postpartum with diastasis recti abdominis: A randomized controlled clinical trial. Front Public Health. 2022;10:1003361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 20. | Gluppe S, Ellström Engh M, Bø K. Primiparous women's knowledge of diastasis recti abdominis, concerns about abdominal appearance, treatments, and perceived abdominal muscle strength 6-8 months postpartum. A cross sectional comparison study. BMC Womens Health. 2022;22:428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Kianpour M, Moshirenia F, Kheirabadi G, Asghari G, Dehghani A, Dehghani-Tafti A. The Effects of Inhalation Aromatherapy with Rose and Lavender at Week 38 and Postpartum Period on Postpartum Depression in High-risk Women Referred to Selected Health Centers of Yazd, Iran in 2015. Iran J Nurs Midwifery Res. 2018;23:395-401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 22. | Jafari-Koulaee A, Elyasi F, Taraghi Z, Sadat Ilali E, Moosazadeh M. A Systematic Review of the Effects of Aromatherapy with Lavender Essential Oil on Depression. Cent Asian J Glob Health. 2020;9:e442. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |