Published online May 19, 2024. doi: 10.5498/wjp.v14.i5.607
Revised: February 6, 2024
Accepted: April 28, 2024
Published online: May 19, 2024
Processing time: 171 Days and 1.1 Hours
Depression, a prevalent and complex mental health condition, presents a significant global health burden. Depression is one of the most frequent mental disorders; deaths from it account for 14.3% of people worldwide. In recent years, the integration of complementary and alternative medicine, including traditional Chinese medicine (TCM), has gained attention as a potential avenue for ad
Core Tip: Traditional Chinese Medicine (TCM) emerges as a promising area for intervention in the face of the global health burden that depression poses. This review scrutinizes the efficacy of TCM in alleviating depression, delving into the intricate mechanisms behind herbal formulations, acupuncture, and mind-body practices. As one of the most prevalent mental disorders worldwide, depression demands innovative approaches, and the integration of complementary and alternative medicine offers a compelling avenue. Through evaluating research studies, clinical trials, and meta-analyses, this review not only assesses the current state of TCM in depression management but also its potential for transformative impact, bridging ancient roots with modern resilience.
- Citation: Yang Y, Chen YK, Xie MZ. Exploring the transformative impact of traditional Chinese medicine on depression: Insights from animal models. World J Psychiatry 2024; 14(5): 607-623
- URL: https://www.wjgnet.com/2220-3206/full/v14/i5/607.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i5.607
Depression, a complex and pervasive mental health disorder, is one of our time's most prevalent and impactful global health challenges. Characterized by persistent sadness, loss of interest or pleasure, and a range of cognitive and physical symptoms, depression profoundly affects an individual's emotional well-being, daily functioning, and overall quality of life. With a global prevalence estimated at over 300 million people, depression is a leading cause of disability worldwide[1]. The first comprehensive statistical study of subthreshold depression prevalence estimates. According to the findings, 11.02% of the population displayed symptoms of mild-to-moderate depression. The youngest age group (14.17%) had the highest prevalence, followed by the oldest (12.95%) and then adults (8.92%)[2]. Depression is one of the most frequent mental disorders; deaths from it make up 14.3% worldwide. It is a multifaceted condition that can manifest in various forms, from mild to severe, and impacts people of all ages and demographics. It affects an individual's personal, professional, and social functioning. Depression can include persistent sorrow, loss of interest, sleep difficulties, and cognitive deficits. These symptoms can lower quality of life, work productivity, relationships, and healthcare use[3].
Depression has high direct healthcare costs, indirect costs from diminished work productivity, and intangible costs from human suffering. Depression has ripple effects on families, communities, and society, emphasizing the need for effective interventions and a thorough understanding of its repercussions[4]. Self-care measures and psychological therapy are recommended for those with mild to moderate depression as an initial course of treatment. Medication may be administered if the patient's condition does not improve. The effectiveness of selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine, paroxetine, and sertraline for this aim is diminished by their potentially harmful side effects[5]. Despite the advancements in conventional treatments, the prevalence of depression and the limitations of existing interventions have led to exploring complementary and alternative approaches, such as traditional Chinese medicine (TCM)[6].
Among these approaches, TCM has garnered attention for its holistic perspective and potential to provide novel avenues for alleviating depressive symptoms. TCM, rooted in ancient Chinese philosophies and practices, offers a holistic framework that views health as a harmonious balance between mind, body, and spirit[7]. This approach emphasizes the interconnection of various bodily systems, environmental factors, emotions, and energy flows. The holistic nature of TCM aligns with the multifaceted manifestations of depression. According to TCM principles, depression can be understood as a disruption in the flow of vital energy, or "qi", as well as imbalances in the yin and yang forces within the body[8]. TCM encompasses a spectrum of modalities, including herbal remedies, acupuncture, dietary therapies, and mind-body practices such as Tai Chi and Qigong, each targeting specific aspects of these imbalances. The integration of these modalities is believed to restore harmony and enhance overall well-being[9].
In recent years, there has been growing interest in evaluating the efficacy of TCM interventions for depression. As conventional treatments may not provide satisfactory outcomes for all individuals, the potential of TCM to offer alternative or complementary strategies is gaining recognition. Several studies have investigated the effects of TCM modalities on depressive symptoms, exploring their mechanisms of action and potential synergies with conventional treatments[10]. By addressing depression through a holistic lens that considers both physiological and psychological factors, TCM presents a unique perspective that has the potential to fill gaps in current treatment paradigms.
This comprehensive review seeks to delve into the existing body of research that examines the efficacy of TCM in alleviating depression. By critically analyzing a wide range of studies, clinical trials, and meta-analyses, this review aims to provide a comprehensive overview of the current state of TCM interventions for depression management. The review aims to contribute to a deeper understanding of TCM's role in mental health care by synthesizing empirical evidence and discussing underlying mechanisms. Additionally, it will shed light on potential areas for further research and integration of TCM modalities into conventional treatment approaches, offering insights into a more holistic and patient-centered approach to depression management.
The goal of TCM, a medical practice with roots dating back at least 2300 years, is a form of alternative medicine that draws on the expertise of Chinese doctors for more than 3500 years. TCM can be divided into two primary classes: preparations and materials. Chinese herbal medicine (CHM) and its various parts are the primary constituents of TCM materials[11]. Most TCM preparations consist of Chinese patent medicine, TCM granules, and various TCM clinical preparations. Although acupuncture and herbal remedies have been used for at least 2,200 years, the first recorded account of Chinese Medicine is found in the Huangdi Neijing (The Yellow Emperor's Inner Classic) from the third century BCE[12].
TCM is deeply rooted in a holistic understanding of health and well-being, guided by key principles and fundamental concepts that have shaped its philosophy for centuries. The concepts of Yin and Yang are central to TCM's worldview, representing opposing yet interconnected forces that are integral to all aspects of existence[13]. Yin embodies darkness, passivity, and coolness, while Yang embodies light, activity, and warmth. Health is seen as the harmonious balance and dynamic interplay between these opposing forces, and any disruption in this balance is thought to lead to illness[14]. Another cornerstone of TCM is the concept of Qi (pronounced "Chee"), often described as vital energy or life force. Qi flows through meridian channels, sustaining all bodily functions and maintaining a harmonious equilibrium. Health is maintained when Qi flows smoothly and unobstructed, but blockages or imbalances in this flow can lead to discomfort or disease. TCM interventions, such as acupuncture and herbal remedies, aim to restore the balanced flow of Qi throughout the body[15].
The Five Elements Theory is another fundamental concept in TCM that illuminates the intricate relationships and interdependencies in the natural world and the human body. This theory identifies five elements – Wood, Fire, Earth, Metal, and Water – each embody distinct qualities, attributes, and associations. These elements are not merely static components but dynamic forces that influence and regulate various aspects of health and well-being[16]. In TCM philosophy, the Five Elements represent universal energies that manifest within the human body and its surroundings. Each element is linked to specific organs, tissues, emotions, seasons, colors, and tastes. The interactions between the elements are characterized by two primary cycles: The Generating Cycle and the Controlling Cycle[17]. The Generating Cycle illustrates how each element nourishes and supports the subsequent one. For instance, Wood generates Fire, Fire generates Earth, Earth generates Metal, and Metal generates Water[18]. On the other hand, the Controlling Cycle elucidates how elements can exert influence over one another, maintaining a harmonious balance. For instance, Wood controls Earth, Earth controls Water, Water controls Fire, Fire controls Metal, and Metal controls Wood[19].
The Five Element Theory is a valuable diagnostic and treatment tool in TCM practice. By analyzing an individual's constitution and identifying patterns of imbalance among the elements, practitioners can tailor interventions to restore harmony and well-being. This holistic approach recognizes the interconnectedness of bodily functions, emotions, and environmental factors, offering a comprehensive perspective on health and illness beyond the physical[20]. As a result, the Five Element Theory plays a pivotal role in guiding TCM practitioners in their pursuit of optimal health and balance for their patients. There are numerous traditional Chinese remedies available that can help restore balance. Acupuncture, moxibustion, and cupping techniques stimulate blood flow to the skin[21]. According to Sankararaman et al[22] Chinese healers recommend a beverage prepared using a wide range of therapeutic herbs or dried animal parts, such as snakes, scorpions, insects, and deer antlers.
TCM is based on the concept of Qi, also known as vital breath, which is believed to flow through meridians that are not visible to the naked eye. According to Ji et al[23], this energy network connects components such as organs, tissues, veins, nerves, cells, atoms, and consciousness. In TCM, there are 12 primary meridians that each correspond to a specific organ. According to Jin et al[24], meridians create additional networks that are not visible. These networks are influenced by circadian rhythms, seasons, and planetary movements.
Music therapy using the five elements: TCM encompasses the five elements of music therapy, a treatment modality rooted in traditional Chinese music and influenced by the philosophical concepts of Yin Yang and the five elements. The five musical tones, namely Jiao, Zhi, Gong, Shang, and Yu, symbolically correspond to the five internal organs, namely the liver, heart, spleen, lung, and kidney, as well as the five associated emotions, namely anger, joy, anxiety, concern, and fear[25]. By balancing the Yin and Yang energies and regulating the circulation of Qi and blood within the human body, this practice has various functions. It can alleviate feelings of depression and nourish the liver, promote a sense of calmness in the heart and mind, regulate Qi and eliminate phlegm, strengthen the spleen and enhance blood nou
In a study, Yang et al[28] employed a combination of five therapeutic components, including music and acupuncture, to treat female individuals diagnosed with depression. The research findings indicate that integrating several therapeutic approaches resulted in a notable decrease in symptoms of sadness, anxiety, and adverse emotional reactions. Patients with post-stroke depression were randomly allocated to the control or treatment groups by Wang et al[29]. Primary care was provided to both groups, while music therapy with five components was given to the therapeutic group. The study discovered that participants' symptoms of depression were reduced by five-element music therapy. Long treatment cycles for depression are unstable and prone to recurrence.
Additionally, antidepressants are costly. Patients sometimes discontinue treatment due to financial hardship and the treatment cycle. The 5 Elements Music therapy is effective for treating depression as it is not limited by time or place, making it more straightforward to accept by sufferers[30].
Emotion-driven therapy: Medical professionals use emotion-led treatment to address patients experiencing abnormal emotions and psychological concerns, such as depression, doubt, anxiety, and low self-esteem. This approach focuses on non-drug interventions that restore the patient's emotional well-being and promote harmony in their overall energy (Qi)[31]. Several treatment methods are available, including environmental adaptation therapy, emotional guidance therapy, and language enlightenment. In their study, Petersson et al[32] implemented psychiatric counseling and mental nursing interventions in patients with depression. The results revealed that these interventions effectively reduced depressive symptoms and anxiety, ultimately improving the patient's overall state of life. Foroughe[33] implemented emotional nursing interventions for patients experiencing post-stroke depression, including providing empathy therapy. The findings indicated that emotional nursing interventions significantly impacted the patient's mental and psychological well-being.
In a study that Kashkouli et al[34] carried out, patients with moderate postpartum depression were divided into intervention and control groups. The control group received standard nursing care, whereas the intervention group received a structured psychological therapy intervention. The study's findings indicate that psychological counseling has demonstrated efficacy in alleviating symptoms of depression.
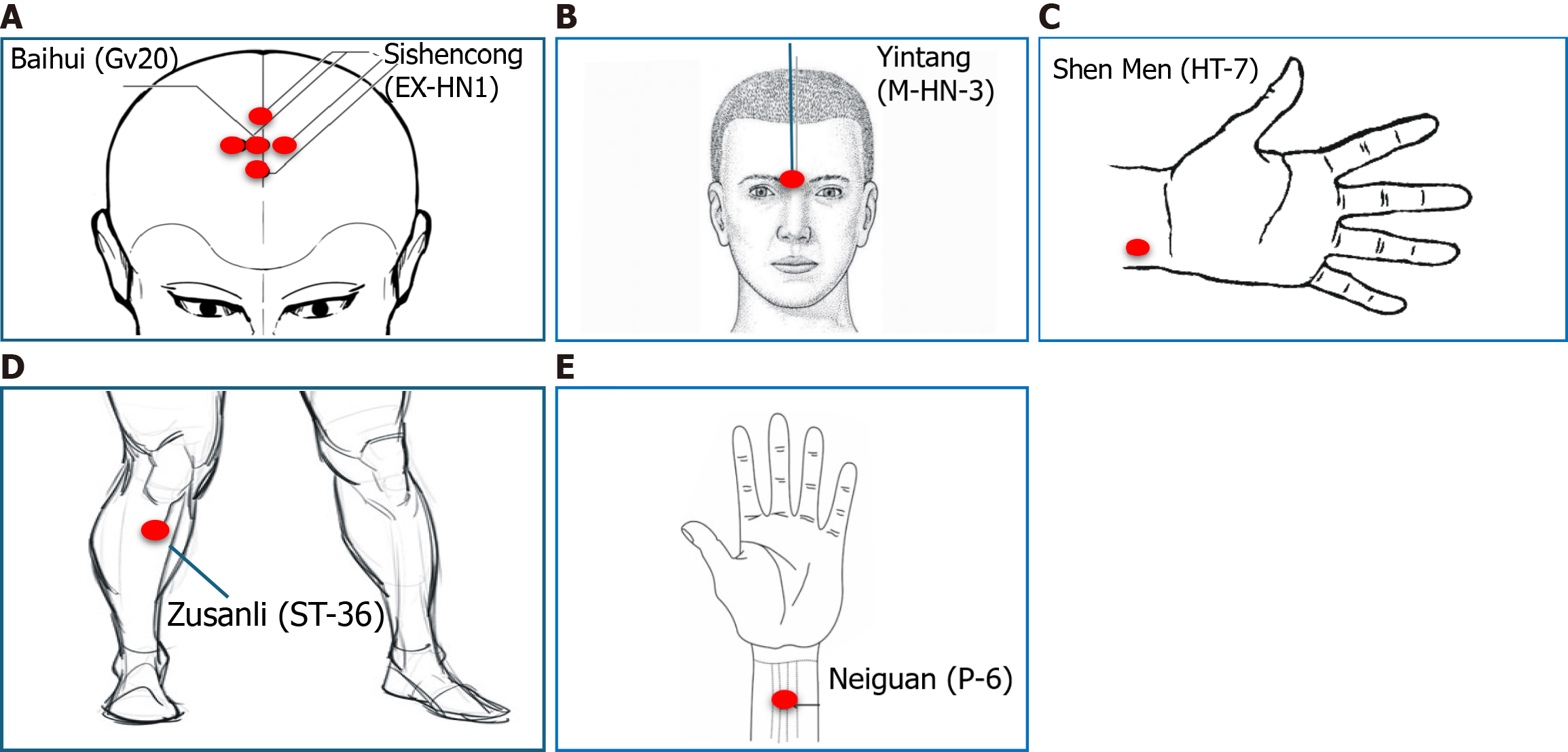
Acupuncture: Acupuncture, a cornerstone of TCM, presents a distinctive therapeutic approach to managing depression. During an acupuncture session, fine needles are meticulously inserted into specific acupoints along the body's meridians, aiming to regulate the flow of Qi, the vital life force. This process is believed to restore the balance of Yin and Yang energies within the body, addressing emotional and physical imbalances contributing to depressive symptoms[35]. By stimulating these acupoints, acupuncture is thought to alleviate the stagnation of Qi and promote its smooth circulation, facilitating the release of endorphins and other neurotransmitters that can enhance mood and alleviate emotional distress[36].
The acupuncture procedure for depression typically involves a personalized approach. Acupoints are carefully selected based on the individual's constitution, symptom presentation, and underlying energetic imbalances. Practitioners may focus on specific acupoints related to emotional well-being, stress reduction, and regulating vital organs such as the liver and spleen[37]. Moreover, acupuncture sessions are often accompanied by relaxation techniques to enhance the therapeutic experience. As a holistic approach, acupuncture addresses the interconnected nature of mind and body, acknowledging that emotional well-being is closely linked to the free flow of energy throughout the body's meridians. The practice of acupuncture in treating depression underscores the integration of Eastern healing wisdom into modern therapeutic strategies for mental health[38].
Acupuncture and associated therapies include acupuncture, electroacupuncture, warm acupuncture, and moxibustion. Acupuncture, often combined with moxibustion, forms a holistic therapeutic approach within TCM, utilizing needle stimulation and applying heat on acupoints by herb (Artemisia moxa cones) to balance Qi and enhance well-being. According to Ou et al[39], the utilization of database retrieval revealed that moxibustion and acupuncture interventions had demonstrated efficacy in reducing the severity of depression among patients diagnosed with depression. In a database analysis of 67 randomized controlled studies, Zhao et al[40] discovered that acupuncture helps alleviate depression problems such as nausea, diarrhea, and sleeplessness. By examining the animal model of depressed people, it was demonstrated that acupuncture could treat primary depression and lessen the adverse reactions of medications. Similarly, Zhao et al[41] conducted randomized trials to determine the effects of acupuncture and SSRIs on treating anxiety, somatization, sleep disturbances, and the depressive symptoms of moderate to severe depression.
A comprehensive meta-analysis involving the systematic search and screening of several databases determined that the combined administration of acupuncture and antidepressants yielded superior efficacy compared to using antidepressants in isolation. Pregnant women with depression received therapy by Abujilban et al[42] with standard care and acupuncture. The outcomes demonstrated that acupuncture was practical and efficient for enhancing mental wellness. Participants with mild to moderate depression have been treated with fluoxetine and ghost point acupuncture by Yang et al[43]. The findings demonstrated that acupuncture and pharmacological therapy can significantly enhance the clinical treatment's impact. Acupuncture offers the advantages of being less expensive and having fewer adverse effects than medication therapy. According to the survey, after six weeks, the effectiveness of various acupuncture treatments for treating depression ranges from 70% to 83.7%, comparable to or even higher than the effectiveness of antidepressant Western medicines. Acupuncture has a unique therapeutic impact on depression[44](Figure 1).
Nutritional therapy: Depression treatment can make use of nutrition. This is crucial because theories suggest that specific nutrients required for the brain's proper operation also impact the neurochemical and biological processes involved in the onset and course of depression. Additionally, there is growing research that links eating habits to the onset of severe depression and emphasizes the value of nutrition in preserving mental health. According to reports, the monoamines glutamate and Gamma-aminobutyric acid (GABA) linked to depression are synthesized due to food[45].
As more noradrenaline, dopamine, and serotonin, all required for mood regulation, are broken down, monoamine oxidase levels are likewise higher in depressed people. Essential for appropriate brain activities, polyunsaturated fatty acids, particularly omega-3 fatty acids, are standard cell membrane elements. The primary forms of -3 fatty acids are -linolenic acid, which is primarily found in plants like canola oil, soy, and walnut, and the long-chain docosahexaenoic and eicosapentaenoic acids, which are most abundant in seafood[46]. Docosahexaenoic and eicosapentaenoic acids are abundant in fish, including sardines, anchovies, herring, mackerel, salmon, trout, and some eggs and animal products. High fish eating has been linked to lower depression risk.
Additionally, Protein insufficiency causes neurotransmitter and cognitive dysfunction. Tyrosine and tryptophan are precursors for synthesizing serotonin, while glutamate is the precursor for glutamate and GABA. Whole grains, almonds, oats, beans, fish, chicken, eggs, cheese, and milk are vital sources of tryptophan and tyrosine[47].
Poor tryptophan diets diminish brain serotonin, causing depression symptoms like anxiety, obsessions, and com
Herbal therapy: In China, Japan, and Korea, CHM plays a crucial role in both TCM and conventional medicine. China's list of essential medications includes CHM injections, pills, capsules, and decoctions. TCM utilizes various herbs' healing properties to enhance the organs' functioning and promote overall wellness[52]. TCM practitioners can harness herbs' healing properties beyond their chemical and physical qualities. The practitioner carefully chooses the herbal mixture that aligns with the body's energy vibration. Chinese herbal formulas incorporate complementary ingredients[53]. TCM herbal formulations comprise plants with a wide range of therapeutic properties to aid the body in regaining balance. The Chinese apothecary categorized each plant part by its curative properties and gave them all names[54].
Sun et al[55] conducted a thorough study of scientific research on the antidepressant properties of herbal medicine and discovered 45 antidepressant herbal products using different in vitro and in vivo investigations. The antidepressant mechanisms may involve the participation of many signaling pathways that regulate the microbiota, endocrine system, antioxidation processes, anti-inflammation responses, neurogenesis, and neurotransmitter activity. Importantly, herbal remedies can alter a broader range of biological pathways and processes to treat depression and prevent the negative consequences of antidepressant medications[56].
Wang et al[57] conducted research using molecular docking and network pharmacology to investigate the mechanism of Sinisan Formula (SNSF) in treating depression. SNSF is a widely recognized TCM formula that comprises four herbs: Licorice (Gancao), Aurantii Fructus Immaturus (Zhishi), Paeoniae Radix Alba (Shaoyao), and Bupleurum chinense (Chaihu). In the SNSF database, 91 active compounds are associated with 112 targets associated with depression. Additionally, SNSF might modulate its antidepressant properties by managing the signaling pathway of neuroactive ligand-receptor, GABA, dopamine, and 5-hydroxytryptamine relationships[58]. Numerous TCM remedies have been reported for their potential efficacy in managing depression.
Baihe, scientifically known as Lilium brownii var. Viridulum possesses properties associated with nourishing Yin and moisturizing the lungs, clearing the heart, and promoting mental tranquillity. Dihuang, scientifically known as Rehmannia glutinosa, contains therapeutic properties such as heat-clearing and blood-cooling actions, Yin nourishment, and fluid generation[59]. The Baihe Dihuang decoction is commonly administered to address cognitive instability, absent-mindedness, agitation, and depressive symptoms. Additionally, brain-derived neurotrophic factor (BDNF), Akt, TrkB-dependent phosphoinositide 3-kinase (PI3K), and mTOR1 synapses may be involved in the critical signal pathways of Baihe Dihuang Decoction in the multi-target treatment of depression and GABAergic and glutamatergic synapses[60]. Lu et al[61] discovered that Baihe Dihuang decoction decreased monoamine oxidase activity in an animal model of chronic mild unpredictable stress, which prevented the breakdown of monoamine neurotransmitters like norepinephrine, 5-hydroxytryptamine, and dopamine and exhibited antidepressant effects.
Jin Si Tao, known as Hypericum monogynum L., is an herbal plant. It is known for its various beneficial effects, including relaxing the liver and alleviating depression, as well as clearing heat and dampness. Additionally, it has properties that can reduce swelling and relieve pain[62]. Sadeghi et al[63] reported that when comparing the two treatments' effects on patients with mild and moderate depression, they discovered that Hypericum perforatum was more effective than antidepressants. Hypericin and several flavonoids were identified as the primary antidepressant components in Jin Si Tao (Hypericum monogynum L.), according to an analysis of clinical data by Gao et al[64]. These compounds may potentially participate in the treatment of depression by exerting inhibitory effects on 5-hydroxytryptamine, monoamine oxidase B, and monoamine oxidase A. Additionally, they control gene expression in the hypothalamus and the hypothalamic-adrenal axis.
The fundamental combination of Shaoyao (Paeonia lactiflora) and Chaihu (Bupleurum) is the basis for prescriptions such as Xiao Chaihu decoction, Sini powder, and Xiaoyao powder. Chaihu (Bupleurum) relieves fever, soothes the liver, relieves depression, and lifts Yang Qi, whereas Shaoyao (Paeonia lactiflora) nourishes blood, collects Yin, soothes the liver, relieves pain, calms the liver, and suppresses Yang[65]. Xie et al[66] study the effects of Shaoyao (Paeonia lactiflora) and Chaihu (Bupleurum) with antidepressants on their chemical, target, and mechanism using network pharmacology and a persistent and unpredictable mild stress rat paradigm. Similarly, Shen and colleagues found that Shaoyao (Paeonia lactiflora) and Chaihu (Bupleurum) regulate arginine and proline metabolism and are antidepressants. Frequent and unstable mild stress develops in a rat depression model[67].
Moreover, Proteomics was employed to study Chaihu (Bupleurum) and Shaoyao's antidepressant mechanisms. The findings imply that this system is linked to neuroprotection, oxidative stress, immunological response, and neuroplasticity[68]. Wu et al[69] discovered in a rat swimming experiment that Bupleurum's primary antidepressant, saikosaponin, has the same effect on depression as fluoxetine on high-dose saikosaponin. The efficiency of Shaoyao (Paeonia lactiflora) extract in depression animal models suggests that paeoniflorin or a combination of the two may be the potent antidepressant component.
Chaihu Shugan San can effectively treat depression by releasing liber-qi stagnation from rage or distress, according to the Chinese medical classic "Jingyue Quanshu". The Chinese herb blends Chaihu Shugan San contains seven distinct herbs: Glycyrrhiza uralensis Fisch (GanCao), Citrus aurantium L (ZhiKe), Cyperus rotundus L (XiangFu), Ligusticum chuanxiong Hort. (ChuanXiong), Paeonia lactiflora Pall. (BaiShao), Citrus reticulata Blanco (ChenPi), Bupleurum chinense DC (CaiHu)[70]. Its antidepressant action may affect several targets and pathways, including potential control of 110 DEPs and neurotransmitter transmission cycles, according to a proteomics study. Kaempferol, luteolin, and quercetin were likely active sub
Kai-Xin-San (KXS) is frequently used to treat depression. Each formula is a concoction of various herbs that are said to function concurrently on a variety of pathogenic targets. Their formulation and dose depend on the symptoms of certain people. When treating complex disorders like depression, TCM's holistic, multidrug, and multi-target approach meshes well with the therapeutic ethos of systems medicine[72]. A meta-analysis used sucrose consumption and 5-HT levels in a depression model to evaluate KXS's depression treatment efficacy. Eight sucrose preference trials included 70 mice; four 5-HT studies contained 38 animals. The KXS trial demonstrated positive results in depression treatment[73]. The information provided by Chen et al[74] leads one to believe that miR-1281 targets ADCY1 and DVL1. The results indicate a novel link between miR-1281 and depression based on the in vivo identification of miRNA expression profiles. KXS can also stimulate the signal transduction pathways for Wnt/-catenin and cAMP/PKA/ERK/CREB, according to in vitro tests. MiR-1281, which targets ADCY1 and DVL1, is down-regulated during this activation, resulting in the protection of neuronal cells.
The Chinese drug regulatory body approved Shuganjieyu, a combination of Acanthopanax senticosus (Rupr. [Maxim.], CiWuJia), and GuanYeLianQiao Hypericum perforatum L. (GuanYeLianQiao) as the first CHM for the treatment of depression[75]. The potential antidepressant efficacy of Shuganjieyu capsules is believed to be attributed to an elevation in phosphorylation levels of the cyclic adenosine monophosphate response element binding protein and an upregulation of BDNF expression in the medial prefrontal cortex and hippocampal CA3 region of a rat model exhibiting depressive symptoms[76]. Further studies are needed to explore the potential antidepressant effects of Shuganjeyu capsules.
A three-herb decoction called Dai-Kenchu-To (DKT) is used to treat GI issues. DKT therapy has been shown to stop bacterial translocation in rats under extreme stress and maintain microbiome diversity. Additionally, studies have shown that DKT improves small intestine motility in dogs and rats, avoids postoperative intestinal blockage in rats, and enhances intestinal blood flow in rodents. It is abundantly apparent from these studies that DKT dramatically improves GI tract functionality and can completely prevent the danger of GI tract dysregulation in the pathophysiology of depression[77].
Since ancient times, China has employed Xiao Yao San (XYS) decoction and its variations as the most popular CHM for treating depression. The mixture is prepared using a combination of eight different herbs, such as Glycyrrhiza uralensis Fisch (GanCao), Mentha haplocalyx Briq (BoHe), and Pori cocos [Schw.] Wolf (FuLing), Zingiber officinale Rosc. (GanJiang), Angelica sinensis [Oliv.] Diel (DangGui), rhizome of Atractylodes macrocephala Koidz (BaiZhu), Bupleurum chinense D (ChaiHu), Paeonia lactiflora Pal (BaiShao). It is essential to highlight that Angelica sinensis is commonly utilized in this formula to enhance blood quality and facilitate blood circulation[78]. Zeng et al[79] reviewed 26 randomized controlled trials on XYS for depression. The results showed that XYS and antidepressants were equally effective. The results above provide evidence of combining XYS with antidepressant medication instead of using antidepressants alone. Both XYS and antidepressants have fewer side effects than either alone. It is essential to approach this finding with caution in light of the potential influence of publication bias and the limitations in the quality of clinical research.
According to preclinical research, XYS improves BDNF expression in the hippocampus, regulates the hypothalamic-pituitary-adrenal (HPA) axis, increases 5-HT levels in the cerebral cortex and hippocampus, and lowers cytokine levels in the blood when administered to stress-induced animal models. Researching TCM formulas presents several challenges. The relationships between distinct herbals' constituent parts can make understanding their action methods more difficult. Future research on TCM formulae can use this study's technique and process as a model[80]. In addition to the mentioned herbal therapies, other traditional botanical remedies have also been reported for their potential effectiveness in alleviating depression symptoms (Table 1).
| Ref. | Herbs | Herbal constituents | Administration dosage | Models | Mechanism of action |
| Terpenes and phenylpropanoids | |||||
| Alotaibi et al[78], 2022 | Illicium dunnianum Tutch. | Macranthol | 10, 20, 40 mg/kg, p.o. | CUMS mice | BDNF |
| Dai et al[56], 2022 | Magnolia officinalis Rehd et Wils. | Honokiol | 2, 4, 8 mg/kg, i.g. | CUMS mice | The HPA axis/BDNF |
| Zhao et al[40], 2023 | Psoralea corylifolia Linn. | Bakuchiol analogs | 0.03-333 μM | Tr-CHO cells | Monoamine |
| Zeng et al[79], 2021 | Hemsleya amabilis Diels | Cucurbitacin IIa | 2.5, 5 mg/kg, i.p | CUMS mice | BDNF |
| Chen et al[80], 2023 | Crocus sativus L. | Crocin | 12.5, 25, 50 mg/kg, i.p. | Rats | BDNF |
| Adam et al[116], 2023 | Perilla frutescens (L.) Britt. | Rosmarinic acid | 5 and 10 mg/kg, i.p. | CUS Rats | BDNF |
| Carbohydrates | |||||
| Bildziukevich et al[117], 2023 | Acanthopanax Miq. | Chiisanoside | 2.5 and 5 mg/kg, i.p | LPS-induced mice | BDNF |
| Salehi et al[118], 2023 | Aconitum carmichaelii Debeaux | Fuzi polysaccharide 1 | 50, 100 mg/kg, i.p. | Mice | BDNF |
| Li et al[119], 2022 | Morinda officinalis How | Oligosaccharide | 5, 10, 125, 500 mM | CORT-induced PC12 | The HPA axis |
| Alkaloids | |||||
| Salehi et al[118], 2023 | Aconitum carmichaelii Debeaux | Total alkaloid | 10, 30 mg/kg, i.g. | Ovariectomized mice | BDNF |
| Ali et al[120], 2023 | Stephania tetrandra S. Moore | Tetrandrine | 10, 20, 40 mg/kg, i.g. | CUMS Rats | Monoamine/BDNF |
| Shayganfard[121], 2023 | Berberis aristata Linn. | Berberine Chloride | 5, 10, 20 mg/kg, i.p | Male albino mice | Monoamine |
| Sun et al[122], 2023 | Scutellaria baicalensis Georgi | Baicalein | 1, 2, 4 mg/kg, i.p. | CUMS mice | BDNF |
| Flavonoids | |||||
| Yu et al[123], 2022 | Pueraria lobate (Willd.) Ohwi | Puerarin | 60 and 120 mg/kg, i.g | CUS Rats | Monoamine/the HPA axis |
| Yu et al[123], 2022 | Pueraria lobate (Willd.) Ohwi | Pueraria isoflavone | 10 and 100 mg/kg | Ovariectomy mice | BDNF |
| Wang et al[124], 2021 | Apocynum venetum L. | Flavonoid Extract | 25, 50, 100 mg/ml | CORT-induced PC12 | BDNF |
| Mu and Ma[125], 2022 | Gastrodia elata Bl. | Gastrodin | 50, 100, 200 mg/kg, i.p. | CUS Rats | BDNF |
| Glycosides | |||||
| Nagakura[126], 2022 | Gentiana lutea L. | Gentiopicroside | 50, 100, 200 mg/kg, i.g. | Reserpine-induced mice | Glutamate transmission |
| Yin et al[127], 2023 | Paeonia lactiflora Pall. | Total glycosides | 160 mg/kg, p.o. | CORT-induced rats | BDNF |
| Sánchez et al[128], 2023 | Rhodiola rosea L. | Salidroside | 20, 40 mg/kg, p.o | Behavioral despair rats | The HPA axis/BDNF |
| Saponins | |||||
| Liu et al[129], 2023 | Anemarrhena asphodeloides Bunge | YY-23 | 20 mg/kg, i.g. | CMS mice | Glutamate transmission |
| Zhuang et al[58], 2023 | Bupleurum chinense DC. | Saikosaponin D | 0.75 and 1.50 mg/kg, i.g. | CUMS rats | The HPA axis |
| Yoon et al[130], 2023 | Panax ginseng C.A. Mey. | Ginsenoside Rg1 | 40 mg/kg, i.p. | CUMS rats | BDNF |
| Tian et al[131], 2023 | Anemarrhena asphodeloides Bunge | Sarsasapogenin | 12.5, 25, 50 mg/kg, p.o. | CUMS mice | Monoamine |
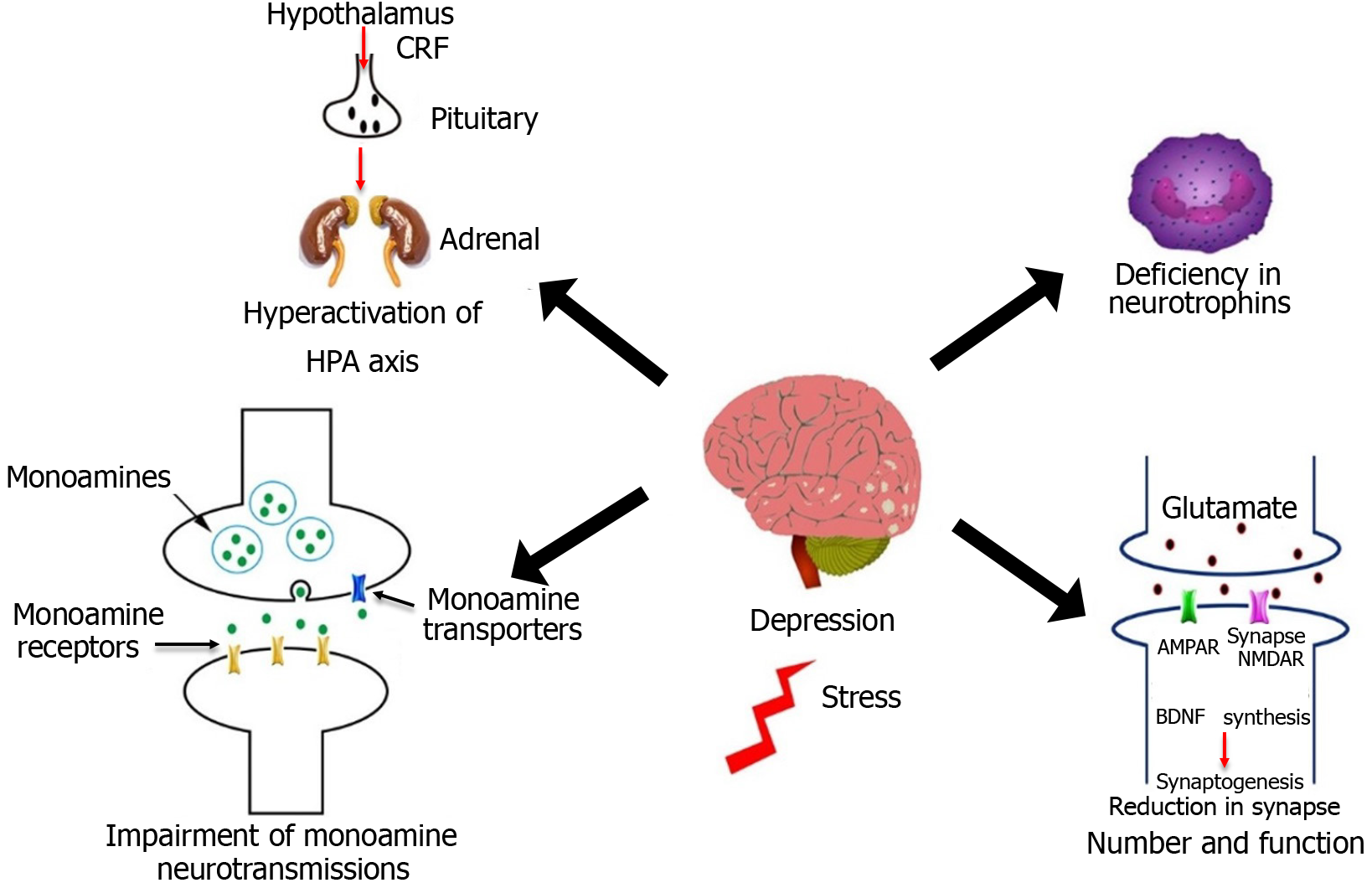
Stress triggers the activation of the HPA axis, often accompanied by elevated levels of glucocorticoids. These increased glucocorticoid levels can negatively affect neurons' survival and the generation of new neurons, ultimately leading to depressive symptoms. It is crucial to emphasize that interactions involving neurological, hormonal, or inflammatory signals occur between the central nervous system (CNS) and the HPA axis, immunological system, or endocrine system. These systems form a network that plays a crucial role in the mechanism of action of antidepressants. For example, antidepressants that work on monoamines can counteract the heightened activity of the HPA axis induced by stress. Additionally, they can diminish the secretion of pro-inflammatory cytokines from activated microglia, thereby mitigating alterations in inflammatory pathways[81].
In a similar vein, agents that are capable of reducing inflammatory effects have been found to exhibit antidepressant-like activity in animal models. This activity is believed to result from the interaction between the central nervous and immune systems[82]. These include glucocorticoid receptor antagonists, vasopressin receptor antagonists, and antagonists of the receptors for corticotropin-releasing hormone. By preventing the actions of specific receptors, these substances may be effective antidepressants. This would help to stop the adverse effects of hormone secretions caused by the overactivity of the HPA axis due to stress[83].
Ginsenoside Rg3, a protopanaxadiol ginsenoside from Panax ginseng C. A. Mey., has been shown to have anxiolytic and antidepressant-like effects in animal models of chronic unpredictable stress by dehyperactivating the HPA axis by lowering corticotropin-releasing hormone, corticosterone, and adrenocorticotropic hormone[84]. Research has shown that this molecule exhibits anti-inflammatory effects by decreasing the levels of inflammatory cytokines in mice stimulated with lipopolysaccharide (LPS).
The development of fast-acting antidepressants has recently focused on inhibiting glutamate transmission. Enhancing glutamate transmission with drugs like NMDA receptor channel blockers and its positive allosteric modulators and acetylcholine muscarinic (AChM) receptor antagonists can quickly repair stress-induced synaptic defects by increasing BDNF release and synapse function[85]. As the first rapid-acting antidepressant, ketamine [the S (+) enantiomer of the NMDA receptor antagonist ketamine] was licensed in 2019 to treat severe depression. Datura stramonium L. Hyoscyamus niger L., and Datura metel L., are all members of the Solanaceae Juss family of plants containing Scopolamine. This significant tropane alkaloid can easily penetrate the brain-blood barrier and block AChM1 receptors in the CNS[86]. The latest study has shown that an antidepressant effect of Scopolamine can be seen after just one dose (25 g/kg) in rats. A rise in glutamate transmission and synapse function in the spine is thought to be responsible for its antidepressant effects. This effect is mediated by blocking the AChM1 receptor on GABA interneurons[87].
Chaihu-jia-Longgu-Muli-tang and Yueju pills are two herbal formulae lately showing rapid-acting antidepressant-like actions in animal models, joining Scopolamine. Depression-like behaviors were reduced, BDNF expression was enhanced in the hippocampus, AktmTOR signaling was activated in the prefrontal cortex[88], and NR1 expression was downregulated when a dose of Yueju pill ethanol extracts (3 g/kg) was administered. The administration of Chaihu-jia-Longgu-Muli-tang at a dose of 2.1 g/kg has been found to have a quick-acting antidepressant effect in mice undergoing olfactory bulbectomy[89]. This effect is achieved by activating the AktmTOR signaling pathway and restoring the balance between AMPA and NMDA receptors in the prefrontal cortex. Additionally, these substances have been shown to produce antidepressant effects in chronic animal models via monoaminergic systems and the HPA axis[90].
According to monoamine speculation, depression is produced by impaired monoamine neurotransmissions. Inhibiting monoamine reabsorbing transporters improves synaptic cleft monoamine supply and transmissions. Conventional antidepressants primarily target monoamine reuptake transporters for serotonin (5-HT) and norepinephrine (NE)[91]. Likewise, other proteins, such as postsynaptic receptors and metabolic enzymes, also contribute to monoamine transmissions. The monoamine-based inhibitors increase 5-HT or NE transmission, altering firing activity in the locus coeruleus or dorsal raphe nucleus in various ways[92]. The efficacy of Polygala tenuifolia Willd (Yuanzhi) has been demonstrated in clinical practice, showing expectorant, tonic, tranquilizer, and antipsychotic effects. This plant is commonly included in empirical formulations used to treat depression, including KXS. Before Yuanzhi-1, a triterpenoid saponin derived from Polygala tenuifolia Willd., was recently discovered to be a triple monoamine reuptake inhibitor with high efficacy, its mode of action in the treatment of depression had not been thoroughly characterized[93].
In addition, various derivatives of Yuanzhi-1 have demonstrated antidepressant-like actions in animal behavioral models compared to those of the standard antidepressant duloxetine[94]. Ibogaine, a hallucinogenic alkaloid found in Tabernanthe iboga, is one example of how it has been empirically utilized to treat depression. Serotonin and dopamine transporters have been demonstrated to be inhibited by ibogaine. However, unlike other transporter ligands, ibogaine inhibits these transporters non-competitively. It appears to bind to the extracellular surface of a conformation of the transporter that faces the cytoplasm[95] (Figure 2).
Lack of BDNF affects depression's pathogenesis. Stress-induced downregulation of CREB mRNA level, as well as its phosphorylation, BDNF expression, and neurogenesis, can be restored by antidepressant medicines[96]. This suggests that an agent capable of directly stimulating the BDNF signaling cascade could be an effective antidepressant. The potential drug targets in the BDNF cascade should aim to enhance CREB activity and BDNF expression[97]. Additionally, they should activate the BDNF receptor TrkB or stimulate post-receptor signaling cascades like Ras-Raf-ERK, PI3K-Akt, and PLCγ[98]. Furthermore, Ginsenoside Rg5 has been found to have antidepressant-like effects. It reverses the reduction in hippocampal BDNF expression and TrkB phosphorylation caused by chronic social defeat[99].
TCM can potentially prevent the onset of depression during its early stages effectively. There is a connection between immune dysregulation, particularly concerning inflammatory processes and depressive symptoms[100]. Specifically, elevated levels of pro-inflammatory cytokines in the bloodstream and the resulting activation of microglia in the brain contribute to neurobiological alterations associated with depression. These changes ultimately give rise to the behavioral symptoms characteristic of depression. In contrast to the administration of endotoxins like LPS, chronic unpredictable mild stress treatment increases the immune system's pro-inflammatory or neuroinflammatory response in the blood and brain by activating the IDO pathway or pro-inflammatory cytokines[101]. It is vital to note that the deregulation of the peripheral immune system significantly influences the etiology of depression. Through increased blood-brain barrier permeation, peripheral cytokines can be effectively carried into the CNS, decreasing serotonin neurotransmission and stimulating the axis of HPA[102].
Bupleurum chinense is a plant frequently utilized for its medicinal properties in treating inflammation and infectious diseases. The compound Saikosaponin-D is a triterpenoid saponin extracted from Bupleurum chinense. It possesses various pharmacological effects, including anti-inflammatory and antidepressant activity[96]. Recently, icariin, a prenylated flavonoid extracted from Epimedium brevicornu Maxim, has been shown to reduce inflammation and oxidative stress-induced brain damage by inhibiting NF-κB signaling and the NLRP3-inflammasome/caspase-1/IL-1β axis in the hippocampus. Trans-cinnamaldehyde, a bioactive component of Cinnamomum cassia Presl, inhibits microglia activation and reduces stress-induced inflammation. In animal studies, trans-cinnamaldehyde has antidepressant effects by inactivating the NF-κB/NLRP3 inflammasome pathway[103].
Therefore, it is possible to utilize anti-inflammatory agents to proactively prevent depression by addressing immune dysregulation before it leads to neurobiological alterations in the brain. However, no CHM components have been shown to affect cytokine receptors specifically[104]. Recently, the anti-inflammatory activity of a key drug category known as "Qing-Re-Yao" has been investigated. These medicines are specifically designed to treat syndromes related to inflammation. TCM formulations designed to alleviate depressed symptoms caused by inflammation typically use at least one herb in this particular category. The study's findings revealed that a significant % of herbs, precisely 93%, demonstrated anti-inflammatory properties through at least one underlying mechanism. Moreover, approximately 68% of the herbs exhibited anti-inflammatory activity through two or more mechanisms[105].
Ensuring the safety of TCM interventions for depression is a critical consideration in pursuing holistic well-being. TCM encompasses diverse modalities, including acupuncture, herbal remedies, and mind-body practices, each with its safety profile and potential side effects[106]. Acupuncture is considered safe when trained and licensed practitioners adhere to rigorous hygiene and sterilization standards. However, minor side effects like mild bruising, bleeding, or temporary discomfort at the needle insertion sites may occur. These effects are typically transient and self-limiting.
Moreover, individuals seeking acupuncture for depression should ensure that practitioners are qualified and adhere to established safety guidelines[107]. Herbal medicine is another prominent facet of TCM that requires careful consideration. It is essential to recognize that herbs can carry risks, particularly in interactions with conventional medications or the potential for allergic reactions. The safety of TCM herbal prescriptions hinges on the expertise of the practitioner in selecting appropriate herbs and dosages tailored to the individual's needs[108].
Open communication about medical history, existing medications, and any adverse reactions is essential to mitigate potential risks and ensure a safe and effective treatment approach. TCM herbal formulations, often comprising a combination of various plant materials, minerals, and animal products, may lead to adverse reactions or interactions when used alongside conventional pharmaceuticals[109]. For example, certain TCM herbs could affect the metabolism of medications, leading to altered drug concentrations in the body. Moreover, there may be the potential for allergic reactions or sensitivities to specific herbal components[110].
TCM therapy for depression is accompanied by challenges that warrant careful consideration. Firstly, the lack of standardized treatment protocols challenges ensuring consistent and replicable outcomes. TCM therapies, which often involve a combination of herbal formulations, acupuncture techniques, and other practices, can vary in their application and dosages. Additionally, the lack of large-scale, high-quality clinical trials on TCM therapy for depression makes it difficult for healthcare practitioners to safely offer these therapies as part of comprehensive treatment strategies[111]. Secondly, the potential for herb-drug interactions is a concern that requires close attention. Many TCM herbal remedies consist of complex formulations derived from multiple ingredients, raising the possibility of interactions with conventional medications[112]. Furthermore, the cultural gap challenge complicates integrating TCM therapy into mainstream mental health care. Differences in diagnostic paradigms, treatment philosophies, and language barriers can hinder communication and collaboration between TCM practitioners and conventional healthcare providers[113].
The challenge of ensuring quality control and safety in TCM therapies cannot be understated. TCM herbal products, mainly when sourced from unregulated markets, may carry contamination risks or adulteration. Moreover, the lack of standardized outcome measures for assessing the effectiveness of TCM therapy for depression poses a significant limitation[114]. Unlike conventional clinical trials that rely on standardized depression rating scales, TCM interventions may require tailored or alternative measures that capture their unique therapeutic effects[115]. This limitation un
For healthcare practitioners, patients, and policymakers contemplating TCM as a viable treatment option for depression, a multifaceted approach is essential. Firstly, fostering open and respectful communication between conventional healthcare providers and TCM practitioners is paramount. Collaboration allows for a comprehensive understanding of the patient's health journey, ensuring that TCM interventions align with the overall treatment plan and are well-coordinated with other therapies. Healthcare practitioners should actively educate themselves about TCM principles and practices, enabling them to engage in informed discussions with patients about potential benefits, risks, and interactions. Incorporating TCM into a patient's care requires careful consideration of their medical history, current medications, and individual preferences, focusing on personalized, patient-centered care.
Patients considering TCM for depression should prioritize informed decision-making. Seeking care from qualified TCM practitioners who possess appropriate credentials and experience is crucial. Patients should engage in open dialogues with TCM practitioners and conventional healthcare providers, disclosing all relevant medical information and ongoing treatments. It is crucial to approach TCM interventions with realistic expectations, recognizing that they may complement but not replace conventional therapies. Patients should proactively assess their responses to TCM interventions, providing feedback to TCM and traditional practitioners to ensure a holistic and integrated approach to their mental well-being.
Policymakers play a pivotal role in facilitating the integration of TCM into mental health care systems. Developing guidelines and regulations that uphold safety, efficacy, and ethical standards in TCM practice is imperative. Policymakers should advocate for robust research initiatives to further explore the potential of TCM in depression treatment, fostering evidence-based practice. Creating pathways for interdisciplinary collaboration, training programs, and information sharing among healthcare practitioners from TCM and conventional backgrounds can foster a cohesive, patient-centric approach to mental health care. By embracing these recommendations, harmonious integration of TCM into mainstream mental health care can be achieved, offering patients a broader spectrum of choices for managing depression and promoting holistic well-being.
This comprehensive review underscores the multifaceted landscape of TCM as a potential therapeutic avenue in alleviating depression. An extensive analysis of diverse studies and empirical evidence shows that TCM offers a holistic and integrative approach that extends beyond the conventional boundaries of Western Medicine. The synthesis of findings reveals promising outcomes in applying TCM modalities such as acupuncture, herbal medicine, mind-body practices, and dietary interventions for managing depressive symptoms. The collective body of research reviewed here indicates that TCM therapies have the potential to contribute positively to depression management, promoting emotional well-being and enhancing overall quality of life. However, the intricate interplay of cultural, scientific, and practical factors requires careful navigation. Exploring TCM's efficacy in depression treatment is an ongoing endeavor that demands continued interdisciplinary collaboration, rigorous clinical investigation, and enhanced dialogue between TCM practitioners, conventional healthcare providers, patients, and policymakers. While our preclinical research has provided promising insights into the transformative impact of TCM on depression, we acknowledge the necessity for rigorous clinical investigations to strengthen the validity of these preliminary results. As part of our ongoing research, we are actively planning and initiating controlled clinical trials that will meticulously assess the efficacy of TCM interventions using validated clinometric scales. These trials aim to provide a robust foundation for translating our preclinical findings into clinically relevant outcomes, ultimately contributing to the broader understanding of TCM in treating depression. While this review underscores the potential of TCM, it is essential to acknowledge the existing limitations, such as the heterogeneity of study designs, the need for more robust clinical trials, and the necessity for standardized outcome measures. These limitations emphasize the imperative for further research that employs rigorous methodologies to elucidate TCM's mechanisms of action, optimal application, and long-term effects. As we move forward, harnessing the collective wisdom of both Eastern and Western traditions holds the promise of a more holistic and patient-centered approach to depression management that bridges cultural divides and embraces the strengths of diverse therapeutic paradigms. Ultimately, the efficacy of TCM in alleviating depression remains a dynamic field ripe for exploration, collaboration, and the advancement of patient care in mental health.
We express our sincere gratitude to the funding organizations for their financial support, which enabled us to carry out this research and contribute to advancing knowledge in our field. The funders had no role in study design, data collection and analysis, publication decisions, or manuscript preparation.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade C, Grade C
Novelty: Grade B, Grade C
Creativity or Innovation: Grade B, Grade C
Scientific Significance: Grade B, Grade D
P-Reviewer: Mazza M, Italy; Pavón L, Mexico S-Editor: Lin C L-Editor: A P-Editor: Zhao S
| 1. | Zhang Y, Folarin AA, Sun S, Cummins N, Vairavan S, Qian L, Ranjan Y, Rashid Z, Conde P, Stewart C, Laiou P, Sankesara H, Matcham F, White KM, Oetzmann C, Ivan A, Lamers F, Siddi S, Simblett S, Rintala A, Mohr DC, Myin-Germeys I, Wykes T, Haro JM, Penninx BWJH, Narayan VA, Annas P, Hotopf M, Dobson RJB; RADAR-CNS Consortium. Associations Between Depression Symptom Severity and Daily-Life Gait Characteristics Derived From Long-Term Acceleration Signals in Real-World Settings: Retrospective Analysis. JMIR Mhealth Uhealth. 2022;10:e40667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Zhang R, Peng X, Song X, Long J, Wang C, Zhang C, Huang R, Lee TMC. The prevalence and risk of developing major depression among individuals with subthreshold depression in the general population. Psychol Med. 2023;53:3611-3620. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 65] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 3. | Bai J, Li J, Zhang D. The History of the Introduction of the Concept of Depression Into China. Front Psychiatry. 2022;13:889329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Hofmarcher T, Romild U, Spångberg J, Persson U, Håkansson A. The societal costs of problem gambling in Sweden. BMC Public Health. 2020;20:1921. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Wang Z, Li H, Kang Y, Liu Y, Shan L, Wang F. Risks of Digestive System Side-Effects of Selective Serotonin Reuptake Inhibitors in Patients with Depression: A Network Meta-Analysis. Ther Clin Risk Manag. 2022;18:799-812. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 6. | Yang X, Shi C, Bao T, Zhang Z. Editorial: Traditional Chinese medicine for depression and anxiety. Front Psychiatry. 2023;14:1217886. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Gao J, Zhang WJ, Yang F. A Review of Traditional Chinese Medicine for the Treatment of Depression. Psychosom Med Res. 2022;4:6. [DOI] [Full Text] |
| 8. | Zohuri B, Kim C. Acupuncture driven depression treatment: a noninvasive approach with acupuncture and oriental medication. Med Clin Res. 2022;7:01. [DOI] [Full Text] |
| 9. | Yap SY, Ng FL, Subramaniam M, Lim YM, Foo CN. Traditional Chinese Medicine Body Constitutions as Predictors for Depression: A Systematic Review and Meta-Analysis. Behav Sci (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Xu Y. Exploring meanings of health and well-being: a Chinese perspective from its etymological origin and the Taoist philosophy. Ment Health Relig Cu. 2023;26:1-15. [DOI] [Full Text] |
| 11. | Cheung H, Doughty H, Hinsley A, Hsu E, Lee TM, Milner-Gulland EJ, Possingham HP, Biggs D. Understanding Traditional Chinese Medicine to Strengthen Conservation Outcomes. People Nat. 2021;3:115-128.. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 12. | Yagüe E, Sun H, Hu Y. East Wind, West Wind: Toward the modernization of traditional Chinese medicine. Front Neurosci. 2022;16:1057817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Cook CA. The First Documented Experience of Qi and an Account of Healing Failure: 4th Century BCE. Chin Med Cul. 2023;6:139-146. [DOI] [Full Text] |
| 14. | Dollar B. An Examination of Qi Through the Lens of Western Medicine. D. Thesis, Honors College. 2021. Available from: https://baylor-ir.tdl.org/items/e64700b4-443f-4d7f-b631-7aae72e96748. |
| 15. | Yasser N, Qasim MS, Mahmood RA. The Theory of Yin-Yang: A Study in Selected Odes by John Keats. Himalayan J Edu Lit. . [DOI] [Full Text] |
| 16. | Kneeland ET, Simpson LE. Emotion malleability beliefs influence emotion regulation and emotion recovery among individuals with depressive symptoms. Cogn Emot. 2022;36:1613-1621. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Stanley-Baker M. A means for cohering natural knowledge. In: Routledge Handbook of Chinese Medicine. 1st ed. New York: Routledge, 2022. |
| 18. | Wang X, Yin X, Liu P, Wang A, Mu W, Xu J, Lu W, Chen Z, Zhou Y, Xu S, Wang Y. The effect of Baduanjin Qigong combined with five-elements music on anxiety and quality of sleep in asymptomatic patients with COVID-19 infection: A randomised controlled trial. Heliyon. 2023;9:e18962. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 19. | Aplin-Houtz M, Lane E, Leahy S, Willey S, Rowsey A. The Other Big Five: an Evaluation and Validation of a Measure for the Five Elements of Personality from Traditional Chinese Medicine. SSRN Electron. J 2023. [DOI] [Full Text] |
| 20. | ChenYG. Disclosing Central-Earth Splenic Theory Based Upon two TCM Five-Element Models. J Altern Complement Integr Med. 2023;9:365. [DOI] [Full Text] |
| 21. | Huang YT, Chang CC. Discussion on depression by thinking of traditional Chinese Medicine. Med Theor Hypothesis. 2023;6:1. [DOI] [Full Text] |
| 22. | Sankararaman S, Velayuthan S, Chen Y, Robertson J, Sferra TJ. Role of Traditional Chinese Herbal Medicines in Functional Gastrointestinal and Motility Disorders. Curr Gastroenterol Rep. 2022;24:43-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 23. | Ji W, Yang Y, Pei T, He M, Li X, Duan B. The Influence of TCM Emotional Nursing on Anxiety and Depression in Patients with Atrial Fibrillation. Am J Public Health. 2023;11:1-4. [DOI] [Full Text] |
| 24. | Jin W, Tao Y, Wang C, Wang L, Ao X, Su M, Hu B, Ouyang Y, Liu J, Li H. Infrared Imageries of Human Body Activated by Tea Match the Hypothesis of Meridian System. Phenomics. 2023;3:502-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 25. | Hartmann M, Mavrolampados A, Toiviainen P, Saarikallio S, Foubert K, Brabant O, Snape N, Ala-Ruona E, Gold C, Erkkilä J. Musical interaction in music therapy for depression treatment. Psychol Music. 2023;51:33-50. [DOI] [Full Text] |
| 26. | Li JY, Guo KL, Lin JQ, Xu ZX. Effectiveness of five elements music therapy on negative emotions of tumor patients: a systematic review and grading recommendations (GRADE) system. Psychosom Med Res. 2023;5:3. [DOI] [Full Text] |
| 27. | Park JI, Lee IH, Lee SJ, Kwon RW, Choo EA, Nam HW, Lee JB. Effects of music therapy as an alternative treatment on depression in children and adolescents with ADHD by activating serotonin and improving stress coping ability. BMC Complement Med Ther. 2023;23:73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 30] [Reference Citation Analysis (0)] |
| 28. | Yang Y, Su W, Zang C, Tan Y, Zhang Y, Zhou Z, Lu W, Wu S, Zhang X, Wu C. Traditional Chinese medicines (TCMs) with varied meridians (Gui-Jing) differentially alleviate the adverse impact of Coptis chinensis on gut microbiota. J Ethnopharmacol. 2023;307:116256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 29. | Wang Q, Ma S, Xue F, Wang J, He M, Pang K, Wang H. Acupuncture therapy for post-stroke depression: A scoping review of randomized controlled trials. Eur J Integr Med. 2023;61:102263. [DOI] [Full Text] |
| 30. | Li W, Wenwen Z, Yawen G, Ling W. Research progress of depression in TCM. Front Med Sci Res. 2023;5. [DOI] [Full Text] |
| 31. | Eseadi C, Ngwu MO. Significance of music therapy in treating depression and anxiety disorders among people with cancer. World J Clin Oncol. 2023;14:69-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (7)] |
| 32. | Petersson EL, Forsén E, Björkelund C, Hammarbäck L, Hessman E, Weineland S, Svenningsson I. Examining the description of the concept "treatment as usual" for patients with depression, anxiety and stress-related mental disorders in primary health care research - A systematic review. J Affect Disord. 2023;326:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 33. | Foroughe M. Emotion Focused Therapy for Youth. 1st ed. New York: Routledge, 2023: 22. [DOI] [Full Text] |
| 34. | Kashkouli M, Jahanian Sadatmahalleh S, Ziaei S, Kazemnejad A, Saber A, Darvishnia H, Azarbayjani K. Relationship between postpartum depression and plasma vasopressin level at 6-8 weeks postpartum: a cross-sectional study. Sci Rep. 2023;13:3518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 35. | Denk JG. The Impact of a Music Therapy Support Group on Perceived Stress, Anxiety, and Depression in Long-Term Caregivers: A Pilot Study. Music Ther Perspectives. 2023;41:28-36. [DOI] [Full Text] |
| 36. | Rajakumar KD, Mohan J, Kanagasabai A. An IoT-Based Emotion Analysis and Music Therapy. In: Big Data, Cloud Computing, and IoT. 1st ed. Florida: Chapman and Hall/CRC, 2023. [DOI] [Full Text] |
| 37. | Zang L, Cheng C, Zhou Y, Liu X. Music therapy effect on anxiety reduction among patients with cancer: A meta-analysis. Front Psychol. 2022;13:1028934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (1)] |
| 38. | Yao J, Chen C, Guo Y, Yang Y, Liu X, Chu S, Ai Q, Zhang Z, Lin M, Yang S, Chen N. A Review of Research on the Association between Neuron-Astrocyte Signaling Processes and Depressive Symptoms. Int J Mol Sci. 2023;24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 39. | Ou Y, Lin D, Ni X, Li S, Wu K, Yuan L, Rong J, Feng C, Liu J, Yu Y, Wang X, Wang L, Tang Z, Zhao L. Acupuncture and moxibustion in patients with cancer-related insomnia: A systematic review and network meta-analysis. Front Psychiatry. 2023;14:1108686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 40. | Zhao W, Wang Y, Hou J, Ding W, Suo W, Liu Z, Zhou Y, Zhao H. Efficacy and safety of non-pharmacological therapy under the guidance of TCM theory in the treatment of anxiety in patients with myocardial infarction: A protocol for systematic review and meta-analysis. PLoS One. 2023;18:e0288154. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 41. | Zhao FY, Kennedy GA, Spencer SJ, Conduit R, Zhang WJ, Fu QQ, Zheng Z. The Role of Acupuncture in the Management of Insomnia as a Major or Residual Symptom Among Patients With Active or Previous Depression: A Systematic Review and Meta-Analysis. Front Psychiatry. 2022;13:863134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 42. | Abujilban S, Al-Omari H, Issa E, ALhamdan A, Al-Nabulsi L, Mrayan L, Mahmoud KF, Kernohan WG. Effectiveness of Telephone-Based Interpersonal Psychotherapy on Antenatal Depressive Symptoms: A Prospective Randomized Controlled Trial in The Kingdom of Jordan. J Am Psychiatr Nurses Assoc. 2023;10783903231171595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 43. | Yang NN, Lin LL, Li YJ, Li HP, Cao Y, Tan CX, Hao XW, Ma SM, Wang L, Liu CZ. Potential Mechanisms and Clinical Effectiveness of Acupuncture in Depression. Curr Neuropharmacol. 2022;20:738-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 69] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 44. | Lee YS, Kim SY, Lee H, Chae Y, Lee MS. ACURATE: A guide for reporting sham controls in trials using acupuncture. Integr Med Res. 2023;12:100955. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 45. | Ekong MB, Iniodu CF. Nutritional therapy can reduce the burden of depression management in low income countries: A review. IBRO Neurosci Rep. 2021;11:15-28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 46. | Burton TC, Lv N, Tsai P, Peñalver Bernabé B, Tussing-Humphreys L, Xiao L, Pandey GN, Wu Y, Ajilore OA, Ma J. Associations between fecal short-chain fatty acids, plasma inflammatory cytokines, and dietary markers with depression and anxiety: Post hoc analysis of the ENGAGE-2 pilot trial. Am J Clin Nutr. 2023;117:717-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 47. | Liu C, Rao W, Cui Z, Chen P, Lei K, Mai K, Zhang W. Comparative evaluation on the effects of dietary docosahexaenoic acid on growth performance, fatty acid profile, and lipid metabolism in two sizes of abalone Haliotis discus hannai Ino. Aquaculture. 2023;25. [DOI] [Full Text] |
| 48. | Bruncsics B, Hullam G, Bolgar B, Petschner P, Millinghoffer A, Gecse K, Eszlari N, Gonda X, Jones DJ, Burden ST, Antal P, Deakin B, Bagdy G, Juhasz G. Genetic risk of depression is different in subgroups of dietary ratio of tryptophan to large neutral amino acids. Sci Rep. 2023;13:4976. [DOI] [Full Text] |
| 49. | Nguyen HD, Oh H, Hoang NHM, Jo WH, Kim MS. Environmental science and pollution research role of heavy metal concentrations and vitamin intake from food in depression: a national cross-sectional study (2009-2017). Environ Sci Pollut Res Int. 2022;29:4574-4586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 50. | Ekinci GN, Sanlier N. The relationship between nutrition and depression in the life process: A mini-review. Exp Gerontol. 2023;172:112072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 50] [Reference Citation Analysis (0)] |
| 51. | Zhang Y, Ding J, Liang J. Associations of Dietary Vitamin A and Beta-Carotene Intake With Depression. A Meta-Analysis of Observational Studies. Front Nutr. 2022;9:881139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 52. | Luo X, Zhang Y, Li H, Ren M, Liu Y, Kuang Z, Cai Y, Chen Y, Ni X. Clinical Evidence on the Use of Chinese Herbal Medicine for Acute Infectious Diseases: An Overview of Systematic Reviews. Front Pharmacol. 2022;13:752978. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 53. | Zhao L, Zhang H, Li N, Chen J, Xu H, Wang Y, Liang Q. Network pharmacology, a promising approach to reveal the pharmacology mechanism of Chinese medicine formula. J Ethnopharmacol. 2023;309:116306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 374] [Article Influence: 187.0] [Reference Citation Analysis (0)] |
| 54. | Jia Y, Wang M, Lambers PH, van Andel T. The catalogue of the Westhoff collection of Chinese materia medica (c. 1870): Evidence of interaction between a Chinese medicine practitioner and the Dutch in Indonesia. J Ethnopharmacol. 2024;318:116987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 55. | Sun Y, Zhao J, Rong J. Dissecting the molecular mechanisms underlying the antidepressant activities of herbal medicines through the comprehensive review of the recent literatures. Front Psychiatry. 2022;13:1054726. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 56. | Dai W, Feng K, Sun X, Xu L, Wu S, Rahmand K, Jia D, Han T. Natural products for the treatment of stress-induced depression: Pharmacology, mechanism and traditional use. J Ethnopharmacol. 2022;285:114692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 46] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 57. | Wang H, Liu J, He J, Huang D, Xi Y, Xiao T, Ouyang Q, Zhang S, Wan S, Chen X. Potential mechanisms underlying the therapeutic roles of sinisan formula in depression: Based on network pharmacology and molecular docking study. Front Psychiatry. 2022;13:1063489. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 58. | Zhuang W, Liu SL, Xi SY, Feng YN, Wang K, Abduwali T, Liu P, Zhou XJ, Zhang L, Dong XZ. Traditional Chinese medicine decoctions and Chinese patent medicines for the treatment of depression: Efficacies and mechanisms. J Ethnopharmacol. 2023;307:116272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 31] [Reference Citation Analysis (0)] |
| 59. | Kou Y, Li Z, Yang T, Shen X, Wang X, Li H, Zhou K, Li L, Xia Z, Zheng X, Zhao Y. Therapeutic potential of plant iridoids in depression: a review. Pharm Biol. 2022;60:2167-2181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 60. | Liu XY, ZhengRW. Promoting acupuncture-moxibustion to be world leading discipline: Tuidong Zhenjiu Chengwei Guojilingxian De Yiliucueke. Int J Clin Acupunct. 2023;33:299. [DOI] [Full Text] |
| 61. | Lu R, Zhang L, Wang H, Li M, Feng W, Zheng X. Echinacoside exerts antidepressant-like effects through enhancing BDNF-CREB pathway and inhibiting neuroinflammation via regulating microglia M1/M2 polarization and JAK1/STAT3 pathway. Front Pharmacol. 2022;13:993483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 24] [Reference Citation Analysis (0)] |
| 62. | Zhu Y, Wu Z, Zhao D, Wu X, He R, Wang Z, Peng D, Fang Y. Clinical Guideline (CANMAT 2016) Discordance of Medications for Patients with Major Depressive Disorder in China. Neuropsychiatr Dis Treat. 2023;19:829-839. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 63. | Sadeghi A, Ghorayshi F, Baghshahi H, Akbari H, Memarzadeh MR, Taghizadeh M, Safaei A. The antidepressant effect of combined extracts of Hypericum perforatum and Echium amoenum supplementation in patients with depression symptoms: A randomized clinical trial. Avicenna J Phytomed. 2023;13:328-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 64. | Gao Z, Wang Y, Yu H. A Chinese Classical Prescription Chaihu Shugan Powder in Treatment of Post-Stroke Depression: An Overview. Medicina (Kaunas). 2022;59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 65. | Tu M, Xiong S, Lv S, Wu X, Hu H, Hu R, Fang J, Shao X. Acupuncture for Major Depressive Disorder: A Data Mining-Based Literature Study. Neuropsychiatr Dis Treat. 2023;19:1069-1084. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 66. | Xie Z, Xie H, Peng X, Hu J, Chen L, Li X, Qi H, Zeng J, Zeng N. The antidepressant-like effects of Danzhi Xiaoyao San and its active ingredients. Phytomedicine. 2023;119:155015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 67. | Shen Z, Yu M, Dong Z. Research Progress on the Pharmacodynamic Mechanisms of Sini Powder against Depression from the Perspective of the Central Nervous System. Medicina (Kaunas). 2023;59. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 68. | Zhang M, Li A, Yang Q, Li J, Wang L, Liu X, Huang Y, Liu L. Beneficial Effect of Alkaloids From Sophora alopecuroides L. on CUMS-Induced Depression Model Mice via Modulating Gut Microbiota. Front Cell Infect Microbiol. 2021;11:665159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 69. | Wu S, Li HM, Bing YF, Zheng Y, Li WL, Zou X, Qu ZY. Bupleurum scorzonerifolium: Systematic research through pharmacodynamics and serum pharmacochemistry on screening antidepressant Q-markers for quality control. J Pharm Biomed Anal. 2023;225:115202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 70. | Kang D, Dong H, Shen Y, Ou J, Zhao J. The clinical application of Chinese herbal medication to depression: A narrative review. Front Public Health. 2023;11:1120683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 71. | Fan Q, Liu Y, Sheng L, Lv S, Yang L, Zhang Z, Guo J, Fan Y, Hu D. Chaihu-Shugan-San inhibits neuroinflammation in the treatment of post-stroke depression through the JAK/STAT3-GSK3β/PTEN/Akt pathway. Biomed Pharmacother. 2023;160:114385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 35] [Reference Citation Analysis (0)] |
| 72. | Elias E, Zhang AY, Manners MT. Novel Pharmacological Approaches to the Treatment of Depression. Life (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 73. | Bo M, Zhang H, Xu J, Zhao H, Jia X, Wang G, Lu Z. Systematic review of Kaixinsan in treating depression: Efficacy and pharmacological mechanisms. Front Behav Neurosci. 2022;16:1061877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 74. | Chen C, Xu YJ, Zhang SR, Wang XH, Hu Y, Guo DH, Zhou XJ, Zhu WY, Wen AD, Tan QR, Dong XZ, Liu P. MiR-1281 is involved in depression disorder and the antidepressant effects of Kai-Xin-San by targeting ADCY1 and DVL1. Heliyon. 2023;9:e14265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 75. | Zhang YW, Cheng YC. Challenge and Prospect of Traditional Chinese Medicine in Depression Treatment. Front Neurosci. 2019;13:190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 76. | Yan ZY, Jiao HY, Chen JB, Zhang KW, Wang XH, Jiang YM, Liu YY, Xue Z, Ma QY, Li XJ, Chen JX. Antidepressant Mechanism of Traditional Chinese Medicine Formula Xiaoyaosan in CUMS-Induced Depressed Mouse Model via RIPK1-RIPK3-MLKL Mediated Necroptosis Based on Network Pharmacology Analysis. Front Pharmacol. 2021;12:773562. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 77. | Jiang N, Wang H, Huang H, Lv J, Zeng G, Wang Q, Bao Y, Chen Y, Liu X. The Antidepressant-Like Effects of Shen Yuan in a Chronic Unpredictable Mild Stress Rat Model. Front Psychiatry. 2021;12:622204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 78. | Alotaibi GHS, Shivanandappa TB, Chinnadhurai M, Reddy Dachani S, Dabeer Ahmad M, Abdullah Aldaajanii K. Phytochemistry, Pharmacology and Molecular Mechanisms of Herbal Bioactive Compounds for Sickness Behaviour. Metabolites. 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 79. | Zeng Y, Wang J, Huang Q, Ren Y, Li T, Zhang X, Yao R, Sun J. Cucurbitacin IIa: A review of phytochemistry and pharmacology. Phytother Res. 2021;35:4155-4170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 80. | Chen Z, Gu J, Lin S, Xu Z, Xu H, Zhao J, Feng P, Tao Y, Chen S, Wang P. Saffron essential oil ameliorates CUMS-induced depression-like behavior in mice via the MAPK-CREB1-BDNF signaling pathway. J Ethnopharmacol. 2023;300:115719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 43] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 81. | Shi Y, Gu L, Zhang X, Chen M. Traditional Chinese medicine mediated tumor suppression by regulating psychological factors. Med Nov Technol Devices. 2022;16:100162. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 82. | Mapunda JA, Tibar H, Regragui W, Engelhardt B. How Does the Immune System Enter the Brain? Front Immunol. 2022;13:805657. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 84] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 83. | Reul JM, Holsboer F. On the role of corticotropin-releasing hormone receptors in anxiety and depression. Dialogues Clin Neurosci. 2002;4:31-46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 84. | Sur B, Lee B. Ginsenoside Rg3 modulates spatial memory and fear memory extinction by the HPA axis and BDNF-TrkB pathway in a rat post-traumatic stress disorder. J Nat Med. 2022;76:821-831. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 85. | Wei Y, Chang L, Hashimoto K. Molecular mechanisms underlying the antidepressant actions of arketamine: beyond the NMDA receptor. Mol Psychiatry. 2022;27:559-573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 162] [Article Influence: 54.0] [Reference Citation Analysis (0)] |
| 86. | Cerne R, Lippa A, Poe MM, Smith JL, Jin X, Ping X, Golani LK, Cook JM, Witkin JM. GABAkines - Advances in the discovery, development, and commercialization of positive allosteric modulators of GABA(A) receptors. Pharmacol Ther. 2022;234:108035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 65] [Article Influence: 21.7] [Reference Citation Analysis (0)] |
| 87. | Tartt AN, Mariani MB, Hen R, Mann JJ, Boldrini M. Dysregulation of adult hippocampal neuroplasticity in major depression: pathogenesis and therapeutic implications. Mol Psychiatry. 2022;27:2689-2699. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 131] [Cited by in RCA: 220] [Article Influence: 73.3] [Reference Citation Analysis (0)] |
| 88. | Zou Z, Huang J, Yang Q, Zhang Y, Xu B, Wang P, Chen G. Repeated Yueju, But Not Fluoxetine, Induced Sustained Antidepressant Activity in a Mouse Model of Chronic Learned Helplessness: Involvement of CaMKII Signaling in the Hippocampus. Evid Based Complement Alternat Med. 2022;2022:1442578. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 89. | Sharma A, Bhalla S, Mehan S. PI3K/AKT/mTOR signalling inhibitor chrysophanol ameliorates neurobehavioural and neurochemical defects in propionic acid-induced experimental model of autism in adult rats. Metab Brain Dis. 2022;37:1909-1929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 90. | McLaughlin L. Serotonin and the Brain: Exploring the 5-HT System's Role in Depression. Cornell Undergrad Res J. 2023;2:54-74. [DOI] [Full Text] |
| 91. | Johnston JN. Investigation of the rapid-acting antidepressant-like effects of reelin in parallel to ketamine. Ph.D, York University. 2022. Available from: https://dspace.library.uvic.ca/items/5c7f1c47-0117-4909-8865-fd49010601dc. |
| 92. | Xie Y, Yang Y, Yuan X, Liu Y, He X. Herb pair of Polygala tenuifolia Willd and Acorus tatarinowii Schott decoction attenuates seizures and alleviates anxiety in mice: Evidence for modulating inflammation, alleviating oxidative stress and mediating GABA pathway. Pak J Pharm Sci. 2023;36:565-577. [PubMed] |
| 93. | Yu S, Dong X, Ma R, Ji H, Yu J, Liu A. Characterization of a polysaccharide from Polygala tenuifolia willd. with immune activity via activation MAPKs pathway. Bioorg Chem. 2023;130:106214. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 94. | Rocha JM, Reis JAS, Bouso JC, Hallak JEC, Dos Santos RG. Identifying setting factors associated with improved ibogaine safety: a systematic review of clinical studies. Eur Arch Psychiatry Clin Neurosci. 2023;273:1527-1542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 95. | Gliwińska A, Czubilińska-Łada J, Więckiewicz G, Świętochowska E, Badeński A, Dworak M, Szczepańska M. The Role of Brain-Derived Neurotrophic Factor (BDNF) in Diagnosis and Treatment of Epilepsy, Depression, Schizophrenia, Anorexia Nervosa and Alzheimer's Disease as Highly Drug-Resistant Diseases: A Narrative Review. Brain Sci. 2023;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 30] [Reference Citation Analysis (0)] |
| 96. | Bhatt S, Devadoss T, Jha NK, Baidya M, Gupta G, Chellappan DK, Singh SK, Dua K. Targeting inflammation: a potential approach for the treatment of depression. Metab Brain Dis. 2023;38:45-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 45] [Reference Citation Analysis (0)] |
| 97. | Miyao M, Hirotsu A, Tatsumi K, Tanaka T. Prior exposure to stress exacerbates neuroinflammation and causes long-term behavior changes in sepsis. Heliyon. 2023;9:e16904. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 98. | Twaij BAAR, Al-Hakeim HK, Altufaili MF. Review on the neuron damage parameters in patients with end-stage renal disease. J Popul Ther Clin Pharmacol. 2023;30: e408-e420. [DOI] [Full Text] |
| 99. | Yip KM, Lee KM, Ng TB, Xu S, Yung KKL, Qu S, Cheung AKL, Sze SCW. An anti-inflammatory and anti-fibrotic proprietary Chinese medicine nasal spray designated as Allergic Rhinitis Nose Drops (ARND) with potential to prevent SARS-CoV-2 coronavirus infection by targeting RBD (Delta)- angiotensin converting enzyme 2 (ACE2) binding. Chin Med. 2022;17:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 100. | Xu G, Xiao Q, Huang B, Lei H, Yin Z, Huang L, Zhou Z, Tian H, Huang F, Liu Y, Sun M, Zhao L, Liang F. Clinical Evidence for Association of Acupuncture with Improved Major Depressive Disorder: A Systematic Review and Meta-Analysis of Randomized Control Trials. Neuropsychobiology. 2023;82:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 101. | Hu H, Li Z, Cheng Y, Gao H. The Efficacy and Safety of Acupuncture for Depression-Related Insomnia: Protocol for a Systematic Review and Meta-Analysis. J Pain Res. 2022;15:1939-1947. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 102. | Jansen C, Baker JD, Kodaira E, Ang L, Bacani AJ, Aldan JT, Shimoda LMN, Salameh M, Small-Howard AL, Stokes AJ, Turner H, Adra CN. Medicine in motion: Opportunities, challenges and data analytics-based solutions for traditional medicine integration into western medical practice. J Ethnopharmacol. 2021;267:113477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 103. | Beurel E, Toups M, Nemeroff CB. The Bidirectional Relationship of Depression and Inflammation: Double Trouble. Neuron. 2020;107:234-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 1259] [Article Influence: 251.8] [Reference Citation Analysis (0)] |
| 104. | Guan F, Lam W, Hu R, Kim YK, Han H, Cheng YC. Majority of Chinese Medicine Herb Category "Qing Re Yao" Have Multiple Mechanisms of Anti-inflammatory Activity. Sci Rep. 2018;8:7416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 105. | Chung JY, Tang PM, Chan MK, Wang L, Huang XR, To KF, Ma RC, Lan HY. AANG Prevents Smad3-dependent Diabetic Nephropathy by Restoring Pancreatic β-Cell Development in db/db Mice. Int J Biol Sci. 2022;18:5489-5502. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 106. | Xu M, Yang C, Nian T, Tian C, Zhou L, Wu Y, Li Y, Deng X, Li X, Yang K. Adverse effects associated with acupuncture therapies: An evidence mapping from 535 systematic reviews. Chin Med. 2023;18:38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 107. | Manzoor S, Hoda N. A comprehensive review of monoamine oxidase inhibitors as Anti-Alzheimer's disease agents: A review. Eur J Med Chem. 2020;206:112787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 148] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 108. | Welz AN, Emberger-Klein A, Menrad K. Why people use herbal medicine: insights from a focus-group study in Germany. BMC Complement Altern Med. 2018;18:92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 158] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 109. | Tangkiatkumjai M; Boardman H; Walker DM. Potential factors that influence usage of complementary and alternative medicine worldwide: a systematic review. BMC Complement Med Ther. 2020;20:363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 109] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 110. | Feng Y, Liu J, Liu P, Teng J. Traditional Chinese exercises on depression: A network meta-analysis. Medicine (Baltimore). 2024;103:e37319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Reference Citation Analysis (0)] |
| 111. | Dong Y, Kuang X, Dong L, Chao G, Qi J, Zhang X, Yao J. Exploring the efficacy of traditional Chinese medicine exercise in alleviating anxiety and depression in older adults: a comprehensive study with randomized controlled trial and network meta-analysis. Front Psychol. 2023;14:1290471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 112. | Che CT, Wang ZJ, Chow MS, Lam CW. Herb-herb combination for therapeutic enhancement and advancement: theory, practice and future perspectives. Molecules. 2013;18:5125-5141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 136] [Cited by in RCA: 120] [Article Influence: 10.0] [Reference Citation Analysis (1)] |
| 113. | Yang FR, Zhu XX, Kong MW, Zou XJ, Ma QY, Li XJ, Chen JX. Xiaoyaosan Exerts Antidepressant-Like Effect by Regulating Autophagy Involves the Expression of GLUT4 in the Mice Hypothalamic Neurons. Front Pharmacol. 2022;13:873646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 114. | Salmerón-Manzano E, Garrido-Cardenas JA, Manzano-Agugliaro F. Worldwide Research Trends on Medicinal Plants. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 149] [Article Influence: 29.8] [Reference Citation Analysis (0)] |
| 115. | van Wyk AS, Prinsloo G. Health, safety, and quality concerns of plant-based traditional medicines and herbal remedies. S Afr J Bot. 2020;133:54-62. [DOI] [Full Text] |
| 116. | Adam G, Robu S, Flutur MM, Cioanca O, Vasilache IA, Adam AM, Mircea C, Nechita A, Harabor V, Harabor A, Hancianu M. Applications of Perilla frutescens Extracts in Clinical Practice. Antioxidants (Basel). 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 117. | Bildziukevich U, Wimmerová M, Wimmer Z. Saponins of Selected Triterpenoids as Potential Therapeutic Agents: A Review. Pharmaceuticals (Basel). 2023;16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 118. | Salehi A, Ghanadian M, Zolfaghari B, Jassbi AR, Fattahian M, Reisi P, Csupor D, Khan IA, Ali Z. Neuropharmacological Potential of Diterpenoid Alkaloids. Pharmaceuticals (Basel). 2023;16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 119. | Li L, Huo B, Wang Y, Gong Y, Zhang Y, Liu T, Sha G, Zheng T. Efficacy of Chinese herbal medicine on poststroke depression in animal models: A systematic review and meta-analysis. Front Neurol. 2022;13:1095444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 120. | Ali A, Martins AMC, Alam W, Khan H. Chapter 9 - Neuroprotective effects of alkaloids. Phytonutrients Neurol Disord. 2023;245-257. [DOI] [Full Text] |
| 121. | Shayganfard M. Berberine: Is it a Promising Agent for Mental Disorders Treatment? Curr Mol Pharmacol. 2023;16:307-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 122. | Sun C, Gao M, Qiao M. Research progress of traditional Chinese medicine compound "Xiaochaihu Decoction" in the treatment of depression. Biomed Pharmacother. 2023;159:114249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 123. | Yu CC, Du YJ, Li J, Li Y, Wang L, Kong LH, Zhang YW. Neuroprotective Mechanisms of Puerarin in Central Nervous System Diseases: Update. Aging Dis. 2022;13:1092-1105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 124. | Wang AR, Mi LF, Zhang ZL, Hu MZ, Zhao ZY, Liu B, Li YB, Zheng S. Saikosaponin A improved depression-like behavior and inhibited hippocampal neuronal apoptosis after cerebral ischemia through p-CREB/BDNF pathway. Behav Brain Res. 2021;403:113138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 66] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 125. | Mu D, Ma Q. A Review of Antidepressant Effects and Mechanisms of Three Common Herbal Medicines: Panax ginseng, Bupleurum chinense, and Gastrodia elata. CNS Neurol Disord Drug Targets. 2022;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 126. | Nagakura Y. Therapeutic Approaches to Nociplastic Pain Based on Findings in the Reserpine-Induced Fibromyalgia-Like Animal Model. J Pharmacol Exp Ther. 2022;381:106-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Reference Citation Analysis (0)] |
| 127. | Yin P, Han X, Yu L, Zhou H, Yang J, Chen Y, Zhang T, Wan H. Pharmacokinetic analysis for simultaneous quantification of Saikosaponin A- paeoniflorin in normal and poststroke depression rats: A comparative study. J Pharm Biomed Anal. 2023;233:115485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 128. | Sánchez IA, Cuchimba JA, Pineda MC, Argüello YP, Kočí J, Kreider RB, Petro JL, Bonilla DA. Adaptogens on Depression-Related Outcomes: A Systematic Integrative Review and Rationale of Synergism with Physical Activity. Int J Environ Res Public Health. 2023;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 129. | Liu C, Cong Z, Wang S, Zhang X, Song H, Xu T, Kong H, Gao P, Liu X. A review of the botany, ethnopharmacology, phytochemistry, pharmacology, toxicology and quality of Anemarrhena asphodeloides Bunge. J Ethnopharmacol. 2023;302:115857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 130. | Yoon S, Iqbal H, Kim SM, Jin M. Phytochemicals That Act on Synaptic Plasticity as Potential Prophylaxis against Stress-Induced Depressive Disorder. Biomol Ther (Seoul). 2023;31:148-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 17] [Reference Citation Analysis (0)] |
| 131. | Tian YE, Mengtao XU, Jingpeng FANG, Qinxuan, WU, Xiaoyan ZOU, Fangqin YAN, Zhixing QING. Antidepressant-like active ingredients and their related mechanisms of functional foods or medicine and food homologous products. Digit Chinese Med. 2023;6:9-27. [DOI] [Full Text] |