Published online Feb 19, 2024. doi: 10.5498/wjp.v14.i2.266
Peer-review started: November 30, 2023
First decision: December 15, 2023
Revised: December 26, 2023
Accepted: January 22, 2024
Article in press: January 22, 2024
Published online: February 19, 2024
Processing time: 67 Days and 20.5 Hours
Sepsis is a serious infectious disease caused by various systemic inflammatory responses and is ultimately life-threatening. Patients usually experience depre
To investigate the effects of sepsis, a one-hour bundle (H1B) management was combined with psychological intervention in patients with sepsis.
This retrospective analysis included 300 patients with sepsis who were admitted to Henan Provincial People’s Hospital between June 2022 and June 2023. Acc
After intervention (T1), the scores of the Hamilton Anxiety scale and Hamilton Depression scale in the CG were significantly lower than those in the SG (P < 0.001). Sleep time, sleep quality, sleep efficiency, daytime dysfunction, sleep disturbance dimension score, and the total score in the CG were significantly lower than those in the SG (P < 0.001). The appreciation of life, mental changes, relationship with others, personal strength dimension score, and total score of the CG were significantly higher than those of the SG (P < 0.001). The scores for mental health, general health status, physiological function, emotional function, physical pain, social function, energy, and physiological function in the CG were significantly higher than those in the SG (P < 0.001). The mechanical ventilation time, intensive care unit stay time, and 28-d mortality of the CG were significantly lower than those of the SG (P < 0.05).
H1B management combined with psychological intervention can effectively alleviate the negative emotions of patients with sepsis and increase their quality of sleep and life.
Core Tip: This study investigated changes in negative emotions, quality of life, and prognosis of patients with sepsis after one-hour bundle (H1B) management and psychological intervention. The results showed that the Hamilton Anxiety scale, Hamilton Depression scale, and Pittsburgh Sleep Quality Index scores of the patients were significantly lower after the intervention, and the Post Traumatic Growth Inventory scores were higher than those before the intervention. These results indicate that H1B management combined with psychological intervention can effectively improve negative emotions, sleep quality, post-traumatic growth levels, and quality of life in patients with sepsis.
- Citation: Xia M, Dong GY, Zhu SC, Xing HM, Li LM. Sepsis one-hour bundle management combined with psychological intervention on negative emotion and sleep quality in patients with sepsis. World J Psychiatry 2024; 14(2): 266-275
- URL: https://www.wjgnet.com/2220-3206/full/v14/i2/266.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i2.266
Sepsis is a clinical syndrome characterized by dysregulated systemic, metabolic, and pathological host responses to infection. Sepsis is associated with the release of a large number of inflammatory mediators, which exert their effects through the neuroendocrine-immune regulatory network and may lead to septic shock and organ failure in severe cases[1]. At present, sepsis is the leading cause of death from critical illness worldwide[2]. It is conservatively estimated that approximately 31.5 million patients are affected by sepsis and its complications each year, resulting in approximately 5.3 million deaths globally[3]. In China, a downward trend in the fatality rate of sepsis has been observed with technological advancements and improvements in the management of medical conditions; nonetheless, the reported incidence and fatality rate of sepsis are approximately 28% and 70%, respectively[4]. Therefore, the treatment and clinical management of patients with sepsis have become critical issues that urgently need addressing.
Currently, the clinical treatment of sepsis mainly focuses on infection control, early fluid resuscitation, and correction of the pathophysiological state. Previous studies[5] have shown that patients with sepsis are emotionally depressed and have a poor overall sleep status during treatment, which has a significant impact on their prognosis. In 2018, researchers at Brown University in the United States proposed a sepsis one-hour bundle (H1B) management for patients with sepsis, which included lactic acid level detection, blood cultures for broad-spectrum antibacterial drug use, administration of antibiotics, and fluid resuscitation within the first hour of treatment. Compared with conventional 3-h and 6-h mana
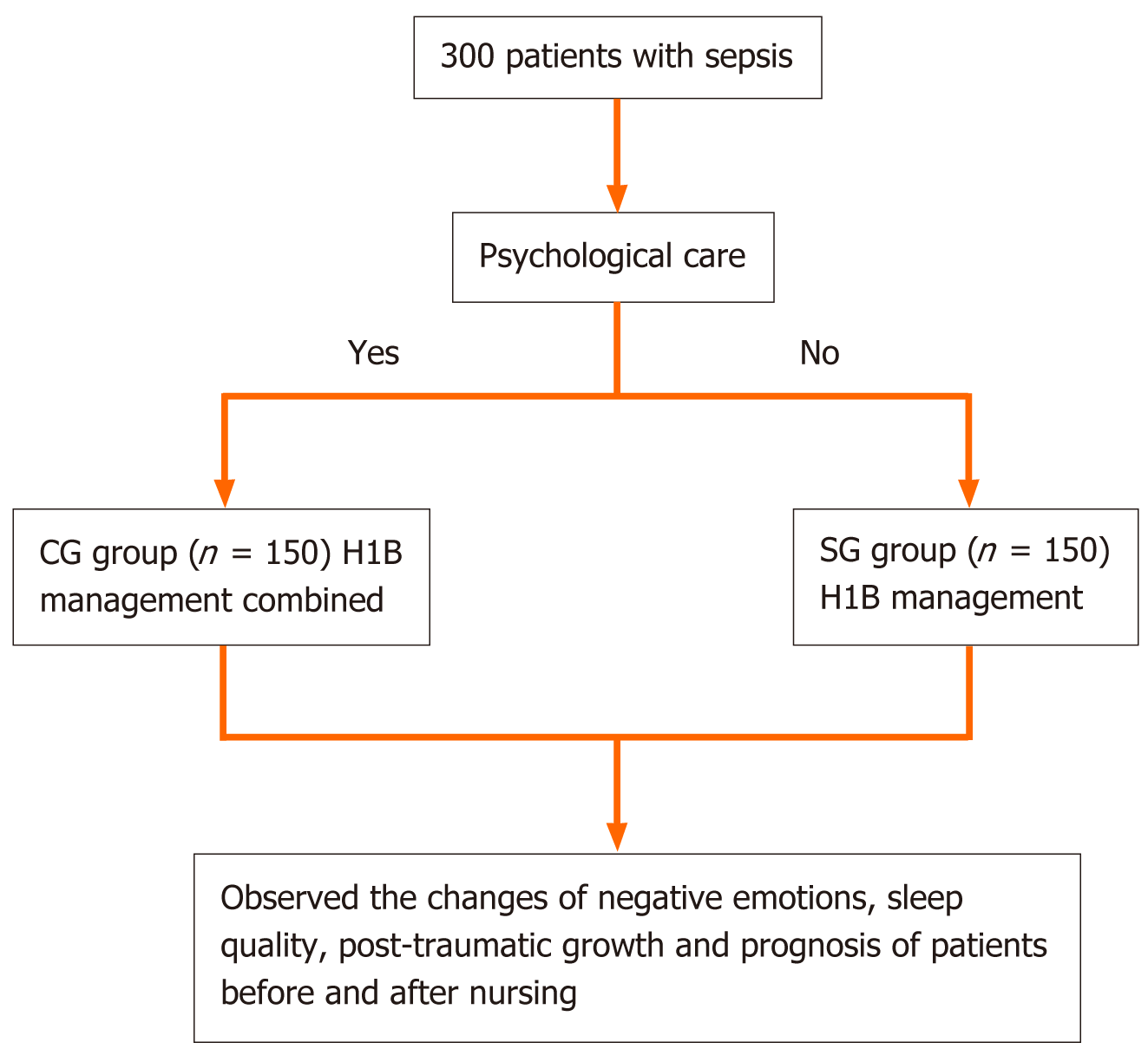
In a retrospective analysis, patients with sepsis admitted to Henan Provincial People’s Hospital between June 2022 and June 2023 were selected as study participants. After rigorous screening, 300 patients with sepsis were included in this study. Participants were classified into two groups according to the intervention methods used: a simple group (SG; n = 150) and a combined group (CG; n = 150). Patients in the SG underwent H1B management only, whereas those in the CG underwent H1B management combined with psychological intervention.
The inclusion criteria were as follows: (1) Patients between 18 and 75 years old; (2) patients meeting the diagnostic criteria for sepsis[1,8]; (3) all patients were admitted to the intensive care unit (ICU); (4) the baseline data, clinical characteristics and laboratory indices of all patients were complete; and (5) all participants indicated that they were willing and able to actively cooperate with the clinical nursing intervention. The following exclusion criteria applied: (1) Patients with cardiovascular disease, autoimmune disease, or malignant tumor; (2) pregnant or lactating women; (3) patients with abnormal liver, kidney, and other organ functions and mental abnormalities; and (4) patients who died, were brain-dead, or abandoned treatment within 24 h of admission.
The following diagnostic criteria for sepsis applied[1,8]: presence of organ dysfunction, quick Sequential Organ Failure Assessment (qSOFA) ≥ 2 score indicates sepsis; Sepsis 3.0 = infection + SOFA ≥ 2 score. The qSOFA score is based on the following items[9]: (1) Respiratory rate ≥ 22 times/min; (2) altered state of consciousness; (3) systolic blood pressure ≤ 100 mmHg. One point is allocated for each item and a score ≥ 2 points is considered suspected sepsis.
H1B management: The H1B intervention team is composed of 1 deputy chief physician, 1 attending physician, 2 physicians, and 8 nurses. The teams were divided into four groups that cooperated with each other in the nursing process of patients. All nurses underwent training in sepsis education, pharmacotherapy of sepsis, physiological function, role function, psychological intervention applied in this study, and identifying categories of patient behavior. Patient management involved the following: (1) Communication with the attending physician within 1 h after admission and blood gas analysis, blood cultures, administration of antibiotics, blood resuscitation, and vasoactive drug use within 1h of admission; (2) administration of anti-infection therapy, explaining to the patient the use of antibiotics and vasoactive drugs, with timely contact with the pharmacy to prepare a sufficient quantity of common antibiotics, including imipenem, piperacillin, vancomycin, cefoperazone, and sulbactam; and (3) mechanical ventilation in cases of hypoxia, tachycardia, hypotension, poor systemic perfusion, and pyrexia, with fluid resuscitation, and drugs such as milrinone to enhance cardiac function, vasopressors, subcutaneous pumping of insulin to lower blood sugar, and furosemide. A central venous catheter was placed for central venous pressure monitoring.
Psychological intervention: Psychological intervention is conducted after the patient's life is out of danger and involves several steps: (1) Obtaining the trust of the patient involves considering factors such as the patient’s cultural background, their personality, and psychological characteristics, using honest communication, and conveying a warm attitude to establish a good relationship with the patient; (2) the psychological intervention plan requires an analysis of the psychological problems of the patients and the formulation of an intervention tailored to the psychological characteristics of the patient. Effective psychological intervention should be provided to patients as early as possible; and (3) implementation of the plan requires good communication with patients, the provision of care, and demonstrating a warm demeanor to reduce the patient’s sense of loneliness. Through health education, sepsis knowledge promotion, and the distribution of informational leaflets, patients can develop an accurate understanding of sepsis. By explaining cases of successful treatment, patients can properly understand their disease and manage unnecessary worries and doubts. Prolonged hospitalization may prevent the patient from fulfilling their role in the family and society. Responsible nursing staff should enhance communication with patients, try to maintain the pre-admission healthy living habits of patients, meet their reasonable needs as much as possible, and help patients become familiar with the ward environment as soon as possible to reduce discomfort. This approach allows negative emotions to be effectively alleviated and enables patients to actively cooperate with clinical treatment, adopt an optimistic attitude towards completing rehabilitation goals at each stage, and achieve physical recovery.
Baseline characteristics, including sex, age, body mass index (BMI), and type of sepsis, were compared between the two groups.
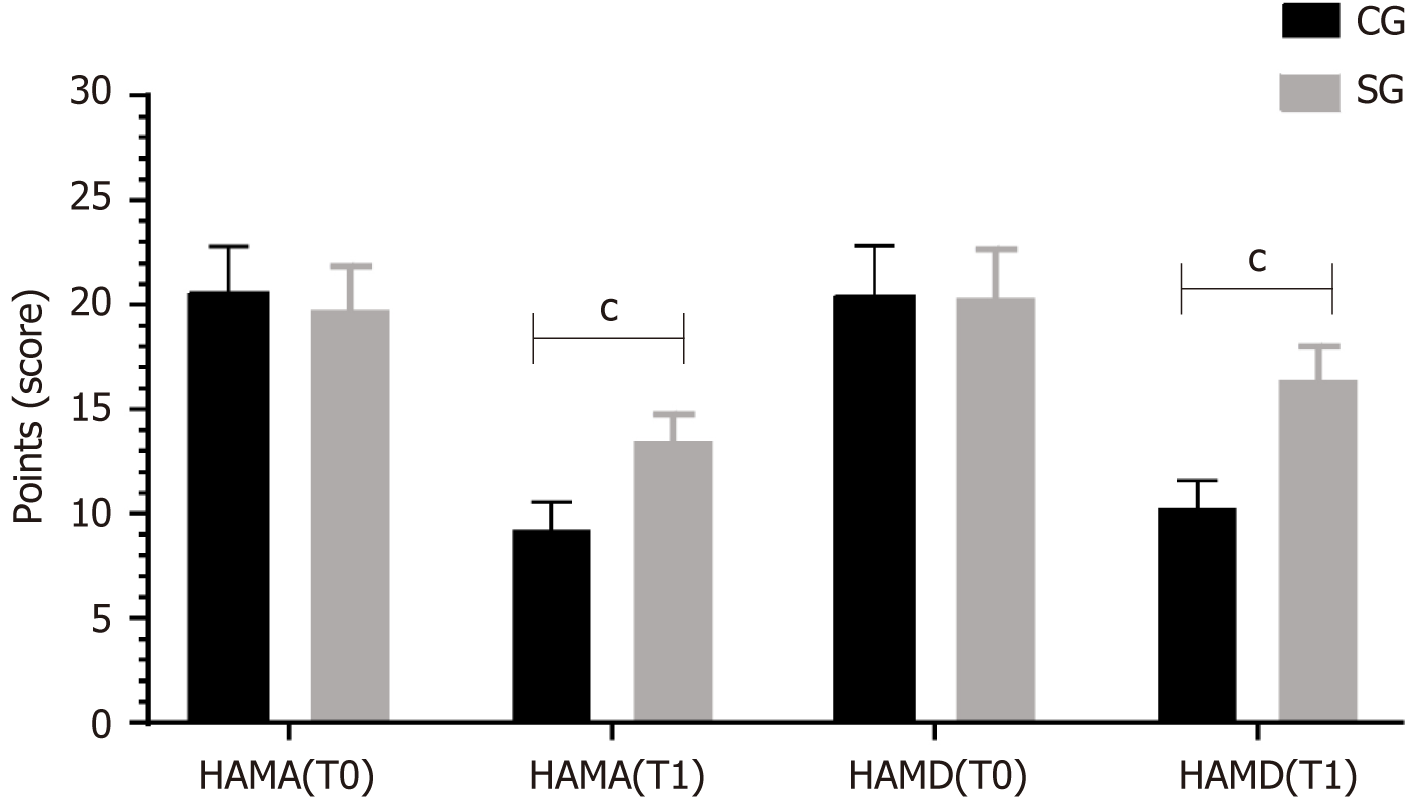
The emotional scores of the two groups were compared before (T0) and after (T1) the intervention. The Hamilton Anxiety scale (HAMA) and the Hamilton Depression scale (HAMD) were used to evaluate anxiety, depression, and mood[10]. The HAMA score rates the severity of anxiety as follows: < 7 indicates no anxiety, ≥ 7 indicates possible anxiety, ≥ 14 indicates certain anxiety, ≥ 21 indicates obvious anxiety, and > 29 indicates severe anxiety. The HAMD score rates the severity of depression as follows: < 7 indicates no depression, ≥ 7 indicates probable depression, ≥ 17 indicates certain depression, and > 24 indicates severe depression.
The sleep conditions at T0 and T1 were compared between the two groups. The Pittsburgh Sleep Quality Index (PSQI)[11] was used to evaluate sleep quality. The PSQI includes seven dimensions: time to fall asleep, sleep time, sleep quality, sleep efficiency, hypnotic drugs, daytime dysfunction, and sleep disorders. A 0- to 3-point scale is used with higher scores indicating worse sleep quality.
The post-traumatic growth levels at T0 and T1 were compared between the groups. Post Traumatic Growth Inventory (PTGI)[12] assesses levels of post-traumatic growth. PTGI evaluated the level of post-traumatic growth according to five dimensions: Appreciation of life, new possibilities, spiritual changes, relationships with others, and personal strength, with a total of 20 items. Each item is rated on a 0 to 5-point Likert scale, with 0 indicating that no such changes were experienced after trauma and 5 indicating considerable changes after trauma. The total score ranges from 0 to 100 with a higher score indicating more changes in post-traumatic growth.
The health survey status at T0 and T1 were compared between the groups. The MOS36-item short-form health survey (SF-36)[13] assesses quality of life according to eight aspects: mental health, general health status, physiological function, emotional function, physical pain, social function, energy, and physiological function. The final score of each aspect is calculated as follows: Final score = (actual score - lowest possible score for that aspect)/difference between lowest and highest possible scores for that aspect × 100%. The actual score is the sum of all the scores for a particular aspect and each dimension is scored on a scale from 0 to 100.
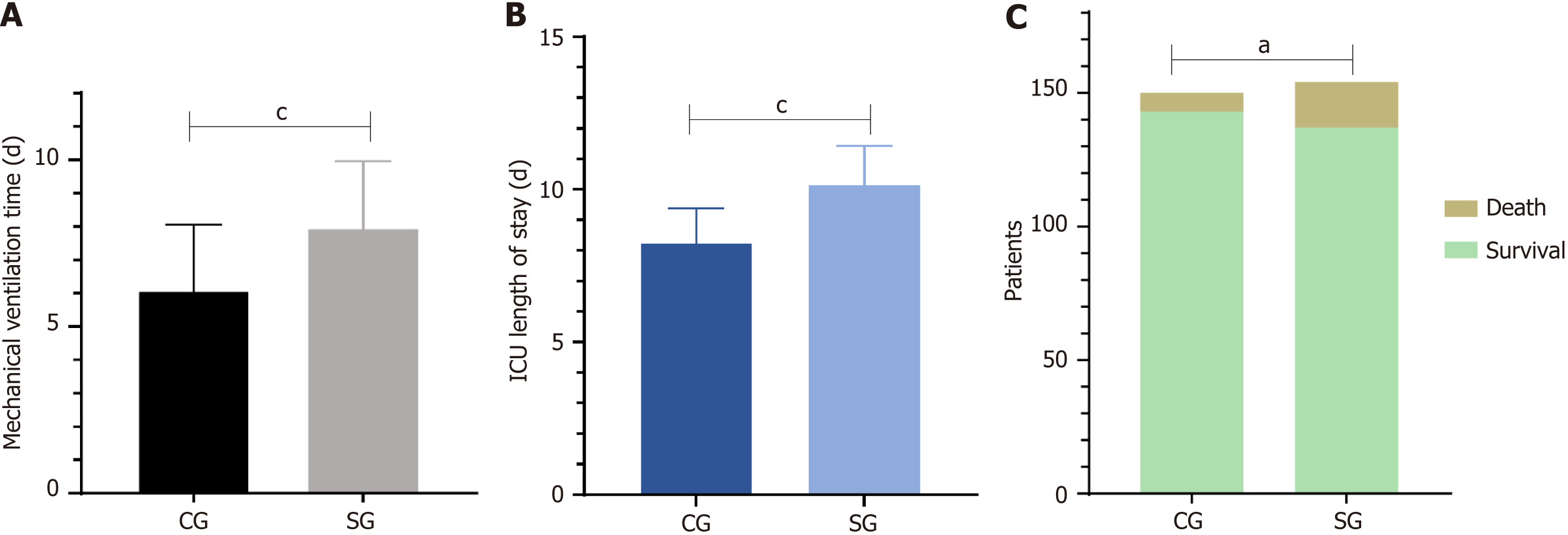
Comparison of prognosis between the groups. Differences in mechanical ventilation time, ICU stay time, and 28-d mortality between the two groups were compared.
Statistical analyses were performed using IBM SPSS statistics for Windows, version 26.0. The measurement data conforming to normal distribution are represented as mean ± SD, using a t test. Counting data are expressed as percentage of frequency (n%), by χ2 test. A P value < 0.05 was considered statistically significant.
A flowchart of the analysis in this study is presented in Figure 1. Sex, age, disease duration, BMI, and infection type were compared between the two groups (P > 0.05; Table 1).
| Index | CG (n = 150) | SG (n = 150) | χ2/t value | P value |
| Sex | 0.054 | 0.817 | ||
| Male | 81 (54.00) | 79 (52.67) | ||
| Female | 69 (46.00) | 71 (47.33) | ||
| Age (yr) | 58.27 ± 4.36 | 58.33 ± 4.51 | -0.130 | 0.897 |
| BMI (kg/m2) | 25.33 ± 1.57 | 25.29 ± 1.47 | 0.172 | 0.864 |
| Infection type | 0.272 | 0.965 | ||
| Abdominal infection | 39 (26.00) | 42 (28.00) | ||
| Respiratory tract infection | 60 (40.00) | 58 (38.67) | ||
| Bacteremia | 32 (21.33) | 33 (22.00) | ||
| Miscellaneous | 19 (12.67) | 17 (11.33) |
At T1, the HAMA and HAMD scores of the two groups were significantly lower than those at T0 (P < 0.05), and the scores of the CG group were lower than those of the SG group (P < 0.05; Figure 2).
At T1, the time to fall asleep, sleep time, sleep quality, sleep efficiency, hypnotic drugs, daytime dysfunction, sleep disturbance dimension score, and total PSQI score in the two groups were lower than those at T0 (P < 0.05). Each dimension score was lower in the CG group than that in the SG group (P < 0.05; Table 2).
| Dimensional | CG (n = 150) | SG (n = 150) | ||||||
| T0 | T1 | t value | P value | T0 | T1 | t value | P value | |
| Time to fall asleep | 2.72 ± 0.47 | 1.19 ± 0.53c | 0.058 | < 0.001 | 2.72 ± 0.50 | 1.75 ± 0.56 | 15.722 | < 0.001 |
| Sleep time | 2.65 ± 0.59 | 1.12 ± 0.38c | 26.512 | < 0.001 | 2.68 ± 0.47 | 1.83 ± 0.37 | 17.309 | < 0.001 |
| Sleep quality | 1.97 ± 0.37 | 1.09 ± 0.33c | 22.165 | < 0.001 | 1.94 ± 0.31 | 1.70 ± 0.46 | 5.292 | < 0.001 |
| Sleep efficiency | 2.38 ± 0.53 | 1.22 ± 0.50c | 19.259 | < 0.001 | 2.45 ± 0.51 | 1.78 ± 0.42 | 12.494 | < 0.001 |
| Hypnotic drugs | 2.38 ± 0.48 | 1.34 ± 0.48c | 18.717 | < 0.001 | 2.38 ± 0.48 | 1.84 ± 0.37 | 10.836 | < 0.001 |
| Daytime dysfunction | 2.17 ± 0.38 | 1.35 ± 0.48c | 16.416 | < 0.001 | 2.17 ± 0.38 | 1.66 ± 0.48 | 10.334 | < 0.001 |
| Dyssomnia | 2.53 ± 0.50 | 1.23 ± 0.42c | 24.126 | < 0.001 | 2.52 ± 0.50 | 1.65 ± 0.48 | 15.332 | < 0.001 |
| Total score | 16.80 ± 1.23 | 8.545 ± 1.18c | 59.284 | < 0.001 | 16.87 ± 1.22 | 12.22 ± 1.24 | 32.709 | < 0.001 |
At T1, the appreciation of life, new possibilities, spiritual changes, relationships with others, and personal power dimension scores of the PTGI in the two groups were higher than those at T0 (P < 0.05). Each dimension score was higher in the CG group than that in the SG group (P < 0.05) (Table 3).
| Dimension | CG (n = 150) | SG (n = 150) | ||||||
| T0 | T1 | t value | P value | T0 | T1 | t value | P value | |
| Appreciation of life | 15.33 ± 2.47 | 21.36 ± 3.28c | -17.984 | < 0.001 | 15.28 ± 2.53 | 17.55 ± 2.86 | -7.272 | < 0.001 |
| New possibilities | 8.54 ± 1.26 | 10.37 ± 1.75c | -10.401 | < 0.001 | 8.62 ± 1.18 | 9.13 ± 1.42 | -3.409 | < 0.001 |
| Mental changes | 4.76 ± 1.14 | 6.15 ± 1.28c | -9.966 | < 0.001 | 4.69 ± 1.16 | 5.12 ± 1.09 | -3.282 | < 0.001 |
| Relations with others | 16.27 ± 2.52 | 21.48 ± 3.35c | -15.204 | < 0.001 | 16.33 ± 2.48 | 18.67 ± 2.18 | -8.680 | < 0.001 |
| Individual force | 14.39 ± 2.25 | 17.65 ± 2.84c | 1-0.991 | < 0.001 | 14.41 ± 2.27 | 15.72 ± 2.53 | -4.707 | < 0.001 |
| Total score | 59.30 ± 4.51 | 77.01 ± 5.71c | -29.802 | 0.001 | 59.34 ± 4.47 | 66.19 ± 4.72 | -12.913 | < 0.001 |
In both groups, the SF-36 scores for mental health, general health status, physiological function, emotional function, physical pain, social function, energy, and physiological function were higher at T1 than those at T0 (P < 0.05). CG were higher than SG (P < 0.05) (Table 4).
| Dimension | CG (n = 150) | SG (n = 150) | ||||||
| T0 | T1 | t value | P value | T0 | T1 | t value | P value | |
| Mental health | 67.59 ± 6.73 | 81.13 ± 7.94c | -15.932 | < 0.001 | 68.15 ± 6.82 | 73.59 ± 7.24 | -6.706 | < 0.001 |
| General health status | 61.28 ± 6.35 | 85.21 ± 7.65c | -29.446 | < 0.001 | 61.57 ± 6.23 | 72.13 ± 7.08 | -13.728 | < 0.001 |
| Physiological functions | 59.37 ± 5.86 | 78.42 ± 7.53c | -24.444 | < 0.001 | 58.76 ± 5.94 | 64.53 ± 6.17 | -8.247 | < 0.001 |
| Emotional function | 53.45 ± 5.72 | 81.22 ± 7.52c | -36.013 | < 0.001 | 52.33 ± 5.68 | 74.28 ± 7.06 | -29.664 | < 0.001 |
| Body pain | 62.57 ± 6.18 | 82.54 ± 7.93c | -24.334 | < 0.001 | 62.49 ± 6.20 | 73.45 ± 7.18 | -14.145 | < 0.001 |
| Social function | 63.54 ± 6.20 | 85.70 ± 7.01c | -28.986 | < 0.001 | 62.87 ± 6.25 | 74.33 ± 6.95 | -15.007 | < 0.001 |
| Energy | 68.93 ± 6.84 | 84.51 ± 7.55c | -18.725 | < 0.001 | 68.79 ± 6.86 | 75.62 ± 7.34 | -8.317 | < 0.001 |
| Physiologic function | 80.82 ± 7.58 | 93.82 ± 3.69c | -18.890 | < 0.001 | 80.98 ± 7.68 | 86.15 ± 7.87 | -5.753 | < 0.001 |
The mechanical ventilation time of the CG group was (6.08 ± 2.07) d, ICU hospitalization time was (8.25 ± 1.13) d, and the 28-d mortality rate was 4.67%, which were significantly lower than those of the SG group [(7.96 ± 2.12) d, (10.15 ± 1.28) d, 11.33%] (P < 0.05; Figure 3).
Sepsis is a serious infection, which can cause host response disorders and lead to organ dysfunction. Without timely and effective treatment, severe sepsis and septic shock can develop, which are associated with high mortality[14]. The sepsis inflammatory response generates many inflammatory mediators through a cascade effect, causing infiltration of human tissues and organs, resulting in functional failure and shock to multiple organs, or death[15]. Optimal intervention is crucial to prevent organ dysfunction and improve patient quality of life and prognosis. Studies have shown[16] that cluster management can promote prognosis and improve the quality of life of critically ill patients, and psychological intervention with cocoa can alleviate anxiety and depression in patients with sepsis, effectively preventing the occurrence of post-traumatic stress disorder, and improving the long-term prognosis of patients. Therefore, to understand the emotional state, sleep status, and post-traumatic growth level of patients with sepsis, we explored the effect of a 1-h cluster management combined with psychological intervention in patients with sepsis. Cluster management nursing is an emerging clinical nursing model using various evidence-based intervention methods to improve nursing outcomes. Compared with the traditional model, cluster management has the characteristics of scientific validity, feasibility, and high efficiency, which reduces the blindness of clinical nursing and makes it more easily accepted by patients[17,18]. In this study, the HAMA and HAMD scores of patients in the CG group were significantly lower than those of the patients in the SG group, suggesting that 1-h cluster management combined with psychological intervention can effectively alleviate the negative mood of patients with sepsis. In this study, detection of lactic acid level was completed sequentially through H1B management intervention; blood culture specimens were obtained; and antibiotics, fluid resuscitation, and vasopressor therapy were administered. H1B management intervention also promotes knowledge about health and sepsis among patients, thereby improving their disease awareness levels. Furthermore, patient medication management and anti-infection care should be optimized to eliminate concerns about the disease. Treatment and nursing care were combined with psychological intervention to help patients face their disease and cooperate with the intervention, and with counseling to relieve anxiety and depression[19].
Our study also found that at T1, the PSQI scores of the CG group were markedly lower than those of the SG group, suggesting that H1B management combined with psychological intervention can improve sleep quality in patients admitted to the ICU with sepsis. This finding may be explained by the fact that negative emotions and respiratory dysfunction are the main reasons affecting sleep quality[20]. The combination of cluster management and psychological intervention improves patient understanding of the disease, and anti-infective drugs are prepared in advance to provide timely and effective treatment[21]. Careful monitoring of the patient’s condition and timely and effective management of hypoxia, hypotension, and poor systemic perfusion should also be performed. In addition to the psychological inter-vention, explaining successful cases of treatment, strengthening patient confidence, optimizing communication with patients, creating a comfortable ward environment, keeping patients happy, and improving negative emotions are also paramount[22]. Furthermore, intervention to reduce oxygen consumption and relieve shortness of breath is also important to improve sleep quality. In this study, at T1, the PTGI scores of the CG were markedly higher than those of the SG, indicating that H1B management combined with psychological intervention can accelerate the post-traumatic growth of patients with sepsis. Research has shown[23] that anxiety and depression in patients with cancer are closely related to post-traumatic growth; that is, lower levels of anxiety and depression promote post-traumatic growth in patients. Therefore, the post-traumatic growth of patients with sepsis may be related to cluster management and psychological interventions to improve negative emotions. Post-traumatic growth is closely related to coping styles and social support. Psychological nursing intervention can regulate the negative emotions of patients and improve patient understanding of the disease, providing them with the knowledge and confidence to cope with and overcome the disease[24].
By analyzing the quality of life of patients based on their health status, our study also found that at T1, the scores of each dimension of the SF-36 scale in the CG group were higher than those in the SG group, indicating that H1B manage
In summary, H1B management combined with psychological nursing intervention can effectively alleviate negative emotions in patients with sepsis, increase sleep quality, and enhance post-traumatic growth and quality of life.
Cluster management has been rapidly developing and increasingly recognized in the clinical care of critically ill patients. Psychological interventions have considerable impact on the mood, sleep, and quality of life of critically ill patients. Therefore, we analyzed the influence of one-hour bundle (H1B) management combined with psychological interventions in patients with sepsis.
Severe cases of sepsis are often accompanied by mood and sleep disorders. We postulate that H1B management combined with psychological interventions may have an important impact on patients with sepsis.
The purpose of this research was to discuss the effects of H1B management combined with psychological intervention on negative emotions, sleep quality, and post-traumatic growth in patients with sepsis and to provide a reference for clinical treatment.
Patients were divided into a group undergoing H1B management only (simple group, SG) and a group undergoing H1B management combined with psychological intervention (combination group, CG). The clinical data were retrospectively analyzed to compare the influence of negative emotions, sleep quality, post-traumatic growth, and prognosis of patients in the two groups before (T0) and after (T1) intervention.
At T1, the Hamilton Anxiety scale and Hamilton Depression scale scores of the CG group were significantly lower than those of the SG group. The Pittsburgh Sleep Quality Index score of the CG group was significantly lower than that of the SG group. The Post Traumatic Growth Inventory score of the CG group was significantly higher than that of the SG group. The MOS36-item short-form health survey scores of the CG group were higher than those of the SG group. The mechanical ventilation time, intensive care unit stay time, and 28-d mortality of the CG group were lower than those of the SG group. These differences were significant (P < 0.05).
H1B management combined with psychological nursing interventions can effectively alleviate the adverse emotions of patients with sepsis, increase quality of sleep, and enhance the level of post-traumatic growth and quality of life.
Future research should further explore the impact of H1B management combined with psychological intervention on patients with sepsis from the perspective of negative emotions, sleep quality, post-traumatic growth, and prognosis. These findings may provide a reference for nursing management and treatment strategies for patients with sepsis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kotera Y, United Kingdom S-Editor: Gong ZM L-Editor: A P-Editor: Zhang YL
| 1. | Fernando SM, Rochwerg B, Seely AJE. Clinical implications of the Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). CMAJ. 2018;190:E1058-E1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 88] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 2. | Komorowski M, Celi LA, Badawi O, Gordon AC, Faisal AA. The Artificial Intelligence Clinician learns optimal treatment strategies for sepsis in intensive care. Nat Med. 2018;24:1716-1720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 400] [Cited by in RCA: 535] [Article Influence: 76.4] [Reference Citation Analysis (0)] |
| 3. | Fleischmann C, Scherag A, Adhikari NK, Hartog CS, Tsaganos T, Schlattmann P, Angus DC, Reinhart K; International Forum of Acute Care Trialists. Assessment of Global Incidence and Mortality of Hospital-treated Sepsis. Current Estimates and Limitations. Am J Respir Crit Care Med. 2016;193:259-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1639] [Cited by in RCA: 2312] [Article Influence: 256.9] [Reference Citation Analysis (0)] |
| 4. | Pei F, Yao RQ, Ren C, Bahrami S, Billiar TR, Chaudry IH, Chen DC, Chen XL, Cui N, Fang XM, Kang Y, Li WQ, Li WX, Liang HP, Lin HY, Liu KX, Lu B, Lu ZQ, Maegele M, Peng TQ, Shang Y, Su L, Sun BW, Wang CS, Wang J, Wang JH, Wang P, Xie JF, Xie LX, Zhang LN, Zingarelli B, Guan XD, Wu JF, Yao YM; Shock and Sepsis Society of Chinese Research Hospital Association; China Critical Care Immunotherapy Research Group; International Federation of the Shock Societies (IFSS). Expert consensus on the monitoring and treatment of sepsis-induced immunosuppression. Mil Med Res. 2022;9:74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 29] [Reference Citation Analysis (0)] |
| 5. | Shen G, He Y, Ni J, Jiang L, Xia Z, Liu H, Pan S, Wang H, Hu W, Li X. Effects of comprehensive nursing on negative emotion and prognosis of patients with sepsis. Am J Transl Res. 2021;13:8221-8227. [PubMed] |
| 6. | Yang H, Wang W, Li Y, Tian L, Jing M, Hu Y. [Application effect of 1-hour bundle in the treatment of patients with sepsis]. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2019;31:1087-1090. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Jorgensen AL. Nurse Influence in Meeting Compliance With the Centers for Medicare and Medicaid Services Quality Measure: Early Management Bundle, Severe Sepsis/Septic Shock (SEP-1). Dimens Crit Care Nurs. 2019;38:70-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Esposito S, De Simone G, Boccia G, De Caro F, Pagliano P. Sepsis and septic shock: New definitions, new diagnostic and therapeutic approaches. J Glob Antimicrob Resist. 2017;10:204-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 136] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 9. | Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15803] [Cited by in RCA: 17171] [Article Influence: 1907.9] [Reference Citation Analysis (2)] |
| 10. | Zhang S, Chen H, Zhang M, Sun X, Liu X. Reduction of depression symptoms in laryngeal cancer patients receiving psychology services. Am J Transl Res. 2020;12:6637-6645. [PubMed] |
| 11. | Zhang C, Zhang H, Zhao M, Li Z, Cook CE, Buysse DJ, Zhao Y, Yao Y. Reliability, Validity, and Factor Structure of Pittsburgh Sleep Quality Index in Community-Based Centenarians. Front Psychiatry. 2020;11:573530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 75] [Article Influence: 15.0] [Reference Citation Analysis (1)] |
| 12. | Cormio C, Muzzatti B, Romito F, Mattioli V, Annunziata MA. Posttraumatic growth and cancer: a study 5 years after treatment end. Support Care Cancer. 2017;25:1087-1096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 13. | Ware JK, Owens BD, Akelman MR, Karamchedu NP, Fadale PD, Hulstyn MJ, Shalvoy RM, Badger GJ, Fleming BC. Preoperative KOOS and SF-36 Scores Are Associated With the Development of Symptomatic Knee Osteoarthritis at 7 Years After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2018;46:869-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Marchand EP, Villemure JG, Rubin J, Robitaille Y, Ethier R. Solitary osteochondroma of the thoracic spine presenting as spinal cord compression. A case report. Spine (Phila Pa 1976). 1986;11:1033-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 43] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 15. | Font MD, Thyagarajan B, Khanna AK. Sepsis and Septic Shock - Basics of diagnosis, pathophysiology and clinical decision making. Med Clin North Am. 2020;104:573-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 199] [Article Influence: 39.8] [Reference Citation Analysis (0)] |
| 16. | Sanghvi S, Podlog M, Aycock RD. Does the Severe Sepsis and Septic Shock Early Management Bundle (SEP-1) Improve Survival in Septic Adults? Ann Emerg Med. 2019;73:363-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Chen X, Deng C, Tan G, Zheng H, Yang T, Zhang X. Application efficacy of bundled nursing management in care of elderly patients with pressure ulcers. Am J Transl Res. 2021;13:6738-6744. [PubMed] |
| 18. | Pun BT, Balas MC, Barnes-Daly MA, Thompson JL, Aldrich JM, Barr J, Byrum D, Carson SS, Devlin JW, Engel HJ, Esbrook CL, Hargett KD, Harmon L, Hielsberg C, Jackson JC, Kelly TL, Kumar V, Millner L, Morse A, Perme CS, Posa PJ, Puntillo KA, Schweickert WD, Stollings JL, Tan A, D'Agostino McGowan L, Ely EW. Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15,000 Adults. Crit Care Med. 2019;47:3-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 397] [Cited by in RCA: 629] [Article Influence: 104.8] [Reference Citation Analysis (0)] |
| 19. | Uffen JW, Oosterheert JJ, Schweitzer VA, Thursky K, Kaasjager HAH, Ekkelenkamp MB. Interventions for rapid recognition and treatment of sepsis in the emergency department: a narrative review. Clin Microbiol Infect. 2021;27:192-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 20. | Simor P, Harsányi A, Csigó K, Miklós G, Lázár AS, Demeter G. Eveningness is associated with poor sleep quality and negative affect in obsessive-compulsive disorder. J Behav Addict. 2018;7:10-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Odawara K. [Biochemical study of diphenylhydantoin gingival hyperplasia--effect of DPH on intermolecular cross-links of rat gingival collagen]. Kanagawa Shigaku. 1987;21:519-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 22. | Ding X, Yao J. Peer Education Intervention on Adolescents' Anxiety, Depression, and Sleep Disorder during the COVID-19 Pandemic. Psychiatr Danub. 2020;32:527-535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 23. | Gori A, Topino E, Sette A, Cramer H. Pathways to post-traumatic growth in cancer patients: moderated mediation and single mediation analyses with resilience, personality, and coping strategies. J Affect Disord. 2021;279:692-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 24. | Shi G, Shi T, Liu Y, Cai Y. Relationships between dyadic coping, intimate relationship and post-traumatic growth in patients with breast cancer: A cross-sectional study. J Adv Nurs. 2021;77:4733-4742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 25. | Nannan Panday RS, Minderhoud TC, Chantalou DS, Alam N, Nanayakkara PWB. Health related quality of life in sepsis survivors from the Prehospital Antibiotics Against Sepsis (PHANTASi) trial. PLoS One. 2019;14:e0222450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 26. | Rababa M, Bani Hamad D, Hayajneh AA. Sepsis assessment and management in critically Ill adults: A systematic review. PLoS One. 2022;17:e0270711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 16] [Reference Citation Analysis (0)] |
| 27. | Lasater KB, Sloane DM, McHugh MD, Cimiotti JP, Riman KA, Martin B, Alexander M, Aiken LH. Evaluation of hospital nurse-to-patient staffing ratios and sepsis bundles on patient outcomes. Am J Infect Control. 2021;49:868-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 28. | Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, Lemeshow S, Osborn T, Terry KM, Levy MM. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis. N Engl J Med. 2017;376:2235-2244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1077] [Cited by in RCA: 1393] [Article Influence: 174.1] [Reference Citation Analysis (0)] |