Published online Dec 19, 2024. doi: 10.5498/wjp.v14.i12.1982
Revised: October 29, 2024
Accepted: November 11, 2024
Published online: December 19, 2024
Processing time: 74 Days and 2.7 Hours
Alzheimer’s disease (AD) is a common type of dementia due to neuronal impair
We report a case of a 68-year-old woman with a 2-year history of AD. She initially presented with memory loss, progressively more severe, leading to a depressive and anxious status. The clinical symptoms also included severe sleep distur
This case report suggested that bright light therapy can have a positive effect on sleep quality in elderly patients with AD and can be used as an effective and safe non-pharmacological treatment.
Core Tip: This report describes the case of a patient who developed Alzheimer’s disease, accompanied by sleep disorders, depression and anxiety; we provided bright-light therapy (BLT) to improve her sleep quality. BLT can reduce the duration of daily sleep and nighttime restlessness, with a higher efficacy than medications in improving sleep. This case report suggested that BLT can have a positive effect on sleep quality in elderly patients with Alzheimer’s disease and can be used as an effective and safe non-pharmacological treatment.
- Citation: Mei X, Zou CJ, Zheng CY, Hu J, Zhou DS. Effect of bright-light therapy on depression and anxiety of a patient with Alzheimer’s disease combined with sleep disorder: A case report. World J Psychiatry 2024; 14(12): 1982-1987
- URL: https://www.wjgnet.com/2220-3206/full/v14/i12/1982.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i12.1982
Alzheimer’s disease (AD) is a neurodegenerative disorder with various clinical manifestations, including cognitive decline, mental and behavioral alterations, and sleep disturbances[1]. The bidirectional relationship between AD and sleep disorders has been investigated extensively; sleep disturbances are a risk factor for AD and also a consequence of this disease[2]. A growing body of literature has examined sleep quality and cognitive function in elderly patients with AD[3]. Sleep disturbances exacerbate systemic inflammation and increase β-amyloid accumulation; β-amyloid a one of the major factors in AD pathogenesis[4]. Therefore, improving of sleep quality might have beneficial effect in AD. The cognitive decline cannot be completely eliminated; however, reducing sleep disturbances could prolong the cognitive abilities of patients with AD[5]. Multiple pharmacological and non-pharmacological approaches have been proposed for clinical treatment[6]. Bright-light therapy (BLT) is a non-pharmacological method usually adopted in elderly patients with sleep disorders[7,8]. Previous studies have shown that BLT can reduce depression and improve sleep quality in patients with mild cognitive impairment and neurodegenerative diseases[9-11]. Therefore, BLT is increasingly reco
A 68-year-old woman presented with progressive memory loss, cognitive decline, and symptoms of dementia.
In the month before admission, she started having poor nighttime sleep quality or insomnia and being active in her room at night, heavily affecting her family’s rest, and was accompanied to our hospital for treatment.
The patient’s illness began 2 years prior, initially with short-term memory loss and incoherent speech. Later, the symptoms gradually worsened, and the patient started forgetting what she said immediately before, being unable to return home after a walk, and requiring assistance by the police and supervision from her family in daily life. She frequently believed her family stole her possessions and became depressed, irritable, and suspicious, often reprimanding her family members without reason.
The patient denied any family history of AD.
At the initial consultation, the patient was conscious and cooperative in conversation; however, she could not recall immediate events or what she ate for her last meal and was not aware of being in the hospital. She was poorly oriented in time and space and towards other persons, with reduced volitional activity and lack of self-awareness.
Blood counts, ultrasensitive C-reactive protein, and biochemistry were unremarkable.
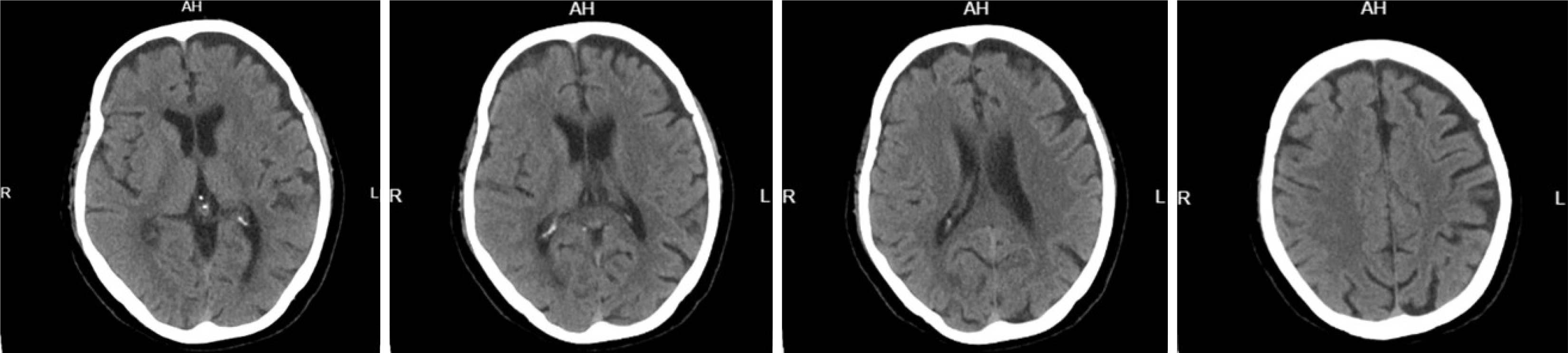
A head computed tomography scan showed evident cerebral atrophy and no other organic lesions or cerebral infarct foci (Figure 1). No other somatic diseases possibly causing mental disorders were noted, and she had no history of hyper
The patient was diagnosed using the Diagnostic and Statistical Manual of Mental Disorders, fifth edition criteria[13]. The patient was diagnosed with AD by two research psychiatrists and provision of informed consent. The cognitive level was evaluated by Mini-Mental State Examination (MMSE) score < 17, 20, and 24 in patient with education levels of illiteracy, primary school, and junior high school, respectively[14]. The disease course was more than 3 months. Donepezil or memantine was used to improve the cognitive level. The patient has no history of other severe mental illnesses. The MMSE of the patient score was 17. Based on these findings, the patient was diagnosed with AD accompanied by psycho-behavioral symptoms and was subsequently hospitalized.
The phototherapy equipment (Figure 2) was designed by the Geriatrics Center of the Ningbo Kangning Hospital as described in our previous study[15]. It was mounted on a portable cart, and the intensity of the light source was adjustable from 0 to 20000 lux. The treatment was provided for 30 minutes twice a day, during 8:30 am to 9:00 am and 16:30 pm to 17:00 pm. The patient was seated 0.5-1 m from the light source; the light intensity provided was 14000 lux, for a 4-week course of treatment. The patient faced the light source and sited in a comfortable chair. After that, the nurse secures the portable cart and turns the light to patient, and reminds the patient that he or she is ready to begin treatment. During the course of treatment, patient was asked to remain quiet and not to get up and walk around. The patient was administered memantine oral solution 7.5 mL/quaque mane and carboplatin capsules 3 mg/bis in die, for intellectual stimulation, and olanzapine tablets 5 mg/day for antipsychotic treatment. Moreover, she underwent light therapy to improve the poor nighttime sleep quality.
After 4 weeks of hospitalization, the cognitive level was stable (MMSE: 18), whereas the psychiatric symptoms decreased, and the family reported improved mood and disappearance of paranoia. The patient’s sleep quality markedly improved, with notable decrease in daytime sleep, increase in nighttime sleep, and absence of nocturnal activity.
We presented a case of severe AD complicated with sleep disturbances, treated with BLT. Sleep problems are common in patients with AD and place a high burden on their caregivers. Several medications can be used to increase sleep duration and improve its quality; however, the risk of side effects can also increase. Non-pharmacological treatment could be useful to avoid the risk of using multiple drugs in elderly patients with comorbidities. BLT can help regulate the sleep-wake cycle in older adults with dementia[16]. In a previous study, BLT was suggested to supplement daylight as a trigger for the suprachiasmatic nucleus (SCN)[17]. It can be used at any time during the day to promote wakefulness and reduce daytime sleep, realigning the patients’ circadian rhythm to the typical sleep timings[18]. In this study, we provided BLT after breakfast and after dinner to maintain the wakeful state in the patient. There is a 4-hour interval between the time of BLT after dinner and the time of going to sleep at night, so it does not affect the patient’s sleep. Additionally, an adequate sleep duration and circadian rhythm have a beneficial effect on the gut microbiota and digestive function[19].
Moreover, BLT is a well-established method to improve mood in seasonal affective disorder[20], and the effect of BLT on patients with non-seasonal depression has also been examined in a large number of clinical trials, as reported in a review[21]. In this case, the patient presented with depressive symptoms; with BLT, these symptoms markedly improved, though the cognitive dysfunction remained stable. The BLT mechanism of action has been investigated in previous studies; intrinsically photosensitive retinal ganglion cells project to the SCN and mediate the effects of light on learning. Mood regulation by light, on the other hand, requires an SCN-independent pathway linking intrinsically photosensitive retinal ganglion cells to a previously unrecognized thalamic region, named perihabenular nucleus[22]. The SCN can also be stimulated by BLT to enhance spatial memory[23]. BLT is known to improve nighttime sleep. A quality night’s sleep can be rejuvenating and enhance the patient’s ability to concentration during the daytime. Although BLT was reported to enhance spatial memory, whether it can improve memory to recall immediate events and become more oriented in time and space for those with reduced volitional activity and lack of self-awareness need to be studied in future.
BLT can also have positive effects on delirium and sundowning syndrome[24]. Circadian-related disorders and alterations in sleep-wake patterns are common complaints in elderly individuals, especially those diagnosed with AD[25]. Light is the main stimulus of the circadian melatoninergic system; therefore, patients with AD should be encouraged to walk outdoors in natural light. The strength and limitation of BLT: Although very few patients reported transient side effects including headaches and eyestrain during the course of the BLT, it was still an effectiveness non-invasive therapy for clinical application. Comparing to medication, BLT is suitable for patients with comorbid conditions, such as hypertension, diabetes mellitus, or a history of stroke, and reduces the physical burden of drug interactions on older adults with multiple health issues. Combined pharmacological and non-pharmacological measures could be adopted in elderly patients before considering multiple pharmacological measures.
This case report suggested that BLT can have a positive effect on sleep quality in elderly patients with AD and can be used as an effective and safe non-pharmacological treatment.
The authors wish to acknowledge the patient, his family and his medical staff for their assistance.
| 1. | Mander BA, Winer JR, Jagust WJ, Walker MP. Sleep: A Novel Mechanistic Pathway, Biomarker, and Treatment Target in the Pathology of Alzheimer's Disease? Trends Neurosci. 2016;39:552-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 312] [Cited by in RCA: 322] [Article Influence: 35.8] [Reference Citation Analysis (0)] |
| 2. | Irwin MR, Vitiello MV. Implications of sleep disturbance and inflammation for Alzheimer's disease dementia. Lancet Neurol. 2019;18:296-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 340] [Article Influence: 56.7] [Reference Citation Analysis (0)] |
| 3. | Dzierzewski JM, Dautovich N, Ravyts S. Sleep and Cognition in Older Adults. Sleep Med Clin. 2018;13:93-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 171] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 4. | Irwin MR, Olmstead R, Carroll JE. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol Psychiatry. 2016;80:40-52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1387] [Cited by in RCA: 1257] [Article Influence: 139.7] [Reference Citation Analysis (0)] |
| 5. | Wang C, Holtzman DM. Bidirectional relationship between sleep and Alzheimer's disease: role of amyloid, tau, and other factors. Neuropsychopharmacology. 2020;45:104-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 342] [Article Influence: 68.4] [Reference Citation Analysis (0)] |
| 6. | Blackman J, Swirski M, Clynes J, Harding S, Leng Y, Coulthard E. Pharmacological and non-pharmacological interventions to enhance sleep in mild cognitive impairment and mild Alzheimer's disease: A systematic review. J Sleep Res. 2021;30:e13229. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 79] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 7. | Lin TH, Yang CC, Lee SY, Chang CM, Tsai IJ, Wei CY, Yang CP. The effect of bright light therapy in migraine patients with sleep disturbance: A prospective, observational cohort study protocol. Front Aging Neurosci. 2022;14:1041076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 8. | van Maanen A, Meijer AM, van der Heijden KB, Oort FJ. The effects of light therapy on sleep problems: A systematic review and meta-analysis. Sleep Med Rev. 2016;29:52-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 302] [Cited by in RCA: 240] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 9. | Sekiguchi H, Iritani S, Fujita K. Bright light therapy for sleep disturbance in dementia is most effective for mild to moderate Alzheimer's type dementia: a case series. Psychogeriatrics. 2017;17:275-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Lin F, Su Y, Weng Y, Lin X, Weng H, Cai G, Cai G. The effects of bright light therapy on depression and sleep disturbances in patients with Parkinson's disease: a systematic review and meta-analysis of randomized controlled trials. Sleep Med. 2021;83:280-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 11. | Videnovic A, Klerman EB, Wang W, Marconi A, Kuhta T, Zee PC. Timed Light Therapy for Sleep and Daytime Sleepiness Associated With Parkinson Disease: A Randomized Clinical Trial. JAMA Neurol. 2017;74:411-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 171] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 12. | Ooms S, Ju YE. Treatment of Sleep Disorders in Dementia. Curr Treat Options Neurol. 2016;18:40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 74] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 13. | First MB. Diagnostic and statistical manual of mental disorders, 5th edition, and clinical utility. J Nerv Ment Dis. 2013;201:727-729. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 267] [Article Influence: 22.3] [Reference Citation Analysis (0)] |
| 14. | Li H, Jia J, Yang Z. Mini-Mental State Examination in Elderly Chinese: A Population-Based Normative Study. J Alzheimers Dis. 2016;53:487-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 338] [Article Influence: 48.3] [Reference Citation Analysis (0)] |
| 15. | Mei X, Zou C, Si Z, Xu T, Hu J, Wu X, Zheng C. Antidepressant effect of bright light therapy on patients with Alzheimer's disease and their caregivers. Front Pharmacol. 2023;14:1235406. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Tan JSI, Cheng LJ, Chan EY, Lau Y, Lau ST. Light therapy for sleep disturbances in older adults with dementia: a systematic review, meta-analysis and meta-regression. Sleep Med. 2022;90:153-166. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Pail G, Huf W, Pjrek E, Winkler D, Willeit M, Praschak-Rieder N, Kasper S. Bright-light therapy in the treatment of mood disorders. Neuropsychobiology. 2011;64:152-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 181] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 18. | Faulkner SM, Bee PE, Meyer N, Dijk DJ, Drake RJ. Light therapies to improve sleep in intrinsic circadian rhythm sleep disorders and neuro-psychiatric illness: A systematic review and meta-analysis. Sleep Med Rev. 2019;46:108-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 63] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 19. | Matenchuk BA, Mandhane PJ, Kozyrskyj AL. Sleep, circadian rhythm, and gut microbiota. Sleep Med Rev. 2020;53:101340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 262] [Article Influence: 52.4] [Reference Citation Analysis (0)] |
| 20. | Pjrek E, Friedrich ME, Cambioli L, Dold M, Jäger F, Komorowski A, Lanzenberger R, Kasper S, Winkler D. The Efficacy of Light Therapy in the Treatment of Seasonal Affective Disorder: A Meta-Analysis of Randomized Controlled Trials. Psychother Psychosom. 2020;89:17-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 21. | Al-Karawi D, Jubair L. Bright light therapy for nonseasonal depression: Meta-analysis of clinical trials. J Affect Disord. 2016;198:64-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 124] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 22. | Fernandez DC, Fogerson PM, Lazzerini Ospri L, Thomsen MB, Layne RM, Severin D, Zhan J, Singer JH, Kirkwood A, Zhao H, Berson DM, Hattar S. Light Affects Mood and Learning through Distinct Retina-Brain Pathways. Cell. 2018;175:71-84.e18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 311] [Article Influence: 44.4] [Reference Citation Analysis (0)] |
| 23. | Huang X, Huang P, Huang L, Hu Z, Liu X, Shen J, Xi Y, Yang Y, Fu Y, Tao Q, Lin S, Xu A, Xu F, Xue T, So KF, Li H, Ren C. A Visual Circuit Related to the Nucleus Reuniens for the Spatial-Memory-Promoting Effects of Light Treatment. Neuron. 2021;109:347-362.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 24. | Zou C, Mei X, Li X, Hu J, Xu T, Zheng C. Effect of light therapy on delirium in older patients with Alzheimer's disease-related dementia. J Psychiatr Res. 2022;149:124-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 25. | Peter-Derex L, Yammine P, Bastuji H, Croisile B. Sleep and Alzheimer's disease. Sleep Med Rev. 2015;19:29-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 301] [Article Influence: 30.1] [Reference Citation Analysis (0)] |