Published online Dec 19, 2024. doi: 10.5498/wjp.v14.i12.1815
Revised: October 5, 2024
Accepted: October 28, 2024
Published online: December 19, 2024
Processing time: 187 Days and 22.1 Hours
Eating disorders (EDs) have increasingly become a public health problem glo
To estimate the burden of EDs in children and adolescents (ages 5-19 years) at the global, regional, and national levels.
Retrieved from Global Burden of Disease Study 2019 for EDs, including anorexia nervosa and bulimia nervosa, we extracted the disability-adjusted life years (DALYs) and prevalence rates with 95% uncertainty intervals between 1990-2019. The temporal trends of the DALYs and prevalence rates of EDs were assessed according to the estimated annual percentage changes.
In our study, we found that the burden of EDs continuously increased globally from 1990 to 2019. Although females accounted for more EDs cases, the burden of EDs in males had a greater increment. Meanwhile, the burden of EDs was associated with the high sociodemographic index (SDI) over the past 30 years and the human development indexes in 2019.
EDs, predominantly in high-income countries, are rising globally, especially in Asia, highlighting the need for resource planning and medical policy prioritization across all SDI quintiles.
Core Tip: This study offered a comprehensive assessment of the global burden of eating disorders (EDs) among children and adolescents over three decades using data from the Global Burden of Disease Study 2019. We observed a continuous increase in the disability-adjusted life years and prevalence rates of anorexia nervosa and bulimia nervosa worldwide. Notably, while EDs predominantly affected females, the relative increase in burden was more significant among males. The study highlighted an association between higher sociodemographic index regions and increased EDs burden, underscoring the need for targeted healthcare strategies across varying socioeconomic landscapes.
- Citation: Chen Q, Huang S, Peng JY, Xu H, Wang P, Shi XM, Li SQ, Luo R, Zhang W, Shi L, Peng Y, Wang XH, Tang XW. Trends and prevalence of eating disorders in children and adolescents. World J Psychiatry 2024; 14(12): 1815-1826
- URL: https://www.wjgnet.com/2220-3206/full/v14/i12/1815.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i12.1815
Eating disorders (EDs), which are characterized by abnormal eating habits, overconcern with body image and weight-control behaviors, are severe psychiatric illnesses that include anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED). With the highest mortality rate among all psychiatric disease, AN is a serious mental disorder typified by starvation and malnutrition[1]. BN is characterized by repetitive episodes of binge eating followed by compensatory actions to avoid weight gain[2]. In addition to the impairment in psychosocial functioning and physical health, compared with those without these disorders, people with EDs have higher health care costs, and for those who die prematurely, lost lifetime income[3].
EDs can affect people of all ages, genders, ethnicities, sexual orientations, and geographic locations. There is evidence of sex differences, as females have an 8 times greater likelihood of having AN or BN than males, and periods of elevated risk of onset, including childhood and adolescence. These disorders can lead to significant impairments in cognitive development, physical health, and psychosocial function, which can go undetected for months or even years. At the same time, there has been a 25% increase in the prevalence of EDs globally[4,5]. Thus, focusing on children and adolescents is essential for implementing early intervention strategies and improving long-term outcomes.
The Global Burden of Disease (GBD) Study 2019, a comprehensive global effort, involves the measurement of the burden of mental disorders using disability-adjusted life years (DALYs) to assess the disparity between the current health status and an ideal situation where the entire population is disease free to an advanced age.
In this study, we used GBD 2019 data to estimate the trends and annual changes in DALYs and the prevalence of EDs in children and adolescents at the regional, national, and global levels. Furthermore, we determined the association between the burden of EDs and level of development as quantified by human development indices (HDIs).
Covering 204 countries and regions, GBD 2019 offered a comprehensive assessment of the global health burden of 369 diseases and injuries from 1990 to 2019. Details on the general methods used are available on the official website (GBD, Institute for Health Metrics and Evaluation; healthdata.org). The GBD 2019 divided 204 countries into 21 regions, and these countries or territories were stratified into five regions based on the sociodemographic index (SDI): Low, low-middle, middle, high-middle, and high. Furthermore, the HDIs of all countries were obtained from the official website (Human Development Index, Human Development Reports; undp.org)[6].
The burden of EDs was quantified by the rates of DALYs and prevalence rates retrieved from the Global Health Data Exchange query tool (VizHub, GBD Results; healthdata.org), with 95% uncertainty intervals (95%UIs) calculated according to the GBD 2019 global age-standard population. We also described the burden of EDs subdivided type: AN and BN.
EDs were defined based on the criteria from the International Classification of Diseases (ICD) and the diagnostic and statistical manual of mental disorders (DSM), including different versions of the ICD (ICD-9 and ICD-10) and DSM (DSM-5, DSM-III, DSM-III-R, DSM-IV, and DSM-IV-TR). There were no EDs cases before the age of 5 years, as assumed by the GBD 2019, which was in accordance with the corresponding cause in the EDs death model. Considering that the GBD 2019 has no precisely designated age categories (i.e., age < 10 is considered a child, age 10-19 is considered an adolescent), we divided the children and adolescents into three groups by age: 5-9 years, 10-14 years, and 15-19 years[7,8].
The estimated annual percentage change (EAPC) was evaluated to clarify the secular trends in the burden of EDs more fully. When calculating the EAPC, the calendar year used as the variable X and ln (rate) used as the variable Y were fitted to a regression line: Y = α + βx + ε, where the EAPC was calculated [100 × (exp (β) - 1)] with its 95%UI obtained from the fitted regression model. An upward trend could be considered if the EAPC > 0 and 95%UI > 0. Conversely, a downward trend could be considered if the EAPC > 0 and 95%UI > 0. Otherwise, the rates were regarded as stable.
Along with the EAPCs and HDIs in 2019, the associations between the EAPCs and rates in 1990 were assessed at the national level using Pearson’s correlation analysis and scatterplots. The HDIs indicate the availability and quality of medical services in each country.
R (version 4.1.3, R core team) was used to perform all the statistical procedures. All P values < 0.05 were considered statistically significant.
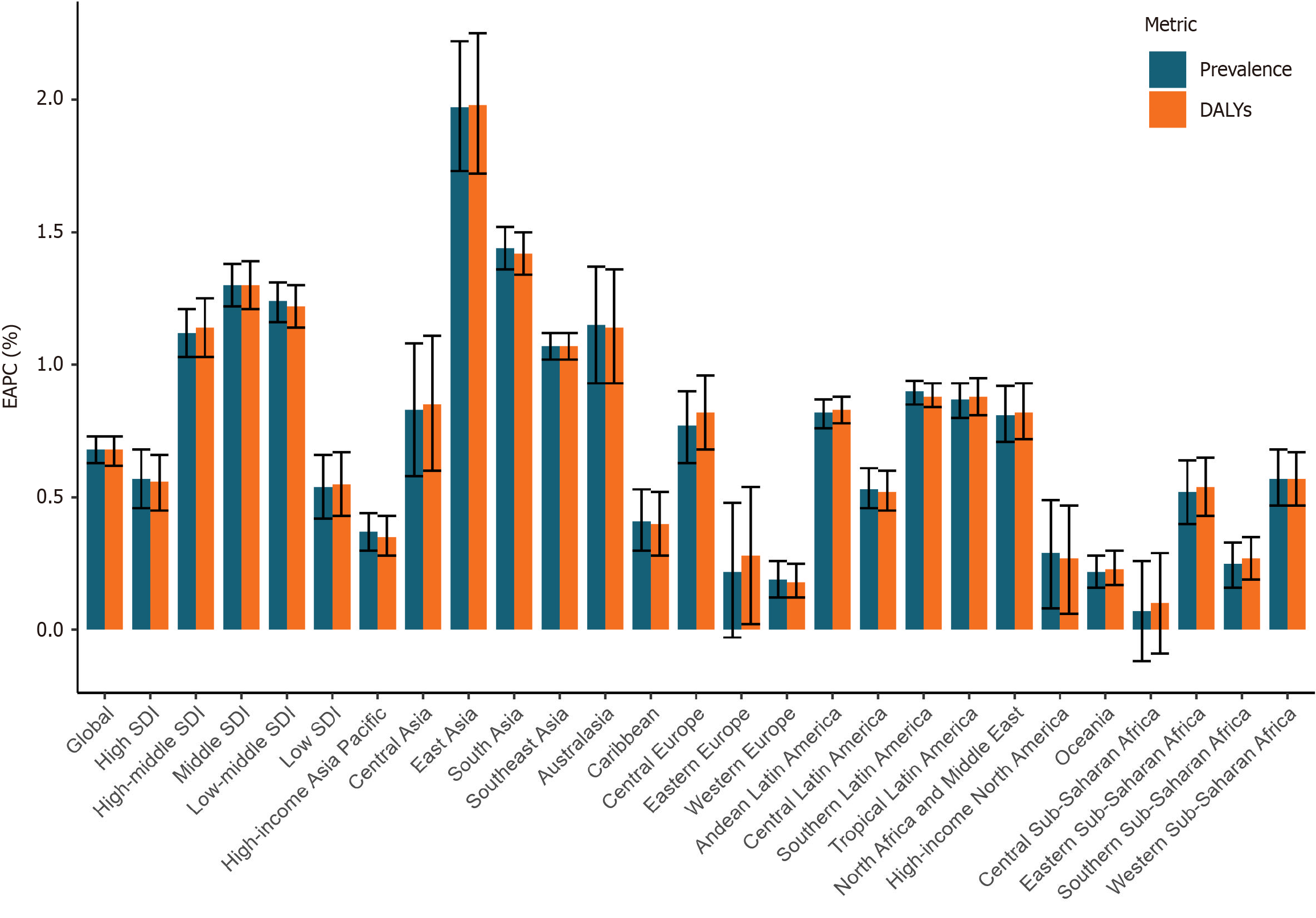
As shown in Table 1, the DALY rate of EDs at the global level gradually increased from 11.03 (95%UI: 6.12-17.72) per 100000 people in 1990 to 12.92 (95%UI: 7.12-20.97) per 100000 people in 2019, with an EAPC of 0.68 (95%UI: 0.62-0.73; Figure 1). Moreover, an increasing trend was also observed in the prevalence rate from 116.66 (95%UI: 79.78-172.01) in 1990 per 100000 people to 137.36 (95%UI: 93.24-203.11) in 2019 per 100000 people, with an average rate of 0.68 (95%UI: 0.63-0.73; Figure 1).
| Prevalence (95%UI) | DALYs (95%UI) | |||||
| Rate in 1990 (per 100000 population) | Rate in 2019 (per 100000 population) | EAPC (1990-2019) | Rate in 1990 (per 100000 population) | Rate in 2019 (per 100000 population) | EAPC (1990-2019) | |
| Global | 116.66 (79.78-172.01) | 137.36 (93.24-203.11) | 0.68 (0.63-0.73) | 11.03 (6.12-17.72) | 12.92 (7.12-20.97) | 0.68 (0.62-0.73) |
| Sex | ||||||
| Male | 74.37 (50.29-110.67) | 89.82 (60.03-134.94) | 0.78 (0.73-0.84) | 7.09 (3.91-11.72) | 8.51 (4.71-14.12) | 0.78 (0.72-0.85) |
| Female | 160.91 (111.16-237.28) | 187.84 (128.69-278.59) | 0.64 (0.59-0.69) | 15.15 (8.57-24.17) | 17.60 (9.89-28.34) | 0.64 (0.58-0.69) |
| Aetiology | ||||||
| Anorexia nervosa | 53.63 (34.86-79.10) | 60.67 (39.31-89.93) | 0.56 (0.52-0.61) | 4.99 (2.78-8.35) | 5.66 (3.15-9.62) | 0.57 (0.51-0.62) |
| Bulimia nervosa | 65.29 (35.91-112.75) | 78.81 (43.27-136.07) | 0.75 (0.70-0.81) | 6.03 (2.91-11.14) | 7.26 (3.51-13.60) | 0.76 (0.70-0.82) |
| Socio-demographic index | ||||||
| High SDI | 299.36 (207.55-448.68) | 348.17 (239.80-519.36) | 0.57 (0.46-0.68) | 28.11 (16.03-45.81) | 32.45 (18.25-53.04) | 0.56 (0.45-0.66) |
| High-middle SDI | 140.06 (96.78-208.68) | 180.32 (122.09-268.88) | 1.12 (1.03-1.21) | 13.25 (7.35-21.47) | 17.02 (9.44-27.79) | 1.14 (1.03-1.25) |
| Middle SDI | 92.70 (62.71-137.46) | 127.24 (85.94-190.46) | 1.30 (1.22-1.38) | 8.82 (4.90-14.31) | 12.03 (6.59-19.62) | 1.30 (1.21-1.39) |
| Low-middle SDI | 76.24 (51.53-112.46) | 106.44 (72.15-158.41) | 1.24 (1.16-1.31) | 7.22 (4.02-11.58) | 10.02 (5.54-16.18) | 1.22 (1.14-1.30) |
| Low SDI | 68.49 (46.47-100.95) | 80.38 (53.89-118.39) | 0.54 (0.42-0.66) | 6.47 (3.58-10.44) | 7.58 (4.20-12.28) | 0.55 (0.43-0.67) |
| Region | ||||||
| High-income Asia Pacific | 285.39 (196.42-419.28) | 320.41 (220.92-478.15) | 0.37 (0.30-0.44) | 27.11 (15.26-43.7) | 30.48 (17.14-49.63) | 0.35 (0.28-0.43) |
| Central Asia | 92.37 (63.29-136.71) | 98.59 (66.23-145.22) | 0.83 (0.58-1.08) | 8.79 (4.82-14.56) | 9.41 (5.24-15.38) | 0.85 (0.60-1.11) |
| East Asia | 68.76 (45.77-102.21) | 102.83 (68.86-153.09) | 1.97 (1.73-2.22) | 6.67 (3.63-10.73) | 9.93 (5.55-16.12) | 1.98 (1.72-2.25) |
| South Asia | 70.42 (47.56-103.77) | 105.56 (71.36-156.29) | 1.44 (1.36-1.52) | 6.68 (3.7-10.85) | 9.93 (5.51-16.06) | 1.42 (1.34-1.50) |
| Southeast Asia | 68.95 (46.53-101.56) | 94.80 (63.78-137.60) | 1.07 (1.02-1.12) | 6.56 (3.69-10.67) | 9.01 (5.00-14.43) | 1.07 (1.02-1.12) |
| Australasia | 532.55 (358.55-822.91) | 642.40 (458.62-902.39) | 1.15 (0.93-1.37) | 49.69 (27.35-84.76) | 59.45 (34.84-95.13) | 1.14 (0.93-1.36) |
| Caribbean | 144.60 (96.82-219.61) | 149.19 (102.06-223.98) | 0.41 (0.3-0.53) | 13.61 (7.61-21.96) | 14.00 (7.67-23.33) | 0.40 (0.28-0.52) |
| Central Europe | 116.32 (78.80-175.62) | 139.85 (94.41-210.18) | 0.77 (0.63-0.90) | 10.90 (5.94-17.80) | 13.2 (7.22-21.69) | 0.82 (0.68-0.96) |
| Eastern Europe | 117.66 (79.92-175.80) | 117.20 (80.21-172.70) | 0.22 (-0.03-0.48) | 11.29 (6.31-18.24) | 11.26 (6.33-17.97) | 0.28 (0.02-0.54) |
| Western Europe | 381.80 (269.38-568.79) | 400.24 (273.13-603.52) | 0.19 (0.12-0.26) | 35.72 (20.50-58.66) | 37.28 (20.88-61.76) | 0.18 (0.12-0.25) |
| Andean Latin America | 153.87 (100.49-239.82) | 190.08 (125.35-297.51) | 0.82 (0.76-0.87) | 14.43 (7.79-24.44) | 17.91 (9.79-30.26) | 0.83 (0.78-0.88) |
| Central Latin America | 147.26 (99.41-222.31) | 170.20 (116.58-255.62) | 0.53 (0.46-0.61) | 13.88 (7.60-22.96) | 16.02 (8.79-26.23) | 0.52 (0.45-0.60) |
| Southern Latin America | 218.40 (147.13-331.21) | 275.00 (181.83-418.71) | 0.90 (0.85-0.94) | 20.48 (11.20-34.32) | 25.85 (14.07-42.95) | 0.88 (0.84-0.93) |
| Tropical Latin America | 151.49 (103.53-219.35) | 188.20 (129.48-277.01) | 0.87 (0.80-0.93) | 14.08 (7.92-23.05) | 17.48 (9.84-28.51) | 0.88 (0.81-0.95) |
| North Africa and Middle East | 148.28 (99.21-228.58) | 179.56 (118.89-275.01) | 0.81 (0.71-0.92) | 13.88 (7.53-23.43) | 16.79 (9.08-27.91) | 0.82 (0.72-0.93) |
| High-income North America | 315.82 (214.28-474.18) | 356.89 (242.46-543.67) | 0.29 (0.08-0.49) | 29.44 (16.23-48.98) | 32.87 (18.07-54.22) | 0.27 (0.06-0.47) |
| Oceania | 68.28 (44.42-100.92) | 72.02 (46.08-107.19) | 0.22 (0.16-0.28) | 6.46 (3.58-10.67) | 6.84 (3.73-11.23) | 0.23 (0.17-0.30) |
| Central Sub-Saharan Africa | 74.02 (48.53-108.66) | 74.26 (49.07-111.50) | 0.07 (-0.12-0.26) | 6.96 (3.91-11.22) | 7.01 (3.79-11.42) | 0.10 (-0.09-0.29) |
| Eastern Sub-Saharan Africa | 64.43 (43.29-95.11) | 75.92 (51.59-110.99) | 0.52 (0.40-0.64) | 6.08 (3.40-9.80) | 7.19 (4.02-11.52) | 0.54 (0.43-0.65) |
| Southern Sub-Saharan Africa | 109.01 (73.73-164.18) | 114.62 (77.31-168.01) | 0.25 (0.16-0.33) | 10.29 (5.70-16.77) | 10.84 (6.00-17.6) | 0.27 (0.19-0.35) |
| Western Sub-Saharan Africa | 75.83 (51.77-111.61) | 88.52 (59.61-131.32) | 0.57 (0.47-0.68) | 7.18 (4.02-11.52) | 8.34 (4.59-13.39) | 0.57 (0.47-0.67) |
As shown in Supplementary Table 1, the DALY rate of AN at the global level gradually increased from 4.99 (95%UI: 2.78-8.35) per 100000 people in 1990 to 5.66 (95%UI: 3.15-9.62) per 100000 people in 2019, indicating an increase of 0.57 (95%UI: 0.51-0.62; Supplementary Figure 1). The global prevalence rate of AN increased from 53.36 (95%UI: 34.86-79.10) per 100000 people in 1990 to 60.67 (95%UI: 39.31-89.93) per 100000 people in 2019, indicating an increase of 0.56 per year (95%UI: 0.52-0.61; Supplementary Figure 1). The DALY rate of BN at the global level gradually increased from 6.03 (95%UI: 2.91-11.14) per 100000 people in 1990 to 7.26 (95%UI: 3.51-13.60) per 100000 people in 2019 (Supplementary Table 2), with an EAPC of 0.76 (95%UI: 0.70-0.82; Supplementary Figure 2). The global prevalence rate of BN increased from 65.29 (95%UI: 35.91-112.75) per 100000 people in 1990 to 78.81 (95%UI: 43.27-136.07) per 100000 people in 2019, indicating an increase of 0.75 per year (95%UI: 0.70-0.81; Supplementary Figure 2).
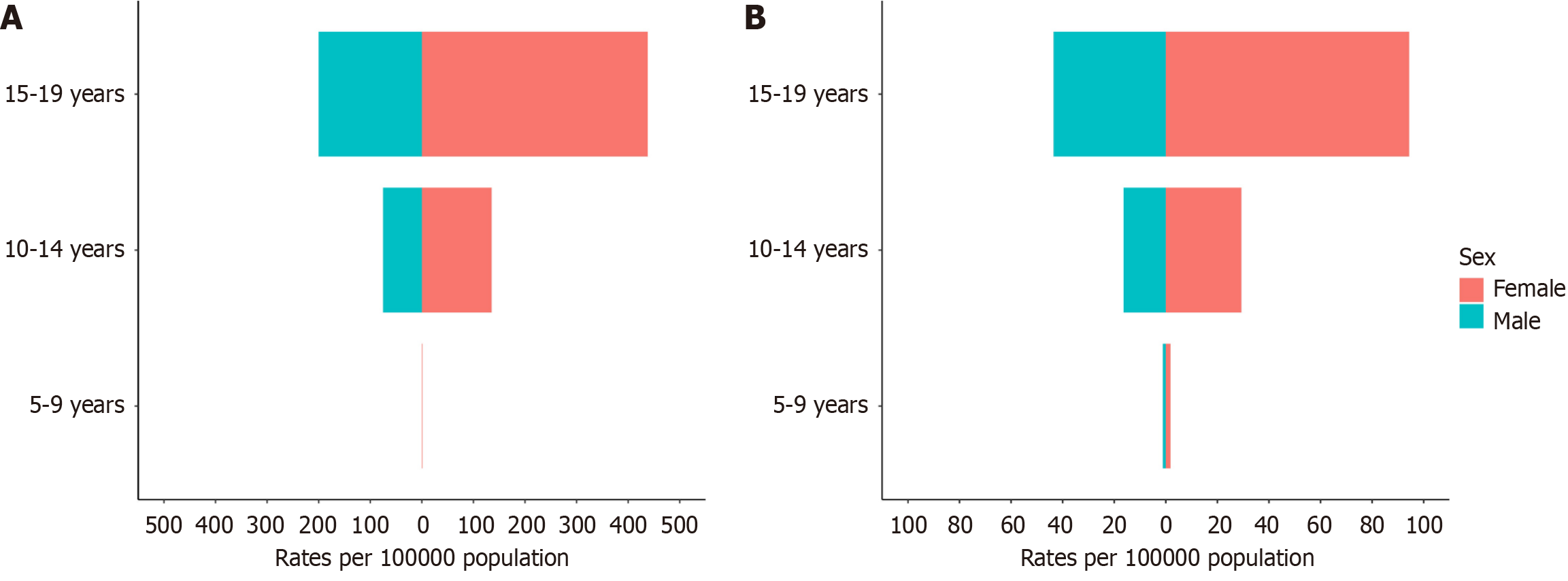
The rate of DALYs [17.60 (95%UI: 9.89-28.34) vs 8.51 (95%UI: 4.71-14.12) per 100000 people], and prevalence [187.84 (95%UI: 128.69-278.59) vs 89.82 (95%UI: 60.03-134.94) per 100000 people] of EDs in 2019 among females was higher than that among males. However, men had greater increases than women did in terms of DALYs and the prevalences of EDs (Table 1), AN (Supplementary Table 1), and BN (Supplementary Table 2). We also analyzed these indices in different age groups in terms of EDs (Figure 2), AN (Supplementary Figure 3), and BN (Supplementary Figure 4). The highest DALY and prevalence rates concerning EDs and its subtypes were reported among those aged 15-19 years.
The highest DALY and prevalence rates concerning EDs and its subtypes in 2019 were found in the high-SDI region. All the SDI regions in the observed period showed an increasing trend in these indices, with the greatest increases observed in the middle-SDI and low-middle-SDI regions in terms of EDs (Figure 1), AN (Supplementary Figure 1), and BN (Supplementary Figure 2).
As shown in Table 1, at the regional level, Australasia recorded the highest DALY (59.45, 95%UI: 34.84-95.13 per 100000 people) and prevalence (642.40, 95%UI: 458.62-902.39 per 100000 people) rates of EDs. There was an increasing trend in all geographic regions in the past 30 years in the DALY and prevalence rates, except for Eastern Europe and Central Sub-Saharan Africa. The greatest increase in these indices was observed in East Asia (EAPC for DALYs = 1.98, 95%UI: 1.72-2.25; EAPC for prevalence = 1.97, 95%UI: 1.73-2.22), followed by South Asia (EAPC for DALYs = 1.42, 95%UI: 1.34-1.5; EAPC for prevalence = 1.44, 95%UI: 1.36-1.52).
In 2019, Australasia had the highest DALY and prevalence rates for AN (DALYs = 22.55, 95%UI: 13.12-36.74; prevalence = 243.99, 95%UI: 168.36-341.27 per 100000 people; Supplementary Table 1) and BN (DALYs = 36.90, 95%UI: 19.96-64.25; prevalence = 402.81, 95%UI: 258.27-632.07, per 100000 people; Supplementary Table 2). Similar to EDs, there was an increasing trend in all geographic regions in the past 30 years in the DALY and prevalence rates for AN and BN, except for Eastern Europe and Central Sub-Saharan Africa. The most significant increase in these indices was detected in East Asia in terms of AN (EAPC for DALYs = 1.77, 95%UI: 1.54-2.00; EAPC for prevalence = 1.73, 95%UI: 1.52-1.94) and BN (EAPC for DALYs = 2.21, 95%UI: 1.92-2.51; EAPC for prevalence = 2.19, 95%UI: 1.92-2.46), followed by South Asia.
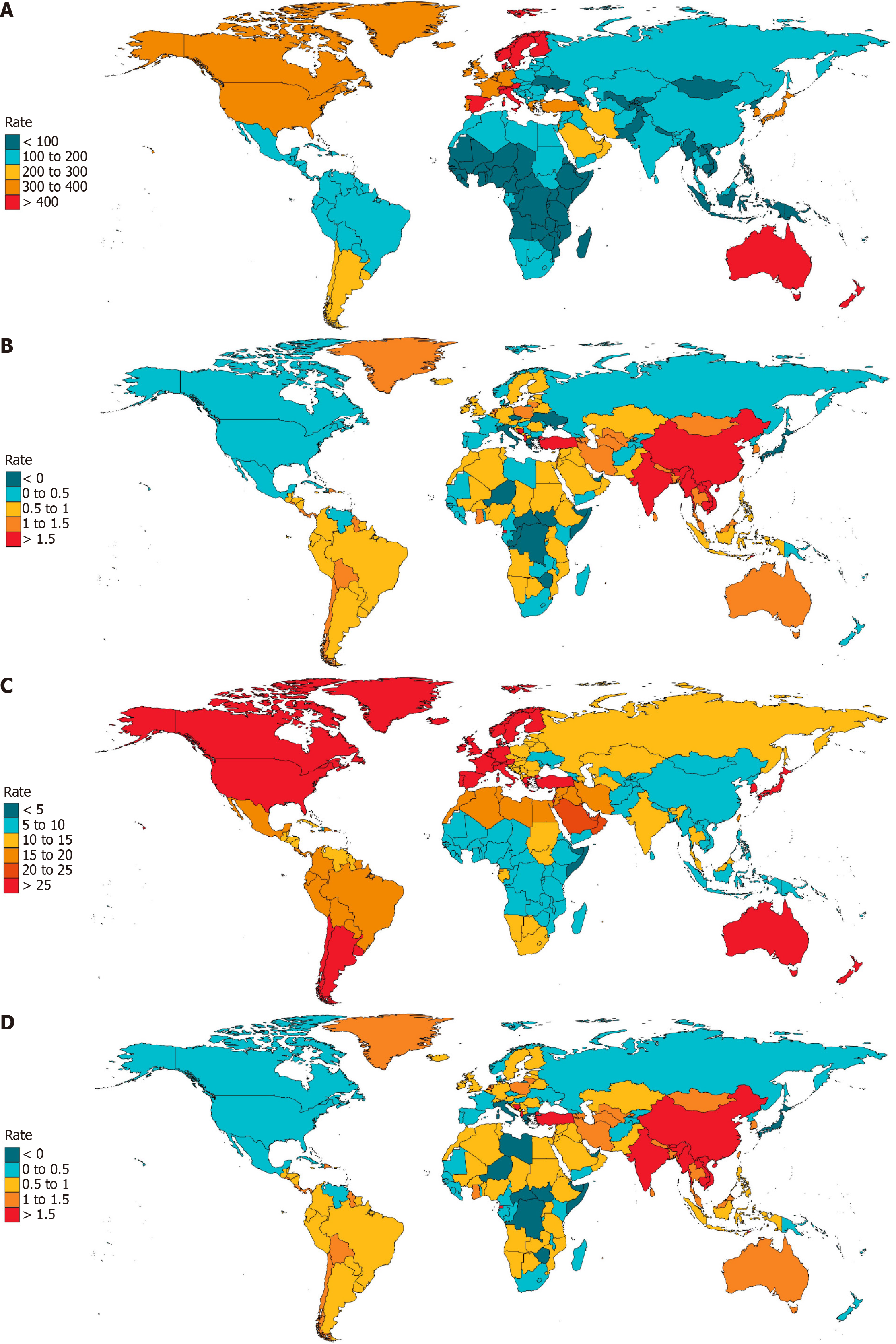
At the national level, as listed in Supplementary Table 3, the highest DALY and prevalence rates of EDs in 2019 were reported in Monaco, followed by Australia and Spain (Figure 3A and C). An increasing trend was detected in the DALY and prevalence rates of EDs in 204 countries and territories. The three countries with the greatest increase from 1990 to 2019 were Equatorial Guinea, Turkey, and China (Figure 3B and D).
As presented in Supplementary Table 4, the highest DALY and prevalence rates of AN in 2019 were found in Australia, followed by Monaco and Spain (Supplementary Figure 5A and Supplementary Figure 6A). As presented in Supplementary Table 5, Monaco, Australia, and Spain were the three countries with the highest DALY and prevalence rates of BN in 2019 (Supplementary Figure 7A and Supplementary Figure 8A). During the observed period, increasing trends were detected in the DALY and prevalence rates of AN and BN in 204 countries and territories. The three countries with the greatest increase due to AN were Equatorial Guinea, the Netherlands, and China (Supplementary Figure 5B and Supplementary Figure 6B), whereas Equatorial Guinea, Turkey, and China had the highest EAPCs in DALYs and prevalence of BN (Supplementary Figure 7B and Supplementary Figure 8B).
The associations between SDI levels and burden estimates of EDs for each geographic region during the observation period are presented in Figure 4; positive associations are shown. In the past 30 years, the number of SDIs has increased in all geographic regions. There was a slight increase in the burden estimates, as the SDIs increased when the SDIs were less than 0.67. Conversely, a more rapid increase with increasing SDIs was detected in burden estimates when the SDIs were above 0.67.
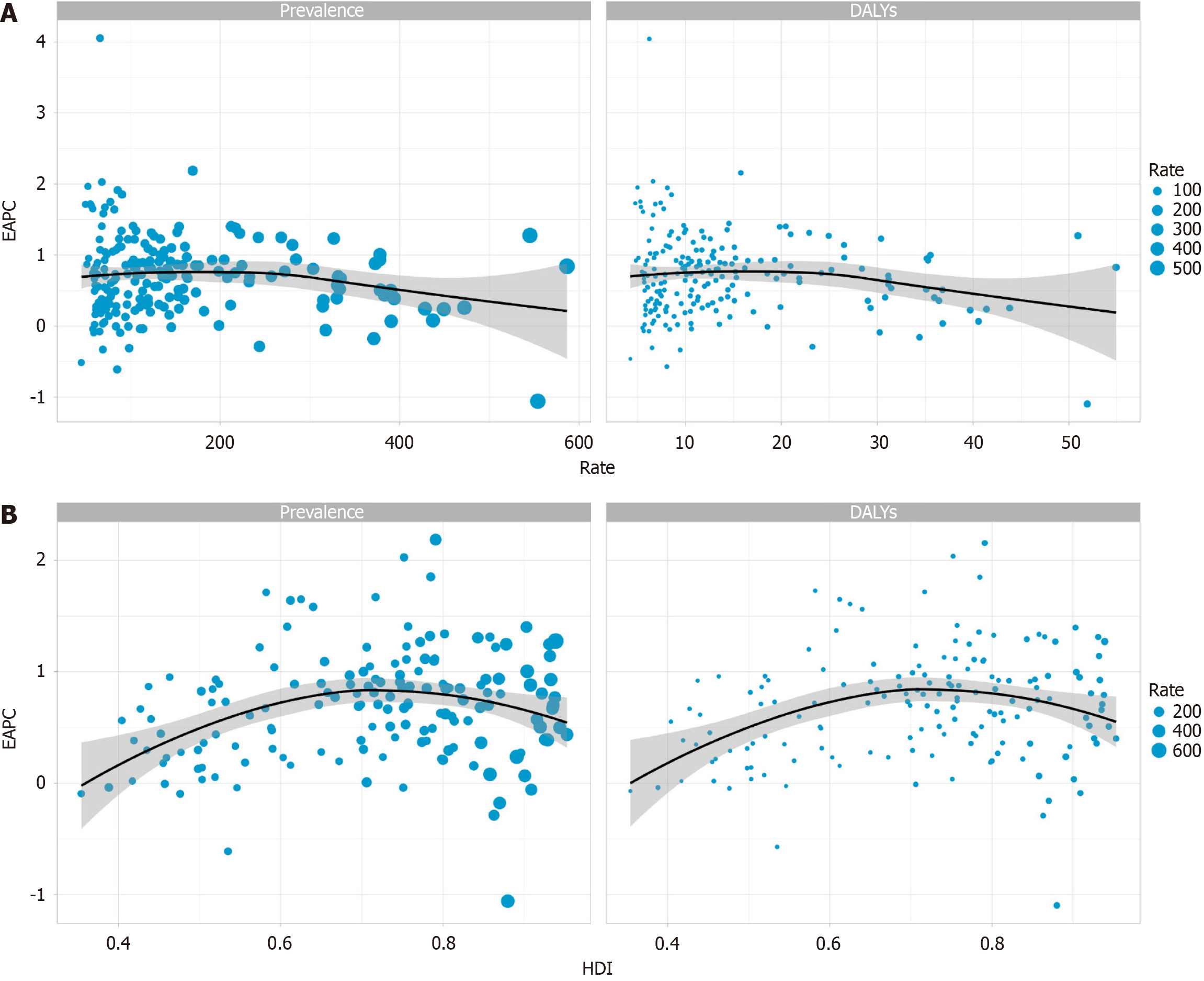
As shown in Figure 5, there was a negative association between the rates and the EAPCs in the DALY (ρ = -0.141, P = 0.045) and prevalence (ρ = -0.133, P = 0.057) rates. A positive correlation was detected between the human development indices in 2019 and the EAPCs in the DALY (ρ = 0.199, P = 0.012) and prevalence (ρ = 0.200, P = 0.012) rates of EDs when HDIs < 0.7, whereas a negative association was detected when HDIs > 0.7.
To our knowledge, the present study is the first to explore trends in and the prevalence of EDs in children and ado
The burden of EDs has increased globally and peaks at 15-19 years among children and adolescents[9,10]. This trend is consistent with the change in the DSM-5, which includes broadened diagnostic criteria to promote inclusion[11]. Ornstein revealed that the proposed DSM-5 criteria substantially increased the prevalences of AN and BN among young patients[12]. In accordance with this increasing trend in EDs, there was a rapid increase in the overall burden of mental illness.
Economic growth may be another important factor. For example, China’s rapidly developing economy and urba
In line with previous consensus, we found that the burden of EDs was gender-related and that the DALY and prevalence rates of EDs were greater for women than men in all age groups[16-18]. Given the emphasis on attractiveness in female gender role stereotypes and the correlations between thinness, femininity, and beauty, girls may be particularly susceptible to engaging in unhealthy weight-control behaviors. Moreover, as semiclosed environments, campuses can exacerbate sociocultural pressures to maintain a thin body shape, and females are more significantly affected by these conditions[19]. Furthermore, there is ongoing debate regarding whether there is a correlation with Western culture or the contemporary influence of the media[18]. EDs were historically considered the most common gender-related mental illnesses, with females experiencing the majority of cases. However, according to recent evidence, approximately 25% of individuals with AN and BN are male, which indicates that this disease burden in male patients is a health problem that warrants attention[20].
In fact, although females still accounted for more ED cases, males had a greater increase in DALY and prevalence rates than females did. Gorrell explained why the burden of EDs has been underestimated among males[20]. First, EDs have been regarded as female phenomena, leading to the neglect of males over the past several decades of research efforts. Second, a lack of insight, denial, secrecy, and shame related to having a “female disorder” could contribute to male patients’ refusal to seek treatment. Third, the diagnostic criteria are biased toward females, resulting in low diagnostic efficiency in males. To address this gap, it is important to eliminate amenorrhea as a diagnostic criterion for AN in the DSM-5, improving the accuracy of the prevalence estimates among males[11]. Early research findings demonstrated that up to 42% of men who were diagnosed with an ED were identified as homosexual or bisexual[21,22]. Notably, given that adolescence is a crucial period in the development of gender identity and sexual orientation as well as body image disturbances, EDs may disproportionately impact vulnerable youth. Lesbian, gay, bisexual, and transgender (LGBT) youth, as indicated by the extant literature, are especially vulnerable to body dissatisfaction and EDs[23,24]. Therefore, more concern and support should be provided to male patients and LGBT youth.
The highest burdens of EDs and its subtypes were observed in the high-SDI region. This result was consistent with those of Castaldelli-Maia, who demonstrated that countries with higher SDI levels had a greater prevalence of mental and substance use disorders, indicating a greater recognition of mental disorders in developed countries as a sign of relatively greater allocation of resources toward mental health and higher education levels[25]. Another reason for the higher prevalence of these disorders in high-income Western countries, such as America, could be the development of psychiatric diagnostic criteria, which are largely impacted by local schools of psychiatry. Moreover, the validity of these psychiatric diagnostic manuals (e.g., DSM-5 and ICD-10) is weak in some areas, leading to systematic differences.
Although more ED cases can be found in the industrialized Western world, a greater increase in the burden of EDs was observed in Asian countries, including China and India. Moreover, the greatest increasing trend among the five SDI regions was observed in middle-SDI regions. With almost one-fifth of the world’s population, China, which is classified as part of the middle-SDI region, is the third fastest-growing country in terms of the burden of EDs. According to Huang, China has undergone economic development and social changes at an unprecedented rate in the past 30 years, leading to tremendous changes in its urbanization, education, population structure, culture, social concept, and so on[13]. These changes may increase psychological pressure, resulting in mood, cognitive, and behavioral disorders, along with related problems[13,26]. In addition to the economic growth and urbanization in these areas, globalization could also increase the risk of exposure to risk factors. For example, another study conducted in India showed that increasing exposure to global body image trends may contribute to an increase in EDs[27]. Furthermore, the lack of awareness, insufficient coverage of mental health services, and stigma attached to these disorders in these areas could pose great challenges to the diagnosis, prevention, and treatment of EDs.
The burden of EDs varies across regions and countries. Although AN has historically been regarded as a possible “culture-bound syndrome” rooted in Western culture, which emphasizes body dissatisfaction and EDs, they are wide
It was found that the burden of EDs increases with increasing SDI, and a positive correlation was detected between HDIs and the burden of EDs. This may be due to more social pressure and greater use of electronic media in these high socioeconomic countries[25]; it could also be due to the insufficient coverage of mental health services in developing countries, leading to a relatively lower diagnosis rate[27].
This study investigated the trends and prevalences of EDs in children and adolescents and the associations with SDI over the past 30 years and HDIs in 2019. Our study revealed the increasing burden of EDs among males and LGBT youth. However, there are several limitations of our study. First, this research shared the limitations of the GBD 2019 database that which have been detailed in previous studies[31]. Whereas GBD 2019 employed several techniques to mitigate bias and inaccuracy, completely eliminating bias remains a challenge[32]. Second, only AN and BN were included in GBD 2019, whereas BED, which is one of the most prevalent EDs, was not included. The potential inclusion of BED when quantifying the burden of EDs, as the GBD is designed for continual updates, offers an opportunity to increase the accuracy of estimating the burden. Third, considering the diversity of cultures, different results may be obtained when the same diagnostic tools are used across cultures. Therefore, the development of diagnostic criteria needs to consider cultural factors[33].
Although the greatest burden of EDs remains in high-income Western countries, a global increase was observed across all SDI regions, particularly in Asia. These results are helpful for resource planning and medical policy prioritization.
We appreciate the Institute of Health Metrics and Evaluation for providing the Global Burden of Disease 2019 in the public domain.
| 1. | Herpertz-Dahlmann B. Adolescent eating disorders: update on definitions, symptomatology, epidemiology, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2015;24:177-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 241] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 2. | Wade TD. Recent Research on Bulimia Nervosa. Psychiatr Clin North Am. 2019;42:21-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Samnaliev M, Noh HL, Sonneville KR, Austin SB. The economic burden of eating disorders and related mental health comorbidities: An exploratory analysis using the U.S. Medical Expenditures Panel Survey. Prev Med Rep. 2015;2:32-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 59] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 4. | Mairs R, Nicholls D. Assessment and treatment of eating disorders in children and adolescents. Arch Dis Child. 2016;101:1168-1175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 5. | Treasure J, Duarte TA, Schmidt U. Eating disorders. Lancet. 2020;395:899-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 512] [Article Influence: 102.4] [Reference Citation Analysis (0)] |
| 6. | GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11327] [Cited by in RCA: 9637] [Article Influence: 1927.4] [Reference Citation Analysis (35)] |
| 7. | American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. American Psychiatric Publishing, Inc., 1994. |
| 8. | American Psychiatric Association. Desk Reference to the Diagnostic Criteria From DSM-5-TR®. 5th ed. American Psychiatric Publishing, 2022. |
| 9. | Li Z, Wang L, Guan H, Han C, Cui P, Liu A, Li Y. Burden of Eating Disorders in China, 1990-2019: An Updated Systematic Analysis of the Global Burden of Disease Study 2019. Front Psychiatry. 2021;12:632418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Lantzouni E, Grady R. Eating Disorders in Children and Adolescents: A Practical Review and Update for Pediatric Gynecologists. J Pediatr Adolesc Gynecol. 2021;34:281-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Call C, Walsh BT, Attia E. From DSM-IV to DSM-5: changes to eating disorder diagnoses. Curr Opin Psychiatry. 2013;26:532-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 107] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 12. | Ornstein RM, Rosen DS, Mammel KA, Callahan ST, Forman S, Jay MS, Fisher M, Rome E, Walsh BT. Distribution of eating disorders in children and adolescents using the proposed DSM-5 criteria for feeding and eating disorders. J Adolesc Health. 2013;53:303-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 13. | Huang Y, Wang Y, Wang H, Liu Z, Yu X, Yan J, Yu Y, Kou C, Xu X, Lu J, Wang Z, He S, Xu Y, He Y, Li T, Guo W, Tian H, Xu G, Xu X, Ma Y, Wang L, Wang L, Yan Y, Wang B, Xiao S, Zhou L, Li L, Tan L, Zhang T, Ma C, Li Q, Ding H, Geng H, Jia F, Shi J, Wang S, Zhang N, Du X, Du X, Wu Y. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6:211-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1590] [Cited by in RCA: 1360] [Article Influence: 226.7] [Reference Citation Analysis (0)] |
| 14. | Smink FR, van Hoeken D, Hoek HW. Epidemiology of eating disorders: incidence, prevalence and mortality rates. Curr Psychiatry Rep. 2012;14:406-414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1058] [Cited by in RCA: 1098] [Article Influence: 84.5] [Reference Citation Analysis (0)] |
| 15. | Killen JD, Hayward C, Litt I, Hammer LD, Wilson DM, Miner B, Taylor CB, Varady A, Shisslak C. Is puberty a risk factor for eating disorders? Am J Dis Child. 1992;146:323-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Wu J, Liu J, Li S, Ma H, Wang Y. Trends in the prevalence and disability-adjusted life years of eating disorders from 1990 to 2017: results from the Global Burden of Disease Study 2017. Epidemiol Psychiatr Sci. 2020;29:e191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 74] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 17. | Piao J, Huang Y, Han C, Li Y, Xu Y, Liu Y, He X. Alarming changes in the global burden of mental disorders in children and adolescents from 1990 to 2019: a systematic analysis for the Global Burden of Disease study. Eur Child Adolesc Psychiatry. 2022;31:1827-1845. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 94] [Article Influence: 31.3] [Reference Citation Analysis (0)] |
| 18. | Litmanen J, Fröjd S, Marttunen M, Isomaa R, Kaltiala-Heino R. Are eating disorders and their symptoms increasing in prevalence among adolescent population? Nord J Psychiatry. 2017;71:61-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Striegel-Moore RH, Silberstein LR, Rodin J. Toward an understanding of risk factors for bulimia. Am Psychol. 1986;41:246-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 80] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Gorrell S, Murray SB. Eating Disorders in Males. Child Adolesc Psychiatr Clin N Am. 2019;28:641-651. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 96] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 21. | Herzog DB, Norman DK, Gordon C, Pepose M. Sexual conflict and eating disorders in 27 males. Am J Psychiatry. 1984;141:989-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 70] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Carlat DJ, Camargo CA Jr, Herzog DB. Eating disorders in males: a report on 135 patients. Am J Psychiatry. 1997;154:1127-1132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 224] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 23. | Milano W, Ambrosio P, Carizzone F, De Biasio V, Foggia G, Capasso A. Gender Dysphoria, Eating Disorders and Body Image: An Overview. Endocr Metab Immune Disord Drug Targets. 2020;20:518-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 24. | McClain Z, Peebles R. Body Image and Eating Disorders Among Lesbian, Gay, Bisexual, and Transgender Youth. Pediatr Clin North Am. 2016;63:1079-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 85] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 25. | Castaldelli-Maia JM, Bhugra D. Analysis of global prevalence of mental and substance use disorders within countries: focus on sociodemographic characteristics and income levels. Int Rev Psychiatry. 2022;34:6-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 74] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 26. | Yang XJ. China's rapid urbanization. Science. 2013;342:310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 27. | India State-Level Disease Burden Initiative Mental Disorders Collaborators. The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990-2017. Lancet Psychiatry. 2020;7:148-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 229] [Cited by in RCA: 371] [Article Influence: 74.2] [Reference Citation Analysis (1)] |
| 28. | Miller MN, Pumariega AJ. Culture and eating disorders: a historical and cross-cultural review. Psychiatry. 2001;64:93-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 144] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 29. | Martínez-González MA, Gual P, Lahortiga F, Alonso Y, de Irala-Estévez J, Cervera S. Parental factors, mass media influences, and the onset of eating disorders in a prospective population-based cohort. Pediatrics. 2003;111:315-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 68] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 30. | Kim YR, Nakai Y, Thomas JJ. Introduction to a special issue on eating disorders in Asia. Int J Eat Disord. 2021;54:3-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 31. | GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223-1249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5702] [Cited by in RCA: 5064] [Article Influence: 1012.8] [Reference Citation Analysis (1)] |
| 32. | Xie J, Wang M, Long Z, Ning H, Li J, Cao Y, Liao Y, Liu G, Wang F, Pan A. Global burden of type 2 diabetes in adolescents and young adults, 1990-2019: systematic analysis of the Global Burden of Disease Study 2019. BMJ. 2022;379:e072385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 116] [Article Influence: 38.7] [Reference Citation Analysis (0)] |
| 33. | Castelpietra G, Knudsen AKS, Agardh EE, Armocida B, Beghi M, Iburg KM, Logroscino G, Ma R, Starace F, Steel N, Addolorato G, Andrei CL, Andrei T, Ayuso-Mateos JL, Banach M, Bärnighausen TW, Barone-Adesi F, Bhagavathula AS, Carvalho F, Carvalho M, Chandan JS, Chattu VK, Couto RAS, Cruz-Martins N, Dargan PI, Deuba K, da Silva DD, Fagbamigbe AF, Fernandes E, Ferrara P, Fischer F, Gaal PA, Gialluisi A, Haagsma JA, Haro JM, Hasan MT, Hasan SS, Hostiuc S, Iacoviello L, Iavicoli I, Jamshidi E, Jonas JB, Joo T, Jozwiak JJ, Katikireddi SV, Kauppila JH, Khan MAB, Kisa A, Kisa S, Kivimäki M, Koly KN, Koyanagi A, Kumar M, Lallukka T, Langguth B, Ledda C, Lee PH, Lega I, Linehan C, Loureiro JA, Madureira-Carvalho ÁM, Martinez-Raga J, Mathur MR, McGrath JJ, Mechili EA, Mentis AA, Mestrovic T, Miazgowski B, Mirica A, Mirijello A, Moazen B, Mohammed S, Mulita F, Nagel G, Negoi I, Negoi RI, Nwatah VE, Padron-Monedero A, Panda-Jonas S, Pardhan S, Pasovic M, Patel J, Petcu IR, Pinheiro M, Pollok RCG, Postma MJ, Rawaf DL, Rawaf S, Romero-Rodríguez E, Ronfani L, Sagoe D, Sanmarchi F, Schaub MP, Sharew NT, Shiri R, Shokraneh F, Sigfusdottir ID, Silva JP, Silva R, Socea B, Szócska M, Tabarés-Seisdedos R, Torrado M, Tovani-Palone MR, Vasankari TJ, Veroux M, Viner RM, Werdecker A, Winkler AS, Hay SI, Ferrari AJ, Naghavi M, Allebeck P, Monasta L. The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990-2019: Findings from the Global Burden of Disease Study 2019. Lancet Reg Health Eur. 2022;16:100341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 147] [Article Influence: 49.0] [Reference Citation Analysis (0)] |