Published online Jan 19, 2024. doi: 10.5498/wjp.v14.i1.179
Peer-review started: November 1, 2023
First decision: November 17, 2023
Revised: November 27, 2023
Accepted: December 20, 2023
Article in press: December 20, 2023
Published online: January 19, 2024
Processing time: 79 Days and 5.7 Hours
As the burden of mental disorders among patients with atrial fibrillation (AF) increases, researchers are beginning to pay close attention to the risk and prevalence of these comorbidities. Although studies have independently analyzed the risk of comorbidity with depression and anxiety in patients with AF, no study has systematically focused on the global epidemiology of these two mental disorders.
To explore the prevalence of depression and anxiety in patients with AF.
Five databases were searched from their date of establishment until January 2023. Observational studies reporting the comorbidity of AF with depression and anxiety, were included in this study. Basic information, such as the first author/ publication year, study year, study type, and prevalence of depression and anxiety, were extracted. STATA SE 15.1 was used to analyze the data. Subgroup, meta-regression, and sensitivity analyses were performed to estimate study heterogeneity.
After a thorough search, 26 studies were identified and included in this meta-analysis. The prevalence rates of depression and anxiety in adults with AF were 24.3% and 14.5%, respectively. Among adult males with AF, the prevalence was 11.7% and 8.7%, respectively, whereas in females it was 19.8% and 10.1%, respectively. In older adults with AF, the prevalence rates of depression and anxiety were 40.3% and 33.6%, respectively. The highest regional prevalence of depression and anxiety was observed in European (30.2%) and North American (19.8%) patients with AF.
In this study, we found that the prevalence of depression and anxiety among patients with AF varies with sex, region, and evaluation scales, suggesting the need for psychological interventions for patients with AF in clinical practice.
Core Tip: Mental disorders are risk factors for the development of atrial fibrillation (AF). The global prevalence of AF comorbidity with depression and anxiety is not clear. This is the first study to evaluate the global prevalence of two types of psychiatric disorders (depression and anxiety) in patients with AF from the aspects of age, sex, country, and evaluation scale for depression and anxiety.
- Citation: Zhang S, Zhang N, Liu L, Zheng W, Ma ZL, Qiao SY, Zhao YL, Wei YH, Wu G, Yu QT, Deng B, Shen L. Global epidemiology of mental disorder in atrial fibrillation between 1998-2021: A systematic review and meta-analysis. World J Psychiatry 2024; 14(1): 179-193
- URL: https://www.wjgnet.com/2220-3206/full/v14/i1/179.htm
- DOI: https://dx.doi.org/10.5498/wjp.v14.i1.179
Atrial fibrillation (AF), an irregular and rapid heart rate, is one of the most common cardiac arrhythmias[1,2]. The prevalence of AF has increased steadily over the past three decades, with approximately 60 million people worldwide currently suffering from it[3]. It has been demonstrated that age, gender, smoking, alcohol consumption, hypertension, diabetes, and genetic predisposition are all recognized risk factors for the development and progression of AF[4,5]. The continued increase in AF prevalence and mortality adversely affects patients' quality of life with a significant burden on health and economic development[6].
Recently, mental disorders have become a serious concern worldwide. As reported by WHO in 2019, 970 million people worldwide have mental disorders, with anxiety and depression being the two most common categories[7]. Emerging evidence has shown that patients with acute and chronic cardiovascular diseases are at a higher risk of developing mental disorders[8]. Mental disorders are also on the agenda for patients with AF. Studies have shown that patients with AF have a poorer quality of life than patients with other cardiovascular diseases, regardless of disease symptoms[9], which directly affects their psychological well-being. In another study, several factors affecting Health-related quality of life in patients with AF included depression and anxiety[10]. Although studies have independently analyzed the risk of comorbidity with depression and anxiety in patients with AF[11], no study has systematically focused on the global epidemiology of these two mental disorders. Therefore, we aimed to analyze the epidemiology of AF’s co-morbidity with depression and anxiety.
This study was conducted according to the PRISMA 2009 statement and Meta-analysis of Observational Studies in Epidemiology guidelines (Supplementary Table 1). This study was registered in the PROSPERO (No. CRD42023405975) database.
Two researchers (Zhang S and Zhang N) independently searched the PubMed, Embase, CNKI, Wanfang, and Sinomed databases from their construction date to January 2023 using a combination of subject and free words. The primary search terms were: “AF”, “mental health”, “depression”, “anxiety”, “affective symptoms”, “psychological distress”, “epidemiology”, “prevalence”, and “incidence”. The details are shown in Supplementary Tables 2-6.
The criteria for inclusion in this study were as follows: (1) Epidemiological studies reporting co-morbidity of AF with depression and anxiety; (2) observational studies, including cohort studies and cross-sectional studies; (3) studies published in Chinese or English; and (4) no restrictions for age, gender, and country.
The exclusion criteria were as follows: (1) Literature not relevant to the topic of the study; (2) duplicate studies; (3) case-control studies and non-observational studies; and (4) unavailability of full texts.
Two investigators (Zheng W and Ma ZL) separately extracted the key constituents for inclusion in the study. The following information was retrieved: first author/publication year, study year, study type, age, region (country), type of mental health, diagnostic criteria for mental health, generation, number of cases of AF, and prevalence of comorbidities. If the prevalence was not stated in the study or if the study was cross-sectional, we used the following formula: Cases/total number of subjects in the observational group × 100%.
Two researchers (Zhao YL and Qiao SY) evaluated the quality of the pooled research. The Agency for Healthcare Research and Quality tool was used to estimate the risk of bias in cross-sectional studies. Additionally, the Newcastle-Ottawa Scale was used to assess the cohort studies. The researchers graded each study based on the entries of the scale and classified them as high (8-11), moderate (4-7), and low (0-3) quality.
We used STATA SE 15.1 for data analysis, and the I2 test was used to evaluate heterogeneity. A fixed-effects model was used if the I2 value was < 50%; otherwise, a random-effects model was applied. Heterogeneity was assessed by subgroup, meta-regression, and sensitivity analyses. Publication bias was determined using Egger’s and Begg’s linear tests. If there was a publication bias, the trim-and-fill method was used to estimate the number of missing studies to rectify it. We used the R 4.2.2 software to visualize world maps for the prevalence of depression and anxiety in patients with AF.
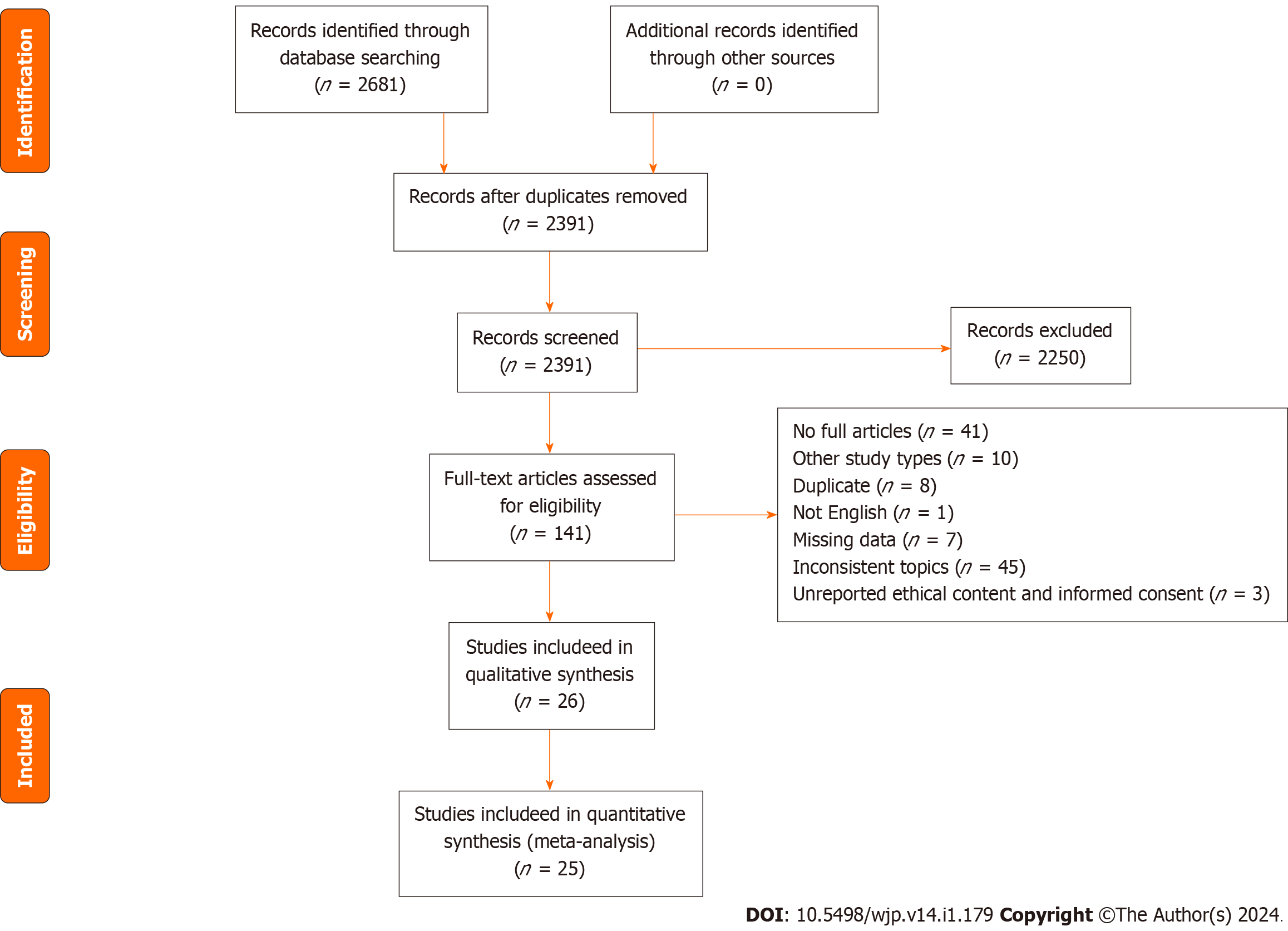
We identified 2681 studies. A total of 2391 studies remained after removing duplicates, of which 1851 were thematic discrepancies, 370 were reviews, and 29 were duplicates. Subsequently, 141 full-text articles were assessed for eligibility. From these, 115 studies were removed due to irrelevant topics, missing data, or other study types. Finally, 26 studies[12-37] were used in the meta-analysis (Figure 1).
Of the included studies, 25 and 14 analyzed the prevalence of depression and anxiety in patients with AF, respectively. One study reported the prevalence of AF in patients with depression[14]. Details were shown in Table 1.
| Ref. | Study year | Study type | Region (country) | Type of MH | Diagnostic criteria of MH | Age (mean ± SD) (yr)1 | Generation (yr) | AF (n) | P (MH in AF); Total (M/F) (%) |
| Thrall et al[20] | - | - | Europe (United Kingdom) | D and A | Depression-BDI; anxiety-STAI | 66.30 11 | Adult (≥ 18 y) | 101 | D (38.00); A (28.00/38.00) |
| Ariansen et al[35] | - | - | Europe (Norway) | D | HADS | - | Adult (≥ 75 y) | 27 | 11.10 |
| Gehi et al[32] | 2008-2011 | Cohort study | North America (United States) | D and A | Depression-PHQ-9; anxiety-HADS | 61.70 13.50 | Adult (≥ 18 y) | 300 | D (50.00); A (17.00) |
| Ball et al[31] | SAFETY | Oceania (Austria) | D | CES-D | 75 13 | Adult (≥ 45 y) | 335 | 29.00 | |
| Schnabel et al[30] | 2007 | Population-based Gutenberg Health Study | Europe (Germany) | D | PHQ-9 | 64.8 8.2 | Adult (35-74 y) | 309 | 8.00 |
| Thompson et al[19] | 2009-2012 | Cohort study | North America (United States) | D and A | Anxiety-HADS-A Depression-PHQ-9 | 61.60 13.30 | Adult (≥ 18 y) | 378 | D (39.40/16.9); A (17.72) |
| von Eisenhart Rothe et al[21] | 2005-2008 | Cross-sectional study | Europe (Germany) | D | MDI scale | - | Adult (≥ 18 y) | 702 | 73.00 |
| Hsu et al[29] | - | Population based community health survey | Asia (China) | D and A | HADS | 74.90 6.90 | Adult (≥ 65 y) | 1732 | D (14.00); A (36.00) |
| Wändell et al[28] | 2001-2007 | Cohort study | Europe (Sweden) | D and A | ICD-10 | - | Adult (≥ 45 y) | 12283 (6702/5750) | D (8.50) (6.10/10.90); A (4.03) (2.70/5.40) |
| Hu et al[12] | 2000-2010 | Cohort study | Asia (China) | D and A | ICD-9-CM | 72.70 13.40 | Adult (≥ 18 y) | 88259 | D (1.57); A (1.06) |
| Rewiuk et al[13] | 2007-2012 | Population-based, multicenter study | Europe (The Republic of Poland) | D | GDS | 78.0 7.7 | Adult (65-104) | 788 | 41.24 |
| Polikandrioti et al[15] | - | - | Europe (Greece) | D and A | HADS | - | Adult (≥ 18 y) | 170 | Anxiety-low (38.25) (39.80/35.30); anxiety-moderate (26.47) (31.40/15.70); anxiety-high (34.71) (28.80/49.00); depression-low (63.53) (65.80/60.80); depression-moderate (15.29) (14.50/17.60); depression-high (20.00) (19.70/21.60) |
| Hagengaard et al[16] | 2005-2014 | Cohort study | Europe (Denmark) | D and A | ICD-10 | - | - | 146377 | D (0.29); A (0.07) |
| Uchmanowicz et al[17] | 2019 | Cross-sectional study | Europe (The Republic of Poland) | D | HADS GDS | 70.27 3.48 | Adult (≥ 65y) | 100 | Anxiety (HADS 8-10) (22.00); anxiety (HADS 11-21) (20.00); depression (HADS 8-10) (26.00); depression (HADS 11-21) (28.00); depression (GDS 6-15) (51.00) |
| Krupenin et al[18] | 2017-2018 | - | Europe (Russia) | D and A | GDS | 782 | Adult (≥ 65 y) | 48 | 41.67 |
| Wang et al[22] | - | SAGE-AF Study | North America (United States) | D and A | Anxiety-GAD Depression-PHQ-9 | 76.00 7.00 | Adult (≥ 65 y) | 1244 | D (29.00); A (24.00) |
| Kim et al[23] | 2009-2018 | Cohort study | Asia (Korea) | D | ICD-10 | 46.99 14.06 | Adult (≥ 20 y) | 5031222 | 3.00 (1.04/1.92) |
| Jankowska-Polańska et al[24] | - | Cohort study | Europe (The Republic of Poland) | D and A | HADS | 70 7 | Adult (≥ 60 y) | 158 | Depression (8-10) (37.97); depression (11-21) (37.87); anxiety (8-10) (32.91); anxiety (11-21) (48.10) |
| Feng et al[25] | 2006-2008 | HUNT study | Europe (Germany) | D and A | HADS | 53.4 15.2 | Adult (≥ 20y) | 37402 | D (2.20); A (4.90) |
| Wändell et al[28] | 1998-2012 | Cohort study | Europe (Sweden) | D and A | ICD-10 | - | Adult (≥ 45 y) | 537513 (287959/249554) | D (3.91) (3.46/4.44); A (2.70) (2.23/3.25) |
| Piwoński et al[27] | - | Cross-sectional study | Europe (The Republic of Poland) | D | BDI | - | Adult (18-79 y) | 124 (57/67) | 47.58 (43.86/50.75) |
| Wu et al[33] | 2020-2021 | - | Asia (China) | D | PHQ-9 | - | Adult (≥ 18 y) | 329 | 35.56 |
| Fenger-Grøn et al[34] | 2005-2016 | - | Europe (Denmark) | D | ICD-8/ICD-10 | 78.7 10.1 | Adult (18-100 y) | 147162 | 12.16 |
| Rosman et al[36] | - | Cohort study | North America (USA) | D and A | ICD-9 | 30.29 9.19 | Adult (18-60 y) | 988090 | 9.04 |
| Zhang et al[37] | 2012-2013 | Cross-sectional study | Asia (China) | D | PHQ-9 | 63.3 9.5 | Adult (≥ 35 y) | 134 | 63.00 |
After evaluating and scoring the studies, we found that they had scores ranging from 4 to 7, all of which were of moderate quality. The details are listed in Supplementary Tables 7 and 8.
Depression: The aggregated prevalence of depression in patients with AF was 22.0% (95%CI: 0.207-0.233). the prevalence was 24.3% (95%CI: 0.228-0.257) in adults and 40.3% (95%CI: 0.264-0.541) in patients ≥ 60 years. Additionally, the prevalence of depression in patients with AF differed between men [11.7% (95%CI: 0.088-0.147)] and women [19.8% (95%CI: 0.1494-0.252)] (Table 2, Supplementary Figures 1-4). We found in the study that evaluated the prevalence of AF in patients with depression that 46.37% of 6055 patients with depression had AF (Supplementary Table 9).
| Study or subgroup | Prevalence (95%CI) | I² (%) | P value |
| Depression | |||
| Overall prevalence | 22.0 (0.207, 0.233) | 100 | < 0.001 |
| Prevalence in adults | 24.3 (0.228, 0.257) | 100 | < 0.001 |
| Gender | |||
| Male | 11.7 (0.088, 0.147) | 97.3 | < 0.001 |
| Female | 19.8 (0.144, 0.252) | 98.7 | < 0.001 |
| Age group | |||
| ≥ 60 yr | 40.3 (0.264, 0.541) | 100 | < 0.001 |
| Other ages | 20.4 (0.188, 0.221) | 100.0 | < 0.001 |
| Study design | |||
| Cross-sectional study | 58.2 (0.468, 0.695) | 91.7 | < 0.001 |
| Cohort study | 15.3 (0.124, 0.182) | 100 | < 0.001 |
| Others | 24.4 (0.217, 0.271) | 99.9 | < 0.001 |
| Region | |||
| Asia | 8.6 (0.072, 0.100) | 100 | < 0.001 |
| Europe | 30.2 (0.274, 0.330) | 99.9 | < 0.001 |
| North America | 28.8 (0.145, 0.431) | 99.3 | < 0.001 |
| Oceania | 29.0 (0.242, 0.341) | 0 | - |
| Diagnostic criteria | |||
| BDI | 43.4 (0.370, 0.499 | 0 | - |
| HADS | 32.3 (0.187, 0.459) | 99.5 | < 0.001 |
| PHQ-9 | 34.4 (0.225, 0.463) | 98.3 | < 0.001 |
| MDI | 72.8 (0.693, 0.761) | 0 | - |
| CES-D | 29.0 (0.242, 0.341) | 0 | - |
| ICD | 6.3 (0.039, 0.087) | 100 | < 0.001 |
| GDS | 44.1 (0.380, 0.503) | 41.2 | 0.183 |
| Anxiety | |||
| Overall prevalence | 13.0 (0.117, 0.142) | 99.9 | < 0.001 |
| Prevalence in adults | 14.5 (0.132, 0.158) | 99.7 | < 0.001 |
| Gender | |||
| Male | 8.7 (0.063, 0.111) | 97.9 | < 0.001 |
| Female | 10.1 (0.069, 0.133) | 97.3 | < 0.001 |
| Age group | |||
| ≥ 60yr | 33.6 (0.246, 0.425) | 95.2 | < 0.001 |
| Other ages | 7.6 (0.063, 0.088) | 99.7 | < 0.001 |
| Region | |||
| Asia | 1.1 (0.010, 0.012) | - | - |
| Europe | 13.9 (0.118, 0.159) | 99.2 | < 0.001 |
| North America | 19.8 (0.149, 0.248) | - | - |
| Study design | |||
| Cross-sectional study | 42.0 (0.322, 0.523) | 0 | - |
| Cohort study | 8.1 (0.053, 0.109) | 99.2 | < 0.001 |
| Other | 24.8 (0.218, 0.277) | 99.6 | < 0.001 |
| Diagnostic criteria | |||
| STAI | 28.7 (0.201, 0.386) | - | - |
| HADS | 31.2 (0.174, 0.449) | 99.4 | < 0.001 |
| ICD | 2.6 (0.013, 0.039) | - | - |
| GAD | 24.0 (0.217, 0.265) | - | - |
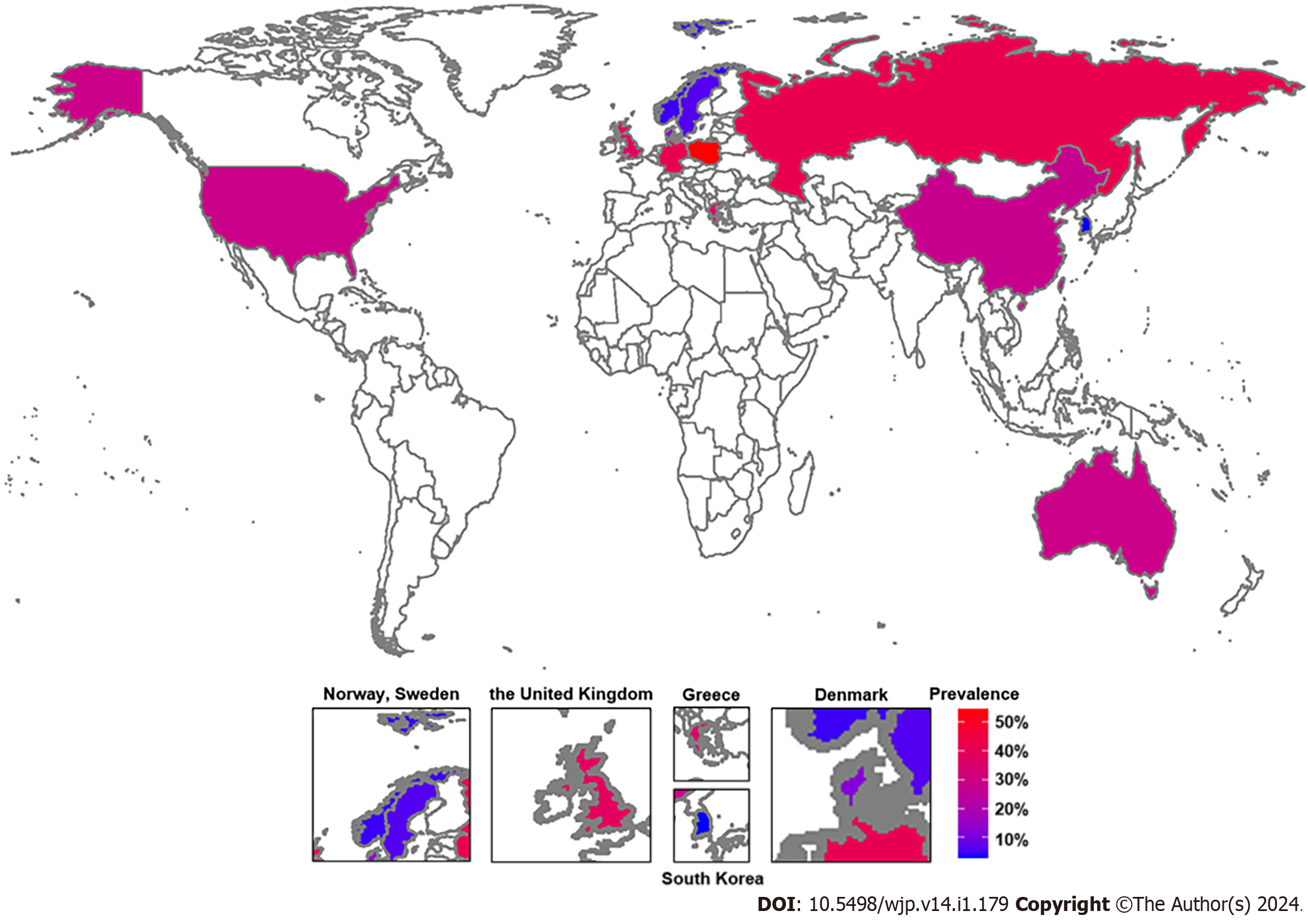
In terms of continents, the prevalence of AF co-morbidity with depression in Europe, Asia, North America, and Oceania was 30.2% (95%CI: 0.274-0.330), 8.6% (95%CI: 0.072-0.100), 28.8% (95%CI: 0.145-0.431), and 29.0% (95%CI: 0.242-0.341), respectively (Table 2, Supplementary Figure 5). European countries such as Poland, Greece, Russia, United Kingdom, Germany, Norway, Sweden and Denmark had a prevalence of 54.5% (95%CI: 0.390-0.700), 35.3% (95%CI: 0.281-0.430), 43.8% (95%CI: 0.295-0.588), 38.6% (95%CI: 0.291-0.488), 37.9% (95%CI: 0.356-0.401), 2.2% (95%CI: 0.021-0.024), 4.0% (95%CI: 0.039-0.040), and12.0% (95%CI: 0.118-0.122), respectively. Similarly, in Asia, countries such China and Korea had a prevalence of 27.8% (95%CI: 0.143-0.412) and 3.0% (95%CI: 0.030-0.030), respectively. The prevalence rates in Oceania and North America were consistent with those in Australia and the United States (Table 2, Supplementary Figure 6). The worldwide prevalence of depression among patients with AF is shown in Figure 2.
We analyzed the impact of different study types on prevalence and found a 58.2% (95%CI: 0.468-0.695) prevalence in cross-sectional, 15.3% (95%CI: 0.124-0.182) in cohort and 24.4% (95%CI: 0.217-0.271) in other studies (Table 2, Supplementary Figure 7). We subsequently analyzed the comorbidity rate of depression in patients with AF using various depression evaluation scales such as beck depression inventory, hospital anxiety and depression scale (HADS), patient health questionnaire (PHQ-9), the major depression inventory, center for epidemiological studies depression scale, international classification of diseases (ICD), and the geriatric depression scale with rates of 43.4% (95%CI: 0.370-0.499), 32.3% (95%CI: 0.187-0.459), 34.4% (95%CI: 0.225-0.463), 72.8% (95%CI: 0.693-0.761), 29.0% (95%CI: 0.242-0.341), 6.3% (95%CI: 0.039-0.087), and 44.1% (95%CI: 0.380-0.503), respectively (Table 2, Supplementary Figure 8).
Anxiety: In estimating the prevalence of anxiety in patients with AF, the meta-analysis identified an overall prevalence of 13.0% (95%CI: 0.117-0.142); 14.5% (95%CI: 0.132–0.158) in adults, 33.6% (95%CI: 0.246-0.425) in older adults ≥ 60 years old, 8.7% (95%CI: 0.063-0.111) in males, and 10.1% (95%CI: 0.069-0.133) in females (Table 2, Supplementary Figures 9-12).
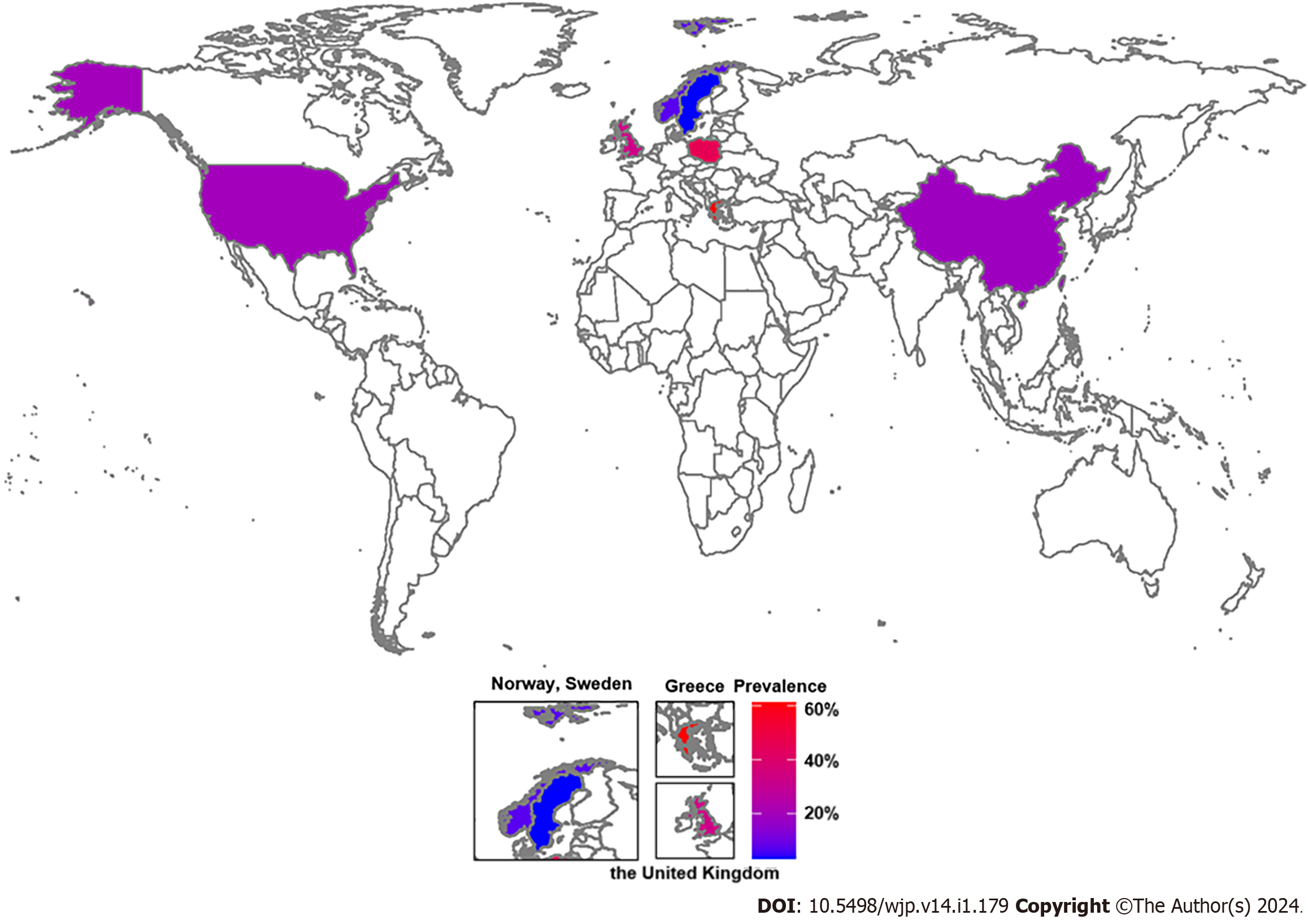
Only three continents, Asia, Europe, and North America, reported a prevalence of anxiety in patients with AF. These were 1.10% (95%CI: 0.010-0.012), 13.9% (95%CI: 0.118-0.159), and 19.8% (95%CI: 0.149-0.248), respectively (Table 2, Supplementary Figure 13). Five studies reported the prevalence in five individual European countries, including Greece, 61.8% (95%CI: 0.540-0.691); Poland, 45.7% (95%CI: 0.396-0.518); United Kingdom, 33.3% (95%CI: 0.268-0.398); Norway, 4.9% (95%CI: 0.047-0.051); and Sweden, 2.7% (95%CI: 0.027-0.028). In Asia and North America, the prevalence of co-morbidity of anxiety with AF was reported only in China and the United States at 1.10% (95%CI: 0.010-0.012) and 19.8% (95%CI: 0.149-0.248), respectively (Table 2, Supplementary Figure 14). The worldwide prevalence of anxiety among patients with AF is shown in Figure 3.
A comparison of the occurrence of anxiety in patients with AF among different observational study types showed a prevalence of 42.0% (95%CI: 0.322-0.523), 8.1% (95%CI: 0.053-0.109), and 24.8% (95%CI: 0.218-0.277) in cross-sectional, cohort and other studies, respectively (Table 2, Supplementary Figure 15). Four criteria were used to diagnose anxiety. The prevalence rate using the state-trait anxiety inventory, HADS, ICD, and generalized anxiety disorder scale was 28.7% (95%CI: 0.201-0.386), 31.2% (95%CI: 0.174-0.449), 2.6% (95%CI: 0.013-0.039), 24.0% (95%CI: 0.217-0.265), respectively (Table 2, Supplementary Figure 16)
A meta-regression analysis was conducted to examine the sources of heterogeneity in the prevalence of anxiety and depression among patients with AF. We found that the diverse study types, diagnostic criteria, and age groups were sources of heterogeneity in the prevalence of AF comorbidity with anxiety (Table 3).
| Possible source of heterogeneity | Number of studies | Coef (95%CI) | P value |
| Depression | |||
| Study design | 24 | 0.40 (-0.18, 0.98) | 0.18 |
| Cross-sectional study | 4 | 1.34 (0.21, 2.47) | 0.02 |
| Cohort study | 6 | -1.76 (-3.03, -0.49) | 0.01 |
| Others | 14 | -1.11 (-2.28, 0.05) | 0.06 |
| Region | 24 | 0.46 (-0.12, 1.04) | 0.11 |
| Asia | 5 | -0.82 (-2.29, 0.64) | 0.27 |
| Europe | 14 | -0.12 (-1.33, 1.10) | 0.85 |
| North America | 4 | 0.29 (-0.87, 1.44) | 0.63 |
| Oceania | 1 | 0.16(-2.38, 2.70) | 0.90 |
| Age group | 24 | -0.67(-1.67, 0.33) | 0.19 |
| ≥ 60 | 7 | 0.33 (-0.70, 1.36) | 0.53 |
| Other ages | 17 | -0.33 (-1.36, 0.70) | 0.53 |
| Diagnostic criteria | 24 | -0.22(0.45, 0.02) | 0.07 |
| BDI | 2 | 0.28 (-2.22, 2.78) | 0.83 |
| HADS | 6 | -2.96 (-2.23, 1.64) | 0.76 |
| PHQ-9 | 6 | 0.02 (-1.86, 1.91) | 0.98 |
| MDI | 1 | 0.93 (-1.56, 3.42) | 0.47 |
| CES-D | 1 | 0.40 (-1.95, 2.76) | 0.74 |
| ICD | 6 | -1.73 (-3.64, 0.17) | 0.07 |
| GDS | 2 | 0.44 (-1.60, 2.48) | 0.67 |
| Anxiety | |||
| Region | 13 | -0.24 (-1.01, 0.52) | 0.53 |
| Asia | 2 | -1.03 (-2.87, 0.81) | 0.27 |
| Europe | 8 | 1.00 (-0.98, 2.97) | 0.32 |
| North America | 3 | 1.14 (-1.16,3.43) | 0.32 |
| Study design | 13 | -0.21 (-1.07, 0.65) | 0.63 |
| Cross-sectional study | 1 | 1.95 (-0.59, 4.50) | 0.13 |
| Cohort study | 4 | -1.30 (-2.61, 0.01) | 0.05 |
| Others | 8 | 1.22 (-0.15, 2.60) | 0.08 |
| Age group | 13 | -1.38 (-2.53, -0.24) | 0.02 |
| ≥ 60 | 5 | 1.15 (-0.13, 2.43) | 0.08 |
| Other ages | 8 | -1.15 (-2.43, 0.13) | 0.08 |
| Diagnostic criteria | 14 | -0.84 (-1.63, -0.05) | 0.04 |
| STAI | 1 | 0.15 (-2.01, 2.32) | 0.89 |
| HADS | 9 | 0.07 (-1.54, 1.67) | 0.94 |
| ICD | 3 | -2.36 (-4.11, -0.61) | 0.01 |
| GAD | 1 | 0.51 (-2.10, 3.13) | 0.70 |
We performed a sensitivity analysis of the prevalence of depression and anxiety in patients with AF and found that the results were robust after applying the respective exclusions (Supplementary Figures 17 and 18).
We analyzed the publication bias for the prevalence of depression and anxiety in adults with AF using Egger’s and Begg’s linear tests. We found the publication bias for these two disorders (Supplementary Figures 19-22). These parameters were then evaluated using the trim-and-fill method. We discovered an increase of 34 and 20 studies on depression and anxiety, respectively, among patients with AF after five iterations. The prevalence of depression and anxiety in patients with AF decreased to 15.8% (95%CI: 0.14-0.17) and 7.9% (95%CI: 0.066-0.091), respectively.
To our knowledge, this is the first study to present the global prevalence of depression and anxiety in patients with AF. After a systematic and holistic evaluation, we identified a 22.0% and 13.0% prevalence of depression and anxiety, respectively, in patients with AF and 24.3% and 14.5% in adults. Furthermore, the prevalence of depression and anxiety in patients with AF was 11.7% and 8.7%, 19.8% and 10.1%, 40.3% and 33.6% in males, females and the elderly, respectively. This prevalence varied in regional distribution. A higher percentage of European (30.2%) and North American (19.8%) patients with AF experienced depression and anxiety, respectively, than those in other continents. Furthermore, the highest percentage of patients with AF and depression and anxiety were found in Poland (54.5%) and Greece (61.8%), respectively. Cardiovascular diseases remain the primary cause of morbidity worldwide, with the total disability-adjusted life years caused by AF and atrial flutter at 8.39 million in 2019[38]. Anxiety, inflammation, and left atrial dilation are significant predictors of the quality of life in patients with AF[39]. Another study indicated that as the severity of AF-specific symptoms increases, there is a positive correlation between the levels of anxiety and depression[19]. Furthermore, one-third of patients with AF were reported to have persistent levels of depression and anxiety at a 6-month follow-up[20]. These findings underscore the importance of identifying and increasing interventions for psychological factors in patients with AF. Our study demonstrated that depression and anxiety in patients with AF exhibit sex and regional differences. The prevalence of AF comorbidity with both depression and anxiety appears to be higher in females than males. This may be linked to sex differences, as studies have shown that women are more likely to develop AF than men[40]. The differences in biological factors between men and women, such as sex hormones, X and Y chromosomes, reactions to stimuli, and body fats, contribute to the sex differences[40]. Age is a crucial risk factor for AF, and its prevalence increases with age. We found that patients with AF aged > 60 years had a higher probability of co-morbidity with depression and anxiety. Furthermore, the high prevalence of depression among patients with AF in Poland may be related to the inclusion of older populations in the reported studies. Additionally, the increasing disease burden due to the aging population in developed countries may contribute to the increasing prevalence of AF[41], the higher prevalence of depression and anxiety in Europe and North America in our study may be related to this aspect. Pathogenic links exist between AF and psychiatric disorders. Autonomic nerves innervate the heart, and AF can be induced when the cardiac action potential receives a rapid discharge stimulus[42]. Previous studies have shown that in states of depression and anxiety, sympathetic nerves are overexcited, and catecholamine secretion increases. High concentrations of catecholamines can damage vascular endothelial cells and cause palpitations on the one hand, leading to the formation of arrhythmic substrates; on the other hand, they accelerate the heart rate, shorten the atrioventricular node's refractory period, depolarize the atrial ectopic pacing point, trigger the feedback mechanism, resulting in AF. In addition, catecholamines can overstimulate β-adrenergic receptors, affect calmodulin expression, impair calcium handling systems, and lead to atrial remodeling[43-45]. Inflammation is another important link between AF and depression or anxiety. Studies have shown that patients with AF have significantly higher serum levels of ultrasensitive C-reactive protein and interleukin 6, and anxiety and depression are strongly associated with these two inflammatory mediators[46,47]. The renin-angiotensin-aldosterone system (RAAS) is also implicated in AF and mental disorders. Anxiety and depression contribute to an active RAAS, which is accompanied by an increase in angiotensin secretion. Elevated levels of angiotensin II promote cardiac fibrosis, slow down cardiomyocyte signaling, and damage the myocardium, leading to myocardial remodeling and an increase in the number of folds, which provides a favorable environment for the development of AF[48-51]. Additionally, it has been demonstrated that chronic stimulation of a rat depression model with sigma-1 receptors with antidepressant effects attenuates atrial electrical remodeling, fibrosis, and AF susceptibility[52]. Furthermore, patients with significant depression share the ZHX3 and ADI1P1 genes with AF patients[53]. Overall, there are few studies on the co-morbidity mechanisms of AF and psychiatric disorders, which could be a direction for future research.
AF treatment involves using antiarrhythmic drugs, direct-current cardioversion, catheter ablation, or surgical ablation to restore and maintain sinus rhythm[54]. A recent randomized controlled trial showed that symptoms of depression and anxiety significantly improved in patients who underwent catheter ablation of AF[55]. In addition, there is evidence of significant improvement in depression and anxiety in patients with AF after treatment with newer anticoagulants, such as rivaroxaban and dabigatran, compared with oral warfarin[56,57]. Some antidepressants protect the body from cardiovascular damage. However, the use of antidepressants in the treatment of AF has been poorly studied[58]. Paroxetine is an antidepressant that reduces the number of episodes of paroxysmal AF and may exert its therapeutic effect by modulating the vagal tone in the brain and inhibiting vasovagal reflexes[59]. In addition, exercise therapy, such as yoga, is an effective option for managing depression and anxiety in patients with AF[60].
Few studies have reported the prevalence of depression and anxiety in patients with AF. Zhuo et al[61] elucidated the correlation between preoperative depression in patients with AF and recurrence after catheter ablation. Three studies analyzed the prevalence and risk index of depression and anxiety in patients with AF[10,11,62]. This study not only presents an analysis of the rate of depression and anxiety in patients with AF but also highlights regional discrepancies in their prevalence by country, allowing for a more visual representation of the data.
Although we tried to be as rigorous as possible, this study had a few limitations. First, the studies we included were published in English or Chinese, which may have resulted in language bias. Second, the prevalence of anxiety in patients with AF was reduced after the trim-and-fill method. This might result from the inclusion of only observational studies in our analysis and our inability to find the “gray literature” in our study. However, after sensitivity analyses, the conclusions were robust. Third, although AF is divided into various types, such as paroxysmal and persistent AF, our study did not address this aspect because no previous study has analyzed the prevalence of diverse types of AF. Additionally, the scales and diagnostic criteria used to evaluate anxiety and depression differed in the included studies, leading to significant differences in prevalence. In the meta-regression, we also found that different scales were a source of heterogeneity and then divided them into subgroups for analysis. Further studies are needed to analyze the prevalence of depression and anxiety in patients with different types of AF and standardize the evaluation criteria for anxiety and depression as much as possible. The mechanism of AF comorbidity with depression and anxiety can be elucidated using molecular biology and cellular immunology, which is another direction for future research. Moreover, large-scale observational epidemiological studies are needed to analyze its prevalence and provide a basis for clinical diagnosis and treatment.
We integrated and systematically analyzed the prevalence of two psychiatric disorders, depression and anxiety, in patients with AF. We found that the prevalence of comorbid psychiatric disorders in patients with AF was associated with sex and region. These facts underscore the need for clinicians to actively engage in mental health interventions in managing patients with AF.
Atrial fibrillation (AF), an irregular and rapid heart rate, is one of the most common types of cardiac arrhythmias. Research has shown that patients with AF are more prone to psychological problems than the general population. These problems increases the recurrence rate of AF while seriously affecting the quality of life, morbidity, and mortality rate of patients.
Anxiety and depression are the two most common mental health disorders worldwide. Studies have independently analyzed the risk of comorbidity with depression and anxiety in patients with AF. No study has systematically focused on the global epidemiology of these two mental disorders in patients with AF. A deeper understanding of the prevalence of comorbid depression and anxiety in these patients is essential in guiding clinical management.
To explore the prevalence of depression and anxiety in patients with AF.
Five databases were searched from their establishment until January 2023. Observational studies reporting the co-morbidity of AF with depression and anxiety–were included. STATA SE 15.1 was applied to analyze the data. Subgroup, meta-regression, and sensitivity analyses were performed to estimate study heterogeneity.
The prevalence rates of depression and anxiety in adults with AF were 24.3% and 14.5%, respectively. Among adult males with AF, the prevalence of depression and anxiety were 11.7% and 8.7%, respectively. This prevalence varied with sex, age and region; in females, it was 19.8% and 10.1%, and 40.3% and 33.6% in the older adults, respectively. The highest prevalence rate of depression and anxiety was observed in European (30.2%) and North American (19.8%) patients with AF. Furthermore, the prevalence varied according to the different evaluation scales.
We found that the prevalence of depression and anxiety among patients with AF was differentially distributed according to sex, region, and evaluation scales, suggesting the need for psychological interventions for patients with AF in clinical practice.
To explore this association further, future studies should focus on assessing the prevalence of depression and anxiety in patients with different types of AF, delineating the mechanisms of AF comorbidity with depression and anxiety using molecular biology and cellular immunology, and carrying out a large-scale observational epidemiological study to analyze its prevalence and provide a basis for clinical diagnosis and treatment.
We thank Professor Xin Li for his guidance and suggestions and Dr. Shun-xian Zhang for his biostatistics review.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen IH, China; Hosak L, Czech Republic; Setiawati Y, Indonesia S-Editor: Qu XL L-Editor: A P-Editor: Chen YX
| 1. | Baman JR, Passman RS. Atrial Fibrillation. JAMA. 2021;325:2218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 62] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 2. | Narayan SM, Cain ME, Smith JM. Atrial fibrillation. Lancet. 1997;350:943-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Elliott AD, Middeldorp ME, Van Gelder IC, Albert CM, Sanders P. Epidemiology and modifiable risk factors for atrial fibrillation. Nat Rev Cardiol. 2023;20:404-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 169] [Reference Citation Analysis (1)] |
| 4. | Kornej J, Börschel CS, Benjamin EJ, Schnabel RB. Epidemiology of Atrial Fibrillation in the 21st Century: Novel Methods and New Insights. Circ Res. 2020;127:4-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 906] [Article Influence: 181.2] [Reference Citation Analysis (0)] |
| 5. | Staerk L, Sherer JA, Ko D, Benjamin EJ, Helm RH. Atrial Fibrillation: Epidemiology, Pathophysiology, and Clinical Outcomes. Circ Res. 2017;120:1501-1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 629] [Cited by in RCA: 807] [Article Influence: 100.9] [Reference Citation Analysis (2)] |
| 6. | Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL; ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42:373-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3176] [Cited by in RCA: 6452] [Article Influence: 1613.0] [Reference Citation Analysis (0)] |
| 7. | World Health Organization. Mental disorders. June 8, 2022. [cited 2 February 2023]. Available from: https://www.who.int/news-room/fact-sheets/detail/mental-disorders. |
| 8. | Goldfarb M, De Hert M, Detraux J, Di Palo K, Munir H, Music S, Piña I, Ringen PA. Severe Mental Illness and Cardiovascular Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2022;80:918-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 93] [Reference Citation Analysis (0)] |
| 9. | Bubien RS, Knotts-Dolson SM, Plumb VJ, Kay GN. Effect of radiofrequency catheter ablation on health-related quality of life and activities of daily living in patients with recurrent arrhythmias. Circulation. 1996;94:1585-1591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 185] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 10. | Lomper K, Ross C, Uchmanowicz I. Anxiety and Depressive Symptoms, Frailty and Quality of Life in Atrial Fibrillation. Int J Environ Res Public Health. 2023;20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Wu H, Li C, Li B, Zheng T, Feng K, Wu Y. Psychological factors and risk of atrial fibrillation: A meta-analysis and systematic review. Int J Cardiol. 2022;362:85-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 12. | Hu WS, Lin CL. Suicide attempt in patients with atrial fibrillation - A nationwide cohort study. Prog Neuropsychopharmacol Biol Psychiatry. 2019;92:470-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Rewiuk K, Wizner B, Klich-Rączka A, Więcek A, Mossakowska M, Chudek J, Szybalska A, Broczek K, Zdrojewski T, Grodzicki T. Atrial fibrillation independently linked with depression in community-dwelling older population. Results from the nationwide PolSenior project. Exp Gerontol. 2018;112:88-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Rizzi SA, Knight S, May HT, Woller SC, Stevens SM, Steinberg BA, Bair TL, Anderson JL, Muhlestein JB, Knowlton KU, Bunch TJ. Depression as a Driving Force for Low Time in Therapeutic Range and Dementia in Patients With and Without Atrial Fibrillation. Am J Cardiol. 2021;153:58-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Polikandrioti M, Koutelekos I, Vasilopoulos G, Gerogianni G, Gourni M, Zyga S, Panoutsopoulos G. Anxiety and Depression in Patients with Permanent Atrial Fibrillation: Prevalence and Associated Factors. Cardiol Res Pract. 2018;2018:7408129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 44] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 16. | Hagengaard L, Polcwiartek C, Andersen MP, Sessa M, Krogager ML, Gislason G, Schou M, Torp-Pedersen C, Søgaard P, Kragholm KH. Incident atrial fibrillation and risk of psychoactive drug redemptions and psychiatric hospital contacts: a Danish Nationwide Register-based Follow-up Study. Eur Heart J Qual Care Clin Outcomes. 2021;7:76-82. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Uchmanowicz I, Lomper K, Gros M, Kałużna-Oleksy M, Jankowska EA, Rosińczuk J, Cyrkot T, Szczepanowski R. Assessment of Frailty and Occurrence of Anxiety and Depression in Elderly Patients with Atrial Fibrillation. Clin Interv Aging. 2020;15:1151-1161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 18. | Krupenin P, Gabitova M, Bordovsky S, Kirichuk Y, Napalkov D, Preobrazhenskaya I, Sokolova A. Impact of atrial fibrillation on the rate of mild cognitive impairment in the elderly. J Neurol Sci. 2018;394:75-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Thompson TS, Barksdale DJ, Sears SF, Mounsey JP, Pursell I, Gehi AK. The effect of anxiety and depression on symptoms attributed to atrial fibrillation. Pacing Clin Electrophysiol. 2014;37:439-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Thrall G, Lip GY, Carroll D, Lane D. Depression, anxiety, and quality of life in patients with atrial fibrillation. Chest. 2007;132:1259-1264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 209] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 21. | von Eisenhart Rothe AF, Goette A, Kirchhof P, Breithardt G, Limbourg T, Calvert M, Baumert J, Ladwig KH. Depression in paroxysmal and persistent atrial fibrillation patients: a cross-sectional comparison of patients enroled in two large clinical trials. Europace. 2014;16:812-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 22. | Wang W, Saczynski J, Lessard D, Mailhot T, Barton B, Waring ME, Sogade F, Hayward R, Helm R, McManus DD. Physical, cognitive, and psychosocial conditions in relation to anticoagulation satisfaction among elderly adults with atrial fibrillation: The SAGE-AF study. J Cardiovasc Electrophysiol. 2019;30:2508-2515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Kim YG, Lee KN, Han KD, Han KM, Min K, Choi HY, Choi YY, Shim J, Choi JI, Kim YH. Association of Depression With Atrial Fibrillation in South Korean Adults. JAMA Netw Open. 2022;5:e2141772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 30] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 24. | Jankowska-Polańska B, Polański J, Dudek K, Sławuta A, Mazur G, Gajek J. The Role of Sleep Disturbance, Depression and Anxiety in Frail Patients with AF-Gender Differences. J Clin Med. 2020;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Feng T, Malmo V, Laugsand LE, Strand LB, Gustad LT, Ellekjær H, Loennechen JP, Mukamal K, Janszky I. Symptoms of anxiety and depression and risk of atrial fibrillation-The HUNT study. Int J Cardiol. 2020;306:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 26. | Wändell P, Carlsson AC, Li X, Sundquist J, Sundquist K. Association Between Relevant Co-Morbidities and Dementia With Atrial Fibrillation-A National Study. Arch Med Res. 2019;50:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Piwoński J, Piwońska A, Jędrusik P, Stokwiszewski J, Rutkowski M, Bandosz P, Drygas W, Zdrojewski T. Depressive symptoms and cardiovascular diseases in the adult Polish population. Results of the NATPOL2011 study. Kardiol Pol. 2019;77:18-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Wändell P, Carlsson AC, Gasevic D, Wahlström L, Sundquist J, Sundquist K. Depression or anxiety and all-cause mortality in adults with atrial fibrillation--A cohort study in Swedish primary care. Ann Med. 2016;48:59-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 29. | Hsu NW, Tsao HM, Chen HC, Lo SS, Chen SA, Chou P. Different Impacts of Atrial Fibrillation and Cardiac Premature Contractions on the Health-Related Quality of Life in Elderly People: The Yilan Study. Tohoku J Exp Med. 2016;238:75-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 30. | Schnabel RB, Michal M, Wilde S, Wiltink J, Wild PS, Sinning CR, Lubos E, Ojeda FM, Zeller T, Munzel T, Blankenberg S, Beutel ME. Depression in atrial fibrillation in the general population. PLoS One. 2013;8:e79109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 31. | Ball J, Carrington MJ, Wood KA, Stewart S; SAFETY Investigators. Women versus men with chronic atrial fibrillation: insights from the Standard versus Atrial Fibrillation spEcific managemenT studY (SAFETY). PLoS One. 2013;8:e65795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 32. | Gehi AK, Sears S, Goli N, Walker TJ, Chung E, Schwartz J, Wood KA, Guise K, Mounsey JP. Psychopathology and symptoms of atrial fibrillation: implications for therapy. J Cardiovasc Electrophysiol. 2012;23:473-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 33. | Wu JH, Li ST, Li QF, Jiang C, Li X, Ning M, Hu R, Du X, Dong JZ, Ma CS. The relationship between severity of atrial fibrillation symptoms and depression of patients and their caregivers. Zhongguo Yiyao. 2021;16:819-822. |
| 34. | Fenger-Grøn M, Vestergaard CH, Frost L, Davydow DS, Parner ET, Christensen B, Ribe AR. Depression and Uptake of Oral Anticoagulation Therapy in Patients With Atrial Fibrillation: A Danish Nationwide Cohort Study. Med Care. 2020;58:216-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 35. | Ariansen I, Dammen T, Abdelnoor M, Tveit A, Gjesdal K. Mental health and sleep in permanent atrial fibrillation patients from the general population. Clin Cardiol. 2011;34:327-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 36. | Rosman L, Lampert R, Ramsey CM, Dziura J, Chui PW, Brandt C, Haskell S, Burg MM. Posttraumatic Stress Disorder and Risk for Early Incident Atrial Fibrillation: A Prospective Cohort Study of 1.1 Million Young Adults. J Am Heart Assoc. 2019;8:e013741. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 37. | Zhang XY. Association between depression and atrial fibrillation in rural populations of Liaoning Province. M.Sc. Thesis, China Medical University. 2017. Available from: https://d.wanfangdata.com.cn/thesis/ChJUaGVzaXNOZXdTMjAyMzA5MDESCFkzMjY4Mjk2Ggh2bG1raWN5aQ%3D%3D. |
| 38. | Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, Barengo NC, Beaton AZ, Benjamin EJ, Benziger CP, Bonny A, Brauer M, Brodmann M, Cahill TJ, Carapetis J, Catapano AL, Chugh SS, Cooper LT, Coresh J, Criqui M, DeCleene N, Eagle KA, Emmons-Bell S, Feigin VL, Fernández-Solà J, Fowkes G, Gakidou E, Grundy SM, He FJ, Howard G, Hu F, Inker L, Karthikeyan G, Kassebaum N, Koroshetz W, Lavie C, Lloyd-Jones D, Lu HS, Mirijello A, Temesgen AM, Mokdad A, Moran AE, Muntner P, Narula J, Neal B, Ntsekhe M, Moraes de Oliveira G, Otto C, Owolabi M, Pratt M, Rajagopalan S, Reitsma M, Ribeiro ALP, Rigotti N, Rodgers A, Sable C, Shakil S, Sliwa-Hahnle K, Stark B, Sundström J, Timpel P, Tleyjeh IM, Valgimigli M, Vos T, Whelton PK, Yacoub M, Zuhlke L, Murray C, Fuster V; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76:2982-3021. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6994] [Cited by in RCA: 6374] [Article Influence: 1274.8] [Reference Citation Analysis (0)] |
| 39. | Charitakis E, Barmano N, Walfridsson U, Walfridsson H. Factors Predicting Arrhythmia-Related Symptoms and Health-Related Quality of Life in Patients Referred for Radiofrequency Ablation of Atrial Fibrillation: An Observational Study (the SMURF Study). JACC Clin Electrophysiol. 2017;3:494-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 40. | Suman S, Pravalika J, Manjula P, Farooq U. Gender and CVD- Does It Really Matters? Curr Probl Cardiol. 2023;48:101604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 41] [Reference Citation Analysis (0)] |
| 41. | Chugh SS, Havmoeller R, Narayanan K, Singh D, Rienstra M, Benjamin EJ, Gillum RF, Kim YH, McAnulty JH Jr, Zheng ZJ, Forouzanfar MH, Naghavi M, Mensah GA, Ezzati M, Murray CJ. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129:837-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2658] [Cited by in RCA: 3336] [Article Influence: 278.0] [Reference Citation Analysis (0)] |
| 42. | Khan AA, Lip GYH, Shantsila A. Heart rate variability in atrial fibrillation: The balance between sympathetic and parasympathetic nervous system. Eur J Clin Invest. 2019;49:e13174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 101] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 43. | Severino P, Mariani MV, Maraone A, Piro A, Ceccacci A, Tarsitani L, Maestrini V, Mancone M, Lavalle C, Pasquini M, Fedele F. Triggers for Atrial Fibrillation: The Role of Anxiety. Cardiol Res Pract. 2019;2019:1208505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 44. | Ran Q, Zhang C, Wan W, Ye T, Zou Y, Liu Z, Yu Y, Zhang J, Shen B, Yang B. Pinocembrin ameliorates atrial fibrillation susceptibility in rats with anxiety disorder induced by empty bottle stimulation. Front Pharmacol. 2022;13:1004888. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 45. | Varró A, Tomek J, Nagy N, Virág L, Passini E, Rodriguez B, Baczkó I. Cardiac transmembrane ion channels and action potentials: cellular physiology and arrhythmogenic behavior. Physiol Rev. 2021;101:1083-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 126] [Article Influence: 25.2] [Reference Citation Analysis (0)] |
| 46. | Hazarapetyan L, Zelveian PH, Grigoryan S. Inflammation and Coagulation are Two Interconnected Pathophysiological Pathways in Atrial Fibrillation Pathogenesis. J Inflamm Res. 2023;16:4967-4975. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 47. | Milaneschi Y, Kappelmann N, Ye Z, Lamers F, Moser S, Jones PB, Burgess S, Penninx BWJH, Khandaker GM. Association of inflammation with depression and anxiety: evidence for symptom-specificity and potential causality from UK Biobank and NESDA cohorts. Mol Psychiatry. 2021;26:7393-7402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 185] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 48. | Vian J, Pereira C, Chavarria V, Köhler C, Stubbs B, Quevedo J, Kim SW, Carvalho AF, Berk M, Fernandes BS. The renin-angiotensin system: a possible new target for depression. BMC Med. 2017;15:144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 92] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 49. | Murck H, Held K, Ziegenbein M, Künzel H, Koch K, Steiger A. The renin-angiotensin-aldosterone system in patients with depression compared to controls--a sleep endocrine study. BMC Psychiatry. 2003;3:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 79] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 50. | Chrissobolis S, Luu AN, Waldschmidt RA, Yoakum ME, D'Souza MS. Targeting the renin angiotensin system for the treatment of anxiety and depression. Pharmacol Biochem Behav. 2020;199:173063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 51. | Healey JS, Morillo CA, Connolly SJ. Role of the renin-angiotensin-aldosterone system in atrial fibrillation and cardiac remodeling. Curr Opin Cardiol. 2005;20:31-37. [PubMed] |
| 52. | Liu X, Qu C, Yang H, Shi S, Zhang C, Zhang Y, Liang J, Yang B. Chronic stimulation of the sigma-1 receptor ameliorates autonomic nerve dysfunction and atrial fibrillation susceptibility in a rat model of depression. Am J Physiol Heart Circ Physiol. 2018;315:H1521-H1531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 53. | Zhang F, Cao H, Baranova A. Shared Genetic Liability and Causal Associations Between Major Depressive Disorder and Cardiovascular Diseases. Front Cardiovasc Med. 2021;8:735136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 54. | January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 2019;140:e125-e151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1137] [Cited by in RCA: 1941] [Article Influence: 323.5] [Reference Citation Analysis (0)] |
| 55. | Al-Kaisey AM, Parameswaran R, Bryant C, Anderson RD, Hawson J, Chieng D, Segan L, Voskoboinik A, Sugumar H, Wong GR, Finch S, Joseph SA, McLellan A, Ling LH, Morton J, Sparks P, Sanders P, Lee G, Kistler PM, Kalman JM. Atrial Fibrillation Catheter Ablation vs Medical Therapy and Psychological Distress: A Randomized Clinical Trial. JAMA. 2023;330:925-933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 34] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 56. | Cosansu K, Ureyen CM, Yılmaz S. Effect of novel oral anticoagulants on Hospital Anxiety and Depression Scale scores. Herz. 2019;44:743-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 57. | Turker Y, Ekinozu I, Aytekin S, Turker Y, Basar C, Baltaci D, Kaya E. Comparison of Changes in Anxiety and Depression Level Between Dabigatran and Warfarin Use in Patients With Atrial Fibrillation. Clin Appl Thromb Hemost. 2017;23:164-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 58. | Chang L, Liu N. The Safety, Efficacy, and Tolerability of Pharmacological Treatment of Depression in Patients with cardiovascular disease: A look at antidepressants and integrative approaches. Heart and Mind. 2017;1:8-16. [DOI] [Full Text] |
| 59. | Shirayama T, Sakamoto T, Sakatani T, Mani H, Yamamoto T, Matsubara H. Usefulness of paroxetine in depressed men with paroxysmal atrial fibrillation. Am J Cardiol. 2006;97:1749-1751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 60. | . Yoga and atrial fibrillation. Eur Heart J. 2016;37:2855. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 61. | Zhuo C, Ji F, Lin X, Jiang D, Wang L, Tian H, Xu Y, Liu S, Chen C. Depression and recurrence of atrial fibrillation after catheter ablation: a meta-analysis of cohort studies. J Affect Disord. 2020;271:27-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 62. | Fu Y, He W, Ma J, Wei B. Relationship between psychological factors and atrial fibrillation: A meta-analysis and systematic review. Medicine (Baltimore). 2020;99:e19615. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |