Published online Aug 19, 2023. doi: 10.5498/wjp.v13.i8.533
Peer-review started: May 6, 2023
First decision: May 19, 2023
Revised: June 15, 2023
Accepted: July 5, 2023
Article in press: July 5, 2023
Published online: August 19, 2023
Processing time: 103 Days and 3.1 Hours
As the perioperative risk of elderly patients with extremely unstable hip fractures (EUHFs) is relatively high and therapeutic effect is not satisfactory, new thera-peutic strategies need to be proposed urgently to improve the efficacy and clinical outcomes of such patients.
To determine the influence of two surgical treatment modalities on postoperative cognitive function (CF) and delirium in elderly patients with EUHFs.
A total of 60 elderly patients consecutively diagnosed with EUHF between September 2020 and January 2022 in the Chongqing University Three Gorges Hospital were included. Of them, 30 patients received conventional treatment (control group; general consultation + fracture type-guided internal fixation), and the other 30 received novel treatment (research group; perioperative multidisciplinary treatment diagnosis and treatment + individualized surgical plan + risk prediction). Information on hip function [Harris hip score (HHS)], perioperative risk of orthopedic surgery [Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity (POSSUM)], CF [Montreal cognitive assessment scale (MoCA)], postoperative delirium [mini-cognitive (Mini-Cog)], adverse events (AEs; internal fixation failure, infection, nonunion, malunion, and postoperative delirium), and clinical indicators [operation time (OT), postoperative hospital length of stay (HLOS), ambulation time, and intraoperative blood loss (IBL)] were collected from both groups for comparative analyses.
The HHS scores were similar between both groups. The POSSUM score at 6 mo after surgery was significantly lower in the research group compared with the control group, and MoCA and Mini-Cog scores were statistically higher. In addition, the overall postoperative complication rate was significantly lower in the research than in the control group, including reduced OT, postoperative HLOS, ambulation time, and IBL.
The new treatment modality has more clinical advantages over the conventional treatment, such as less IBL, faster functional recovery, more effectively optimized perioperative quality control, improved postoperative CF, mitigated postoperative delirium, and reduced operation-related AEs.
Core Tip: Characterized by severe fragmentation, extreme instability, and treatment-refractory, extremely unstable hip fractures (EUHFs) in the elderly population carry a higher perioperative risk. Given the unsatisfactory treatment outcomes of EUHFs in the elderly, there is an urgent need to develop new therapeutic strategies to improve the efficacy and clinical outcomes in these patients, thus providing a guarantee for their life, health, and quality of life.
- Citation: Zhou X, Chen XH, Li SH, Li N, Liu F, Wang HM. Effects of surgical treatment modalities on postoperative cognitive function and delirium in elderly patients with extremely unstable hip fractures. World J Psychiatry 2023; 13(8): 533-542
- URL: https://www.wjgnet.com/2220-3206/full/v13/i8/533.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i8.533
Extremely unstable hip fractures (EUHFs) account for approximately one-fourth of all hip fractures, mainly including Garden grade III and IV fractures of the femoral neck, A2 and A3 intertrochanteric femur fractures, and Seinsheimer type III and IV subtrochanteric femoral fractures, characterized by severe fragmentation, extreme instability, and treatment-refractory[1,2]. EUHF has a predilection for two groups of people: Young people who have suffered major trauma and elderly people with severe osteoporosis and minor trauma[3]. Elderly patients with EUHF have a higher perioperative risk due to their poorer physical conditions than young and middle-aged people and the high likelihood of comorbidities such as hyperlipidemia, hyperglycemia, hypertension, and other internal diseases[4]. Clinically, the surgical treatment modality for elderly patients with EUHF is selected mainly on the fracture type, which not only leads to unsatisfactory treatment outcome but may also cause postoperative cognitive dysfunction in > 40% and postoperative delirium in 5%-61% of patients, severely affecting their quality of life (QoL)[5,6]. Therefore, it is imperative to develop novel treatment strategies to improve the efficacy and clinical outcomes in elderly patients with EUHF and to provide a guarantee for their life, better health, and improved QoL.
Multidisciplinary treatment (MDT) is a diagnosis and treatment model that gathers the backbones of EUHF-related departments, such as geriatrics, critical medicine, anesthesiology, mental health, and rehabilitation medicine, to tailor personalized examination and treatment plans for patients to improve patient diagnosis and treatment experience and enhance treatment efficacy[7-9]. A randomized controlled trial including elderly patients with hip fractures also observed significant improvement in postoperative clinical outcomes using MDT, which suggested that MDT has great application potential in elderly patients with EUHF[10]. On the other hand, anatomic reduction, internal fixation, and effective control of postoperative adverse events (AEs) for EUHFs are the keys to successful surgery due to the vulnerability to fractures of the area involved and the complexity and involvement of the surrounding muscle groups[11,12]. We believe that individualized customization + fracture type co-determined internal fixation is a feasible and safe program, and risk prediction and advance treatment through Mini-Cog plus orthopedic Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity (POSSUM) scale assessment can further help minimize the surgical risks.
To test our conjecture and supplement the evidence-based new treatment model (MDT diagnosis and treatment + individualized surgical plan + risk prediction) still lacks, this study compared the clinical effects of the two surgical treatment modalities through a clinical cohort study to optimize and scientifically guide the clinical treatment.
This study comprised 60 elderly patients diagnosed consecutively with EUHF in the Chongqing University Three Gorges Hospital between September 2020 and January 2022. Of 60, 30 patients were treated using the conventional treatment model of general consultation plus fracture type-guided internal fixation (control group), and the other 30 patients received a new treatment model of perioperative MDT diagnosis and treatment + individualized surgical plan + risk prediction (research group). The two patient groups had similar baseline data (P > 0.05), which was clinically comparable.
Patients diagnosed with extremely unstable femoral intertrochanteric fractures (Garden grade III or IV fractures of the femoral neck, A2 or A3 intertrochanteric femur fractures, or Seinsheimer type III or type IV subtrochanteric femoral fractures), but not old or pathological fractures, using computed tomography, magnetic resonance imaging, and other imaging examinations[13,14], with no severe osteoporosis, t value ≥ -2.5, normal communication and cognitive abilities, and active cooperation were included.
The exclusion criteria were as follows: Other hip diseases; serious nerve; vascular or muscle injuries; other joint diseases; femoral head necrosis; serious infections; diseases such as coagulation dysfunction, cardiopulmonary disease, and renal failure; drug and alcohol addiction; and history of severe trauma around the hip joint.
The control group received conventional treatment, with the following specific measures: Post-admission general consultation was provided to the patients and relevant examinations and treatment were further conducted according to the consultation. The patient’s underlying diseases were stabilized preoperatively; however, another preoperative evaluation was conducted by the anesthesiologist. The surgical protocol was selected depending on the patient’s fracture type. After surgery, the patient’s vital signs, mental state, food intake, blood routine, biochemical indexes, drainage volume, and cardiopulmonary function were obtained, and bilateral lower limb vascular ultrasonography was performed. Prophylactic antibiotics were used within 24 h after surgery, and anticoagulant therapy composed of low molecular weight heparin and rivaroxaban was routinely given. Postoperatively, the affected limb was raised according to the patient’s fracture type, surgical condition, and general condition. In addition, the patient was instructed to perform quadriceps isometric contraction and ankle pump exercises. Those with good wound healing, no hip pain, sound mind, good appetite, no serious complications, and no serious abnormalities in various laboratory indexes were discharged.
The research group adopted a new treatment model, perioperative MDT diagnosis and treatment + individualized surgical plan + risk prediction. Details of the treatment methods are described as follows: (1) After admission, an MDT team, which was led by orthopedic surgeons and composed of professional backbones with intermediate titles or above in geriatrics, critical medicine, anesthesiology, mental health, rehabilitation medicine, and other related departments, was set up. The MDT team evaluated the patients’ specific conditions, formulated personalized examination and treatment plans, and opened green channels to shorten the waiting time for examinations. In addition, the mental state of the patients was adjusted to actively prepare them for surgery, and the time between admission and operation was shortened as much as possible; (2) A surgical protocol was jointly developed based on each patient’s treatment and fracture type, as assessed by the MDT team. If the hemoglobin count was > 90 g/L after blood transfusion, with no hypertension, lower limb deep venous thrombosis (except for those undergoing inferior vena cava filter placement), preoperative delirium, and serious basic diseases, the internal fixation scheme was determined according to the fracture type. For those with preoperative hypoproteinemia, moderate-to-severe anemia that cannot be corrected, severe underlying diseases, and delirium, among others, the internal fixation method was comprehensively considered in combination with the fracture type, and proximal femoral locking plate (PFLP) fixation was performed when necessary; and (3) During the perioperative period, patients were assessed using the Mini-Cog and orthopedic POSSUM scales for delirium and risk prediction, respectively. Patients who were not eligible for surgery at the time were treated by relevant specialists and re-evaluated after their condition improved. The post-surgical patients were re-evaluated by the MDT team, and timely and effective treatment was given if necessary. Those with multiple medical diseases and more serious conditions were admitted to the intensive care unit after the operation. In addition, mental health practitioners assessed the patients’ mental state before and after surgery to better guide the treatment. Moreover, rehabilitation physicians instructed patients to exercise to improve muscle strength and joint range of motion and assisted with early ambulation. Other routine diagnoses, treatments, and discharge standards after the operation were the same as in the control group.
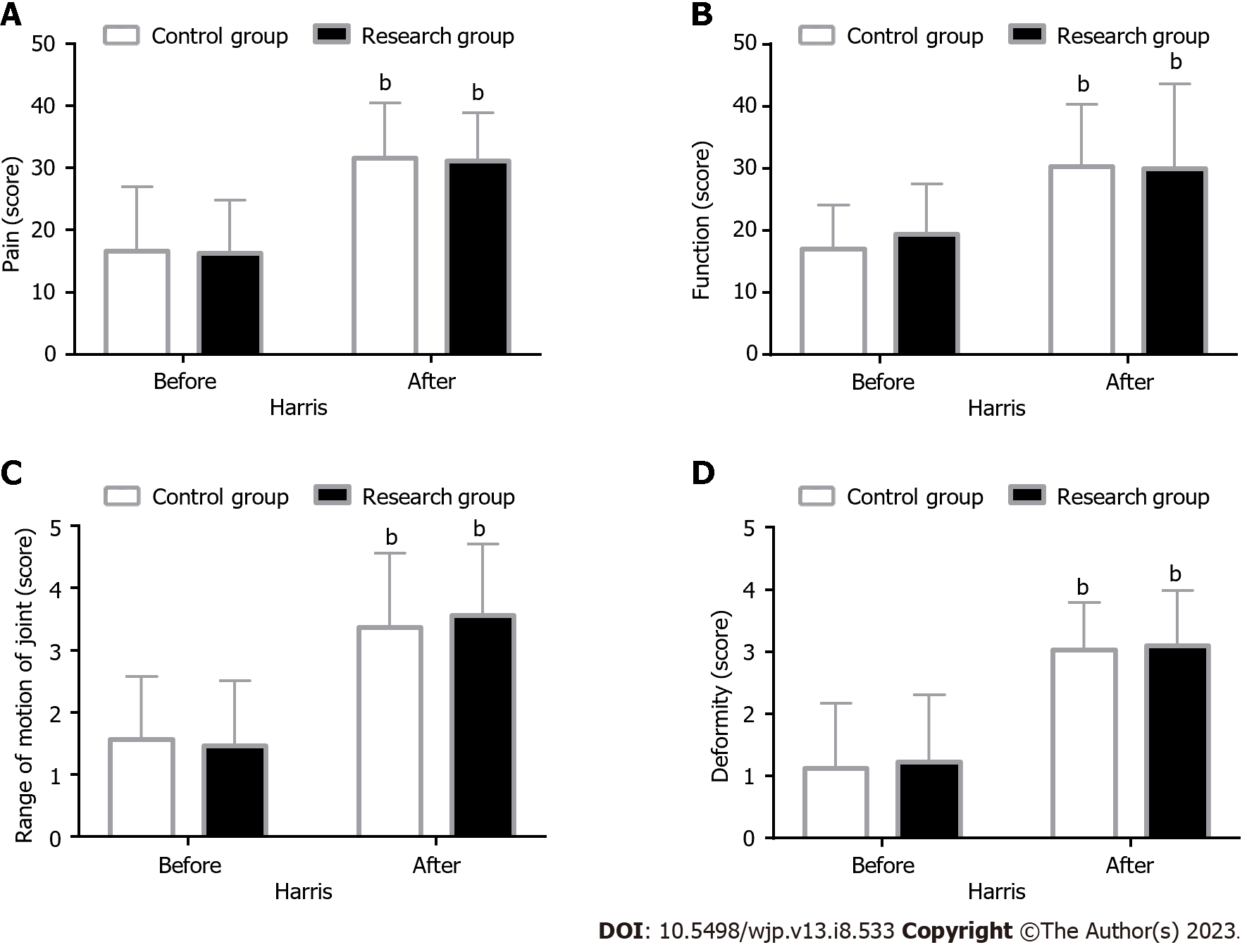
Hip function: Patients’ hip function was assessed using the Harris Hip Score (HHS) before and 6 mo after surgery for pain (0-44 points), function (0-47 points), deformity (0-4 points), and range of motion (0-5 points) components, with a total score of 100 points. A higher score indicated a better hip functional recovery.
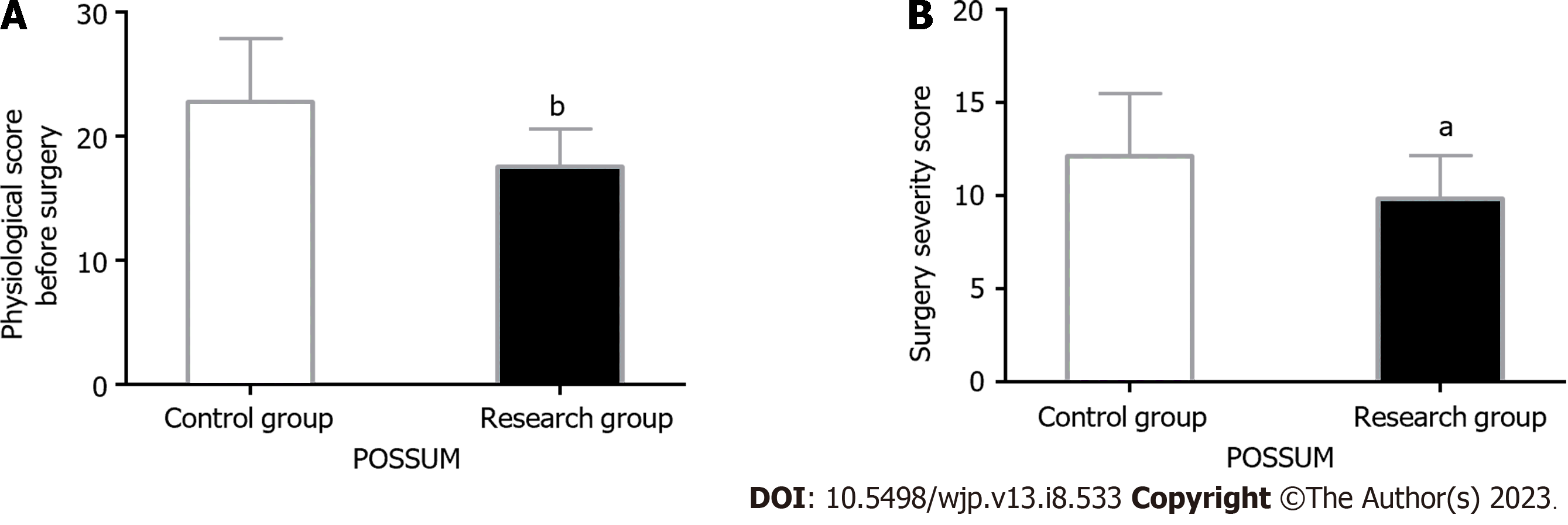
Preoperative risk assessment: The orthopedic POSSUM scoring system, which consists of 12 variables forming the physiological assessment (score range 12-96) and 6 variables forming the operative severity assessment (score range 6-48), was used to evaluate the surgical risk of patients. A higher score suggested a greater risk.
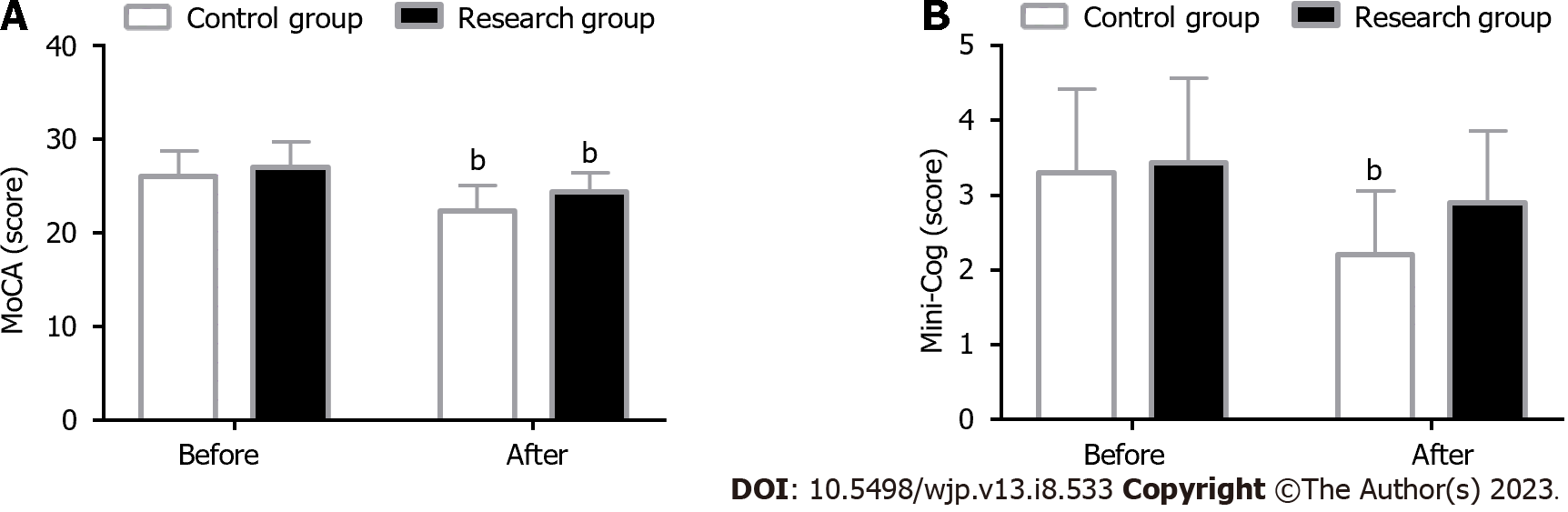
Cognitive function assessment: Using the Montreal Cognitive Assessment Scale (MoCA; score range 0-30), the patients’ cognitive function (CF) was assessed from 11 items in 8 knowledge fields (memory, language, attention and concentration, executive functions, visuospatial skills, abstraction, calculations, and orientation). In addition, the patients’ intelligence was assessed using the Mini-Cognitive (Mini-Cog) scale (score range 0-5). Scores on both scales were proportional to CF.
Incidence rate of AEs: AEs that occurred during treatment, such as internal fixation failure, infection, nonunion, malunion, and postoperative delirium, were observed and recorded in all patients, and the incidence rate was calculated.
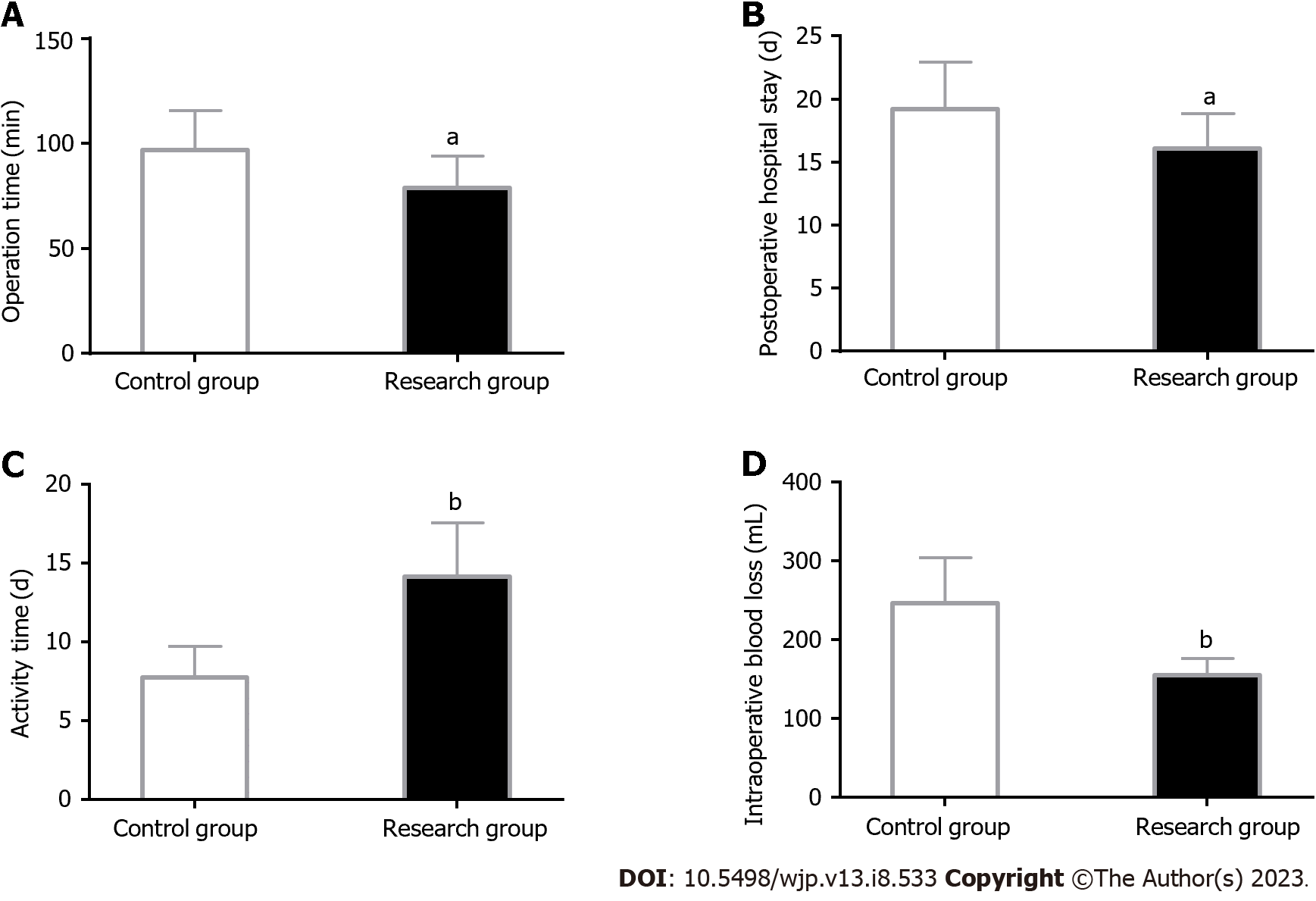
Clinical indicators: Clinical indicators, including operation time (OT), postoperative hospital length of stay (HLOS), ambulation time, and intraoperative blood loss (IBL), were recorded and compared.
All statistical analyses were performed using SPSS 20.0. The mean ± SEM was used to describe continuous variables, and the t-test was used for comparison between groups. Categorical variables were expressed as percentages, and the χ2 test was used for intergroup comparison. P < 0.05 was considered statistically significant.
A comparative analysis of patient general data, such as sex, age, fracture site, hypertension, and diabetes, showed clinical comparability between both groups (P > 0.05; Table 1).
| Categories | Control group (n = 30) | Research group (n = 30) | χ2 value | P value |
| Sex | 0.067 | 0.796 | ||
| Male | 14 (46.67) | 15 (50.00) | ||
| Female | 16 (53.33) | 15 (50.00) | ||
| Age (yr) | 63.20 ± 5.32 | 62.40 ± 6.04 | 0.544 | 0.588 |
| Fracture site | 0.617 | 0.432 | ||
| Left | 11 (36.67) | 14 (46.67) | ||
| Right | 19 (63.33) | 16 (53.33) | ||
| Hypertension | 0.635 | 0.426 | ||
| Yes | 17 (56.67) | 20 (66.67) | ||
| No | 13 (43.33) | 10 (33.33) | ||
| Diabetes | 0.373 | 0.542 | ||
| Yes | 8 (26.67) | 6 (20.00) | ||
| No | 22 (73.33) | 24 (80.00) |
The patients’ hip joint function was evaluated by assessing the pain, function, range of motion, and deformity components of the HHS. The analysis showed no significant intergroup difference in HHS scores before and after intervention (P > 0.05). However, the intragroup comparison revealed markedly elevated HHS scores in both groups after intervention (P < 0.05) (Figure 1).
After the analysis using the orthopedic POSSUM scale, it was found that the preoperative physiological and operative severity scores of the research group were significantly reduced as compared to the control group (P < 0.05) (Figure 2).
A comparative analysis of patients’ CF using the MoCA and Mini-Cog showed no significant difference in both scores between groups prior to the intervention (P > 0.05). After the intervention, the MoCA score was significantly reduced in both groups (P < 0.05), with an even higher score in the research group (P < 0.05). In terms of the Mini-Cog score, a significant decrease was observed in the control group (P < 0.05) as opposed to a non-significant decrease in the research group after intervention (P > 0.05); however, comparatively, the score remained significantly higher in the research group (P < 0.05) (Figure 3).
According to the statistics on internal fixation failure, infection, nonunion, malunion, and postoperative delirium, the total incidence of AEs was found to be significantly lower in the research than in the control group (P < 0.05; Table 2).
| Events | Control group (n = 30) | Research group (n = 30) | χ2 value | P value |
| Internal fixation failure | 1 (3.33) | 1 (3.33) | - | - |
| Infection | 2 (6.66) | 1 (3.33) | - | - |
| Nonunion | 2 (6.66) | 1 (3.33) | - | - |
| Malunion | 2 (6.66) | 0 (0.00) | - | - |
| Postoperative delirium | 3 (10.00) | 0 (0.00) | - | - |
| Total | 10 (33.33) | 3 (10.00) | 4.812 | 0.028 |
The measurement of clinical indexes revealed less OT, postoperative HLOS, and IBL and early ambulation in the research group than in the control group (P < 0.05) (Figure 4).
Conventional treatment is less effective in the treatment of elderly patients with EUHFs, and surgery is currently the treatment of choice to help patients regain their independence, including work ability, faster after injury[15]. In addition, the general consultation model adopted in conventional treatment has some shortcomings, such as delayed treatment time due to repeated preoperative consultation and examination, which leads to various complications in some patients waiting for surgery, including loss of the optimal timing for surgery[16]. Given the above problems, developing effective solutions to optimize the diagnosis and treatment experience of elderly patients with EUHF is imperative.
In this study, the new treatment model was based on MDT diagnosis and treatment + individualized surgical plan + risk prediction, with holistic sequential trauma treatment as the concept[17]. However, the conventional treatment model included general consultation + fracture type-guided internal fixation as the main program and local trauma theory as the main guidance[18]. Herein, significantly enhanced hip joint function, reflected in significantly elevated HHS scores in pain, function, range of motion, and deformity dimensions, was observed in both cohorts after surgery. However, no significant intergroup differences were observed, which suggested that the two surgical treatment modalities had similar effects in elderly patients with EUHF. This may be attributed to the guiding exercise for hip functional rehabilitation administered to patients in both treatment protocols. According to Wu et al[19], the application of MDT in combination with perioperative management in elderly patients with intertrochanteric fractures not only significantly reduced perioperative symptoms but also effectively facilitated postoperative rehabilitation and long-term improvement of hip function, similar to our findings. Surgical treatment of hip fractures is known to be extremely life-threatening for elderly patients, and the prediction and evaluation of surgical risk based on individual differences can be helpful to improve surgical outcomes[14,20]. Therefore, in this study, we used orthopedic POSSUM and Mini-Cog scales to predict the surgical risk and postoperative delirium in elderly patients with EUHF. The data from the orthopedic POSSUM scale showed that the research group had lower preoperative physiological and operative severity scores than the control group, indicating reduced surgical risk under the intervention of the new treatment model. This may be attributed to the preoperative prediction, accurate assessment, and advanced management of complications in patients under the new treatment model. Previous studies have shown that the POSSUM scale has a certain application value in the risk assessment of hip fracture surgery in elderly patients. Risk management based on this scale, combined with the cooperation of the MDT team, can help reduce the mortality and readmission rates of elderly patients with fractures in the perioperative period and improve their functional outcomes[21,22]. Regarding the MoCA and Mini-Cog scores, the post-interventional scores in the research group were notably higher than the post-interventional values in the control group, indicating that the new treatment model can help prevent postoperative cognitive impairment and delirium in such patients. Postoperative cognitive dysfunction and delirium, which are common postoperative complications in elderly patients with hip fractures, have been associated with a significant increase in postoperative serum S100A12 levels[23,24]. Similarly, Zhu et al[25] suggested that perioperative geriatric comprehensive assessment for elderly patients with hip fractures can not only shorten the preoperative waiting time and total hospital stay compared with conventional consultation but also reduce the risk of postoperative delirium, in line with our findings.
Among various AEs, the incidence of internal fixation failure, infection, nonunion, malunion, and postoperative delirium was significantly lower in the research than in the control group, suggesting that it is safe for elderly patients with EUHF to receive the new treatment. The aforementioned prevention of postoperative cognitive impairment and delirium helps to avoid prolonged bed rest, subsequently reducing the risk of bedsores and pulmonary infection, including the incidence of postoperative AEs and mortality[26]. In addition, the orthopedic POSSUM scale was introduced in this study for preoperative comprehensive assessment, allowing for causative or symptomatic treatment of the problems found in the evaluation to significantly reduce postoperative AEs, which also explains the above results[27]. Finally, we found that patients in the research group had more clinical advantages than those in the control group in terms of OT, postoperative HLOS, ambulation time, and IBL, suggesting that the new treatment model can shorten treatment time, promote patients’ rehabilitation, and improve surgical safety. This may be attributed to the emphasis on local trauma and the neglect of overall trauma in the conventional treatment model, which often leads to long OT, excessive bleeding, and more postoperative complications[28,29]. On the contrary, the new treatment model links the difficulty of anatomical reduction with the operation tolerance time and anesthesia mode and applies traditional PFLP fixation to a small number of patients with poor basic conditions. PFLP fixation, a simple clinical procedure, can not only reduce the interference to the blood supply at the fracture end but also increase the stability and strength of the nail-bone combination, which is conducive to shortening the OT while maintaining a certain therapeutic effect[30]. In a study by Rui et al[31], the new treatment model formulated by the MDT team for hip fractures in the elderly is beneficial to shorten the OT and postoperative HLOS, in line with our findings.
The new treatment model using MDT diagnosis and treatment + individualized surgical plan + risk prediction was superior to the conventional treatment model of general consultation + fracture type-guided internal fixation in clinical efficacy to a certain extent. The main clinical advantages of the novel treatment model were lower surgical risks, lower incidence of postoperative AEs, more effectively accelerated patient recovery, and prevention against postoperative cognitive dysfunction and delirium, which can improve the treatment efficacy and experience of elderly patients with EUHF and provide more accurate evidence to guide clinical application.
Given the current high perioperative risk of extremely unstable hip fractures (EUHFs) in elderly patients and the unsatisfactory treatment outcomes, there is an urgent need to propose new treatment strategies to treat these patients.
To improve the efficacy and clinical outcome of EUHFs in the elderly, it is necessary to explore and optimize the relevant treatment strategies.
This study focuses on the clinical application effects of two surgical treatment modalities in older adults with EUHFs.
First, 60 older adults consecutively diagnosed as EUHFs between September 2020 and January 2022 in the Chongqing University Three Gorges Hospital were selected as the research participants, among which 30 cases in the control group (Con) received conventional treatment (general consultation + fracture type-guided internal fixation) and the other 30 cases in the research group (Res) received novel treatment [perioperative multi-disciplinary treatment (MDT) diagnosis and treatment + individualized surgical plan + risk prediction]. Information on hip function (Harris hip score, HHS), perioperative risk of orthopedic surgery (Physiological and Operative Severity Score for the Enumeration of Mortality and Morbidity, POSSUM), CF (Montreal cognitive assessment scale, MoCA), postoperative delirium (mini-cognitive, Mini-Cog), AEs (internal fixation failure, infection, nonunion, malunion, and postoperative delirium), clinical indicators (OT; postoperative hospital length of stay, HLOS; ambulation time; intraoperative blood loss, IBL) were collected from both groups for comparative analyses.
The HHS scores were similar between both groups. The POSSUM score at 6 mo after surgery was significantly lower in the research group compared with the control group, and MoCA and Mini-Cog scores were statistically higher. In addition, the overall postoperative complication rate was significantly lower in the research than in the control group, including reduced OT, postoperative HLOS, ambulation time, and IBL.
With comparable efficacy in fracture healing, the new treatment modality has some clinical advantages over the conventional treatment, such as less IBL, faster functional recovery, more effectively optimized perioperative quality control, improved postoperative cognitive function, mitigated postoperative delirium, and reduced operation-related adverse events.
The novel treatment model of MDT diagnosis and treatment + individualized surgical plan + risk prediction can improve the therapeutic efficacy and experience of elderly patients with EUHFs, providing more accurate evidence to guide the management of EUHFs in clinical practice.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cowie H, United Kingdom; Fitzpatrick O, United States S-Editor: Chen YL L-Editor: A P-Editor: Chen YX
| 1. | Zhong G, Teng L, Li HB, Huang FG, Xiang Z, Cen SQ. Surgical Treatment of Internal Fixation Failure of Femoral Peritrochanteric Fracture. Orthop Surg. 2021;13:1739-1747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Grønhaug KML, Dybvik E, Matre K, Östman B, Gjertsen JE. Intramedullary nail versus sliding hip screw for stable and unstable trochanteric and subtrochanteric fractures: 17,341 patients from the Norwegian Hip Fracture Register. Bone Joint J. 2022;104-B:274-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 37] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 3. | Liu D, Liu HZ, Ma ML, Zhou N, Wang H. The Clinical Efficacy of Minimally Invasive Clamp-Assisted Reduction and Open Reduction with Wire Cerclage for Unstable Subtrochanteric Fractures. J Healthc Eng. 2022;2022:5340504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 4. | Lin TC, Wang PW, Lin CT, Chang YJ, Lin YJ, Liang WM, Lin JC. Primary hemiarthroplasty after unstable trochanteric fracture in elderly patients: mortality, readmission and reoperation. BMC Musculoskelet Disord. 2021;22:403. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Tzimas P, Samara E, Petrou A, Korompilias A, Chalkias A, Papadopoulos G. The influence of anesthetic techniques on postoperative cognitive function in elderly patients undergoing hip fracture surgery: General vs spinal anesthesia. Injury. 2018;49:2221-2226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 60] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 6. | Chen YR, Chen YL, Chen WY, Lin YC, Jane SW. [Evidence-Based Nursing Care of Older Adult Patient With Postoperative Delirium and Hip Fracture]. Hu Li Za Zhi. 2021;68:90-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Savoie MB, Laffan A, Brickman C, Daniels B, Levin A, Rowen T, Smith J, Van Blarigan EL, Hope TA, Berry-Lawhorn JM, Anwar M, Van Loon K. A multi-disciplinary model of survivorship care following definitive chemoradiation for anal cancer. BMC Cancer. 2019;19:906. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Wilson H. Multi-disciplinary care of the patient with acute hip fracture: How to optimise the care for the elderly, traumatised patient at and around the time of the fracture to ensure the best short-term outcome as a foundation for the best long-term outcome. Best Pract Res Clin Rheumatol. 2013;27:717-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Pearce O, Al-Hourani K, Kelly M. Ankle fractures in the elderly: Current concepts. Injury. 2020;51:2740-2747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Halbert J, Crotty M, Whitehead C, Cameron I, Kurrle S, Graham S, Handoll H, Finnegan T, Jones T, Foley A, Shanahan M; Hip Fracture Rehabilitation Trial Collaborative Group. Multi-disciplinary rehabilitation after hip fracture is associated with improved outcome: A systematic review. J Rehabil Med. 2007;39:507-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 88] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Wang J, Ma JX, Lu B, Bai HH, Wang Y, Ma XL. Comparative finite element analysis of three implants fixing stable and unstable subtrochanteric femoral fractures: Proximal Femoral Nail Antirotation (PFNA), Proximal Femoral Locking Plate (PFLP), and Reverse Less Invasive Stabilization System (LISS). Orthop Traumatol Surg Res. 2020;106:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Zhou ZB, Chen S, Gao YS, Sun YQ, Zhang CQ, Jiang Y. Subtrochanteric femur fracture treated by intramedullary fixation. Chin J Traumatol. 2015;18:336-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Sun Q, Li G, Ge W, Lu G, Cai M, Li S. [Effectiveness analysis of surgical treatment of ipsilateral femoral neck fracture and subtrochanteric fracture]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31:1043-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Temiz A, Durak A, Atici T. Unstable intertrochanteric femur fractures in geriatric patients treated with the DLT trochanteric nail. Injury. 2015;46 Suppl 2:S41-S46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2018;19:369. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 169] [Cited by in RCA: 195] [Article Influence: 27.9] [Reference Citation Analysis (0)] |
| 16. | Dash SK, Panigrahi R, Palo N, Priyadarshi A, Biswal M. Fragility Hip Fractures in Elderly Patients in Bhubaneswar, India (2012-2014): A Prospective Multicenter Study of 1031 Elderly Patients. Geriatr Orthop Surg Rehabil. 2015;6:11-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 17. | Lambe K, Guerra S, Salazar de Pablo G, Ayis S, Cameron ID, Foster NE, Godfrey E, Gregson CL, Martin FC, Sackley C, Walsh N, Sheehan KJ. Effect of inpatient rehabilitation treatment ingredients on functioning, quality of life, length of stay, discharge destination, and mortality among older adults with unplanned admission: an overview review. BMC Geriatr. 2022;22:501. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Varady NH, Ameen BT, Chen AF. Is Delayed Time to Surgery Associated with Increased Short-term Complications in Patients with Pathologic Hip Fractures? Clin Orthop Relat Res. 2020;478:607-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Wu F, Hao X, Su J, Cao B. Efficacy Study of Multidisciplinary Team Participating in the Perioperative Administration for Elderly Patients With Intertrochanteric Fractures: A Prospective Randomized Controlled Trail. J Am Acad Orthop Surg. 2023;31:e540-e549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 20. | Chang W, Lv H, Feng C, Yuwen P, Wei N, Chen W, Zhang Y. Preventable risk factors of mortality after hip fracture surgery: Systematic review and meta-analysis. Int J Surg. 2018;52:320-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 103] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 21. | Wanjiang F, Xiaobo Z, Xin W, Ye M, Lihua H, Jianlong W. Application of POSSUM and P-POSSUM scores in the risk assessment of elderly hip fracture surgery: systematic review and meta-analysis. J Orthop Surg Res. 2022;17:255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 22. | Merloz P. Optimization of perioperative management of proximal femoral fracture in the elderly. Orthop Traumatol Surg Res. 2018;104:S25-S30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 23. | Bhushan S, Huang X, Duan Y, Xiao Z. The impact of regional versus general anesthesia on postoperative neurocognitive outcomes in elderly patients undergoing hip fracture surgery: A systematic review and meta-analysis. Int J Surg. 2022;105:106854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 48] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 24. | Li QH, Yu L, Yu ZW, Fan XL, Yao WX, Ji C, Deng F, Luo XZ, Sun JL. Relation of postoperative serum S100A12 levels to delirium and cognitive dysfunction occurring after hip fracture surgery in elderly patients. Brain Behav. 2019;9:e01176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Zhu T, Yu J, Ma Y, Qin Y, Li N, Yang H. Effectiveness of Perioperative Comprehensive Evaluation of Hip Fracture in the Elderly. Comput Intell Neurosci. 2022;2022:4124354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Yates M, Watts JJ, Bail K, Mohebbi M, MacDermott S, Jebramek JC, Brodaty H. Evaluating the Impact of the Dementia Care in Hospitals Program (DCHP) on Hospital-Acquired Complications: Study Protocol. Int J Environ Res Public Health. 2018;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Shields L, Henderson V, Caslake R. Comprehensive Geriatric Assessment for Prevention of Delirium After Hip Fracture: A Systematic Review of Randomized Controlled Trials. J Am Geriatr Soc. 2017;65:1559-1565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 28. | Johnson B, Stevenson J, Chamma R, Patel A, Rhee SJ, Lever C, Starks I, Roberts PJ. Short-term follow-up of pertrochanteric fractures treated using the proximal femoral locking plate. J Orthop Trauma. 2014;28:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 29. | Luthringer TA, Elbuluk AM, Behery OA, Cizmic Z, Deshmukh AJ. Salvage of failed internal fixation of intertrochanteric hip fractures: clinical and functional outcomes of total hip arthroplasty versus hemiarthroplasty. Arthroplast Today. 2018;4:383-391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 30. | Polat G, Akgül T, Ekinci M, Bayram S. A biomechanical comparison of three fixation techniques in osteoporotic reverse oblique intertrochanteric femur fracture with fragmented lateral cortex. Eur J Trauma Emerg Surg. 2019;45:499-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Rui Y, Qiu X, Zou J, Xie T, Ma B, Lu P, Li Y, Liu S, Jin J, Deng C, Cui Y, Wang X, Ma M, Ren L, Yang Y, Wang C, Chen H. [Clinical application of multidisciplinary team co-management in geriatric hip fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33:1276-1282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |