Published online Jul 19, 2023. doi: 10.5498/wjp.v13.i7.461
Peer-review started: January 20, 2023
First decision: February 21, 2023
Revised: February 27, 2023
Accepted: April 24, 2023
Article in press: April 24, 2023
Published online: July 19, 2023
Processing time: 179 Days and 4 Hours
Depression and anxiety were both ranked among the top 25 leading causes of global burden of diseases in 2019 prior to the coronavirus disease 2019 (COVID-19) pandemic. The pandemic affected, and in many cases threatened, the health and lives of millions of people across the globe and within the first year, global prevalence of anxiety and depression increased by 25% with the greatest influx in places highly affected by COVID-19.
To explore the psychological impact of the pandemic and resultant restrictions in different countries using an opportunistic sample and online questionnaire in different phases of the pandemic.
A repeated, cross-sectional online international survey of adults, 16 years and above, was carried out in 10 countries (United Kingdom, India, Canada, Bangladesh, Ukraine, Hong Kong, Pakistan, Egypt, Bahrain, Saudi Arabia). The online questionnaire was based on published approaches to understand the psychological impact of COVID-19 and the resultant restrictions. Five standardised measures were included to explore levels of depression [patient health questionnaire (PHQ-9)], anxiety [generalized anxiety disorder (GAD) assessment], impact of trauma [the impact of events scale-revised (IES-R)], loneliness (a brief loneliness scale), and social support (The Multi-dimensional Scale of Perceived Social support).
There were two rounds of the online survey in 10 countries with 42866 participants in Round 1 and 92260 in Round 2. The largest number of participants recruited from the United Kingdom (112985 overall). The majority of participants reported receiving no support from mental health services throughout the pandemic. This study found that the daily cumulative COVID-19 cases had a statistically significant effect on PHQ-9, GAD-7, and IES-R scores. These scores significantly increased in the second round of surveys with the ordinary least squares regression results with regression discontinuity design specification (to control lockdown effects) confirming these results. The study findings imply that participants’ mental health worsened with high cumulative COVID-19 cases.
Whist we are still living through the impact of COVID-19, this paper focuses on its impact on mental health, discusses the possible consequences and future implications. This study revealed that daily cumulative COVID-19 cases have a significant impact on depression, anxiety, and trauma. Increasing cumulative cases influenced and impacted education, employment, socialization and finances, to name but a few. Building a database of global evidence will allow for future planning of pandemics, particularly the impact on mental health of populations considering the cultural differences.
Core Tip: This study explores the effect of cumulative coronavirus disease 2019 cases on mental health, more specifically on anxiety, depression, and trauma. Negative impact on mental health was found internationally, with individuals struggling to receive support from mental health services. Results also show that as the pandemic continued, mental health scores got worse.
- Citation: Rathod S, Pallikadavath S, Graves E, Rahman MM, Brooks A, Rathod P, Bhargava R, Irfan M, Aly R, Mohammad Saleh Al Gahtani H, Salam Z, Chau SWH, Paterson TSE, Turner B, Gorbunova V, Klymchuk V, Phiri P. Effects of cumulative COVID-19 cases on mental health: Evidence from multi-country survey. World J Psychiatry 2023; 13(7): 461-477
- URL: https://www.wjgnet.com/2220-3206/full/v13/i7/461.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i7.461
Depression and anxiety conditions both ranked among the top 25 leading causes of global burden of diseases in 2019 prior to the coronavirus disease 2019 (COVID-19) pandemic[1]. On January 30, 2020, the World Health Organization (WHO) declared a public health emergency of international concern and governments were urged to prepare for the global spread of COVID-19 from East Asia[2]. The COVID-19 pandemic affected, and in many cases threatened the health and lives of millions of people across the globe[2].
In the first year of the COVID-19 pandemic, global prevalence of anxiety and depression increased by 25%, and overall, the pandemic was estimated to have caused 137.1 (95%UI: 92.5–190.6) additional disability adjusted life years per 100000 population for Major Depressive Disorder and 116.1 per 100000 population (95%UI: 79.3–163.80) for anxiety disorders according to a scientific brief released by the WHO[3]. A number of factors have been implicated including, but not limited to, the stress of social and self-isolation, loneliness, restrictions due to lockdowns[4,5], fear of infection and death of self and near ones, grief and bereavement, worries regarding jobs and finances, as well as impact on education, relationships and on carers[6].
Long COVID described the presence of persistent symptoms following infection from the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus[7]. This can last weeks or months after initial infection[7,8]. Common symptoms of long COVID include breathlessness, fatigue, headaches, and weakness as well as reduced quality of life[7,9]. The most common mental health problems experienced by individuals with long COVID were anxiety, depression, and post-traumatic stress disorder (PTSD)[9,10]. A scoping review of 239 patients found that 3-mo post-COVID, 37.2% experienced PTSD, 35.6% experienced anxiety, and 46.9% were experiencing depression[11,12]. These effects were maintained at 6-mo[11]. Overall, symptoms were more prevalent in women and hospitalized patients[9]. A number of population groups have been shown to have been more adversely affected, including young people and women[7], individuals with vulnerabilities and pre-existing mental health conditions[9,11]. Evidence on healthcare workers, who were frontline during the pandemic has been equivocal with different studies showing a range of impact in this group[11,13]. The greatest increases in depression and anxiety were found in places highly affected by COVID-19 as indicated by decreased human mobility and daily COVID-19 infection rates[3].
Each country across the globe has responded to the pandemic guided by their population, resources, number of cases, socio demographics, political landscape, and culture[14]. Given the unique situation we faced, the authors sought to explore the psychological impact of the pandemic and resultant restrictions in different countries, using an opportunistic sample and online questionnaire that was established at the beginning of the pandemic.
This international study aimed to investigate and report the psychological impact of cumulative COVID-19 cases in the participant sites. A repeated, cross-sectional online international survey of adults, 16 years and above, was carried out in 10 countries (United Kingdom, India, Canada, Bangladesh, Ukraine, Hong Kong, Pakistan, Egypt, Bahrain, Saudi Arabia). The online questionnaire was based on published approaches, to understand the psychological impact of COVID-19 and the resultant restrictions. Five standardised measures were included to explore levels of depression [patient health questionnaire-9 (PHQ-9)][15], anxiety [generalized anxiety disorder (GAD)-7; Generalised Anxiety Disorder Assessment][16], impact of trauma [the impact of events scale-revised (IES-R)][17], loneliness (a brief loneliness scale)[18], and social support (The Multi-dimensional Scale of Perceived Social support)[19]. Further details of the methodology are documented in earlier publications by the group[9,13].
The survey was repeated to capture the dynamic impact of the pandemic. The questionnaire was changed for each round depending on the stage of pandemic, government policies, and circumstances in each country at the time. In order to make the questionnaire relevant to each country, it was available in different languages and various adaptations were made to ensure that local culture and responses to the pandemic were considered. For this reason, each country published the questionnaire at a slightly different time and some of the questions were variable. As an example, the “Keyworker” status did not exist in many countries and was only used where relevant. Another example, in the Ukraine questionnaire version, the question about exceeding the recommended limits of alcohol was excluded because of the absence of such recommended limits.
In the United Kingdom, the survey was conducted thrice with the corresponding two rounds of the survey in the other countries. The dates of the surveys in the participant countries are noted below. The surveys were publicised to the general population including students and healthcare professionals through social media. Most countries collaborated internally to capture a wide population. As an example, the leads in Ukraine collaborated with Ukrainian organizations including Mental health for Ukraine Project, National Psychological Association of Ukraine, Ukrainian Association of Cognitive-Behavioural Therapy, and Zhytomyr State University to help further with dissemination. Due to the unusual circumstances of the time, this was the best way to disseminate the survey.
Southern Health NHS Foundation Trust in the United Kingdom led and co-ordinated the online survey with support from the participant countries. The survey was advertised to staff, patients, and the public with a weblink to the survey platform.
Cumulative COVID-19 case data has been derived from Microsoft Azure Open dataset, which is a population open dataset[20]. Mental health scores are derived from the online survey and is sample data. In both data, time is day. Although cumulative COVID-19 cases data is available daily (for around last two years), mental health scores in the study were not available for each day during that time. The availability of mental health scores on a specific day depended on whether the survey was conducted on that day by a participant.
The study has used regression analyses, using cross section data of all countries that participated in the study. Separate regression analysis was conducted for survey round 1 and 2. In both regressions, we used dummies for all individual characteristics listed in Table 1 as control variables. Vulnerabilities including requiring shielding, experience of coronavirus, pre-existing mental health conditions, and mental health support, had extremely low response rates therefore, we have recoded missing values into no category, to increase sample sizes in regressions.
| Arabic | Bangladesh | Canada | China | India | Pakistan | United Kingdom | Ukraine | ||||||||
| 1 | 2 | 1 | 2 | 1 | 2 | 1 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | |
| Observations | 1121 | 909 | 299 | 746 | 8648 | 5920 | 178 | 1427 | 68 | 803 | 160 | 29134 | 83851 | 1256 | 606 |
| Percent of above observations | |||||||||||||||
| Healthcare professional | |||||||||||||||
| No | 40 | 9 | 67 | 69 | 88 | 91 | 65 | 65 | 40 | 44 | 41 | 47 | 66 | 79 | 74 |
| Yes | 38 | 66 | 4 | 5 | 7 | 9 | 19 | 19 | 44 | 0 | 34 | 43 | 22 | 9 | 10 |
| Missing | 22 | 25 | 29 | 26 | 5 | 0 | 16 | 16 | 16 | 56 | 25 | 10 | 12 | 12 | 16 |
| Age category | |||||||||||||||
| Under 25 | 10 | 4 | 69 | 68 | 8 | 16 | 2 | 20 | 7 | 20 | 51 | 6 | 6 | 35 | 15 |
| 25-44 | 44 | 61 | 14 | 14 | 36 | 36 | 43 | 44 | 44 | 35 | 26 | 36 | 31 | 43 | 54 |
| 45-54 | 16 | 9 | 2 | 1 | 15 | 16 | 12 | 11 | 16 | 3 | 4 | 23 | 19 | 9 | 13 |
| 55 and over | 7 | 3 | 1 | 1 | 37 | 32 | 26 | 13 | 21 | 2 | 1 | 26 | 34 | 2 | 3 |
| Missing | 22 | 22 | 14 | 17 | 5 | 0 | 17 | 13 | 12 | 40 | 18 | 10 | 11 | 11 | 15 |
| White ethnicity | |||||||||||||||
| No | 77 | 21 | 92 | 89 | 20 | 21 | 9 | 88 | 88 | 81 | 73 | 9 | 15 | 3 | 3 |
| Yes | 1 | 57 | 0 | 0 | 76 | 78 | 79 | 0 | 0 | 0 | 0 | 82 | 74 | 88 | 82 |
| Missing | 22 | 22 | 8 | 11 | 4 | 0 | 12 | 12 | 12 | 19 | 27 | 10 | 11 | 9 | 15 |
| Christian religion | |||||||||||||||
| No | 8 | 73 | 92 | 87 | 48 | 52 | 8 | 80 | 78 | 81 | 75 | 48 | 46 | 21 | 22 |
| Yes | 70 | 4 | 0 | 0 | 47 | 47 | 32 | 7 | 9 | 0 | 0 | 41 | 39 | 69 | 62 |
| Missing | 22 | 22 | 8 | 13 | 5 | 1 | 60 | 13 | 13 | 19 | 25 | 11 | 15 | 11 | 16 |
| Gender | |||||||||||||||
| Female | 50 | 27 | 22 | 23 | 56 | 54 | 61 | 60 | 56 | 49 | 61 | 74 | 61 | 77 | 74 |
| Male | 28 | 51 | 68 | 63 | 39 | 45 | 24 | 27 | 31 | 31 | 18 | 15 | 26 | 13 | 9 |
| Missing | 22 | 22 | 10 | 14 | 5 | 1 | 15 | 13 | 13 | 20 | 21 | 11 | 13 | 11 | 16 |
| Attended university | |||||||||||||||
| No | 78 | 79 | 91 | 88 | 51 | 53 | 85 | 38 | 79 | 80 | 83 | 90 | 89 | 90 | 85 |
| Yes | 0 | 0 | 0 | 0 | 43 | 47 | 0 | 50 | 9 | 0 | 0 | 0 | 0 | 0 | 0 |
| Missing | 22 | 21 | 9 | 12 | 6 | 0 | 15 | 13 | 12 | 20 | 18 | 10 | 11 | 10 | 15 |
| Living at own home | |||||||||||||||
| No | 43 | 52 | 64 | 53 | 35 | 41 | 37 | 49 | 0 | 43 | 41 | 25 | 29 | 54 | 41 |
| Yes | 35 | 26 | 26 | 35 | 61 | 59 | 51 | 39 | 0 | 38 | 40 | 66 | 61 | 36 | 44 |
| Missing | 22 | 22 | 10 | 12 | 5 | 0 | 13 | 12 | 100 | 19 | 19 | 10 | 11 | 10 | 15 |
| Vulnerable according to government category | |||||||||||||||
| No | 63 | 34 | 74 | 52 | 63 | 66 | 71 | 68 | 0 | 68 | 46 | 70 | 67 | 76 | 54 |
| Age ≥ 70 | 1 | 40 | 9 | 36 | 15 | 34 | 5 | 7 | 0 | 2 | 31 | 4 | 21 | 1 | 29 |
| Chronic disease | 2 | 0 | 1 | 0 | 6 | 0 | 2 | 1 | 0 | 2 | 0 | 6 | 0 | 4 | 0 |
| Diabetes | 2 | 0 | 0 | 0 | 3 | 0 | 4 | 1 | 0 | 0 | 0 | 2 | 0 | 0 | 0 |
| Other | 3 | 0 | 3 | 0 | 7 | 0 | 1 | 2 | 0 | 3 | 0 | 5 | 0 | 3 | 0 |
| Missing | 28 | 26 | 13 | 12 | 6 | 0 | 16 | 19 | 100 | 25 | 23 | 13 | 12 | 16 | 17 |
| Vulnerable according to government category and require shielding | |||||||||||||||
| No | 64 | 0 | 85 | 0 | 75 | 0 | 77 | 72 | 0 | 67 | 0 | 77 | 0 | 72 | 0 |
| Yes | 6 | 0 | 2 | 0 | 13 | 0 | 5 | 6 | 0 | 6 | 0 | 7 | 0 | 11 | 0 |
| Missing | 30 | 100 | 14 | 100 | 12 | 100 | 18 | 22 | 100 | 26 | 100 | 16 | 100 | 17 | 100 |
| Whether experienced coronavirus | |||||||||||||||
| No | 23 | 0 | 42 | 0 | 28 | 0 | 58 | 35 | 0 | 28 | 0 | 22 | 0 | 31 | 0 |
| Yes | 49 | 29 | 40 | 23 | 63 | 12 | 26 | 43 | 25 | 43 | 48 | 64 | 25 | 52 | 47 |
| Missing | 28 | 71 | 17 | 77 | 8 | 88 | 16 | 22 | 75 | 29 | 53 | 14 | 75 | 17 | 53 |
| Pre-existing mental health condition | |||||||||||||||
| No | 42 | 0 | 46 | 1 | 62 | 1 | 74 | 67 | 3 | 40 | 0 | 53 | 0 | 60 | 0 |
| Yes | 28 | 3 | 41 | 5 | 31 | 21 | 8 | 11 | 4 | 35 | 11 | 31 | 18 | 23 | 9 |
| Missing | 30 | 97 | 13 | 95 | 7 | 79 | 18 | 22 | 93 | 25 | 89 | 16 | 82 | 17 | 91 |
| Drinking alcohol | |||||||||||||||
| No | 68 | 64 | 76 | 77 | 20 | 54 | 28 | 57 | 47 | 0 | 0 | 13 | 75 | 17 | 0 |
| Yes | 5 | 1 | 12 | 6 | 74 | 22 | 56 | 24 | 35 | 0 | 5 | 75 | 11 | 69 | 1 |
| Missing | 27 | 35 | 13 | 17 | 5 | 24 | 16 | 19 | 18 | 100 | 95 | 12 | 14 | 14 | 99 |
| Whether taking drug | |||||||||||||||
| No | 71 | 65 | 81 | 73 | 83 | 86 | 79 | 78 | 82 | 71 | 69 | 85 | 83 | 83 | 77 |
| Yes | 0 | 4 | 8 | 11 | 12 | 14 | 6 | 2 | 1 | 3 | 6 | 2 | 3 | 3 | 2 |
| Missing | 28 | 31 | 11 | 15 | 5 | 0 | 15 | 20 | 16 | 26 | 25 | 13 | 13 | 14 | 21 |
| Ever experienced suicidal thoughts | |||||||||||||||
| No | 9 | 61 | 70 | 69 | 67 | 77 | 74 | 68 | 66 | 55 | 55 | 59 | 60 | 60 | 53 |
| Yes | 62 | 7 | 18 | 16 | 27 | 23 | 10 | 12 | 16 | 19 | 18 | 27 | 26 | 24 | 28 |
| Missing | 29 | 32 | 13 | 15 | 6 | 1 | 16 | 21 | 18 | 26 | 27 | 13 | 14 | 16 | 19 |
| Having mental health support from | |||||||||||||||
| No support | 18 | 1 | 27 | 3 | 13 | 4 | 6 | 5 | 3 | 30 | 4 | 14 | 5 | 13 | 2 |
| Health service provider | 6 | 1 | 5 | 1 | 11 | 6 | 2 | 3 | 1 | 8 | 3 | 12 | 8 | 6 | 5 |
| Other | 3 | 1 | 7 | 1 | 7 | 10 | 2 | 2 | 1 | 4 | 3 | 5 | 4 | 7 | 1 |
| Missing | 73 | 97 | 61 | 95 | 69 | 80 | 90 | 89 | 94 | 58 | 90 | 69 | 83 | 75 | 91 |
In both regressions, the main independent variable, daily cumulative COVID-19 cases, is converted into million unit (by dividing COVID-19 case by 1000000). The purpose is to scale up its coefficients.
The relationship between average mental health scores and average cumulative COVID-19 cases maybe be contaminated or biased by lockdown effects. To control for such effects, we added lockdown dummy, trend and their interaction following the specification in regression discontinuity design (RDD).
There were two rounds of the online survey in eight country groups as shown in Table 1. Egypt, Saudi Arabia, and Bahrain were analysed as a single group (labelled Arabic speaking countries). Hong Kong did not participate in the second round due to difficulties in recruitment. While there were three rounds in the United Kingdom, we have only used data from the corresponding two rounds with other participant countries. The United Kingdom has the largest number of participants in both rounds (29134 and 83851, respectively).
In the first round of the survey, participants who reported being healthcare professionals are higher in the United Kingdom (43%). In the second round, Arabic speaking countries had the highest number of participants who reported as healthcare professionals (66%), with a sample size of 909.
Age follows a bell shaped or downward distribution. Female participants were higher than male in most countries. In Canada, United Kingdom and Ukraine, most participants were White. Christian religion was reported the dominant religion in the Western countries. In round one in the Arabic speaking countries, most survey participants reported as Christians too. In most countries, survey participants did not report University education. Most survey participants lived in their own homes. Low proportion of participants reported experiencing COVID-19, but a high percent of participants followed social distancing guidelines. Most of the participants did not report any pre-existing physical health conditions. Alcohol consumption was reported by participants in Canada, United Kingdom, and Ukraine. Most participants did not report taking drugs. Majority participants did not report receiving support from mental health services. Where received, mental health support was reported through general practitioners and many participants did not respond to this question as it was only relevant if they reported experiencing mental health problems.
Table 2 shows means and SD of PHQ-9, GAD-7 and IES-R by country and survey rounds, with number of respondents
| PHQ-9 | GAD-7 | IES-R | |||||
| Round 1 | Round 2 | Round 1 | Round 2 | Round 1 | Round 2 | ||
| Arabic | Mean | 7.85 | 6.27 | 5.28 | 4.56 | 20.81 | 17.14 |
| SD | 6.97 | 6.88 | 5.78 | 5.56 | 18.79 | 19.12 | |
| n | 596 | 481 | 596 | 486 | 539 | 430 | |
| Missing | 525 | 428 | 525 | 423 | 582 | 479 | |
| Bangladesh | Mean | 8.07 | 7.45 | 5.76 | 5.45 | 23.28 | 21.86 |
| SD | 5.79 | 6.91 | 5.38 | 5.69 | 18.08 | 20.35 | |
| n | 205 | 462 | 205 | 485 | 179 | 419 | |
| Missing | 94 | 284 | 94 | 261 | 120 | 327 | |
| Canada | Mean | 6.11 | 6.97 | 4.40 | 4.94 | 15.10 | 16.96 |
| SD | 6.44 | 6.70 | 5.32 | 5.46 | 17.87 | 18.24 | |
| n | 7653 | 5721 | 7684 | 5770 | 7329 | 5554 | |
| Missing | 995 | 199 | 964 | 150 | 1319 | 366 | |
| China | Mean | 4.38 | 3.25 | 11.61 | |||
| SD | 4.91 | 4.20 | 13.63 | ||||
| n | 127 | 124 | 117 | ||||
| Missing | 51 | 54 | 61 | ||||
| India | Mean | 4.99 | 4.07 | 3.46 | 2.43 | 14.65 | 10.24 |
| SD | 5.56 | 5.34 | 4.38 | 3.31 | 16.49 | 12.00 | |
| n | 820 | 41 | 823 | 42 | 741 | 38 | |
| Missing | 607 | 27 | 604 | 26 | 686 | 30 | |
| Pakistan | Mean | 8.55 | 8.64 | 5.10 | 5.37 | 19.02 | 19.59 |
| SD | 7.34 | 7.51 | 5.56 | 5.42 | 17.26 | 19.18 | |
| n | 412 | 85 | 413 | 90 | 376 | 75 | |
| Missing | 391 | 75 | 390 | 70 | 427 | 85 | |
| United Kingdom | Mean | 7.70 | 8.21 | 5.46 | 6.04 | 17.01 | 19.19 |
| SD | 6.47 | 7.03 | 5.51 | 5.92 | 17.51 | 18.93 | |
| n | 22166 | 64382 | 22343 | 65056 | 20780 | 59966 | |
| Missing | 6968 | 19469 | 6791 | 18795 | 8354 | 23885 | |
| Ukraine | Mean | 6.63 | 7.81 | 4.17 | 5.02 | 14.93 | 15.55 |
| SD | 6.10 | 6.51 | 4.65 | 5.20 | 15.34 | 15.41 | |
| n | 860 | 421 | 863 | 426 | 782 | 382 | |
| Missing | 396 | 185 | 393 | 180 | 474 | 224 | |
| Total | Mean | 7.24 | 8.09 | 5.11 | 5.93 | 16.55 | 18.98 |
| SD | 6.49 | 7.01 | 5.45 | 5.88 | 17.57 | 18.88 | |
| n | 32839 | 71593 | 33051 | 72355 | 30843 | 66864 | |
| Missing | 10027 | 20667 | 9815 | 19905 | 12023 | 25396 | |
For each country, cumulative COVID-19 cases (the cumulative number of people who suffered coronavirus in official records) varied over time. Mental health scores (on the 3 scales: PHQ-9, GAD-7 and IES-R) in each country varied over time and by individuals’ responses during the survey period.
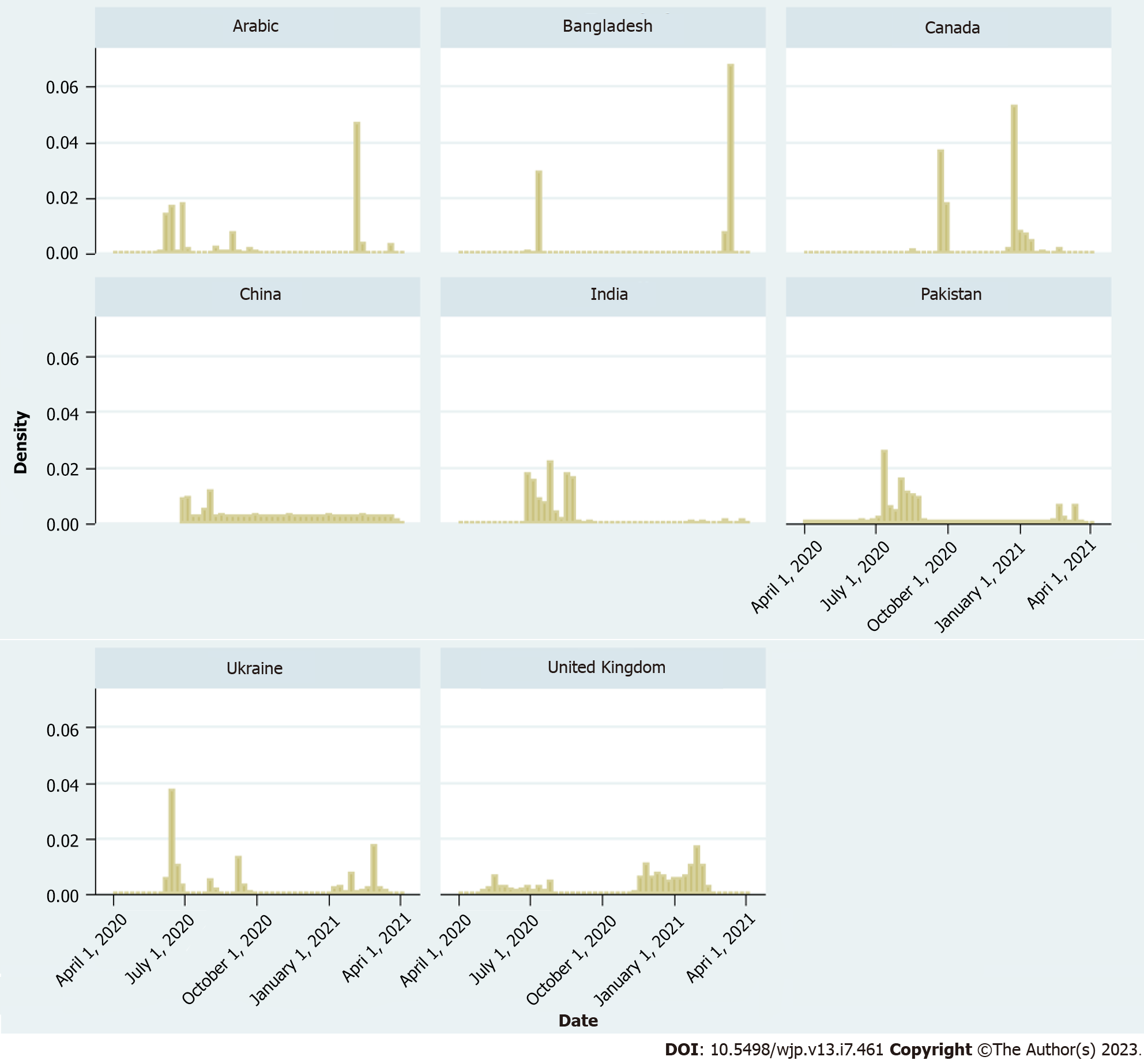
Figure 1 shows a histogram of day/time by country. Two long bars in Bangladesh indicate that survey responses in both rounds were received during short windows, although the survey was open for three months each time in each site. The same pattern is seen in Canada and Hong Kong. Survey periods in Arabic speaking sites and Ukraine seem longer but scattered, meaning that for several days, survey data including mental health scores were not available during the three month period. India and Pakistan showed good density for moderately wider periods in round 1. United Kingdom showed the longest periods of survey responses in both rounds, which indicates that survey data including mental health scores were available for relatively more days in United Kingdom despite the fact that the survey was available for the same number of months at each site.
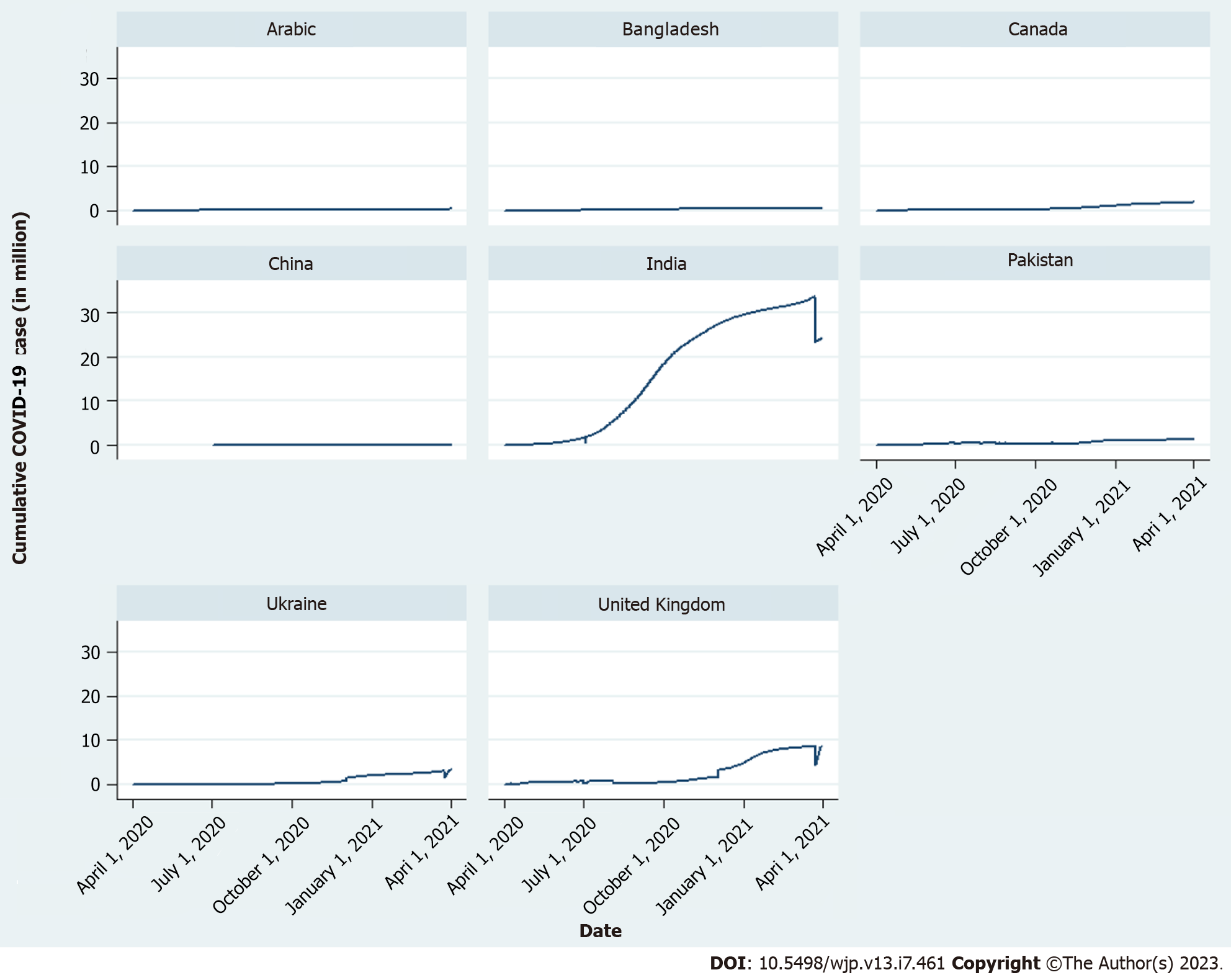
Daily cumulative COVID-19 cases (in million) have been plotted for each country, from April 1, 2020 to April 1, 2021 (Figure 2). As India had high COVID-19 cases, we have scaled down the COVID-19 cases by converting its unit into million, to raise the coefficients of cumulative COVID-19 case in regressions. United Kingdom also had high figures (reached nearly 10 million in March 2021). Ukraine and Canada reached relatively high figures. Other countries including Hong Kong had lower figures for cumulative COVID-19 cases. Therefore, the lines are relatively flat (near zero). Hong Kong had low figures at those periods as different countries had their spikes at different times. The figure shows downward movement of lines in India and United Kingdom, because COVID-19 cases were revised.
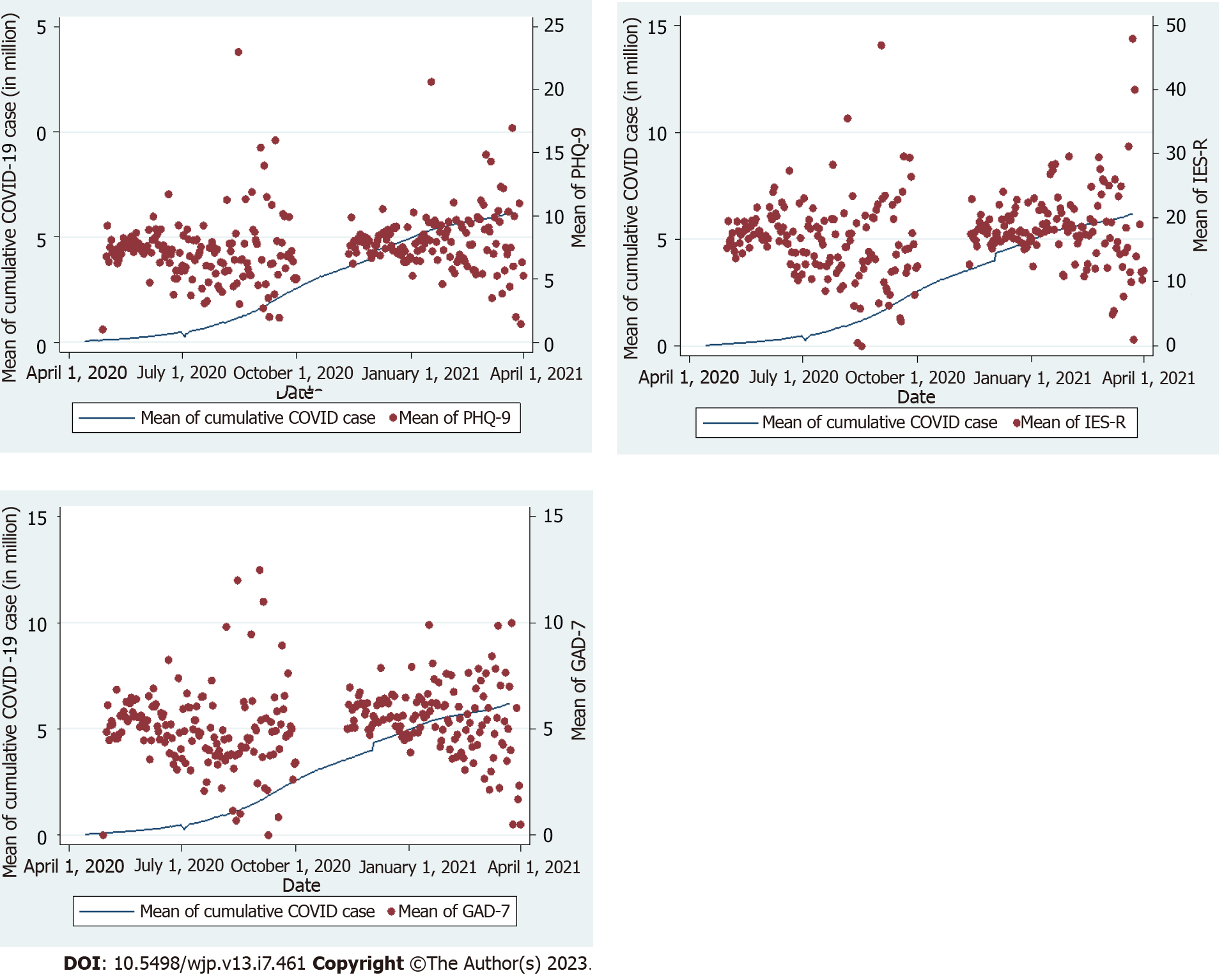
In survey data of the countries, scores of three mental health scales were available for several individuals in a day. They are reported as averages in a day. Country averages of those averages are taken to get single values in each day. Country average of cumulative COVID-19 cases are also taken. In Figure 3, scatter plots of average values of PHQ-9, GAD-7 and IES-R are shown in three different subplots. Average cumulative COVID-19 cases are plotted in line with three subplots. While left vertical axes measure the average cumulative COVID-19 cases, the right vertical axes measure three average values of mental health scores/indices. As mental health is an individual characteristic, average mental health scores fluctuated over time, and were not uniform like average cumulative COVID-19 cases. However, average mental health scores had less fluctuation/scatter at the beginning of each round (especially at the beginning of the second round). At that time, average mental health scores showed upward movement with average cumulative COVID-19 cases. In more scatter areas, such positive relation between average cumulative COVID-19 cases and average mental health scores is not seen. As less scatter zones showed a positive relation, we can expect an overall positive relation between them. To control for bias or contamination effect of lockdown, we added lockdown dummy, trend and their interaction following the specification in RDD.
Table 3 shows lockdown and survey periods of participant countries in the study. In each round, we have made normalized trend by subtracting lockdown easing/withdraw dates of countries (as lockdown start dates do not fall in survey periods) from trend. Zero is a common cut-off date; based on that we made a discontinuity dummy (1 = above cut-off, 0 = below cut-off), that captured negative effects of lockdown or withdraw on mental health. To capture different slopes on either side of the cut-off, we took interaction of normalized trends and the discontinuity dummy.
| Country | First lockdown | Second lockdown | Survey period | Can we capture lockdown effects? | |||
| Start | End | Start | End | Round 1 | Round 2 | ||
| Bangladesh | March 26, 2020 | May 16, 2020 | April 5, 2021 | July 14, 2021 | July 1, 2020-July 25, 2020 | January 19, 2021-March 18, 2021 | No |
| Canada | March 18, 2020 | May 18, 2020 | November 7, 2020 | January 8, 2021 | August 18, 2020-October 2, 2020 | December 21, 2020-March 30, 2021 | No |
| China | January 23, 2020 | April 8, 2020 | June 24, 2020-August 7, 2020 | No | |||
| India | March 25, 2020 | June 7, 2020 | April 19, 2021 | May 31, 2021 | July 1, 2020-September 20, 2020 | January 22, 2021-April 1, 2021 | No |
| Pakistan | March 24, 2020 | May 9, 2020 | May 8, 2021 | May 18, 2021 | June 10, 2020-September 24, 2020 | February 2, 2021-March 29, 2021 | No |
| Saudi Arabia | March 29, 2020 | June 21, 2020 | June 3, 2020-October 7, 2020 | January 16, 2021-April 1, 2021 | Yes, in round 1 | ||
| Ukraine | March 17, 2020 | April 24, 2020 | June 11, 2020-September 30, 2020 | January 7, 2021-March 25, 2021 | No | ||
| United Kingdom | March 23, 2020 | July 4, 2020 | November 5, 2020 | December 2, 2020 | April 28, 2020-August 6, 2020 | November 12, 2020-February 18, 2021 | Yes, in both rounds |
Table 4 shows regression results for round 1 and Table 5 for round 2. Both tables show two regression results for each mental health score/index, the dependent variable. The first one does not include RDD specification, while the second one does. When RDD specification is included, the results are for United Kingdom only.
| PHQ-9 | GAD-7 | IES-R | ||||
| Round 1 | Round 2 | Round 1 | Round 2 | Round 1 | Round 2 | |
| Daily cumulative COVID-19 case/1000000 | 0.075a | 2.121c | 0.041 | 1.750c | 0.225a | 1.543a |
| [-0.01, 0.16] | [1.58, 2.66] | [-0.03, 0.11] | [1.28, 2.22] | [-0.02, 0.47] | [-0.05, 3.14] | |
| Dummy for first lockdown withdraw | -0.658c | -0.450c | -1.224b | |||
| [-0.97, -0.34] | [-0.73, -0.17] | [-2.16, -0.29] | ||||
| Dummy for first lockdown withdraw1(date-first lockdown withdraw date) | -0.018c | -0.014c | -0.043c | |||
| [-0.03, -0.01] | [-0.02, -0.01] | [-0.07, -0.02] | ||||
| Date-first lockdown withdraw date | 0.006b | 0.000 | 0.004 | |||
| [0.00, 0.01] | [-0.00, 0.01] | [-0.01, 0.02] | ||||
| Healthcare professional (1 = yes, 0 = no) | -0.402c | -0.737c | -0.328c | -0.631c | -1.394c | -2.185c |
| [-0.54, -0.26] | [-0.89, -0.58] | [-0.45, -0.21] | [-0.77, -0.49] | [-1.81, -0.98] | [-2.65, -1.72] | |
| Age (base: Below 25) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| 25-44 | -1.084c | -1.428c | -0.482c | -0.713c | -2.350c | -2.091c |
| [-1.34, -0.83] | [-1.75, -1.11] | [-0.71, -0.26] | [-0.99, -0.43] | [-3.10, -1.60] | [-3.02, -1.16] | |
| 45-54 | -1.958c | -2.345c | -1.456c | -1.737c | -3.992c | -3.366c |
| [-2.24, -1.68] | [-2.69, -1.99] | [-1.70, -1.21] | [-2.05, -1.43] | [-4.83, -3.15] | [-4.39, -2.34] | |
| 55 and over | -2.956c | -3.108c | -2.179c | -2.284c | -5.568c | -4.085c |
| [-3.24, -2.67] | [-3.47, -2.75] | [-2.43, -1.93] | [-2.60, -1.97] | [-6.42, -4.72] | [-5.15, -3.02] | |
| White (1 = yes, 0 = no) | 0.360c | 0.482c | 0.299c | 0.413c | -1.120c | -0.054 |
| [0.17, 0.55] | [0.23, 0.74] | [0.13, 0.47] | [0.19, 0.64] | [-1.69, -0.55] | [-0.80, 0.69] | |
| Christian (1 = yes, 0 = no) | -0.206c | -0.036 | 0.018 | 0.222c | 0.522c | 0.829c |
| [-0.34, -0.07] | [-0.19, 0.12] | [-0.10, 0.13] | [0.08, 0.36] | [0.13, 0.91] | [0.37, 1.29] | |
| Male (1 = yes, 0 = no) | -1.189c | -1.231c | -1.039c | -1.042c | -2.997c | -3.719c |
| [-1.34, -1.03] | [-1.43, -1.03] | [-1.18, -0.90] | [-1.22, -0.86] | [-3.46, -2.53] | [-4.31, -3.13] | |
| Attended university (1 = yes, 0 = no) | -1.141c | 0.000 | -0.545c | 0.000 | -1.254c | 0.000 |
| [-1.34, -0.94] | [0.00, 0.00] | [-0.72, -0.37] | [0.00, 0.00] | [-1.85, -0.65] | [0.00, 0.00] | |
| Living at own home (1 = yes, 0 = no) | -0.885c | -1.105c | -0.489c | -0.692c | -1.432c | -2.270c |
| [-1.04, -0.73] | [-1.30, -0.91] | [-0.63, -0.35] | [-0.86, -0.52] | [-1.89, -0.97] | [-2.83, -1.71] | |
| Vulnerable according to government category (base: Not vulnerable) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Aged 70 or above | -0.898c | -1.105c | -0.764c | -0.985c | -1.954c | -2.909c |
| [-1.18, -0.62] | [-1.52, -0.69] | [-1.01, -0.52] | [-1.35, -0.62] | [-2.81, -1.10] | [-4.19, -1.63] | |
| Chronic disease | 0.361b | 0.345b | 0.533c | 0.543c | 1.245c | 1.644c |
| [0.08, 0.64] | [0.03, 0.66] | [0.29, 0.78] | [0.26, 0.83] | [0.41, 2.08] | [0.70, 2.59] | |
| Diabetes | 0.034 | -0.064 | 0.102 | 0.139 | 0.867 | 1.185 |
| [-0.43, 0.49] | [-0.63, 0.50] | [-0.30, 0.50] | [-0.36, 0.64] | [-0.50, 2.23] | [-0.49, 2.86] | |
| Other | 0.915c | 0.846c | 0.390c | 0.355b | 0.811a | 1.208b |
| [0.62, 1.21] | [0.49, 1.20] | [0.13, 0.65] | [0.04, 0.67] | [-0.07, 1.70] | [0.15, 2.27] | |
| Vulnerable according to government category and require shielding (1 = yes, 0 = no) | 1.087c | 1.096c | 0.909c | 0.945c | 4.281c | 3.513c |
| [0.83, 1.34] | [0.76, 1.43] | [0.68, 1.13] | [0.65, 1.24] | [3.51, 5.05] | [2.52, 4.50] | |
| Experienced coronavirus (1 = yes, 0 = no) | 0.324c | 0.220b | 0.237c | 0.181b | 0.410a | 0.547b |
| [0.18, 0.47] | [0.05, 0.39] | [0.11, 0.36] | [0.03, 0.33] | [-0.01, 0.83] | [0.05, 1.05] | |
| Pre-existing mental health condition (1 = yes, 0 = no) | 3.447c | 3.256c | 3.158c | 3.091c | 8.608c | 8.227c |
| [3.26, 3.63] | [3.04, 3.47] | [3.00, 3.32] | [2.90, 3.28] | [8.06, 9.16] | [7.60, 8.86] | |
| Drinking alcohol (1 = yes, 0 = no) | 0.251c | -0.082 | 0.234c | -0.101 | 0.410 | -0.277 |
| [0.08, 0.42] | [-0.30, 0.13] | [0.08, 0.38] | [-0.29, 0.09] | [-0.10, 0.92] | [-0.91, 0.36] | |
| Taking drug (1 = yes, 0 = no) | 0.794c | 1.303c | 0.725c | 0.729c | 2.262c | 2.527c |
| [0.48, 1.11] | [0.76, 1.84] | [0.45, 1.00] | [0.25, 1.21] | [1.33, 3.19] | [0.95, 4.11] | |
| Ever experienced suicidal thoughts (1 = yes, 0 = no) | 3.101c | 2.976c | 1.623c | 1.503c | 6.054c | 5.812c |
| [2.95, 3.25] | [2.80, 3.15] | [1.49, 1.75] | [1.35, 1.66] | [5.61, 6.50] | [5.30, 6.32] | |
| Mental health support from (base: No support) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
| Health service provider | 0.134 | 0.245a | -0.052 | -0.021 | 0.008 | -0.030 |
| [-0.11, 0.37] | [-0.03, 0.52] | [-0.26, 0.16] | [-0.26, 0.22] | [-0.71, 0.72] | [-0.85, 0.79] | |
| Other | 1.072c | 1.269c | 0.521c | 0.666c | 3.042c | 3.542c |
| [0.77, 1.38] | [0.91, 1.63] | [0.25, 0.79] | [0.35, 0.98] | [2.14, 3.95] | [2.49, 4.59] | |
| Constant | 7.050c | 7.213c | 4.651c | 4.590c | 16.577c | 16.791c |
| [6.73, 7.37] | [6.69, 7.73] | [4.37, 4.93] | [4.13, 5.05] | [15.62, 17.54] | [15.26, 18.32] | |
| Observations | 28560 | 21077 | 28710 | 21202 | 26913 | 19785 |
| Adjusted R2 | 0.279 | 0.261 | 0.214 | 0.203 | 0.180 | 0.172 |
| PHQ-9 | GAD-7 | IES-R | ||||
| Round 1 | Round 2 | Round 1 | Round 2 | Round 1 | Round 2 | |
| Daily cumulative COVID-19 case/1000000 | 0.195c | 0.433c | 0.129c | 0.557c | 0.454c | 1.265c |
| [0.18, 0.21] | [0.23, 0.63] | [0.11, 0.15] | [0.38, 0.74] | [0.40, 0.51] | [0.67, 1.86] | |
| Dummy for second lockdown withdraw | -0.507c | -0.343b | -1.077b | |||
| [-0.83, -0.18] | [-0.63, -0.05] | [-2.04, -0.11] | ||||
| Dummy for second lockdown withdraw1(date-second lockdown withdraw date) | -0.034c | -0.038c | -0.104c | |||
| [-0.06, -0.01] | [-0.06, -0.02] | [-0.18, -0.03] | ||||
| Date-second lockdown withdraw date | 0.013 | -0.002 | 0.034 | |||
| [-0.01, 0.03] | [-0.02, 0.02] | [-0.03, 0.10] | ||||
| Healthcare professional (1 = yes, 0 = no) | -0.693c | -0.747c | -0.540c | -0.587c | -2.325c | -2.551c |
| [-0.80, -0.58] | [-0.86, -0.63] | [-0.64, -0.44] | [-0.69, -0.48] | [-2.65, -2.00] | [-2.89, -2.21] | |
| Age (base: Below 25) | ||||||
| 25-44 | -1.147c | -1.339c | -0.333c | -0.445c | -1.043c | -0.715b |
| [-1.34, -0.96] | [-1.55, -1.13] | [-0.50, -0.16] | [-0.63, -0.26] | [-1.60, -0.49] | [-1.33, -0.10] | |
| 45-54 | -2.059c | -2.245c | -1.310c | -1.421c | -2.263c | -1.750c |
| [-2.27, -1.85] | [-2.47, -2.02] | [-1.50, -1.12] | [-1.63, -1.22] | [-2.88, -1.65] | [-2.42, -1.08] | |
| 55 and over | -3.455c | -3.639c | -2.424c | -2.521c | -4.792c | -4.223c |
| [-3.66, -3.25] | [-3.87, -3.41] | [-2.61, -2.24] | [-2.72, -2.32] | [-5.40, -4.18] | [-4.89, -3.55] | |
| White (1 = yes, 0 = no) | -0.291c | -0.243c | -0.326c | -0.249c | -2.114c | -1.667c |
| [-0.42, -0.16] | [-0.38, -0.11] | [-0.44, -0.21] | [-0.37, -0.13] | [-2.49, -1.74] | [-2.07, -1.27] | |
| Christian (1 = yes, 0 = no) | -0.017 | 0.018 | 0.174c | 0.183c | 0.752c | 0.795c |
| [-0.11, 0.08] | [-0.08, 0.12] | [0.09, 0.26] | [0.10, 0.27] | [0.47, 1.03] | [0.50, 1.09] | |
| Male (1 = yes, 0 = no) | -1.470c | -1.476c | -1.491c | -1.523c | -4.418c | -4.798c |
| [-1.57, -1.37] | [-1.58, -1.37] | [-1.58, -1.40] | [-1.62, -1.43] | [-4.72, -4.12] | [-5.12, -4.48] | |
| Attended university (1 = yes, 0 = no) | -0.699c | 0.000 | -0.543c | 0.000 | -0.174 | 0.000 |
| [-0.96, -0.43] | [0.00, 0.00] | [-0.78, -0.31] | [0.00, 0.00] | [-0.95, 0.60] | [0.00, 0.00] | |
| Own home (1 = yes, 0 = no) | -1.328c | -1.391c | -0.899c | -0.957c | -2.985c | -3.338c |
| [-1.44, -1.22] | [-1.51, -1.27] | [-1.00, -0.80] | [-1.06, -0.85] | [-3.32, -2.65] | [-3.69, -2.99] | |
| Vulnerable according to government category and require shielding (1 = yes, 0 = no) | 1.355c | 1.393c | 1.083c | 1.124c | 3.932c | 3.929c |
| [1.25, 1.46] | [1.28, 1.51] | [0.99, 1.18] | [1.02, 1.23] | [3.61, 4.26] | [3.59, 4.27] | |
| Experienced coronavirus (1 = yes, 0 = no) | 0.747c | 0.715c | 0.566c | 0.535c | 2.601c | 2.398c |
| [0.64, 0.85] | [0.61, 0.82] | [0.47, 0.66] | [0.44, 0.63] | [2.30, 2.91] | [2.08, 2.71] | |
| Pre-existing mental health condition (1 = yes, 0 = no) | 2.808c | 2.745c | 2.278c | 2.266c | 7.150c | 7.160c |
| [2.62, 2.99] | [2.55, 2.94] | [2.11, 2.44] | [2.10, 2.44] | [6.60, 7.70] | [6.60, 7.73] | |
| Drinking alcohol (1 = yes, 0 = no) | 2.300c | 2.506c | 1.714c | 1.875c | 5.976c | 6.400c |
| [2.17, 2.43] | [2.36, 2.65] | [1.60, 1.83] | [1.75, 2.00] | [5.59, 6.37] | [5.98, 6.82] | |
| Taking drug (1 = yes, 0 = no) | 1.232c | 1.359c | 0.539c | 0.562c | 3.126c | 3.270c |
| [1.01, 1.46] | [1.10, 1.62] | [0.34, 0.74] | [0.33, 0.79] | [2.46, 3.79] | [2.51, 4.03] | |
| Ever experienced suicidal thoughts (1 = yes, 0 = no) | 4.405c | 4.379c | 2.749c | 2.716c | 9.625c | 9.747c |
| [4.29, 4.52] | [4.26, 4.49] | [2.65, 2.85] | [2.61, 2.82] | [9.30, 9.95] | [9.41, 10.09] | |
| Mental health support from (base: No support) | ||||||
| Health service provider | 0.322c | 0.342c | -0.024 | -0.051 | -0.124 | -0.288 |
| [0.10, 0.55] | [0.11, 0.57] | [-0.22, 0.17] | [-0.26, 0.15] | [-0.79, 0.54] | [-0.97, 0.39] | |
| Other | 1.041c | 1.300c | 0.686c | 0.854c | 2.979c | 3.572c |
| [0.78, 1.31] | [1.02, 1.58] | [0.45, 0.92] | [0.61, 1.10] | [2.20, 3.76] | [2.75, 4.40] | |
| Constant | 8.201c | 8.292c | 6.023c | 5.496c | 17.577c | 16.168c |
| [7.98, 8.42] | [7.84, 8.74] | [5.83, 6.22] | [5.10, 5.90] | [16.94, 18.21] | [14.84, 17.50] | |
| Observations | 62938 | 57985 | 63545 | 58547 | 58966 | 54202 |
| Adjusted R2 | 0.315 | 0.318 | 0.228 | 0.230 | 0.222 | 0.228 |
In round 1, the cumulative COVID cases had statistically significant effect on all three mental health scores with RDD specification. For example, as United Kingdom had 7.70 average GAD-7, the increase size 1.75 in regression was nearly 23% (1.75 × 100/7.70). So, for a one million increase in cumulative daily COVID cases, GAD-7 increased by 23 percent.
In round 2 (Table 5), all three mental health indices increased statistically and significantly due to increase in cumulative COVID cases, with and without RDD specification. Without RDD specification, for a one million increase in cumulative COVID cases, the increase in PHQ-9 was 0.195 (2.38%), GAD-7 0.129 (2.14%), and IES-R 0.454 (2.37%). With RDD specification, for a one million increase in cumulative COVID cases, the increase in PHQ-9 was 0.433 (5.27%), GAD-7 0.577 (9.55%), and IES-R 1.265 (6.59%). Results with RDD specification implied that United Kingdom had higher effects than other countries.
In both regression tables, lockdown withdraw dummy in RDD specification showed that lockdown withdraw had statistical and significant effects on mental health indices, which supported the findings of our previous paper that showed that lockdown increased participants mental health scores, or worsened participant’s mental health[8].
In both regression tables, compared to the youngest age group (under 25), other age groups had lower scores on the mental health scales, meaning better mental health. Non-White participants reported better mental health than White participants, in most cases. Non-Christians reported better mental health than Christians in both rounds. In both rounds, higher educated participants had better mental health than the lowest educated group.
To demonstrate heterogeneous effects of cumulative COVID cases on mental health scores for different countries, we ran regressions without RDD specification for each country separately, but we included all characteristics used in previous regressions. RDD specification was only applicable to United Kingdom data.
For China (Hong Kong), cumulative COVID cases was extremely low, and therefore, the coefficients of daily cumulative COVID cases were extremely high. Similarly high and low coefficients in different countries depended on scales of cumulative COVID cases in the relevant countries.
Most countries did not show any significant effects. United Kingdom had very good distribution of survey respondents over a long period of time. Therefore, regression results for United Kingdom are more reliable than others. The results are statistically positive in both rounds in the United Kingdom. The first round in the United Kingdom showed statistically and significantly higher positive results. As we have seen in Table 4, such significance vanishes with the inclusion of RDD specification.
Using repeated cross sectional survey data of eight country groups and cumulative COVID-19 cases of same countries from Microsoft AZURE, this study found that the daily cumulative COVID-19 cases had a statistically significant effect on three mental health scale indices: Depression, anxiety, and trauma. Ordinary least squares regression results with RDD specification to control for lockdown effects confirms the results. The results are dominated by data in the United Kingdom, which has the largest number of respondents with wider distribution over time. The study findings imply that participants’ mental health worsened with high cumulative COVID-19 cases. Daily cases did not show any impact on mental health scores of participants. The study also highlights other important demographic information and differences due to impact of the COVID-19 pandemic on different countries’ participants.
These findings are understandable, considering the significant impact of COVID-19 pandemic on the lives of people across the globe and similar results from other data. Evidence from the Centre for Disease Control and Prevention has shown that fear and stress related to the COVID-19 has led to symptomatology, including change in sleep and eating patterns, worsening of premorbid psychiatric conditions, and increased use of substances (e.g., alcohol, tobacco, drugs), which add to the mental health burden[21]. Quadros et al[22] conducted a scoping review and concluded that females, younger adults, urban residents, divorcees, healthcare workers, those in quarantine settings, those in suspicion of being infected, and those with mental health problems, were found to be at an increased risk of COVID-19-related fear[22].
High cumulative COVID-19 cases not only presented a fear of infection and mortality, especially in vulnerable groups, but also impacted on education, jobs, ability to socialize, relationships, loneliness, and other socio-cultural and socioeconomic variables. Most studies have shown an impact on young people’s mental health as does this study and the same study in United Kingdom participants has shown an increase in suicidal thoughts[23,24]. High cumulative cases additionally meant the implementation of public health interventions and lockdowns restricting activities. Our findings from the United Kingdom data of the same study demonstrate the positive association of lockdown relaxation and face covering policies on the mental health of participants evidencing the impact of these interventions on mental health of populations as also demonstrated by the international data in this study[9].
These results add to existing global evidence of the psychological impact of the COVID-19 pandemic and previous studies that have demonstrated the adverse impact of population shocks on population mental health[25-27]. A systematic review of data published between January 2020 to January 2021 during the COVID-19 pandemic found that daily SARS-CoV-2 infection rates and reductions in human mobility were associated with increased prevalence of major depressive disorder[28]. These findings have been confirmed by the WHO[3].
In our study, participants from Hong Kong, India and Ukraine had lower mental health scores than other countries’ participants. It is not possible to make conclusions on these findings as the number of participants were small and there would be an element of time of participation in the survey.
Different countries had their case number surges and lockdowns at different times during the pandemic. Similarly different countries followed a different trajectory depending on their populations, readiness to respond, political, cultural, financial, and technical landscape. As an example, Ukraine underwent change in ministers three times during the pandemic. There were other determinants of response to the pandemic including levels of awareness, stigma, fear in the early phases of pandemic and attributions to the illness based on cultural explanations[11].
Since the COVID-19 pandemic, the need for mental health support services has increased significantly[29]. This has been particularly difficult due to isolation and distancing measures, causing a physical barrier to help-seeking and treatment implementation[29,30]. Mental health rehabilitation interventions aim to increase social skills and teach coping strategies through training and increased social interactions[29]. This can help individuals with various mental health conditions but is especially useful for those with anxiety or depression[30]. Social and peer support is an integral part of mental health rehabilitation, yet the isolating protection measures of the COVID-19 pandemic pose a barrier[30].
Measures, such as regular testing or online programmes, are some actions which help to overcome these unprecedented circumstances[30,31]. Many organisations and facilities moved their services online in order to provide continuous psychological support for their clients[30,31]. This will ensure that services can continue to operate whilst controlling the spread of the pandemic[31]. The United Kingdom government has published a COVID-19 Mental Health and Wellbeing Recovery Action Plan to accommodate for mental health interventions throughout and post-pandemic[32]. The plan outlines various measures including support for young people, assistance within the employment sector, and accessible and widely available support for frontline healthcare workers[32]. Whilst mental health has always been a pressing matter, the pandemic has amplified its prevalence and affects across all demographic groups[32]. As there were rigid isolation regulations in place, this made the imple
The results of this study should be interpreted considering its limitations. The timing of the study was such that most countries were in different phases of the pandemic. To conduct a study in that unusual environment meant that some may not consider this a cross sectional study in the epidemiological sense, and it could be difficult to judge the true population prevalence and make international comparisons. For this reason, we have explained the landscape of the different countries separately. This limitation could not have been avoided given the unpredictable nature of the spread of virus, even if confined parameters had been used. Additionally, where many cultural adaptations were made to account for the differences in the countries, it may still be difficult to draw conclusions about the differences in these populations which might be attributable to COVID as the measures are all taken after the onset of the pandemic. Another limitation concerning cumulative cases is that in many low and middle income countries, public health infrastructures and disease notification are very different to those used in high income countries, meaning that the potential for under-ascertainment of cases is much higher. The study has a high number of missing cases and non-random selection of participants are further limitations. In some participating centres the numbers are small. Many surveys were in circulation during this time in all the participating countries, especially during the second round, which may have affected the participation in the survey. Most studies of similar kind have reported small numbers.
The results from the current study add to developing evidence of the psychological impact of COVID-19, especially daily cumulative cases on three mental health indices. Building a database of evidence will allow for future planning of pandemics, particularly the impact on mental health of populations and the cultural differences.
The coronavirus disease 2019 (COVID-19) pandemic had a huge effect on mental health across the globe. As the pandemic developed over time, international rates of mental health conditions increased. It would be insightful to explore how the increasing cases of COVID-19 impacted mental health throughout the pandemic.
Exploring the impacts of COVID-19 on mental health with help construct a better understanding of the current mental health situation across the globe. It will also help to inform pandemic preparedness policies around mental health services.
This study aimed to explore the psychological implications of the increasing COVID-19 case throughout the pandemic across various countries.
A repeated, cross-sectional online international survey of adults was carried out in 10 countries. Five standardised psychological measures were included to explore the psychological impact of cumulative COVID-19 cases. This was carried out at two timepoints in all countries, aside from the United Kingdom which collected data at 3 timepoints.
There were two rounds of the online survey in eight country groups with 42866 participants recruited in Round 1 and 92260 recruited in Round 2. This study found that the daily cumulative COVID-19 cases had a statistically significant effect on three depression, anxiety, and trauma. Trauma scores were higher across all countries compared to those for anxiety and depression. All scores increased in Round 2 in all countries.
Considering the significant impact of COVID-19, understanding the effects will enable for adequate services and support to be put in place. This evidence dataset will also help inform the policies and strategies for pandemic preparedness.
COVID-19 has had enduring effects in all aspects of life including physical and mental health.
We would like to thank all the participants who gave their time to complete the survey. We also thank our collaborators–NHS and non-NHS organisations that disseminated the survey. We would specially like to thank Sana Sajid, for administrative support.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Nursing and Midwifery Council (NMC), No. 98I1393.
Specialty type: Psychiatry
Country/Territory of origin: United Kingdom
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen JK, China; Rahmati M, Iran; Stoyanov D, Bulgaria S-Editor: Fan JR L-Editor: A P-Editor: Liu JH
| 1. | GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11327] [Cited by in RCA: 9637] [Article Influence: 1927.4] [Reference Citation Analysis (35)] |
| 2. | World Health Organization. WHO Director-General's statement on IHR emergency committee on novel coronavirus (2019-nCoV). 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov). |
| 3. | World Health Organization. Mental Health and COVID-19: Early evidence of the pandemic’s impact: Scientific brief. In (pp. 1-13): 2020. Mental Health and COVID-19: Early evidence of the pandemic’s impact: Scientific brief, 2 March 2022. Available from: https://www.who.int/. |
| 4. | Memish ZA, Ahmed QA, Schlagenhauf P, Doumbia S, Khan A. No time for dilemma: mass gatherings must be suspended. Lancet. 2020;395:1191-1192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 5. | Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. 2008;136:997-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 531] [Cited by in RCA: 514] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 6. | Phiri P, Ramakrishnan R, Rathod S, Elliot K, Thayanandan T, Sandle N, Haque N, Chau SW, Wong OW, Chan SS, Wong EK, Raymont V, Au-Yeung SK, Kingdon D, Delanerolle G. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: A systematic review and meta-analysis. EClinicalMedicine. 2021;34:100806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 71] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 7. | United Nations. Policy Brief: The Impact of COVID-19 on Women. In Prevention, C. f. D. C. a. 2022. Coping with Stress. Policy Brief: The Impact of COVID-19 on Women-World. Available from: https://reliefweb.int/. |
| 8. | Raveendran AV, Jayadevan R, Sashidharan S. Long COVID: An overview. Diabetes Metab Syndr. 2021;15:869-875. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 427] [Cited by in RCA: 540] [Article Influence: 135.0] [Reference Citation Analysis (0)] |
| 9. | Rathod S, Pallikadavath S, Graves E, Rahman MM, Brooks A, Soomro MG, Rathod P, Phiri P. Impact of lockdown relaxation and implementation of the face-covering policy on mental health: A United Kingdom COVID-19 study. World J Psychiatry. 2021;11:1346-1365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 10. | Shanbehzadeh S, Tavahomi M, Zanjari N, Ebrahimi-Takamjani I, Amiri-Arimi S. Physical and mental health complications post-COVID-19: Scoping review. J Psychosom Res. 2021;147:110525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 176] [Article Influence: 44.0] [Reference Citation Analysis (0)] |
| 11. | Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020;89:531-542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2189] [Cited by in RCA: 1892] [Article Influence: 378.4] [Reference Citation Analysis (0)] |
| 12. | Houben-Wilke S, Goërtz YM, Delbressine JM, Vaes AW, Meys R, Machado FV, van Herck M, Burtin C, Posthuma R, Franssen FM, Vijlbrief H, Spies Y, van 't Hul AJ, Spruit MA, Janssen DJ. The Impact of Long COVID-19 on Mental Health: Observational 6-Month Follow-Up Study. JMIR Ment Health. 2022;9:e33704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 83] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 13. | Rathod S, Pallikadavath S, Young AH, Graves L, Rahman MM, Brooks A, Soomro M, Rathod P, Phiri P. Psychological impact of COVID-19 pandemic: Protocol and results of first three weeks from an international cross-section survey - focus on health professionals. J Affect Disord Rep. 2020;1:100005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Rathod S. Impact of culture on response to COVID-19. Br Med J. 2022;369:1556.. [RCA] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 15. | Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. SLACK. 2002;32:509-515. |
| 16. | Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21545] [Cited by in RCA: 28616] [Article Influence: 1192.3] [Reference Citation Analysis (0)] |
| 17. | Weiss DS, Marmar CR. The Impact of Event Scale—Revised. In J. P. Wilson & T. M. Keane (Eds.), Assessing psychological trauma and PTSD. The Guilford Press, 1997: 399–411. Available from: https://psycnet.apa.org/record/1997-97162-013. |
| 18. | Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res Aging. 2004;26:655-672. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3310] [Cited by in RCA: 2651] [Article Influence: 126.2] [Reference Citation Analysis (0)] |
| 19. | Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52:30-41. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5738] [Cited by in RCA: 5699] [Article Influence: 154.0] [Reference Citation Analysis (0)] |
| 20. | Microsoft. COVID Tracking Project. 2022. Available from https://Learn.microsoft.com/en-us/azure/open-datasets/dataset-covid-tracking?tabs=azure-storage. |
| 21. | Centre for Disease Control and Prevention. Coping with Stress 2022. Available from: https://www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/index.html. |
| 22. | Quadros S, Garg S, Ranjan R, Vijayasarathi G, Mamun MA. Fear of COVID 19 Infection Across Different Cohorts: A Scoping Review. Front Psychiatry. 2021;12:708430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 102] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 23. | Aknin LB, De Neve JE, Dunn EW, Fancourt DE, Goldberg E, Helliwell JF, Jones SP, Karam E, Layard R, Lyubomirsky S, Rzepa A, Saxena S, Thornton EM, VanderWeele TJ, Whillans AV, Zaki J, Karadag O, Ben Amor Y. Mental Health During the First Year of the COVID-19 Pandemic: A Review and Recommendations for Moving Forward. Perspect Psychol Sci. 2022;17:915-936. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 209] [Article Influence: 69.7] [Reference Citation Analysis (0)] |
| 24. | Rathod S, Phiri P, Pallikadavath S, Graves E, Brooks A, Rathod P, Lin S. The Psychological Impact of COVID-19 Pandemic on Suicidal Thoughts in the United Kingdom. BJPsych Open. 2022;8(S1):S69-S69. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 25. | Economou M, Madianos M, Peppou LE, Patelakis A, Stefanis CN. Major depression in the era of economic crisis: a replication of a cross-sectional study across Greece. J Affect Disord. 2013;145:308-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 180] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 26. | Lee S, Guo WJ, Tsang A, Mak AD, Wu J, Ng KL, Kwok K. Evidence for the 2008 economic crisis exacerbating depression in Hong Kong. J Affect Disord. 2010;126:125-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 78] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 27. | Madianos M, Economou M, Alexiou T, Stefanis C. Depression and economic hardship across Greece in 2008 and 2009: two cross-sectional surveys nationwide. Soc Psychiatry Psychiatr Epidemiol. 2011;46:943-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 88] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 28. | COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700-1712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2518] [Cited by in RCA: 2649] [Article Influence: 662.3] [Reference Citation Analysis (0)] |
| 29. | Chaturvedi SK. Covid-19, Coronavirus and Mental Health Rehabilitation at Times of Crisis. J Psychosoc Rehabil Ment Health. 2020;7:1-2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 30. | Aamir A, Awan S, de Filippis R, Diwan MN, Ullah I. Effect of COVID-19 on Mental Health Rehabilitation Centers. J Psychosoc Rehabil Ment Health. 2021;8:97-100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 31. | Pinals DA, Hepburn B, Parks J, Stephenson AH. The Behavioral Health System and Its Response to COVID-19: A Snapshot Perspective. Psychiatr Serv. 2020;71:1070-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 32. | H. M. Government. COVID-19 mental health and wellbeing recovery action plan. London: H M Government; 2021. COVID-19 mental health and wellbeing recovery action plan-GOV.UK. Available from: https://www.gov.uk/. |
| 33. | McDaid D. Viewpoint: Investing in strategies to support mental health recovery from the COVID-19 pandemic. Eur Psychiatry. 2021;64:e32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 49] [Article Influence: 12.3] [Reference Citation Analysis (0)] |