Published online Mar 19, 2023. doi: 10.5498/wjp.v13.i3.126
Peer-review started: October 12, 2022
First decision: October 30, 2022
Revised: November 17, 2022
Accepted: February 14, 2023
Article in press: February 14, 2023
Published online: March 19, 2023
Processing time: 156 Days and 9.4 Hours
Tardive sensory syndrome (TSS) is a subtype of tardive syndrome (TS), and its etiology is still uncertain. Lurasidone is an atypical antipsychotic that has high affinity for dopamine D2- and serotonergic 5HT2A- and 5-HT7-receptors.
A 52-year-old woman, previously diagnosed with schizophrenia, and with no history of movement disorders and no sensory paresthesia, had taken lurasidone, initiate dose 40 mg daily then up titration to 120 mg daily, since March 2021, and developed mandibular sensory (pain) paresthesia after 3 mo of administration. After switching from lurasidone to quetiapine, she reported obvious impr-ovement in her mandibular pain.
It is noteworthy that TSS is a rare subtype of TS, and lurasidone, an atypical antipsychotic, usually has a lower risk of causing TS. In light of the temporal relationship, it is therefore concluded that use of lurasidone might have caused TSS in this patient. We reported this rare case as a reminder that clinicians should adopt a cautious approach when prescribing atypical antipsychotics, so as to prevent TS.
Core Tip: Tardive sensory syndrome is a subtype of tardive syndrome (TS), and its etiology is still uncertain. Lurasidone is an atypical antipsychotic that has high affinity for dopamine D2- and serotonergic 5HT2A- and 5-HT7-receptors. We reported a 52-year-old woman with schizophrenia developed mandibular sensory (pain) paresthesia after 3 mo of administration of lurasidone. This case report reminds clinicians should adopt a cautious approach when prescribing atypical antipsychotics, so as to prevent TS.
- Citation: Lin MC, Chang YY, Lee Y, Wang LJ. Tardive sensory syndrome related to lurasidone: A case report. World J Psychiatry 2023; 13(3): 126-130
- URL: https://www.wjgnet.com/2220-3206/full/v13/i3/126.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i3.126
Tardive syndrome (TS) is an iatrogenic condition resulting from exposure to chronic dopamine receptor blocking agents (DRBA), and is a more expansive phenomenological spectrum that encompasses tardive dyskinesia (TD), tardive dystonia, tardive akathisia, tardive sensory syndrome (TSS), tardive parkinsonism, and tardive tics[1]. TS is a distressing adverse effect of medication that might impair patients’ quality of life and even increase the risk of suicide[2]. Lurasidone is an atypical antipsychotic that exerts its effects through high affinity for dopamine D2- and serotonergic 5HT2A- and 5-HT7-receptors[3]. To our knowledge, there is no report of TSS as a side effect of lurasidone in the literature. Here, we describe a patient with schizophrenia who had been treated with lurasidone for 3 mo, and later developed TSS.
A 52-year-old female developed mandibular sensory paresthesia and pain after 3 mo of lurasidone administration, without orofacial dyskinesia, hands tremor, limbs rigidity, bradykinesia, axial dystonia, retrocollis, torticollis, or blepharospasm.
A 52-year-old female had been diagnosed with schizophrenia since April 2001, and was treated with various antipsychotics, including risperidone 1 mg/d, amisulpride 200 mg/d, quetiapine 200 mg/d, ziprasidone 40 mg/d, and clozapine 125 mg/d, with a duration of a few months, respectively. The most long duration of main regimen was olanzapine 10-25 mg daily (June 2013-March 2021), which was fully effective, but was discontinued due to the adverse side effect of weight gain. Consequently, the main regimen was shifted to lurasidone, initiate dose 40 mg/d then up titration to 120 mg/d since March 2021. However, she developed mandibular sensory paresthesia and pain after 3 mo of lurasidone administration, without orofacial dyskinesia, hands tremor, limbs rigidity, bradykinesia, axial dystonia, retrocollis, torticollis, or blepharospasm.
A 52-year-old female with no history of medical disease, movement disorders or sensory paresthesia had been diagnosed with schizophrenia since April 2001.
The patient had no developmental delay, and had elementary school education level with poor academic performance. She had introverted personality as premorbid personality and poor interpersonal relationship. She could keep her occupational function as a cleaner since young adult until now. She got married at her 20’s and divorced at her 32’ while she was diagnosed of schizophrenia. The patient denied psychiatric family history.
We also consulted a dentist to rule out oral infection or other lesions. Both the aforementioned laboratory tests and dental consultation showed negative findings. Due to the defining features, TSS was suspected[4]. Severity was evaluated on the basis of an Extrapyramidal Symptom Rating Scale (ESRS) score of 18 points[5] before we changed antipsychotics to quetiapine monotherapy.
A series of laboratory tests including complete blood count, liver function, renal function, diabetes mellitus lipid profile, copper, ceruloplasmin, thyroid function, rheumatoid factor, antinuclear antibody, immunoglobulin (Ig)A, IgG, anti-2 glycoprotein 1Ab, anticardiolipin Ab IgG, anticardiolipin Ab IgM. Anti-ENA, a venereal disease research laboratory test, HBs antigen, hepatitis C virus antibody, cryoglobulin identification, a homocysteine test and brain computed tomography (CT), were performed to rule out a secondary organic etiology. We also consulted a dentist to rule out oral infection or other lesion. The aforementioned laboratory tests and dental consultation both showed negative findings.
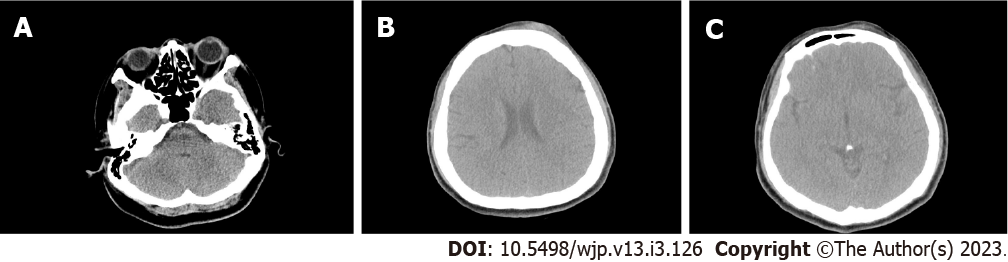
The brain CT image and report are demonstrated in Figure 1. Technique of examination: Axial brain CT with 5 mm section from vertex to skull base without contrast enhancement; normal ventricular size; normal appearance of cerebral fissures, cisterns & sulci; no evidence of intracranial hemorrhage; no midline deviation; no abnormal parenchymal attenuation change; no definite bony fracture; well pneumatization of bilateral mastoid cells; unremarkable of paranasal sinus; symmetrical and smooth contours of nasopharynx; and left frontal scalp swelling. There is no evidence of intracranial hemorrhage.
After lurasidone was switched to quetiapine 300 mg/d, the aforementioned sensory discomfort was significantly ameliorated, and remission was achieved.
After 1 mo, the ESRS scores improved by 65% (from 18 to 6); at the outpatient clinic follow-up, the visual analog scale scores for pain measurement decreased to 0/10 after 6 mo in remission.
TSS, manifested with unpleasant, burning or pain sensation in the oral or genital regions, is a chronic and specific type of TS. However, the pathophysiology of TSS remains uncertain[6]. D2 hypersensitivity alone seems to be insufficient to account for TS, or TSS. One theory has been proposed to elucidate the pathophysiology of TS; some atypical agents (clozapine and quetiapine in particular) have a relatively low affinity for D2 receptors that loosely bind to postsynaptic D2 receptors in the striatum then dissociate quickly, but some DRBAs act as binding tightly and have long-lasting effects on the receptors[7], which may explain why remission of TS is achieved after cross-shifting of lurasidone to quetiapine, as in our case. Another explanation for TS is that TS is attributed to defective adaptation of 5-HT2A, vesicular monoamine transporter type 2 levels, metabotropic and N-methyl-D-aspartatic acid receptors in the striatum, that as demonstrated in effect of antipsychotic drugs on nonhuman primates[7]. In addition, both pro- and antinociceptive effects of 5-HT2A receptor activation likely appear in other studies, but converging evidence underscores that peripheral 5 HT-2A receptors have an excitatory role in acute, sub-chronic and chronic pain transmission[8,9].
That then is another reasonable explanation why the remission of TS was achieved after cross-shifting of lurasidone to quetiapine in this case. A similar explanation may have been offered in a previous report of TSS related to trazodone which is a potent serotonin 5-HT2A and 5-HT2C receptors antagonist and a weak serotonin reuptake inhibitor that results in more dopamine release[10]. An alternative hypothesis, supported by human and animal neuropathological studies, indicates that TS is a neurodegenerative disorder involved in striatal interneurons damaged by oxidative stress. This theory assumes that dopaminergic receptor blockade may lead to elevated turnover rates of dopamine and free radical produced by monoamine oxidase[6]. Eleven cases of TSS associated with antipsychotic drugs have been reported, and each case suffered from profound pain distress that required treatment[11]. This symptomatic syndrome is chronic and affects predominantly older women, according to unmodifiable patient-related and disease-related risk factors for TD[12]. In general, for mild to moderate TS, it is recommended to reduce the dose of neuroleptics, switch to atypical medications, or discontinue antipsychotic treatment altogether in the hope of promoting remission[13]. Lurasidone, classified as a second-generation antipsychotic, has few adverse side effects pharmacologically related to TS. To date, a 4-patient study has indicated lurasidone as a potential cause of tardive dystonia and tardive akathisia[14]. That the TSS seen in our case was related to lurasidone can be indicated by the temporal relationship. Even though this temporal relationship suggests that our patient’s TSS was mainly related to the use of lurasidone, we could not rule out the effects of the previous use of other antipsychotics[13].
To our knowledge, this might be the first report to indicate that TSS occurred during lurasidone treatment. It is important that clinicians should adopt a cautious approach when prescribing atypical antipsychotics to prevent the development of TS, although these medications have a lower risk of causing TS.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Agrawal P, United States; Nardello R, Italy; Wang P, China; Yang L, China S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Frei K, Truong DD, Fahn S, Jankovic J, Hauser RA. The nosology of tardive syndromes. J Neurol Sci. 2018;389:10-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 52] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 2. | Caroff SN. Overcoming barriers to effective management of tardive dyskinesia. Neuropsychiatr Dis Treat. 2019;15:785-794. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 3. | European Medicines Agency. Assessment Report Latuda. [cited 15 September 2022]. Available from: https://www.readkong.com/page/assessment-report-latuda-european-medicines-agency-8849714. |
| 4. | Truong DD, Frei K. Setting the record straight: The nosology of tardive syndromes. Parkinsonism Relat Disord. 2019;59:146-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Chouinard G, Margolese HC. Manual for the Extrapyramidal Symptom Rating Scale (ESRS). Schizophr Res. 2005;76:247-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 307] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 6. | Mulroy E, Balint B, Bhatia KP. Tardive syndromes. Pract Neurol. 2020;20:368-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Factor SA. Management of Tardive Syndrome: Medications and Surgical Treatments. Neurotherapeutics. 2020;17:1694-1712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 8. | Rahman W, Bannister K, Bee LA, Dickenson AH. A pronociceptive role for the 5-HT2 receptor on spinal nociceptive transmission: an in vivo electrophysiological study in the rat. Brain Res. 2011;1382:29-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Courteix C, Dupuis A, Martin PY, Sion B. 5-HT2A receptors and pain. In: Guiard B, Di Giovanni G. 5-HT2A Receptors in the Central Nervous System. The Receptors. Cham: Humana Press, 2018. |
| 10. | Lin CC, Lin PY, Lee Y, Chang YY, Chen CH. Tardive dystonia and tardive sensory syndrome related to trazodone: a case report. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:1609-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Ford B, Greene P, Fahn S. Oral and genital tardive pain syndromes. Neurology. 1994;44:2115-2119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Montagna P, Pierangeli G, Avoni P, Cortelli P, Tinuper P, Lugaresi E. Tardive pain. Neurology. 1995;45:2113-2114. [PubMed] |
| 13. | Chen CY, Chiang HL, Fuh JL. Tardive syndrome: An update and mini-review from the perspective of phenomenology. J Chin Med Assoc. 2020;83:1059-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 14. | Tripathi R, Reich SG, Scorr L, Guardiani E, Factor SA. Lurasidone-Induced Tardive Syndrome. Mov Disord Clin Pract. 2019;6:601-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |