Published online Nov 19, 2023. doi: 10.5498/wjp.v13.i11.919
Peer-review started: September 5, 2023
First decision: September 14, 2023
Revised: September 20, 2023
Accepted: October 11, 2023
Article in press: October 11, 2023
Published online: November 19, 2023
Processing time: 73 Days and 1 Hours
An acute myocardial infarction (AMI) is often treated with direct coronary intervention and requires home-based rehabilitation. Caregivers of patients with AMI need adequate social support to maintain high-quality care; however, their social support function is low, and relevant indicators for intervention must be identified.
To analyze the correlation between social support for primary caregivers, their anxiety, and depression, when caring for patients with AMI after interventional therapy.
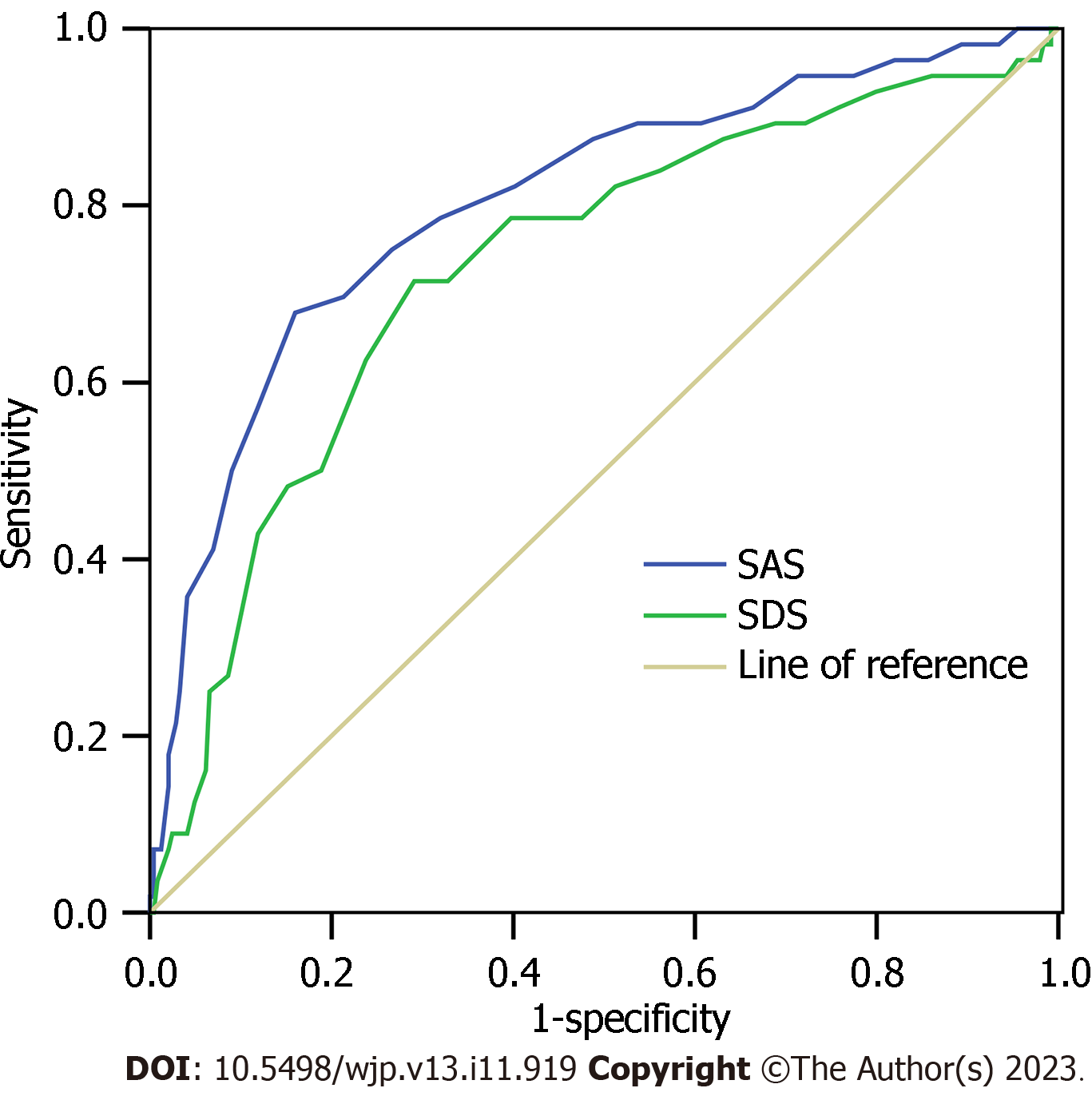
Using convenience sampling, we selected 300 primary caregivers of patients with AMI who had undergone interventional therapy. The Social Support Rating Scale (SSRS), Self-Rating Anxiety Scale (SAS), and Self-Rating Depression Scale (SDS) were used to assess the primary caregivers. A Pearson’s correlation analysis was used to analyze the correlations between the SSRS, SAS, and SDS, and a multiple logistic regression analysis was used to analyze the factors influencing the low social support function of primary caregivers. The receiver operating characteristic curve and area under the curve (AUC) were used to evaluate the pre-dictive ability of the SAS and SDS for low social support function in primary caregivers.
Considering the norm among Chinese people, AMI caregivers’ objective support, subjective support, support utilization, and SSRS scores were lower, while their SAS and SDS scores were higher. The SSRS scores of female caregivers were higher than those of the male caregivers (t = 2.123, P = 0.035). The Pearson correlation analysis showed that objective support, subjective support, support utilization, and SSRS total scores were significantly correlated with both SAS (r = -0.414, -0.460, -0.416, -0.535) and SDS scores (r = -0.463, -0.379, -0.349, -0.472). Among the 300 AMI caregivers, 56 cases (18.67%) had a low level of support function (SSRS ≤ 22 points). Logistic regression model analysis showed that SAS and SDS were independent risk factors for low social support function of AMI caregivers, regardless of adjustment for other variables (P < 0.05). SAS and SDS predicted that the AUC of AMI caregivers with low support function was 0.84, sensitivity was 67.9 and 71.4, and specificity was 84.0 and 70.9, respectively.
The social support function of the primary caregiver of patients with AMI after interventional therapy was lower and negatively correlated with anxiety and depression in the primary caregiver.
Core Tip: High levels of social support help caregivers implement care. Intervention in the social support function of the primary caregiver is beneficial for the postoperative recovery of patients with acute myocardial infarction (AMI) after interventional therapy. To find a new intervention direction, we proposed a relationship between the social support function of primary caregivers of patients with AMI, and anxiety and depression; this is a breakthrough in improving the social support function of primary caregivers.
- Citation: Bao J, Wang XY, Chen CH, Zou LT. Relationship between primary caregivers’ social support function, anxiety, and depression after interventional therapy for acute myocardial infarction patients. World J Psychiatry 2023; 13(11): 919-928
- URL: https://www.wjgnet.com/2220-3206/full/v13/i11/919.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i11.919
Acute myocardial infarction (AMI) is myocardial necrosis caused by acute or persistent ischemia and hypoxia in the coronary arteries. It is typically characterized by persistent chest pain[1]. Usually, after rest and use of nitrates, patients do not receive complete relief but experience arrhythmia, shock, or heart failure, resulting in loss of daily living ability and serious mental and behavioral disorders. According to relevant surveys and research data, the incidence of AMI in China has increased sharply in recent years, with the average annual number of new cases exceeding 500000[2]. Acute ST-elevation myocardial infarction (STEMI) within 12 h is usually treated with direct coronary intervention[3]. Postoperatively, most patients require home-based rehabilitation and caregiver care. During rehabilitation, the physical and mental state of the caregiver affects the prognosis and degree of recovery of the patient. The patient’s condition also affects the physical and psychological states, as well as the quality of the caregiver’s life, thus affecting their ability and quality of care[4]. Caregivers experience physical and emotional stress during the long-term care process. As a relative of the patient, the caregiver experiences heavy emotional stress and shoulders financial pressure. Studies have found that if caregivers receive sufficient social support, they can maintain their physical and mental health better and adapt to their caregiving role[5]. Ensuring a high social support function for caregivers has a positive clinical significance for patients’ rehabilitation. However, there is a lack of effective intervention strategies to improve caregivers’ social support, and more clinical evidence is needed to support the factors related to social support. Research has found that caregivers of patients with AMI often have different negative emotional levels of anxiety and depression[6,7]. Therefore, we propose that the social support function of caregivers of patients with AMI may be related to anxiety and depression. Based on this, we selected 300 primary caregivers of patients undergoing interventional treatment for AMI.
Considering the above, this study aims to investigate the levels of social support, anxiety, and depression among caregivers of AMI patients, and analyze the correlation between the social support function of main caregivers and their anxiety and depression after interventional therapy, to provide a reference for improving the quality of home care.
Using convenience sampling, we selected 300 primary caregivers of patients with AMI who received concurrent interventional treatment at the Affiliated Hospital of Jiangnan University, between January 2021 and December 2022.
Patients needed to comply with the following conditions: (1) Show AMI symptoms and evidence of myocardial ischemia[8]; (2) Be diagnosed with acute STEMI within 12 h and treated with coronary intervention; and (3) Be 18 years or older. The caregiver was required to meet the following conditions: (1) Be at least 18 years of age; (2) Be the patient’s immediate family member and has been caring for the patient for the longest time (i.e., is the patient's primary caregiver); (3) Have normal reading and writing ability and be able to complete the questionnaire independently; and (4) Be aware of this research and voluntarily agree to be investigated. The caregiver could not have the following conditions: (1) Mental abnormalities or intellectual disabilities; (2) Language expression and communication barriers; (3) A history of alcohol or drug dependence; or (4) Be a paid caregiver.
General information questionnaire. Based on a literature review and expert consultation, a general information questionnaire was prepared, which included age, gender, number of hospitalizations, payment method of medical expenses, proportion of out-of-pocket medical expenses to family income, course of the disease, heart function, and daily living ability. Caregivers’ general information included age, gender, education level, marital status, relationship with patients, monthly family income, caretaking experience, number of other caregivers, etc., as well as the age of patients, time from onset to admission, and Killip grade.
The Social Support Rating Scale (SSRS)[9] was created by domestic scholar Xiao Shui-Yuan in 1986, to assess the status of people’s social support, including subjective support, objective support, and support utilization. The scale comprises three dimensions and ten items, with the total score being the sum of the scores for each item. Higher scores indicate higher levels of social support. The total score is 66 points, of which ≤ 22 points are rated as low level, 23–44 points as medium, and 45–66 points as high. The retest reliability is 0.92, and the reliability and validity of all items are high (Cronbach’s α coefficient was 0.89–0.94). The SSRS Chinese norm refers to the work of Zhang et al[10], in which a norm established based on the population of the whole country as a sampling population. This is the reference value.
The Self-Rating Anxiety Scale (SAS)[11], developed by Zung in 1971, was used to assess the subjective feelings of patients with anxiety. The scale contains 20 items and the score criteria are as follows: 1 point for no or very little time; 2 points for a small amount of time; 3 points for more time; and 4 points for most of the time. The scores were added together to obtain a rough score, and multiplied by 1.25 to obtain a standard score. The higher the score, the greater the anxiety. The Cronbach’s α coefficient of the scale was 0.931.
The Self-Rating Depression Scale (SDS)[12] developed by Zung in 1965 was used to assess the subjective feelings of patients with depression, with a total of 20 items. The scoring criteria for each item were as follows: Occasionally, 1 point; sometimes, 2 points; often, 3 points; and always, 4 points. The total score is rough, and the gross score multiplied by 1.25 equals the standard score. Higher scores indicate more severe depression. The Cronbach’s α coefficient of the scale was 0.927. Both SAS and SDS Chinese norms refer to the literature of Kang[13], which provides a norm based on the population of the whole country as a sampling population, and has reference value.
Community doctors or nurses with uniform training conducted household surveys with primary caregivers or invited them to community health service institutions to complete the surveys. The researcher informed the primary caregivers of the purpose, significance, and participation method of the survey and encouraged them to provide their informed consent, which was explained to them in simple and understandable language. Subsequently, the primary caregivers completed the questionnaire. The researchers assisted those with low cultural or language abilities in completing the questionnaires. Questionnaires were completed with confidential information and collected immediately. A total of 329 questionnaires were sent out; 306 questionnaires were returned, and 300 effective questionnaires were obtained; an effective rate of 98.04%.
To reduce the risk of privacy disclosure, the respondents were surveyed anonymously. We arranged the questionnaire survey in an independent room, allowed the investigator and primary caregiver to be present during the investigation, and entered the data through double cross-entry and cross-examination.
SPSS (version 23.0) was used for the data analysis and processing. Case numbers described counting data; mean ± standard deviation describes measurement data tested by a line test or an F-test; a Pearson’s correlation was used to analyze correlation, a multiple linear regression explored risk factors, and receiver operator characteristic curve (ROC) and area under the curve (AUC) predicted ability evaluation; Test level: α = 0.05.
Compared with the Chinese norm, the objective support, subjective support, support utilization, and total scores of AMI caregivers were lower (P < 0.05) (Table 1).
| SSRS items | SSRS score (n = 300) | Chinese norm (n = 3342) | t value | P value |
| Objective support | 7.05 ± 1.6 | 9.1 ± 3.0 | 11.690 | < 0.001 |
| Subjective support | 16.9 ± 5.0 | 23.5 ± 4.3 | 25.110 | < 0.001 |
| Support utilization | 4.7 ± 1.3 | 7.8 ± 2.0 | 26.350 | < 0.001 |
| Total scores of AMI caregivers | 28.56 ± 5.31 | 40.5 ± 2.8 | 64.230 | < 0.001 |
Compared with the Chinese norm, the scores of SAS and SDS among caregivers of patients with AMI were higher (P < 0.05) (Table 2).
| Items | Scores (n = 300) | Chinese norm (n = 1338) | t value | P value |
| SAS | 41.26 ± 6.58 | 29.78 ± 10.07 | 18.860 | < 0.001 |
| SDS | 44.16 ± 7.54 | 33.46 ± 8.55 | 20.000 | < 0.001 |
There were no differences in the SSRS scores among different age groups, gender, education level, marital status, relationship with patients, monthly family income, caregiving experience, number of other caregivers, age of patients, time from onset to admission, or Killip rating of patients (P > 0.05); however, the SSRS scores of female caregivers were higher than those of male caregivers (P < 0.05) (Table 3).
| Characteristics | Cases | SSRS scores | t/F value | P value |
| Age | 1.317 | 0.189 | ||
| < 60 yr | 229 | 29.47 ± 6.96 | ||
| ≥ 60 yr | 71 | 28.25 ± 6.34 | ||
| Gender | 2.123 | 0.035 | ||
| Female | 172 | 29.47 ± 6.96 | ||
| Male | 128 | 27.89 ± 5.49 | ||
| Education levels | 1.172 | 0.311 | ||
| Junior high school and below | 83 | 28.96 ± 7.16 | ||
| High school or technical secondary school | 100 | 30.07 ± 6.24 | ||
| College or above | 117 | 28.71 ± 6.98 | ||
| Marital status | 3.382 | 3.382 | ||
| Never married | 80 | 28.44 ± 8.03 | ||
| Married | 153 | 27.42 ± 5.45 | ||
| Divorced or widowed | 67 | 29.84 ± 6.25 | ||
| Relationship with patients | 0.8741 | 0.874 | ||
| Mate | 105 | 27.98 ± 5.67 | ||
| Parent | 98 | 27.76 ± 6.70 | ||
| Sons and daughters | 65 | 29.09 ± 7.09 | ||
| Other | 32 | 29.28 ± 7.11 | ||
| Monthly family income | 0.607 | 0.546 | ||
| < 5000 RMB | 96 | 28.72 ± 6.85 | ||
| 5000–10000 RMB | 128 | 27.95 ± 5.39 | ||
| > 10000 RMB | 76 | 28.79 ± 6.76 | ||
| Caregiving experience | 0.149 | 0.882 | ||
| No | 202 | 29.29 ± 7.46 | ||
| Yes | 98 | 29.16 ± 6.30 | ||
| Number of other caregivers | 1.036 | 1.036 | ||
| 0 | 55 | 29.62 ± 6.15 | ||
| 1 or 2 | 157 | 28.65 ± 7.003 | ||
| ≥ 3 | 88 | 27.95 ± 6.67 | ||
| Age of patients | 0.571 | 0.568 | ||
| < 60 yr | 221 | 28.63 ± 7.42 | ||
| ≥ 60 yr | 79 | 29.17 ± 6.59 | ||
| Time from onset to admission | 0.683 | 0.495 | ||
| < 10 h | 114 | 29.21 ± 6.64 | ||
| ≥ 10 h | 186 | 28.64 ± 7.23 | ||
| Killip rating of patients | 1.065 | 0.288 | ||
| Level 1 or 2 | 221 | 28.82 ± 7.15 | ||
| Level 3 or 4 | 79 | 27.84 ± 6.64 |
Through the Pearson correlation analysis, objective support, subjective support, support utilization, and total SSRS scores were found to be negatively correlated with SAS (r = -0.414, -0.460, -0.416, -0.535, respectively) and SDS scores (r = -0.463, -0.379, -0.349, -0.472, respectively) (P < 0.05) (Table 4).
| SSRS items | SAS score | SDS score | ||
| r value | P value | r value | P value | |
| Objective support | -0.414 | < 0.001 | -0.463 | < 0.001 |
| Subjective support | -0.460 | < 0.001 | -0.379 | < 0.001 |
| Support utilization | -0.416 | < 0.001 | -0.349 | < 0.001 |
| Total SSRS score | -0.535 | < 0.001 | -0.472 | < 0.001 |
Among the 300 AMI caregivers, 56 cases (18.67%) had a low level of support function (SSRS ≤ 22 points). We used the support function (1 = low level, 0 = medium-high level) as the dependent variable and the characteristic indicators as self-variables (assigned values are shown in Table 5) of the logistic regression model analysis. SAS and SDS were independent determinants of low support function among AMI caregivers, regardless of adjustment for other variables (P < 0.05) (Table 6).
| Independent variable | Assignment |
| Age | 0 = < 60 yr, 1 = ≥ 60 yr |
| Gender | 0 = female, 1 = male |
| Education levels | 0 = junior high school and below, 1 = high school or technical secondary school, 2 = college or above |
| Marital status | 0 = spinsterhood, 1 = married, 2 = divorced or widowed |
| Relationship with patients | 0 = mate, 1 = parent, 2 = sons and daughters, 3 = other |
| Monthly family income | 0 = < 5000 RMB, 1 = 5000–10000 RMB, 2 = > 10000 RMB |
| Caregiving experience | 0 = no, 1 = yeas |
| Number of other caregivers | 0 = 0, 1 = 1 or 2, 2 = ≥ 3 |
| Age of patients | 0 = < 60 yr, 1 = ≥ 60 yr |
| Time from onset to admission | 0 = < 10 h, 1 = ≥ 10 h |
| Killip rating of patients | 0 = level 1 or 2, 1 = level 3 or 2 |
| Independent variable | B | SE | Wals | P value | OR | 95% CI | |
| Lower limit | Upper limit | ||||||
| No other variables were adjusted | |||||||
| SAS | 0.177 | 0.032 | 30.813 | < 0.001 | 1.194 | 1.121 | 1.271 |
| SDS | 0.070 | 0.026 | 7.288 | 0.007 | 1.072 | 1.019 | 1.128 |
| Constant | -12.392 | 1.723 | 51.741 | < 0.001 | < 0.001 | ||
| After adjusting for other variables | |||||||
| SAS | 0.193 | 0.035 | 30.566 | < 0.001 | 1.213 | 1.133 | 1.300 |
| SDS | 0.068 | 0.028 | 6.008 | 0.014 | 1.071 | 1.014 | 1.131 |
| Age | -0.261 | 0.488 | 0.287 | 0.592 | 0.770 | 0.296 | 2.003 |
| Gender | 0.133 | 0.395 | 0.113 | 0.737 | 1.142 | 0.527 | 2.477 |
| Education levels | 0.550 | 0.760 | |||||
| High school or technical secondary school | 0.298 | 0.452 | 0.434 | 0.510 | 1.347 | 0.555 | 3.269 |
| College or above | -0.044 | 0.449 | 0.010 | 0.922 | 0.957 | 0.397 | 2.306 |
| Marital status | 0.140 | 0.932 | |||||
| Married | 0.091 | 0.535 | 0.029 | 0.864 | 1.096 | 0.384 | 3.127 |
| Divorced or widowed | -0.073 | 0.462 | 0.025 | 0.875 | 0.930 | 0.376 | 2.298 |
| Relationship with patients | 1.974 | 0.578 | |||||
| Parent | 0.253 | 0.694 | 0.133 | 0.715 | 1.288 | 0.331 | 5.019 |
| Sons and daughters | 0.759 | 0.699 | 1.179 | 0.278 | 2.135 | 0.543 | 8.400 |
| Other | 0.339 | 0.728 | 0.217 | 0.641 | 1.404 | 0.337 | 5.848 |
| Monthly family income | 3.042 | 0.218 | |||||
| 5000–10000 RMB | 0.453 | 0.462 | 0.960 | 0.327 | 1.573 | 0.636 | 3.893 |
| > 10000 RMB | -0.281 | 0.519 | 0.293 | 0.588 | 0.755 | 0.273 | 2.087 |
| Caregiving experience | -0.294 | 0.399 | 0.540 | 0.462 | 0.746 | 0.341 | 1.631 |
| Number of other caregivers | 1.015 | 0.602 | |||||
| 1 or 2 | 0.351 | 0.552 | 0.406 | 0.524 | 1.421 | 0.482 | 4.188 |
| ≥ 3 | 0.416 | 0.418 | 0.991 | 0.320 | 1.515 | 0.668 | 3.435 |
| Age of patients | -0.051 | 0.439 | 0.013 | 0.908 | 0.950 | 0.402 | 2.249 |
| Time from onset to admission | -0.008 | 0.385 | 0.000 | 0.983 | 0.992 | 0.467 | 2.108 |
| Killip rating of patients | -0.172 | 0.424 | 0.164 | 0.685 | 0.842 | 0.367 | 1.933 |
| Constant | -13.699 | 2.070 | 43.780 | < 0.001 | < 0.001 | — | — |
The AUC of the SAS and SDS for predicting AMI caregivers with low social support function was 0.84, sensitivity was 67.9 and 71.4, and specificity was 84.0 and 70.9, respectively (Table 7 and Figure 1).
| Test result variable | AUC | SE | P value | 95%CI | Sensitivity (%) | Specificity (%) | Optimum cutoff value |
| SAS | 0.84 | 0.84 | < 0.001 | 0.737, 0.872 | 67.9 | 84.0 | 45.5 |
| SDS | 0.84 | 0.84 | < 0.001 | 0.655, 0.807 | 71.4 | 70.9 | 47.5 |
At present, the mental health outlook of family caregivers of patients with AMI in China is not optimistic, which directly affects their caring ability. The poor caring ability of caregivers not only affects the condition and prognosis of patients with AMI but also affects their physical and mental health. Therefore, it is necessary to explore the relationship between the social support function of primary caregivers, their anxiety, and their depression.
The occurrence of AMI affects not only patients, but also their families and caregivers[14]. Compared with the norms in China, caregivers’ objective support, subjective support, support utilization, and total SSRS scores were lower, while the SAS and SDS scores were higher. This indicates that the social support function of primary caregivers was generally low, and that negative emotions of anxiety and depression were more common, which should be considered. These results confirm those of previous studies[15,16]. The social support function of primary caregivers was generally low, which may be due to an imperfect medical security system and deficiencies in follow-up and community nursing, resulting in less social support for primary caregivers. Additionally, problems such as drug side effects and social discrimination can indirectly lead to primary caregivers’ self-isolation and reluctance to seek outside help, thereby greatly reducing the availability of social support. Good social support stems from the need for spiritual comfort and support from family, friends, and community. This situation serves as a warning to medical staff to pay attention to social support, assist primary caregivers in establishing social support systems, and enhance their social support functions.
Anxiety is defined as an inner restlessness and fear with no obvious objective causes, whereas depression is defined as persistent low mood in terms of clinical characteristics of the state of mind. The long-term care of patients with AMI undergoing interventional surgery negatively affects the mental health of their primary caregivers. Because AMI is often associated with varying degrees of dysfunction after surgery, the primary caregiver must provide frequent in-bed turning and back-patting to prevent bedsores and transfer patients between beds and wheelchairs. The primary caregiver takes care of the patient in various aspects, such as daily activities, daily living, and diet, and expends a lot of physical strength, time, and energy, which is extremely costly for the body and mind of the primary caregiver and must be maintained for a long time. Primary caregivers also face personality changes in patients with AMI, which will produce psychological reactions such as helplessness, depression, anger, loneliness, and boredom during the care process, affecting normal emotional functions. Patients who have not fully recovered after surgery may relapse[17]; moreover, their primary caregivers must consider both the patient’s condition and the financial burden it brings. Such repeated worries aggravate anxiety and depression.
Social support refers to the help people receive from society or others through their social networks; it includes objective support, subjective support, and support utilization. According to the results of our Pearson’s correlation analysis, objective support, subjective support, support utilization, and total SSRS scores were significantly negatively correlated with SAS and SDS scores, suggesting that with the increase in anxiety and depression among primary caregivers of patients with AMI, their social support function is lower, which is consistent with some existing research results[18,19]. Further, our multiple linear regression analysis found that the SAS score [odds ratio (OR) = 1.194] and SDS score (OR = 1.072) were independent influencing factors of low social support function in primary caregivers; these two indicators could accurately predict the risk of low social support, and the sensitivity and specificity of the prediction reached more than 65%. The results showed that, after excluding other interfering factors, the lower the anxiety and depression experienced by the primary caregiver, the stronger the social support function. A possible explanation for this effect is that the lower the social support function of the primary caregiver, the greater the caring burden[20], and the more likely it is to produce anxiety and depression. Research also shows that good social support can not only promote the physical health of caregivers, but also effectively relieve their depression and anxiety[13]. According to research by the Chinese Academy of Social Sciences, social support can not only improve the psychological satisfaction of the body, but also alleviate its negative emotions[21]. Therefore, the community should not only pay attention to the primary caregivers of AMI patients undergoing interventional surgery, but should also strengthen the care and help of caregivers by providing adequate psychological support and encouragement. Family visits, caregiver experience exchange platforms, rehabilitation guidance, and other measures can reduce the burden on caregivers, improve the mental health of caregivers and patients, and achieve a win–win outcome.
The limitations of this study is that it is a single-center study, and the results can only reflect part of the population; therefore, whether it can be generalized to the general population is unknown. Further, the inclusion of characteristic indicators of primary caregivers is limited, meaning that potential impact indicators may have been overlooked. Therefore, future studies should include multi-center data and add characteristic indicators to enhance the reliability of the results of this study.
The social support function of the primary caregiver of patients with AMI after interventional therapy was low and negatively correlated with anxiety and depression of the primary caregiver. For primary caregivers with anxiety and depression, timely attention and providing a deep examination of underlying issues should be provided to reduce adverse emotional distress, so that the caregiver can maintain a happy mood and implement care.
After interventional therapy, most patients need care at home, from their caregivers. The social support function of primary caregivers is an important factor affecting the quality of care and prognosis of patients. Primary caregivers often experience varying degrees of anxiety and depression.
It is necessary to understand the correlation indicators of primary caregivers’ social support functions to better guide clinical interventions. Considering that primary caregivers tend to have different levels of anxiety and depression, we speculate that their social support function may be related to anxiety and depression.
To explore the relationship between anxiety, depression, and the social support function of primary caregivers of patients with acute myocardial infarction (AMI) undergoing interventional surgery.
Investigate the primary caregivers of AMI patients undergoing interventional surgery using the Social Support Rating Scale (SSRS), Self-Rating Anxiety Scale (SAS), and Self-Rating Depression Scale (SDS). The correlation between the SSRS and SAS or SDS was evaluated using a Pearson’s correlation analysis, multiple linear regression, receiver operator characteristic curve (ROC), and area under the curve (AUC).
The SSRS was negatively correlated with the SAS and SDS scores. SAS and SDS were independent factors for low SSRS and could predict the risk of low SSRS.
The social support function of primary caregivers of AMI patients undergoing interventional surgery is associated with anxiety and depression.
Based on the Pearson’s correlation analysis, multiple linear regression, ROC, and AUC, we comprehensively analyzed the correlation between the SSRS, SAS, and SDS scores of primary caregivers of patients with AMI who underwent interventional surgery, confirming that the social support function of primary caregivers is closely related to anxiety and depression, which is instructive for clinical intervention.
Conflict of interest statement: The authors declare no conflict of interest.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Knas M, Poland; Quansah F, Ghana S-Editor: Lin C L-Editor: A P-Editor: Chen YX
| 1. | Henry TD, Tomey MI, Tamis-Holland JE, Thiele H, Rao SV, Menon V, Klein DG, Naka Y, Piña IL, Kapur NK, Dangas GD; American Heart Association Interventional Cardiovascular Care Committee of the Council on Clinical Cardiology; Council on Arteriosclerosis, Thrombosis and Vascular Biology; and Council on Cardiovascular and Stroke Nursing. Invasive Management of Acute Myocardial Infarction Complicated by Cardiogenic Shock: A Scientific Statement From the American Heart Association. Circulation. 2021;143:e815-e829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 150] [Article Influence: 37.5] [Reference Citation Analysis (0)] |
| 2. | Boyanpally A, Cutting S, Furie K. Acute Ischemic Stroke Associated with Myocardial Infarction: Challenges and Management. Semin Neurol. 2021;41:331-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Kim YH, Her AY, Jeong MH, Kim BK, Hong SJ, Kim S, Ahn CM, Kim JS, Ko YG, Choi D, Hong MK, Jang Y. Prediabetes versus type 2 diabetes mellitus based on pre-percutaneous coronary intervention thrombolysis in myocardial infarction flow grade in patients with ST-segment elevation myocardial infarction after successful newer-generation drug-eluting stent implantation. Diab Vasc Dis Res. 2021;18:1479164121991505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Xiao P, Zhou Y. Factors associated with the burden of family caregivers of elderly patients with femoral neck fracture: a cross-sectional study. J Orthop Surg Res. 2020;15:234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Li FY, Jiao NJ, Zhu SH, Guo K. Influence of supportive psychological intervention on social support and care burden of family members of patients with coronary heart disease undergoing percutaneous coronary intervention. Zhongguo Yiyao Daobao. 2022;19:163-166. [DOI] [Full Text] |
| 6. | Wang HN, Li J. Effects of peer support education based on IMB model in main caregivers of elderly patients with myocardial infarction. Zhonghua Xiandai Huli Zazhi. 2021;27:4149-4152. [DOI] [Full Text] |
| 7. | Yang TT, Zhao ZJ. The effect of social support intervention on the care of the family members of patients with acute myocardial infarction. Zhonghua Quanke Yixue. 2018;16:813-815+819. [DOI] [Full Text] |
| 8. | Mitsis A, Gragnano F. Myocardial Infarction with and without ST-segment Elevation: a Contemporary Reappraisal of Similarities and Differences. Curr Cardiol Rev. 2021;17:e230421189013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 9. | Li Z, Ge J, Feng J, Jiang R, Zhou Q, Xu X, Pan Y, Liu S, Gui B, Wang Z, Zhu B, Hu Y, Yang J, Wang R, Su D, Hashimoto K, Yang M, Yang C, Liu C. Less Social Support for Patients With COVID-19: Comparison With the Experience of Nurses. Front Psychiatry. 2021;12:554435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Zhang R, Liu XM, Lai YL. Effect of comprehensive intervention on depression and anxiety in relatives of schizophrenic patients. Linchuang Jingshen Yixue Zazhi. 2018;28:256-258. [DOI] [Full Text] |
| 11. | Hou YJ, Li YJ, Wang X, Hui NN, Zhu HL, Ma M, Zhang ZX, Wang MX. Relationship of college students' risk perception of COVID-19 and their anxiety and depression: A moderated mediation model. Xi'an Jiaotong Daxue Xuebao Yixueban. 2023;44:177-184. [DOI] [Full Text] |
| 12. | Posluszny DM, Bovbjerg DH, Syrjala KL, Agha M, Dew MA. Correlates of anxiety and depression symptoms among patients and their family caregivers prior to allogeneic hematopoietic cell transplant for hematological malignancies. Support Care Cancer. 2019;27:591-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Kang JM, Chen XY, Chen L, Wu CK, Deng YL, Li WY. Analysis on relativity between social support and quality of life of family caregivers of patients with stroke sequelae. Zhongguo Yiyao Daobao. 2020;17:57-60. |
| 14. | Qin YP. The application of family nursing based on timing theory in AMI patients and its influence on family caring ability and quality of life of patients. Guoji Hulixue Zazhi. 2019;38:3832-3834. [DOI] [Full Text] |
| 15. | Lan K, Pan YL, Wang Q, Chen S. Analysis of influencing factors of caregiver preparedness at discharge of patients with chronic heart failure based on the individual and family self-management theory. Zhongguo Shiyong Huli Zazhi. 2023;39:699-706. [DOI] [Full Text] |
| 16. | Verkleij M, Appelman I, Altenburg J, Twisk J, Quittner AL, Haarman E. Anxiety and depression in Dutch patients with primary ciliary dyskinesia and their caregivers: associations with health-related quality of life. ERJ Open Res. 2021;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 17. | Ma LX, Chen Y, Kou J, Sui YJ. Two-year prognosis of patients with acute myocardial infarction after interventional operation and its influencing factors. Hainan Yixue. 2022;33:2048-2051. [DOI] [Full Text] |
| 18. | Lin C, Tong Y, Bai Y, Zhao Z, Quan W, Liu Z, Wang J, Song Y, Tian J, Dong W. Prevalence and correlates of depression and anxiety among Chinese international students in US colleges during the COVID-19 pandemic: A cross-sectional study. PLoS One. 2022;17:e0267081. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 19. | Yang J, Hou HR, Tan JP, Wang XX, Xu J. Burden and influencing factors of caregivers for patients with Alzheimer's disease. Zhongguo Linchuang Baojian Zazhi. 2019;22:170-173. [DOI] [Full Text] |
| 20. | Jin M, Li L, Yao JL. Role of Social Support in the Quality of Life and Burden of Care of Primary Caregivers of Pa-tients with Liver Cancer. -Jiefangjun Huli Zazhi. 2020;37:65-68, 75. [DOI] [Full Text] |
| 21. | Zhang H, Jiang W, Li YJ. Correlation analysis of postoperative cardiac transplant recipients of social support and anxiety depression status and physical function. Zhongguo Xinxueguanbing Yanjiu. 2019;17:420-425. [DOI] [Full Text] |