Published online Nov 19, 2023. doi: 10.5498/wjp.v13.i11.912
Peer-review started: September 12, 2023
First decision: September 25, 2023
Revised: October 9, 2023
Accepted: October 27, 2023
Article in press: October 27, 2023
Published online: November 19, 2023
Processing time: 65 Days and 23.7 Hours
The psychological state of patients with post stroke limb movement disorders undergoes a series of changes that affect rehabilitation training and recovery of limb motor function.
To determine the correlation between motor rehabilitation and the psychological state of patients with limb movement disorders after stroke.
Eighty patients with upper and lower limb dysfunction post stroke were retro
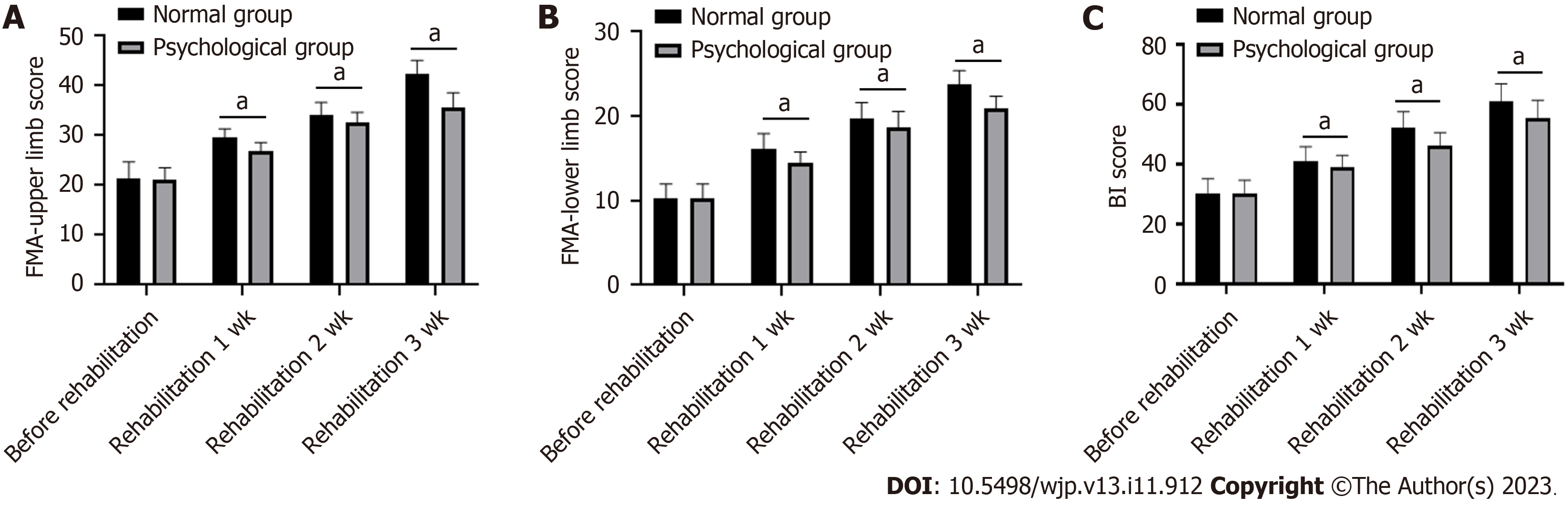
After 1, 2, and 3 wk of rehabilitation, both the Fugl-Meyer assessment and Barthel index scores improved compared to their respective baseline scores (P < 0.05). A greater degree of improvement was observed in the normal group compared to the psychological group (P < 0.05). There was a negative correlation between negative emotions and limb rehabilitation (-0.592 ≤ r ≤ -0.233, P < 0.05), and between negative emotions and daily living ability (-0.395 ≤ r ≤ -0.199, P < 0.05).
There is a strong correlation between motor rehabilitation and the psychological state of patients with post stroke limb movement disorders. The higher the negative emotions, the worse the rehabilitation effect.
Core Tip: Stroke, also known as a cerebrovascular accident, is characterized by an acute and rapid onset and is the most common cerebrovascular disease. Stroke can cause limb dysfunction, resulting in functional limitations. Some people may experience a series of changes in their psychological state after illness, which affects rehabilitation training and recovery of limb function. The results of this study showed a strong correlation between the recovery of limb function with rehabilitation and psychological state of stroke patients. Therefore, it is necessary to pay close attention to psychological changes during rehabilitation, and implement timely adjustments and interventions for future rehabilitation.
- Citation: Li XW, Xin YF, Chang AH, Zhang XG, Weng Y, Yang JH, Fu QZ. Correlation study between motor rehabilitation level and psychological state in patients with limb movement disorders after stroke. World J Psychiatry 2023; 13(11): 912-918
- URL: https://www.wjgnet.com/2220-3206/full/v13/i11/912.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i11.912
Stroke can be subdivided into cerebral hemorrhage and cerebral infarction[1]. It is a clinical emergency that causes ischemic damage to the brain tissue due to the blockage or sudden rupture of small- and medium-sized blood vessels in the brain. According to the most recently published statistics, stroke ranks first as the leading cause of mortality in China, and is the main cause of accidental deaths, except for car accidents and falls from high altitudes[2]. Patients with stroke may experience swallowing and limb dysfunction, and in severe cases, they may lose their ability to take care of themselves, increasing the burden on their families and taking a serious negative toll on their mental health and resilience[3]. Therefore, it is necessary to pay close attention to psychological changes during rehabilitation, and implement timely adjustments and interventions for future rehabilitation and restoring the patient’s quality of life.
The current medical disease model incorporates biological, psychological, and social factors. Medical workers should shift their treatment methods from traditional treatments to biological, psychological, and social models[4]. As the patient is anxious and worried when seeking medical treatment, the complex psychological effects can have pathogenic consequences[5]. Therefore, we should pay attention to the patients’ psychological states, carefully observe their psychological reactions, and implement targeted psychological interventions based on their characteristics[6]. Related studies have shown that psychological interventions can reduce anxiety, depression, and fear in patients by reducing the heart rate, blood pressure, and catecholamine levels in blood and urine, and alleviate tension during exercise[7]. It can inhibit the activity of nociceptive neurons in the central area of the cerebral cortex, reduce their excitability, increase the pain threshold, and alleviate pain[8].
According to previous reports, there is a correlation between recovery and psychological state of the patient[9]. The better the patient’s psychological state, the better will be their limb function recovery, and their quality of life will also improve accordingly[10]. This article mainly studied the correlation between the recovery of limb function owing to rehabilitation and psychological resilience in elderly stroke patients to provide a reference for psychological nursing and quality of life intervention in elderly stroke patients.
Eighty patients with limb dysfunction after stroke who were admitted to the First Affiliated Hospital of Henan University of Science and Technology from May 2022 and May 2023 were retrospectively selected. The inclusion criteria were as follows: (1) A confirmed diagnosis of stroke on head computed tomography or magnetic resonance imaging according to the diagnostic criteria proposed by the American Heart Association/American Stroke Association for stroke[11]; (2) The course of treatment is more than 21 d, and the condition is stable without recurrence; (3) The patient has a clear sense of autonomy and good cognitive ability; and (4) Patients with limb dysfunction after stroke. The exclusion criteria included: (1) Other serious cardiovascular and cerebrovascular diseases; (2) Patients with malignant tumors; (3) Patients with mental illness; (4) Patients with unstable vital signs; (5) Patients with previous stroke but residual upper and lower limb dysfunction and other sequelae; and (6) Patients with a history of surgery, fractures, arthritis, or pain that affects the recovery of upper and lower limb function. Based on the Hospital Anxiety and Depression Scale (HADS) scores before the start of rehabilitation, the patients were divided into the psychological group (those with HADS scores ≥ 8) and the normal group (those with HADS scores < 8).
The HADS index was used to evaluate the psychological state of patients[12]. This is a 14-item scale with seven items rated as anxiety and seven items rated as depression. If the HADS score is ≥ 8, it indicates symptoms of anxiety and depression. If the HADS score is < 8, the patient’s psychological state is considered normal.
The Fugl-Meyer assessment (FMA) was used to evaluate the patient’s upper and lower limb motor function[13]. There were 50 items with a total maximum score of 100 points. The upper limb score consists of 33 items and 66 points. The lower upper limb score consists of 17 items and with a total of 34 points.
The Barthel index (BI) for activities of daily living[14] was used to assess the patients’ daily living abilities. The BI includes 10 items, with a total of 100 points. Except for walking on flat ground and bed-to-chair transfer, the full score was 15 points, whereas the full score for grooming and bathing was 5 points. The remaining items had a total score of 10 points.
SPSS 20.0 was used to statistically analyze the data. The measurement data were represented by (mean ± SD), and the t-test was used for intergroup comparisons. The counting data is represented in the form of percentage, and χ2 is used for the intergroup comparisons. Pearson’s correlation analysis was used to analyze the relationship between the rehabilitation of limb function and the psychological status of patients as well as the relationship between daily living ability and psychological status. Statistical significance was set at P < 0.05.
As shown in Table 1, there were no differences between gender (male, 60% vs 62.5%), age (65.33 ± 4.59 vs 65.90 ± 4.91), body mass index (25.43 ± 2.08 vs 25.86 ± 1.74), and course of disease (27.93 ± 7.11 vs 27.83 ± 7.88) between the normal and psychological groups (P > 0.05). The results showed that most stroke patients with motor disorders were classified as elderly and the duration of the disease was between 1 and 2 mo.
| Index | Normal group (n = 40) | Psychological group (n = 40) | t/χ2 | P value |
| Gender (male, %) | 24 (60%) | 25 (62.5%) | -0.053 | 0.818 |
| Age (yr) | 65.33 ± 4.59 | 65.90 ± 4.91 | -0.541 | 0.590 |
| BMI (kg/m2) | 25.43 ± 2.08 | 25.86 ± 1.74 | -0.997 | 0.322 |
| Course of disease (d) | 27.93 ± 7.11 | 27.83 ± 7.88 | 0.060 | 0.953 |
As shown in Figures 1A and B, there was no difference in the FMA scores of the upper and lower limbs between the normal and psychological groups (P > 0.05). After 1, 2, and 3 wk of rehabilitation, the FMA scores of the upper and lower limbs improved in both groups (P < 0.05). In addition, the FMA scores of the upper and lower limbs in the normal group had more substantial improvement than those in the psychological group (P < 0.05).
Figure 1C shows that before rehabilitation, there was no difference in the BI scores between the normal and psychological groups (P > 0.05). After 1, 2, and 3 wk of rehabilitation, the BI score improved in both groups (P < 0.05), and the BI score in the normal group was higher than that in the psychological group (P < 0.05).
As shown in Table 2, there was a negative correlation between anxiety and upper, lower limb FMA scores at 1-, 2- and 3-wk post rehabilitation (P < 0.05). There was a negative correlation between depression and upper, lower limb FMA scores at 1-, 2- and 3-wk post rehabilitation (P < 0.05). These results suggested a negative correlation between negative emotions and limb rehabilitation.
| FMA score of upper limb | FMA score of lower limb | |||||
| 1 wk | 2 wk | 3 wk | 1 wk | 2 wk | 3 wk | |
| Anxiety | r = -0.341 | r = -0.339 | r = -0.592 | r = -0.288 | r = -0.289 | r = -0.454 |
| P = 0.005 | P = 0.002 | P < 0.001 | P = 0.010 | P = 0.009 | P < 0.001 | |
| Depression | r = -0.319 | r = -0.233 | r = -0.585 | r = -0.369 | r = -0.255 | r = -0.475 |
| P = 0.012 | P = 0.038 | P < 0.001 | P = 0.001 | P = 0.023 | P < 0.001 | |
There was a negative correlation between anxiety and BI scores at 2- and 3-wk post rehabilitation (P < 0.05), and there was a negative correlation between depression and BI scores at 1-, 2- and 3-wk post rehabilitation (P < 0.05) (Table 3). These results suggest a negative correlation between negative emotions and activities of daily living.
| BI score | |||
| 1 wk | 2 wk | 3 wk | |
| Anxiety | r = -0.199 | r = -0.377 | r = -0.395 |
| P = 0.077 | P = 0.001 | P < 0.001 | |
| Depression | r = -0.233 | r = -0.379 | r = -0.387 |
| P = 0.038 | P = 0.001 | P < 0.001 | |
The incidence of cerebrovascular diseases and stroke, which is the most common type of cerebrovascular disease[15], has increased annually, and they generally occur in the younger and middle-aged group[16]. Once affected by stroke, patients with mild disease may experience delayed movement, whereas those with severe disease phenotypes may experience limb dysfunction and even death. Some people may experience a series of changes in their psychological state after illness, which affects rehabilitation training and recovery of limb function[17]. Elderly people have decreased bodily functions, more comorbidities, and a strong psychological dependence on their families[18]. After a period of illness, they not only have to endure the torment of illness but also the inconveniences of life. These patients bear significant psychological pressure as a result.
Many patients find it difficult to complete role conversion in a short time; the rehabilitation training initiative is poor, the effect is not obvious, depression and pessimism appear, psychological resilience becomes affected, and it is easily complicated with acute stress disorder; that is, some separation symptoms, such as mental, movement, and personality dysfunction appear in the early stages of the illness[19]. Those with avoidance and high vigilance towards illness events deliberately avoid the facts about one’s own illness, suspect the gaze of others, are unable to control one’s emotions and temper, and are prone to irritability, anger, and poor sleep quality[20].
This study used the HADS to evaluate the psychological status of patients with limb movement disorders after stroke and to determine whether they had anxiety and depression before rehabilitation initiation. In previous studies that followed-up stroke patients, it was hypothesized that fear of pain affects post-stroke functional recovery; however, there was no correlation between the two[21]. It is recommended that patients pay attention to their fears and receive reasonable psychological interventions. Related studies suggest that anxiety and depression affect the recovery of limb function in stroke patients[22]. Our study showed that the motor function and daily living ability of stroke patients in the psychological group were lower than those in the normal group after 1-, 2-, and 3-wk of rehabilitation, indicating that anxiety and depression negatively impact the recovery of motor function and daily living ability. Further, our research showed a significant negative correlation between negative emotions such as anxiety and depression, motor function, and self-life ability. This was because patients in the psychological group had a poor psychological state and lacked the ability to withstand stress[23]. They are unable to establish a good buffer time after the illness, which is not conducive to the creation of positive emotions and is even less conducive to the recovery of upper and lower limb function after stroke[24].
Therefore, we should attach importance to the psychological state of patients before rehabilitation, and it is recommended that future studies address the following points to achieve better outcomes: Firstly, rehabilitation plans should be developed to improve patients’ quality of life, take effective psychological intervention measures, and observe and evaluate the actual effects. This may be done by equipping dedicated psychologists with the correct resources to strengthen research on the psychological status of stroke patients before rehabilitation. Secondly, optimal treatment methods should be adopted to reduce and eliminate the adverse effects of psychological factors on limb motor function before rehabilitation. Furthermore, attention should be paid to the psychological rehabilitation of patients after discharge and to strengthen follow-up procedures. Finally, the active cooperation between psychologists and rehabilitation physicians must be strengthened to minimize negative psychological impacts.
Our study has several limitations. There are many factors that affect the recovery of limb motor function, and psychological factors are only one of them. This study only considered the effects of anxiety and depression on limb motor function recovery before rehabilitation. Further research is needed to investigate the effects of other factors on recovery of limb motor function. The evaluation of various indices in this study are mostly in the form of a subjective numeric rating scale. At the same time, due to differences in language expression and understanding among ethnic minorities, there may have been errors in the measurement of each indicator. In the future, more objective indicators such as imaging findings should be used to quantify the results more accurately. This study only examined the impact of psychological factors before rehabilitation on limb motor function rehabilitation, without considering the impact of psychological factors, and it did not consider effective psychological intervention measures for adverse psychological outcomes. This must be investigated in the future. Finally, sample size of this study was small, and future multi-center studies with larger sample sizes are needed to confirm this finding.
In summary, there is a certain correlation between the psychological state of patients with limb disorders after stroke and their level of limb rehabilitation; the greater the negative emotions, the worse the rehabilitation effect. In clinical practice, healthcare workers can assist in the rehabilitation of patients’ limb functions by improving their psychological state, indirectly improving their quality of life.
The rehabilitation of limb function in patients with limb movement disorders after stroke is influenced by their psychological state.
Exploring whether healthcare workers can accelerate the recovery of limb function in stroke patients by improving their psychological state and indirectly improving their quality of life.
The aim of this study was to investigate the correlation between the level of motor rehabilitation and the psychological state of patients with limb movement disorders post stroke.
Eighty patients with limb dysfunction after stroke were retrospectively selected. The Fugl-Meyer assessment motor function and Barthel index daily living ability scales were used to investigate limb movement disorders and daily living ability, and a correlation between the two indices and psychological state was observed.
There was a negative correlation between negative emotions and limb rehabilitation and between negative emotions and daily living ability.
The better the psychological state of patients with limb movement disorders after stroke, the more significant the rehabilitation effect on limb function recovery.
When performing limb function rehabilitation in patients with limb movement disorders after stroke, it is necessary to pay attention to the patient’s psychological state. A good psychological state can accelerate recovery.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Elbeddini A, Canada; Ijomah W, United Kingdom S-Editor: Wang JJ L-Editor: A P-Editor: Xu ZH
| 1. | Tater P, Pandey S. Post-stroke Movement Disorders: Clinical Spectrum, Pathogenesis, and Management. Neurol India. 2021;69:272-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 54] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 2. | Wu S, Wu B, Liu M, Chen Z, Wang W, Anderson CS, Sandercock P, Wang Y, Huang Y, Cui L, Pu C, Jia J, Zhang T, Liu X, Zhang S, Xie P, Fan D, Ji X, Wong KL, Wang L; China Stroke Study Collaboration. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18:394-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 645] [Cited by in RCA: 1018] [Article Influence: 203.6] [Reference Citation Analysis (0)] |
| 3. | Zhang Q, Fu Y, Lu Y, Zhang Y, Huang Q, Yang Y, Zhang K, Li M. Impact of Virtual Reality-Based Therapies on Cognition and Mental Health of Stroke Patients: Systematic Review and Meta-analysis. J Med Internet Res. 2021;23:e31007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 52] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 4. | Wetzler S, Schwartz B, Wetzler S, Patel U, Counts N. Treatment of Serious Mental Illness in Medical and Mental Health Settings. Psychiatr Serv. 2020;71:789-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Smith PJ, Merwin RM. The Role of Exercise in Management of Mental Health Disorders: An Integrative Review. Annu Rev Med. 2021;72:45-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 151] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 6. | Lambert JLW, Segaert S, Ghislain PD, Hillary T, Nikkels A, Willaert F, Lambert J, Speeckaert R. Practical recommendations for systemic treatment in psoriasis according to age, pregnancy, metabolic syndrome, mental health, psoriasis subtype and treatment history (BETA-PSO: Belgian Evidence-based Treatment Advice in Psoriasis; part 1). J Eur Acad Dermatol Venereol. 2020;34:1654-1665. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 7. | Silva LAD, Doyenart R, Henrique Salvan P, Rodrigues W, Felipe Lopes J, Gomes K, Thirupathi A, Pinho RA, Silveira PC. Swimming training improves mental health parameters, cognition and motor coordination in children with Attention Deficit Hyperactivity Disorder. Int J Environ Health Res. 2020;30:584-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 8. | Cahill SM, Egan BE, Seber J. Activity- and Occupation-Based Interventions to Support Mental Health, Positive Behavior, and Social Participation for Children and Youth: A Systematic Review. Am J Occup Ther. 2020;74:7402180020p1-7402180020p28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 9. | Kristo I, Mowll J. Voicing the perspectives of stroke survivors with aphasia: A rapid evidence review of post-stroke mental health, screening practices and lived experiences. Health Soc Care Community. 2022;30:e898-e908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Ledochowski J, Desrocher M, Williams T, Dlamini N, Westmacott R. Mental health outcomes in children with acquired dystonia after basal ganglia stroke and associations with cognitive and motor outcomes. Child Neuropsychol. 2020;26:691-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Yew KS, Cheng EM. Diagnosis of acute stroke. Am Fam Physician. 2015;91:528-536. [PubMed] |
| 12. | Garaiman A, Mihai C, Dobrota R, Jordan S, Maurer B, Flemming J, Distler O, Becker MO. The Hospital Anxiety and Depression Scale in patients with systemic sclerosis: a psychometric and factor analysis in a monocentric cohort. Clin Exp Rheumatol. 2021;39 Suppl 131:34-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 13. | Crow JL, Harmeling-van der Wel BC. Hierarchical properties of the motor function sections of the Fugl-Meyer assessment scale for people after stroke: a retrospective study. Phys Ther. 2008;88:1554-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 14. | Yang H, Chen Y, Wang J, Wei H, Jin J. Activities of daily living measurement after ischemic stroke: Rasch analysis of the modified Barthel index. Medicine (Baltimore). 2021;100:e24926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 15. | Guzik A, Bushnell C. Stroke Epidemiology and Risk Factor Management. Continuum (Minneap Minn). 2017;23:15-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 214] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 16. | Doria JW, Forgacs PB. Incidence, Implications, and Management of Seizures Following Ischemic and Hemorrhagic Stroke. Curr Neurol Neurosci Rep. 2019;19:37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 17. | Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, Fisher M, Pandian J, Lindsay P. World Stroke Organization (WSO): Global Stroke Fact Sheet 2022. Int J Stroke. 2022;17:18-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 1248] [Article Influence: 416.0] [Reference Citation Analysis (0)] |
| 18. | Xiong F, Liao X, Xiao J, Bai X, Huang J, Zhang B, Li F, Li P. Emerging Limb Rehabilitation Therapy After Post-stroke Motor Recovery. Front Aging Neurosci. 2022;14:863379. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 19. | Sharififar S, Shuster JJ, Bishop MD. Adding electrical stimulation during standard rehabilitation after stroke to improve motor function. A systematic review and meta-analysis. Ann Phys Rehabil Med. 2018;61:339-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 20. | Mavaddat N, Ross S, Dobbin A, Williams K, Graffy J, Mant J. Training in positivity for stroke? A qualitative study of acceptability of use of Positive Mental Training (PosMT) as a tool to assist stroke survivors with post-stroke psychological problems and in coping with rehabilitation. NeuroRehabilitation. 2017;40:259-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Gyawali P, Chow WZ, Hinwood M, Kluge M, English C, Ong LK, Nilsson M, Walker FR. Opposing Associations of Stress and Resilience With Functional Outcomes in Stroke Survivors in the Chronic Phase of Stroke: A Cross-Sectional Study. Front Neurol. 2020;11:230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 22. | Lin RC, Chiang SL, Heitkemper MM, Weng SM, Lin CF, Yang FC, Lin CH. Effectiveness of Early Rehabilitation Combined With Virtual Reality Training on Muscle Strength, Mood State, and Functional Status in Patients With Acute Stroke: A Randomized Controlled Trial. Worldviews Evid Based Nurs. 2020;17:158-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 23. | Tsai SJ, Li CC, Tsai SM, Kao SC, Pai HC. The effect of action modules on resilience and psychological health of stroke patients: A pilot non-randomised control trial. J Clin Nurs. 2023;32:311-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 24. | Hinwood M, Ilicic M, Gyawali P, Kluge MG, Coupland K, Smith A, Nilsson M, Walker FR. Exploration of stress management interventions to address psychological stress in stroke survivors: a protocol for a scoping review. BMJ Open. 2020;10:e035592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |